ABSTRACT
Aim:
Internal disc displacement of the temporomandibular joint (TMJ) is identified by an anomaly between the condylar-disc assembly, which, in many cases, may lead to discomfort and malfunction of the chewing function. The study’s objective was to assess the effects of four distinct treatment approaches on temporomandibular disorder cases with anterior disc displacements focusing on their chewing efficiency.
Materials and Methods:
One hundred participants suffering from reducible TMJ disc displacement were selected for enrollment in the study. Subjects were divided equally into four groups: group I patients were treated with behavioral therapy; group II patients were treated with low-level laser therapy (LLLT); group III patients were treated with anterior repositioning splints; and group IV patients were treated with flat plane splints. Chewing efficiency was assessed utilizing the fractional sieving method and a synthetic food substitute was created using silicon impression material. The statistical analysis encompassed comparisons of chewing efficiency between groups and between baseline and posttreatment within each group, employing analysis of variance (ANOVA) and paired t tests, respectively.
Results:
Using the paired t test, a significant difference in chewing efficiency values as expressed by the median particle size was observed between the baseline and 6-month values in all groups (P < 0.05), except for group I where no significant change was noted over the 6 months (P > 0.05). The one-way ANOVA test revealed a statistically significant difference among groups following therapies (P ˂ 0.05). The post hoc Tukey test was employed for pairwise comparisons and revealed statistically significant variances in the main values of chewing efficiency among all groups at a 95% confidence level (P ˂ 0.05).
Conclusion:
The study’s results suggest that occlusal splints and LLLT are more effective in improving chewing efficiency than behavioral interventions.
Keywords: Anterior repositioning splint, behavioral therapy, chewing efficiency, low-level laser therapy, occlusal splints, temporomandibular joint disorder
INTRODUCTION
The relation between masticatory system function and temporomandibular joint (TMJ) disorders (TMD) has been a subject of interest in the field of dentistry for a considerable period. TMD, occlusion, and oral function all have intricate relationships with one another. Insufficient knowledge about the ideal treatment approach for TMD has resulted in the development of various concepts and therapeutic approaches, leading to significant controversy.[1] The diagnosis of TMDs relies on the patient’s history, clinical assessment, and the utilization of valuable diagnostic tools, such as the Research Diagnostic Criteria for TMDs (RDC/TMD).[2] The RDC/TMD comprises two axes: axis I for the physical evaluation of the TMJ and its related structures, and axis II for the psychosocial evaluation of the patient.[3] An anomalous relationship between the condyle and the disc, which is linked to the immobility of the disc, is a characteristic of TMJ disc displacement.[4] This anomalous relationship can cause pain and dysfunctional indicators such as joint clicking and muscle soreness. Disc displacement of TMJ can be categorized into three distinct classifications: disc displacement with reduction, disc displacement with reduction with intermittent locking, and disc displacement without reduction, which may or may not be accompanied by restriction of the mouth opening.[5] A specific type of internal derangement, termed anterior disc displacement with reduction, occurs when the articular disc shifts forward, resulting in an audible clicking sound during mouth opening, which has a high prevalence in adolescents and preadolescents population.[6,7] Numerous therapeutic approaches have been proposed to treat TMJ disc displacement. Anterior repositioning splints and flat plane splints are among the most widely utilized interventions.[8] Nevertheless, the existing body of evidence concerning these splints demonstrates inconsistent long-term treatment results.[9,10]
The increase in vertical occlusion and the potential to alter the mandibular postural position may account for the impact caused by the occlusal splints.[11] The reported efficacy of occlusal splint has been linked to reduced loading of the TMJs[12] and decreased neuromuscular activity, in addition to the placebo effect.[13] Behavioral therapy is a type of treatment that modifies how patients perceive pain by applying behavioral science theories and techniques. The goal is to help patients with chronic TMD pain develop better-coping mechanisms and get rid of psychological disorders.[14] Behavioral therapy comprises a diverse spectrum of therapeutic interventions, encompassing modalities including re-education, biofeedback, cognitive behavioral treatment, and various relaxation methods.[15,16,17]
To produce anti-inflammatory and analgesic effects, low-level laser therapy (LLLT) has been employed as a noninvasive treatment for pain management in TMD patients.[18,19] Previous investigations have demonstrated the success of a noninvasive therapy for reducing pain and enhancing the range of jaw mobility.[20,21]
Given the aforementioned literature, the purpose of the current research was to assess the impact of four distinct therapeutic options, namely behavioral therapy, LLLT, anterior repositioning splint, and flat splint, on the chewing efficiency of individuals diagnosed with anterior disc displacement with reduction (ADDwR) of the TMJ. The study hypothesized that the difference in the effects of various treatment options on chewing efficiency would be statistically nonsignificant.
MATERIALS AND METHODS
Following the findings of a prior study,[22] a sample size of 100 participants (64 females and 36 males) was chosen for this randomized clinical trial. The selected participants’ ages ranged from 19 to 44 years old. Following acceptance from the Faculty Research Ethics Committee, participants were randomly chosen from the prosthodontics department’s clinics of Al-Azhar University’s Faculty of Dentistry (Boys, Cairo, Egypt), from March 2016 until April 2020. Before treatment, all participants underwent clinical and radiographic diagnosis of TMJ by magnetic resonance imaging bilaterally in both open and closed positions. Participants identified with unilateral ADDwR of the TMJ, as well as those whose main complaints included joint pain, clicking, and limitation of jaw mobility, fulfilled the requirements for eligibility to be enrolled in the study. An experienced investigator conducted the diagnosis of the participant following the RDC/TMD diagnostic tool.[3] Subjects who had a history of chemotherapy or radiation therapy in the head and neck area, prior TMJ surgery, or systemic inflammatory joint disease were excluded from the study. Before their enrollment in the study, each participant signed an informed consent form. The participants were then randomly allocated into four groups of 25 participants each using statistical package for the social sciences (SPSS, IBM Corp., Armonk, NY, USA) software;
Group I: patients of this group received behavioral therapy; the participants were instructed to utilize heat packs, abstain from consuming tough foods, and avoid uncomfortable working and sleeping postures to maximize the relaxation of their TMJ. The participants were advised to follow the previous recommendations for the whole 6 months of their therapy.
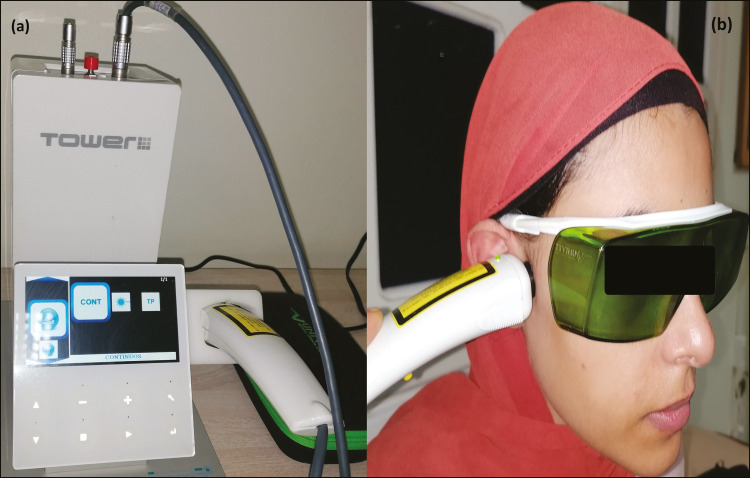
Group II: during the 4-week therapy period, patients received two sessions of LLLT per week. The device employed was the TOWER LIGHT LASER (ELETTRONICA PAGANI, Milan, Italy), which generates a low-level laser with a wavelength of 808 nm, that is, produced by stimulating a solid-state source. The procedure was modified to utilize a consistent power output of 70 mW and energy doses of 105 J/cm2 using continuous mode. Each treatment visit entailed the administration of low-level laser at five pre-defined TMJ locations (anterior, superior, posterior, postero-inferior points of the mandibular condyle, and in the external meatus of the ears) with a 60-s exposure time for each location [Figure 1A and B].
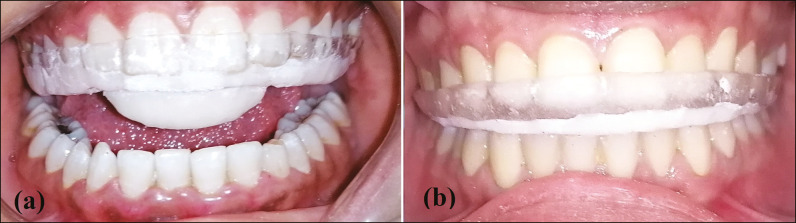
Group III: the anterior repositioning splint was created following the method outlined by Okeson,[23] involving self-curing acrylic resin and a 2-mm thick Folidur N/clear; Polyethylene terephthalate thermoplastic sheet (aldente Dentalprodukte GmbH, Horgenzell, Germany). This design necessitates the mandible to be repositioned anteriorly to alleviate pain and clicking. The success of anterior repositioning appliance fabrication depends on finding the most suitable anterior mandibular posture to eliminate the TMJ’s pain and clicking. Participants were directed to use the splint for 12 h daily over 6 months [Figure 2B].
Group IV: a flat plane splint was created following the method outlined by Okeson[23] using a 2-mm thick, polyethylene terephthalate sheet and cold-curing acrylic resin. The occlusal appliance was designed with a flat occlusal surface to touch the opposing teeth at the centric relation position, as well as to provide canine guidance during protrusive and lateral movements. During the construction of the splint, manual manipulation was used to guide the patients to close in the centric relation position. participants were directed to use the splint for 12 h daily over 6 months period [Figure 2B].
Figure 1:
(A) Laser device. (B) Using the LLLT for the treatment of the patient with ADDwR
Figure 2:
(A) Anterior repositioning splint. (B) Flat plane occlusal splint
MEASURING CHEWING EFFICIENCY
Chewing efficiency was measured using the fractional sieving method, which measures the ability of an individual to pulverize a certain amount of test food, which breaks down the food into smaller particles. The extent of food pulverization can be evaluated by sieving to examine chewed food particles. The size distribution of test food’s particles is analyzed, and typically represented by X50; the median particle size. The fractional sieving method used in the current study provided a quantitative measure of chewing efficiency. By analyzing the test food’s particles retrieved after chewing, researchers were able to evaluate the efficacy of the various treatments on chewing efficiency. High-consistency condensation silicon impression was utilized as a test food (Silaplast Futur; Detax, Ettlingen, Germany). Experimental procedures were carried out as described by previous studies[24,25]; the silicon impression was given to the participants in parts of eight cubes, each having an 8 mm wide edge. Before the chewing process, all cubes were weighed. The remaining fragments of the test food were retrieved from the patient’s mouth after 60 chewing cycles. The retrieved fragments underwent filtering, drying, and weighing. An assembly of eight sieves and a bottom tray was used to sieve the chewed food particles. The sieves had mesh diameters ranging from 0.5 to 5.6 mm. The chewed food particles retrieved from each sieve along with the bottom tray were measured using laboratory balance. It is possible to determine the distribution of the particle sizes by weight by mathematical calculation through the following equation of Rosin Rammler[24,25];
where Qw represents the weight percentage of particles smaller than X. The median particle size (X50) is the size at which 50% of the chewed fragments can pass through a theoretical sieve opening. The parameter b represents the degree to which the chewed fragments are homogenous in size. The chewing efficiency of all subjects was measured before treatment and 6 months.
STATISTICAL ANALYSIS
The SPSS© Statistics for Windows version 20.0 program (IBM Corp) was utilized to collect, tabulate, and statistically analyze the data. One-way analysis of variance (ANOVA) test and post hoc Tukey test at 95% confidence level (P ≤ 0.05) were used for comparison between groups and the paired t test was employed for comparing each group’s pre and post-treatment data.
RESULTS
The chewing efficiency mean values of the four groups at the initial treatment session and 6 months later as expressed by the median particle size, X50 are displayed in Table 1; where X50 denotes the size of a hypothetical sieve that would allow half of the weight of the crushed food to pass through it.
Table 1:
Mean and SD values for chewing efficiency as expressed by the median particle size, X50 at baseline and after 6 months (P ≤ 0.05)
| Time of measurements | T and P values | Group I | Group II | Group III | Group IV |
|---|---|---|---|---|---|
| Before treatment | 4.57 ± 1.13 | 4.84 ± 1.16 | 4.29 ± 1.05 | 4.07 ± 0.96 | |
| After 6 months | 4.38 ± 1.02 | 3.57 ± 0.86 | 2.86 ± 0.82 | 1.24 ± 0.87 | |
| Paired t test | T value | 1.83 | 1.83 | 1.83 | 1.83 |
| P value | 0.52 | 0.03 | 0.02 | 0.00 | |
| Significance | Nonsignificant | Significant | Significant | Significant |
Time comparison with paired t test revealed a significant change in chewing efficiency between the baseline and 6-month values in all groups (P < 0.05) except in group I where there was no significant change in chewing efficiency over the 6 months (P > 0.05).
The one-way ANOVA analysis indicated that there was no statistically significant variance among the various groups before the initiation of treatment (P > 0.05). After the treatment, the one-way ANOVA analysis indicated a statistically significant disparity among the various groups (P < 0.05). Additionally, the post hoc Tukey test indicated statistically significant variances in the mean values of chewing efficiency between all groups at a 95% confidence level (P < 0.05), as shown in Table 2.
Table 2:
Pairwise comparisons using post hoc Tukey test for comparing the chewing efficiency between different groups
| Pairwise comparisons | Mean Difference |
P value | Significance | |
|---|---|---|---|---|
| Group I versus | Group II | 0.810* | 0.004 | Significant |
| Group III | 1.521* | 0.000 | Significant | |
| Group IV | 3.141* | 0.000 | Significant | |
| Group II versus | Group III | 0.711* | 0.013 | Significant |
| Group IV | 2.331* | 0.000 | Significant | |
| Group III versus | Group IV | 1.620* | 0.000 | Significant |
*Denotes significant difference (P ≤ 0.05)
DISCUSSION
Chewing efficiency is a crucial parameter in assessing the chewing function of patients with TMD. Typically, these individuals exhibit lower chewing efficiency compared to healthy individuals.[26,27] Following therapy, patients with TMD typically experience an improvement in their chewing efficiency. However, their chewing efficiency remains lower than that of healthy persons.[28,29,30,31] There are several methods to evaluate chewing function like fractional sieving, measuring time or the number of chewing cycles, color-changing chewing gums, optical scanning method, and dye release method but fractional sieving is the oldest and most widely used method.[24,32,33] It measures the capacity to pulverize certain test materials using a standardized sieve system after a predetermined number of chewing strokes. To improve reproducibility, synthetic test food was utilized. The mathematical equations described in previous studies were used for data analysis.[24,25] Chewing efficiency was evaluated preoperatively and after each therapeutic intervention; behavioral therapy, LLLT, flat splint, and ARS. No participant in the four treatment groups has experienced any serious side effects, such as teeth mobility or occlusion change.
There was a notable improvement in the chewing efficiency of ADDwR cases after treatment with LLLT, ARS, and flat plane splint (P ˂ 0.05), also there were statistically significant differences observed among the various groups after treatment (P < 0.05), so the null hypothesis was rejected.
There was a significant increase in the chewing efficiency of ADDwR cases for the flat plane splint group more than that of the ARS group, LLLT group, and behavior therapy group (P < 0.05). While there was a notable increase in the chewing efficiency of ADDwR cases for the ARS group more than that of the LLLT group and behavior therapy group (P < 0.05), these findings were consistent with those of Kümbüloğlu et al.[34] who reported a significant improvement effect of the occlusal splint on the chewing efficiency of TMD subjects. It would be beneficial to explore the potential mechanisms by which the various treatment modalities could have impacted chewing efficiency. For instance, LLLT might have stimulated tissue healing, reduced inflammation, or enhanced muscle function in the TMJ area. The ARS could have assisted in repositioning the condyle, resulting in improved occlusion and chewing function. The flat plane splint might have provided a stable occlusal surface, thereby enhancing chewing efficiency. Examining these mechanisms can offer insight into why certain treatments were more successful in improving chewing efficiency. The superior chewing efficiency observed in the flat plane splint group compared to the ARS, LLLT, and behavioral therapy groups may be attributed to the specific design and function of the splint. The flat plane splint provides a stable occlusal surface that promotes balanced occlusal contacts and even distribution of occlusal forces, resulting in improved chewing efficiency.
In the current study there was a considerable improvement in chewing function as expressed by the median particle size; X50 after treatment with LLLT, this was in agreement with a previous investigation conducted by de Moraes Maia et al.[35] The significant improvement in chewing function observed in the current study after LLLT treatment suggests that LLLT may have beneficial effects on the masticatory system. LLLT is known to have various physiological effects, including promoting tissue healing, reducing inflammation, and enhancing muscle function. These effects may have contributed to the observed improvement in chewing function, as indicated by the decrease in median particle size (X50). The reduction in particle size suggests improved chewing efficiency and the ability to break down food particles more effectively. On the other hand, this finding was at variance with Carrasco et al.[36] who evaluated the impact of low-intensity laser on chewing efficiency in TMD and reported nonsignificant differences after treatment. The discrepancy between the findings of the current research and the previous research by Carrasco et al.[36] could be attributed to several factors. First, differences in the study design, including sample size, treatment protocol, and outcome measures, may have contributed to the contrasting results. Additionally, variations in the characteristics of the selected individuals, such as the duration and intensity of TMD pain, may have influenced the treatment outcomes. It is also essential to bear in mind that the effectiveness of LLLT may vary depending on the specific parameters used, such as wavelength, power density, and treatment duration.
There is a lack of research in the literature related to the impact of behavioral and self-care interventions on the chewing function of patients with persistent TMD symptoms. The study’s findings indicate that behavioral therapy did not significantly enhance the chewing efficiency of individuals with ADDwR; these results were contrary to those of Michelotti et al.,[37,38] whose findings demonstrated a significant improvement in masticatory capacity after treatment with these therapies. This may be explained by the fact that every patient is unique, and what works best for one might not work as well for another. It is essential to consider individual patient needs, and preferences in addition behavioral therapy may offer other advantages like pain reduction, improved patient compliance, or psychological well-being.
All treatment modalities used in the current study are considered noninvasive methods in the management of ADDwR cases, others reported that noninvasive methods (occlusal splint) had marked improvement for ADDwR cases more than invasive methods.[10] The study’s limitation lies in its limited follow-up period, which did not provide enough time to fully resolve the debate surrounding various conservative treatment methods for TMD. Therefore, more investigations are necessary to assess the long-term effectiveness of these treatment options. The selected individuals varied in age, ranging from 19 to 44 years old. Age can affect chewing performance, as older individuals may experience changes in muscle strength, dental status, and overall oral health. Age-related differences could potentially confound the relationship between the treatment interventions and chewing efficiency. TMD is a complex condition that often requires a multidisciplinary approach for optimal management. Future studies could explore the effectiveness of combining different interventions, such as LLLT, ARS, flat plane splint, and behavioral therapy, to determine if a synergistic effect can be achieved and if it leads to greater improvements in chewing efficiency and overall treatment outcomes.
CONCLUSION
Among the treatments studied, behavioral therapy did not lead to a significant change in chewing efficiency over 6 months. In contrast, the other treatments (LLLT, anterior repositioning splint, and flat plane splint therapy) did result in significant changes. This could indicate that the occlusal splints and low-level therapy might have a more pronounced impact on chewing efficiency than behavioral interventions.
FINANCIAL SUPPORT AND SPONSORSHIP
The authors did not receive any funding for the study, writing, and/or publishing of this article.
CONFLICTS OF INTEREST
There are no conflicts of interest.
AUTHOR CONTRIBUTIONS
Study conception and design: EAA, AAB, and MAH. Data collection and acquisition: ANE, EAA, EA, and MO. Data analysis: EAA, ANE, YB, MO, and AAB. Data interpretation: MAH, MO, EA, and AAB. Manuscript writing: ANE, EAA, EA, AAB, and YB. Review and editing: EAA, EA, MO, YB, and MAH. The final draft of the article was approved by all authors for publication.
ETHICAL POLICY AND INSTITUTIONAL REVIEW BOARD STATEMENT
The study received ethical approval from the Research Ethical Committee of the Faculty of Dental Medicine, Al-Azhar University, under the reference number 502-04-16.
PATIENT DECLARATION OF CONSENT
All participants enrolled in the study signed an informed consent form following ethical guidelines.
DATA AVAILABILITY STATEMENT
Upon request, the corresponding author will provide the data supporting the study’s findings.
ACKNOWLEDGEMENT
None.
Glossary
List of Abbreviations
- ADDwR:
Anterior disc displacement with reduction
- ANOVA:
Analysis of variance
- ARS:
Anterior repositioning splint
- LLLT:
Low-level laser therapy
- RDC/TMD:
Research Diagnostic Criteria for Temporomandibular Disorders
- TMD:
Temporomandibular joint disorders
- TMJ:
Temporomandibular joint
REFERENCES
- 1.Gil-Martínez A, Paris-Alemany A, López-de-Uralde-Villanueva I, La Touche R. Management of pain in patients with temporomandibular disorder (TMD): Challenges and solutions. J Pain Res. 2018;11:571–87. doi: 10.2147/JPR.S127950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matheson EM, Fermo JD, Blackwelder RS. Temporomandibular disorders: Rapid evidence review. Am Fam Physician. 2023;107:52–8. [PubMed] [Google Scholar]
- 3.Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet J-P, et al. International RDC/TMD Consortium Network, International Association for Dental Research. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache. 2014;28:6–27. doi: 10.11607/jop.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang CL, Wang DH, Yang MC, Hsu WE, Hsu ML. Functional disorders of the temporomandibular joints: Internal derangement of the temporomandibular joint. Kaohsiung J Med Sci. 2018;34:223–30. doi: 10.1016/j.kjms.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 5.Durham J, Newton-John TRO, Zakrzewska JM. Temporomandibular disorders. BMJ. 2015;350:h1154. doi: 10.1136/bmj.h1154. [DOI] [PubMed] [Google Scholar]
- 6.de Melo Júnior PC, Aroucha JMCNL, Arnaud M, Lima MGS, Gomes SGF, Ximenes R, et al. Prevalence of TMD and level of chronic pain in a group of Brazilian adolescents. PLoS One. 2019;14:e0205874. doi: 10.1371/journal.pone.0205874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valesan LF, Da-Cas CD, Réus JC, Denardin ACS, Garanhani RR, Bonotto D, et al. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin Oral Investig. 2021;25:441–53. doi: 10.1007/s00784-020-03710-w. [DOI] [PubMed] [Google Scholar]
- 8.Warburton G, Patel N, Anchlia S. Current treatment strategies for the management of the internal derangements of the temporomandibular joint: A global perspective. J Maxillofac Oral Surg. 2022;21:1–13. doi: 10.1007/s12663-021-01509-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Moraissi EA, Farea R, Qasem KA, Al-Wadeai MS, Al-Sabahi ME, Al-Iryani GM. Effectiveness of occlusal splint therapy in the management of temporomandibular disorders: Network meta-analysis of randomized controlled trials. Int J Oral Maxillofac Surg. 2020;49:1042–56. doi: 10.1016/j.ijom.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 10.Helal MA, Agou SH, Bayoumi A, Imam A, Hassan AH. Management of internal derangement of temporomandibular joint disc displacement with reduction using two different lines of treatment. Braz Dent Sci. 2021;24:8. [Google Scholar]
- 11.Liu MQ, Lei J, Han JH, Yap AU, Fu KY. Metrical analysis of disc-condyle relation with different splint treatment positions in patients with TMJ disc displacement. J Appl Oral Sci. 2017;25:483–9. doi: 10.1590/1678-7757-2016-0471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferreira FM, Cézar Simamoto-Júnior P, Soares CJ, Ramos A, Fernandes-Neto AJ. Effect of occlusal splints on the stress distribution on the temporomandibular joint disc. Braz Dent J. 2017;28:324–9. doi: 10.1590/0103-6440201601459. [DOI] [PubMed] [Google Scholar]
- 13.Alkhutari AS, Alyahya A, Rodrigues Conti PC, Christidis N, Al-Moraissi EA. Is the therapeutic effect of occlusal stabilization appliances more than just placebo effect in the management of painful temporomandibular disorders? A network meta-analysis of randomized clinical trials. J Prosthet Dent. 2020;126:24–32. doi: 10.1016/j.prosdent.2020.08.015. [DOI] [PubMed] [Google Scholar]
- 14.Zhang Q, Zhang J, Ran W, Yu S, Jin Y. Effectiveness of cognitive behavioral therapy on kinesiophobia and oral health-related quality of life in patients with temporomandibular disorders, study protocol for a randomized controlled trial. Medicine (Baltimore) 2020;99:e23295. doi: 10.1097/MD.0000000000023295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Noma N, Watanabe Y, Shimada A, Usuda S, Iida T, Shimada A, et al. Effects of cognitive behavioral therapy on orofacial pain conditions. J Oral Sci. 2020;63:4–7. doi: 10.2334/josnusd.20-0437. [DOI] [PubMed] [Google Scholar]
- 16.Florjanski W, Malysa A, Orzeszek S, Smardz J, Olchowy A, Paradowska-Stolarz A, et al. Evaluation of biofeedback usefulness in masticatory muscle activity management-A systematic review. J Clin Med. 2019;8:766. doi: 10.3390/jcm8060766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tournavitis A, Sandris E, Theocharidou A, Slini T, Kokoti M, Koidis P, et al. Effectiveness of conservative therapeutic modalities for temporomandibular disorders-related pain: A systematic review. Acta Odontol Scand. 2023;81:286–97. doi: 10.1080/00016357.2022.2138967. [DOI] [PubMed] [Google Scholar]
- 18.Abdel-Gawwad EA, Abdullah AAB, Farhat MY, Helal MA. Effect of using Photobiomodulation, stabilization, and anterior repositioning splints on the pain level of subjects with temporomandibular joint disc displacement with reduction. Braz Dent Sci. 2021;24:1–8. [Google Scholar]
- 19.Ahmad SA, Hasan S, Saeed S, Khan A, Khan M. Low-level laser therapy in temporomandibular joint disorders: A systematic review. J Med Life. 2021;14:148–64. doi: 10.25122/jml-2020-0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Melchior Mde O, Venezian GC, Machado BC, Borges RF, Mazzetto MO. Does low intensity laser therapy reduce pain and change orofacial myofunctional conditions? Cranio. 2013;31:133–9. doi: 10.1179/crn.2013.021. [DOI] [PubMed] [Google Scholar]
- 21.Emam AM, Abdel-Gawwad EA, Baiomy AAA, Farhat MY, Atito E, Helal MA. Efficacy of occlusal splints and low-level laser therapy on the mandibular range of motion in subjects with temporomandibular joint disc displacement with reduction. J Int Soc Prev Community Dent. 2023;13:229–36. doi: 10.4103/jispcd.JISPCD_159_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kurt H, Mumcu E, Sülün T, Diraçoǧu D, Ünalan F, Aksoy C, et al. Comparison of effectiveness of stabilization splint, anterior repositioning splint and behavioral therapy in treatment of disc displacement with reduction. Turk J Phys Med Rehab. 2011;57:25–30. [Google Scholar]
- 23.Okeson JP. Occlusal Appliance Therapy: Management of temporomandibular Disorders and Occlusion. 5th ed. St. Louis: Mosby; 2003. pp. 220–442. [Google Scholar]
- 24.Eberhard L, Schindler HJ, Hellmann D, Schmitter M, Rammelsberg P, Giannakopoulos NN. Comparison of particle-size distributions determined by optical scanning and by sieving in the assessment of masticatory performance. J Oral Rehabil. 2012;39:338–48. doi: 10.1111/j.1365-2842.2011.02275.x. [DOI] [PubMed] [Google Scholar]
- 25.Eberhard L, Schneider S, Eiffler C, Kappel S, Giannakopoulos NN. Particle size distributions determined by optical scanning and by sieving in the assessment of masticatory performance of complete denture wearers. Clin Oral Investig. 2015;19:429–36. doi: 10.1007/s00784-014-1266-6. [DOI] [PubMed] [Google Scholar]
- 26.Ferreira CLP, Sforza C, Rusconi FME, Castelo PM, Bommarito S. Masticatory behaviour and chewing difficulties in young adults with temporomandibular disorders. J Oral Rehabil. 2019;46:533–40. doi: 10.1111/joor.12779. [DOI] [PubMed] [Google Scholar]
- 27.Massaroto Barros B, Biasotto-Gonzalez DA, Bussadori SK, Gomes C, Politti F. Is there a difference in the electromyographic activity of the masticatory muscles between individuals with temporomandibular disorder and healthy controls? A systematic review with meta-analysis. J Oral Rehabil. 2020;47:672–82. doi: 10.1111/joor.12941. [DOI] [PubMed] [Google Scholar]
- 28.Li C-X, Liu X, Gong Z-C, Liu H, Jumatai S. Effects of condyle on disc status of the reducing and nonreducing anterior disc displacement of the temporomandibular joint based on 3D reconstructive imaging: A pilot study. Quintessence Int. 2023;54:156–66. doi: 10.3290/j.qi.b3512027. [DOI] [PubMed] [Google Scholar]
- 29.Marcelino V, De Rovere S, Paço M, Gonçalves M, Marcelino S, Guimarães AS, et al. Masticatory function in individuals with temporomandibular disorders: A systematic review and meta-analysis. Life (Basel, Switzerland) 2023;13:472. doi: 10.3390/life13020472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mohammed EA, Abdullah AAB, Helal MA. Effect of four conservative treatment methods on the muscular activity of masseter and temporalis muscles for subjects with temporomandibular joint disc displacement with reduction. Al-Azhar J Dent Sci. 2022;25:401–8. [Google Scholar]
- 31.Pelai EB, Foltran-Mescollotto F, de Castro-Carletti EM, de Moraes M, Rodrigues-Bigaton D. Comparison of the pattern of activation of the masticatory muscles among individuals with and without TMD: A systematic review. Cranio. 2023;41:102–11. doi: 10.1080/08869634.2020.1831836. [DOI] [PubMed] [Google Scholar]
- 32.Zhang Y, Jia J, Wang X, Chen J, van der Glas HW. Particle size distributions following chewing: Transformation of two-dimensional outcome from optical scanning to volume outcome from sieving. J Food Eng. 2021;309:110663. [Google Scholar]
- 33.Elgestad Stjernfeldt P, Wårdh I, Trulsson M, Faxén Irving G, Boström A-M. Methods for objectively assessing clinical masticatory performance: Protocol for a systematic review. Syst Rev. 2017;6:20. doi: 10.1186/s13643-016-0403-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kümbüloğlu O, Saracoglu A, Bingöl P, Hatipoğlu A, Ozcan M. Clinical study on the comparison of masticatory efficiency and jaw movement before and after temporomandibular disorder treatment. Cranio. 2013;31:190–201. doi: 10.1179/crn.2013.030. [DOI] [PubMed] [Google Scholar]
- 35.de Moraes Maia ML, Ribeiro MA, Maia LG, Stuginski-Barbosa J, Costa YM, Porporatti AL, et al. Evaluation of low-level laser therapy effectiveness on the pain and masticatory performance of patients with myofascial pain. Lasers Med Sci. 2014;29:29–35. doi: 10.1007/s10103-012-1228-7. [DOI] [PubMed] [Google Scholar]
- 36.Carrasco TG, Mazzetto MO, Mazzetto RG, Mestriner W., Jr Low intensity laser therapy in temporomandibular disorder: A phase II double-blind study. Cranio. 2008;26:274–81. doi: 10.1179/crn.2008.037. [DOI] [PubMed] [Google Scholar]
- 37.Michelotti A, Iodice G, Vollaro S, Steenks MH, Farella M. Evaluation of the short-term effectiveness of education versus an occlusal splint for the treatment of myofascial pain of the jaw muscles. J Am Dent Assoc. 2012;143:47–53. doi: 10.14219/jada.archive.2012.0018. [DOI] [PubMed] [Google Scholar]
- 38.Michelotti A, Steenks MH, Farella M, Parisini F, Cimino R, Martina R. The additional value of a home physical therapy regimen versus patient education only for the treatment of myofascial pain of the jaw muscles: Short-term results of a randomized clinical trial. J Orofac Pain. 2004;18:114–25. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Upon request, the corresponding author will provide the data supporting the study’s findings.