Abstract
Introduction
Colonic lipomas (CL) are rare non-epithelial benign tumors. Giant Colonic lipomas (>4 cm) can cause serious complications such as bowel obstruction, massive bleeding, perforation, and intussusception. Early diagnosis is difficult and preoperative discrimination between malignant lesions and large cl is challenging. Surgical resection is the cornerstone of the treatment.
Case presentation
A 57-year-old woman presented to our surgical department complaining about intermittent crampy abdominal pain with an alternation of diarrhea and constipation for the last 7 months. After radiological and endoscopic investigations, the diagnosis of colo-colonic intussusception caused by colonic lipoma was confirmed. The patient underwent laparoscopic enucleation and a histopathological examination of the specimen confirmed the diagnosis of colonic lipoma.
Discussion
Colonic lipomas (CL), though rare (0.2 to 4 %), are the third most common benign colon tumors. Typically affecting adult women (57 %), these non-epithelial growths can vary in size from 2 mm to 30 cm, often remaining asymptomatic until complications arise. Colonic lipomas may lead to intussusception or bowel obstruction, with clinical presentation depending on size and location. Diagnosis relies on abdominal CT scans or MRI, while treatment options include surveillance, endoscopic, or surgical resection. Laparoscopic approaches offer favorable postoperative outcomes, although precise localization remains a challenge. Endoscopic techniques are limited, particularly for larger or difficult-to-access lipomas, necessitating expert care.
Conclusion
Giant colonic lipoma can cause colonic intussusception leading to emergency operation. We think that laparoscopic enucleation seems to be the ideal treatment choice, especially when the malignancy cannot be excluded.
Keywords: Colonic lipoma-endoscopy-enucleation-intussusception, Laparoscopy-mesh
Highlights
-
•
The rarity of the case: Emphasizing the exceptional occurrence of colo-colonic intussusception due to a large colonic lipoma in a 57-year-old woman.
-
•
The importance of imaging: Emphasizing the crucial role of imaging techniques.
-
•
Adequate management and successful laparoscopic approach: Highlighting the efficacy of laparoscopic management in this complex scenario, showcasing successful enucleation of the colonic lipoma to treat the intussusception.
1. Introduction
Intussusception, a rare condition in adults, involves the telescoping of one segment of the bowel into another. This phenomenon was first described by Barbette of Amsterdam in 1674 [1]. Despite its rarity, intussusception accounts for up to 5 % of gastrointestinal obstructions and has an overall annual incidence of around 2–3 cases per 1,000,000 of the general population [2]. Concurrently, lipomas in the gastrointestinal tract are also infrequent. Baurer was the first to describe these benign tumors, which are reported in only 0.2 %–4.4 % of previous autopsy studies [3,4]. Lipomas, the second most common benign tumors in the small bowel, primarily occur in the ileum and duodenum. They are typically asymptomatic and do not require treatment. However, in some cases, large CLs can lead to serious complications such as bowel obstruction, massive bleeding, perforation, and intussusception. Early diagnosis of CLs is challenging, and preoperative differentiation between malignant lesions and large CLs poses difficulties. In this context, we present a case of successful laparoscopic enucleation of a giant colonic lipoma.
This case report has been reported in line with the SCARE Criteria 2023 [5].
2. Case presentation
A 57-year-old woman was admitted to our surgical department due to intermittent abdominal pain accompanied by alternating episodes of diarrhea and constipation over the past 7 months. Her medical history included hypertension and dyslipidemia, with no reported appetite or weight loss. There was no familial medical history noted. Physical examination and per rectal examination were unremarkable, and laboratory results fell within normal ranges.
Colonoscopy revealed a large polypoid non-pedunculated submucosal mass, suggesting a submucosal lipoma near the right colonic flexure, occupying approximately 2/3 of the colonic lumen (Fig. 1). A substantial biopsy confirmed the presence of a lipoma.
Fig. 1.

Colonoscopy showed a hemispherical tumor located at the right colonic flexure. The lesion was soft and compressible covered with normal mucosa.
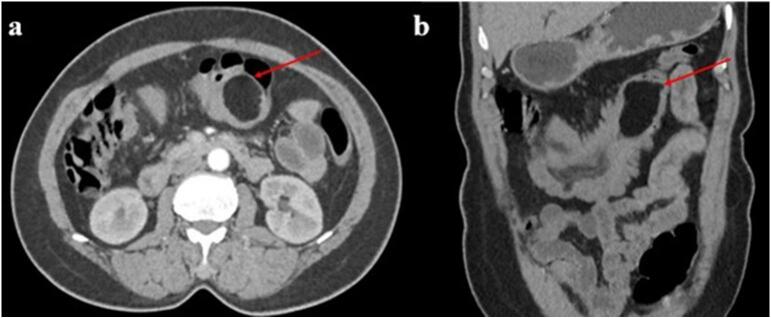
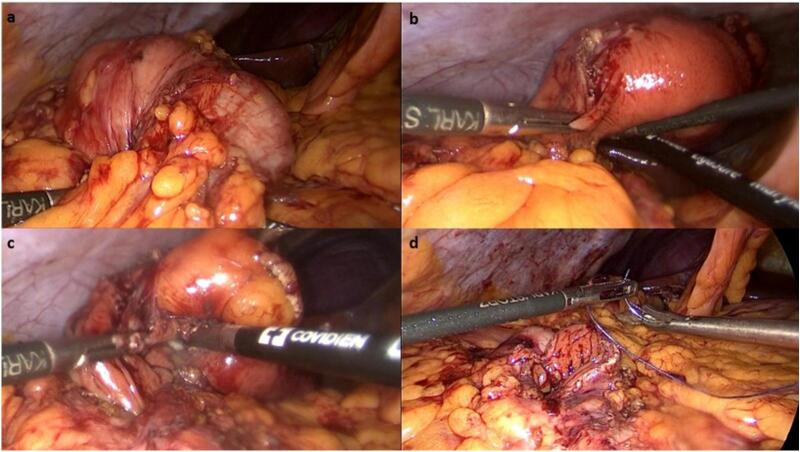
To rule out other synchronous lesions of the ascending colon, CT colonography was performed, showing colo-colonic intussusception of the right transverse colon caused by an ovoid homogeneous fatty density lesion measuring 5 cm ∗ 4.4 cm (Fig. 2). Due to the large size of the lipoma, laparoscopic surgery was performed, revealing colo-colonic intussusception of the right transverse colon. Laparoscopic enucleation was carried out by an expert colorectal surgeon, and colotomy was repaired with an intracorporeal two-layer hand-sewn suture (Fig. 3). Histological examination confirmed the diagnosis of a lipoma.
Fig. 2.
The Axial (a) and coronal (b) CT scan of the abdomen showed colo-colonic intussusception in the level of the right transversal colon caused by an ovoid homogeneous fatty density lesion (the red arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 3.
Initial laparoscopic exploration reveals a colo-colonic intussusception (a) secondary to a giant yellowish submucosal colonic mass (b, c). The laparoscopic enucleation was made and the colotomy was sutured (d).
The postoperative course was uneventful, and the patient was discharged home five days later. She remains well and asymptomatic after one year of follow-up.
3. Discussion
We present an unusual case of laparoscopic management of a giant colonic lipoma inducing colo-colonic intussusception, highlighting the complex nuances of its management. Our study underscores the crucial importance of thorough assessment in such clinical scenarios and the necessity for prompt and appropriate action. However, it is important to note certain limitations such as a short follow-up duration.
Colonic lipoma (CL) is a rare disease (0.2 to 4 %) and is considered the third most common benign colon tumor after hyperplastic and adenomatous polyps [6,7]. Generally, CL affects adult women (57 %) [3]. These non-epithelial benign tumors present as a sessile polypoid mass, rarely pedunculated, with dimensions ranging from 2 mm to 30 cm [3,4]. In approximately 90 % of cases, they arise from the submucosa but occasionally extend into the muscularis propria [5].
Generally, they are presented as one small asymptomatic lesion [[6], [7], [8]]. For a considerable time, these tumors are still clinically silent until they reach a large size and become symptomatic. The local mass effect can be harmful, causing an expected complication (intussusception, bowel obstruction, bleeding…) [7,8]. Also, the clinical presentation depends on the lipoma's size and involved segment of the colon. In a recent review, Tasselli and al reported the colonic lipoma causing colo-colic intussusception was localized more frequently at the transverse colon (28 %), followed by the sigmoid (20 %), the cecum (19 %), the ascending colon (15 %), the descending colon (14 %), and the rectum (4 %) [6]. Both clinical symptoms, physical examination, and laboratory tests are not specific.
The abdominal CT scan is the best non-invasive diagnostic tool for CL [7,8]. Its sensitivity ranges from 71.4 % to 87.5 %, with a specificity close to 100 %. Colonic lipomas are identified as homogenous masses with fatty densitometric values of −40 to −120 Hounsfield unit (HU) and smooth border [4]. A Target sign or sausage-shaped soft tissue mass is usually seen.
In addition, the abdominal scan can distinguish between other challenging differential diagnoses like liposarcomas. However, small lipoma (<2 cm) and artefacts (large faecal volume) are considered serious CT limitations.
In some situations, the preoperative diagnosis can be difficult, so magnetic resonance imaging can detect lipomas with a signal intensity characteristic of adipose tissue on T1-weighted and fat-suppressing images [7,8].
When it's permitted, Colonoscopy can easily visualize the lipoma as a fatty pedunculated or sessile [4]. A biopsy is needed to confirm the diagnosis and eliminate malignancy. Also, endoscopy can help identify and treat infra-radiologic lesions.
Treatment for colonic lipomas is various and includes active surveillance and endoscopic or surgical resection.
Small lipomas (<2 cm) don't have a potential for malignant degeneration and usually, these lesions are asymptomatic and follow-up is sufficient [7,8,10].
In other situations, (older patient, symptomatic lesions, large lipoma >4 cm [11], complicated lipoma), resection is recommended. Endoscopic or surgical resection depends on some criteria like the lipoma size, location, and the presence or absence of complications.
The majority of authors recommend surgery as the standard method of treatment for every colonic lipoma >2 cm [7,8,10,11]. In the literature, surgical excision may include colotomy with local excision (or enucleation), limited colon resection, or segmental resection. The choice of these surgical procedures depends on the lipoma size, location, and the presence or absence of definite preoperative [7,8,10,11].
For complicated situations like colonic intussusception, surgery is the cornerstone of the treatment. It seems reasonable that conservative surgical procedures like enucleation or limited colon resection can be performed only if malignancy is excluded. Segmental resection is the safe surgical option in other situations where the preoperative diagnosis is uncertain.
It was reported that laparoscopy offers better postoperative outcomes than conventional laparotomy. Mini-invasive approach cause less postoperative pain, a shorter period of ileus and disability, a shorter hospital stay, and recovery period, and quicker recoveries when compared to open colectomies. However, Boler et al. reported that laparoscopic resection can be limited by the inability to definitively locate certain lipomas [9]. A variety of endoscopic (clips, tattooing with India-ink…) and radiologic techniques have been described to localize an area or site within the colon.
On the other hand, the endoscopic mucosal resection was limited to small pedunculated lipomas (<2 cm) [[6], [7], [8]]. For large lipomas, the endoscopic approach was described in rare cases. Electrocautery snare is was the preferred technique. Others technics like ‘Ligate and Let Go’ or endoscopic reduction of colo-colonic intussusception with a wedged balloon and injection pressure, have also been reported [8].
However, these procedures need to be done by well-trained endoscopists at highly experienced centres where surgery could be made at any time. Also, we must keep in mind that endoscopic excision of difficult lipoma (sessile or broadly based lipomas or large lipoma with usual serosal involvement) is associated with a high rate of perforation and haemorrhage.
4. Conclusion
Our study underscores the importance of thorough assessment in the management of giant colonic lipomas inducing colo-colonic intussusception. While laparoscopic enucleation may seem appealing, it is crucial to consider the possibility of malignancy and opt for open or laparoscopic surgical resection if necessary, in line with oncological principles. Further research is needed to enhance surgical techniques and ensure optimal outcomes for patients.
Patient consent
Written informed consent was obtained from the patient for the publication of this case report and its accompanying images. A copy of the written consent is available for the Editor-in-Chief of this journal to review upon request.
Declaration of generative AI in scientific writing
AI tools were not used for the elaboration of the manuscript.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Funding
This research did not receive funding from any specific grant provided by public, commercial, or not-for-profit organizations.
Ethical approval
Ethical approval is not applicable/waived at our institution. Due to the specific nature of case reports, which involve detailed descriptions of observations and interventions that have already been conducted on patients, as opposed to prospective studies involving planned interventions, our institution does not require formal ethical approval for such cases. We recognize the importance of ethics in medical research and are fully committed to upholding ethical standards in our medical and research practices.
Author contribution
Med Dheker Touati and Anis Belhadj contributed to manuscript writing andediting, and data collection; Ahmed Bouzid and Fahd Khefacha contributed to data analysis; Ahmed Saidani and Faouzi Chebbi contributed to conceptualization and supervision; All authors have read and approved the final manuscript.
Guarantor
Dr. Med Dheker Touati.
Research registration number
N/A.
Conflict of interest statement
No conflicts of interest.
References
- 1.Kansoun A., Mohtar I.A., Bahmad M., Houcheimi F., Maanieh N., Hazim M., et al. Colo-colic intussusception secondary to colon lipoma: a case report. Int. J. Surg. Case Rep. 5 mars 2021;81 doi: 10.1016/j.ijscr.2021.105695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manouras A., Lagoudianakis E.E., Dardamanis D., Tsekouras D.K., Markogiannakis H., Genetzakis M., et al. Lipoma induced jejunojejunal intussusception. World J. Gastroenterol. 14 juill 2007;13(26):3641–3644. doi: 10.3748/wjg.v13.i26.3641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zubaidi A., Al-Saif F., Silverman R. Adult intussusception: a retrospective review. Dis. Colon Rectum. oct 2006;49(10):1546–1551. doi: 10.1007/s10350-006-0664-5. [DOI] [PubMed] [Google Scholar]
- 4.Grasso E., Guastella T. Giant submucosal lipoma cause colo-colonic intussusception. A case report and review of literature. Ann. Ital. Chir. 2012;83(6):559–562. [PubMed] [Google Scholar]
- 5.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A., et al. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. Lond. Engl. 1 mai 2023;109(5):1136–1140. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Panagiotakis G.I., Andreou A.G., Petrakis I.E., Tzardi M., Daskalogiannaki M., Chalkiadakis G.E. Laparoscopic resection of a sigmoid colon lipoma in a young female patient: a case report and review of the literature. Oncol. Lett. 2017;13:1303–1306. doi: 10.3892/ol.2017.5594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Menegon Tasselli F., Urraro F., Sciaudone G., et al. Colonic lipoma causing bowel intussusception: an up-to-date systematic review. J. Clin. Med. 2021;10(21):5149. doi: 10.3390/jcm10215149. (Published 2021 Nov 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crocetti D., Sapienza P., Sterpetti A.V., et al. Surgery for symptomatic colon lipoma: a systematic review of the literature. Anticancer Res. 2014;34(11):6271–6276. [PubMed] [Google Scholar]
- 9.Boler D.E., Baca B., Uras C. Laparoscopic resection of colonic lipomata: when and why? Am. J. Case Rep. 2013;14:270–275. doi: 10.12659/AJCR.889247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goyal V., Ungsunan P. Lipoma of the colon: should asymptomatic to be treated? Am. Surg. 2013;79:E45–E46. (PMID: 23317607) [PubMed] [Google Scholar]
- 11.Jiang L., Jiang L.S., Li F.Y., Ye H., Li N., Cheng N.S., et al. Giant submucosal lipoma located in the descending colon: a case report and review of the literature. World J. Gastroenterol. 2007;13:5664–5667. doi: 10.3748/wjg.v13.i42.5664. [DOI] [PMC free article] [PubMed] [Google Scholar]