Recent antibiotic use is a well documented risk factor for infection or colonisation with resistant pathogens.1–7 Despite this recognition, unnecessary antibiotic prescribing remains common. In the United States more than a fifth of all antibiotic prescriptions for children and adults are written for upper respiratory tract infections or bronchitis, conditions that are almost always viral.8,9 Similar rates of unnecessary antibiotic use have been described in Britain.10 These findings are consistent with results from focus groups among doctors, in which participants have estimated that 10% to 50% of outpatient antibiotic prescriptions are unnecessary.11
Only limited data are available to evaluate whether reducing antibiotic prescribing will reduce the spread of resistance. In Finland the proportion of group A streptococcal infections resistant to macrolides was nearly halved after a successful campaign to reduce the use of macrolide antibiotics.12 A cross sectional survey in Iceland found that carriage of penicillin resistant pneumococci was strongly associated with both individual and community-wide levels of antimicrobial use,13 and there is some evidence that an intervention programme has decreased the proportion of pneumococcal infections caused by penicillin resistant strains.14
Summary points
Unnecessary antibiotic use for viral illness is common and has led to increasing rates of antibiotic resistance among Streptococcus pneumoniae and other community acquired pathogens
Factors that contribute to antibiotic overuse include lack of education, patients’ expectations, past experience, and economic incentives
Multifaceted interventions are needed to reduce unnecessary antibiotic use; peer education and feedback on doctors’ use of antibiotics can promote behaviour change
Educational interventions for the public should include a public relations campaign with simple messages, clinic based patient education, and community outreach activities
Health organisations should develop policies to support judicious antibiotic use and evaluate whether existing policies may unintentionally promote overuse of antibiotics
Factors contributing to overuse of antibiotics
Achieving more judicious prescribing of antibiotics requires (a) an understanding of the factors that promote overuse and the barriers to change and (b) the implementation of effective strategies for changing behaviour. Well targeted but ineffective interventions and effective but poorly targeted strategies are equally futile. Both the message and the media are key elements. Results of formative research in the United States suggest that four major factors promote the overuse of antibiotics: lack of education, prior experience, patients’ expectations, and economics (table). Lack of education applies to both providers and patients. Surveys of primary care doctors show that many have inaccurate knowledge regarding the need for antibiotics in patients with purulent rhinitis,15,16 and many family practitioners do not follow expert recommendations for diagnosis and management of pharyngitis.17
Patients’ lack of knowledge and past experience contribute to increased demand for antibiotics. Many patients have received antibiotics for viral respiratory illness, and these treatments were perceived as effective because the infections were generally self limiting. Patients with lower educational levels seem to have the greatest misconceptions about antibiotic use and upper respiratory infections.18–20
Whether real or perceived, patients’ expectations for antibiotics affect doctors’ prescribing behaviour.10,11 Years of prescribing or taking antibiotics for viral respiratory infections have created a cycle of supply and demand, reinforcing behaviours that are detrimental in an era of increasing antibiotic resistance. Breaking this cycle will require educating the public that past practices are no longer optimal and convincing doctors that a patient’s satisfaction is based more on communication than on prescription.21
Economic factors contributing to overprescription will vary substantially by country, depending on the type of medical care system. However, for providers, time pressures and the desire to maximise the patient’s satisfaction (and thereby also retain him or her as a possible patient in the future), and for both providers and patients the desire to avoid follow up visits, are probably universal.
Diagnostic uncertainty can also contribute to unnecessary antibiotic use. Occasional diagnostic uncertainty is inevitable, but it should occur infrequently when an appropriate clinical evaluation is performed and the findings are interpreted accurately. This will reduce the likelihood that a clinician will prescribe an antibiotic “just in case” an infection is bacterial. Performing a throat culture for pharyngitis and use of pneumatic otoscopy for diagnosing otitis media are two evaluation techniques that can reduce diagnostic uncertainty. Appropriate clinical evaluation, combined with good communication and shared decision making, will minimise the risk of incorrect diagnosis, patients’ dissatisfaction, or other adverse outcome. Guidelines have recently been published to help clinicians evaluate common respiratory illnesses appropriately.22
Strategies to reduce inappropriate use of antibiotic
Among providers
Most doctors are aware that antibiotic resistance is an emerging problem created largely by the overuse of antibiotics.16,23 This widespread awareness suggests that providing information or education alone will be insufficient to change their prescribing behaviour. Overcoming barriers to more judicious prescribing will require development of materials to support change, implementation of effective techniques to catalyse that change, and development of supportive structures in healthcare organisations. Key elements include evidence based recommendations for diagnosis and treatment backed by professional societies; materials for patient education; and information to facilitate provider-patient communication. Materials developed by the US Centers for Disease Control and Prevention in conjunction with other organisations are listed in the box. Similar materials have also been developed by healthcare organisations, health departments, and at academic centres.
Materials available to support an intervention programme on antibiotic use
Principles of judicious antibiotic use for paediatric infections22
Academic sheets providing one page summaries of the principles of antibiotic use
Posters for educating patients
Pamphlets for educating patients
Question and answer sheets for viral respiratory diagnoses
A “prescription pad” including recommendations for symptomatic treatment for patients with viral respiratory infections
A letter to childcare providers stating that the child can return to day care without an antibiotic
These materials are available from the Center for Disease Control and Prevention (tel: 00 1 404 639 4702)
Guidelines for managing otitis media with effusion are available from the Agency for Health Care Policy and Research.24 The Infectious Diseases Society of America has published guidelines for diagnosing and managing pharyngitis25 and is developing other guidelines. A recent review has suggested that locally developed guidelines are more likely to be accepted and followed than those developed nationally without local input or recognition of local needs.26
Development of clinical practice guidelines must be supported by other educational activities, as multifaceted interventions tend to be more effective than single interventions.27 Formal continuing medical education conferences and distribution of printed materials have little impact on doctors’ behaviour unless reinforced by other strategies.27,28 These and other activities, however, may enhance the adoption of clinical practice guidelines if they are actively promoted to clinicians and endorsed by “opinion leaders” in each community.
Many studies have shown that education at an individual or small group level and peer education are effective strategies to change doctors’ antibiotic prescribing behaviour.29–33 Face to face interactions are supported by the common practice of pharmaceutical companies sending out representatives to promote their products. The effectiveness of peer education is enhanced when the message is delivered or endorsed by local opinion leaders and is made relevant to the doctor’s own practice. Previous successful programmes have used retired doctors29 and clinical pharmacists.30 Establishing credibility, defining clear objectives for behaviour change, and repetition and reinforcement are all important for peer education.31 In addition, clinicians must have the opportunity to voice their own concerns and provide feedback. Implementing peer education on a broad scale may be difficult and expensive because of the need to identify, train, and support sufficient educators. An alternative worth exploring is video presentation of information. Although costs would be substantially reduced, the ability to tailor discussion to each clinician’s needs would be lost.
Providing feedback to clinicians regarding their own antibiotic prescribing practices has been a successful technique for achieving behaviour change.34 Feedback can entail comparisons with peers or with a standard or indicator. As with practice guidelines, feedback may be most effective when the system is developed with local input, where clinicians accept the measures as important, fair, and relevant to their own practices. The availability of prescribing data may be a limiting factor in some healthcare systems.
New communications technologies such as the internet enhance the potential to disseminate practice guidelines and provide feedback to clinicians. Computer assisted decision support has been used effectively to improve antibiotic prescribing in hospitals and could be extended to outpatient settings.35 The willingness of a busy practitioner to use computer support during consultations with patients, however, has not been assessed.
A limitation of all intervention strategies is that some providers will participate and others will not. Participation may be enhanced in a single payer system (system of nationalised care where all costs are paid from one source) or a managed care organisation, where incentives or sanctions can be provided. Convincing local opinion leaders to change practices will result in eventual diffusion of the changes throughout the community, leading to a change in the standard of care. For this reason, identifying and educating opinion leaders as a priority group would be effective, particularly if resources are limited. Educating future healthcare providers about the importance of judicious antibiotic use will have long term impact and is a useful adjunct to strategies focused on current providers.
“To write prescriptions is easy, but to come to an understanding with people is hard” 36
Among patients and the public
A multifaceted approach is needed to increase the public’s understanding of antibiotic resistance and to change expectations about use of antibiotics. The key elements should include a public relations campaign, clinic based education, and community outreach activities. Conducting a public relations campaign with paid advertising is an effective but expensive strategy to change health related behaviour. Educating the public about the difference between bacterial and viral infections, and the potential risk of taking antibiotics, is more complex than other health education messages because the risk to benefit ratio is less clear. A successful public relations effort will require expertise in marketing and communications. Some companies may be willing to sponsor components of a public relations campaign as a community service. In recent years the popular media have been increasing their coverage of antibiotic resistance, and this can enhance the impact of other public education efforts.
Educational interventions for patients and parents at outpatient clinics must be an important component of a public education campaign. Information provided during a medical consultation is immediately relevant and is likely to be viewed as authoritative. Clinicians should obtain information material compiled for patients or review the content of their own material to ensure that messages about appropriate antibiotic use are emphasised. Medical providers should also seek opportunities for community partnerships to disseminate similar messages widely. For example, educational information can be disseminated through community organisations, schools, childcare centres, and pharmacies. In the short term, patients are likely to benefit from a reduction in unnecessary visits and therapy. In the long term, it is likely that decreased rates of resistance will improve health and cost outcomes.
Intervention strategies for judicious antibiotic use and approaches to enhance effectiveness of such strategies
| Strategy | Approaches to enhance effectiveness |
| Clinical practice guidelines | Develop with local input; promote actively |
| Peer (or small group) education | Recruit respected source as educator; clearly communicate objectives; encourage discussion and tailor to local practice; distribute supportive materials; repeat and reinforce messages |
| Develop with local input; provide peer comparison or compare with standard or indicator | |
| Use as a component of a multifaceted programme; obtain support of opinion leaders and professional societies | |
| Feedback | Use as a component of a multifaceted programme; obtain support of opinion leaders and professional societies |
| Deliver in varied settings using various media; avoid clutter—use a few consistent clear messages; develop local partnerships | |
| Direct mailing of information | |
| Lectures and continuing medical education | |
| Education of patients and the public | |
Policy support
Interventions must be supported by national and local policies that promote judicious antibiotic use. National goals should be developed to reduce unnecessary use, and progress toward those goals should be monitored. Where needed, databases should be established to support feedback interventions and programme evaluation. Economic factors that may affect practices must be carefully considered and, where necessary, modified. Antibiotic overuse may be an unintended consequence of quality assurance tools, such as surveys of patients’ satisfaction or profiling rates of follow up visits. Support is also needed to encourage appropriate diagnostic testing, even if this represents a short term direct cost. Sponsorship of continuing education and requirements for professional licensure are other potential policy options.
Table.
Provider and patient factors contributing to overuse of antibiotics
| Contributing factor | Providers | Patients and public |
|---|---|---|
| Lack of education | Suboptimal approach to diagnosis and treatment; lack of knowledge of the natural course of viral disease | Insufficient knowledge of viral v bacterial infection |
| Experience | Diagnostic and prescribing habits from the pre-antibiotic resistance era | Prior antibiotic treatment for viral infections (perceived as effective) |
| Expectations | Belief that patients expect antibiotics; belief that satisfaction is related to prescription | Belief that some conditions require antibiotic treatment—for example, purulent rhinitis |
| Economics | Time pressures; incentives linked to satisfaction surveys; profiling on return visits | Need to return to work or return child to day care |
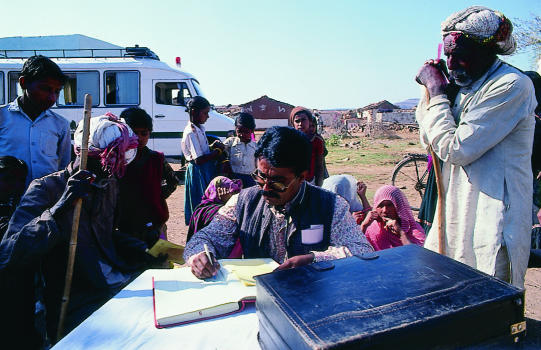
Figure.
Educating doctors and patients is a global challenge
Acknowledgments
Competing interests: None declared.
References
- 1.Radetsky MS, Istre GR, Johansen TL, Parmelee SW, Lauer BA, Wiesenthal AM, et al. Multiply resistant pneumococcus causing meningitis: its epidemiology within a day-care centre. Lancet. 1981;2:771–773. doi: 10.1016/s0140-6736(81)90184-7. [DOI] [PubMed] [Google Scholar]
- 2.Pallares R, Gudiol F, Linares J, Ariza J, Rufi G, Murgui L, et al. Risk factors and response to antibiotic therapy in adults with bacteremic pneumonia caused by penicillin-resistant pneumococci. N Engl J Med. 1987;317((1):18–22. doi: 10.1056/NEJM198707023170104. [DOI] [PubMed] [Google Scholar]
- 3.Guillemot D, Carbon C, Balkau B, Geslin P, Lecoeur H, Vauzelle-Kervroedan F, et al. Low dosage and long treatment duration of beta-lactam: Risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA. 1998;279:365–370. doi: 10.1001/jama.279.5.365. [DOI] [PubMed] [Google Scholar]
- 4.Tan TQ, Mason EO, Jr, Kaplan SL. Penicillin-resistant systemic pneumococcal infections in children: a retrospective case-control study. Pediatrics. 1993;92:761–767. [PubMed] [Google Scholar]
- 5.Clavo-Sanchez AS, Giron-Sanchez JA, Lopez-Prieto D, Canueto-Quintero J, Sanchez Porto A, Vergara-Campos A, et al. Multivariate analysis of risk factors for infection due to penicillin-resistant and multidrug resistant Streptococcus pneumoniae: a multicenter study. Clin Infect Dis. 1997;24:1052–1059. doi: 10.1086/513628. [DOI] [PubMed] [Google Scholar]
- 6.Fairchild MP, Ashton WS, Fischer GW. Carriage of penicillin resistant pneumococci in a military population in Washington, DC: risk factors and correlation with clinical isolates. Clin Infect Dis. 1996;22:966–972. doi: 10.1093/clinids/22.6.966. [DOI] [PubMed] [Google Scholar]
- 7.Dowell SF, Schwartz BS. Resistant pneumococci: protecting patients through judicious use of antibiotics. Am Fam Phys. 1997;55:1647–1654. [PubMed] [Google Scholar]
- 8.Nyquist AC, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA. 1998;279:875–877. doi: 10.1001/jama.279.11.875. [DOI] [PubMed] [Google Scholar]
- 9.Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA. 1997;278:901–904. [PubMed] [Google Scholar]
- 10.MacFarlane J, Holmes W, MacFarlane R, Britten N. Influence of patients’ expectations on antibiotic management of acute lower respiratory tract illness in general practice: questionnaire study. BMJ. 1997;315:1211–1214. doi: 10.1136/bmj.315.7117.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schwartz B, Barden L, Dowell S, Lackey C. Atlanta, GA: Centers for Disease Control and Prevention; 1998. Why doctors overprescribe antibiotics: results of focus group discussions with pediatricians (Ped) and family physicians (FP) and application to a resistance prevention campaign (abstract). Presented at the International Conference on Emerging Infectious Diseases, Atlanta, 1998; p. 66. [Google Scholar]
- 12.Seppala H, Klaukka T, Vuopio-Varkila I, Muotiala A, Helenius H, Lager K, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. N Engl J Med. 1998;337:441–446. doi: 10.1056/NEJM199708143370701. [DOI] [PubMed] [Google Scholar]
- 13.Arason V, Kristinsson K, Sigurdsson J, Stefánsdóttir G, Mölstad S, Gudmundsson S. Do antimicrobials increase the carriage rate of penicillin-resistant pneumococci in children? Cross sectional prevalence study. BMJ. 1996;313:387–391. doi: 10.1136/bmj.313.7054.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stephenson J. Icelandic researchers are showing the way to bring down rates of antibiotic-resistant bacteria [news] JAMA. 1996;275:175. [PubMed] [Google Scholar]
- 15.Mainous AG, Hueston WJ, Eberlein C. Colour of respiratory discharge and antibiotic use. Lancet. 1997;350:1077. doi: 10.1016/S0140-6736(05)70457-8. [DOI] [PubMed] [Google Scholar]
- 16.Schwartz RH, Freij BJ, Ziai M, Sheridan MJ. Antimicrobial prescribing for acute purulent rhinitis in children: a survey of pediatricians and family practitioners. Pediatr Infect Dis J. 1997;16:185–190. doi: 10.1097/00006454-199702000-00004. [DOI] [PubMed] [Google Scholar]
- 17.McIsaac WJ, Goel V. Sore throat management practices of Canadian family physicians. Fam Pract. 1996;14((1):34–39. doi: 10.1093/fampra/14.1.34. [DOI] [PubMed] [Google Scholar]
- 18.Mainous AG, Zoorob RJ, Oler MJ, Haynes OM. Patient knowledge of upper respiratory infections: implications for antibiotic expectations and unnecessary utilization. J Fam Pract. 1997;45((1):75–83. [PubMed] [Google Scholar]
- 19.Chan CS. What do patients expect from consultations for upper respiratory tract infections? Fam Pract. 1996;13:229–235. doi: 10.1093/fampra/13.3.229. [DOI] [PubMed] [Google Scholar]
- 20.Trepka MJ, Belongia CA, Davis JP. Atlanta, GA: Centers for Disease Control and Prevention; 1998. Knowledge, attitudes and practices of caregivers regarding antibiotic use for children’s upper respiratory infections (abstract). Presented at the International Conference on Emerging Infectious Diseases, Atlanta, 1998; p. 68. [Google Scholar]
- 21.Hamm RM, Hicks RJ, Bemben DA. Antibiotics and respiratory infections: are patients more satisfied when expectations are met? J Fam Pract. 1996;43:56–62. [PubMed] [Google Scholar]
- 22.Dowell SF. Principles of judicious use of antimicrobial agents for pediatric upper respiratory tract infections. Pediatrics. 1998;101(suppl 1):163–184. [Google Scholar]
- 23.Schwartz B, Bell DM, Hughes JM. Preventing the emergence of antimicrobial resistance. A call for action by clinicians, public health officials, and patients. JAMA. 1997;278:944–945. doi: 10.1001/jama.278.11.944. [DOI] [PubMed] [Google Scholar]
- 24.Otitis Media Guideline Panel. Clinical practice guideline: otitis media with effusion in young children. Rockville, MD: Agency for Health Care Policy and Research; 1994. (Report No 94-0622.) [PubMed] [Google Scholar]
- 25.Bisno AL, Gerber MA, Gwaltney JM, Kaplan AL, Schwartz RH. Diagnosis and management of group A streptococcal pharyngitis: a practice guideline. Clin Infect Dis. 1997;25:574–583. doi: 10.1086/513768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet. 1993;342:317–322. doi: 10.1016/0140-6736(93)92244-n. [DOI] [PubMed] [Google Scholar]
- 27.Davis DA, Thomson MA, Oxmen AD, Haynes RB. Changing physician performance: a systematic review of the effect of continuing medical education strategies. JAMA. 1995;274:700–705. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
- 28.Soumerai S, McLaughlin T, Avorn J. Improving drug prescribing in primary care: a critical analysis of the experimental literature. Milbank Q. 1989;67:268–317. [PubMed] [Google Scholar]
- 29.Schaffner W, Ray W, Federspiel C, Miller W. Improving antibiotic prescribing in office practice. JAMA. 1983;250:1728–1732. [PubMed] [Google Scholar]
- 30.Avorn J, Soumerai S. Improving drug-therapy decisions through educational outreach. N Engl J Med. 1983;308:1457–1463. doi: 10.1056/NEJM198306163082406. [DOI] [PubMed] [Google Scholar]
- 31.Soumerai S, Avorn J. Principles of educational outreach (“academic detailing”) to improve clinical decision making. JAMA. 1990;263:549–556. [PubMed] [Google Scholar]
- 32.De Santis G, Harvey K, Howard D, Mashford M, Moulds R. Improving the quality of antibiotic prescription patterns in general practice. Med J Aust. 1994;160:502–505. [PubMed] [Google Scholar]
- 33.Ekedahl A, Andersson S, Hovelius B, Molstad S, Liodholm H, Melandor A. Drug prescription attitudes and behaviour of general practitioners. Effects of a problem oriented educational programme. Eur J Clin Pharmacol. 1995;47:381–387. doi: 10.1007/BF00196849. [DOI] [PubMed] [Google Scholar]
- 34.Schoenbaum SC. Feedback of clinical practice information. HMO Pract. 1993;7:5–11. [PubMed] [Google Scholar]
- 35.Evans RS, Pestotnik SL, Classen DC, Clemmer TP, Weaver LK, Orme JF, et al. A computer-assisted management program for antibiotics and other antiinfective agents. N Engl J Med. 1998;338:232–238. doi: 10.1056/NEJM199801223380406. [DOI] [PubMed] [Google Scholar]
- 36.Kafka F. A country doctor. Selected short stories. New York: Modern Linguists; 1952. [Google Scholar]