Abstract
Background:
Cryptococcal meningitis (CM) is one of the deadliest opportunistic infections related to HIV/AIDS. A research gap exists surrounding the barriers to CM diagnosis, treatment delivery, and care from the healthcare provider’s perspective.
Objectives:
The purpose of this study was to elucidate provider’s behaviors, to identify barriers and facilitators to diagnose and treat CM, and to assess their knowledge of CM, cryptococcal screening, and treatment.
Design, setting, and participants:
A convergent mixed-methods study among twenty healthcare providers who provided CM patient referrals to Lira Regional Referral Hospital in Lira, Uganda.
Methods:
Surveys and interviews were conducted to obtain information from healthcare providers who referred CM patients to Lira Regional Referral Hospital from 2017 to 2019. Questions related to provider education, knowledge, barriers to CM care, and patient education were inquired to understand the providers’ perspectives.
Results:
Nurses had the least amount of CM knowledge with half knowing the cause of CM. Approximately half the participants knew about CM transmission, but only 15 % knew the duration of CM maintenance therapy. Most participants (74 %) last had education regarding CM during didactic training. In addition, 25 % disclosed they never educate patients due to time constraints (30 %) and lack of knowledge (30 %). Nurses (75 %) were least likely to provide patient education. Most participants acknowledged their lack of CM knowledge and attributed it to a lack of education and perceived inexperience with CM.
Conclusions:
Providers’ gaps in knowledge due to the lack of education and experience contributes to decreased patient education, and the lack of access to appropriate supplies affects their provision for CM diagnosis, treatment, and care. These results can guide evidence-based interventions to improve health providers’ knowledge. Recommendations for standardized CM education should be developed for both providers and patients in collaboration with professional boards and the Uganda Ministry of Health.
Keywords: Cryptococcal meningitis, Mixed methods, Healthcare providers, Barriers to care, Uganda
1. Introduction
Cryptococcal meningitis (CM) is a serious opportunistic infection commonly associated with HIV/AIDS which kills 181,000 people annually (Center for Disease Control (CDC), 2018). Most of the current research on CM focuses on determining the best medication combinations and therapies to improve mortality and morbidity. However, little research has been conducted with the people at the front line of service: the healthcare providers. There is a lack of information about the barriers providers face when caring for patients with CM. Understanding provider experiences will provide crucial information on existing service gaps and how to improve CM care at local health facilities, which are the patient’s first point of entry for health care. (Link et al., 2022b) Current studies support the need for ongoing education for health providers and confirm that CM education is being conducted in some areas (Faini et al., 2019; Lofgren et al., 2018; Meiring et al., 2016; Nalintya et al., 2018), but the level of knowledge and frequency of CM education for providers is unknown in rural areas such as northern Uganda.
2. Background
A recent analysis of a CM diagnosis and treatment program at Lira Regional Referral Hospital found that 34.1 % of patients were referred from surrounding health facilities, (Link et al., 2022a), while 52.5 % diagnosed with CM sought treatment, ≥3 times at local health facilities before hospitalization at Lira Regional Referral Hospital (Link et al., 2022b). Among participants who died, 70 % sought care ≥3 times, while those who survived, 35 % sought care ≥3 times (Link et al., 2022b). These multiple visits suggest that misdiagnosis or missed diagnosis contributed to delays in CM care, leading to poorer outcomes. Only 20 % of referred CM patients received their diagnosis before they arrived at Lira Regional Referral Hospital (Link et al., 2022b). Outcomes could be improved if patients were diagnosed earlier at local health centers to avoid delays in treatment.
A case study of a patient in northern Uganda admitted for recurrent CM illustrates some of the barriers associated with CM care. At the time of readmission, it was reported that “[the patient] was not aware of the cause, treatment options, duration, or the need for long-term/life-long suppression therapy for her condition” (Bongomin and Atikoro, 2018). This highlights the lack of patient knowledge of CM and emphasizes the barriers that surround patient education. Our study investigated the providers’ practices and barriers to patient education on CM. It also inquired about the experiences providers had regarding their own CM education, knowledge, and practices around diagnosis and treatment to better understand and identify the gaps in providing quality and timely CM care.
3. Methods
A convergent mixed methods design was used to collect qualitative and quantitative data. Surveys were conducted first, immediately followed by semi-structured interviews. This design allowed for responses that either expanded, supported, or contradicted the responses between the qualitative and quantitative data by using interviews to further probe and investigate differences.
3.1. Theoretical framework
The Integrated Behavioral Model (IBM) was used as the theoretical framework which guided surveys and interview questions to assess the key behavioral constructs and factors related to diagnosis, treatment, referral, education, and overall CM care (Fig. 1). The model asserts that intention or motivation are components of predicting behavior (Daniel Montaño and Kasprzyk, 2008, 2015) which integrates factors of behavioral intention, such as the environment, habit, knowledge, and saliency of the behavior while incorporating the baseline theoretical constructs of attitude, perceived norms, and personal agency (Kasprzyk et al., 1998). The model helped to categorize the qualitative data collected into specific components of participants’ behaviors as well as their perceived attitudes, norms, and agency (Fig. 2). Using this framework we were able to analyze primary themes among the different categories and synthesize larger themes which are highlighted in the results and discussion.
Fig. 1.
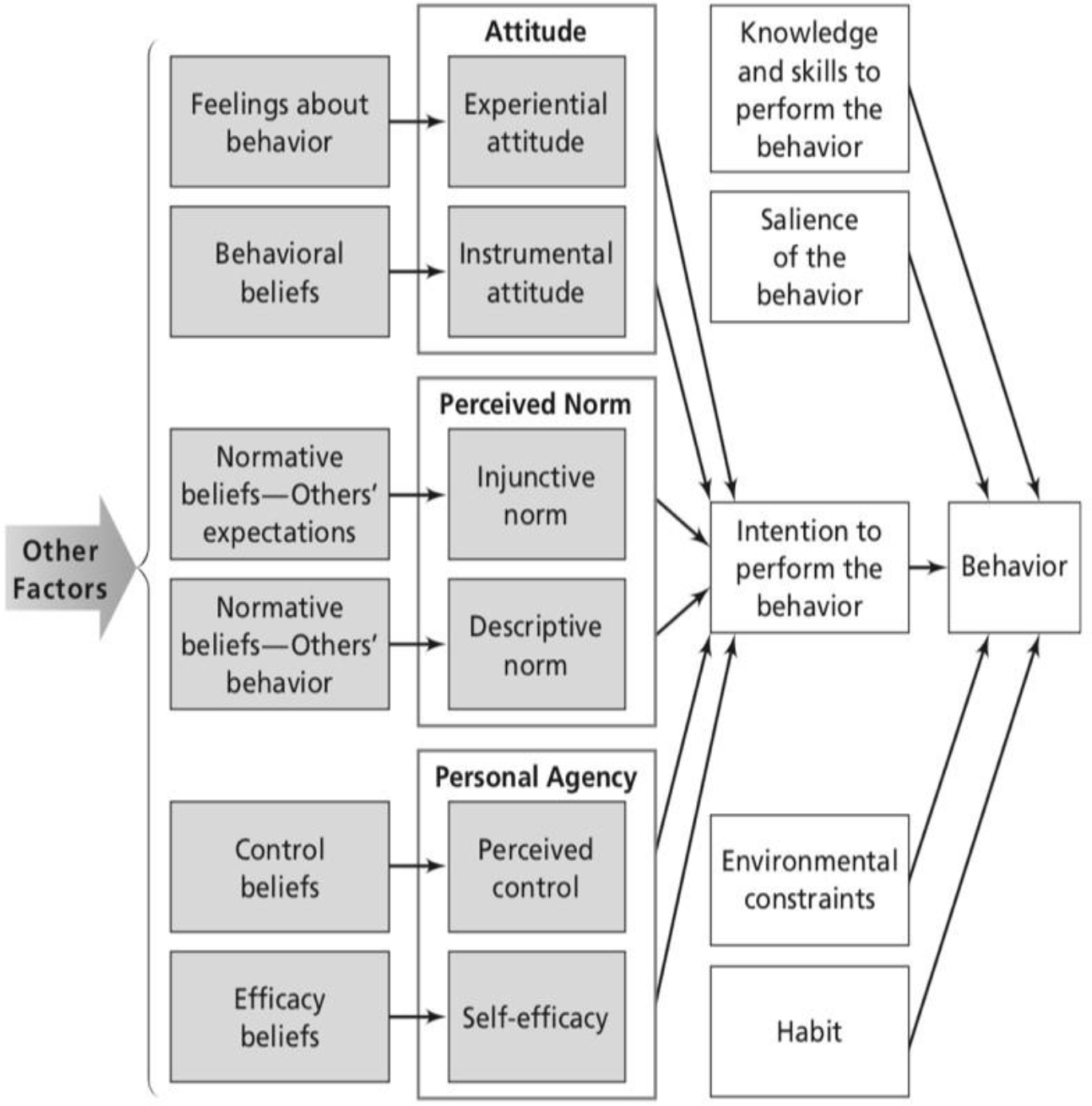
Integrated behavioral model (IBM).
Fig. 2.
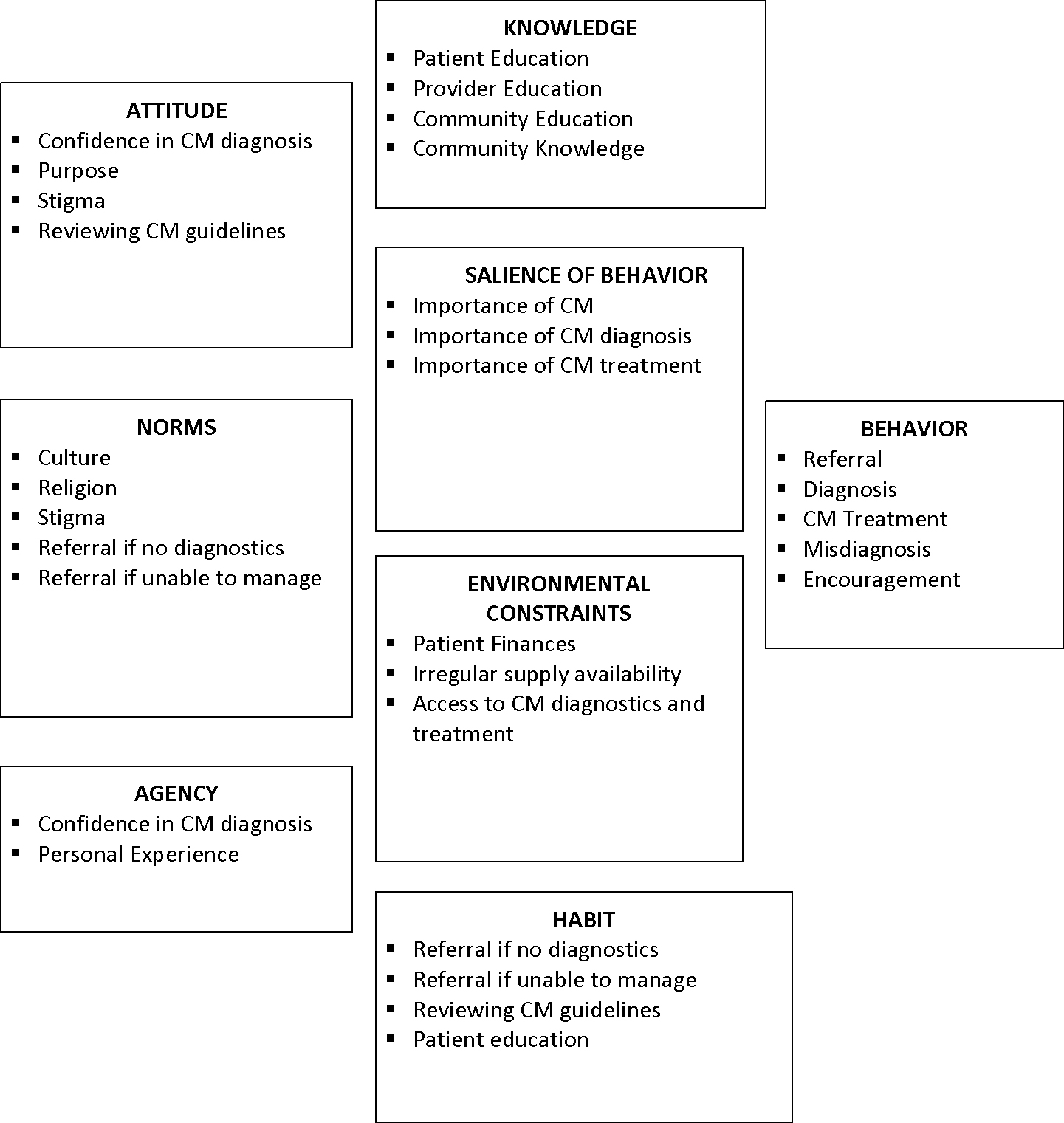
Integrated behavioral model framework for provider coding.
3.2. Setting
Lira is in the Lango subregion of rural northern Uganda and is surrounded by nine districts (Nabongo B 2019, personal communication, January 27). These districts encompass several types of health facilities including district hospitals and clinics: health centers II, III, IV, and private facilities. Health center II sites provide outpatient prevention and treatment services for approximately 500 residents, while health center IIIs provide maternity and some inpatient services, as well as basic laboratory services for a population of 20,000 people (World Health Organization (WHO), 2017). Health center II and III facilities are primarily staffed by nurses who fulfill the duties of a primary care provider when clinical officers are not present. Health center IV locations have more traditional responsibilities of general hospital care, whereas referral hospitals like Lira Regional Referral Hospital provide additional specializations in psychiatry, radiology, ophthalmology, and surgical services (World Health Organization (WHO), 2017). Nurses and allied health professionals make up the majority of the healthcare staff in the lower-level facilities, especially in rural areas, while medical officers are more commonly found in the urban areas, where they work at health center IV sites. The smaller facilities provide referrals to Lira Regional Referral Hospital, which is one of two referral hospitals in this region of Uganda (Oketch, 2012) and serves approximately 2.2 million people (Nabongo B 2019, personal communication, January 27).
3.3. Sample
3.3.1. Clinic sites
Ten health center level III and IV sites (public and private) that referred patients to Lira Regional Referral Hospital were selected for this study. These sites were purposively selected based on the number of CM patients referred to Lira Regional Referral Hospital between February 2017 and February 2019.
3.3.2. Providers
Two healthcare providers aged ≥18, who diagnose and treat patients were selected from each of the ten sites. A total of 20 healthcare providers were enrolled and agreed to participate in the surveys and interviews. At many of the sites, only two available staff were on duty due to the size of the facility.
3.4. Procedures
3.4.1. Surveys
The in-charge supervisors at each of the ten health centers were contacted by telephone as a courtesy call to explain the study and to obtain verbal consent to come to their health facility. Once onsite, the incharge identified two providers for our study staff to approach for the survey and interview. After explanations of the study were provided and consent was signed by the healthcare provider, REDCap (Research Electronic Data Capture) surveys were completed on an electronic tablet and were proctored by trained interviewers in English. All documents were uploaded to the server at the end of each day. REDCap is a secure, HIPPA compliant, web-based application that is used for creating and managing online surveys and databases (Harris et al., 2009). Information obtained from the surveys inquired about the provider’s demographics, as well as their knowledge of CM, HIV stigma, patient education, and current Ugandan guidelines for CM screening and treatment.
3.4.2. Semi-structured interviews
Semi-structured qualitative interviews using interview guides followed the surveys, and were conducted in English, and audio recorded. Qualitative interviews were conducted until data saturation was reached, and no new information was elicited. The recordings were transcribed by study staff and audits were conducted with each transcriber to verify the validity of the transcriptions. Intermittent audits of the transcription were also conducted to ensure the quality and accuracy of the transcripts.
The interviews inquired about providers’ experiences with CM patients. Specifically, providers were asked about their knowledge and education on CM, their perception of barriers to CM diagnosis and treatment, CM patient education, and recommendations to decrease barriers to improve CM outcomes and education (Appendix A). The interviews ranged from 19 to 45 min. After 20 participant interviews were conducted, no new information or themes were identified, and data saturation was reached.
3.5. Ethics approval
Regional ethics approval by the Gulu University Research Ethics Committee (GUREC-017019), national ethics approval from the Uganda National Council of Science and Technology (UNCST, SS 5151), and the University of Washington Institutional Review Board (STUDY00007770) were obtained for this study. Permission was also obtained from the Lira District Health Officer to enter the private and public health centers in Lira District. Written informed consent for study participation was completed before the commencement of the surveys on an electronic tablet using REDCap.
4. Analysis
4.1. Surveys
Descriptive statistics were used for responses from the surveys on demographic information and barriers to education, diagnosis, and treatment. Survey questions also assessed patient education practices and perceived CM knowledge among their patients. All quantitative analysis was performed using R version 3.6.0 (R Foundation for Statistical Computing, Vienna, Austria) (R Core Team, 2020).
4.2. Transcripts
Interview data were analyzed using a content analysis approach guided by the IBM and used ATLAS.ti (version 8.4) to facilitate the coding of the semi-structured interview transcripts (Scientific Software Development, 2019). Initial coding and memo writing was performed by the first author using the IBM framework as the foundation in the development of the codebook. Additional codes were added as new themes from the interviews were identified. From the codes, networks, and memos we identified major themes related to providers’ behaviors and perceptions towards education, diagnosis, and treatment for CM. A primary codebook provided continuity in coding between the coders to ensure accuracy and minimize discrepancies in coding between the PI and one additional coder. Discrepancies were resolved by discussions with the PI and the coder to understand why the transcript excerpts were coded a specific way. After further clarification, codes were either updated or left in their original form (Appendix B).
5. Results
5.1. Surveys
5.1.1. Provider Demographics
Most participants were male (60 %) with an average age of 32.7 years (Table 1). The cadre of health providers was nurses (40 %) (2 comprehensive, 6 enrolled), medical officers (25 %), and clinical officers (35 %). Clinical officers are providers that have similar roles and responsibilities as physician assistants in the United States. Enrolled nurses have two years of training in nursing, while comprehensive nurses have two years of training in both nursing and midwifery. More nurses (87.5 %) worked in health center III facilities as compared to 60 % of medical officers and 57 % of clinical officers who worked at these facilities. The average number of years of employment at the health center was 5.2. Approximately half worked at private health centers and the other half at public facilities.
Table 1.
Provider Demographic Information
| Demographic Information | N= 20 |
|---|---|
| Age (mean, SD) | 32.7, ±8.2 |
| Sex: Male (N, %) | 12 (60%) |
| Employment status: full time (N, %) | 19 (95%) |
| Years employed (mean, SD) | 5.2, ±4.4 |
| Provider Type | N, % |
| Nurse | 8, 40 |
| Medical Officers | 5, 25 |
| Clinical Officers | 7, 35 |
| Health Center Type | |
| Health Center III | 7, 70 |
| Health Center IV | 3, 30 |
| Providers by Health Center | |
| Health Center III | |
| Nurse | 7, 87.5 |
| Clinical Officer | 4, 57.1 |
| Medical Officer | 3, 60 |
| Health Center IV | |
| Nurse | 1, 12.5 |
| Clinical Officer | 3, 42.9 |
| Medical Officer | 2, 40 |
5.1.2. Provider Knowledge of CM
Approximately half the participants (45 %) did not know that CM was transmitted through the air, and 25 % did not know that it was caused by a fungus (Table 2). Only 15 % knew that the duration of CM maintenance lasted until the CD4 count reached ≥200. The current gold standard of CM diagnosis is CSF culture, followed by CrAg LFA (cryptococcal antigen lateral flow assay); however, 40 % of the participants believed that India ink was the best way to diagnose CM. India ink has a sensitivity and specificity of 86.1 % and 97.3 % (Elizabeth Nalintya et al., 2016), compared to CrAg LFA with 99.3 % sensitivity and 99.1 % specificity (Rajasingham et al., 2019a; Rajasingham et al., 2019b). All the participants identified that immunosuppressed patients were the most susceptible to CM.
Table 2.
Provider Knowledge
| N, % | |
|---|---|
| CM Cause | |
| *Fungus | 15, 75 |
| Bacteria, Virus, or TB | 5, 25 |
| CM Transmission | |
| *Airborne | 11, 55 |
| Blood, contact, sexual contact | 9, 45 |
| Who is susceptible to CM? | |
| Immunocompromised | 20, 100 |
| What is the length of CM maintenance treatment | |
| 1 month | 5, 25 |
| 6 months | 9, 45 |
| 1 year | 3, 15 |
| *CD4 ≥200 | 3, 15 |
| What CD4 is used to screen for CM? | |
| *<200 | 7, 35 |
| Other | 13, 65 |
| What diagnostic tests do you use for CM? | |
| Lumbar Puncture or CSF analysis | 9, 45 |
| India Ink | 4, 20 |
| CrAg test | 11, 55 |
| CBC/Blood Culture | 2, 10 |
| I don’t know | 2, 10 |
| What treatment do you give most often for CM? | |
| Ampho B | 8, 40 |
| Fluconazole | 7, 35 |
| Ampho B and fluconazole | 5, 35 |
| What do you need to diagnose CM more accurately? | |
| India Ink | 5, 25 |
| *CSF/Lumbar Puncture | 4, 20 |
| *CrAg Test | 3, 15 |
| *CSF Culture | 5, 25 |
| Blood Culture | 2, 10 |
| X-ray | 1, 5 |
| I Don’t know | 1, 5 |
| Availability of Amphotericin B | |
| Not available | 13, 65 |
| Sometimes available | 7, 35 |
Denotes correct answer
5.1.3. Cadre specific knowledge among providers
The majority of those who did not know the basic facts of CM were nurses, with only half knowing the cause of CM or how it was contracted. While all the medical officers knew the cause and 80 % knew about CM transmission. Lastly, 85.7 % of clinical officers knew the cause of CM, while fewer knew about its transmission (42.9 %, Table 3). When asked how long CM maintenance therapy should last, only three participants (15 %) answered this question correctly, two were medical officers, and one was a clinical officer.
Table 3.
Provider Knowledge by Cadre
| N, % | |
|---|---|
| CM Cause *Fungus | |
| Medical Officers | 5, 100 |
| Clinical Officers | 6, 85.7 |
| Nurse | 1, 12.5 |
| CM Transmission *Airborne | |
| Medical Officers | 4, 80 |
| Clinical Officers | 3, 42.9 |
| Nurse | 4, 50 |
| Who is susceptible to CM? | |
| *Immunocompromised | 20, 100 |
| Length of CM maintenance treatment: *CD4 ≥200 | |
| Medical Officers | 2, 75 |
| Clinical Officers | 1, 14.3 |
| Nurse | 0, 0 |
| What CD4 is used to screen for CM: *CD4 ≤200 | |
| Medical Officers | 2, 40 |
| Clinical Officers | 4, 57.1 |
| Nurse | 1, 12.5 |
| What treatment do you give most often for CM: *Ampho B and Fluconazole | |
| Medical Officers | 3, 60 |
| Clinical Officers | 2, 28.6 |
| Nurse | 0, 0 |
| Amphotericin B is available | |
| Medical Officers | 3, 60 |
| Clinical Officers | 3, 42.9 |
| Nurse | 1, 12.5 |
| What do you need to diagnose CM more accurately? | |
| India Ink | |
| Medical Officers | 1, 20 |
| Clinical Officers | 1, 14.3 |
| Nurse | 3, 37.5 |
| * CSF/Lumbar Puncture | |
| Medical Officers | 1, 20 |
| Clinical Officers | 2, 28.6 |
| Nurse | 0, 0 |
| * CrAg Test | |
| Medical Officers | 0, 0 |
| Clinical Officers | 2, 28.6 |
| Nurse | 0, 0 |
| * CSF Culture | |
| Medical Officers | 3, 60 |
| Clinical Officers | 3, 42.9 |
| Nurse | 0, 0 |
| Blood Culture | |
| Medical Officers | 0, 0 |
| Clinical Officers | 0, 0 |
| Nurse | 2, 25 |
| I Don’t know | |
| Medical Officers | 0, 0 |
| Clinical Officers | 0, 0 |
| Nurse | 1, 20 |
Denotes correct answer
5.1.4. Patient Knowledge and Education of CM
When asked about their patient’s knowledge about CM, most of the participants (90 %) did not believe that their patients knew the symptoms of CM, and half did not think that patients knew about CM before they acquired the disease (Table 4). Most participants disclosed that they never (25 %) or rarely/sometimes (35 %) gave education about CM to their patients, and the reasons were due to time constraints (30 %) and lack of knowledge (30 %). Among the providers who never and rarely/sometimes provided education 75 % were nurses, 42.9 % were clinical officers, and 40 % were medical officers. However, more clinical officers believed that their patients had not heard of CM before their diagnosis (71.4 %) compared to nurses (50 %) and medical officers (20 %).
Table 4.
Patient Knowledge and Education
| N, % | |
|---|---|
| Do patients know about CM symptoms? | |
| Yes | 2, 10 |
| No | 18, 90 |
| How many patients heard about CM before their diagnosis? | |
| None | 10, 50 |
| Few | 6, 30 |
| Most know | 2, 10 |
| I don’t know | 2, 10 |
| How often do you educate your patients about CM? | |
| Never | 5, 25 |
| Rarely | 2, 10 |
| Sometimes | 5, 25 |
| Monthly | 2, 10 |
| Weekly | 3, 15 |
| Daily | 3, 15 |
| What prevents you from educating your patients? | |
| Lack of knowledge | 6, 30 |
| CM is not common | 2, 10 |
| Workload/lack of time | 6, 30 |
| Patients no show/missed appts | 1, 5 |
| Nothing | 5, 25 |
| Patients know about CM symptoms | |
| Medical Officers | 1, 20 |
| Clinical Officers | 1, 14.3 |
| Nurse | 0, 0 |
| Patients haven’t heard about CM | |
| Medical Officers | 1, 20 |
| Clinical Officers | 5, 71.4 |
| Nurse | 4, 50 |
| Never Educate Patients on CM | |
| Medical Officers | 0, 0 |
| Clinical Officers | 2, 28.6 |
| Nurse | 3, 37.5 |
| Lack of knowledge prevents patient education | |
| Medical Officers | 0, 0 |
| Clinical Officers | 2, 28.6 |
| Nurse | 4, 50 |
| Nothing prevents from educating patients | |
| Medical Officers | 3, 60 |
| Clinical Officers | 3, 42.9 |
| Nurse | 0, 0 |
5.2. Semi-structured interviews
The interviews with participants revealed key barriers to CM care for healthcare providers and their patients. Common barriers to CM care were identified as lack of a) education, b) knowledge, c) experience, and d) diagnostics and supplies. These factors were significant obstacles for participants in their pursuit for timely and accurate CM diagnosis, care, and patient education to reduce CM mortality and morbidity.
5.2.1. Providers had inadequate CM education after formal training
Most participants (75 %) had no CM training since medical or nursing school, which for some was over 15–20 years ago. Some (25 %) had training within the last two years and were either medical officers or clinical officers. No nurses had recent training, as evidenced by the following statement:
I have never been trained…in school – not specifically. The cryptococcal meningitis was only being mentioned as one of the infections of the brain, following immunosuppression or malnutrition.
(Nurse, M, age 30)
5.2.2. Lack of CM knowledge impacts the ability to recognize and treat CM
Participants readily admitted their lack of CM knowledge and specifically mentioned the topics of CM symptoms, diagnostics, and treatments. This supported the survey findings, as no one in our sample answered all the CM knowledge questions correctly. Without this knowledge, participants reported that they cannot adequately recognize, treat, or educate patients with CM.
I think I can say inadequate knowledge about cryptococcal meningitis. It can be the major barrier because if you don’t know or if you cannot suspect what you don’t know…if you don’t have any knowledge about cryptococcus just like anybody, you may not be able to even think of it or prevent [it].
(Clinical officer, M, 39)
In 2016, an updated Uganda Clinical Guidelines was distributed and included protocols for CM diagnosis and treatment. One-third of the participants admitted that they had never reviewed the national guidelines for CM screening and treatment. Most of the participants who did not look at the guidelines or have access were nurses (57 %), while others reviewed it sporadically.
…guidelines are there, but if the client is before you and there is no suspicion, then reviewing it might take some other time. It is not always reviewed, once in a while, if you suspect.
(Clinical officer, F, age 34)
5.2.3. Inexperience with CM disease and insufficient supplies can delay care
The majority of the participants worked in health center III facilities and occasionally saw or recognized CM patients in practice. Due to the lack of diagnostics and treatments at their facility, seriously ill patients that presented to their health center were transferred to higher-level facilities that had the capacity for diagnosis and treatment which perpetuated their lack of knowledge and inexperience with CM. This lack of experience coupled with insufficient knowledge can contribute to the lack of recognition, leading to missed or misdiagnosis and the participants were cognizant of this.
…they always say the eyes sees what it knows (laughs) as well you can also analyze what you know but if it’s something that you don’t know, automatically you hear them, you can see them but you can do nothing about it.
(Clinical officer, M, age 25)
Most health center III facilities had limited capacity for diagnosis and treatment. Some of the patients who were “severe cases” or those who were “not doing well” were referred to Lira Regional Referral Hospital. The following statement is how some justified their decision for patient referral.
If the government fails and we have seen that this patient is presenting with the signs of cryptococcal meningitis, eh, we always refer them to main hospital (Lira Regional Referral Hospital) because we know there it is a free service. And with the fluconazole, the price is very high. Other people they cannot afford, so we always end up referring them to the government hospital where they can get free service…
(Nurse, F, age 30)
The lack of proper diagnostics and treatments and lack of patient finances were all factors for the impetus for a referral. Participants at health center III facilities referred patients when they presented with CM symptoms, while those at health center IV facilities and some private clinics attempted diagnostics and treatment before referring to Lira Regional Referral Hospital. The decision to refer considered their capacity for diagnosis and available treatment.
…reagents [for CM testing] are not there, ok. Um, always like for us, here, it can take five months without [reagents]. And every time, [we] need to refer them somewhere.
(Clinical officer, M, age 39)
Participants shared that they needed more supplies to improve care for their patients. Those who had available diagnostic and treatment supplies gained some knowledge and experience about CM treatment compared to those who immediately referred their patients.
5.2.4. Continued CM education for providers is a necessity
Having available CME courses on the topics of CM can offer healthcare providers the most current information for diagnosis and treatment. Participants voiced the importance of education for themselves and their patients and shared the following insights:
Education is, I believe, that it’s one of the best, approaches to healthcare because once somebody knows about what is happening to them or what is likely to happen to them, then they are capable of regulating or preventing themselves of getting into such a thing… and also by updating somebody with sufficient knowledge—They say that education is power; knowledge is power.
(Medical officer, M, age 34)
Participants admitted they needed more education about CM, including its cause, mode of transmission, diagnosis, and treatment and recommended continuing medical education (CME) for healthcare staff and organizing CM education days to improve education at their facility. Uganda has continuing education requirements for medical officers, clinical officers, and nurses; however, it does not specify what topics of education need to be reviewed. No participant shared that they play an active role in CME at their facility, but some had training on CM outside of their academic training (n = 5).
5.2.5. Patient education is the responsibility of the healthcare provider
All participants believed it was important to educate their patients on CM to improve outcomes and prevent CM from reoccurring. However, without their own education and proper knowledge, they cannot provide the necessary information for their patients. They understood that patient education brings awareness about the disease and the symptoms for prompt presentation to care and facilitates early diagnosis and treatment. These feelings were reflected in the following statement:
…it is important to me because… health educating a patient—It will make that patient who is down there or who is having those signs to come up or come to the hospital and get treatment. And to me, it will be a great privilege to me in a way that I would have reduced [the] morbidity rate...
(Nurse, F, age 30)
Lastly, participants emphasized the importance of prompt evaluation by not delaying care. They know the severity of the disease increases if patients delay seeking care which delays diagnosis and treatment. Educating patients about the potential outcomes of this disease may prompt patients to seek treatment sooner when their symptoms first begin.
We should always ask signs and symptoms that suggest they are heading to and give appropriate treatment and also give health education to the community…we should also give that health education.
(Nurse, F, age 32)
Participants want to educate patients on topics of basic CM facts, ART adherence, disease severity, and the importance of prompt presentation to care. They also recommended topics focused on general CM knowledge, diagnosis, treatment, and information about other common diseases that they see frequently in their facilities such as diabetes and hypertension. They believed that through education, they can improve diagnosis and treatment to become better clinicians and educators for their patients and their community.
6. Discussion
This is one of few studies conducted with healthcare providers assessing their experience with CM in rural Uganda. Using the IBM framework, this study identified several key themes under knowledge, environmental constraints, habits, agency and norms regarding providers’ experience and behaviors in the diagnosis and care of patients with CM. The themes encompassed gaps in knowledge due to the lack of education and lack of experience which contributes to decreased patient education, and the lack of access to appropriate supplies which affects their provision for CM diagnosis, treatment, and care.
6.1. Education and knowledge
6.1.1. Lack of education contributes to limited knowledge of CM
Most participants reported they had no recent CM training beyond medical or nursing school, except for a few medical and clinical officers. Those who had the least amount of knowledge, experience, and training were nurses, even though they are commonly the first point of contact for patients and constitute the majority of lower-level (level II and III) health center providers in Uganda (World Health Organization (WHO), 2017). According to the World Health Organization (WHO), the “lack of provider education and awareness about cryptococcal disease has also been identified as a cause of suboptimal management” (World Health Organisation (WHO), 2016). Uganda has continuing professional development in the form of continuing education units (CEUs) for healthcare professionals but activities do not require specific medical education topics (Republic of Uganda Ministry of Health, 2016; Republic of Uganda Ministry of Health, 2017). Crucial gaps related to provider education and knowledge of CM were revealed and dispelled assumptions that healthcare workers are knowledgeable about CM.
6.1.2. Provider knowledge through education is needed to educate patients
All participants believed they are responsible for providing patient education and requested continuing medical education through CEUs to provide quality education to their patients. Education must first be given to providers so that they can then pass their knowledge on to patients and provide awareness for CM. In addition to the lack of provider education, other barriers such as the lack of time and knowledge were supported by a previous study which found that staff shortages, limited opportunity for continuing education, and lack of time interfered with patient education (Beagley, 2011).
6.1.3. Lack of recognition and available supplies contribute to missed or misdiagnosis
Many nurses and other providers acknowledged their lack of experience with CM which perpetuated insufficient knowledge and lack of recognition of this disease. Some participants reported a lack of contact with CM patients; however, they may have encountered such a patient but did not recognize it due to their lack of knowledge and/or inexperience. This poses concerns for patients who have less severe presentations which may increase the potential of missed or misdiagnosis and reinforces the need for provider education to increase knowledge and awareness of CM. Missed or misdiagnosis was observed among participants in a previous study which found CM patients presenting to health centers multiple times before finally being referred to the referral hospital which also found poorer outcomes among those who had diagnosis and treatment delays (Link et al., 2022b).
The lack of available supplies and treatments also contributed to missed or misdiagnosis. Diagnostic errors can lead to delayed care and death among patients. The WHO reported that the burden of errors in primary care settings is higher in middle-to low-income countries specifically due to lack of diagnostic tests, fewer qualified healthcare providers, and paper-based charting (World Health Organisation (WHO), 2016). The recommendations to remedy future errors can be accomplished through improving provider education and skills, patient knowledge through education, access to testing, and learnings from past errors (World Health Organisation (WHO), 2016). These recommendations bolster the need to educate healthcare providers, especially in these lower-level health centers, and to increase the access to diagnostic tests which can mitigate future errors and barriers to CM care.
Education for nurses and other healthcare providers will impart the necessary knowledge to recognize CM symptoms and prescribe the appropriate diagnostic tests and treatments based on the Uganda Clinical guidelines. This knowledge will also allow providers to educate their patients about early symptoms of CM and the importance of prompt evaluation and treatment. Implementing these interventions can improve overall care for CM and encourage patient engagement in health care to improve health outcomes.
The challenges faced by the participants caring for CM patients in this study are not uncommon, especially in rural parts of the world. Additionally, the lack of education and knowledge around this neglected opportunistic infection is not unusual (Bongomin and Atikoro, 2018; Deming et al., 2019; Link et al., 2022b). The findings and recommendations of this study from Uganda apply to other rural areas, as many countries have similar healthcare systems, barriers to care, and lack of education and knowledge. Much of what we learned from this study and the recommendations can be translated to other countries to help treat, prevent, and improve patient outcomes from this deadly form of meningitis.
6.2. Limitations
Our clinical sites were chosen based on the number of CM referrals made to Lira Regional Referral Hospital. This may have introduced selection bias, as not all health centers surrounding the hospital had an equal chance of being selected. Participants were selected by the in-charge supervisor at each clinic site as the supervisors were more aware of the provider’s schedule and availability to participate in the study. However, this sampling method and our small sample size may have diminished the representativeness of healthcare providers and their experiences in rural Uganda. Despite the small number of interviews conducted, data saturation was achieved, as no new information was obtained after our last interview.
6.3. Conclusion
This study identified gaps related to CM education and knowledge among healthcare providers which directly impact patient education, recognition of CM infection, and delays to care and treatment. To address these gaps to care, education on CM is needed for providers to improve knowledge and pass this knowledge to their patients. Additionally, supplies for diagnosis and treatment are needed at the lower-level health facilities where most patients go for initial care and where delays occur due to missed or misdiagnosis.
6.3.1. Recommendations
Education through a formal in-service training program and CMEs should be provided in collaboration with local professional boards or the regional referral hospitals. An education curriculum developed for patient and provider education can incorporate comprehensive information about HIV, CM, and other OIs to increase patient and provider knowledge. Both curricula should be developed at the government level for continuity and consistent messaging of CM information which can be disseminated during clinic visits and through public service announcements. Lastly, providing a rapid point-of-care test like the cryptococcal antigen lateral flow assay (CrAg LFA) test can equip providers with an accurate and reliable test for CM detection. These recommendations aim to increase CM knowledge and early CM recognition for patients and providers to obtain timely diagnosis and treatment, which can save lives.
Funding
This study was supported by the Robert Wood Johnson Foundation, Future of Nursing Scholars and Fellowship; GO Health Travel Fellowship, University of Washington (UW) Department of Global Health; Boeing International Fellowship, UW Graduate School; Hester McClaws Fellowship, UW School of Nursing; Fulbright U.S. Student Fellowship; Fogarty Global Health Fellowship [grant number D43 TW009345]; University of Minnesota Medical School; National Institute of Allergy and Infectious Diseases [grant number T32AI055433]; and Fulbright U.S. Scholars Program.
Appendix A. Provider semi-structured interview questions
| Provider | Interview questions |
|---|---|
|
| |
| 1. | What disease or illnesses do you feel you need more information on? |
| 2. | How important is it for you to know about CM? |
| 3. | How confident are you to be able to accurately diagnose CM? |
| 2. | What makes it easy to diagnose CM |
| 3. | What makes it difficult to diagnose CM |
| 4. | What prevents you from diagnosing patients for CM? |
| 5. | How do you get access to the items you need to diagnose or treat your patients for CM? |
| 6. | What are other ways you can get the supplies you need for diagnosis and treatment for CM patients? |
| 7. | What is the importance to diagnose a patient correctly with CM? |
| 8. | What does a patient need to look like before you refer them to LRRH? |
| 9. | What type of patient gets CM? |
| 10. | What prevents you from treating patients with CM or cryptococcal disease? |
| 11. | Please describe your CM training to me. |
| 12. | How often do you review the guidelines for CM screening and treatment? |
| 13. | What should patients know to help improve outcomes of CM? |
| 14. | What should providers know to help improve outcomes of CM? |
| 15. | What should CM patients do to improve their morbidity and mortality outcomes? |
| 16. | How can providers improve CM morbidity and morbidity? |
| 17. | Whose responsibility is it to educate patients? |
| 18. | How important is it for you to provide education to your patients? |
| 19. | What recommendations do you have to make CM education easier for providers? |
| 20. | What recommendations do you have to decrease barriers to CM diagnosis and treatment for yourself and patients? |
| 21. | Is there any other feedback you want to give or questions you have? |
Appendix B. Provider barriers codebook
| Provider barriers | Theme | Code | Subcode | Example |
|---|---|---|---|---|
|
| ||||
| LACK OF PROVIDER EDUCATION | Education | Schooling | I have never been trained...in school – not specifically. (Nurse, M) No, it’s [CM training] what I learnt in medical school. (Medical officer, M) |
|
| Continuing medical education | Not when I am here, I think, I think when I was still in school [last time for CM training]. (Medical officer, 27) Outside School I didn’t have any. [CM] training. (Nurse, M) | |||
| LACK OF PROVIDER KNOWLEDGE | Knowledge | Cryptococcal meningitis knowledge | I think I can say inadequate knowledge about cryptococcal meningitis. It can be the major barrier because if you don’t know or if you cannot suspect what you don’t know. (Clinical officer, M) That alone, I can’t deceive because I have never seen... have never reviewed it [clinical guidelines]. (Nurse, F) |
|
| Uganda clinical guidelines | ...no guideline is available. (Clinical officer, F) I’ve not yet reviewed the guidelines, I’ve never reviewed, maybe people review it but me personally, I’ve not. (Nurse, M) |
|||
| GAPS RELATED TO INADEQUATE PROVIDER KNOWLEDGE | Missed/misdiagnosis | ...they [the patient] will not tell you everything, so basing on their symptoms you may miss it, you may just send them and do other tests... (Clinical officer, M) ... lack of clinical knowledge or skills on how to diagnose and then secondly when you have the strips, the test strips are faulty, so the result may become negative when actually the patient is what positive. (Medical officer, 27) | ||
| Patient education | ... health educating a patient—It will make that patient who is down there or who is having those signs to come up or come to the hospital and get treatment. (Nurse, F) ...also give health education to the community...we should also give that health education. (Nurse, F) |
|||
| LACK OF SUPPLIES | Diagnostics | ...reagents [for CM testing] are not there. (Clinical officer, M) ...lack of the diagnostic materials. (Nurse, M) | ||
| Treatment | ...the fluconazole, the price is very high. Other people they cannot afford, so we always end up referring them to the government hospital where they can get free service. (Nurse, F) The drugs at times are not here. (Clinical officer, F) | |||
Footnotes
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
CRediT authorship contribution statement
Abigail Link: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Writing – original draft, Writing – review & editing. Mark Okwir: Resources, Supervision, Writing – review & editing. Sarah Iribarren: Methodology, Writing – review & editing. David Meya: Methodology, Supervision, Writing – review & editing. Paul Bohjanen: Supervision, Writing – review & editing. Danuta Kasprzyk: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
References
- Beagley L, 2011. Educating patients: understanding barriers, learning styles, and teaching techniques. J. PeriAnesth. Nurs. 26 (5), 331–337. [DOI] [PubMed] [Google Scholar]
- Bongomin F, Atikoro L, 2018. Recurrence of cryptococcal meningitis and the hidden role of patient education and social support. Case Rep. Neurol. Med. 2018, 8125096. 10.1155/2018/8125096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control (CDC), 2018. Cryptococcus: screening for opportunistic infection among people living with HIV/AIDS. Retrieved from. https://www.cdc.gov/fungal/pdf/at-a-glance-508c.pdf.
- Deming M, Mark A, Nyemba V, Heil EL, Palmeiro RM, Schmalzle SA, 2019. Cognitive biases and knowledge deficits leading to delayed recognition of cryptococcal meningitis. IDCases 18, e00588. 10.1016/j.idcr.2019.e00588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faini D, Kalinjuma AV, Katende A, Mbwaji G, Mnzava D, Nyuri A, Letang E, 2019. Laboratory-reflex cryptococcal antigen screening is associated with a survival benefit in Tanzania. J. Acquir. Immune Defic. Syndr. 80 (2), 205–213. 10.1097/qai.0000000000001899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG, 2009. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42 (2), 377–381. 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasprzyk D, Montano DE, Fishbein M, 1998. Application of an integrated behavioral model to predict condom use: a prospective study among high HIV risk groups1 Y1 – 1998 Y2 - Sep. J. Appl. Soc. Psychol. 17, 1557. 10.1111/j.1559-1816.1998.tb01690.x (M1 - Journal Article). [DOI] [Google Scholar]
- Link A, Okwir M, Meya D, Kasprzyk D, Nabongo B, Okello J, Bohjanen P, 2022a. Impact of a Cryptococcal Meningitis Diagnosis and Treatment Program at Lira Regional Referral Hospital in Rural. Plos Global Health, Northern Uganda (In press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link A, Okwir M, Nabongo B, Meya D, Iribarren S, Bohjanen P, Kasprzyk D, 2022b. Delays in cryptococcal meningitis diagnosis and care: a mixed methods study in rural Uganda. Ann. Glob. Health 88 (1), 22. 10.5334/aogh.3524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lofgren SM, Nalintya E, Meya DB, Boulware DR, Rajasingham R, 2018. A qualitative evaluation of an implementation study for cryptococcal antigen screening and treatment in Uganda. Medicine (Baltimore) 97 (31), e11722. 10.1097/MD.0000000000011722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meiring S, Fortuin-de Smidt M, Kularatne R, Dawood H, Govender NP, 2016. Prevalence and hospital management of amphotericin B deoxycholate-related toxicities during treatment of HIV-associated cryptococcal meningitis in South Africa. PLoS Negl. Trop. Dis. 10 (7), e0004865 10.1371/journal.pntd.0004865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montaño D, Kasprzyk D, 2008. Theory of reasoned action, theory of planned behavior, and the integrated behavioral model. In: Glanz K, Rimer BK, Viswanath K (Eds.), Behavior and Health Education Theory, Research, and Practice, 4th ed. CA Jossey-Bass, 989 Market Street, San Francisco, pp. 67–96. [Google Scholar]
- Montaño D, Kasprzyk D, 2015. Theory of reasoned action, theory of planned behavior, and the integrated behavioral model. In: Glanz V, Rimer (Eds.), Health Behavior: Theory, Research and Practice, 5 ed. Jossey-Bass Publishers, Inc, San Francisco, CA. [Google Scholar]
- Nalintya E, Kiggundu R, Meya D, 2016. Evolution of cryptococcal antigen testing: what is new? Curr. Fungal Infect. Rep. 10 (2), 62–67. 10.1007/s12281-016-0256-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nalintya E, Meya DB, Lofgren S, Huppler Hullsiek K, Boulware DR, Rajasingham R, 2018. A prospective evaluation of a multisite cryptococcal screening and treatment program in HIV clinics in Uganda. J. Acquir. Immune Defic. Syndr. 78 (2), 231–238. 10.1097/qai.0000000000001669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oketch B, 2012. Lira hospital faces doctor shortage. Retrieved from. https://mobile.monitor.co.ug/News/-/691252/1531678/-/format/xhtml/-/mx4et9/-/index.html.
- R Core Team, 2020. R: a language and environment for statistical computing. In: 3.6.3 ed., Vol. Holding the Windsock. R Foundation for Statisical Computing, Vienna, Austria. [Google Scholar]
- Rajasingham R, Meya DB, Greene GS, Jordan A, Nakawuka M, Chiller TM, Larson BA, 2019a. Evaluation of a national cryptococcal antigen screening program for HIV-infected patients in Uganda: a cost-effectiveness modeling analysis. PLoS One 14 (1), e0210105. 10.1371/journal.pone.0210105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajasingham R, Wake RM, Beyene T, Katende A, Letang E, Boulware DR, 2019b. Cryptococcal meningitis diagnostics and screening in the era of point-of-care laboratory testing. J. Clin. Microbiol. 57 (1) 10.1128/jcm.01238-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Republic of Uganda Ministry of Health, 2016. Continuing Professional Development Framework for Nurses and Midwives in Uganda. Uganda MOH, Kampala, Uganda. [Google Scholar]
- Republic of Uganda Ministry of Health, 2017. In: Council MADP (Ed.), Continuing Professional Development (CPD) Accreditation and Certification Guidelines Uganda. Uganda MOH, Kampala, Uganda. [Google Scholar]
- Scientific Software Development, 2019. ATLAS.ti 8 Windows User Manual. Scientific Software Development, Berlin, Germany. [Google Scholar]
- World Health Organisation (WHO), 2016. Diagnostic Errors: Technical Series on Safer Primary Care. WHO, Geneva, Switzerland. Retrieved from. http://apps.who.int/iris. [Google Scholar]
- World Health Organization (WHO), 2017. Primary Health Care Systems (PRIMASYS): Case Study From Uganda, Abridged Version. World Health Organization, Geneva, Switzerland. [Google Scholar]


