Abstract
Background/aims
Medial tibial stress syndrome (MTSS), also known as “shin splint”, is most often described as exertional leg pain along the shinbone (tibia), which occurs due to the inflammation of the muscles, tendons, and bone tissue in this area. This study aims to assess the prevalence, risk factors, and their association with the development of MTSS, as well as the effective treatments that reduce pain and improve functions among the Saudi general population.
Materials and method
The present cross-sectional study was conducted on the general population of Saudi Arabia through an electronic survey over a period of three months. The study sample of 443 patients was deemed and considered. The study included participants from the general population in Saudi Arabia above the age of 18. A structured self-response questionnaire was given to the participants after institutional research ethical approval was obtained for the study.
Results
Among the 443 participants, the majority were male (n = 228, 51.5%), aged 18-29 (n = 227, 51.2%), and residing in the central region of Saudi Arabia (n = 398, 89.8%). Most participants reported engaging in sporting activities (n = 211, 47.6%), with high-intensity training being the most common (n = 93, 44.1%). Only a small proportion (n = 8, 1.8%) reported a previous diagnosis of MTSS. Analysis revealed associations between MTSS prevalence and certain demographic factors, including walking surface preferences and engagement in specific sports. Treatment strategies for MTSS included rest, ice application, physiotherapy, and pain-relieving medication, with varying degrees of satisfaction and recurrence rates among participants.
Conclusion
The study provides valuable insights into the prevalence, risk factors, management, and preventive measures related to MTSS among the Saudi general population. While certain demographic factors and exercise practices were associated with MTSS prevalence, effective treatment options such as rest, physiotherapy, and appropriate footwear were reported. Moreover, adherence to preventive measures such as stretching, proper footwear selection, and gradual training progression may help mitigate the risk of MTSS development.
Keywords: distal tibia, athletic leg pain, exertional leg pain, medial tibial stress syndrome, shin splints
Introduction
Medial tibial stress syndrome (MTSS), also known as “shin splint”, is most often described as exertional leg pain along the shinbone (tibia), which occurs due to the inflammation of the muscles, tendons, and bone tissue in this area [1]. Shin splints affect between 13.6% and 20% of runners and contribute to up to 60% of lower limb injuries [2]. Individuals with MTSS frequently have bilateral pain or discomfort on the medial side of the tibia, most frequently in the distal region. The discomfort is normally worse the next day, but it will subside gradually, commonly felt in the middle of the medial tibia. However, it can impact the entire length of the leg. In cases of severe and chronic MTSS [3], pain may be felt even at rest. Shin splints were seen in more females (55.3%) than males (44.7%) [4]. Training on hard surfaces or uneven surfaces, as well as footwear changes, are etiological factors in the development of shin splints [5]. Moreover, military recruits and runners are all at risk of shin splints. Those who have recently increased or adjusted their training routines, as well as those who have not adequately warmed up or have hyper-pronation of the foot, are prone to MTSS. This type of injury can interfere with an athlete's performance and all of their activities [6]. Runners who had previously sustained a running injury were more than twice as likely to experience an MTSS [7]. Individuals with a higher BMI and those who had previously worn orthotic devices for an extended period of time were shown to be more prone to developing MTSS [8]. Additionally, people with vitamin D insufficiency, osteoporosis, and flat feet are more likely to get shin splints [9]. During running, heel striking induces fast internal rotation of the tibia as the calcaneus transitions from an inverted to an everted position, resulting in traction periostitis of the soleus or flexor digitorum longus muscles, bending, and bowing of the tibia. Excessive pronation puts more strain on the posterior tibial tendon, slowing the internal rotation of the tibia and lowering the arch [5]. In another study, MTSS was associated with decreased hip internal rotation and increased ankle plantar flexion [10]. A study also found no link between the deep crural fascia, soleus, flexor digitorum longus, and tibialis at the posterior border of the tibialis, where pain showed as MTSS. Furthermore, a navicular drop was assessed with feet shoulder-width apart, and it was revealed to be significantly associated with MTSS [8]. Several investigations found reduced tibial bone mineral densities in the MTSS region, which improved to normal levels once the MTSS symptoms ceased [11,12]. Another study discovered microcracks without a repair response in biopsies collected from painful locations in athletes with MTSS, indicating decreased bone repair activity [13]. Running on hills and uneven surfaces should be avoided, but wearing the right shoes is a crucial tool in treating pes cavus, pes planus, and limiting rearfoot valgus [14]. Arch supports are often recommended to improve lower extremity biomechanics, neuromuscular coordination, muscle fatigue, and pressure distribution in the foot, hence reducing the risk of overuse injuries. Therefore, utilizing an arch support orthosis while running may be a useful method for returning the foot's pressure distribution pattern to normal [15]. Lower-limb muscular stretching has never been shown to prevent MTSS [16]. While flexibility and strength training should be started to correct any muscular imbalances, non-steroidal anti-inflammatory medicines (NSAIDs) can also be used to treat MTSS [14]. Therefore, the purpose of this study was to assess the prevalence, risk factors, and their association with the development of MTSS, as well as the effective treatments that reduce pain and improve functions among the Saudi general population.
Materials and methods
Study design
The present cross-sectional study was conducted on the general population of Saudi Arabia through an electronic survey over a period of three months. The study sample of 443 people was deemed and considered as estimated by the OpenEpi web tool (Centers for Disease Control and Prevention, Atlanta, GA) with a 95% confidence level. The study included participants from the general population in Saudi Arabia above the age of 18. The data were collected via an online questionnaire. Informed consent was obtained from all participants, and their anonymity and confidentiality were maintained throughout the study and used only for scientific research purposes. The ethical approval of the study was obtained by the chairman of the Institutional Review Board (IRB) Prof. AbdulAziz Al-Akaabba at Imam Mohammad Ibn Saud Islamic University research ethics committee in Riyadh, Saudi Arabia (reference number: 564/2023; dated: 20-3-2024).
A structured self-response questionnaire was given to the participants to assess many variables. The questionnaire evaluated a range of aspects, beginning with information regarding sociodemographics such as age, gender, height, weight, occupation, and residential areas. According to their age, the participants were divided into 18-29, 30-49, and 50 or above. Residential areas were grouped as northern, southern, eastern, western, and middle regions. Moreover, participants were asked generally about their average daily step count, usual walking surfaces, shoe types, continuous running time, whether or not they participate in any sports, and the type of sport they engage in. In addition, participants were asked about their medical condition, including their smoking habits, if they have ever been diagnosed with shin splint/medial tibial stress syndrome, foot or leg deformities "flatfoot or bowlegs'', and a family history of bone diseases or medial tibial stress syndrome, as well as fractures, surgery, or trauma related to their legs. Furthermore, shinbone conditions include pain complaints on the left, right, or both; duration of pain; treatment; preventive care; satisfaction with the management; and recurrence after obtaining the full course of management. The MTSS score consists of 15 questions, including frequency and the content of sporting activities, and the nature and description of pain after sporting activities while standing, walking, performing common daily activities, at rest, and at night [17,18].
Statistical analysis
Microsoft Excel (Microsoft® Corp., Redmond, WA) was used for collecting, cleaning, and coding the included data, while Statistical Product and Service Solutions (SPSS, version 26; IBM SPSS Statistics for Windows, Armonk, NY) was used for data analysis. Mean and standard deviation were used for ongoing variables, while frequency and percentages were used for the description of categorical variables. Chi-test, t-test, and ANOVA were used when adequate, where all statements were considered significant at a p value lower than 0.05.
Results
The study encompassed a total of 443 participants from the general population of Saudi Arabia, of which (n = 228, 51.5%) were male and (n = 215, 48.5%) were female. In terms of age distribution, the majority fell within the 18-29 age bracket, constituting (n = 227, 51.2%), followed by aged between 30 and 49 (n = 159, 35.9%) and aged 50 or older (n = 57, 12.9%). The mean height recorded was 165.65 cm (SD = 14.91), with a mean weight of 75.34 kg (SD = 19.01), resulting in an average BMI of 30.33 kg/m² (SD = 48.23). Regarding BMI categorization, 4.5% (n = 20) were underweight, 35.7% (n = 158) were of normal weight, 34.1% (n = 151) were overweight, and 25.7% (n = 114) were classified as obese. Occupationally, the majority of participants identified as students (n = 142, 32.1%), followed by office workers (n = 115, 25.9%) and unemployed individuals (n = 60, 13.5%). Healthcare workers constituted a smaller proportion (n = 13, 2.9%), while professional athletes accounted for only 0.5% (n = 2) of the sample. Additionally, the residential distribution indicated a predominance of participants from the central region (n = 398, 89.8%), with lesser representation from the eastern (n = 15, 3.4%), western (n = 22, 5%), southern (n = 5, 1.1%), and northern regions (n = 3, 0.7%) (Table 1).
Table 1. Demographic factors of the participants.
The data have been presented as count, N (%), mean, and standard deviation.
SD: Standard deviation
| Demographics | Count | N (%) | |
| Gender | Male | 228 | 51.5% |
| Female | 215 | 48.5% | |
| Age | 18-29 | 227 | 51.2% |
| 30-49 | 159 | 35.9% | |
| 50 or older | 57 | 12.9% | |
| Height (cm) | Mean (SD) | 165.65 (14.91) | |
| Weight (Kg) | Mean (SD) | 75.34 (19.01) | |
| BMI (Kg/m2) | Mean (SD) | 30.33 (48.23) | |
| BMI | Underweight | 20 | 4.5% |
| Normal weight | 158 | 35.7% | |
| Overweight | 151 | 34.1% | |
| Obese | 114 | 25.7% | |
| Occupation | Student | 142 | 32.1% |
| Office worker | 115 | 25.9% | |
| Healthcare worker | 13 | 2.9% | |
| Professional athlete | 2 | 0.5% | |
| Academic | 44 | 10.0% | |
| Farmer | 1 | 0.2% | |
| Fieldwork | 21 | 4.7% | |
| Military | 18 | 4.1% | |
| Unemployed | 60 | 13.5% | |
| Housewife | 8 | 1.8% | |
| Retired | 19 | 4.3% | |
| Residential area | Central region | 398 | 89.8% |
| Eastern region | 15 | 3.4% | |
| Western region | 22 | 5.0% | |
| Southern region | 5 | 1.1% | |
| Northern region | 3 | 0.7% | |
Concerning exercise habits, the majority of participants reported walking less than 5,000 steps per day (n = 245, 55.3%), followed by 29.6% (n = 131) walking between 5,000 and 7,500 steps. Most participants reported walking on even or hard surfaces (n = 365, 82.4%) and wearing specific running shoes (n = 237, 53.5%) during their exercise routines. Furthermore, the majority did not engage in continuous running, with 72% (n = 319) reporting no running activity per day. Among those who did engage in sports, various activities were reported, with high-intensity training (n = 93, 44.1%) and running (n = 42, 19.9%) being the most prevalent (Table 2).
Table 2. General information considering exercise practice among the participants.
The data have been presented as count and N (%).
| General Information | Count | N (%) | |
| How many steps do you walk per day? | Less than 5000 steps | 245 | 55.3% |
| 5000 to 7500 steps | 131 | 29.6% | |
| 7500 to 10000 steps | 48 | 10.8% | |
| 10000 to 12500 steps | 17 | 3.8% | |
| More than 12500 steps | 2 | 0.5% | |
| Most of the time I walk on: | Uneven surfaces (construction area, hiking) | 23 | 5.2% |
| Even or hard surfaces (treadmill, sidewalk or buildings) | 365 | 82.4% | |
| Customized surfaces (running tracks) | 37 | 8.4% | |
| Soft surfaces (sand, grass) | 18 | 4.1% | |
| Most of the time I wear: | Specific running shoes | 237 | 53.5% |
| Formal/non-specific running shoes | 125 | 28.2% | |
| Slippers | 71 | 16.0% | |
| No shoes | 10 | 2.3% | |
| What is your continues running time per day? | No running | 319 | 72.0% |
| Less than 30 min | 74 | 16.7% | |
| 30 to 45 min | 30 | 6.8% | |
| 45 to 59 min | 9 | 2.0% | |
| An hour to an hour and a half | 9 | 2.0% | |
| More than an hour and a half | 2 | 0.5% | |
| Do you play any kind of sport? | No | 232 | 52.4% |
| Yes | 211 | 47.6% | |
| What does the sport you play include? | Jumping (e.g., volleyball) | 14 | 6.6% |
| Running (e.g., football) | 42 | 19.9% | |
| High-intensity training (resistance training) | 93 | 44.1% | |
| Low-intensity training (swimming) | 34 | 16.1% | |
| Walking | 28 | 13.3% | |
Table 3 presents the prevalence of shin splints/MTSS and other associated medical conditions among the participants. The majority (n = 435, 98.2%) reported no prior diagnosis of shin splints/MTSS, while only 1.8% (n = 8) confirmed such a diagnosis. Regarding family history, 96.2% (n = 426) stated no familial occurrence of bone diseases, or MTSS, with 3.8% (n = 17) reporting a positive family history. Moreover, 91% (n = 403) denied any previous diagnosis of foot or leg deformities such as flatfoot or bowlegs, while 9% (n = 40) acknowledged such conditions. Concerning tobacco use, the majority (n = 342, 77.2%) reported never smoking, while 16.7% (n = 74) were current smokers, and 6.1% (n = 27) were former smokers. Additionally, 89.2% (n = 395) reported no history of leg-related fractures, surgeries, or traumas, while 10.8% (n = 48) confirmed experiencing such incidents, with the distribution indicating involvement of both legs (n = 13, 27.1%), the left leg (n = 19, 39.6%), and the right leg (n = 16, 33.3%).
Table 3. The prevalence of shin splint/medial tibial stress syndrome and other medical conditions.
The data have been presented as count and N (%).
| Medical Condition | Count | N (%) | |
| Have you ever been diagnosed with shin splint/medial tibial stress syndrome? | No | 435 | 98.2% |
| Yes | 8 | 1.8% | |
| Is there any family history of bone diseases or medial tibial stress syndrome? | No | 426 | 96.2% |
| Yes | 17 | 3.8% | |
| Have you ever been diagnosed with any foot or leg deformities (flatfoot or bowlegs)? | No | 403 | 91.0% |
| Yes | 40 | 9.0% | |
| Have you ever smoked tobacco? | Never | 342 | 77.2% |
| Yes, current | 74 | 16.7% | |
| Yes, but smoked in the past | 27 | 6.1% | |
| Have you had any fracture, surgery or trauma related to your leg? | No | 395 | 89.2% |
| Yes | 48 | 10.8% | |
| In which leg have you had a fracture, surgery or trauma? | Both | 13 | 27.1% |
| Left | 19 | 39.6% | |
| Right | 16 | 33.3% | |
Table 4 elucidates the prevalence and characteristics of shin pain among the participants. Of the total, 21% (n = 93) reported experiencing shin pain currently or previously, with complaints in both shins (n = 50, 53.8%), the left shin only (n = 25, 26.9%), and the right shin only (n = 18, 19.4%). Among those experiencing pain, the majority reported the most complaints in the left shin (n = 51, 54.8%). Pain distribution varied, with some experiencing pain predominantly in the high (n = 22, 23.7%), medium (n = 34, 36.6%), or lower (n = 12, 12.9%) parts of the shin, while others reported pain across the entire shin (n = 25, 26.9%). The duration of pain varied, with 21.5% (n = 20) reporting pain lasting less than six weeks and 78.5% (n = 73) experiencing pain for longer durations. Moreover, 68.8% (n = 64) of participants had not received treatment for their pain, with 31.2% (n = 29) having sought treatment. Of those treated, 58.6% (n = 17) expressed satisfaction with the management received, while 41.4% (n = 12) were not satisfied. Furthermore, 79.3% (n = 23) reported a recurrence of shin pain after completing the management course.
Table 4. Prevalence of shin pain and its characteristics.
The data have been presented as count and N (%).
| Shinbone Pain | Count | N (%) | |
| Presence of shin pain now/previously? | No | 350 | 79.0% |
| Yes | 93 | 21.0% | |
| I have complaints in: | Both shins | 50 | 53.8% |
| Only left shin | 25 | 26.9% | |
| Only right shin | 18 | 19.4% | |
| I have most complaints in: | Left shin | 51 | 54.8% |
| Right shin | 42 | 45.2% | |
| I have the pain mostly in: | High part of shin | 22 | 23.7% |
| Medium part of shin | 34 | 36.6% | |
| Lower part of shin | 12 | 12.9% | |
| Complete | 25 | 26.9% | |
| I have the pain for: | Less than 6 weeks | 20 | 21.5% |
| Less than 6 weeks | 73 | 78.5% | |
| Have you actually experienced treatment for the pain? | No | 64 | 68.8% |
| Yes | 29 | 31.2% | |
| Are you satisfied with the management you have experienced? | No | 12 | 41.4% |
| Yes | 17 | 58.6% | |
| Have the symptoms of shin pain reoccurred after the management course? | No | 6 | 20.7% |
| Yes | 23 | 79.3% | |
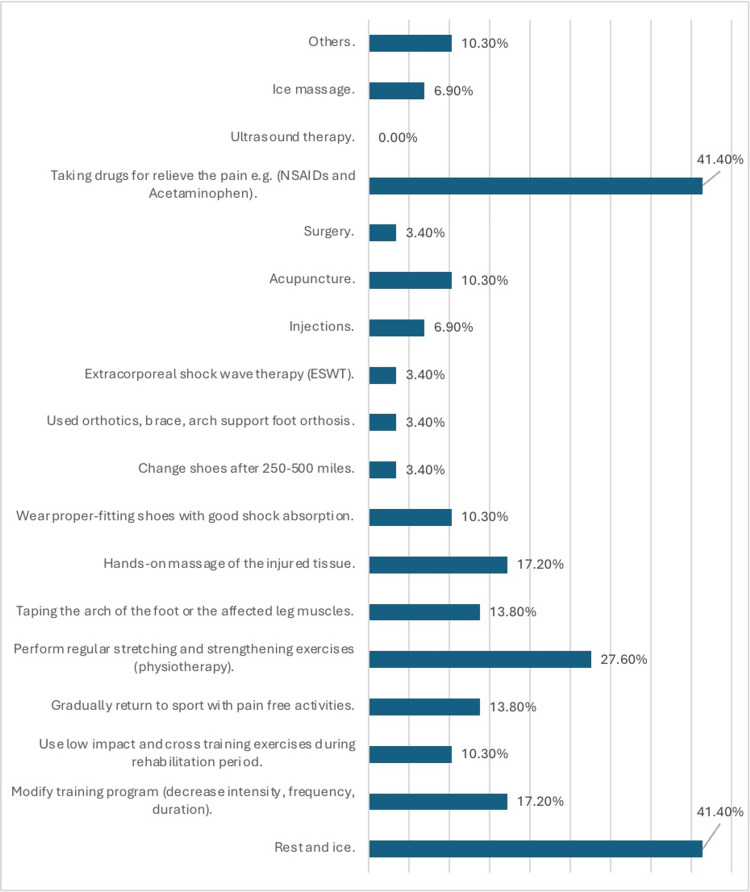
The treatment strategies reported by the 29 participants who sought treatment for shin pain are summarized in Figure 1. Common strategies included rest and ice (n = 12, 41.4%), taking pain-relieving drugs (n = 12, 41.4%), and regular stretching and strengthening exercises (n = 8, 27.6%).
Figure 1. Treatment strategies reported by 29 participants.
The data have been presented as N (%).
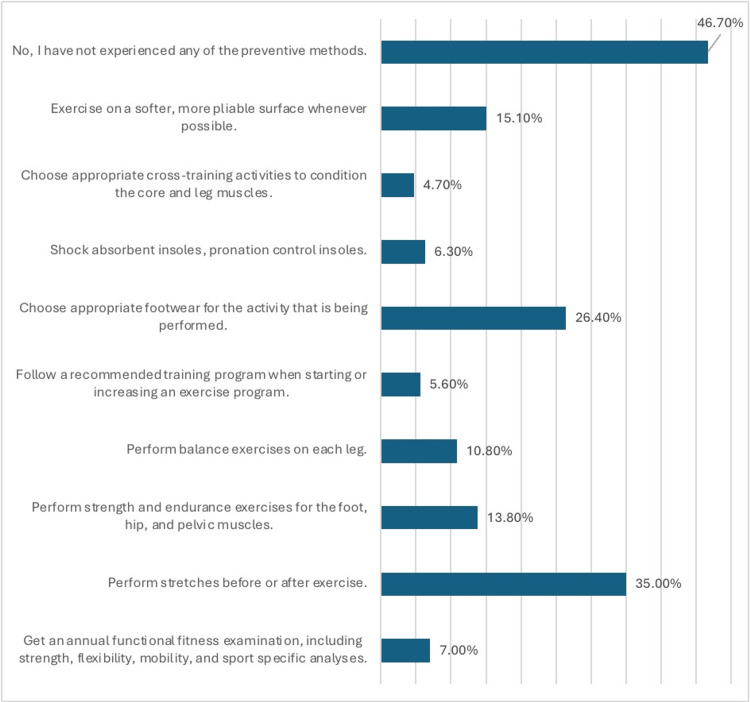
Figure 2 outlines the preventive methods for shin pain among the participants. Notable preventive measures included performing stretches before or after exercise (n = 155, 35%), choosing appropriate footwear (26.4%), and exercising on softer surfaces when possible (n = 67, 15.1%). However, 46.7% (n = 207) of the participants reported not having experienced any of the preventive methods.
Figure 2. Preventive methods for shin pain among the participants (N-443).
The data have been presented as N (%).
The assessment of participants' experiences regarding shin pain and its impact on their sporting activities revealed several significant findings. Presently, the majority (n = 381, 86%) reported being able to perform all of their usual sporting activities, while a smaller proportion reported experiencing limitations due to shin pain, with 5.9% (n = 26) being forced to reduce their activities and 1.6% (n = 7) unable to engage in any sporting activity. Additionally, participants indicated varying degrees of adjustment to their sporting activities due to shin pain, with 72.7% (n = 322) reporting no adjustments and smaller percentages (n = 45, 10.2%) reporting slight, substantial (n = 28, 6.3%), or complete adjustments (n = 22, 5%). Notably, 5.9% (n = 26) reported being unable to participate in any sporting activities due to shinbone pain. Regarding the onset and persistence of pain during sporting activities, the majority reported experiencing no pain during activities (n = 345, 77.9%), while 16.9% (n = 75) reported some pain, and 1.8% (n = 8) reported a lot of pain. When the pain did occur, it typically manifested after 15 minutes of starting the activity for 13.5% (n = 60) of participants, immediately for 3.4% (n = 15), and within the first 15 minutes for 4.5% (n = 20). However, a sizable proportion (n = 15, 3.4%) reported being unable to engage in any sporting activity due to shin pain. After engaging in sporting activities, 71.6% (n = 317) reported experiencing no pain, while 12.6% (n = 56) reported pain disappearing within 12 hours and 7% (n = 31) within 12 hours to two days. Conversely, 4.7% (n = 21) reported pain persisting for longer than two days, with 4.1% (n = 18) unable to engage in any further activities due to shin pain. Similar patterns were observed for pain experienced while standing, walking, and going up or down stairs, with varying degrees of pain reported, and a small proportion reporting being unable to engage in activities due to pain. At rest, the majority reported no pain in the shin (n = 372, 84%), while 9.7% (n = 43) reported sensitivity, and 5.4% (n = 24) reported pain. During the night, 82.8% (n = 367) reported no pain, while 9.7% (n = 43) reported occasional sensitivity, and smaller percentages reported waking up due to pain (n = 25, 5.6%) or experiencing sleep disturbances due to pain (n = 8, 1.8%). Additionally, participants reported varying degrees of pain when touching their shin, with the majority (n = 365, 82.4%) experiencing no pain, while smaller percentages reported pain when bumping (n = 31, 7%), pressing (n = 34, 7.7%), or rubbing, pressing, and bumping their shin (n = 13, 2.9%). Overall, the mean MTSS score was relatively low, indicating mild symptoms on average among participants (mean = 1.09, SD = 1.98) (Supplement Table 7).
Table 5 presents the association between the prevalence of shin splint/MTSS and demographic factors among participants. Among gender groups, a slightly higher proportion of males (n = 5, 2.2%) reported a diagnosis of shin splint/MTSS compared to females (n = 3, 1.4%), although the difference was not statistically significant (p = 0.529). Similarly, no significant associations were observed between age groups, BMI categories, occupation, residential areas, or daily step counts and the prevalence of shin splint/MTSS (all p-values > 0.05). However, significant associations were found between the prevalence of shin splint/MTSS and certain exercise-related factors. Participants who primarily walked on uneven surfaces, such as construction areas or hiking trails, exhibited a higher prevalence of shin splint/MTSS (n = 2, 8.7%) compared to those who walked on other surfaces (p = 0.017). Similarly, participants who engaged in continuous running for longer durations per day showed a higher prevalence of shin splint/MTSS, with significant differences observed between different running time categories (p = 0.000). Furthermore, participants who reported engaging in any kind of sport had a significantly higher prevalence of shin splint/MTSS (n = 7, 3.3%) compared to those who did not participate in sports (n = 1, 0.4%) (p = 0.023).
Table 5. The association between the prevalence of shin splint/medial tibial stress syndrome and demographic factors.
The data have been presented as count, N (%), and p-value.
*p value <0.05 is considered significant.
| Demographics | Have you ever been diagnosed with shin splint/medial tibial stress syndrome? | |||||
| No | Yes | |||||
| Count | N (%) | Count | N (%) | Overall p-value | ||
| Gender | Male | 223 | 97.8% | 5 | 2.2% | 0.529 |
| Female | 212 | 98.6% | 3 | 1.4% | ||
| Age | 18-29 | 224 | 98.7% | 3 | 1.3% | 0.686 |
| 30-49 | 155 | 97.5% | 4 | 2.5% | ||
| 50 or older | 56 | 98.2% | 1 | 1.8% | ||
| BMI | Underweight | 20 | 100.0% | 0 | 0.0% | 0.496 |
| Normal weight | 154 | 97.5% | 4 | 2.5% | ||
| Overweight | 150 | 99.3% | 1 | 0.7% | ||
| Obese | 111 | 97.4% | 3 | 2.6% | ||
| Occupation | Student | 141 | 99.3% | 1 | 0.7% | 0.088 |
| Office worker | 113 | 98.3% | 2 | 1.7% | ||
| Healthcare worker | 11 | 84.6% | 2 | 15.4% | ||
| Professional athlete | 2 | 100.0% | 0 | 0.0% | ||
| Academic | 43 | 97.7% | 1 | 2.3% | ||
| Farmer | 1 | 100.0% | 0 | 0.0% | ||
| Fieldwork | 20 | 95.2% | 1 | 4.8% | ||
| Military | 18 | 100.0% | 0 | 0.0% | ||
| Unemployed | 59 | 98.7% | 1 | 1.6% | ||
| Housewife | 8 | 100.0% | 0 | 0.0% | ||
| Retired | 19 | 100.0% | 0 | 0.0% | ||
| Residential area | Central region | 391 | 98.2% | 7 | 1.8% | 0.635 |
| Eastern region | 14 | 93.3% | 1 | 6.7% | ||
| Western region | 22 | 100.0% | 0 | 0.0% | ||
| Southern region | 5 | 100.0% | 0 | 0.0% | ||
| Northern region | 3 | 100.0% | 0 | 0.0% | ||
| How many steps do you walk per day? | Less than 5000 steps | 242 | 98.8% | 3 | 1.2% | 0.682 |
| 5000 to 7500 steps | 128 | 97.7% | 3 | 2.3% | ||
| 7500 to 10000 steps | 47 | 97.9% | 1 | 2.1% | ||
| 10000 to 12500 steps | 16 | 94.1% | 1 | 5.9% | ||
| More than 12500 steps | 2 | 100.0% | 0 | 0.0% | ||
| Most of the time I walk on: | Uneven surfaces (construction area, hiking) | 21 | 91.3% | 2 | 8.7% | 0.017* |
| Even or hard surfaces (treadmill, sidewalk or buildings) | 361 | 98.9% | 4 | 1.1% | ||
| Customized surfaces (running tracks) | 35 | 94.6% | 2 | 5.4% | ||
| Soft surfaces (sand, grass) | 18 | 100.0% | 0 | 0.0% | ||
| Most of the time I wear: | Specific running shoes | 233 | 98.3% | 4 | 1.7% | 0.916 |
| Formal/non-specific running shoes | 122 | 97.6% | 3 | 2.4% | ||
| Slippers | 70 | 98.6% | 1 | 1.4% | ||
| No shoes | 10 | 100.0% | 0 | 0.0% | ||
| What is your continues running time per day? | No running | 318 | 99.7% | 1 | 0.3% | 0.000* |
| Less than 30 min | 72 | 97.3% | 2 | 2.7% | ||
| 30 to 45 min | 29 | 96.7% | 1 | 3.3% | ||
| 45 to 59 min | 7 | 77.8% | 2 | 22.2% | ||
| An hour to an hour and a half | 8 | 88.9% | 1 | 11.1% | ||
| More than an hour and a half | 1 | 50.0% | 1 | 50.0% | ||
| Do you play any kind of sport? | No | 231 | 99.6% | 1 | 0.4% | 0.023* |
| Yes | 204 | 96.7% | 7 | 3.3% | ||
Table 6 presents the association between the MTSS score and demographic factors. Significant associations were found between the MTSS score and several demographic variables. Specifically, males exhibited a lower mean score (0.83) compared to females (1.37), indicating less severe symptoms among males (p = 0.004). Age was also significantly associated with the MTSS score, with older participants demonstrating higher mean scores compared to younger age groups (p = 0.000). Similarly, BMI categories showed significant associations, with higher mean scores observed among participants classified as obese (1.76) compared to those classified as underweight or of normal weight (p = 0.000). Occupation was also significantly associated with the MTSS score, with variations observed among different occupational groups (p = 0.024). Additionally, significant associations were found between the MTSS score and certain exercise-related factors, including walking surface, type of footwear worn, and engagement in sports activities (all p-values < 0.05). Participants diagnosed with a shin splint/MTSS had a substantially higher mean score (3.25) compared to those without the diagnosis (1.05) (p = 0.002), indicating more severe symptoms among individuals with a previous diagnosis.
Table 6. The association between the medial tibial stress syndrome score and demographic factors.
The data have been presented as mean, standard deviation, and p-value.
*p value <0.05 is considered significant.
| Demographics | Medial Tibial Stress Syndrome Score | |||
| Mean | Standard Deviation | Overall p-value | ||
| Gender | Male | 0.83 | 1.65 | 0.004* |
| Female | 1.37 | 2.26 | ||
| Age | 18-29 | 0.76 | 1.57 | 0.000* |
| 30-49 | 1.22 | 2.04 | ||
| 50 or older | 2.07 | 2.82 | ||
| BMI | Underweight | 1.20 | 2.53 | 0.000* |
| Normal weight | 0.59 | 1.30 | ||
| Over-weight | 1.10 | 1.94 | ||
| Obese | 1.76 | 2.48 | ||
| Occupation | Student | 0.77 | 1.74 | 0.024* |
| Office worker | 0.97 | 1.72 | ||
| Healthcare worker | 1.23 | 2.49 | ||
| Professional athlete | 1.00 | 1.41 | ||
| Academic | 1.48 | 1.98 | ||
| Farmer | 0.00 | 0.00 | ||
| Fieldwork | 0.43 | 0.81 | ||
| Military | 1.11 | 1.53 | ||
| Unemployed | 1.57 | 2.64 | ||
| Housewife | 3.00 | 3.89 | ||
| Retired | 1.58 | 2.22 | ||
| Residential area | Central region | 1.06 | 1.98 | 0.696 |
| Eastern region | 1.33 | 1.45 | ||
| Western region | 1.64 | 2.52 | ||
| Southern region | 0.80 | 1.30 | ||
| Northern region | 0.67 | 1.15 | ||
| How many steps do you walk per day? | Less than 5000 steps | 1.13 | 2.09 | 0.717 |
| 5000 to 7500 steps | 1.02 | 1.77 | ||
| 7500 to 10000 steps | 0.98 | 1.96 | ||
| 10000 to 12500 steps | 1.59 | 2.29 | ||
| More than 12500 steps | 0.00 | 0.00 | ||
| Most of the time I walk on: | Uneven surfaces (construction area, hiking) | 2.09 | 2.64 | 0.040* |
| Even or hard surfaces (treadmill, sidewalk or buildings) | 1.00 | 1.88 | ||
| Customized surfaces (running tracks) | 1.49 | 2.51 | ||
| Soft surfaces (sand, grass) | 0.83 | 1.54 | ||
| Most of the time I wear: | Specific running shoes | 0.88 | 1.74 | 0.030* |
| Formal/non-specific running shoes | 1.26 | 1.95 | ||
| Slippers | 1.59 | 2.69 | ||
| No shoes | 0.50 | 1.27 | ||
| What is your continues running time per day? | No running | 1.14 | 2.03 | 0.377 |
| Less than 30 min | 0.78 | 1.74 | ||
| 30 to 45 min | 1.10 | 2.02 | ||
| 45 to 59 min | 0.67 | 1.66 | ||
| An hour to an hour and a half | 2.22 | 2.28 | ||
| More than an hour and a half | 1.00 | 1.41 | ||
| Do you play any kind of sport? | No | 1.30 | 2.21 | 0.023* |
| Yes | 0.87 | 1.68 | ||
| Have you ever been diagnosed with shin splint/medial tibial stress syndrome? | No | 1.05 | 1.93 | 0.002* |
| Yes | 3.25 | 3.41 | ||
Discussion
The present study aimed to assess the prevalence, risk factors, and management strategies associated with MTSS, commonly known as shin splints, among the general population of Saudi Arabia. Our findings shed light on various demographic and exercise-related factors that contribute to the prevalence and severity of MTSS, providing valuable insights for preventive and management approaches.
The prevalence of MTSS in our study population was relatively low, with only 1.8% (n = 8) of participants reporting a previous diagnosis. This finding aligns with previous research indicating a relatively low prevalence of MTSS in the general population [8,19]. However, it is essential to note that the prevalence may vary across different populations and demographic groups. However, our results are lower than those reported in other studies among specific groups, particularly those who practice regular exercises, including a study by Bliekendaal et al. among first-year Dutch physical education teacher education (PETE) students, in which the prevalence of MTSS was 25% (n = 55) during the follow-up period [20]. Verrelst et al. reported a 26% (n = 21) incidence of MTSS among female PETE students over a 29-week follow-up period [21]. Sharma et al. observed an incidence of 7.9% (n = 37) among male recruits (n = 468) during a 26-week training period [22]. Rauh et al. found a 7.2% (n = 54) incidence in female Marine Corps recruits over a 13-week training period [23]. Yates et al. documented an incidence of 35% (n = 40) among 124 naval recruits, with rates of 67.7% (n = 84) for men and 32.3% (n = 40) for women, during a 10-week basic training program [24]. Bennett et al. studied 125 high school cross-country runners, noting a 12% (n = 15) incidence during an eight-week training program [25].
Our study did not find a significant association between gender, age, BMI, occupation, residential area, or daily step count and the prevalence of MTSS. This finding contradicts some previous studies that have suggested an association between certain demographic factors and the risk of MTSS. For example, a study by Yates et al. found that female gender and higher BMI were significant risk factors for developing MTSS [24]. In addition, Bliekendaal et al. showed more women developed MTSS during the follow-up period (39%) than men (21%) [20]. The lack of significant associations in our study may be attributed to the relatively small sample size or differences in population characteristics.
Interestingly, our study identified several exercise-related factors that were significantly associated with the prevalence of MTSS. Participants who primarily walked on uneven surfaces, such as construction areas or hiking trails, exhibited a higher prevalence of MTSS compared to those who walked on other surfaces. This finding is consistent with previous research highlighting the importance of training surface characteristics in the development of MTSS. Pohl et al. demonstrated that running on hard surfaces, such as concrete or asphalt, significantly increased the risk of developing MTSS compared to running on softer surfaces, such as grass or sand [26].
Moreover, participants who engaged in continuous running for longer durations per day showed a higher prevalence of MTSS. This finding underscores the potential role of training volume and intensity in the development of MTSS [8]. Several studies have suggested that excessive or rapid increases in training volume or intensity may overload the tibia and surrounding muscles, leading to the development of MTSS [13]. Therefore, gradual progression and appropriate training modifications are essential for reducing the risk of MTSS among athletes and active individuals.
Additionally, participants who reported engaging in any kind of sport had a significantly higher prevalence of MTSS compared to those who did not participate in sports. This finding highlights the impact of sports participation on the risk of MTSS, emphasizing the importance of sport-specific biomechanical factors and training techniques in MTSS development. Previous research has identified specific sports, such as running, basketball, and soccer, as high-risk activities for MTSS due to repetitive impact loading and biomechanical stress on the tibia [27].
Regarding the severity of MTSS symptoms, our study found significant associations between demographic factors and the MTSS score. Males exhibited less severe symptoms compared to females, while older participants and those classified as obese demonstrated higher MTSS scores. These findings are consistent with previous research suggesting that female gender, older age, and a higher BMI are associated with more severe MTSS symptoms [8,28,29]. The observed differences in symptom severity may be attributed to variations in biomechanical factors, muscle strength, and bone density among different demographic groups.
Furthermore, certain exercise-related factors, such as walking surface, type of footwear worn, and engagement in sports activities, were significantly associated with the MTSS score. Participants diagnosed with MTSS had substantially higher MTSS scores compared to those without the diagnosis, indicating more severe symptoms among individuals with a previous diagnosis. These findings emphasize the importance of identifying and modifying modifiable risk factors and implementing appropriate management strategies to alleviate MTSS symptoms and prevent recurrence.
For treatment options, our study revealed a variety of strategies employed by participants to alleviate the symptoms of MTSS. Among the reported treatments, rest and ice application emerged as commonly utilized approaches, aligning with established recommendations for the initial management of MTSS symptoms [30]. Furthermore, participants frequently engaged in physiotherapy involving regular stretching and strengthening exercises, which have shown efficacy in improving lower limb biomechanics and reducing pain associated with MTSS [13]. Additionally, the use of proper-fitting shoes with adequate shock absorption and the administration of pain-relieving drugs, such as NSAIDs and acetaminophen, were reported by participants as effective strategies for symptom management, consistent with current clinical guidelines [25]. However, it is imperative to acknowledge the individual variability in treatment responses and the importance of personalized approaches tailored to each patient's specific needs and circumstances.
On the other hand, preventive measures taken by participants underscored the importance of addressing modifiable risk factors to mitigate the occurrence and recurrence of MTSS. Our findings indicated that incorporating pre- and post-exercise stretching routines was a commonly adopted practice among participants, aligning with evidence suggesting the role of flexibility exercises in reducing the risk of MTSS [31]. Moreover, participants emphasized the significance of choosing appropriate footwear for their activities, including shock-absorbent insoles and pronation control features, to minimize excessive biomechanical stress on the lower limbs during physical exertion [32]. Furthermore, adhering to recommended training programs and gradually increasing exercise intensity emerged as crucial strategies to prevent overuse injuries such as MTSS, highlighting the importance of structured training regimens and progressive loading protocols in injury prevention [13]. These findings emphasize the need for comprehensive injury prevention programs that encompass education on proper training techniques, footwear selection, and biomechanical principles to optimize musculoskeletal health and reduce the burden of MTSS among athletes and active individuals.
Despite providing valuable insights into the prevalence, risk factors, and management strategies associated with MTSS among the Saudi Arabian population, several limitations should be considered when interpreting the study findings. Firstly, the cross-sectional design of the study limits the establishment of causal relationships between demographic or exercise-related factors and MTSS prevalence or severity. Additionally, reliance on self-reported data, including diagnosis of MTSS and treatment outcomes, may introduce recall bias and affect the accuracy of reported findings. Moreover, the study's reliance on an electronic survey administered to the general population may lead to sampling bias, potentially excluding individuals without internet access or those less inclined to participate in online surveys. In addition, the absence of a detailed description regarding the treatments used in the study, including information on the frequency and duration, poses a limitation. The lack of such details may interfere with the effectiveness of specific treatment approaches for MTSS, which vary depending on factors such as the frequency and duration of interventions. Therefore, future research utilizing longitudinal designs, objective measures of MTSS diagnosis and treatment outcomes, specific details on treatment, and larger more diverse samples is warranted to address these limitations and provide a more comprehensive understanding of MTSS epidemiology and management strategies to facilitate better interpretation of the research.
Conclusions
In conclusion, our study provides valuable insights into the prevalence, risk factors, and management strategies associated with MTSS among the general population of Saudi Arabia. The findings underscore the complex interplay of demographic and exercise-related factors in the development and severity of MTSS and highlight the importance of targeted preventive and management approaches. Future research should focus on further elucidating the underlying mechanisms of MTSS and evaluating the effectiveness of multifaceted interventions in reducing the burden of this common lower limb overuse injury.
Appendices
Table 7. The medial tibial stress syndrome score.
The data have been presented as count and N (%).
MTSS = Medial tibial stress syndrome
| MTSS Score | Count | N (%) | |
| Presently | I perform all of my usual sporting activities. | 381 | 86.0% |
| I am forced to do less of my usual sporting activities due to pain in my shin. | 26 | 5.9% | |
| I am forced to do alternative sporting activities only due to pain in my shin. | 7 | 1.6% | |
| I cannot do any sporting activity due to pain in my shin. | 29 | 6.5% | |
| The frequency of your sporting activities: | I have not reduced the frequency of my sporting activities. | 283 | 63.9% |
| I have reduced the frequency of my sporting activities by 1-25% a week. | 56 | 12.6% | |
| I have reduced the frequency of my sporting activities by 26-50% a week. | 30 | 6.8% | |
| I have reduced the frequency of my sporting activities by 51-75% a week. | 22 | 5.0% | |
| I have reduced the frequency of my sporting activities by 76-100% a week. | 52 | 11.7% | |
| The content of your sporting activities | I have not adjusted my sporting activity. | 322 | 72.7% |
| I have adjusted my sporting activity slightly. | 45 | 10.2% | |
| I have adjusted my sporting activities substantially | 28 | 6.3% | |
| I have adjusted the majority of my sporting activities | 22 | 5.0% | |
| I cannot do any sporting activities due to my shinbone pain | 26 | 5.9% | |
| While performing sporting activities | I have no pain in my shin. | 345 | 77.9% |
| I have some pain in my shin. | 75 | 16.9% | |
| I have a lot of pain in my shin. | 8 | 1.8% | |
| I cannot do any sporting activity, due to my shin pain. | 15 | 3.4% | |
| How long, after you have started a sporting activity, do you feel the pain in your shin? | I have no pain during sporting activities. | 333 | 75.2% |
| After 15 minutes, after I have started. | 60 | 13.5% | |
| Within the first 15 minutes after I have started. | 20 | 4.5% | |
| Immediately after I have started. | 15 | 3.4% | |
| I cannot do any sporting activity do you to my shinbone pain. | 15 | 3.4% | |
| In the case of pain being present during your sporting activities, and you continue the activity, what happens to your pain? | I have no pain during sporting activities. | 313 | 70.7% |
| The pain decreases. | 45 | 10.2% | |
| The pain remains unchanged. | 41 | 9.3% | |
| The pain increases. | 28 | 6.3% | |
| I cannot do any sporting activities due to my shinbone pain. | 16 | 3.6% | |
| If you feel pain in your shin when starting your sporting activity, and you continue the activity, what happens to your pain? | I have no pain during sporting activities. | 316 | 71.3% |
| The pain disappears within 10 minutes. | 31 | 7.0% | |
| The pain disappears after 10 minutes. | 31 | 7.0% | |
| The pain does not disappear. | 46 | 10.4% | |
| I cannot do any sporting activities due to my shinbone pain. | 19 | 4.3% | |
| After sporting activities | I have no pain. | 317 | 71.6% |
| The pain disappears within 12 hours. | 56 | 12.6% | |
| The pain disappears between 12 hours to 2 days. | 31 | 7.0% | |
| The pain remains present for longer than 2 days. | 21 | 4.7% | |
| I cannot do any sporting activity due to my shinbone pain. | 18 | 4.1% | |
| While standing | I have no pain in my shin. | 304 | 68.6% |
| I have some pain in my shin. | 110 | 24.8% | |
| I have a lot of pain in my shin. | 23 | 5.2% | |
| I cannot do any sporting activity, due to my shin pain. | 6 | 1.4% | |
| While walking | I have no pain in my shin. | 337 | 76.1% |
| I have some pain in my shin. | 90 | 20.3% | |
| I have a lot of pain in my shin. | 13 | 2.9% | |
| I cannot do any sporting activity, due to my shin pain. | 3 | 0.7% | |
| While going up or down stairs: | I have no pain in my shin. | 320 | 72.2% |
| I have some pain in my shin. | 93 | 21.0% | |
| I have a lot of pain in my shin. | 21 | 4.7% | |
| I cannot do any sporting activity, due to my shin pain. | 9 | 2.0% | |
| While performing common daily activities: | I have no pain in my shin. | 353 | 79.7% |
| I have some pain in my shin. | 76 | 17.2% | |
| I have a lot of pain in my shin. | 7 | 1.6% | |
| I cannot do any sporting activity, due to my shin pain. | 7 | 1.6% | |
| At rest (sitting or lying down), my shin is: | Not painful. | 372 | 84.0% |
| Sensitive. | 43 | 9.7% | |
| Painful. | 24 | 5.4% | |
| Very painful. | 4 | 0.9% | |
| At night: | I have no pain. | 367 | 82.8% |
| My shin is sometimes sensitive. | 43 | 9.7% | |
| I wake up sometimes because of the pain in my shin. | 25 | 5.6% | |
| I cannot sleep due to the pain in my shin for parts of the night. | 8 | 1.8% | |
| Pain while touching: | I have no pain when touching my shin. | 365 | 82.4% |
| I have pain when I bump my shin. | 31 | 7.0% | |
| I have pain when I press and when I bump my shin. | 34 | 7.7% | |
| I have pain when I rub, press and when I bump my shin. | 13 | 2.9% | |
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Faisal A. Alhazani, Majdi Hashim, Ayedh S. AlQarni, Mazen A. Albogami, Abdulrahman O. Alomar, Abdullah S. Alsultan
Acquisition, analysis, or interpretation of data: Faisal A. Alhazani, Majdi Hashim, Ayedh S. AlQarni, Mazen A. Albogami, Abdulrahman O. Alomar, Abdullah S. Alsultan
Drafting of the manuscript: Faisal A. Alhazani, Majdi Hashim, Ayedh S. AlQarni, Mazen A. Albogami, Abdulrahman O. Alomar, Abdullah S. Alsultan
Critical review of the manuscript for important intellectual content: Faisal A. Alhazani, Majdi Hashim, Ayedh S. AlQarni, Mazen A. Albogami, Abdulrahman O. Alomar, Abdullah S. Alsultan
Supervision: Faisal A. Alhazani, Majdi Hashim, Mazen A. Albogami
Human Ethics
Consent was obtained or waived by all participants in this study. Imam Mohammad Ibn Saud Islamic University Research Ethics Committee Institutional Review Board (IRB) issued approval 564/2023. The ethical approval of the study was obtained by the chairman of the Institutional Review Board (IRB) Prof. AbdulAziz Al-Akaabba at Imam Mohammad Ibn Saud Islamic University research ethics committee in Riyadh, Saudi Arabia via reference number 564/2023. Dated: 20-3-2024. Session no. 66. Protocol is accepted.
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Medial tibial stress syndrome: a review article. Deshmukh NS, Phansopkar P. Cureus. 2022;14:0. doi: 10.7759/cureus.26641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Is high soleus muscle activity during the stance phase of the running cycle a potential risk factor for the development of medial tibial stress syndrome? A prospective study. Naderi A, Moen MH, Degens H. J Sports Sci. 2020;38:2350–2358. doi: 10.1080/02640414.2020.1785186. [DOI] [PubMed] [Google Scholar]
- 3.Rectus femoris muscle injuries in football: a clinically relevant review of mechanisms of injury, risk factors and preventive strategies. Mendiguchia J, Alentorn-Geli E, Idoate F, Myer GD. Br J Sports Med. 2013;47:359–366. doi: 10.1136/bjsports-2012-091250. [DOI] [PubMed] [Google Scholar]
- 4.Prevalence of shin splint in recreational marathon runner. Patel PY, Patil N. https://pesquisa.bvsalud.org/portal/resource/pt/sea-205777 Int J Physiother. 2020;7 [Google Scholar]
- 5.Biomechanical risk factors in the development of medial tibial stress syndrome in distance runners. Tweed JL, Campbell JA, Avil SJ. J Am Podiatr Med Assoc. 2008;98:436–444. doi: 10.7547/0980436. [DOI] [PubMed] [Google Scholar]
- 6.The effects of self-myofascial release using a foam roll or roller massager on joint range of motion, muscle recovery, and performance: a systematic review. Cheatham SW, Kolber MJ, Cain M, Lee M. http://www.ncbi.nlm.nih.gov/pubmed/26618062. Int J Sports Phys Ther. 2015;10:827–838. [PMC free article] [PubMed] [Google Scholar]
- 7.Medial tibial stress syndrome in high school cross-country runners: incidence and risk factors. Plisky MS, Rauh MJ, Heiderscheit B, Underwood FB, Tank RT. J Orthop Sports Phys Ther. 2007;37:40–47. doi: 10.2519/jospt.2007.2343. [DOI] [PubMed] [Google Scholar]
- 8.Risk factors associated with medial tibial stress syndrome in runners: a systematic review and meta-analysis. Newman P, Witchalls J, Waddington G, Adams R. Open Access J Sports Med. 2013;4:229–241. doi: 10.2147/OAJSM.S39331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vitamin D and stress fractures in sport: preventive and therapeutic measures-a narrative review. Knechtle B, Jastrzębski Z, Hill L, Nikolaidis PT. Medicina (Kaunas) 2021;57:223. doi: 10.3390/medicina57030223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Common leg injuries of long-distance runners: anatomical and biomechanical approach. Gallo RA, Plakke M, Silvis ML. Sports Health. 2012;4:485–495. doi: 10.1177/1941738112445871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abnormally decreased regional bone density in athletes with medial tibial stress syndrome. Magnusson HI, Westlin NE, Nyqvist F, Gärdsell P, Seeman E, Karlsson MK. Am J Sports Med. 2001;29:712–715. doi: 10.1177/03635465010290060701. [DOI] [PubMed] [Google Scholar]
- 12.Low regional tibial bone density in athletes with medial tibial stress syndrome normalizes after recovery from symptoms. Magnusson HI, Ahlborg HG, Karlsson C, Nyquist F, Karlsson MK. Am J Sports Med. 2003;31:596–600. doi: 10.1177/03635465030310042001. [DOI] [PubMed] [Google Scholar]
- 13.Microcrack-associated bone remodeling is rarely observed in biopsies from athletes with medial tibial stress syndrome. Winters M, Burr DB, van der Hoeven H, Condon KW, Bellemans J, Moen MH. J Bone Miner Metab. 2019;37:496–502. doi: 10.1007/s00774-018-0945-9. [DOI] [PubMed] [Google Scholar]
- 14.Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Wilder RP, Sethi S. Clin Sports Med. 2004;23:55–81. doi: 10.1016/S0278-5919(03)00085-1. [DOI] [PubMed] [Google Scholar]
- 15.Arch-support foot-orthoses normalize dynamic in-shoe foot pressure distribution in medial tibial stress syndrome. Naderi A, Degens H, Sakinepoor A. Eur J Sport Sci. 2019;19:247–257. doi: 10.1080/17461391.2018.1503337. [DOI] [PubMed] [Google Scholar]
- 16.Medial tibial stress syndrome: evidence-based prevention. Craig DI. J Athl Train. 2008;43:316–318. doi: 10.4085/1062-6050-43.3.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The medial tibial stress syndrome score: a new patient-reported outcome measure. Winters M, Moen MH, Zimmermann WO, Lindeboom R, Weir A, Backx FJ, Bakker EW. Br J Sports Med. 2016;50:1192–1199. doi: 10.1136/bjsports-2015-095060. [DOI] [PubMed] [Google Scholar]
- 18.The medial tibial stress syndrome score: item generation for a new patient reported outcome measure. Winters M. https://www.researchgate.net/publication/307937886_The_medial_tibial_stress_syndrome_score_item_generation_for_a_new_patient_reported_outcome_measure South African J Sport Med. 2017;28:11–16. [Google Scholar]
- 19.Medial tibial stress syndrome and female military recruits. Pulsone R, Williams C. Health (Irvine Calif) 2022;14:273–280. [Google Scholar]
- 20.Incidence and risk factors of medial tibial stress syndrome: a prospective study in physical education teacher education students. Bliekendaal S, Moen M, Fokker Y, Stubbe JH, Twisk J, Verhagen E. BMJ Open Sport Exerc Med. 2018;4:0. doi: 10.1136/bmjsem-2018-000421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Contralateral risk factors associated with exertional medial tibial pain in women. Verrelst R, De Clercq D, Willems TM, Roosen P, Witrouw E. Med Sci Sports Exerc. 2014;46:1546–1553. doi: 10.1249/MSS.0000000000000280. [DOI] [PubMed] [Google Scholar]
- 22.Biomechanical and lifestyle risk factors for medial tibia stress syndrome in army recruits: a prospective study. Sharma J, Golby J, Greeves J, Spears IR. Gait Posture. 2011;33:361–365. doi: 10.1016/j.gaitpost.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 23.Selected static anatomic measures predict overuse injuries in female recruits. Rauh MJ, Macera CA, Trone DW, Reis JP, Shaffer RA. Mil Med. 2010;175:329–335. doi: 10.7205/milmed-d-09-00158. [DOI] [PubMed] [Google Scholar]
- 24.The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. Yates B, White S. Am J Sports Med. 2004;32:772–780. doi: 10.1177/0095399703258776. [DOI] [PubMed] [Google Scholar]
- 25.Factors contributing to the development of medial tibial stress syndrome in high school runners. Bennett JE, Reinking MF, Pluemer B, Pentel A, Seaton M, Killian C. J Orthop Sports Phys Ther. 2001;31:504–510. doi: 10.2519/jospt.2001.31.9.504. [DOI] [PubMed] [Google Scholar]
- 26.Biomechanical predictors of retrospective tibial stress fractures in runners. Pohl MB, Mullineaux DR, Milner CE, Hamill J, Davis IS. J Biomech. 2008;41:1160–1165. doi: 10.1016/j.jbiomech.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 27.The incidence and distribution of stress fractures in competitive track and field athletes. A twelve-month prospective study. Bennell KL, Malcolm SA, Thomas SA, Wark JD, Brukner PD. Am J Sports Med. 1996;24:211–217. doi: 10.1177/036354659602400217. [DOI] [PubMed] [Google Scholar]
- 28.Studying the relation between medial tibial stress syndrome and anatomic and anthropometric characteristics of military male personnel. Sobhani V, Shakibaee A, Khatibi Aghda A, Emami Meybodi MK, Delavari A, Jahandideh D. Asian J Sports Med. 2015;6:0. doi: 10.5812/asjsm.23811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Medial tibial stress syndrome: the relationship between gender and lower-extremity functional performance among collegiate track and field athletes. Sievers ME, Busch AM. Intern J Sport Med Rehabil. 2021;16 [Google Scholar]
- 30.Medial tibial stress syndrome: conservative treatment options. Galbraith RM, Lavallee ME. Curr Rev Musculoskelet Med. 2009;2:127–133. doi: 10.1007/s12178-009-9055-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Current concepts in muscle stretching for exercise and rehabilitation. Page P. http://www.ncbi.nlm.nih.gov/pubmed/22319684. Int J Sports Phys Ther. 2012;7:109–119. [PMC free article] [PubMed] [Google Scholar]
- 32.The impact of stretching on sports injury risk: a systematic review of the literature. Thacker SB, Gilchrist J, Stroup DF, Kimsey CD Jr. Med Sci Sports Exerc. 2004;36:371–378. doi: 10.1249/01.mss.0000117134.83018.f7. [DOI] [PubMed] [Google Scholar]