SUMMARY
The aim of the present study was to explore the stigma and fear of getting sick in health professionals who treat people living with HIV. An exploratory systematic review was conducted. The search was limited to the presence of stigma and fear of getting sick on the part of healthcare workers who treat people living with HIV, documented by the health workers or patients themselves. No language restriction was made and systematic reviews, comments or communications were excluded. The sources of information were Scopus, PubMed/MEDLINE, Science Direct, and the CENTRAL Registry, from the last 5 years. The quality of the evidence was assessed with an adapted tool and the synthesis of the results was carried out using a narrative synthesis approach. Twenty-three articles were included, which related structural stigma, stigma by health professionals and fear of getting sick. Among the findings, data stood out such as that more than 50% of patients reported having experienced discrimination due to HIV and even accumulated stigma for other additional causes. Stigma enacted in healthcare settings was related to suboptimal adherence to treatment (OR 1.38; 95% CI: 1.03–1.84; p=0.028). Stigma is a structural barrier in the care of people living with HIV and generates a psychological, physical, and social health impact for these people. Some limitations of the present study are that, despite searching the major databases, important manuscripts may have been left out. Additionally, there are regions that are not represented in this review because no manuscripts from those areas were found.
Keywords: Social Stigma, Prejudice, HIV, Acquired Immunodeficiency Syndrome
INTRODUCTION
The stigma of people living with HIV (PLWH) is a complex reality that many people have to deal with. Although the social stigma associated with HIV can have a significant impact on the quality of life of those who experience it, self-stigma can lead to a decrease in self-esteem and self-confidence, as well as hiding the condition of living with HIV for fear of discrimination. It is important to note that HIV does not define a person, and living with the virus should not be a cause for shame or discrimination. However, due to a lack of education and awareness about HIV, as well as the associated negative stereotypes, many people still suffer from self-stigma, feeling guilty and self-recriminating in a situation that goes far beyond their responsibility [1–4].
Regarding anticipated stigma, this refers to the prejudices and negative stereotypes that exist in society about HIV and that lead to the exclusion and marginalization of people who could be at risk of contracting it [5, 6]. It can manifest as irrational fear and an attitude of rejection towards people who are considered to carry or be at risk of acquiring HIV, such as those who are in “risk” groups such as sex workers, intravenous drug users, men who have sex with men (MSM) or LGBTQ+ people [5–8].
However, the stigma promulgated towards PLWH by health professionals is a worrying problem. Although health professionals should be a source of support and care, in some cases, they can perpetuate negative stereotypes and treat PLWH in a discriminatory manner [9, 10]. This stigma can manifest itself in various ways, for example, through attitudes of rejection, lack of empathy, or dehumanizing treatment [11]. These behaviors can make people feel ashamed, guilty, or afraid to seek appropriate medical care. Additionally, people may be discouraged from disclosing their HIV status in healthcare for fear of discrimination or judgment, and this may negatively impact their access to healthcare and appropriate patient follow-up [11, 12]. Additionally, professionals’ fear of contracting HIV is an understandable concern [11–13]. Although HIV is not transmitted through everyday contact, there is some apprehension among some healthcare workers about the possibility of exposure to the virus during their work. Importantly, standard precautionary protocols and biosafety measures are highly effective in preventing the spread of HIV and other infections in the clinical setting, in situations where the risk may be significant (for example, exposure to fluids such as blood, secretions, etc.). These protocols include using protective barriers, such as gloves, gowns, and glasses, properly handling sharp instruments, and maintaining hand hygiene [14–16]. However, the fear of contagion can persist due to a lack of information or deep-rooted stigmas. It is essential that health professionals receive adequate training on the ways of HIV transmission and prevention measures so that they can feel safe and confident in their work. Additionally, it is crucial to foster a supportive and understanding environment in the workplace so that patients and professionals feel comfortable in the interaction they engage in due to healthcare [14–16].
Then, the aim of this work was to describe the stigma and fear of getting sick in health professionals who treat PLWH. The research question was: Do health professionals who treat PLWH experience stigma and fear of getting sick?
METHODS
This systematic review was conducted to understand the stigma and fear of getting sick in the care of PLWH. The protocol for this review is registered in the Prospective Registry of Systematic Reviews (PROSPERO), registration number CRD42024512005. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed.
Eligibility criteria
The search was limited to articles addressing the presence of stigma, discrimination, negative attitudes, or fear of getting sick on the part of health professionals who treat PLWH. No language restriction was made, and studies published in several articles in sequence were counted as a single study. Since this systematic review aimed to analyze studies that use primary data, articles published as a systematic review, editorial comments, mathematical models, topic reviews, or short communications were excluded.
Information sources
Three databases were reviewed: Scopus, PubMed/MEDLINE, Science Direct, and the Cochrane Central Register of Controlled Trials (CENTRAL), from January 1, 2019 to February 1, 2024. Selected search terms were combined using boolean operators. Also, a manual reverse search was performed from the references of the articles that were included.
Search strategy
Search formula
TITLE-ABS-KEY(HIV) OR TITLE-ABS-KEY(“Human Immunodeficiency Virus”) OR TITLE-ABSKEY(“ Human Immunodeficiency Viruses”) OR TITLE-ABS-KEY(“AIDS Virus”) OR TITLE-ABSKEY(“ AIDS Viruses”) OR TITLE-ABS-KEY(“Acquired Immune Deficiency Syndrome Virus”) OR TITLE-ABS-KEY(“Acquired Immunodeficiency Syndrome Virus”) OR TITLE-ABS-KEY(“Acquired Immune Deficiency Syndrome”) OR TITLE-ABS-KEY(“ Acquired Immuno-Deficiency Syndrome”) OR TITLE-ABS-KEY(“Acquired Immuno Deficiency Syndrome”) OR TITLE-ABS-KEY(“Acquired Immuno-Deficiency Syndromes”) OR TITLE-ABS-KEY(“Acquired Immunodeficiency Syndromes”) OR TITLE-ABS-KEY(AIDS) OR TITLE-ABS-KEY(“HIV Seropositivity”) OR TITLE-ABS-KEY(“AIDS Serodiagnosis”) OR TITLE-ABS-KEY(“ HIV Seroprevalence”) OR TITLE-ABS-KEY(“ AIDS Dementia Complex”) OR TITLE-ABS-KEY(“Acquired Immunodeficiency Syndrome”) OR TITLE-ABS-KEY(“Acquired Immunodeficiency Syndromes”) AND TITLE-ABS-KEY(“ Social Stigma”) OR TITLE-ABS-KEY(“Social Stigmas”) OR TITLE-ABS-KEY(Stigma) OR TITLE-ABS-KEY(Prejudice) OR TITLE-ABS-KEY (Homophobia) OR TITLE-ABS-KEY(Microaggression) OR TITLE-ABS-KEY(Aggression) OR TITLE-ABS-KEY(Dehumanization) OR TITLE-ABSKEY (Harassment) OR TITLE-ABS-KEY(“Non-Sexual Harassment”) OR TITLE-ABS-KEY(Bullying) OR TITLE-ABS-KEY(“Psychology Rejection”) OR TITLE-ABS-KEY(“Social Discrimination”) OR TITLE-ABS-KEY(“Sexual Harassment”) OR TITLE-ABS-KEY(“Social Marginalization”).
Additionally, a filter was applied for the last five years (2019–2024), and systematic reviews, editorial notes, reviews, and clinical cases were discarded.
Selection process
Two researchers (YAP and IDLM) independently reviewed the manuscripts. The first step was to review the titles and abstracts of all references retrieved through the searches and identify the studies that met the inclusion criteria. Subsequently, articles that at least one of the researchers considered potentially eligible were selected. In the second step, the full-text manuscripts were reviewed, and the inclusion or exclusion decision was made according to the selection criteria. In case of disagreement at any step, discrepancies were resolved by discussion between the reviewers.
Data collection process
Two authors (YAP and IDLM) extracted the data using a standardized protocol and a predesigned form. The following information was extracted from each included study: author(s), year of publication, location, objectives, sample size, methodology used, exposures, results, and critical results. This compilation was done using Microsoft Excel. The author was contacted to request the information if any relevant data was not included in the article.
Data items
The primary outcomes that were sought were the presence of structural stigma, self-stigma, anticipated stigma, stigma on the part of health professionals, and health professionals’ fear of HIV infection.
Effect measures
Qualitative studies did not provide measures of effect. In observational studies, descriptive statistical measures such as mean and median with the respective standard deviation and interquartile range were provided. Some studies also reported odds ratios with the corresponding 95% confidence intervals.
Synthesis methods
All extracted information was synthesized using a narrative synthesis approach, which allows describing the results of the review in terms of themes, words, or text, grouped according to the categories established for this manuscript: structural stigma, self-stigma, anticipated stigma, stigma on the part of health professionals and fear of health professionals of contagion for HIV.
Assessment of certainty of evidence and risk of bias
Methodological quality was assessed in two ways, the first using an adapted tool, incorporating elements of the Cochrane Collaboration, Consolidated criteria for reporting qualitative research (COREQ), the Strengthening the reporting of observational studies in epidemiology (STROBE), and the Consolidated Standards of Reporting Trials (CONSORT) [17]. The tool included criteria such as eligibility criteria, adequate description of methods and results, sampling strategies, internal validity (credibility for qualitative studies), and generalizability (transferability for qualitative studies) (See Appendix 1). The second form of evaluation was the total compliance of the manuscripts with the COREQ, STROBE, and CONSORT tools. Two authors (YAP and IDLM) carried out this evaluation independently. Discrepancies were resolved by consensus. A score of at least 70% was rated as high, between 40% and 69% as moderate, and below 40% as low quality.
RESULTS
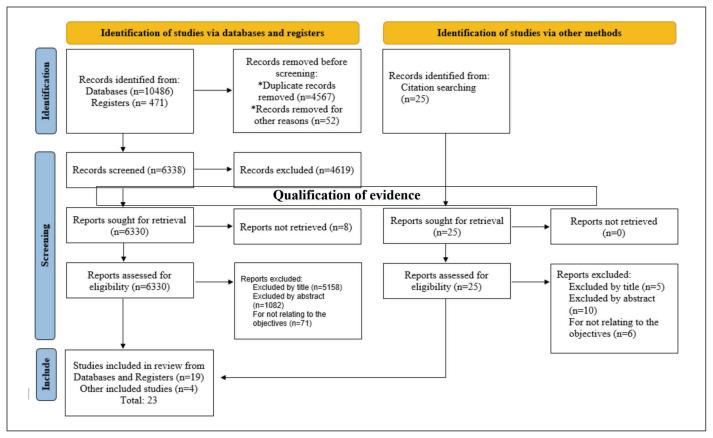
A total of 23 articles were included in the present systematic review (Figure 1).
Figure 1.
PRISMA 2020 flowchart for systematic reviews that included searches of databases, registries, and other sources.
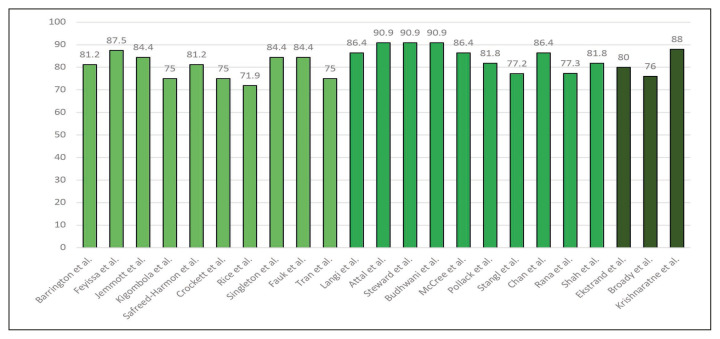
For quality assessment, the tool adapted from Nnko et al. [17] was used, and it was found that the articles had a good level of quality according to the measurement instrument (Table 1). Furthermore, with the reading tools COREQ, STROBE, and CONSORT, the suitability of the reports was verified according to their compliance with these checklists (Figure 2). The characteristics and essential data of the included studies are summarized in Table 2.
Table 1.
Quality assessment of evidence according to the adapted tool, according to the Cochrane Collaboration, COREQ, STROBE, and CONSORT criteria.
| Qualification of evidence | ||
|---|---|---|
|
| ||
| Barrington et al. [18] | Attal et al. [25] | ⊕⊕ Moderate evidence |
| Feyissa et al. [19] | Budhwani et al. [26] | |
| Jemmott et al. [20] | McCree et al. [27] | |
| Crockett et al. [21] | Stangl et al. [28] | |
| Fauk et al. [22] | Chan et al. [29] | |
| Tran et al. [23] | Ekstrand et al. [30] | |
| Langi et al. [24] | ||
|
| ||
| Kigombola et al. [31] | Krishnaratne et al. [36] | ⊕⊕⊕ High evidence |
| Safreed-Harmon et al. [32] | Rana et al. [37] | |
| Rice et al. [33] | Shah et al. [38] | |
| Singleton et al. [34] | Broady et al. [39] | |
| Steward et al. [35] | Pollack et al. [40] | |
Figure 2.
Percentage of total compliance with the COREQ, STROBE, and CONSORT tools (in that order), according to the type of study.
Table 2.
Summary of the studies included in the systematic review.
| Author(s) | Year | Location | Objectives | Sample size | Methodology | Exposures | Results |
|---|---|---|---|---|---|---|---|
| Barrington et al. [18] | 2021 | North Carolina (USA) | To evaluate the HIV testing, care, and treatment experiences of gay Latino men living with HIV. | 14 | Qualitative study with semi-structured interviews. | Internalized stigma of HIV. | Most participants had experienced disruptions in their care due to intersecting stigmatising situations, such as being gay, Latin American or undocumented, as well as structural limitations in accessing healthcare. |
| Feyissa et al. [19] | 2019 | Ethiopia | To assess contextual barriers and facilitators to the implementation of a guideline developed to reduce HIV-related stigma. | 7 | Qualitative study with semi-structured interviews. | Facilitators and barriers to HIV-related stigma and discrimination in healthcare settings. | Key informants noted a gap in the practice of addressing stigma. They also reported that HIV-related stigma had been overlooked in the past about the approach given to medical therapy. |
| Jemmott et al. [20] | 2019 | Philadelphia (USA) | To identify modifiable factors that affect the continuum of HIV care. | 27 | Qualitative study with individual interviews. | Stigma, concerns about healthcare personnel and social support. | Low participation rates in the HIV care continuum. |
| Kigombola et al. [31] | 2023 | Tanzania | To understand the factors that affect the participation in HIV health interventions. | 64 | Qualitative research with a review of documents and meetings with stakeholders. | Stigma, discrimination and the participation of influential leaders in the care of PLWH. | Self-stigma was high, resulting in low self-esteem and low health care seeking. External stigma was also high, resulting in lower utilization of health services. |
| Safreed-Harmon et al. [32] | 2022 | Spain | To obtain qualitative evidence from PLWH and HIV service providers. | Four focus groups: 2 of 15 PLWH and 2 of 16 health professionals. | Literature review and qualitative study with focus group methodology. | Social, physical, psychological and sexuality-related problems in PLWH. | Both service providers and PLWH ranked stigma/discrimination as the biggest problem they face. |
| Ekstrand et al. [30] | 2020 | India | Identifying specific attitudes and behaviours related to HIV stigma and addressing the causes. | 1625 nursing students from 28 faculties and 1557 professionals from 34 hospitals. | Clinical trial with easily adaptable interactive intervention to reduce stigma. | Two self-guided sessions were administered virtually, as well as one in-person skills-based group session. | Knowledge about correct HIV transmission was high at the beginning of the study. However, most were concerned about contracting HIV in work situations. |
| Steward et al. [35] | 2022 | India | To understand how stigma influences support for restrictive policies and discriminatory intentions. | 1540 | Cross-sectional study with the use of questionnaires. | HIV stigma reduction intervention in Indian healthcare settings. | Moral judgments and transmission fears were significantly correlated (r=0.44, p<0.010). Stigma was associated with support for coercive measures (r=0.14, p<0.010) and intentions to discriminate (r=0.15, p<0.010). |
| Crockett et al. [21] | 2021 | USA | Understand how stigma affects the care and treatment of PLWH. | 762 PLWH, and 192 health workers. | Qualitative data from 14 focus groups and quantitative survey data. | HIV-related stigmatisation and intersectional stigmatisation in the healthcare system. | PLWH were more likely to report experiences of discrimination in healthcare settings other than HIV care. Stigmatisation also encompasses other identities such as sexual orientation, gender and economic status. |
| Langi et al. [24] | 2022 | Indonesia | To describe the prevalence and behavioural indicators of stigmatisation toward PLWH. | 234 health workers (116 in the hospital setting and 118 in primary care). | Cross-sectional study with the use of a questionnaire. | Stigma and discrimination against HIV. | There was a high prevalence of health professionals (~75%) who perceived a negative image of PLWH. More than 80 reported discriminatory practises, with a higher proportion of hospital staff than primary care staff (~96% vs. ~85%; p=0.009). |
| Attal et al. [25] | 2021 | Yemen | To determine the prevalence and drivers of HIV stigma among Yemeni healthcare professionals. | 320 health professionals. | Cross-sectional study with the use of a questionnaire. | Stigma towards HIV and its drivers. | 87% stated that they would avoid physical contact and wear gloves during the consultation (96.5%). 93% felt that they had the right to disclose the patient’s HIV status. 38% incorrectly mentioned that HIV can be transmitted through tears, sweat and urine. |
| Broady et al. [39] | 2023 | Australia | To evaluate the effectiveness of an intervention in reducing stigma among healthcare workers. | 653 healthcare workers. | Randomized controlled trial. | Brief online interventions based on social norms theory. | 39.2% stated that they would behave negatively towards a PLWH and 40.4% reported that they had witnessed negative behaviour from other healthcare workers towards these individuals. |
| Krishnaratne et al. [36] | 2020 | Zambia and South Africa | To explore stigma and judgment towards PLWH by health workers. | 1557 | Clinical trial. | Stigma reinforced by the belief that this is a common situation among healthcare workers. | Healthcare workers who had the impression that their colleagues spoke badly about their HIV patients or treated them badly were more likely to have a stigmatising attitude (p<0.01). They would also prefer not to offer services to PLWH (OR=8.38, 95% CI: 3.23–21.72). |
| Budhwani et al. [26] | 2021 | USA | To test the patient-provider racial concordance on the hypothesised association between HIV-related stigma in a healthcare setting. | 931 | Cohort study. | Stigma mediated by racial discordance between healthcare provider and patient. | The interaction effects between experienced stigmatisation and racial dyads were significant (p<0.05). Experienced stigma was significantly associated with lower trust in healthcare providers. |
| Rice et al. [33] | 2019 | USA | To address anticipated stigma through a mixed methods analysis. | 460 participants of the quantitative questionnaire and 76 participants of the interviews. | Mixed methods study; qualitative interview and quantitative questionnaire. | Anticipated stigma in healthcare. | Overall, women of color, from the San Francisco and Jackson sites, and more educated respondents more frequently reported experiences and anticipation of stigma in healthcare settings. |
| McCree et al. [27] | 2023 | USA | To describe experiences of discrimination in HIV healthcare settings. | 3850 | Cross-sectional study. | Experiences of stigma and discrimination in healthcare settings. | 25% experienced discrimination, most commonly attributed to HIV status (63%), sexual orientation (60%) and race/ethnicity (54%) (p<0.05). |
| Singleton et al. [34] | 2023 | USA | To explore stereotype threat within a subgroup of the sexual minority population. | 50 | Qualitative study with analysis of semi-structured interviews. | Experiences of stigma and discrimination in gay adults living with HIV. | One participant mentioned that the healthcare provider was only interested in the treatment of HIV and not in the person. Another participant reported an interaction with his partner that he did not know about: he (the doctor) said: “Give him palliative care; he will die in a few weeks.” |
| Pollack et al. [40] | 2022 | Vietnam | To evaluate the effect of the intervention on HIV-related stigma and discrimination. | 672 health workers. 649 PLWH. | Cross-sectional study with questionnaires applied before and after the intervention. | Multifaceted facility-level intervention following key principles for stigma reduction. | Workers reported reduced stigmatisation after the intervention, including a 49% reduction in observed discrimination, an 86% reduction in fear of infection and an 87% reduction in the use of unnecessary precautions. |
| Stangl et al. [28] | 2019 | Zambia and South Africa | To develop a set of measures to capture key domains of stigma for use in research. | 4053 PLWH, 5782 community members, and 1560 health workers. | Cross-sectional study with the use of questionnaires and scales. | Stigma, fear of getting sick and negative attitudes. | Men perceived more stigmatisation (p= 0.006). Unexpectedly, people with higher education perceived more stigma in healthcare (p<0.001). |
| Chan et al. [29] | 2020 | Hong Kong | To examine how multiple forms of HIV stigma affect the psychological distress and life satisfaction. | 291 PLWH. | Cross-sectional study with the use of quantitative questionnaire. | Experiences of avoidance and/or discrimination from different sources. | 48.8% have disclosed their HIV status to medical staff. 28.9% have experienced avoidance and discrimination by healthcare workers in the last year. |
| Fauk et al. [22] | 2021 | Indonesia | To describe participants’ perceptions of the factors that drive HIV stigma and discrimination. | 52 women and 40 men living with HIV. | Qualitative study with in-depth individual interviews. | Participants’ perceptions and experiences of HIV stigma and discrimination. | Several participants described receiving negative labelling, delays in receiving services or not being seen. They also reported that healthcare professionals disseminated information about their HIV status. |
| Rana et al. [37] | 2023 | Pakistan | To investigate the presence of HIV-related stigma among dental healthcare workers. | 601 | Cross-sectional study with the use of questionnaires. | Stigma associated with HIV/AIDS in dental health professionals. | 95% (n=579) thought there was a risk of contracting HIV despite clinical precautions and 89% (n=534) of respondents were reluctant to treat HIV patients. |
| Tran et al. [23] | 2022 | Vietnam | To investigate different types of stigma (social, internalized, and professional stigma). | 12 PLWH. 5 relatives of patients. 4 clinic directors. 2 focus groups (with 10 clinical care providers). | Qualitative study with semi-structured interviews and focus groups. | Social, internalized and professional stigma. | Healthcare providers reported that some healthcare staff expressed their stigmatisation of HIV through unprofessional behaviour. These interactions were explained by healthcare staff’ lack of experience, training or fear of patients. |
| Shah et al. [38] | 2020 | Oman | To assess HIV-related knowledge, attitudes and practices. | 1281 health workers. | Cross-sectional study that used questionnaires as a data collection instrument. | Knowledge, attitudes and practices related to HIV stigma. | 50% said they would not buy fresh vegetables from a seller living with HIV. In addition, 39% believed that people speak badly about PLWH and 41% that such people lose respect in the community. 45% stated that PLWH should have the right to have children. |
Structural stigma
Structural stigma occurs in the context of some health institutions that, in some ways, limit the rights of PLWH, but also due to policies in some geographic regions that leave groups such as migrants unprotected. In addition, some PLWH recognize the presence of additional stigmatizing behaviors such as homophobia, transphobia, xenophobia, and discrimination against sex workers and intravenous drug users [18]. In one of the qualitative studies, two PLWH reported having been cumulatively stigmatized for being homosexual, Latino, and sex workers, feeling that they were denied health services, which ultimately led to poor adherence to antiretroviral therapy (ART), as they felt like laboratory animals in an experiment [18]. In another qualitative study, one of the participants said that:
“People from nearby communities go to other places to access HIV-related services. Because the HIV clinic is separate from other units of the hospital, and patients are afraid to go there. Because, if they go there, it will be evident by default that they are HIV positive” [19].
Self-stigma
Some studies have shown a high presence of self-stigma. For example, one qualitative study detailed that in the presence of sexually transmitted infections, some patients prefer not to seek healthcare services out of fear that their HIV serostatus would be disclosed [31]. A focus group study found that self-stigma was part of the dynamics when discussing these issues. Healthcare professionals drew attention to the interconnected nature of public stigma, self-stigma, and a wide range of other challenges faced by PLWH that hinder access to healthcare services [32]. Pollack et al. reported in their work that women living with HIV were more likely to report self-stigma (OR=1.85, 95% CI: 1.33–2.58) and to have experienced the disclosure of their serostatus by a healthcare professional without their consent (OR=1.60, 95% CI: 1.10–2.31) [40].
Anticipated stigma
This type of stigma occurs even before a person is diagnosed with the virus. It refers to the prejudices and negative stereotypes that exist in society about HIV and that lead to the exclusion and marginalization of people who could be at risk of contracting it. It can manifest itself in various ways, for example, through irrational fear and rejection towards people considered to be at risk of acquiring HIV. The study by Safreed-Harmon et al., which was based on focus groups, reported that anticipated stigma has important implications for many PLWH regarding social and intimate relationships [32]. Rice et al. documented in their study that, in general, women of color and those with higher levels of education more frequently reported experiences and anticipation of stigma in healthcare settings [33]. Many women expressed concerns about being recognized by other community members during health care. These concerns were prevalent among women who were new to HIV care:
“I started seeing a doctor... I had these sunglasses on when I was first diagnosed; I did not even want people to see my eyes. I was this embarrassed… I thought people would recognize me” [33].
Concerning quantitative data, the work of Rice et al., which evaluated 460 participants, showed that anticipated stigma was significantly greater than experienced stigma (t=13.67; p<0.001) [33]. Notably, anticipated stigma in healthcare settings was more significant for low-income participants (p=0.01), and both anticipated and experienced stigma were more significant for participants who were less adherent to ART (p<0.01).
Stigma on the part of healthcare professionals
One of the qualitative studies reported that in the past, the stigma perceived by patients was not given as much relevance [19]. However, key populations such as MSM, intravenous drug users, and sex workers perceived stigma and discrimination, which resulted in them not going to the hospital and resorting to self-medication to treat their underlying conditions. This same group of patients reported a double stigma associated with being a key population and living with HIV. The participants feared that their health status could reveal their sexual orientation. The negative judgment of health workers constituted an obstacle to accessing health services, as they had encountered critical attitudes and stigma from health workers during clinical visits [31]. One of the participants in a qualitative study from Tanzania commented:
“After they (the health workers) found out that I am a man who has sex with men, they called me into a room full of other health workers and started asking me why I have an immoral habit. I felt my privacy violated and stigmatized.” [31].
Another study discussed situations in which some healthcare providers negatively judged and evaluated the health of gay men. Stating that this bias influences the recommendations or tests prescribed to them:
“[…] lots of people think [that] because you’re a gay man that you’re more promiscuous...you’re jumping in and out of bed with this one and that one, which is not true. And you are constantly having unprotected sex and you do not make good decisions when it comes to choosing partners….it has an effect. And I think doctors without knowing may take that into account, they just may because of their own personal biases because everyone has biases… [34].
Another participant discussed how he felt that healthcare providers do not see PLWH and other identities as important people, highlighting the combined experience of his sexual orientation and HIV status:
“…then you add in the fact that you’re HIV positive and then that you’re gay and you’re well way back there and they don’t view you as important” [34].
This participant reflected on the fact that living with HIV, in addition to having other marginalized identities, such as being gay, negatively impacted the way the healthcare system treated him [34].
In Indonesia, 52 women and 40 men living with HIV were interviewed, and it was reported that some of these people received negative labels or cynical questions. In addition, they experienced a delay in services or were not served due to their HIV status. Likewise, they reported that health professionals spread information about their HIV status to others, showed disgust toward them, and were afraid of contracting HIV. As a result of HIV stigma and discrimination by healthcare providers, some participants felt disappointed, traumatized, and reluctant to access healthcare services in the same facilities where they experienced stigma and discrimination. Some patients decided to hide their serological status from professionals, access services in other health centers, or only consult certain professionals from whom they expect good attitudes and non-discriminatory behavior [22].
The study by Crockett et al. described that, in general, the care environments for PLWH were spaces free of prejudice; however, 51% of PLWH reported experiencing HIV-related discrimination, and 60% reported experiencing more than one experience of discrimination [21]. Stigma enacted in healthcare settings was significantly associated with suboptimal ART adherence among people with HIV (OR=1.38, 95% CI: 1.03–1.84; p=0.028).
Ekstrand et al. reported that when evaluating 1625 nursing students and 1557 professionals, negative attitudes towards PLWH had an average symbolic stigma score of 3.45 on a scale of 1 to 5 for students and 2.95 for workers [30]. Similarly, the mean levels of guilt, that is, agreement that PLWH got what they deserved, were 2.20 and 2.52 on a scale of 1 to 4 for students and workers, respectively. Another study noted that of 320 healthcare providers surveyed, 79% agreed that HIV services should be provided in separate facilities. 25% mentioned that it is best to avoid working with PLWH, while 47% agreed that healthcare workers living with HIV should stop practicing. Additionally, 36% witnessed acts of stigma by a colleague towards PLWH. The most frequently reported forms of abuse were disclosure of HIV status without consent (n=93; 82%), irrational use of infection control measures (n=73; 64%), patient avoidance and unjustified referral (n=69; 60.5%) and carelessness in providing care (n=61; 53.5%). 12% (n=14) witnessed PLWH being subjected to verbal or physical abuse [25]. Also, another manuscript reported that up to 40.4% of professionals had witnessed undignified treatment towards PLWH [39].
According to Krishnaratne et al., health workers who perceived that their coworkers spoke severely about their patients or treated them poorly were more likely to hold critical and stigmatizing attitudes (p<0.01) [36]. Also, healthcare workers who strongly agreed with the statement that their coworkers treat PLWH poorly or speak badly of them were more likely to believe that other people deserve better access to services than PLWH (OR=1.93, 95% CI: 1.15–3.26) or they would prefer not to provide services to PLWH (OR=8.38, 95% CI: 3.23–21.72), respectively. Another study that questioned 3850 PLWH identified that 25% experienced discrimination in a healthcare setting. Among them, discrimination was most frequently attributed to HIV status (63%), sexual orientation (60%), and race/ethnicity (54%) [27]. By sexual orientation, people who identified as bisexual or other (p<0.001) or gay (p=0.043) were significantly more likely to experience discrimination compared to heterosexual people. In comparison, Black MSM (p<0.001) and Hispanic/Latino MSM (p=0.006) were significantly more likely to experience discrimination in healthcare settings than Caucasian MSM [27]. Additionally, one in four transgender people was more likely to experience discrimination than the reference group (cisgender women) (p<0.001). By race/ethnicity, white people experienced the lowest prevalence of discrimination; Hispanic/Latino people (p=0.008) and people who identified as another race/ethnicity or multiracial (p<0.001) were more likely to experience more significant discrimination when they attended HIV treatment centers [27]. In another manuscript, it was reported that 44% of 672 health workers surveyed had observed discrimination by other staff members against PLWH; 54% reported negative attitudes, and 41% reported feeling uncomfortable working with colleagues living with HIV. Additionally, this study evaluated PLWH, who reported experiencing discrimination; 16% reported experiencing stigma, 14% reported that healthcare providers had revealed their HIV status without consent, and 7% reported discriminatory reproductive health counseling [40].
In the study by Stangl et al., perceived stigma in the healthcare environment was associated with both sex and education. Men (M=1.07, SD=0.75; p=0.006) perceived more stigma in healthcare environments than women [28]. Unexpectedly, those with secondary education (M=1.04, SD=0.73; p<0.001) or post-secondary education (M=1.20, SD=0.79; p<0.001) perceived more stigma in the field of healthcare than those with less than high school education. Chan et al. reported that, when questioning 291 PLWH, more than a third of the participants (36.4%) reported cases of avoidance and discrimination by health workers in emergency units, followed by outpatient clinic workers (31.0%) [29]. Especially the results of independent samples t-tests showed that PLWH who experienced stigma reported higher levels of psychological distress and lower levels of life satisfaction.
Fear of health professionals toward HIV infection
The studies indicated a latent concern on the part of health professionals regarding contracting HIV in their work activities. The study by Ekstrand et al. showed that knowledge about correct HIV transmission was high [30]. However, about two-thirds of each sample also had at least one misconception about transmission through casual contact, and most were worried about acquiring HIV in work situations. Something similar was reported in the study by Steward et al., where participants were afraid of HIV transmission (M=1.92, SD=0.79; on a subscale from 0 to 3) [35]. Additionally, higher-paid participants had a greater fear of transmission (p=0.004). Also, they were significantly more likely to support coercive policies related to mandatory disclosure of HIV status (p<0.001) and mandatory HIV testing (p=0.002).
Langi et al. found that approximately 71% of professionals they surveyed in both types of facilities (hospitals and primary care) feared contracting HIV when caring for PLWH [24]. About 64% of all primary care providers would avoid service tasks for PLWH if feasible, a situation far from that of hospital health workers (~53%) (p=0.088). Nevertheless, discriminatory practices were reported by more than 80% and were higher for hospital workers than for their primary care counterparts (~96% vs ~85%; p=0.009). A similar situation was reported by Attal et al., who observed that 87% of the 320 health workers surveyed said they would avoid physical contact with PLWH, wear gloves throughout the consultation (96.5%), use double gloves (91%) or destroy the instruments used in the provision of care (80%). 93% felt they had the right to disclose the HIV status of patients to spouses, family members (88%), and colleagues (99%) [25]. Pollack et al. were other authors who reported that 81% of the healthcare workers they surveyed reported fear of HIV infection, and 69% reported taking unnecessary precautions when caring for PLWH [40].
Other authors reported that, among healthcare workers, fear and prejudice were significantly associated with age, education, and having ever been tested for HIV. Younger (18 to 24 years old, p=0.015) and older (45 years or older, p=0.015) health workers obtained higher scores than health workers between 25 and 44 years old, reflecting that they had more negative attitudes and greater fear of contagion when treating PLWH [28].
DISCUSSION
The stigma experienced by PLWH can manifest itself in different ways, such as structural stigma that refers to public or private entities’ rules, policies, and procedures that limit people’s rights and opportunities, legitimizing power differences and reproducing inequalities and social exclusion. This approach goes beyond the conception of stigma as an individual entity and incorporates analyzing the structural aspects and social determinants contributing to exclusion processes [41–43]. A person with HIV may experience structural stigma in healthcare in several ways, one of which is with limited access to healthcare, specifically when healthcare facility procedures require individuals to disclose their HIV status prior to receiving care at a specific unit, which may discourage individuals from seeking care for fear of discrimination [44–46]. This same situation could be evidenced in the studies by Barrington et al. and Feyissa et al., who reported that patients were afraid to go to clinics where the PLHIV care units were clearly labeled as “HIV centres” and allowed the patients to be identified like HIV positive by other people only for the fact to go to these centres [18, 19].
Another form of structural stigma is cumulative stigma, where PLWH may face multiple forms of stigma and discrimination, including homophobia, transphobia, xenophobia, discrimination toward sex workers, and intravenous drug users [47–49]. This cumulative stigma can have severe consequences for the health of people with HIV, such as a lack of adherence to antiretroviral therapy. Studies such as that of Kogombola et al., Singleton et al., and Crockett et al. showed situations where PLWH were additionally discriminated against for being HIV positive and belonging to the LGBTIQ+ community [21, 31, 34].
Discrimination by healthcare personnel is part of structural stigma, but this review considered it a separate entity. This kind of discrimination may include denial of services, dehumanizing treatment, or violation of confidentiality, which is facilitated by drivers such as lack of knowledge of the pathology, its mode of transmission and treatment, as well as fear of contagion [50–54]. In the quantitative studies included in this review, it was observed that the behaviors perceived by PLWH, coming from healthcare workers, were mainly negative labels, cynical questions, delay in care, refusal of care, and dissemination of serological status without authorization [21, 22]. However, health professionals also documented negative attitudes and stigma, either because they expressed them themselves or because they identified them in colleagues. The principal ways of discrimination were the intention of not wanting to care for PLWH, the disclosure without consent of patients’ serological status, the irrational use of infection control measures, patient avoidance, verbal abuse, physical abuse, and referral were pointed out as unnecessary to other healthcare professional [27, 30, 36, 39, 40].
The fear and shame associated with seeking HIV health services may be related to structural stigma but also anticipated stigma and self-stigma. Some people prefer to travel to other places to obtain HIV-related services due to the fear of being identified as HIV-positive if they visit local clinics, as stated by one of the patients interviewed by Rice et al., who commented that she wore dark glasses during the initial consultations so as not to be recognized [33].
This review has limitations. Firstly, although the sources used are relevant, they may only account for some studies relevant to the objective of this research. The most consulted and extensive databases and resources in Health Sciences were used to compensate for this limitation. Although no exclusion criteria were applied on a geographic basis, some regions are not represented in this review because no manuscripts were found from those areas. It would be interesting to carry out future research in these locations. Another limitation is the synthesis procedure since a narrative synthesis procedure was chosen, which limits the explanatory capacity of the phenomenon studied. It would be relevant to move towards meta-synthesis procedures in future research, for which this review could serve as a data source.
CONCLUSIONS
Structural stigma limits access to health care in multiple ways, as it may require the patient to disclose their HIV status before receiving care in a specific unit, which can be intimidating for a newly diagnosed patient. Also, cumulative stigma is part of structural stigma and involves multiple additional forms of discrimination, such as homophobia, xenophobia, etc. However, one of the most severe forms of discrimination is that which occurs by health personnel, where it is possible to demonstrate behaviours such as negative labels, cynical questions, delay in care, refusal of care, and dissemination of serological status without authorisation. These situations lead to some PLHIV preferring to travel to other places to obtain health services due to fear of being labelled and suffering the negative impact of stigma, which, in general terms, can be associated with poor adherence to treatment.
The internalisation of stigmatisation can cause feelings of shame, fear, isolation and despair. These feelings can lead to people not getting tested or treated for HIV if they test positive. In addition, stigmatisation by healthcare professionals leads to people forgoing medical care and refusing treatment. Both situations, self-stigmatisation and stigmatisation by health professionals, are problems that need to be addressed to ensure access to health services with acceptable quality standards and, above all, to information about HIV/AIDS that is accurate, culturally relevant and accessible to the entire population. Also, action can be taken at an individual level, such as using anti-stigma language and learning to talk about HIV without stigmatising it. Small positive changes can have a significant impact when it comes to ending the stigmatisation of HIV and working to stop it. This will undoubtedly achieve the goals set by the World Health Organisation to tackle the HIV epidemic. In the future, more research should be conducted that looks at quantitative and qualitative data, as this review has shown that a qualitative approach can provide valuable information on aspects related to HIV stigmatisation. Any research effort to improve the quality of life of PLWH is worth the effort.
Supplementary Information
Footnotes
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
REFERENCES
- 1.Ferris-France N, Byrne E, Nyamwanza O, et al. Wakakosha “You are Worth it”: reported impact of a community-based, peer-led HIV self-stigma intervention to improve self-worth and wellbeing among young people living with HIV in Zimbabwe. Front Public Health. 2023;11:1235150. doi: 10.3389/fpubh.2023.1235150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Y, Xiao X, Zhou Y, et al. The mediating role of executive function in the relationship between self-stigma and self-injury or suicidal ideation among men who have sex with men living with HIV. Front Public Health. 2022;10:1066781. doi: 10.3389/fpubh.2022.1066781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruiz-Robledillo N, Clement-Carbonell V, Ferrer-Cascales R, et al. Cognitive functioning and its relationship with self-stigma in men with HIV who have sex with men: the mediating role of health-related quality of life. Psychol Res Behav Manag. 2021;14:2103–2114. doi: 10.2147/PRBM.S332494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rich C, Mavhu W, France NF, et al. Exploring the beliefs, experiences and impacts of HIV-related self-stigma amongst adolescents and young adults living with HIV in Harare, Zimbabwe: A qualitative study. PloS One. 2022;17(5):e0268498. doi: 10.1371/journal.pone.0268498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeng C, Li X, Qiao S, et al. Anticipated stigma and medication adherence among people living with HIV: the mechanistic roles of medication support and ART self-efficacy. AIDS Care. 2020;32(8):1014–1022. doi: 10.1080/09540121.2020.1728213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amarante I, Lippman SA, Sevelius JM, et al. Anticipated stigma and social barriers to communication between transgender women newly diagnosed with hiv and health care providers: a mediation analysis. LGBT Health. 2024;11(3):229–238. doi: 10.1089/lgbt.2023.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tan RK, Kaur N, Kumar PA, et al. Clinics as spaces of costly disclosure: HIV/STI testing and anticipated stigma among gay, bisexual and queer men. Cult Health Sex. 2020;22(3):307–320. doi: 10.1080/13691058.2019.1596313. [DOI] [PubMed] [Google Scholar]
- 8.Knettel BA, Wanda L, Amiri I, et al. Assessing the influence of community health worker support on early antiretroviral therapy adherence, anticipated stigma, and mental health among people living with HIV in Tanzania. AIDS Patient Care STDS. 2021;35(8):308–317. doi: 10.1089/apc.2021.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gázquez-López M, García-García I, González-García A, et al. Validation of the attitudes towards people living with HIV/AIDS scale in nursing students. BMC Nurs. 2023;22(1):245. doi: 10.1186/s12912-023-01414-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aziz M, Abdelrheem S, Mohammed H. Stigma and discrimination against people living with HIV by health care providers in Egypt. BMC Health Serv Res. 2023;23(1):663. doi: 10.1186/s12913-023-09676-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Srithanaviboonchai K, Khemngern P, Chuayen J, et al. Increased work experience associated with less stigmatizing attitudes towards people living with HIV among Thai healthcare personnel. Int J Environ Res Public Health. 2021;18(18):9830. doi: 10.3390/ijerph18189830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rose JS, Laux JM, Fox CM, et al. Development and validation of the mental health professionals’ attitude towards people living with HIV/AIDS scale (MHP-PL-HIV-AS) AIDS Care. 2020;32(S1):10–18. doi: 10.1080/09540121.2020.1822503. [DOI] [PubMed] [Google Scholar]
- 13.Bonacaro A, Stroumpouki T, Triglia C, et al. Nursing students’ attitudes on caring for people living with HIV/AIDS. A European Multicentre Study. Acta Biomed. 2022;93(S2):e2022191. doi: 10.23750/abm.v93iS2.12999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Souza R, Laurentino RV, Fernandes SA, et al. Digital assessment of the knowledge, attitudes and preparedness of dentists towards providing dental treatment to people living with HIV in northern Brazil. Int J Environ Res Public Health. 2023;20(19):6847. doi: 10.3390/ijerph20196847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Warner S, Cheung D, Condon A, et al. Communication and coordination of care for people living with HIV: a qualitative study of the patient perspective. BMC Prim Care. 2024;25(1):19. doi: 10.1186/s12875-023-02243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Earnshaw VA, Cox J, Wong PL, et al. “I want the doctors to know that I am as bright as a candle” Experiences with and hopes for doctor interactions among malaysian key populations and people living with HIV. AIDS Behav. 2023;27(7):2103–2112. doi: 10.1007/s10461-022-03942-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nnko S, Kuringe E, Nyato D, et al. Determinants of access to HIV testing and counselling services among female sex workers in sub-Saharan Africa: a systematic review. BMC Public Health. 2019;19(1):15. doi: 10.1186/s12889-018-6362-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barrington C, Davis DA, Villa-Torres L, et al. Intersectionalities and the HIV continuum of care among gay Latino men living with HIV in North Carolina. Ethn Health. 2021;26(7):1098–1113. doi: 10.1080/13557858.2019.1620177. [DOI] [PubMed] [Google Scholar]
- 19.Feyissa GT, Woldie M, Munn Z, et al. Exploration of facilitators and barriers to the implementation of a guideline to reduce HIV-related stigma and discrimination in the Ethiopian healthcare settings: A descriptive qualitative study. PLoS ONE. 2019;14(5):e0216887. doi: 10.1371/journal.pone.0216887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jemmott JB, Zhang J, Croom M, et al. Barriers and facilitators to engaging african american men who have sex with men in the HIV care continuum: A theory-based qualitative study. J Assoc Nurses AIDS Care. 2019;30(3):352–361. doi: 10.1097/JNC.0000000000000087. [DOI] [PubMed] [Google Scholar]
- 21.Crockett KB, Turan B, Whitfield S, et al. Patient and provider perspectives on HIV stigma in healthcare settings in underserved areas of the US South: A mixed methods study. AIDS Behav. 2022;26(1):112–124. doi: 10.1007/s10461-021-03470-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fauk NK, Hawke K, Mwanri L, et al. Stigma and discrimination towards people living with HIV in the context of families, communities, and healthcare settings: a qualitative study in Indonesia. Int J Environ Res Public Health. 2021;18(10):5424. doi: 10.3390/ijerph18105424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tran HV, Filipowicz TR, Landrum KR, et al. Stigma experienced by people living with HIV who are on methadone maintenance treatment and have symptoms of common mental disorders in Hanoi, Vietnam: a qualitative study. AIDS Res Ther. 2022;19(1):63. doi: 10.1186/s12981-022-00491-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Langi GG, Rahadi A, Praptoraharjo I, et al. HIV-related stigma and discrimination among health care workers during early program decentralization in rural district Gunungkidul, Indonesia: a cross-sectional study. BMC Health Serv Res. 2022;22(1):356. doi: 10.1186/s12913-022-07751-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Attal BA, Al-Rowaishan KM, Akeel AA, et al. HIV stigma in the teaching hospitals in Sana’a, Yemen: a conflict and low-resource setting. BMC Public Health. 2021;21(1):1793. doi: 10.1186/s12889-021-11845-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Budhwani H, Yigit I, Ofotokun I, et al. Examining the relationships between experienced and anticipated stigma in health care settings, patient–provider race concordance, and trust in providers among women living with HIV. AIDS Patient Care STDS. 2021;35(11):441–448. doi: 10.1089/apc.2021.0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCree DH, Beer L, Crim SM, et al. Intersectional discrimination in HIV healthcare settings among persons with diagnosed HIV in the United States, medical monitoring project, 2018–2019. AIDS Behav. 2023;27(11):3623–3631. doi: 10.1007/s10461-023-04076-2. [DOI] [PubMed] [Google Scholar]
- 28.Stangl AL, Lilleston P, Mathema H, et al. Development of parallel measures to assess HIV stigma and discrimination among people living with HIV, community members and health workers in the HPTN 071 (PopART) trial in Zambia and South Africa. J Int AIDS Soc. 2019;22(12):e25421. doi: 10.1002/jia2.25421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chan R, Mak W, Ma G, et al. Interpersonal and intrapersonal manifestations of HIV stigma and their impacts on psychological distress and life satisfaction among people living with HIV: Toward a dual-process model. Qual Life Res. 2021;30(1):145–156. doi: 10.1007/s11136-020-02618-y. [DOI] [PubMed] [Google Scholar]
- 30.Ekstrand ML, Raj T, Heylen E, et al. Reducing HIV stigma among healthcare providers in India using a partly tablet-administered intervention: The DriSti trial. AIDS Care. 2020;32(S2):14–22. doi: 10.1080/09540121.2020.1739221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kigombola A, Lyimo J, Mizinduko M, et al. Low engagement of key populations in HIV health services in Tanzania: analysis of community, legal and policy factors. Pan Afr Med J. 2023;45(S1):8. doi: 10.11604/pamj.supp.2023.45.1.39591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Safreed-Harmon K, Fuster-Ruiz MJ, Pastor de la Cal M, et al. Problems undermining the health-related quality of life of people living with HIV in Spain: a qualitative study to inform the development of a novel clinic screening tool. Health Qual Life Outcomes. 2022;20(1):84. doi: 10.1186/s12955-022-01978-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rice WS, Turan B, Fletcher FE, et al. A mixed methods study of anticipated and experienced stigma in health care settings among women living with HIV in the United States. AIDS Patient Care STDS. 2019;33(4):184–195. doi: 10.1089/apc.2018.0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Singleton MC, Green DC, Enguidanos SM. Identifying healthcare stereotype threat in older gay men living with HIV. J Appl Gerontol. 2023;42(9):1965–1973. doi: 10.1177/07334648231167944. [DOI] [PubMed] [Google Scholar]
- 35.Steward WT, Srinivasan K, Raj T, et al. The influence of transmission-based and moral-based HIV stigma beliefs on intentions to discriminate among ward staff in south indian health care settings. AIDS Behav. 2023;27(1):189–197. doi: 10.1007/s10461-022-03755-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krishnaratne S, Bond V, Stangl A, et al. Stigma and judgment toward people living with HIV and key population groups among three cadres of health workers in South Africa and Zambia: Analysis of data from the HPTN 071 (PopART) Trial. AIDS Patient Care STDS. 2020;34(1):38–50. doi: 10.1089/apc.2019.0131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rana BK, Sarfraz M, Reza TE, et al. A cross-sectional study to assess HIV/AIDS-related stigma and its drivers among dental healthcare providers in Islamabad, Pakistan. Cureus. 2023;15(10):e46769. doi: 10.7759/cureus.46769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shah S, Elgalib A, Al-Wahaibi A, et al. Knowledge, attitudes and practices related to HIV stigma and discrimination among healthcare workers in Oman. Sultan Qaboos Univ Med J. 2020;20(1):29–36. doi: 10.18295/squmj.2020.20.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Broady TR, Brener L, Horwitz R, et al. Reducing stigma towards people living with HIV and people who inject drugs using social norms theory: An online study with Australian health care workers. Drug Alcohol Depend. 2023;249:109953. doi: 10.1016/j.drugalcdep.2023.109953. [DOI] [PubMed] [Google Scholar]
- 40.Pollack TM, Duong HT, Nhat-Vinh DT, et al. A pretest-posttest design to assess the effectiveness of an intervention to reduce HIV-related stigma and discrimination in healthcare settings in Vietnam. J Int AIDS Soc. 2022;25(S1):e25932. doi: 10.1002/jia2.25932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jackson-Best F, Edwards N. Stigma and intersectionality: a systematic review of systematic reviews across HIV/AIDS, mental illness, and physical disability. BMC Public Health. 2018;18(1):919. doi: 10.1186/s12889-018-5861-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mora-Ríos J, Bautista N. Estigma estructural, géneroe interseccionalidad. Implicaciones en la atención a la salud mental. Salud Ment. 2014;37(4):303–312. [Google Scholar]
- 43.Reif S, Wilson E, McAllaster C, et al. The Relationship of HIV-related stigma and health care outcomes in the US deep South. AIDS Behav. 2019;23(3):242–250. doi: 10.1007/s10461-019-02595-5. [DOI] [PubMed] [Google Scholar]
- 44.Becker TD, Poku OB, Chen X, et al. The impact of China-to-US immigration on structural and cultural determinants of HIV-related stigma: implications for HIV care of Chinese immigrants. Ethn Health. 2022;27(3):509–28. doi: 10.1080/13557858.2020.1791316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Karver TS, Atkins K, Fonner VA, et al. HIV-related intersectional stigma and discrimination measurement: state of the science. Am J Public Health. 2022;112(S4):420–432. doi: 10.2105/AJPH.2021.306639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Price DM, Unger Z, Wu Y, et al. Clinic-level strategies for mitigating structural and interpersonal HIV pre-exposure prophylaxis stigma. AIDS Patient Care STDS. 2022;36(3):115–122. doi: 10.1089/apc.2021.0176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rimmler S, Golin C, Coleman J, et al. Structural barriers to HIV prevention and services: perspectives of african american women in low-income communities. Health Educ Behav. 2022;49(6):1022–1032. doi: 10.1177/10901981221109138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brown G, Reeders D, Cogle A, et al. Tackling structural stigma: a systems perspective. J Int AIDS Soc. 2022;25(S1):e25924. doi: 10.1002/jia2.25924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Logie CH, Perez-Brumer A, Mothopeng T, et al. Conceptualizing LGBT stigma and associated HIV vulnerabilities among LGBT persons in Lesotho. AIDS Behav. 2020;24(12):3462–3472. doi: 10.1007/s10461-020-02917-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nyblade L, Stockton MA, Giger K, et al. Stigma in health facilities: why it matters and how we can change it. BMC Med. 2019;17(1):25. doi: 10.1186/s12916-019-1256-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mohammadifirouzeh M, Oh KM, Tanner S. HIV stigma reduction interventions among health care providers and students in different countries: a systematic review. Curr HIV Res. 2022;20(1):20–31. doi: 10.2174/1570162X19666211206094709. [DOI] [PubMed] [Google Scholar]
- 52.Vallejos IC, Sánchez HE, Lagunas LF, et al. Knowledge, attitudes and perceptions of nurses and nursing students towards HIV/AIDS. Invest Educ Enferm. 2010;28(3):345–354. [PMC free article] [PubMed] [Google Scholar]
- 53.Schweitzer AM, Dišković A, Krongauz V, et al. Addressing HIV stigma in healthcare, community, and legislative settings in Central and Eastern Europe. AIDS Res Ther. 2023;20(1):87. doi: 10.1186/s12981-023-00585-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Arias-Colmenero T, Pérez-Morente MA, Ramos-Morcillo AJ, et al. Experiences and attitudes of people with HIV/AIDS: A systematic review of qualitative studies. Int J Environ Res Public Health. 2020;17(2):639. doi: 10.3390/ijerph17020639. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.