Before patients in the United Kingdom are given long term oxygen therapy at home they must have arterial blood gas analysis, which is done at a hospital laboratory. The assessment should be supervised by a respiratory physician. In England and Wales this conflicts with the need for home oxygen to be prescribed by the patient’s general practitioner. In Scotland arrangements are made by the respiratory specialist. Close liaison between general practice and hospital is necessary to ensure appropriate care for the patient. Often this is best organised by respiratory specialist nurses and practice nurses.
The assessments should be made with the patient in a stable state on optimal treatment and must be confirmed by a second assessment at least three weeks later. Several studies show that results from a single estimation are not always confirmed by a repeat analysis 4-12 weeks later. Although the UK criteria specify an arterial carbon dioxide pressure (Paco2) >6 kPa for treatment, it is accepted that patients with a lower Paco2 should have the same treatment. Criteria in other countries differ slightly.
Criteria for long term oxygen in different countries
| United Kingdom | Europe | United States | Australia | |
| Pao2 (kPa) | <7.3 | <7.3or 7.3-8.7 plus cor pulmonale, oedema, packed cell volume>56% | <7.3, saturation<88%or 7.3-7.9 pluscor pulmonale, oedema, packed cell volume>56% | <7.5 plus right ventricular hypertrophy, oedema, polycythaemia,saturation <90% on exercise |
| Paco2 (kPa) | >6 | |||
| FEV1 (l) | <1.5 | |||
| FVC (l) | <2.0 |
The aim of long term oxygen therapy is to maintain arterial oxygen pressure (Pao2) at 9.3-12 kPa. This is usually achieved by a flow rate of 1-3 l/min. Ideally the Pao2 should be over 10.7 kPa to allow for falls during exercise, eating, sleeping, etc.
Prescription of long term oxygen in chronic obstructive pulmonary disease
Make sure other treatment is optimal
Assess patient for suitability (smoking, compliance)
Measure blood gas concentrations with patient in a stable state
Repeat measurements 3-4 weeks later
Arrange home oxygen if appropriate
Follow up for problems and compliance (preferably respiratory nurse visiting home)
Repeat blood gas measurements at 6-12 months
Most doctors would not prescribe home oxygen for people who continue to smoke. The evidence of benefit from trials is based on non-smokers, and the danger of fire is well known.
Devices for home oxygen
Oxygen cylinders
Cylinders provided at home in the United Kingdom contain 1360 l of oxygen, which provides 11 hours of treatment at a flow rate of 2 l/min. Oxygen is supplied by retail pharmacists authorised by health authorities to supply oxygen equipment. They can deliver cylinders to the patient’s home, help with assembly, and advise on use. Oxygen cylinders are prescribed as regular general practice items with further prescriptions needed for replacement cylinders. The oxygen is stored in the cylinders at 2000 psi with a pressure regulator that allows 50 psi to the patient. The valves provided have a medium setting, which delivers 2 l/min, and a high setting, which provides 4 l/min.
Portable cylinders containing 300 l are also available, but they last for only two hours at a flow rate of 2 l/min. This can be extended with an oxygen conservation device (see below). Lightweight portable cylinders are available to minimise any extra work from carrying the equipment during exercise. Portable cylinders can be refilled at home from a source of liquid oxygen by using a special valve but not from large gas cylinders or oxygen concentrators.
Oxygen cylinders should be prescribed for intermittent use at home—that is, occasional relief of dyspnoea at rest or on exercise around the home. Cylinders need to be protected from heat, which causes an increase in their pressure. When oxygen is used for more than 8 hours a day (equivalent to 21 cylinders a month) it becomes cheaper as well as more convenient to provide an oxygen concentrator at home.
Oxygen concentrators
In oxygen concentrators a molecular sieve removes nitrogen from the air giving 95% oxygen, 5% argon. At higher flow rates the oxygen concentration drops to 85-90%. Concentrators contain a synthetic aluminium silicate (zeolite) that traps gas molecules by size and polarity. Standard concentrators are not portable and need a supply of electricity. Regular maintenance of concentrators is essential, and manufacturers’ contracts cover this. Portable concentrators that can run off a 12 volt car battery are available; they cannot be prescribed in the United Kingdom, although patients can buy them. They weigh around 10 kg and have a wheeled trolley. The concentrators should be placed in a well ventilated area with adequate tubing and with multiple outlets to increase patient freedom.
The need and use of oxygen should be monitored at least annually. Time counters on concentrators allow assessment of use, although the machine being switched on does not guarantee that the patient is using it.
Items for inclusion in prescription for oxygen concentrator
Hours of use intended each day
Oxygen flow rate
Masks or cannulae required
Need for humidification
Need for back up oxygen cylinder
In England and Wales the regional contracts are held by three commercial contractors who are responsible for installation, servicing, and emergency repair. The supplier also arranges payment for the electricity used by the concentrator and provides any accessory equipment required. When a patient requires an oxygen concentrator the doctor should phone the supplier’s freephone number (available in British National Formulary and Monthly Index of Medical Specialties). The prescription is then given to the patient to pass on to the supplier. The supplier provides health authorities with information on hours of use, and prescribers should be informed when this differs substantially from the prescribed regimen.
Liquid oxygen
Liquid oxygen provides the most flexible source of home oxygen. The reservoir contains 30 or 40 l liquid oxygen lasting 8-10 days at 2 l/min. The liquid oxygen containers are insulated and at relatively low pressure. Oxygen has a boiling point of −183°C and 1 l of liquid oxygen provides 860 l of gas. Frostbite or burns can occur from contact with the container or tubing. The reservoir is used to fill light portable cylinders containing a litre of liquid oxygen. These will run for up to 8 hours at 2 l/min. In the United States 500 000 patients have liquid oxygen but, although it is available in the United Kingdom, it cannot be supplied on standard NHS prescriptions.
Membrane separator oxygen enrichers
Membrane separator oxygen enrichers contain complex polymer membranes. They also separate water vapour so do not need to be humidified, which is an advantage for transtracheal delivery. They require little maintenance but machines currently available produce concentrations of only 30-40%.
Portable devices
Portable oxygen cylinders can increase exercise tolerance, improving quality of life and the ability to do simple tasks. They can also make it easier for patients to take their inspired oxygen for long enough each day. The lack of liquid oxygen makes portable oxygen difficult for more than occasional use in the United Kingdom. The standard portable cylinders are heavy and last only two hours at 2 l/min. Addition of a demand device can increase length of use.
Devices for delivering oxygen
Masks
Fixed performance masks provide a steady concentration of inspired oxygen that is not altered by variations in ventilation. They should always be used in patients who have chronic obstructive pulmonary disease unless the patient’s carbon dioxide pressure is known to be normal. The Fio2 delivered by variable performance masks varies with changes in the breathing pattern. They can be used when there is no danger of carbon dioxide retention. A flow rate of 2 l/minute is recommended for both types of mask. (See chapter 1 for a full description (BMJ 1998;317:798-801.)
Dangers of home oxygen
Oxygen is not explosive or combustible but enhances the speed of burning and temperature of the flame. Facial burns may occur in those who smoke
Oxygen masks can cause ulceration, soreness, or maceration of the face
Cannulae can cause drying and crusting in the nose
Carbon dioxide retention may develop during exacerbations; this possibility should be reassessed if the patient is becoming drowsy
Frostbite or burns from metal connectors can occur with liquid systems
Cannulae
Nasal cannulae are generally the best way of delivering long term oxygen. They are simple, unobtrusive, and allow eating, talking, and washing to continue relatively unheeded.
The inspired oxygen concentration does not vary much with mouth or nose breathing. However, it does vary with ventilation and inspiratory flow and can vary with time in the same patient. In patients at risk of carbon dioxide retention the reduction in minute ventilation produced by the added inspired oxygen can result in a higher effective inspired oxygen concentration with the same oxygen flow through the cannulae. In acute exacerbations of chronic obstructive pulmonary disease this can produce a vicious cycle of rising Fio2, falling ventilation, and increasing Pao2. As a rough guide 2 l/min produces an inspired oxygen concentration of 25-30%.
Oxygen saving devices
More than half of the respiratory cycle is spent on expiration, and oxygen that flows during this period is wasted. Devices to hold oxygen in a chamber or to pulse the delivery during inspiration can therefore save oxygen. This is most valuable for extending the life of portable cylinders. Reservoir systems such as the “moustache,” with a volume of 20 ml, can reduce oxygen requirements by 50-70% at rest. Pulse delivery systems can extend the life of a portable cylinder up to fourfold. They fit on to any delivery device but have no benefit when fitted on a concentrator. The inspiratory valve from the supply opens on a trigger from negative pressure generated at the start of inspiration. Flow continues for up to a second. Oxygen saving devices are not available on prescription in Britain.
Transtracheal oxygen
A cannula inserted directly in to the trachea is less visible and bypasses the dead space of the upper airway. The upper airway acts as an oxygen reservoir so that a flow rate of 0.5 l/min can be equivalent to 4 l/min by nasal cannulae. Humidification is needed at higher flow rates as the conditioning function of the nose and upper airway is bypassed.
Some side effects are associated with transtracheal oxygen. Around 10% of patients experience cough, 2% haemoptysis, and 7% subcutaneous emphysema. Mucous balls form around the catheter tip in a quarter of patients, although obstruction of the catheter is rare, as is bronchospasm related to the foreign object in the trachea.
Follow up
Patients on home oxygen have advanced disease and, in general, need regular follow up. Many of them will have severely limited exercise tolerance, and visits at home are the easiest form of follow up. A trained specialist respiratory nurse based in a hospital or a practice nurse can do this in most cases.
Compliance
Audits of oxygen prescription have generally shown that prescription often does not follow recommended guidelines. The prescription is often late in the course of the disease and the patient inadequately investigated. Most surveys suggest that fewer than the predicted number of people are receiving long term oxygen in the United Kingdom.
Patients on long term home oxygen should aim for as many hours as possible; 15 hours is the minimum effective time
Many patients fail to reach their 15 hours a day threshold for long term oxygen therapy. In some cases this is because they are given 15 hours as the target to aim for when their oxygen is prescribed. Patients should be encouraged to use the oxygen as many hours of the day as possible, with 15 hours as the minimum requirement. Home visits from the respiratory nurse help to reinforce the instructions.
Ventilatory assistance
Oxygen may be necessary at home as an adjunct to ventilatory support or nasal continuous positive airways pressure for obstructive sleep apnoea. These requirements will need to be established with careful overnight monitoring at home or in hospital. Oxygen at the required rate can be introduced into these systems by a port on or near the mask.
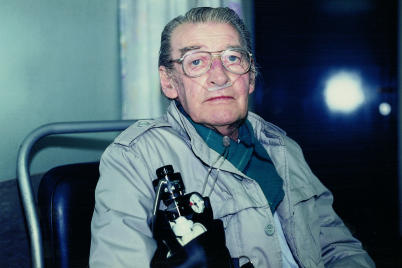
Figure.
Patient using oxygen at home
Figure.
Lightweight portable oxygen cylinder
Figure.
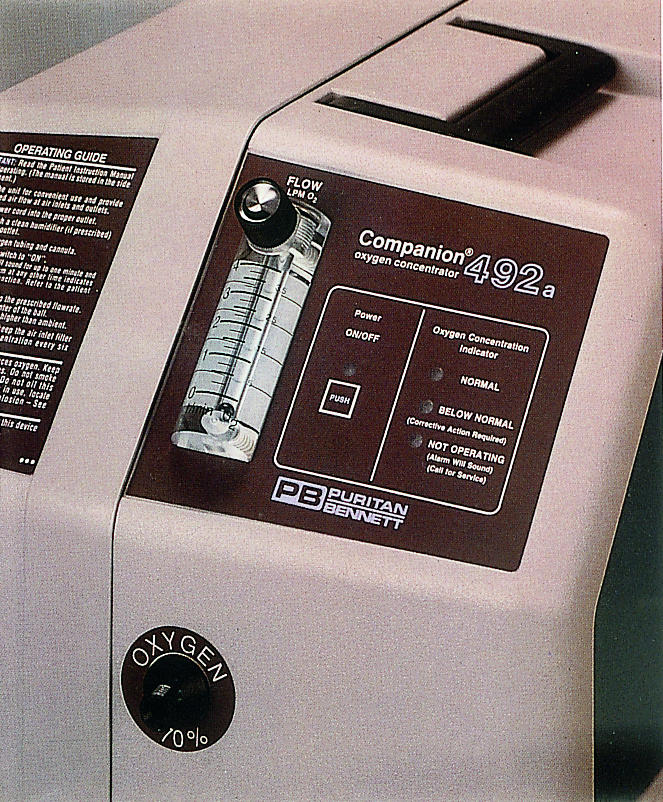

Oxygen concentrator
Figure.


With liquid oxygen, a portable container (left) can be refilled from an oxygen reservoir (right)
Figure.
Patient with portable oxygen cylinder
Figure.
Oxygen conserving device
Figure.
Patient receiving transtracheal oxygen
Figure.
Portable oxygen cylinders help patients increase their use of oxygen
Footnotes
The pictures of a liquid oxygen system are reproduced with permission of the Oxygen Therapy Company, Air Products. The picture of a patient carrying a portable oxygen cylinder is reproduced with permission of BOC Gases.
F Dudley is a general practitioner, Hurley Clinic, London
The ABC of Oxygen is edited by Richard M Leach, consultant physician, and P John Rees, consultant physician, Guy’s and St Thomas’s Hospital Trust, London.