ABSTRACT
Introduction:
Systemic lupus erythematosus (SLE) is an autoimmune disease that affects both men and women differently and has a variety of multisystemic symptoms. One of the diseases most often affected target organs is the skin. Different ethnic and racial groupings may display variations in disease incidence, clinical heterogeneity, and severity depending on environmental, cultural, or genetic factors. This study is conducted to determine the prevalence of SLE’s cutaneous symptoms and their relationship to organ involvement.
Materials and Methods:
Data were gathered for this study from the patient chart, the study design was the retrospective chart review after the consent of the patients and obtaining an ethical approval, The study was carried out in Aseer Central Hospital, Abha Saudi Arabia
Results:
Out of a total of 100 patients 92% were females while 8% were males. The mean (SD) of the age of the respondent was 38.3 (8.5). 89.2 of the respondents had skin manifestations
Conclusion:
A thorough understanding of SLE skin lesions will aid in the accurate identification of the condition and in the effective therapy of lupus patients. In order to more accurately diagnose cutaneous lesions in SLE patients, we need more dermatology and rheumatology clinics that combine expertise together.
Keywords: Dermatology, lupus, malar, rash, rheumatology, SLE
Introduction
Systemic lupus erythematosus (SLE) is an autoimmune disease that affects both men and women differently and has a variety of multisystemic symptoms. One of the diseases most often affected target organs is the skin. Different ethnic and racial groupings may display variations in disease incidence, clinical heterogeneity, and severity depending on environmental, cultural, or genetic factors.[1,2]
A skin condition is one of the most prevalent clinical issues among SLE patients. Lupus erythematosus skin lesions can appear with or without systemic illness. There are various subtypes of cutaneous LE, including acute, subacute, and chronic. The three most common mucocutaneous signs of SLE are mouth ulcers, baldness, and malar rash. Acute, subacute, and chronic cutaneous symptoms are the three categories. The butterfly rashes of acute cutaneous lupus are photosensitive lesions that appear in the malar region. Patients with colorful skin may only experience minimal photosensitivity. The nasolabial folds are typically spared by butterfly rashes, which can range in severity from mild erythema and irritation to severe facial edema. On occasion, it can be challenging cutaneous manifestations in SLE patients in hospital.[3,4,5]
Nephritis, a kidney illness, affects about one-third of persons with SLE. SLE patients may also experience heart issues, such as pericarditis, an inflammation of the sac-like membrane surrounding the heart, and faulty heart valves, which regulate blood flow in the heart. People with SLE are significantly more likely to develop atherosclerosis, a condition that results in heart disease and is brought on by fatty build-up in the blood vessels. The inflammation that characterizes SLE can harm the nerve system and cause seizures, strokes, cognitive impairment, altered sensation, and weakness in the limbs (peripheral neuropathy), as well as other neurological problems. In SLE, depression and anxiety are also prevalent. Cutaneous lesions are the first symptom in 23–28% of SLE patients and can manifest at any stage of the disease, regardless of disease activity. It affects 72–85% of people with SLE. Comparing SLE to other connective tissue disorders using the 11 ACR criteria can be helpful, although the relatively high number of dermatological criteria (malar rash, discoid lesions, photosensitivity, and mouth ulcers) could cause SLE to be overdiagnosed.[4,5,6,7]
With cutaneous signs occurring in 70% to 85% of people throughout the disease and as a presenting symptom in up to 25% of patients, the skin is the second most often affected organ system in SLE.[8]
SLE frequently has cutaneous manifestations. They are less common in children and vary between early- and late-onset SLE.[8] Most SLE patients begin to experience cutaneous symptoms, which are frequently an early indicator of the disease. Despite the fact that the exact cause of LE is unknown, it is known to be a complex condition with genetic and environmental elements that cause immunological activation. Due to the variety of skin lesions linked to LE, they can now be divided into LE-specific and LE-nonspecific lesions.[9]
Retrospective research stated that SLE is becoming more commonly recognized in Saudi Arabia, and the clinical pattern is evident. A prospective multicenter approach including more patients is required to identify the prevalence of SLE and to more accurately define the prognostic factors associated with the illness based on the literature.
This study is conducted to determine the prevalence of SLE’s cutaneous symptoms and their relationship to organ involvement.
Materials and Methods
SLE patients who fulfilled ACR classification criteria at Aseer Central Hospital and Khamis Madani Hospital, after the consent of the patients and approval from the hospital administration. Then we interviewed patients individually, and we filled a Google Form that had 25 questions, targeting diagnosis, and skin manifestations. The study was carried out in Abha Saudi Arabia.
Skin manifestations were defined as acute (butterfly rash, photosensitivity) and chronic (discoid rash).
Following data collection, data were coded and input into the SPSS ver. 20 programs for analysis of descriptive statistics (mean, standard deviation, frequencies, and percentages were computed), and t-test and Chi-square test were used to assess statistical differences at the 5% level of significance. The Saudi Ministry of Health Aseer region approved ethical approval. The investigation lasted from January to April of 2023. After reviewing charts, we have selected patients who fulfilled lupus ACR classification criteria, age 18 and above, Then, we contacted patients individually and interviewed them to fill a Google Form. Afterward, we filled a spreadsheet and started analysis using the most appropriate statistical techniques.
Results
In this, we have used simple random sampling among SLE patients, total proposed sample size was 110, out of 110, total 100 respondents filled the Google Form and respondent, so the response rate was 91%. The mean (SD) of the age of the respondent was 38.3 (8.5).
As per Table 1, most of the respondents were having an age less than 40 years (57%) while 33% lies between the 40 and 50 years age group. 14% had HTN, 11% had kidney disease, 38% had others while 29% had no chronic diseases. 42% got an university level of education, 27%, 26%, and 5% secondary, primary, and middle level of education, 92% were females while 8% were males, 62% were married, 24% were single rest were separated. Current smokers were only 3%
Table 1.
Demographics
| Frequency | Percentage | |
|---|---|---|
| Age in years | ||
| 40-50 | 33 | 33.0 |
| 50-60 | 9 | 9.0 |
| Above 60 | 1 | 1.0 |
| <40 years | 57 | 57.0 |
| Education | ||
| Middle | 5 | 5.0 |
| Primary | 26 | 26.0 |
| Secondary | 27 | 27.0 |
| University | 42 | 42.0 |
| Gender | ||
| Female | 92 | 92.0 |
| Male | 8 | 8.0 |
| Marital Status | ||
| Divorced | 9 | 9.0 |
| Married | 62 | 62.0 |
| Single | 24 | 24.0 |
| Widow | 5 | 5.0 |
| Smoking | ||
| No | 96 | 96.0 |
| Previous smoker | 2 | 2.0 |
| Yes | 3 | 3.0 |
| Total | 100 | 100.0 |
As per Table 2, we have observed that 36% had arthritis joint pain in the past, 57% had nowadays, 7% did not have any sort of arthritis joint pain, 21% currently had circular disc-like rash, 14% had currently a facial rash around the nose and mouth that looks like a butterfly, 36% had blood diseases nowadays, 69% often suffering from dry eyes and mouth, 20% had baldness, 13% were using tropical treatment, 73% had agreed that their skin symptoms worsen with sunlight photosensitivity.
Table 2.
Variables related to SLE
| Frequency | Percentage | |
|---|---|---|
| Arthritis joint pain | ||
| In the past | 36 | 36.0 |
| Not found | 7 | 7.0 |
| Nowadays | 57 | 57.0 |
| A circular disc-like rash | ||
| In the past | 20 | 20.0 |
| Not found | 59 | 59.0 |
| Nowadays | 21 | 21.0 |
| a facial rash around the nose and mouth that looks like a butterfly | ||
| In the past | 31 | 31.0 |
| Not found | 55 | 55.0 |
| Nowadays | 14 | 14.0 |
| Blood diseases anemia, decrease in white blood cells, decrease in platelets | ||
| In the past | 25 | 25.0 |
| Not found | 39 | 39.0 |
| Nowadays | 36 | 36.0 |
| Do you often suffer from dry eyes and mouth? | ||
| No | 31 | 31.0 |
| Yes | 69 | 69.0 |
| Do you suffer from baldness? | ||
| in many places on the scalp | 7 | 7.0 |
| in one specific location on the scalp | 13 | 13.0 |
| Not found | 80 | 80.0 |
| Do you use a topical treatment? | ||
| No | 87 | 87.0 |
| Yes | 13 | 13.0 |
| Do you use tablet pills? | ||
| No | 16 | 16.0 |
| Yes | 84 | 84.0 |
| Do you wear sunscreen? | ||
| Always | 14 | 14.0 |
| Never | 41 | 41.0 |
| Sometimes | 37 | 37.0 |
| Usually | 8 | 8.0 |
| Do your skin symptoms worsen with sunlight photosensitivity? | ||
| No | 27 | 27.0 |
| Yes | 73 | 73.0 |
As per Figure 1, 89.02% of the respondents had skin manifestations problems.
Figure 1.
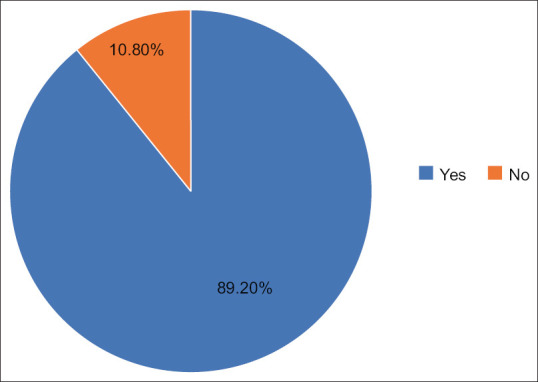
Skin manifestation
As per Figure 2, 61% believed that these diseases creating problems in their lifestyle.
Figure 2.
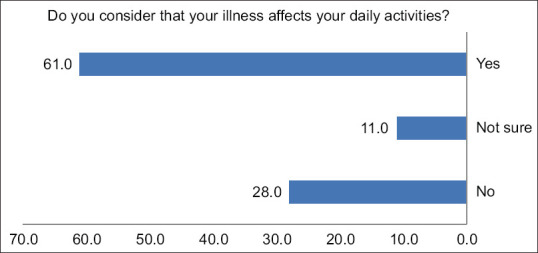
Effect on daily activities
As per Figure 3, 42% of the skin manifestations patients had problems in hands, 25% in foot, 17% in chest, while 8% each in ears and scalp.
Figure 3.
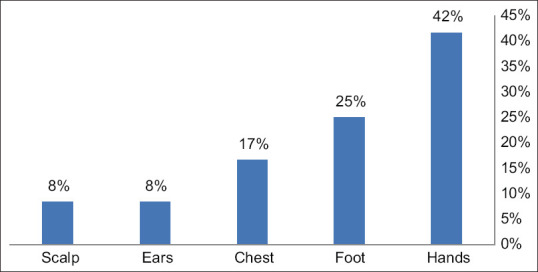
Organs involved
As per Table 3, we did not observe any significant impact of anemia with skin problems in our sample size.
Table 3.
Comparison between anemia and symptoms of skin problems
| Comparison between anemia and symptoms of skin problems | ||||
|---|---|---|---|---|
|
| ||||
| Variables | Freq (%) | Do you have the skin symptoms | Total | |
|
| ||||
| No | Yes | |||
| Blood diseases anemia, decrease in white blood cells, decrease in platelets | ||||
| In the past | Count | 21 | 4 | 25 |
| % | 84.0% | 16.0% | 100.0% | |
| Not found | Count | 35 | 4 | 39 |
| % | 89.7% | 10.3% | 100.0% | |
| Nowadays | Count | 32 | 4 | 36 |
| % | 88.9% | 11.1% | 100.0% | |
| Total | Count | 88 | 12 | 100 |
| % | 88.0% | 12.0% | 100.0% | |
P=0.772
Discussion
SLE is a multiorgan autoimmune disease with a wide range of clinical symptoms. Up to 85% of cases of SLE and cutaneous lupus erythematosus (CLE) may solely affect the skin.[10,11]
Based on the clinical, histopathology, and immunohistology of skin lesions, LE’s cutaneous symptoms are diagnosed. Furthermore, serum autoantibodies are regarded as immunologic indicators for various clinical forms of the disease. Used as a clinical tool, the Cutaneous Lupus Erythematosus Disease Area and Severity Index (CLASI) standardizes the way disease activity is characterized and offers guidance for spotting a clinical change.[12,13,14]
This study aimed to evaluate the prevalence of cutaneous manifestations of SLE and to find out the association with organ involvement. Patients with SLE have both unique and general cutaneous characteristics.
In our study, the mean age was 24 which is in line with Indian-based study, while we had 92% females which is also in line with other published researches.[15,16]
In our study only 12 of the 100 (12%), SLE patients who responded who were hospitalized in our study showed concurrent cutaneous signs, which is slightly fewer than what was previously described by another study. According to a study, the kind and quantity of cutaneous lesions in SLE serve as a valuable and trustworthy indicator of the disease’s activity and prognosis. From the 12 patients who had reported skin issues or symptoms, we discovered that 54.9% of them had three or more cutaneous manifestations, compared to 19.4% who had just one. In our study, more than 70% of the respondents had photosynthesis problems which is in line with other published studies in Kingdom of Saudi Arabia (KSA).[17]
Skin symptoms of SLE, both particular and general, are well reported. The types of skin lesions and their frequency in hospitalized patients were not identified in the earlier investigations. To categorize skin symptoms and mucocutaneous flare among hospitalized SLE patients, a longitudinal metacentric study is required.[18]
Retrospective case review, a lack of cutaneous manifestations documentation, and inability to see a dermatologist were limiting factors for our study.
What was interesting is despite the fact that one of the proposed pathogenesis is skin-induced, less patient used sunscreen, which could be either lack of education from our side or lack of compliance from patient side. We need to do better, to implement the importance of none pharmacological treatment.
To help predict the possibility of systemic disease and to ensure that patients receive timely dermatologic care with the aim of reducing disease activity to prevent damage, it is crucial for the rheumatologist to be knowledgeable about the range of cutaneous disorders in SLE.[19,20]
Conclusion
To reduce hospitalizations and enhance the prognosis, the skin should always be checked and under control as it is frequently implicated in SLE. It is important for dermatologists and rheumatologists to be aware of how frequently cutaneous symptoms lead to hospitalization. SLE is a multisystem condition, and cutaneous symptoms can provide important diagnostic and prognosis information (e.g. LE-specific skin lesions) since they are linked to disease activity. Morbidity has increased as a result of skin lesions. Therefore, a thorough understanding of SLE skin lesions will aid in the accurate identification of the condition and in the effective therapy of lupus patients. In order to more accurately diagnose cutaneous lesions in SLE patients, rheumatologists and dermatologists should contact more frequently.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We are thankful to Mr. Muhammad Abid khan for his efforts in data analysis.
References
- 1.Ghosh A. Cutaneous manifestations of systemic lupus erythematosus. Indian J Rheumatol. 2007;2:156–64. doi:10.1016/S0973-3698(10)60060-X. [Google Scholar]
- 2.Kalkhoran S, Benowitz NL, Rigotti NA. Reprint of: Prevention and treatment of tobacco use: JACC health promotion series. J Am Coll Cardiol. 2018;72:2964–79. doi: 10.1016/j.jacc.2018.10.020. doi:10.1016/j.jacc.2018.10.020. [DOI] [PubMed] [Google Scholar]
- 3.Patel P, Werth V. Cutaneous lupus erythematosus: A review. Dermatol Clin. 2002;20:373–85. doi: 10.1016/s0733-8635(02)00016-5. v, doi:10.1016/s0733-8635(02)00016-5. [DOI] [PubMed] [Google Scholar]
- 4.Kuhn A, Landmann A. The classification and diagnosis of cutaneous lupus erythematosus. J Autoimmun. 2014;48(9):14–9. doi: 10.1016/j.jaut.2014.01.021. doi:10.1016/j.jaut.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 5.Kuhn A, Sticherling M, Bonsmann G. Clinical manifestations of cutaneous lupus erythematosus. J Dtsch Dermatol Ges. 2007;5:1124–37. doi: 10.1111/j.1610-0387.2007.06554.x. doi:10.1111/j.1610-0387.2007.06554.x. [DOI] [PubMed] [Google Scholar]
- 6.Werth VP. Clinical manifestations of cutaneous lupus erythematosus. Autoimmun Rev. 2005;4:296–302. doi: 10.1016/j.autrev.2005.01.003. doi:10.1016/j.autrev.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 7.Grönhagen CM, Nyberg F. Cutaneous lupus erythematosus: An update. Indian Dermatol Online J. 2014;5:7–13. doi: 10.4103/2229-5178.126020. doi:10.4103/2229-5178.126020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anaba EL, Cole-Adeife O, Olaosebikan H, Dawodu OO. Manifestation C, Systemic OF, At E, Diagnosis I, Rheumatology ATA, Lagos CIN. ORIGINAL ARTICLE CUTANEOUS MANIFESTATION OF SYSTEMIC LUPUS ERYTHEMATOSUS AT INITIAL DIAGNOSIS AT A RHEUMATOLOGY. 2021;7:17–23. [Google Scholar]
- 9.Hejazi EZ, Werth VP. Cutaneous lupus erythematosus: An update on pathogenesis, diagnosis and treatment. Am J Clin Dermatol. 2016;17:135–46. doi: 10.1007/s40257-016-0173-9. doi:10.1007/s40257-016-0173-9. [DOI] [PubMed] [Google Scholar]
- 10.Chanprapaph K, Tankunakorn J, Suchonwanit P, Rutnin S. Dermatologic manifestations, histologic features and disease progression among cutaneous lupus erythematosus subtypes: A prospective observational study in Asians. Dermatol Ther (Heidelb) 2021;11:131–47. doi: 10.1007/s13555-020-00471-y. doi:10.1007/s13555-020-00471-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hersh AO, Arkin LM, Prahalad S. Immunogenetics of cutaneous lupus erythematosus. Curr Opin Pediatr. 2016;28:470–5. doi: 10.1097/MOP.0000000000000383. doi:10.1097/MOP.0000000000000383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chanprapaph K, Tubtieng I, Pratumchat N, Thadanipon K, Rattanakaemakorn P, Suchonwanit P. Cutaneous, systemic features and laboratory characteristics of late- versus adult-onset systemic lupus erythematosus in 1006 Thai patients. Lupus. 2021;30:785–94. doi: 10.1177/0961203321991920. doi:10.1177/0961203321991920. [DOI] [PubMed] [Google Scholar]
- 13.Udompanich S, Chanprapaph K, Suchonwanit P. Hair and scalp changes in cutaneous and systemic lupus erythematosus. Am J Clin Dermatol. 2018;19:679–94. doi: 10.1007/s40257-018-0363-8. doi:10.1007/s40257-018-0363-8. [DOI] [PubMed] [Google Scholar]
- 14.Cooper EE, Pisano CE, Shapiro SC. Cutaneous manifestations of “Lupus”: Systemic lupus erythematosus and beyond. Int J Rheumatol. 2021;2021:6610509. doi: 10.1155/2021/6610509. doi:10.1155/2021/6610509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fabbri P, Cardinali C, Giomi B, Caproni M. Cutaneous lupus erythematosus: Diagnosis and management. Am J Clin Dermatol. 2003;4:449–65. doi: 10.2165/00128071-200304070-00002. [DOI] [PubMed] [Google Scholar]
- 16.Petty AJ, Floyd L, Henderson C, Nicholas MW. Cutaneous lupus erythematosus: Progress and challenges. Curr Allergy Asthma Rep. 2020;20:12. doi: 10.1007/s11882-020-00906-8. doi:10.1007/s11882-020-00906-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bourré-Tessier J, Peschken CA, Bernatsky S, Joseph L, Clarke AE, Fortin PR, et al. Association of smoking with cutaneous manifestations in systemic lupus erythematosus. Arthritis Care Res (Hoboken) 2013;65:1275–80. doi: 10.1002/acr.21966. doi:10.1002/acr.21966. [DOI] [PubMed] [Google Scholar]
- 18.Lu Q, Long H, Chow S, Hidayat S, Danarti R, Listiawan Y, et al. Guideline for the diagnosis, treatment and long-term management of cutaneous lupus erythematosus. J Autoimmun. 2021;123:102707. doi: 10.1016/j.jaut.2021.102707. doi:10.1016/j.jaut.2021.102707. [DOI] [PubMed] [Google Scholar]
- 19.Kuhn A, Meuth AM, Bein D, Amler S, Beissert S, Böhm M, et al. Revised cutaneous lupus erythematosus disease area and severity index (RCLASI): A modified outcome instrument for cutaneous lupus erythematosus. Br J Dermatol. 2010;163:83–92. doi: 10.1111/j.1365-2133.2010.09799.x. doi:10.1111/j.1365-2133.2010.09799.x. [DOI] [PubMed] [Google Scholar]
- 20.Alballa SR. Systemic lupus erythematosus in Saudi patients. Clin Rheumatol. 1995;14:342–6. doi: 10.1007/BF02208351. doi:10.1007/BF02208351. [DOI] [PubMed] [Google Scholar]


