The number of people travelling to the high altitude regions, especially South America, Nepal, and India, has risen enormously in the past 10 years. Without special climbing ability these trekkers can be exposed to altitudes they will not have encountered in their home countries. For example, the height of Everest base camp is 5500 m whereas the top of Mount Blanc, the highest mountain in the Alps, is only 4800 m. The areas with the highest mountains are also the areas with the poorest facilities, especially for medical care. Trekkers must therefore understand the effects of altitude on their bodies (hypoxia, cold, and dehydration), the processes of acclimatisation, and prophylaxis against and treatment of altitude illness.
High altitude can also be a problem for people with cardiopulmonary disease, many of whom take long haul flights on commercial aircraft. They need to know how their condition can be affected by the cabin altitude of the aeroplane (typically 1800-2500 m). If there is any doubt they should be assessed before travel to determine whether their condition is likely to worsen significantly during flight.
Oxygen availability and altitude
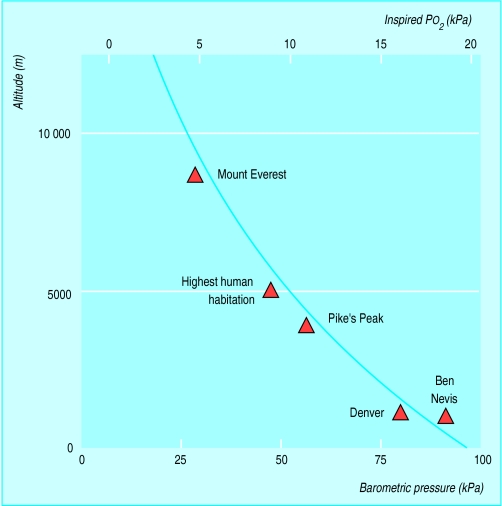
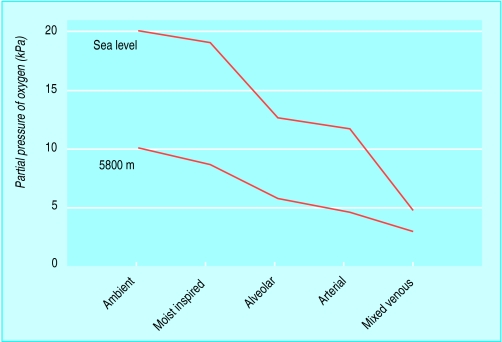
Although the percentage of oxygen in inspired air is constant at different altitudes, the fall in atmospheric pressure at higher altitude decreases the partial pressure of inspired oxygen and hence the driving pressure for gas exchange in the lungs. An ocean of air is present up to 9-10 000 m, where the troposphere ends and the stratosphere begins. The weight of air above us is responsible for the atmospheric pressure, which is normally about 100 kPa at sea level. This atmospheric pressure is the sum of the partial pressures of the constituent gases, oxygen and nitrogen, and also the partial pressure of water vapour (6.3 kPa at 37°C). As oxygen is 21% of dry air, the inspired oxygen pressure is 0.21×(100−6.3)=19.6 kPa at sea level.
Atmospheric pressure and inspired oxygen pressure fall roughly linearly with altitude to be 50% of the sea level value at 5500 m and only 30% of the sea level value at 8900 m (the height of the summit of Everest). A fall in inspired oxygen pressure reduces the driving pressure for gas exchange in the lungs and in turn produces a cascade of effects right down to the level of the mitochondria, the final destination of the oxygen.
Physiological effects of altitude
Lung
Hypoxic ventilatory response
At sea level carbon dioxide is the main stimulus to ventilation. At altitude hypoxia does increase ventilation, but usually only when the inspired oxygen pressure is reduced to about 13.3 kPa (3000 m altitude). At this inspired oxygen pressure the alveolar oxygen pressure is about 8 kPa, and with further increases in hypoxia ventilation rises exponentially. This hypoxic ventilatory response is mediated by the carotid body, and response varies widely among subjects. Interestingly, however, the ability to tolerate altitude does not seem to relate to the presence of a brisk hypoxic ventilatory response. Some climbers with poor hypoxic ventilatory response do particularly well—for example, Peter Habeler, who in 1978 became (with Rheinhold Messner) the first to climb Everest without oxygen.
Pulmonary circulation
In the systemic circulation hypoxia acts as a vasodilator, but in the pulmonary circulation it is a vasoconstrictor. The purpose of hypoxic pulmonary vasoconstriction is unclear. It may help match ventilation and perfusion within the lung, but in hypoxia of altitude the reflex leads to pulmonary hypertension and is associated with high altitude pulmonary oedema.
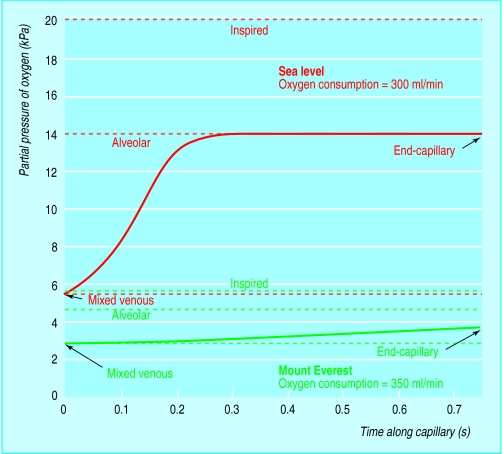
Gaseous diffusion
At sea level gaseous diffusion is probably limited by ventilation-perfusion matching in the lung. At high altitude, however, the alveolar-arterial difference for oxygen is higher than would be predicted from the measured ventilation-perfusion inequality. This is because the decreased driving pressure for oxygen from alveolar gas into arterial blood is insufficient to fully oxygenate the blood as it passes through the pulmonary capillaries. This is more evident on exercise as cardiac output increases and blood spends less time at the gas exchanging surface (diffusion limitation).
Heart
The heart works remarkably well at altitude. Initially there is an increase in cardiac output in relation to physical work but later this settles to sea level values. At all times there is increased heart rate and decreased stroke volume for a given level of work, though the maximum obtainable heart rate falls as higher altitudes are reached.
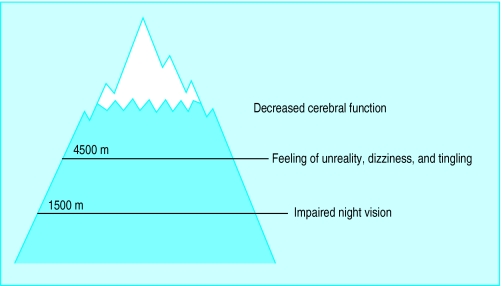
Brain
Hypoxia has progressive effects on the functioning of the central nervous system. Accidents that occur at extreme altitude on Everest and other mountains may be due to poor judgment as a consequence of hypoxic depression of cerebral function. More worrying is that these effects on cerebral function may be permanent. The American Medical Research Expedition to Everest studied its climbers a year after return to sea level and found some enduring abnormalities of cognitive function and ability to perform fast repetitive movements, although most functions tested had returned to pre-expedition values.
Blood
Initially on travelling to altitude haemoglobin concentrations rise through a fall in the plasma volume due to dehydration. Later, hypoxia stimulates production of erythropoietin by the juxtaglomerular apparatus of the kidney so haemoglobin production increases and haemoglobin concentrations may rise to 200 g/l. The increased viscosity of the blood coupled with increased coagulability increases the risk of stroke and venous thromboembolism. Some authors advocate regular venesection in high altitude climbs; others recommend prophylactic aspirin. Neither has been shown scientifically to reduce the incidence of venous or arterial thrombosis.
Acclimatisation
Adequate acclimatisation is essential for safe travelling in the mountains. The climbers adage is “climb high and sleep low.” Ideally acclimatisation should be progressive. At altitudes above 3000 m individuals should climb no more than 300 m per day with a rest day every third day. Anyone suffering symptoms of acute mountain sickness should stop, and if symptoms do not resolve within 24 hours descend at least 500 m.
There can be a tendency, particularly on commercial expeditions, to push on at a rate that is too fast for weaker members of the group. This is dangerous, and the rate of ascent should be set to that of the slowest members of the party.
Recognising altitude related illness
Acute mountain sickness
Acute mountain sickness is self limiting and usually affects previously healthy individuals who go too rapidly to altitude. There may be no symptoms for the first 12-24 hours. Thereafter symptoms develop and usually peak on the second or third day. Symptoms include headache, anorexia, insomnia, and breathlessness. The cause of acute mountain sickness is not understood but is clearly related to hypoxia and factors such as effort, air temperature, previous viral respiratory tract infection, and innate susceptibility. The incidence is quite high. Work at Pheriche, Nepal (4343 m) in 1979 found that 43% of trekkers passing through were experiencing symptoms.
High altitude pulmonary oedema
This life threatening condition may or may not be preceded by symptoms of acute mountain sickness. Breathlessness increases progressively accompanied by a cough productive of white sputum, which is occasionally tinged with blood. Examination will reveal cyanosis and a mild fever (no more than 38.5°C). Left untreated this condition can progress rapidly and be fatal.
Clinical features of high altitude cerebral oedema
Severe headache
Cerebellar ataxia
Irrationality
Hallucinations
Retinal haemorrhages
• Papilloedema
The cause is unknown, but it is related to hypoxic pulmonary vasoconstriction. Those affected have a high pulmonary artery pressure and excess hypoxic pulmonary vasoconstriction at sea level. Calcium antagonists and vasodilators can both treat and prevent high altitude pulmonary oedema.
High altitude cerebral oedema
This is the more malignant form of acute mountain sickness. The symptoms can mimic those of hypothermia, and body temperature should be measured if there is any doubt. If left untreated patients will become unconscious and die.
Treatment
Symptoms of mountain sickness must be taken seriously and subjects must go no higher until the symptoms resolve. If the symptoms do not resolve the patient should descend. Often a descent of only 500 m will greatly improve symptoms. There are also some pharmacological measures which can help.
It is better to prevent mountain sickness than to treat it
Acute mountain sickness
Acute mountain sickness can be prevented in some people by the carbonic anhydrase inhibitor acetazolamide. The studies have been done using acetazolamide at 250 mg twice daily, but I have found 125 mg twice daily sufficient. If acute mountain sickness develops it should be treated with paracetamol and subjects should travel no higher until the symptoms resolve.
High altitude pulmonary oedema
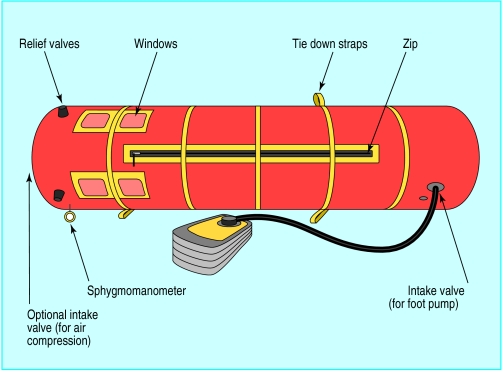
High altitude pulmonary oedema should be treated with nifedipine 20 mg 8 hourly, oxygen, and a Gamow bag if available. The Gamow bag is a portable hyperbaric chamber which allows the environmental pressure around the subject to be increased equivalent to a descent of up to 600 m. This can often improve symptoms considerably, but they will worsen once the subject is taken out of the bag to facilitate descent.
High altitude cerebral oedema
Oxygen and descent with or without a Gamow bag are the mainstay of treatment of high altitude cerebral oedema. Dexamethasone has also been shown to be useful; 8 mg should be given immediately and then 4 mg every 8 hours until the subject can be got to lower altitude.
Use of oxygen at extreme altitude
At extreme altitude (5500-8848 m) supplementary oxygen can be used to prevent the effects of severe hypoxia. Although Everest has been climbed without oxygen, most climbers use supplementary oxygen above 6500 m. However, it is difficult and expensive to arrange oxygen supplies so flow rates are kept low. The oxygen is used when sleeping, normally at 1-2 l/min via a face mask, and when climbing above 8000 m, normally 2-3 l/min. Oxygen is rarely used on mountains other than Everest.
Patients with heart and lung disease
Travelling to high altitude areas
Patients with well controlled heart or lung disease may ask whether it is safe to travel at altitude. The evidence as far as heart disease is concerned is encouraging. There are few reports of sudden cardiac death among trekkers or significant deterioration in cardiac symptoms at altitude. Patients who have had a myocardial infarct or coronary artery bypass graft are probably safe to travel if they remain well three months after their operation or infarct. Patients with cardiac failure can travel providing they are capable of heavy exertion at sea level without difficulty. Patients with systemic hypertension also seem to be safe at altitude. In a study of 935 patients there was no increase in incidence of stroke or cardiac failure in patients with systemic hypertension. Indeed, systemic blood pressure in patients with systemic hypertension falls up to altitudes of 3000 m. No studies have been done on patients with intracardiac shunts. However, patients with unclosed shunts should not travel to altitude as vasoconstriction will change the character of the shunt.
Precautions for asthmatic patients
Increase the prophylactic dose of steroids
Carry a course of oral steroids (prednisolone 30 mg daily for two weeks)
Take a plentiful supply of inhalers
Conditions which require oxygen for air travel
Severe but stable chronic obstructive pulmonary disease (FEV1<1 l, Po2<9 kPa breathing air)
Severe but stable chronic heart failure (New York Heart Association grade III)
Patients with asthma usually do well. Allergen exposure is often less, but the cold, dry air of altitude may worsen asthma. It is more difficult to advise patients with chronic obstructive pulmonary disease. Ideally they should be fully assessed in a respiratory clinic before departure. In particular, gas exchange should be measured as this deteriorates with altitude.
Air travel
Commercial aircraft are pressurised but only to an altitude of 1800-2500 m, and inspired oxygen pressure will be lower than at sea level. This usually has little effect because patients do not exercise during the flight. However, in some patients the reduction in inspired oxygen pressure is critical and additional oxygen may be necessary. Ideally the patient should be assessed in a respiratory clinic before travelling, lung function optimised, and ability to withstand hypoxia tested. However, few units have the low oxygen mixture necessary for this testing and extrapolations have to be made from sea level blood gas concentrations. As a rule of thumb patients should have an arterial oxygen pressure breathing air greater than 9 kPa at sea level to give them an Pao2 at 1500 m above 6.7 kPa.
Cost of inflight oxygen (from Breathe Easy 1997;24:5)
| Airline | Cost of oxygen |
| Air Canada | £38 each way |
| Cathay Pacific | No charge |
| Virgin Atlantic | No charge |
| Caledonian | £42 each way |
| British Airways | £200 return |
| Alitalia | Cost of air fare |
| Singapore Air | 50% cost of air fare |
| Air Malta | No charge |
Studies have shown that as long as patients with serious cardiopulmonary disease are assessed before travel and supplementary oxygen used if necessary the incidence of serious side effects is low during flight. The availability and cost of oxygen on commercial aircraft varies.
Patients with heart and lung disease should contact their doctors early and arrange specialised assessment if necessary. Arrangements for oxygen can be made through the airline reservations office or the medical unit for British Airways. The airline will require a medical form filled in by the general practitioner. Oxygen can be supplied via a Hudson mask (patients using venturi masks or nasal cannulae can bring these with them) at flows up to 4 l/min.
Figure.

Climbing Everest
Figure.
Relation between altitude and inspired oxygen pressure
Figure.
Partial pressure of oxygen in ambient air through to mixed venous blood varies with altitude. Diagram shows representative resting levels at sea level and 5800 m
Figure.
Calculated time course for change in partial pressure of oxygen in pulmonary capillary. At sea level oxygen pressure reaches almost alveolar levels in a third of available time. At the summit of Mount Everest the mixed venous oxygen pressure is lower and never reaches alveolar levels
Figure.
Effect of hypoxia on central nervous system
Figure.
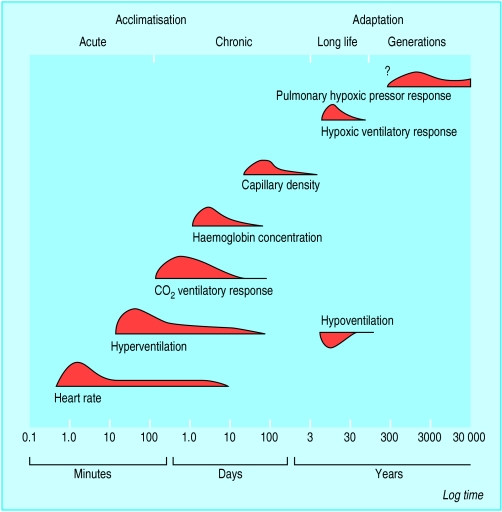
Time course of acclimatisation and adaptive changes plotted on log time scale. The curve of each response denotes the rate of change
Figure.
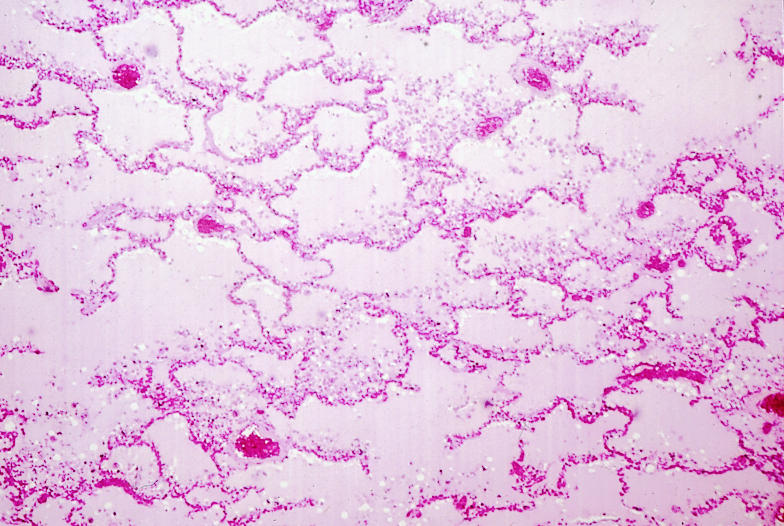
Acute high altitude pulmonary oedema
Figure.
Gamow bag
Figure.

Using low flow oxygen while sleeping at altitude
Figure.
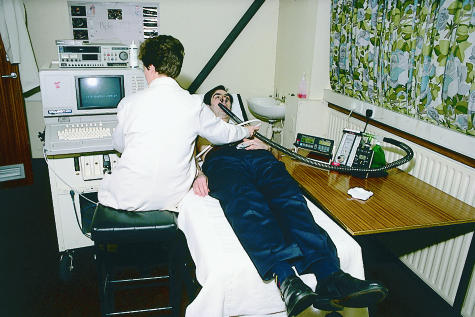
Patient having echocardiography to assess pulmonary pressure response to hypoxia
Footnotes
Andrew J Peacock is consultant physician, department of respiratory medicine, West Glasgow Hospitals University NHS Trust, Glasgow
The ABC of Oxygen is edited by Richard M Leach, consultant physician, department of intensive care, and P John Rees, consultant physician, department of respiratory medicine, Guy’s and St Thomas’s Hospitals Trust, London
The diagram of altitude and inspired oxygen pressure is reproduced with permission from West JB. Respiratory physiology: the essentials. Baltimore: Williams and Wilkins. 1979. The diagram of acclimatisation is reproduced with permission from Ward MP, Milledge JS, and West JB. High altitude medicine and physiology. London: Chapman and Hall, 1995.