ABSTRACT
In recent years, a multitude of studies have been conducted to investigate the assessment of quality of life (QoL) among individuals affected by thalassemia. This scoping review aimed to examine the existing knowledge regarding the QoL and its associated factors among individuals with thalassemia in India. Databases, such as PubMed, SCOPUS, Web of Science, and the Preferred Reporting Items for Systematic Review and Meta-Analysis Extension for Scoping Reviews (PRISMA-ScR) guidelines, were searched. A total of nine articles were included in the review. The included studies mainly investigated children. The Pediatric Quality of Life Inventory (PedsQL) is the most common instrument used most often. Overall, the research findings indicate that individuals who underwent blood transfusion exhibited a lower QoL than those who did not receive blood transfusion. Additionally, it was observed that children diagnosed with thalassemia reported a lower QoL than adults. Nevertheless, the studies exhibited notable methodological deficiencies that constrained the validity and generalizability of the results. Hence, it is imperative to undertake comprehensive QoL research encompassing all regions of India and various thalassemia populations within the country to bridge this evidentiary void.
Keywords: Health-related quality of life, quality of life, scoping review, thalassemia
Introduction
Thalassemia is an autosomal recessive disease in which a genetic mutation causes a decrease in the synthesis rate of one of the globin chains that comprise hemoglobin (Hb). Despite the prevalence of β-thalassemia in India, the condition has been relatively overlooked in scientific and public health discourse, primarily due to prioritizing more immediate health challenges, such as malnutrition and infectious diseases.[1]
Thalassemia syndromes are classified into two subtypes according to their phenotype: transfusion-dependent thalassemias (TDTs) and non-transfusion-dependent thalassemias (NTDTs). Individuals with transfusion-dependent thalassemia (TDT) necessitate regular blood transfusions for survival. In the absence of sufficient transfusion support, they are prone to experiencing diverse complications, ultimately leading to a reduced lifespan. Thalassemia major, severe Hb E/beta(β)-thalassemia, transfusion-dependent Hb H disease, and surviving Hb Bart’s hydrops fetalis are all TDT patients. Patients with thalassemia intermedia, Hb E/β-thalassemia, and Hb H disease were included in the NTDT group.
The global prevalence of individuals carrying the β-thalassemia trait alone is estimated to be approximately 60–80 million. The prevalence of β-thalassemia carriers in the Indian population is estimated to be approximately 3–4%, indicating a substantial number of carriers, ranging from 30 to 40 million individuals, within a population of over one billion.[2] The prevalence of β-thalassemia exhibits heterogeneity across different societies, with specific populations demonstrating notably elevated rates ranging from 5% to 17%.[3] The prevalence of β-thalassemia is higher among the Sindhi and Punjabi populations in India compared to other Indian ethnicities. In India, the average prevalence of the β-thalassemia trait is approximately 3.5%.[4] In most of Asia’s developing countries, including India, the prevalence of thalassemia is inextricably associated with social, cultural, and religious issues. Religious practices, particularly among Muslims, have influenced attitudes toward prenatal diagnosis and termination of pregnant women with thalassemia major.[5]
The management protocol for thalassemia is intricate, enduring, and burdensome, requiring recurrent hospital admissions and blood transfusions, which often adversely affect the child’s physiological and psychological well-being.[6] Health-related quality of life (HRQoL) is a crucial factor to consider when evaluating treatment options for individual patients and allocating healthcare resources for chronic diseases, such as thalassemia. Given the typically unaffordable nature of a cure and the prolonged nature of treatment for thalassemia, HRQoL becomes particularly significant in decision-making processes.[7]
Quality of life (QoL)/health-related quality of life (HRQoL) and thalassemia
The definition of quality of life (QoL) provided by the World Health Organization (WHO) encompasses “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns.” The World Health Organization Quality of Life (WHOQOL) is a significant health outcome, with the ultimate therapeutic goal in chronic conditions being high QoL (Kalliopi Megari). QoL comprises four major components: physical, psychological, social, and environmental.[8]
The concept of “Health-Related Quality of Life (HRQoL)” is comprehensive and refers to the various aspects of health, including “physical, psychological and social domains of health, seen as distinct areas that are influenced by a person’s experiences, beliefs, expectations, and perceptions.” HRQoL is a construct that primarily captures an individual’s health status. However, in specific contexts, HRQoL may encompass additional dimensions related to QoL, such as the environment. QoL is a comprehensive and inclusive concept encompassing various dimensions of an individual’s life, such as education and the social environment. In contrast, HRQoL serves as a tool for evaluating an individual’s subjective perception of their health or disease condition and differentiating between various aspects of life that are influenced by health.[9]
Tools used to measure QoL/HRQoL in patients with thalassemia
Currently, there is a lack of a dedicated instrument for evaluating the QoL in individuals with thalassemia. Nevertheless, the majority of researchers employed the following instruments in their investigations: i) the CDC HRQoL-14 questionnaire and ii) the Short-Form Health Survey (SF-36, SF-12, and SF-8), which is a widely used tool for assessing HRQoL. It consists of questionnaires that measure various aspects of physical and mental health. iii) The Manchester Short Assessment of Quality of Life questionnaire includes 16 items. It is designed to evaluate an individual’s perception of their QoL across different domains. iv) The World Health Organization Quality of Life-BREF (WHOQOL-BREF) is an abbreviated version of the WHOQOL assessment tool. v) The Pediatric Quality of Life Inventory (PedsQL) version 4.0 is utilized in academic research and clinical practice to assess the QoL in pediatric populations. The PedsQL version 4.0 is frequently utilized.
Material and Methods
Our scoping review aims to examine the existing body of knowledge regarding the QoL experienced by individuals with thalassemia in the context of India. This paper examines the diverse factors associated with QoL among individuals affected by thalassemia in India.
Identifying the research questions
What are the different assessment instruments employed for the quantification of QoL and HRQoL among patients diagnosed with thalassemia in the context of India?
What are the different factors associated with the QoL and the condition of thalassemia in India?
Study identification
The search strategy was formulated through a comprehensive review of relevant literature, consultation with subject matter experts, and active participation.
A few key terms used for the search were “Thalassemia” OR “community-acquired Thalassemia” AND “QOL” AND “Quality of life” OR “Patient care management” OR “Case management” OR “Clinical case management” AND “Barriers” OR “Blood transfusion” OR challenges OR obstacle. Five online databases, such as PubMed, SCOPUS, Web of Science, EMBASE, and ProQuest, were searched. The search on various databases was conducted from January 2000 to August 2023.
Inclusion and exclusion criteria
The inclusion criteria for this review encompassed primary studies of various study designs, such as descriptive studies, cross-sectional studies, case–control studies, qualitative studies, case reports, research letters, and editorials. These studies were required to address the QoL among thalassemia patients, specifically within the Indian context. Only studies meeting these criteria were considered eligible for inclusion in the review.
The review excluded meta-analyses and conference papers. The inclusion criteria for this study encompassed the incorporation of research articles that explicitly addressed the outcomes pertaining to thalassemia in their investigations on QoL. Additional criteria included the inclusion of English-language articles.
Study selection and data extraction
The authors conducted a two-stage screening and data extraction process, adhering to the specified eligibility criteria. This process involved independent screening and extraction of information from the title, abstract, and full text by two authors (SC and JS), with any disagreements resolved through arbitration by a third author (BP). In the event of a divergence of opinions, a third reviewer (BP) was consulted as an authoritative figure in the subject matter.
Reporting of study findings
The scoping review undertaken in this study adhered to the five stages outlined in the Arksey and O’Malley framework and the criteria put forward by the Joanna Briggs Institute. The Preferred Reporting Items for Systematic Review and Meta-Analysis Extension for Scoping Reviews (PRISMA-ScR) approach was employed by the researchers.
Results
General characteristics
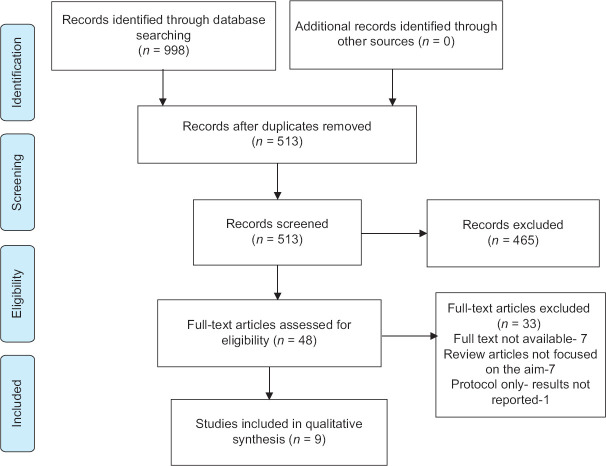
After eliminating 485 duplicate records, the data set consisted of 998 unique records. Of these, 513 articles underwent title screening, resulting in the exclusion of 465 articles. The remaining 48 records underwent a process of abstract screening followed by full-text screening. The scoping review encompassed a total of nine studies. The study selection process is visually represented in Figure 1 using the PRISMA flow diagram.
Figure 1.
PRISMA Flowchart
Of the nine studies, all studies were institutionally based, whereas one study was conducted in a primary health center (clinic), four studies were conducted in tertiary healthcare facilities, and four studies were conducted in a thalassemia day care center as thalassemia patients need frequent blood to manage iron overload. The public healthcare system in India is organized into three tiers, namely, primary, secondary, and tertiary levels, to cater to the needs of the public. Primary healthcare centers are responsible for delivering primary care services, while district and subdivisional hospitals primarily provide secondary care. Tertiary healthcare services are provided by hospitals affiliated with medical colleges. Most individuals with thalassemia necessitate blood transfusions for treatment, with the majority of these interventions being provided at tertiary care facilities and day care centers. The majority of the identified studies are from East India (3), South India (2), North India (2), Central India (1), and West India (1). [Table 1].
Table 1.
Characteristics of the included studies
| Author name, year | City/state, area | Study information design; setting recruitment | Participant’s characteristics (sample size, study, period median/mean age, (years±SD), and sex) | Measurement of QoL | Results |
|---|---|---|---|---|---|
| D. Shaligram et al. 2007[10] | Bangalore Karnataka South India | The cross-sectional study was conducted by the Department of Psychiatry at Bangalore’s National Institute of Mental Health and Neurosciences. TDT patients in day care at two general hospitals in Bangalore were selected. | Sample size: 39 Sample size justification: not provided Study period: not provided Mean age of approximately 11 years (131.12±29.6). | EQ-5D | Psychological issues affected 44% of the children, while 74% had a lower QoL. The main findings were that 67% of participants had anxiety symptoms, 62% had emotional problems, particularly depression, and 49% had conduct issues. About 64% of children had severe pain or discomfort, which affected their QoL. Depression and mobility issues followed, both severe and affecting 33% of the population. |
| Mohemmed Ajij et al. 2015[11] | New Delhi North India | The cross-sectional study was conducted in the thalassemia day care center of Kalawati Saran Children’s Hospital, New Delhi, India. | Sample size: 108 (cases=40; siblings=28; control=40) Sample size justification: not provided Study period: November 2009 to March 2011. The mean age of the cases=15 years; siblings=16.2 years; and controls 15.5 years. | WHOQOL- BREF | Thalassemia patients scored significantly lower on all subscales than controls. They also had a lower health outlook. Mean subscale scores were significantly lower in both the physical (57.7 vs. 72.4, P<0.001) and psychological domains (56.7 vs. 72.3, P<0.001). The siblings also scored poorly in environmental. Among thalassemia patients, school dropout, reduced stature, and delayed puberty have increased. |
| Rajib Saha et al. 2015[12] | Burdwan West Bengal East India | The cross-sectional descriptive epidemiological study was conducted in Burdwan Medical College and Hospital, West Bengal East India. | Sample size: 365 Sample size justification: not provided Study period: July 2011 to June 2012. The mean age of the children was 8.3±2.4 years. | PedsQL version 4.0 and Generic Core Scale. | The multiple linear regression analysis shows several factors that affect the total summary score. The length since splenectomy accounts for 31.2%, the last pretransfusion Hb level for 20.7%, the family history of thalassemia for 17.3%, and the blood transfusion frequency for 1.3%. These variables account for 70.5% of summary score variation. After splenectomy, thalassemic children had a significantly better QoL for 5 years. For better health, maintain a pretransfusion hemoglobin level above 7 g/dl. |
| Sachin Soni et al. 2016[13] | New Delhi North India | The cross-sectional study was conducted in a day care center in New Delhi. | Sample size: 72 Sample size justification: not provided Study period: not available Mean age: mean (SD) age of 14.6 (7.6) years. | PedsQL version 4.0 | Twenty women were among the 72 participants. Participants were 5–39 years old. Participants’ average age was 14.6 years, with a standard deviation of 7.6 years. Pretransfusion hemoglobin levels were above 9 g/dL in 48.6% of study participants. Oral deferasirox was given to 72.2% of patients. In this study, 20.8% of patients had liver impairment due to viral hepatitis or iron overload. Patients had 23.6% growth failure and 4.1% osteoporosis. Additionally, 16.6% of patients had multiple medical conditions.. |
| Sapna Sharma et al. 2016[14] | Mumbai Maharashtra Central India | Gandhi Mission Medical College and Hospital and NMMC Hospital in Navi-Mumbai, India, conducted a cross-sectional study. Cases included children and carers with β-thalassemia major aged 2 to 18 years. The excluded children with β-thalassemia had other serious illnesses. As controls, the study used carers and children and adolescents aged 2 to 18 years without β-thalassemia major. | Sample size: 155 Sample size justification: not provided Study period: April through September 2014. The mean (SD) age of cases was 7.4 (4.7) years, and of controls was 7.1 (3.3) years. | PedsQL | The child report showed significantly lower QoL scores in cases compared to controls (83.7 (10.8) vs. 97.6 (3.3); P<0.001). Parents reported significantly lower total QoL scores in cases compared to controls (84.2 (11.9) vs. 96.7 (3.5); P<0.001). Compared to the control group, caretakers reported a significantly higher prevalence of poor health (29.2% vs. 2.5%, P<0.001). Carers of children with thalassemia were more likely to report poor health than the control group after adjusting for age, gender, socioeconomic level, and parent total QoL score. |
| Kapil Chordiya et al. 2018[15] | Jodhpur Rajasthan West India | The study was conducted at the Dr. SNMC, Jodhpur, Department of Pediatrics. The 8- to 18-year-old adolescents were enrolled in the study. | Sample size: 93 Sample justification: not provided Study period: January 2016 through December 2016. The mean age of children was 11.8±3.2 years. | PedsQL | The average age of the children was 11.8±3.2 years. Physical, emotional, and social functioning had mean scores of 73.9, 82.2, and 83.49, respectively, while school functioning had the lowest mean score of 57.4. The age-group of 8–12 years had a significantly higher mean PedsQL score than the age-group of 13–18 years (P=0.024). The PedsQL scores of monthly transfusion patients (P=0.028) and combination chelation therapy patients (P=0.039) differed significantly. Gender, education, thalassemia, family history, ferritin, splenectomy, and consanguinity did not affect HRQoL. |
| Arulmani Thiyagarajan et al. 2020[16] | Chennai Tamil Nadu South India | The clinic of the thalassemia treatment center presented the study. The study was open to children under 18 with transfusion-dependent (major) thalassemia. Children with debilitating conditions other than thalassemia major were excluded from the study. | Sample size: 125 thalassemia patients and 125 parents Sample justification: provided Study period: January to July 31, 2017. | KIDSCREEN-10 and Ryff Psychological Well-being Scale children and parents, respectively | Family income, children’s education, and parent education affect thalassemia children’s HRQoL, according to our study. Child HRQoL averages 16.28, with a standard deviation of 3.432. Parents’ psychological well-being score averages 83.99, with a standard deviation of 11.41. The psychological well-being of parents positively affects children’s HRQoL. |
| Bijit Biswas et al. 2021[17] | Kolkata West Bengal East India | The hospital-based cross-sectional study was conducted in a Calcutta thalassemia day care unit. The study was limited to children diagnosed with TM. | Sample size: 328 Sample justification: not provided Study period: May 2016 to April 2017 Most of the study participants (37.2%) were aged between 11 and 12 years (5–12 years). | PedsQL version 4.0 | The study revealed that 48.2% of participants had an average body mass index (BMI) of 13.9±1.6 kg/m2. Note that all underweight children in this study showed malnutrition. Kids were neither obese nor overweight. Most of the study participants (37.2%) were 11–12 years old, encompassing the broader range of 5–12 years. |
| Mani Nandy Mitra et al. 2021[18] | Kolkata West Bengal East India | For this study, interviews were conducted with the parents or carers of thalassemia patients who attended a creche that specialized in blood transfusions. Samples of thalassemia day care center children aged 6 to 12 years were taken. | Sample size: 100 Sample justification: not provided Study period: December 1, 2018, to December 31, 2018 | EuroQoL-5 | The study found that 91% of children had mild psychological issues, and 9% had moderate ones. Not one person had a severe disease. The study found that 100% of participants had anxiety and sadness, while 94% had conduct issues. Somatization (77%), low intelligence quotient (IQ) (95%), and behavioral disorders were also present. Worry and despair (94%), pain and discomfort (91%), difficulties with daily activities (83%), and mobility (67%) reduced the QoL for most children. Psychological disorders significantly predicted QoL decline. |
-
QoL and Age
Of the nine included studies, eight studies[10–15,17–19] had respondents from the age-group of 7 to 15 years. Sachin Soni et al.[13] found a negative correlation between age and social functioning. Arulmani Thiyagarajan et al.[16] found that age plays no role in predicting HRQoL. The findings of a study conducted by Sapna Sharma et al.[14] indicate that individuals in all age-groups who were classified as cases had significantly lower total QoL scores than their respective controls.
-
QoL and Physical and Emotional Health
Mani Nandy Mitra et al.[18] revealed that 59% had poor physical health. According to Kapil Chordiya et al.,[15] more frequent hospital visits negatively affect children’s physical and psychological burden and academic performance. A cross-sectional study in New Delhi[13] also found that thalassemia treatment affects physical, emotional, and social functioning, impairing QoL.
-
QoL and Blood Transfusion
Several studies[10,12–15,18] have stated that patients with TDT have a poor QoL. However, Arulmani Thiyagarajan et al.[16] suggested that the transfusion interval does not influence the children’s QoL.
-
QoL and social determinants
Several studies[11,14] have shown that social determinants, such as age, sex, socioeconomic status, and parents’ education, play an essential role in determining the QoL of thalassemia patients.
-
QoL and consanguineous marriage
The QoL of thalassemia patients can be significantly affected by consanguineous marriages, which are marriages between close blood relatives such as first cousins. Thalassemia is a genetic disorder, and the risk of thalassemia is higher in the offspring of consanguineous couples who carry the same recessive thalassemia gene mutations. A study by Saha et al.[12] concluded that consanguineous marriage had a positive correlation with the QoL of thalassemia patients and consanguineous marriage.
Discussion
QoL helps in assessing the population’s health. Various studies have evaluated the QoL concerning physical, environmental, emotional, and social determinants among β-thalassemia children (major—Tx; and intermedia—non-Tx) across the Mediterranean, Asian, Middle Eastern, and Africa.[20–23] Irrespective of the types, studies showed that Tx and non-Tx have been affected by the factors mentioned.[24] In our review, it has been proven that age negatively influences the QoL; the higher the age of the children, the greater it affects their emotional and social functioning.[12,13,15]
Similarly, the studies conducted by Mikael NA et al.[25] Runqi Zhang et al.,[26] and Koorosh Etemad et al.[27] corroborated a negative correlation between QoL. However, the Tx and non-Tx significantly impact HRQoL.[24] The transfusion schedule positively correlates with age, affecting the school performance among thalassemia major children compared to the intermedia.[14,23,27] A study conducted by Ismail et al.[7] and Thavorncharoensap M et al.[28] also identified that age has a different negative impact and significant (P < 0.05) on the children’s QoL.
From this review, we can witness that the physical domain affecting the HRQoL and QoL is significant, and about 59% of them are affected physically.[18] Research conducted by Kaheni et al.[29] and Maha Badawi[30] et al. showed the lowest mean scores of 25 and 54, and the differences can be due to limitations on comparison between age-groups impacting health needs and perception.[31] In addition, treatment methods, such as chelation therapy, which is associated with side effects, cause arthritis and discomfort resulting in physical effects.[10,18]
However, psychosocial impact has been higher compared to physical aspects in studies conducted in India and across the thalassemia-prevalent countries.[15,23–25] Moreover, psychological factors can contribute to adherence to treatment that will synergize with physical[32] characteristics and vice versa.
Transfusion frequency among children with Tx contributes to poor QoL in India.[12–14] These results are in concordance with the studies by Maha Badawi et al.,[30] where the transfusion-dependent children reported poor social functioning, which is likely due to the frequency of visits to the hospital leading to school absenteeism and subsequently affecting the academic requirements and their overall QoL due to morbidity.
As the children grow through repeated transfusion, the treatment procedure has led to anxiety, depression,[10,15] and finally, social withdrawal due to the effects of chronic illness. Accordingly, patients who received it for more than 10 years scored lower HRQoL associated with other complications, which is also notable.[32] However, Wonke et al.[33] suggested that HRQoL and QoL can be improved if patient care is managed with safe blood transfusion and innovative use of iron-chelating drugs. The socioeconomic status of parent’s education played a crucial role in managing the QoL of thalassemia children in our review.[14,34] These studies agree with Sachith Mettananda et al.,[35] which revealed that the fathers’ education and profession had a significant association with higher scores of HRQoL in all aspects, including physical (P < 0.01), psychological (P < 0.01), and social domain (P < 0.01).
Limitations
This review uses a comprehensive search strategy, including academic databases and gray literature sources, to address the limited research on the QoL in thalassemia. The study aimed to align research questions with existing information, and a search was conducted in three well-known academic databases. However, the review has limitations, as it did not evaluate the quality of the literature due to the inclusion of diverse types of records. The review’s comprehensive inclusion criteria were necessary to address the limited research on this subject matter.
Conclusion
The results of our study indicate that children experience a low QoL. Thalassemia adversely affects physical, emotional, social, and school functioning. There is a need to increase parental and family awareness regarding child health, particularly in cases where a particular disease has occurred for the first time. It is advisable to promote the use of support groups, psychosocial counseling, and emotional support. Likewise, pediatricians can organize educational camps to raise awareness about thalassemia management and facilitate problem-solving sessions with the assistance of non-profit organizations. Enhanced healthcare treatments, psychological, continuous care programs, cognitive behavioral therapy, acceptance, and commitment therapy and educational, and self-care programs designated for thalassemia children and parents are essential for a better QoL.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Colah R, Gorakshakar A, Phanasgaonkar S, D’Souza E, Nadkarni A, Surve R, et al. Epidemiology of ?-thalassaemia in Western India: Mapping the frequencies and mutations in sub-regions of Maharashtra and Gujarat. Br J Haematol. 2010;149:739–47. doi: 10.1111/j.1365-2141.2010.08131.x. [DOI] [PubMed] [Google Scholar]
- 2.Verma IC, Bijarnia S. The burden of genetic disorders in India and a framework for community control. Community Genet. 2002;5:192–6. doi: 10.1159/000066335. [DOI] [PubMed] [Google Scholar]
- 3.Jawahirani A, Mamtani M, Das K, Rughwani V, Kulkarni H. Prevalence of ?-thalassaemia in subcastes of Indian Sindhis: Results from a two-phase survey. Public Health. 2007;121:193–8. doi: 10.1016/j.puhe.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 4.Madan N, Sharma S, Sood S, Colah R, Bhatia H. Frequency of ?-thalassemia trait and other hemoglobinopathies in northern and western India. Indian J Hum Genet. 2010;16:16–25. doi: 10.4103/0971-6866.64941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ngim CF, Lai NM, Ibrahim H, Ratnasingam V. Attitudes towards prenatal diagnosis and abortion in a multi-ethnic country: A survey among parents of children with thalassaemia major in Malaysia. J Community Genet. 2013;4:215–21. doi: 10.1007/s12687-012-0133-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Viprakasit V, Ekwattanakit S. Clinical classification, screening and diagnosis for thalassemia. Hematol Oncol Clin North Am. 2018;32:193–211. doi: 10.1016/j.hoc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 7.Ismail A, Campbell MJ, Ibrahim HM, Jones GL. Health related quality of life in Malaysian children with thalassaemia. Health Qual Life Outcomes. 2006;4:1–8. doi: 10.1186/1477-7525-4-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong FY, Yang L, Yuen JWM, Chang KKP, Wong FKY. Assessing quality of life using WHOQOL-BREF: A cross-sectional study on the association between quality of life and neighborhood environmental satisfaction, and the mediating effect of health-related behaviors. BMC Public Health. 2018;18:1–14. doi: 10.1186/s12889-018-5942-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karimi M, Brazier J. Health, health-related quality of life, and quality of life: What is the difference? Pharmacoeconomics. 2016;34:645–9. doi: 10.1007/s40273-016-0389-9. [DOI] [PubMed] [Google Scholar]
- 10.Shaligram D, Girimaji SC, Chaturvedi SK. Psychological problems and quality of life in children with thalassemia. Indian J Pediatr. 2007;74:727–30. doi: 10.1007/s12098-007-0127-6. [DOI] [PubMed] [Google Scholar]
- 11.Ajij M, Pemde HK, Chandra J. Quality of life of adolescents with transfusion-dependent thalassemia and their siblings: A cross-sectional study. J Pediatr Hematol Oncol. 2015;37:200–3. doi: 10.1097/MPH.0000000000000244. [DOI] [PubMed] [Google Scholar]
- 12.Saha R, Misra R, Saha I. Health related quality of life and its predictors among Bengali Thalassemic children admitted to a tertiary care hospital. Indian J Pediatr. 2015;82:909–16. doi: 10.1007/s12098-014-1670-6. [DOI] [PubMed] [Google Scholar]
- 13.Soni S, Thawani R, Idhate T, Kalra M, Mahajan A. Health related quality of life in patients with transfusion-dependent thalassemia. Indian Pediatr. 2016;53:741–2. doi: 10.1007/s13312-016-0923-z. [DOI] [PubMed] [Google Scholar]
- 14.Sharma S, Seth B, Jawade P, Ingale M, Setia MS. Quality of life in children with thalassemia and their caregivers in India. Indian J Pediatr. 2017;84:188–94. doi: 10.1007/s12098-016-2267-z. [DOI] [PubMed] [Google Scholar]
- 15.Chordiya K, Katewa V, Sharma P, Deopa B, Katewa S. Quality of Life (QoL) and the factors affecting it in transfusion-dependent thalassemic children. Indian J Pediatr. 2018;85:978–83. doi: 10.1007/s12098-018-2697-x. [DOI] [PubMed] [Google Scholar]
- 16.Thiyagarajan A, Bagavandas M, Kosalram K. Assessing the role of family well-being on the quality of life of Indian children with thalassemia. BMC Pediatr. 2019;19:1–6. doi: 10.1186/s12887-019-1466-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Biswas B, Naskar NN, Basu K, Dasgupta A, Basu R, Paul B. Malnutrition, its attributes, and impact on quality of life: An epidemiological study among ?-thalassemia major children. Korean J Fam Med. 2021;42:66–72. doi: 10.4082/kjfm.19.0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mitra MN, Bag R, Garg M, Mandal PK, Dolai TK. Psychological Problems and quality of life among transfusion-dependent thalassemic children: Sharing experience from a thalassemia care center in West Bengal, India. Int J Nur Res. 2021;7:8–14. [Google Scholar]
- 19.Biswas B, Naskar NN, Basu K, Dasgupta A, Basu R, Paul B. Care-related quality of life of caregivers of beta-thalassemia major children: An epidemiological study in Eastern India. J Epidemiol Glob Health. 2020;10:168–77. doi: 10.2991/jegh.k.200102.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caocci G, Efficace F, Ciotti F, Roncarolo MG, Vacca A, Piras E, et al. Health related quality of life in Middle Eastern children with beta-thalassemia. BMC Blood Disord. 2012;12:6. doi: 10.1186/1471-2326-12-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Torcharus K, Pankaew T. Health-related quality of life in Thai thalassemic children treated with iron chelation. Southeast Asian J Trop Med Public Health. 2011;42:951–9. [PubMed] [Google Scholar]
- 22.Amoudi AS, Balkhoyor AH, Abulaban AA, Azab AM, Radi SA, Ayoub MD, et al. Quality of life among adults with betathalassemia major in western Saudi Arabia. Saudi Med J. 2014;35:882–5. [PubMed] [Google Scholar]
- 23.Hakeem GLA, Mousa SO, Moustafa AN, Mahgoob MH, Hassan EE. Health-related quality of life in pediatric and adolescent patients with transfusion-dependent ß-thalassemia in upper Egypt (single center study) Health Qual Life Outcomes. 2018;16:1–9. doi: 10.1186/s12955-018-0893-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.European J of Haematology-2023-Cappellini-health-related quality of life in patients with -thalassemia Data from.pdf. doi: 10.1111/ejh.13975. [DOI] [PubMed] [Google Scholar]
- 25.Mikael NA, Al-Allawi NAS. Factors affecting quality of life in children and adolescents with Thalassemia in Iraqi Kurdistan. Saudi Med J. 2018;39:799–807. doi: 10.15537/smj.2018.8.23315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang R, Zhang S, Ming J, Xie J, Liu B, Chen C, et al. Predictors of health state utility values using SF-6D for Chinese adult patients with ?-thalassemia major. Front Public Health. 2023;10:1072866. doi: 10.3389/fpubh.2022.1072866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Etemad K, Mohseni P, Aghighi M, Bahadorimonfared A, Hantooshzadeh R, Taherpour N, et al. Quality of life and related factors in ?-thalassemia patients. Hemoglobin. 2021;45:245–9. doi: 10.1080/03630269.2021.1965617. [DOI] [PubMed] [Google Scholar]
- 28.Thavorncharoensap M, Torcharus K, Nuchprayoon I, Riewpaiboon A, Indaratna K, Ubol BO. Factors affecting health-related quality of life in Thai children with thalassemia. BMC Blood Disord. 2010;10:1–10. doi: 10.1186/1471-2326-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kaheni S, Yaghobian M, Sharefzadah GH, Vahidi A, Ghorbani H, Abderahemi A. Quality of life in children with ?-thalassemia major at center for special diseases. Iran J Ped Hematol Oncol. 2013;3:108–13. [PMC free article] [PubMed] [Google Scholar]
- 30.Badawi MA, Alkhamesi SM, Alsulaimani DS, Khodary A, Almutairi KA, Alsolaimani RS, et al. Patient activation measure among transfusion-Dependent patients with hemoglobinopathies. J Appl Hematol. 2022;13:263–7. [Google Scholar]
- 31.Surapolcha P, Satayasa W, Sinlapamongkolku P, Udomsubpayaku U. Biopsychosocial predictors of health-related quality of life in children with thalassemia in Thammasat University Hospital. J Med Assoc Thai. 2010;93(Suppl 7):65–75. [PubMed] [Google Scholar]
- 32.Shafie AA, Chhabra IK, Wong JHY, Mohammed NS, Ibrahim HM, Alias H. Health-related quality of life among children with transfusion-dependent thalassemia: A cross-sectional study in Malaysia. Health Qual Life Outcomes. 2020;18:1–11. doi: 10.1186/s12955-020-01381-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wonke B. Clinical management of ?-Thalassemia major. Semin Hematol. 2001;38:350–9. doi: 10.1016/s0037-1963(01)90029-0. [DOI] [PubMed] [Google Scholar]
- 34.Ajij M, Pemde HK, Chandra J. Quality of life of adolescents with transfusion-dependent thalassemia and their siblings: A cross-sectional study. J Pediatr Hematol Oncol. 2015;37:200–3. doi: 10.1097/MPH.0000000000000244. [DOI] [PubMed] [Google Scholar]
- 35.Mettananda S, Pathiraja H, Peiris R, Bandara D, De Silva U, Mettananda C, et al. Health related quality of life among children with transfusion dependent ?-thalassaemia major and haemoglobin e ?-thalassaemia in Sri Lanka: A case control study. Health Qual Life Outcomes. 2019;17:1–13. doi: 10.1186/s12955-019-1207-9. [DOI] [PMC free article] [PubMed] [Google Scholar]