SUMMARY
Plague raged in Europe for over 1400 years and was responsible for three major pandemics. Today, plague still poses a serious threat to global public health and surveillance is imperative. Plague is still present in natural reservoirs on several continents, including Africa, Asia and the Americas, and sometimes causes local cases and epidemics.
The Third Plague Pandemic caused millions of deaths worldwide, including in Europe. Plague arrived in Europe in the autumn of 1896 mostly through maritime trade routes, where it spread with several epidemic events until 1945, when, in the port city of Taranto, the last known outbreak was recorded. In this paper, we present an overview of the natural history and pathogenicity of Yersinia pestis, the bacterium responsible for plague, its spread from Asia to Europe during the Third Pandemic, and the therapies used to treat and prevent the disease in Europe, with particular focus on the case of Taranto. In Taranto, the Pasteur Institute’s antiserum antimicrobial therapy, and vaccination were used to treat and stop the advance of the bacterium, with mixed results.
Keywords: Plague, third pandemic, vaccination, historical therapies, Yersinia pestis
THE ETIOLOGY OF PLAGUE
Plague is primarily a zoonosis affecting wild rodents in semi-desertic and desertic regions. Rodents, their parasites and the plague bacterium constitute together the natural reservoirs for the occasional spillover from animals to humans [1]. In Europe, no reservoirs are currently present and likely there were any in the past [1]. Regardless, plague caused in Europe three major Pandemic events with high lethality: the First Pandemic, which started with the Plague of Justinian, from the sixth to the eighth centuries CE; the Second Pandemic, which included the infamous Black Death, from 1346 to the 18th century CE; the Third Pandemic, that had its origin in the 18th-century epidemic in the Chinese province of Yunnan, and spread rapidly worldwide when plague reached Hong Kong in 1894 [2].
As a human disease, plague can manifest in three main clinical forms:
Bubonic plague: highly inflammatory and virulent infection. The incubation period is 2 to 3 days. Once the bacterium enters the organism through the dermis due to the bite of an ectoparasite, it is transported by the lymphatic system to the lymph nodes, where it multiplies and causes the so-called ‘bubo’ (a term that derives from the Greek word βουβών, which means groin), mainly in the inguinal region, in the neck or the axilla. In about 60% of cases, death occurs within a week from the appearance of the bubo, if the disease is not treated with an effective antimicrobial therapy [3–5].
Pneumonic plague: is transmitted from person to person by respiratory droplets and causes pneumonia. The patient may present severe symptoms including high fever, fatigue, and cough with blood. Neutrophils attracted to the lungs are responsible for pneumonia and lung tissue necrosis [6]. The incubation period is from 2 to 3 days and within a day cough with sputum appears. In the absence of adequate pharmacological treatments, death occurs in 99% of cases, 24 hours after the onset of symptoms [5].
Septicemic plague: occurs when the bacterium escapes into the bloodstream and produces a systemic infection. If left untreated, it is fatal in almost all cases. Pulmonary and septicemic forms can be primary and/or secondary to bubonic plague and are usually fatal. Yet, in all three forms, symptoms can worsen rapidly, if left untreated [2].
The causative agent of plague, the gram-negative bacterium Yersinia pestis (originally named Pasturella pestis) was identified in 1894 in Hong Kong by the Pasteurian bacteriologist Alexandre Yersin [7].
Today, modern analysis of ancient DNA has been able to confirm that the same bacterium caused all plague pandemics yet, the presence of Y. pestis was identified as far back as Prehistoric times: its oldest strains have been found in the teeth of the GoK2 individual from the Neolithic period and in Eurasian LNBA1 individuals [2, 8–10]. All these ancient strains are now extinct [6].
The bacterium’s genome consists of a circular chromosome and three plasmids, pCD1, pPCP1, and pMT1, which are responsible for its virulence. The latter two are crucial in distinguishing Y. pestis from the diversifying species, Y. pseudotuberculosis, which has a lower pathogenicity to humans [11]. There is insufficient data on the actual pathogenicity of the prehistoric strains, but we know that they did not contain the Yersinia murine toxin2 located on the pMT1 plasmid, which allows Y. pestis to use arthropods such as fleas as disease vectors and cause bubonic plague. These ancestral strains of Y. pestis should have not been capable of transmitting bubonic plague, but they may only have caused pneumonic and septicemic plague. One strain of Y. pestis likely acquired the key mutation of the ymt gene during its evolution (but not before 1686 cal. BCE; [6, 12]). Another gene associated with the pathogenicity of Y. pestis is the plasminogen activator gene3 located on the pPCP1 plasmid with powerful fibrinolytic activity which is responsible for pneumonic plague. It was already present in the ancestral strains [3, 8].
All these virulence factors made plague able to claim tens of millions of victims in historical times, not only because of its ability to use ectoparasites as vectors but also because of its ability to evade the human immune system and avoid phagocytosis by lymphocytes [6].
The pathogenicity of Y. pestis is characterized by two main phases:
Pre-inflammatory phase: it begins after the ectoparasites have injected the pathogen into the dermis and it has reached the lymphatic system. In this phase, the bacterium is transported by the macrophages to the lymph nodes (bubonic plague) or lungs (pneumonic plague), where it multiplies. The host’s immune system can be evaded by Y. pestis thanks to the presence of the capsular antigen F14, encoded by the caf1 gene, which confers resistance to phagocytosis. Furthermore, the presence of a T3SS5 secretion system, encoded by the pCD1 plasmid, translocates Yops6 proteins from the bacterium to the host, leading to the inhibition of phagocytosis and cytokine production [6]. An essential part of this system is the V antigen (LcrV), a virulence factor that plays also an important role in the pathogenesis of Y. pestis, including delivering Yops into the host cells [3, 13].
Inflammatory phase: it starts with the appearance of clinical symptoms (all plague forms) and may evolve into tissue necrosis if the bacterium multiplies in the blood. The latter event marks the onset of septicemic or pneumonic plague.
The pathogenesis of the disease also includes the sequestration of essential host metals, such as zinc and iron, that are involved in many immune functions [6]. Zinc is a micronutrient that can enhance the cytotoxic activity of Natural Killer defence cells and has anti-inflammatory properties. For example, the presence of sufficient amounts of Zinc in the body has been linked to a reduction in infection with SARS-CoV-2, the causative agent of Covid-19 [14].
FROM CHINA TO THE PORTS OF EUROPE (1899–1950 CA)
It has been estimated that the Third Plague Pandemic caused millions of deaths across the world, and Europe was not spared. Plague arrived in Europe in the autumn of 1896, when two sailors from Mombay died on a ship docked on the river Thames in London. The quick spread of the disease around the world was due to the advent of steamships that facilitated the commercial connection between continents. This new vehicle, as well as the steam locomotive, both introduced at the beginning of the nineteenth century, forced international health authorities to face the arrival of important epidemic-prone infectious diseases in Europe [15]. Microbiology, first introduced at the end of the nineteenth century, furnished new knowledge and three international conferences were held in Europe by health authorities to discuss preventive measures against epidemic diseases (including plague): 1892 in Venice, 1893 in Dresden and 1894 in Paris. Thanks to the effective health measures instituted, from 1899 to 1947, only 1692 cases of plague and 457 deaths were reported in Europe, and they were concentrated in particular in cities with sea or river ports [2]. In the rest of the world, the Third Pandemic has instead caused millions of deaths in just over 100 years, of which 10 million in India alone [3, 16]. The last cases of plague in Europe occurred in Corsica and Italy in 1945 after the end of the Second World War, and in Russia at Kaliningrad in 1947 [2, 16].
The role of rats (black rats and brown rats) and ectoparasites
One of the first to observe that rats were involved in the transmission of the disease was Alexandre Yersin in 1894; his theory was confirmed some years later by Waldemar Haffkine and Paul-Louis Simond, who proposed that the rat flea was the major vector for Y. pestis [4, 6]. Indeed, during the Third Pandemic, epidemics in Asia and India were preceded by a great mortality of rats, whose cadavers literally covered the streets [2]. When a rat dies and its body temperature drops, in the absence of another rat to colonize, its fleas are forced to jump on any other mammal (including humans) to survive [2, 17]. This mechanism was often observed in Asia and India as the main transmission mechanism for sustaining epidemics.
In Europe, during the Third Pandemic, two species of rats could carry plague: Rattus rattus, commonly known as the black rat, was attested in Western Europe till medieval times, whereas Rattus norvegicus, known as the brown rat, originated in Russia and migrated to Europe in the eighteen century. The two species have different behaviours, already studied in the 1950s by the zoologist Davis [18]. The black rat can climb the walls and roofs of the buildings where it lives and is more in contact with humans. Boats are also part of its frequentation range. The brown rat, on the other hand, prefers to be outdoors, in waterways and sewers, given that it can endure the harsh European climate better than R. rattus.
With this knowledge, during the Third Pandemic, rodent control measures were one of the most important procedures carried out to prevent the propagation of the disease both in cities and on ships. Nevertheless, when plague spread in Glasgow in the autumn of 1900, of the more than 300 rats captured, none had signs of infection [19]. Paradoxically, it was observed that in Europe during the Third Pandemic, in the ports where infested rats were found, their number represented a minimal percentage of the rats examined, as if to indicate that they had disembarked from ships shortly before being inspected [2].
Therefore, the evolution of epidemic events in Europe does not appear to be in strong connection whit the death of rats, but rather with a chain of transmission from human to human, by contact, respiration droplets (in the case of pneumonic plague) or spread by other ectoparasites than the rat flea [17, 19]. From the beginning of the last century, rats and their flea Xenopsylla cheopis had been observed to be involved in the transmission of the disease, but other studies suggested that the bacterium can also be carried by other ectoparasites like Pediculus humanus corporis, Ctenocephalides canis and C. felix, while Pulex irritans, the flea infesting humans, seems not to be a good vector of the pathogen [20–23]. Infected rats and their fleas often spread plague over long distances, especially on trading ships, but plague may also have been spread by human ectoparasites, once the epidemic event started [24].
The hygienic conditions of Europe between the end of the nineteenth century and the mid-twentieth century were not such as good to avoid the spread of these ectoparasites which could also infest clothes and baggage and transmit the disease from person to person [2].
Prevention measures
The most plausible hypothesis is that in the twentieth century, plague arrived in Europe mostly through the maritime trade routes, but, the sanitary measures applied, such as improved hygiene and quarantine, played a fundamental role in containing the circulation of disease in Europe, rather than the rodent control [1, 2, 25].
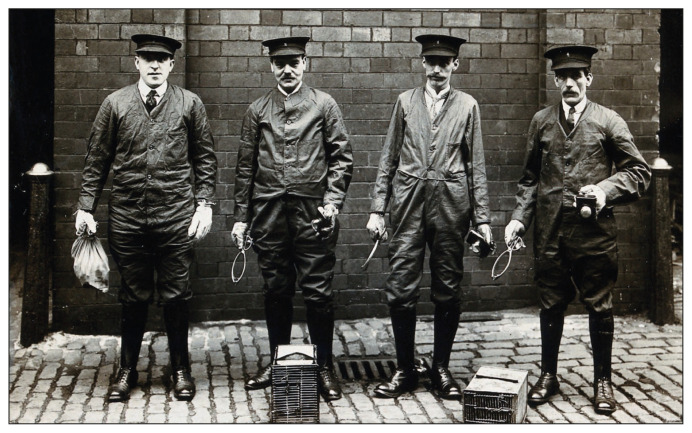
Figure 1.
Liverpool Port Sanitary Authority rat-catchers dressed in protective clothing with traps and equipment, Liverpool, England. Photograph, 1900/1920. (Credit: Wellcome Collection. Public Domain Mark).
As reported by Proust, preventive measures were included, among other actions, the international monitoring of epidemic sites, the control of suspected ships from landing at ports; medical examinations at the time of boarding from an epidemic location; isolation of the infected from healthy people and destruction by fire of their personal objects ([15]; summarized in [1]). On the other hand, reports on rodent control of ships and ports have only become mandatory since 1926 [1].
The control of rats and their fleas involved the use of poisoned baits, but at least for the first 40 years of the twentieth century, there were no effective rodenticides and pesticides, especially in the poorest countries. According to what we reported earlier in the text, the extermination of infected rats may also have induced an opposite effect, that is, the uncontrolled release of their parasites into the environment, which can transmit the disease even after many days. The real turning point may have been the use of insecticides like D.D.T.7, which was introduced during WWII [4].
Furthermore, the improvement of personal hygienic conditions thanks to the introduction in the 1950s of private bathrooms, vacuum cleaners and washing machines could have greatly contributed to the reduction of parasites in the domestic area [2].
In the twentieth century were also adopted the first medical treatments based on the use of antibiotics such as streptomycin, which was administered for the first time in 1945, and vaccines as will be discussed in the following paragraphs [4].
The Plague of Taranto
In Europe, the last known epidemic event was recorded in 1945 in the port city of Taranto, partially still under the control of the Allies, at the end of WWII. This epidemic event was not reported in Public Health Reports due to the post-war situation and the “interregnum” state of the military naval Arsenal between the occupation of the 52 Army Area and the Italian authorities [2]. According to Marisan8 medical Colonel Umberto Monteduro the source of the infection was a ship that transported a cargo of rags, likely from Malta [26, 27].
According to the medical officer dr. Alfonso Leone, who worked on the front line, at the end of the hot summer of 1945 some dead rats were discovered in the Naval Arsenal of Taranto, and at the beginning of September six workers got ill and two died. It was reported that they had similar symptoms and four of them presented the inguinal lymph nodes inflamed [26, 27]. The medical Admiral Giuseppe Barbagallo was immediately suspicious about the situation; biological samples from the buboes were collected and analyzed at the Bacteriological Laboratory of Marisan [27]. The bacteriological analysis found the bacterium of plague. The first case was notified on the 6th of September 1945, and at the end of September, the contagion reached its peak. Military employers and civil authorities immediately applied sanitary measures to control the propagation of the disease. At first, two hospitals had been created, for the isolation and hospitalization of infected people, one civil, and the other military [26]. The civil one was ruled by doctor Arturo Gentile. His contemporaneous records described the anti-contagious measures and the treatments involved that ensured a successful defeat of the disease in only 3 months [28].
Individuals affected by plague, their families and close contacts were isolated in their houses. All the public stores in the city and the churches were closed. Chlorine gas was employed to disinfect the Arsenal’s sewers. The new insecticide D.D.T. was sprayed in the buildings of the Arsenal, docks, and the houses of infected people. The waste was burned and personal hygiene was improved.
An anti-rodent campaign, that killed almost 5.000 rats, led by the British doctor Barnett, was carried out with more than 2000 poison baits placed in the Arsenal area and all over the town. The poisons employed were zinc phosphide (5% Zn3P2) and arsenious oxide (As2O3) [27]. Of the poisoned rats found in the docks, 60% belonged to the R. novergicus species, and the remaining 40% to the R. rattus species, while the rats in the city belonged only to the R. rattus species [29].
On the occasion of this epidemic event, new pharmacological drugs and treatments were employed. All people admitted to the Hospital were treated with an intramuscular injection of Antiserum of the Pasteur Institute, 60–80 cc every 24 hours for 5 up to 7 days, combined with adrenaline and calcium chloride due to its severe side effects [28]. Antimicrobial therapy was also administrated based on penicillin and sulfonamides such as sulfathiazole 3–4 g every 24 hours orally and intravenously for 6 up to 8 days [28]. Nowadays, the therapeutic use of sulfathiazole, which belongs to the class of thiazole sulfonamides with systemic action, has been in general almost abandoned [30]. The pharmacological treatment therapy also included the administration of cardiokinetics such as caffeine, camphor, digitalis and adrenaline, and in case of arterial hypotension, a hypodermoclysis with a physiological solution was administrated. In some cases, the surgical incision of the buboes was helpful for the healing of the tissues [28].
Figure 2.
The witnesses of the Taranto outbreak in 2002. From left to right: Dr Alfonso Leone, Dr Alberto Carducci, Dr Giuseppe Barbagallo. Credit: Giovangualberto Carducci.
Table 1.
Reports of 29 cases of plague in Taranto, from Schulz 1950[29].
| Number of cases | Subjects | Inoculation of vaccine | Outcome |
|---|---|---|---|
| 1–12 | Workers of the parcel office | No | 5 deaths |
| 13 | Worker of the Arsenal | No | Dead |
| 14 | Worker of the Arsenal | Yes | Dead |
| 15 | Worker of the parcel office | Yes | Dead |
| 16 | Carpenter | No | Dead |
| 17 | Stoker | Yes | Recovered |
| 18 | Worker of the Arsenal | Yes | Dead |
| 19 | Stoker | No | Recovered |
| 20 | Worker of the Arsenal | Yes | Dead |
| 21 | Worker of the Arsenal | No | Recovered |
| 22 | Worker of the Arsenal | Yes | Recovered |
| 23 | Worker of the Arsenal | No | Recovered |
| 24 | Civilian | No | Dead |
| 25 | Workman | No | Dead |
| 26 | Sailor | Yes | Dead |
| 27 | Giovanna, Nun working at the military hospital | No | Recovered |
| 28 | Goatherder | No | Dead |
| 29 | Girl of 12 years of age, an officer of Regia Marina’s daughter | No | Recovered |
Many people were inoculated with two injections of a vaccine, made from killed bacilli, prepared by the Italian Istituto Superiore di Sanità, and with a vaccine provided by the Allies [31]. This prophylactic vaccination was first extended to the workers of the Arsenal, then to the families of the officers and non-commissioned officers who lived in the buildings of Maridepo9 and finally to the cohabitants of the sicks. The second injection was administrated to those who had no serious adverse effects to the first one [26].
The last case was notified on the 29th of November 1945. At the end of the outbreak, 15 deadly cases (including a first victim not notified by the Allies) out of 30 cases of bubonic plague among civilian and military personnel were notified [26, 32]. No case of pneumonic plague was recorded. The case fatality rate was 51,7%10 [29], or 50%, when we consider the first case. Of the total cases notified, 7 patients (corresponding to about 23 %) had been inoculated with the vaccine. Of them, 71% died, and only 29% recovered.
According to the clinical reports of Dr Arturo Gentile, two patients hospitalized in the civil Lazzaretto, who received vaccine prophylaxis had different responses to the disease: one was vaccinated 5 days before the onset of the disease, most likely when he was in its incubation phase, a condition that may have exposed his immune system to a greater effort leading to his death. The other patient, on the other hand, was vaccinated 12 days before the onset of symptoms; this timing allowed him to develop immunity and recover well when he was infected with the disease. Gentile, however, does not fail to be surprised by the death of a person who was vaccinated 38 days before the onset of the disease [28].
Thanks to the efforts of the medical officers of the Italian Navy, Italian authorities and British military, the Taranto epidemic was defeated in 83 days, and plague disappeared from Europe.
Thanks to the memory, records and documents of the doctors involved and to the commitment of Alberto and Giovangualberto Carducci in reconstructing the events of the time, these facts were not forgotten and future generations will be able to remember how the plague in Taranto “had covered everything”, but fortunately only for 3 months [33].
Plague during the antimicrobial age
Antibiotics
Antimicrobial drugs represent one of the greatest achievements of modern medicine. The introduction on the pharmaceutical market in the 1940s of penicillin, the first antibiotic discovered by Ian Fleming in 1928, opened the so-called “antibiotic era”. The discovery of streptomycin dates back to 1944 and of chloramphenicol to 1947, while sulfonamides have been employed against plague already in the 1930s [30, 16].
During the last years of WWII, mass production of penicillin started in support of the Allied forces to save the lives of wounded soldiers in Europe. Penicillin was available to the general public and employed in the treatment of infectious diseases first in Australia, on March 1945 in the USA, and in the UK in June 1946 [34]. Streptomycin mainly used as a treatment of tuberculosis, provided effectiveness if administered within 48 hours of the appearance of the first symptoms of bubonic plague [4, 30]. With the use of antibiotics, mortality from plague in the US dropped from 66% to 11% [5]. During the Taranto’s plague, antimicrobials such as penicillin and sulfathiazole have been used against the bubonic form of the infectious disease [27].
Today plague is not nearly as deadly as it once was thanks to antibiotics, but, due to the lack of an effective vaccine, it still represents a threat. Potentially, plague could be employed as a bacteriology weapon and constitute a concern for world public health. The World Health Organization and the Centers for Disease Control and Prevention recommend for those affected appropriate treatments with antimicrobial drugs, which include:
– Ciprofloxacin: antibiotic drug belonging to the class of Fluoroquinolones, administrated orally in adults 750 mg every 12 hours, in children 15 mg/kg every 8–12 hours [35].
– Levofloxacin: antibiotic drug belonging to the class of Fluoroquinolones, administrated orally or intravenously in adults 750 mg every 24 hours, in children 8 mg/kg every 12 hours; a new antibiotic Levaquin containing 250 mg of levofloxacin has been approved on April 27 th 2012, for the treatment of patients with the disease (AIFA) [35].
– Moxifloxacin: antibiotic drug belonging to the class of Fluoroquinolones, administered orally or intravenously in adults, 400 mg every 24 hours, not recommended for children [35].
– Gentamicin: antibiotic drug belonging to the class of Aminoglycosides, administered intravenously or intramuscularly in adults, 5 mg/kg every 24 hours, children 4.5–7.5 mg/kg every 24 hours [35].
– Streptomycin: antibiotic drug belonging to the class of Aminoglycosides is one of the most effective antibiotics, used for decades to treat plague, given intravenously or intramuscularly, 1g every 12 hours in adults and 15 mg/Kg every 12 hours in children [35].
– Cloramphenicol: broad-spectrum antibiotic drug, injected intravenously in adults 25 mg/Kg. Also used in the form of meningitic plague because it can cross the blood-brain barrier [3].
The duration of treatment is 10 to 14 days and must be administrated as soon as plague infection is suspected, according to the Center for Disease Control and Prevention [16].
While prophylaxis against infection recommended the use of the tetracycline Doxycycline 100 mg orally every 12 hours for 7 days [5].
The risk of multi-drug resistance is very common: from 1995 to 2021 seven Y. pestis strains presented antibiotic resistance due to gene point mutations and groups of transferable resistance plasmids from other bacterial species [36]. For these reasons in recent years, new potential antibiotics and drugs against virulence factors are under development [37].
Serum
More than a century ago, the Yersin Antiserum was developed to treat the infection by Yersin himself in 1895. This first serum against plague was obtained by immunizing animals, usually horses. Due to its severe side effects, its use was gradually abandoned [16].
Today, we find Antiserum in two homoeopathic preparations used against Influenza viruses, Homeos 42 and Serum de’ Yersin.
– Homeos 42: Homeopathic pharmaceutical formulation of Cemon company, dispensed in six tubes, each one containing 1 g of globules for the preventive and curative treatment of flulike symptoms and their possible complications. Obtained from a homoeopathic dilution of remedies chosen by the principle of similars established by Samuel Hahnnemann which include Aviaire, Influenzinum, Serum de’ Yersin and biotherapeutic11 bacterial lysates as Streptococcinum, Staphylococcinum, and Klebsiella pneumoniae. To treat influenza one dose should be given within the onset of the first symptoms. For prophylaxis, it is recommended one dose per week from the autumn months to March. Children should receive a half-size dose [38].
– Serum de’ Yersin: Homeopathic pharmaceutical formulation of the Boiron company, in oral pellets also known as granules (multidose tube, containing approximately 80 pellets) and globules (unit dose tube, containing approximately 200 pellets) available in different dilutions. It is used to prevent and treat influenza conditions with symptoms of hyperthermia, gastric and pulmonary involvement, meningeal and encephalitic lethargic syndromes, as well as toxic states of infection [38].
Vaccines
Vaccines against plague are difficult to develop. In fact, immunizing preparations were proven to confer only short-term protection after injection. Currently, we still lack effective and safe vaccines against plague authorized by WHO and CDC [6, 16].
Whole cell-based vaccines:
Vaccines obtained from bacteria inactivated by heat or by chemical compounds (KCW12) and live attenuated (LWC13) had been used mainly in the 19th and 20th centuries to contrast plague [39].
– Haffkine: (KCW) tested during the outbreak in Mombay 1897, it was obtained from a broth culture of bacteria killed by heating at 60 °C. The vaccine was associated with severe adverse effects and was unable to provide complete protection, although it seems to have reduced the risk of infection by 50% [4].
– USP: (KCW) preparation of formaldehyde-killed bacteria, initially produced by the Cutter Biological Laboratories. Effectively tested on mouse models, it was used in the USA and during the Vietnam War, but provided little protection against pneumonic plague [3, 40].
– EV76: Live attenuated vaccine (LCW), based on the EV76 strain, developed in the 1930s and tested in Madagascar, forced the hospitalization of most vaccinated people due to its multiple adverse effects [4].
Subunit vaccines:
In recent years there are several molecular and recombinant based-vaccine under development. These vaccines contain portions of the pathogen (mainly the virulence factor F1 and the V antigen), against which immunization might be obtained, therefore they are new possible candidates to be tested.
– rF1-LcrV: This is a molecular vaccine that has not yet been tested on humans, but has completed phases I and II of clinical trials. The vaccine is composed of a recombinant genetic fusion of F1 and LcrV antigens. The vaccine involves the administration of two doses that guaranteed total protection against bubonic and pulmonary plague in a mouse model [6, 41].
– V10: Patented by the University of Chicago. Efficient on the mouse model and macaques, but has not yet started clinical trials. It is composed of a portion of the V antigen [6, 42].
– RypVax: molecular vaccine manufactured by PharmAthene Inc. containing the separate recombinant antigens F1 and V produced in Escherichia coli [43].
– VTnF1: Based on the F1 pseudocapsule component produced by a genetically attenuated strain of Y. pseudotuberculosis. Oral administration in mice ensured protection against both bubonic and pulmonary plague. It appears to be a promising candidate [6, 44].
– ChAdOx1 Plague: In 2021, the Oxford Vaccine Group investigated a recombinant adenovirus-based vaccine against plague (PlaVac) based on the same technology used in the COVID-19 AstraZeneca vaccine VaxZevria ChAdOx1 - S. ChAdOx1 Plague is obtained from a genetically modified cold adenovirus common in chimpanzees. The genes that encode proteins of the plague bacterium, the F1 and V antigens, have been inserted into the viral vector. The production of these antigens in the host will prepare an immune response. Useful to fight antigens and infection in case of exposure. As it does not contain the bacterium, this vaccine cannot cause the disease. The vaccination is given intramuscularly. In 2021 the Oxford Vaccine Group launched phase I trials for this vaccine in healthy volunteers from 18 to 55 years of age, who has been monitored for 12 months [45].
CONCLUSIONS
Nowadays, plague still represents a serious threat to the world’s public health and surveillance is always required. In several continents, including Africa, Asia and the Americas, plague still exists in wild rodent reservoirs and their fleas and occasionally causes local cases and epidemics [17].
In Africa, plague is considered a re-emerging pathology [46] and frequent intercontinental exchanges in the globalization era can quickly repropose its presence in Europe as well. If rapidly diagnosed, plague today is treatable with antibiotic therapy, but drug-resistant lines are already known. Finally, although biomedical research has recently (in response to COVID-19) implemented new techniques for obtaining vaccines, there is still no authorized vaccine against plague in the Western world. For the moment, only the constant monitoring of places where reservoirs are located (Asia, Africa, Americas) avoids the spread of new epidemics that could reach enormous dimensions, as happened in the past in Europe and other parts of the World.
Acknowledgements
The authors would like to thank Chiara B. Vicentini of the University of Ferrara, for her support during the historical research. We are also indebted to Giovangualberto Carducci and his family for the historical information, photographs and memory about the last plague in Taranto.
Footnotes
Late Neolithic-Bronze Age
ymt
pla
Fraction 1.
Type III secretion system.
Yersinia outer proteins.
Dichloro-diphenyl-trichloroethane.
Directorate of Navy Health.
Navy’s buildings.
Calculated on 29 cases, the English soldier is not included.
Obtained by microbial coltures [47].
Killed Whole Cell.
Live Whole Cell.
Conflict of interest: None.
Funding: None.
REFERENCES
- 1.Stenseth NC, Tao Y, Zhang C, et al. No evidence for persistent natural plague reservoirs in historical and modern Europe. Proc Natl Acad Sci USA. 2022;119(51):e2209816119. doi: 10.1073/pnas.2209816119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bramanti B, Dean KR, Walløe L, Stenseth NC. The Third Plague Pandemic in Europe. Proc R Soc B. 2019;1901;286 doi: 10.1098/rspb.2018.2429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williamson ED, Oyston PCF. Plague Vaccines Plotkin’s Vaccines. 2018;(e4):762–772. [Google Scholar]
- 4.Echenberg M. Pestis redux: The initial years of the third bubonic plague pandemic, 1894–1901. J World Hist. 2002;13(2):429–449. doi: 10.1353/jwh.2002.0033. [DOI] [PubMed] [Google Scholar]
- 5.Bush LM, Vazquez-Pertejo MT. Plague and Other Yersinia Infections. [Internet] MSD Manual Professional Version. 2020. [cited 2023 Apr 2]. Available from: https://www.msdmanuals.com/professional/infectious-diseases/gram-negative-bacilli/plague-and-other-yersinia-infections.
- 6.Demeure CE, Dussurget O, Mas Fiol G, Le Guern AS, Savin C, Pizarro-Cerdá J. Yersinia pestis and plague: an updated view on evolution, virulence determinants, immune subversion, vaccination, and diagnostics. Genes and Immunity. Nature Publishing Group. 2019;20:357–370. doi: 10.1038/s41435-019-0065-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yersin A. La peste bubonique a Hong-Kong. Ann Inst Pasteur. 1894;8:662–667. [Google Scholar]
- 8.Rasmussen S, Allentoft M, Nielsen K, et al. Early divergent strains of Yersinia pestis in Eurasia 5,000 years ago. Cell. 2015;163(3):571–582. doi: 10.1016/j.cell.2015.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rascovan N, Sjögren KG, Kristiansen K, et al. Emergence and Spread of Basal Lineages of Yersinia pestis during the Neolithic Decline. Cell. 2019;176(1–2):295–305e10. doi: 10.1016/j.cell.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Spyrou MA, Tukhbatova RI, Wang CC, et al. Analysis of 3800-year-old Yersinia pestis genomes suggests Bronze Age origin for bubonic plague. Nat Commun. 2018;9:2234. doi: 10.1038/s41467-018-04550-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Achtman M, Morelli G, Zhu P, Wirth T, Diehl I, Kusecek B, et al. Microevolution and history of the plague bacillus, Yersinia pestis. Proc Natl Acad Sci USA. 2004;101(51):17837–17842. doi: 10.1073/pnas.0408026101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spyrou MA, Keller M, Tukhbatova RI, et al. Phylogeography of the second plague pandemic revealed through analysis of historical Yersinia pestis genomes. Nat Commun. 2019;10(1):1–13. doi: 10.1038/s41467-019-12154-0. 101.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mueller CA, Broz P, Müller SA, et al. The V-antigen of Yersinia forms a distinct structure at the tip of injectisome needles. Science. 2005;310(5748):674–676. doi: 10.1126/science.1118476. [DOI] [PubMed] [Google Scholar]
- 14.de Almeida Brasiel PG. The key role of zinc in elderly immunity: A possible approach in the COVID-19 crisis. Clin Nutr ESPEN. 2020 Aug 1;38:65–66. doi: 10.1016/j.clnesp.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Proust A. La Défense de l’Europe contre la peste et la Conférence de Venise de 1897. Paris, France: Masson; 1897. [Google Scholar]
- 16.Barbieri R, Signoli M, Chevé D, et al. Yersinia pestis: the Natural History of Plague. Clin Microbiol Rev. 2020;34(1):1–44. doi: 10.1128/CMR.00044-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bramanti B, Stenseth NC, Walløe L, Lei X. Plague: A Disease Which Changed the Path of Human Civilization. In: Yang R, Anisimov A, editors. Yersinia pestis: Retrospective and Perspective Advances in Experimental Medicine and Biology. Dordrecht: Springer; 2016. pp. 1–26. [DOI] [PubMed] [Google Scholar]
- 18.Davis DE. The scarcity of rats and the Black Death: an ecological history. J Interdiscip Hist. 1986;16(3):455–470. [Google Scholar]
- 19.Dean KR, Krauer F, Schmid BV. Epidemiology of a bubonic plague outbreak in Glasgow, Scotland in 1900. R Soc Open Sci. 2019;6(1):181695. doi: 10.1098/rsos.181695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shennan T, Theodore Shennan B. The Propagation of Plague. Edinb Med J. 1908;23(6):524. [Google Scholar]
- 21.Dean KR, Krauer F, Walløe L, et al. Human ectoparasites and the spread of plague in Europe during the Second Pandemic. Proc Natl Acad Sci USA. 2018;115(6):1304–1309. doi: 10.1073/pnas.1715640115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barbieri R, Drancourt M, Raoult D. The role of louse-transmitted diseases in historical plague pandemics. Lancet Infect Dis. 2021 Feb 1;21(2):e17–25. doi: 10.1016/S1473-3099(20)30487-4. [DOI] [PubMed] [Google Scholar]
- 23.Miarinjara A, Bland DM, Belthoff JR, Hinnebusch BJ. Poor vector competence of the human flea, Pulex irritans, to transmit Yersinia pestis. Parasites and Vectors. 2021;14(1):1–15. doi: 10.1186/s13071-021-04805-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dean KR, Krauer F, Schmid BV. Epidemiology of a bubonic plague outbreak in Glasgow, Scotland in 1900. R Soc Open Sci. 2019;6(1):181695. doi: 10.1098/rsos.181695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barnett SA. Rat control in a plague outbreak in Malta. Epidemiol Infect. 1948;46(1):10–18. doi: 10.1017/s0022172400036019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leone A. Taranto tra guerra e dopoguerra: il minamento della rada di Mar Grande 1943 e l’episodio epidemico di peste bubbonica 1945. Cenacolo. 2000;XII(XXIV) [Google Scholar]
- 27.Carducci Alberto. L’ultima peste in Europa: Taranto 1945. In: Distante A, Portulano-Scoditti M, editors. Atti del XLI Congresso Nazionale. Mesagne (Brindisi), Italy: Giordano Editore; 2001. pp. 163–176. [Google Scholar]
- 28.Gentile A. Rilievi clinici sull’episodio epidemico di peste a Taranto. 1946 [Google Scholar]
- 29.Schultz KH. Control of plague in Taranto, Italy, 1945–1946; an account of a successful programme of rodent extermination. Bull World Health Organ. 1950;2(4):675–685. [PMC free article] [PubMed] [Google Scholar]
- 30.Runti C. Fondamenti di chimica farmaceutica. 1970:514. [Google Scholar]
- 31.Barbalucca G. Di un episodio di peste a Taranto. Rass e Boll di Stat del Comune di Taranto. 1959 [Google Scholar]
- 32.Appeso G. Taranto, quando in città scoppiò l’ultima epidemia di peste nota in Europa. La Gazzetta del Mezzogiorno. 2022 Apr 21; [Google Scholar]
- 33.Camus A. The Plagu. 1947 [Google Scholar]
- 34.Aldridge S, Parascandola J, Sturchio JL. The discovery and development of penicillin 1928–1945 the Alexander Fleming Laboratory Museum, London, UK November 19, 1999: an International Historic Chemical Landmark. American Chemical Society; 1999. [Google Scholar]
- 35.Katzung BG, Trevor AJ, Muccioli G. Farmacologia generale e clinica. Farmacologia Generale E Clinica. Piccin Nuova Libraria spa. 2017:713–734. [Google Scholar]
- 36.Lei C, Kumar S. Yersinia pestis antibiotic resistance: a systematic review. Osong Public Heal Res Perspect. 2022;13(1):24–36. doi: 10.24171/j.phrp.2021.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sebbane F, Lemaître N. Antibiotic therapy of plague: A review. Biomolecules. 2021;11(5):724. doi: 10.3390/biom11050724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Piterá F. Valutazione dell’efficacia del complesso omeopatico Homeos 42 nella profilassi influenzale. Homeos 42 nella Profil della Sindr Influ Stud Oss. 2000:1–12. [Google Scholar]
- 39.Verma SK, Tuteja U. Plague vaccine development: current research and future trends. Front Immunol. 2016;7:602. doi: 10.3389/fimmu.2016.00602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meyer KF. Effectiveness of live or killed plague vaccines in man. Bull World Health Organ. 1970;42(5):653. [PMC free article] [PubMed] [Google Scholar]
- 41.Heath DG, Anderson GW, Mauro JM, et al. Protection against experimental bubonic and pneumonic plague by a recombinant capsular F1-V antigen fusion protein vaccine. Vaccine. 1998;16(11–12):1131–1137. doi: 10.1016/s0264-410x(98)80110-2. [DOI] [PubMed] [Google Scholar]
- 42.Cornelius CA, Quenee LE, Overheim KA, et al. Immunization with recombinant V10 protects cynomolgus macaques from lethal pneumonic plague. Infect Immun. 2008;76(12):5588–5597. doi: 10.1128/IAI.00699-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sun W, Singh AK. Plague vaccine: recent progress and prospects. npj Vaccines. 2019;4(1):11. doi: 10.1038/s41541-019-0105-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Derbise A, Hanada Y, Khalifé M, Carniel E, Demeure CE. Complete Protection against Pneumonic and Bubonic Plague after a Single Oral Vaccination. PLoS Negl Trop Dis. 2015;9(10):e0004162. doi: 10.1371/journal.pntd.0004162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Group OV. Investigating a Vaccine Against Plague (PlaVac) [Internet] 2021. Available from: https://trials.ovg.ox.ac.uk/trials/plague.
- 46.World Health Organization. Plague [Internet] 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/plague.
- 47.Boiron M, Payre-Ficot A. Homéopathie: le conseil au quotidien. France: Editions Boiron; 1996. [Google Scholar]