Abstract
Background:
Smoking is an important risk factor for various metabolic and cardiovascular disorders, and smoking cessation reduces the risk of these conditions. However, weight gain is commonly observed when individuals quit smoking, which often leads to hesitation in pursuing smoking cessation. Weight gain increases the risk of metabolic syndrome (MS). However, previous studies that investigated the relationship between smoking cessation and MS have yielded inconsistent results. Therefore, we conducted a meta-analysis to evaluate the association between smoking cessation and MS.
Methods:
Medline, Embase, Cochrane Library and CINAHL databases, were comprehensively searched from inception to April 2023, to identify relevant studies examining the relationship between smoking cessation and MS, comparing such relationship to that with active smoking. The methodological quality of the selected studies was assessed using the Newcastle–Ottawa Quality Assessment Scale. A random-effects model was used for meta-analysis.
Results:
Of 495 identified studies, 24 were reviewed. The risk of selection bias was identified in all the studies. The overall analysis of 14 studies, including data of combined results for both men and women, revealed an increased risk of MS among ex-smokers compared with that among active smokers (pooled relative risk [RR] 1.18, 95% confidence interval [CI]: 1.08–1.29). From the selected studies, 13 studies analyzing men were extracted for subgroup analysis. Among men, no significant difference in the risk of developing MS was observed between ex-smokers and smokers (pooled RR: 1.05, 95% CI: 0.95–1.17). In men, the risk of MS increased if the cessation period was ≤15 years in men (pooled RR 1.26, 95% CI: 1.01–1.56) and slightly decreased if the cessation period was > 15 years (RR 0.84, 95% CI: 0.70–1.00) in ex-smokers compared with that in current smokers.
Conclusion:
An increased risk of MS was observed in the early stages of smoking cessation compared with current smoking. As the longer duration of smoking cessation, the risk of MS becomes less significant.
Keywords: smoking cessation, weight gain, metabolic syndrome, meta-analysis
1. Introduction
Metabolic syndrome (MS) is a multifaceted concept comprising central obesity, dyslipidemia, high blood pressure, and insulin resistance, and it is also associated with the risk of type 2 diabetes mellitus (T2DM) and cardiovascular disease (CVD).[1] There are various factors that increase the risk of MS, and smoking is known to be one of them. Smoking reduces insulin sensitivity and enhances cardiovascular risk factors.[2] Several studies have demonstrated that smoking is associated with metabolic abnormalities and increases the risk of MS.[3,4] Therefore, quitting smoking is crucial for the long-term reduction of CVD risk.
However, many individuals hesitate to quit smoking because of the potential weight gain that often occurs after quitting, which often leads them to resume smoking. After quitting smoking, weight gain of approximately 4 to 5 kg per year generally occurs,[5] and glucose and lipid metabolism worsens.[6] As weight gain might be also related to some components of MS, whether weight change associated with smoking cessation counteracts the cardiometabolic benefits of smoking cessation is unclear. When considering glycemic control, the risk of new-onset diabetes continues to increase in the first few years after smoking cessation compared to never smokers.[7] However, smoking cessation did not lead to a long-term increase in glycated hemoglobin and may reduce vascular complications in diabetes owing its favorable impact on lipid profile.[8]
Previous studies on smoking cessation and MS have reported inconsistent results regarding the duration of smoking abstinence. Recently, Song et al[9] have reported that smoking cessation within 3 months is associated with an increased risk of developing MS. According to a study analyzed by Shin et al using data from the Korea National Health and Nutrition Examination Survey, the risk of MS increased among former smokers who quit smoking for ≤20 years and the increased risk for MS was no longer present for smokers who quit smoking for >20 years.[10] As such, previous studies have demonstrated that the duration of smoking cessation was very diverse, and definitions of MS and individual baseline information of the study population were different. This may have led to the inconsistent results.
This study aimed to comprehensively assess the risk for MS in ex-smokers and current smokers. By analyzing the risk, this study underscores the importance of lifestyle management and precautions at the initiation of smoking cessation and actively promotes smoking cessation.
2. Methods
2.1. Literature search
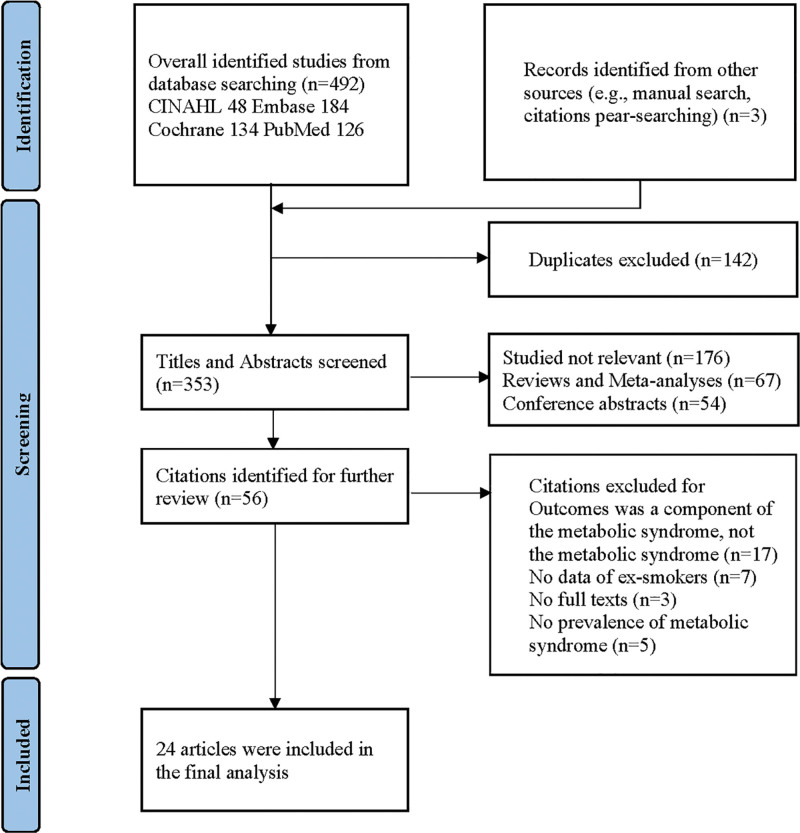
We searched for articles published up to April 30, 2023 in PubMed, Cochrane Library, EMBASE, and CINAHL databases using keywords (smoking cessation or quitting smoking), (MS or syndrome X), and other MeSH words. Only articles published in English were included in the search. A detailed search strategy using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart is shown in Figure 1. This meta-analysis followed the PRISMA[11] and Meta-analysis of Observational Studies in Epidemiology guidelines.[12] This study had been registered in PROSPERO (CRD42024533922).
Figure 1.
Flow diagram of the process for study selection.
2.2. Inclusion and exclusion criteria
Studies were included in the meta-analysis if they met the following criteria: primary observational studies including prospective or retrospective cohort studies, case-control studies, and cross-sectional studies on the relationship between smoking cessation, quitting smoking, and MS; human studies; studies involving prevalence of metabolic syndrome; and in case of overlap between studies, a study with a large number of subjects or a recently conducted study was selected.
Meanwhile, the exclusion criteria were as follows: studies involving only smoking without mention of smoking cessation; in vitro studies; studies in which only simple weight gain or components of MS were mentioned; abstracts, review articles, letters, and case reports; and studies for which the incidence or prevalence of MS was not reported.
2.3. Data extraction and study identification
Two researchers independently reviewed the articles. In case where there were discrepancies, reviewers discussed to reach the final decision. The following data were extracted: title, authors, journal name, year of publication, country, study design, study objective, diagnostic methods for MS, smoking cessation period, and sex.
2.4. Quality assessment
The quality of the selected studies was appraised using the Newcastle–Ottawa Quality Assessment Scale (NOS).[13] The NOS consists of 8 items that evaluate 3 dimensions (selection, 0–4 stars; comparability, 0–2 stars; and exposure for case-control studies or outcome for cohort studies, 0–3 stars). In this study, we presented the number of stars in each dimension for each study.
2.5. Ethical statement
Ethical approval was not necessary, because data from previously published studies in which informed consent was obtained by primary investigators were retrieved and analyzed in this study.
2.6. Statistical analyses
Risk ratios (RR) with corresponding 95% confidence intervals (CI) were calculated for the pooled data estimates. A 2-sided P value < .05 was considered statistically significant. We conducted a χ2 test of heterogeneity and calculated inconsistency index (I2) statistics.[14] A value of I2 of 0% to 25% represents insignificant heterogeneity, 26% to 50% represents low heterogeneity, 51% to 75% represents moderate heterogeneity, and >75% represents high heterogeneity. If significant heterogeneity existed among articles, a random-effects model was selected. Otherwise, a fixed effects model was used for the analysis. The presence of publication bias was evaluated using Egger test and Begg funnel plot.[15] Egger test is a regression method that uses the standardized estimate of the treatment effect as a dependent variable and its precision as an independent variable. In the Egger test, P < .05 indicates the presence of publication bias.[16] All statistical analyses were performed using Review Manager (RevMan V), which is a software provided by the Cochrane Collaboration and IBM SPSS statistics (version 29.0.1.0)
3. Results
3.1. Overview of study selection
Out of a total of 495 studies, 24 were chosen for review. From the pool of 24 studies that were reviewed, 14 studies included data of combined result for both men and women, which were incorporated into the overall analysis. Additionally, 13 studies provided data to be included in the pooled analysis of men. The details of the literature search were presented in a flow diagram (Fig. 1).
3.2. Summary of studies
The characteristics of the eligible studies are summarized in Table 1. Of the 24 articles included in the study, 13 were cross-sectional studies,[10,17–22,25,27–29,31,36] 10 were cohort studies,[3,19,23,24,26,32,33,35,37,38] 1 was a randomized controlled trial (RCT),[30] and 1 was a case-control study.[34] Regarding region, 15 studies in Asia, 4 in Europe, 3 in Middle East, and 2 in America were conducted. The diagnosis of Metabolic syndrome was based on the National Cholesterol Education Program’s Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (NCEP-ATP III)[39] criteria, and it was used in 13 of the studies. The International Diabetes Federation (IDF) criteria[40] were used in 6 studies. The Japan Society for the Study of Obesity (JASSO) criteria[41] for MS was used in 2. World Health Organization (WHO) – West Pacific Region Guidelines and American Heart Association/National Heart, Lung and Blood Institute (AHA/NHLBL) criteria were used in each study. Of the 24 studies included in the research, 13 studies focused only on men, and the remaining studies mostly included men as well. Because in men and women, there is a significant difference in the average smoking rates of the 2 groups, and the reporting rates for smoking status are different, there are limitations in examining both groups together and analyzing the results. Therefore, we divided the results into men and women and subgroup analysis was conducted in men. And detailed additional analysis was performed according to the smoking cessation period.
Table 1.
Characteristics of studies on assessing smoking cessation and risk of metabolic syndrome in meta-analysis.
| Study | Country | Design | Participants | Sample size (total no. of study participants) | Definition of metabolic syndrome | Duration | Cessation period | Mean age ± SD or median age (range) | Quality assessment (Newcastle–Ottawa scale) |
|---|---|---|---|---|---|---|---|---|---|
| Parke al[17] | South Korea | Cross-sectional study | Population based | All 8,650 Men 3,937 Women 4,713 |
NCEP-ATP III | NA | NA | M 42.9 ± 14.7 F 43.2 ± 15.7 |
9 |
| Nakanishi et al[3] | Japan | Prospective cohort study | Population based | Men 3,649 | Modified NCEP-ATP III | 7 yrs | NA | 47.3 ± 6.3 | 8 |
| Tonstad and Svendsen[18] | Norway | Cross-sectional study | Hospital based | All 1,001 Men 705 Women 296 |
NCEP-ATP III | NA | NA | M 48.7 ± 5.7 F 53.6 ± 7.7 |
7 |
| Wannametheeet al[19] | British | Cross-sectional and retrospective cohort study | Population based | Men 3,051 | NCEP-ATP III | 3 yrs | long term ≥ 15 yrs recent < 15 yrs |
40 to 59 | 7 |
| Wada et al20] | Japan | Cross-sectional study | Population based | All 22,892 Men 16,535 Women 6357 |
JASSO | NA | 0 to 5, 6 to 10, 11 to 20, >20 yrs | M 47.9 ± 10.7 F 44.6 ± 11.2 |
7 |
| Chen et al[21] | Taiwan | Cross-sectional study | Population based | Men 1,146 | Modified NCEP-ATP III | NA | 1 to 4, 4 to 12, >12 yrs | 58.5 ± 12.3 | 8 |
| Al-Daghri[22] | Saudi | Cross-sectional study | Population based | All 664 Men 305 Women 359 |
AHA/NHLBI | NA | NA | 25 to 70 | 4 |
| Hishida et al[23] | Japan | Prospective cohort study | Population based | All 5,872 Men 5,479 Women 393 |
JASSO | NA | 2 yrs | 50.4 ± 8.8 | 8 |
| Kim et al[24] | South Korea | Prospective cohort study | Population based | Men 4,542 | WHO Guidelines | 3 yrs | 3 yrs | 42 | 8 |
| Wan et al[25] | Taiwan | Cross-sectional study | Population based | All 514 Men 147 Women 367 |
Modified NCEP-ATP III and IDF* | NA | NA | M 48 ± 5 F 45 ± 4 |
6 |
| Zhu et al[26] | China | Prospective cohort study | Population based | Men 693 | Modified NCEP-ATP III and JCDCG* | 3 yrs (2.9–5.5) | 1 to 4, 5 to 12, ≥13 yrs | 55.3 | 9 |
| Calo et al[27] | Puerto rico | Cross-sectional study | Population based | All 856 Men 294 Women 562 |
NCEP-ATP III | NA | NA | 49.4 ± 15.7 | 7 |
| Kim and So[28] | South Korea | Cross-sectional study | Population based | All 3,971 Men 1,738 Women 2,233 |
Modified NCEP-ATP III | NA | NA | 71.5 ± 5.3 | 9 |
| Udo et al[29] | America | Cross-sectional study | Hospital based | All 429 Men 119 Women 310 |
NCEP-ATP III | NA | NA | 46.2 ± 11.0 | 6 |
| Heggen et al[30] | Norway | RCT | Population based | All 108 Men 29 Women 79 |
IDF | 12 wks | 12 wks | 51 | 8 |
| Saffar Soflaei[31] | Iran | Cross-sectional study | Population based | All 9,840 | IDF | NA | NA | 35 to 65 | 8 |
| Shin et al[10] | South Korea | Cross-sectional study | Population based | Men 6,032 | Modified NCEP-ATP III | NA | ≤10, 11 to ≤20, 21 to ≤30, >30 yrs | 49.3 ± 15.9 | 9 |
| Solak et al[32] | Turkey | Prospective cohort study | Hospital based | All 74 Men 46 Women 28 |
NCEP-ATP III | 12 wks | 12 wks | 41.5 ± 10 | 5 |
| Kim et al[33] | South Korea | Prospective cohort study | Population based | Men 5,809 | Modified NCEP-ATP III | 4 yrs | NA | 40 to 69 | 8 |
| Oh et al[34] | South Korea | Case-control study | Population based | All 17,656 Men 7,093 Women 10,563 |
Modified IDF | NA | NA | NA | 8 |
| Park et al[35] | South Korea | Retrospective cohort study | Population based | All 1,041 Men 997 Women 44 |
Modified IDF | 2.6 yrs | 2.6 yrs | 55.7 ± 8.3 | 8 |
| Kim et al36] | South Korea | Cross-sectional study | Population based | All 808 Men 398 Women 410 |
Modified NCEP-ATP III | NA | NA | M 32.0 ± 3.2 F 29.8 ± 3.1 |
8 |
| Park et al[37] | South Korea | Cohort study | Population based | All 6,099,717 | Modified IDF | 2 yrs | NA | 43.7 ± 13.0 | 8 |
| Suutari-Jääskö et al[38] | Finland | Cohort study | Population based | All 600 Men 281 Women 319 |
IDF | 6 yrs | 6 yrs | 50.0 ± 4.5 | 7 |
AHA/NHLBL = American Heart Association/National Heart Lung and Blood Institute criteria, F = female, IDF = International Diabetes Federation, JASSO = Japan Society for the Study of Obesity, JCDCG = Chinese Joint Committee for Developing Chinese Guidelines on Prevention and treatment of Dyslipidemia in Adults definition, M = male, NA = not applicable, NCEP-ATP III = National Cholesterol Education Program’s Adult Treatment Panel III, SD = standard deviation, WHO guidelines = World Health Organization-West Pacific Region Guidelines.
We used modified NCEP ATP III in this study.
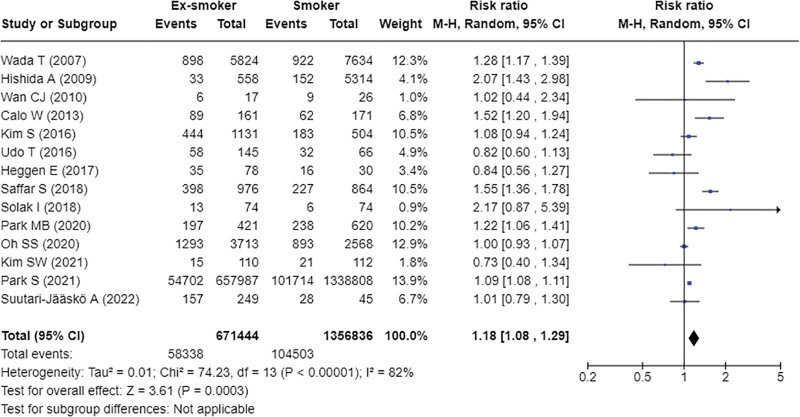
3.3. Smoking cessation and risk of MS
In the overall analysis of the 14 selected studies, including data from the combined results of both men and women, smoking cessation was associated with an increased risk of MS (Fig. 2, pooled RR = 1.18, 95% CI: 1.08–1.29). High heterogeneity was observed across studies (P < .001, I2 = 82%).
Figure 2.
Relative risks of metabolic syndrome for ex-smokers compared with smokers.
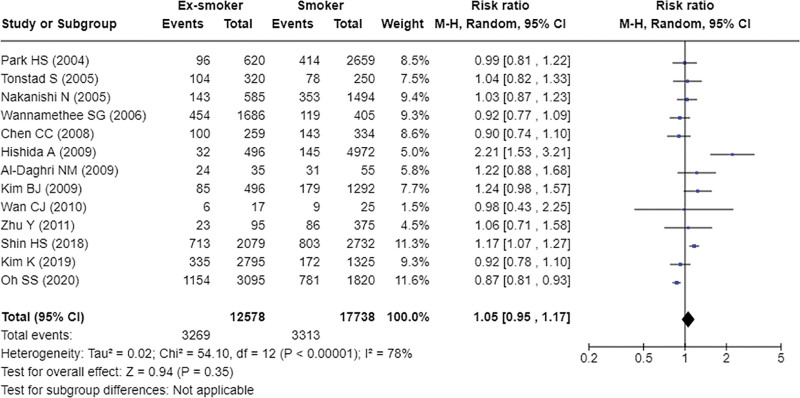
3.4. Subgroup analyses
We performed the pooled estimation for ex-smokers compared with smokers in men. Among ex-smokers compared to smokers, there was no significant evidence of an increased risk of MS in men (Fig. 3, Pooled RR = 1.05, 95% CI:0.95–1.17).
Figure 3.
Relative risks of metabolic syndrome for ex-smokers compared with smokers in men.
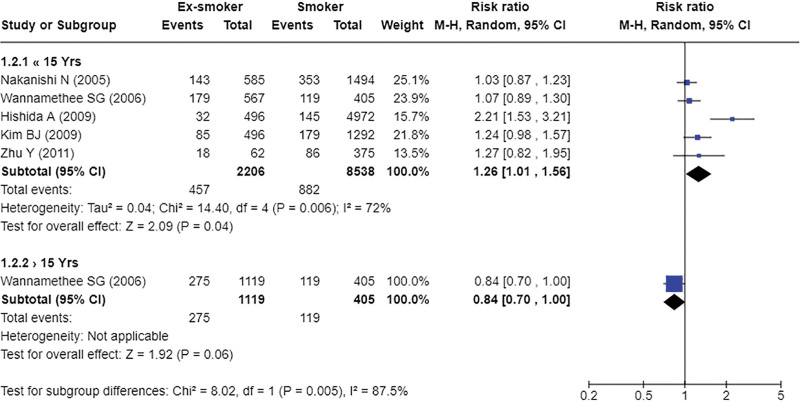
In the stratified analysis based on the duration of smoking cessation, smoking cessation was associated with an increased risk of MS among men if the cessation period was ≤15 years (Fig. 4, pooled RR = 1.26, 95% CI: 1.01–1.56). However, if the cessation period was >15 years, the risk of MS in ex-smokers showed no statistical significance compared to smokers among men (Fig. 4, RR = 0.84, 95% CI: 0.70–1.00).
Figure 4.
Relative risks of metabolic syndrome for ex-smokers with smokers according to smoking cessation period in men (short term vs. long term).
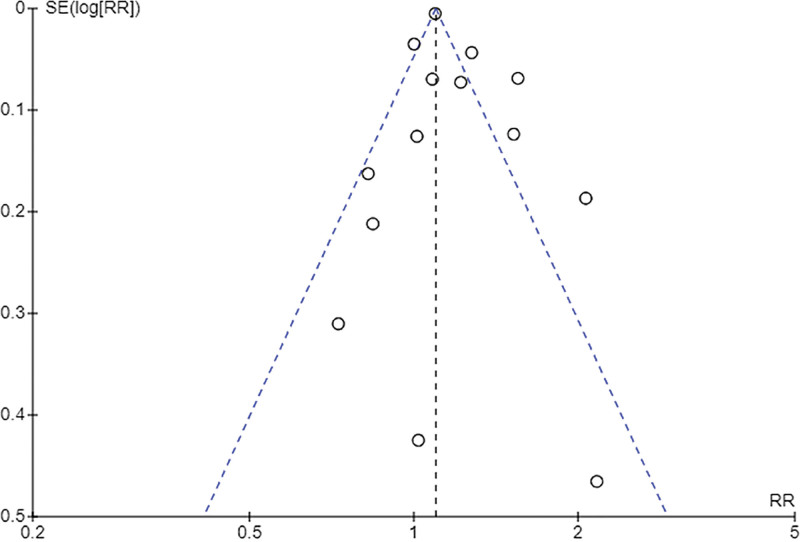
3.5. Evaluation for publication bias
Egger test was performed to assess publication bias and revealed no publication bias (t = 1.911, P = .08). In the analysis that targeted only men, no publication bias was observed (t = 0.343, P = .739). A funnel plot is presented in Figure 5.
Figure 5.
Funnel plot of the relative risks of metabolic syndrome for ex-smokers compared with smokers.
4. Discussion
This study analyzed 24 selected research papers to investigate the relationship between smoking cessation and the risk of MS. The overall findings of the combined results for both men and women suggest that smoking cessation is linked to an increased risk of MS compared to current smoking. However, upon pooled estimation of male ex-smokers compared with current smokers, no significant association between smoking cessation and MS was observed. Further analysis, considering the duration of smoking cessation, showed that men who had quit smoking for ≤15 years exhibited an increased risk of MS. Interestingly, for those with a smoking cessation period of >15 years, the risk of MS among ex-smokers was not significant compared to that among male current smokers.
Wada et al have reported that the risk of MS in ex-smokers gradually decreased over time. The risk of MS in <5 years was the highest among all investigated periods (odds ratio [OR] = 1.36). After 5 years, the OR gradually decreased in 6 to 10 years (OR = 1.28), 11 to 20 years (OR = 1.19), and in the 21 years over (OR = 1.0). Due to the given data constraints, this study categorized the timeframe based on a 15-year span. However, even in previous research, the risk of MS became statistically insignificant after >20 years of smoking cessation adjusted for past smoking amount.[10] The short-term adverse effects on metabolic parameters observed after quitting smoking may gradually improve with prolonged abstinence. The potential for long-term benefits, including reduced risk of MS, provides an encouraging message for individuals who have successfully quit smoking.
This study could not include a pooled analysis owing to the lack of sufficient data, and an association between the risk of MS and the pre-cessation smoking period among quitters was reported in previous studies. One retrospective study revealed that smoking < 20 cigarettes per day did not affect MS for any of the durations investigated. However, individuals smoking ≥ 20 cigarettes per day have demonstrated significant development in MS for over 10 years.[20]
A meta-analysis focusing on active smoking and MS risk was previously conducted. Based on data from 13 prospective cohort studies, active smokers had an increased risk of MS by approximately 26% compared to nonsmokers, especially 34% in male smokers and 19% in male ex-smokers, indicating that smokers had a higher risk of MS than ex-smokers.[42] Unlike the previous study, this study has reported that when analyzing the MS risk among ex-smokers compared to smokers, ex-smokers had an increased risk of MS in the early stages of smoking cessation. Although, no significance in men was observed, the risk increased if the cessation period was <15 years.
The increased risk of MS following smoking cessation can be attributed to several factors. First, weight gain is commonly accompanied by smoking cessation, which likely contributes to the observed association. Weight gain can lead to alterations in insulin sensitivity and lipid metabolism, both of which are key components of MS. The potential for increased weight, worsened glucose and lipid metabolism and subsequent metabolic disturbances have been reported in previous studies.[43,44] In the study conducted by Kim et al, [24] involving a cohort of 4542 men without MS at baseline, the OR for developing MS among ex-smokers was 2.09 for the stable weight group and 2.31 for the weight gain group, when compared to never smokers during the 3-year follow-up. Since only one study focused on weight change, a subgroup analysis could not be conducted in our study. According to this study, the ORs for MS were 1.90 (95% CI: 1.43–2.52) in quitters with weight gain, 0.77 (95% CI: 0.60–1.00) in quitters without weight change, and 0.40 (95% CI: 0.28–0.57) in quitters with weight loss compared with continual smokers.[33] Therefore, the increase in MS risk among ex-smokers underscores the importance of addressing weight management strategies during the smoking cessation period.
The importance of MS should be considered in relation to increased long-term CVD risk. MS is major contributing factor to the risk of CVD.[45] Many previous studies have focused on the combined impact of smoking and MS on CVD, suggesting that smoking itself may trigger MS.[46] A large-scale nationwide cohort study analyzed the CVD prognosis of people with MS status (MS-free, MS-recovery, MS-developed, and MS-chronic) according to smoking status. The risk of incident CVD was the highest for smokers, followed by ex-smokers and nonsmokers for every MS status. In ex-smokers, the risk of CVD varied according to their MS status, with the highest risk observed in the MS-chronic group, followed by the MS-developed, MS-recovery, and MS-free groups.[37] In another study analyzing data from the Framingham Heart Study, smoking cessation reduced CVD risk within 5 years compared to current smokers among heavy smokers (≥20 pack-years). However, after 5 years, the CVD risk for former smokers was significantly higher than that for never smokers.[47] Therefore, managing metabolic risk factors by quitting smoking is an appropriate lifestyle modification strategy to reduce the risk of CVD.
This meta-analysis has several limitations. First, the definition of MS was not the same for each study included in the analysis. This could introduce bias into the estimated risks associated with smoking. Depending on the race or characteristics of the study participants, the criteria were modified to better estimate the MS risks. For example, Asian studies have commonly modified waist circumference thresholds for better alignment with Asian populations. In this study, 58% of the included studies adapted the NCEP III criteria or modified versions to define MS. Second, significant proportion of the included studies were cross-sectional (50%), and the lack of well-designed RCTs or prospective studies resulted in the incomprehensiveness of the current analysis. Each study had slight variations in the study design, subjects, duration of smoking cessation, follow-up period, and adjustment factors. This resulted in significant heterogeneity among studies. Third, some studies did not consider factors such as weight change[24,33,38] or the amount of smoking[20] before cessation, which has had an impact on the analysis Furthermore, only 41% of the studies have reported the duration of smoking cessation,[3,10,19–21,23,24,26,30,32,35,38] and the varying timeframes across different studies make it challenging to integrate the findings. Of the 5 studies involving women,[17,18,22,23,34] available data on the prevalence of MS based on smoking status are scarce, thus making it difficult to include it in the analysis.
Nevertheless, this study is meaningful, as it is the first meta-analysis to directly compare the risk of developing MS between smokers and ex-smokers. Many studies have focused on the association between smoking and the risk of MS or other metabolic abnormalities, and it has been commonly observed that ex-smokers have a lower risk compared to smokers. However, when directly comparing smokers and ex-smokers, significant point of interest in the early stages of smoking cessation, ex-smokers have an increased risk of MS compared to smokers. Although, no significant evidence of an increased the risk of MS was reported in men, the risk of MS increases if the cessation period was <15 years. As MS is also associated with the risk of DM and CVD, the intermediary stage leading to such diseases, this study aimed to emphasize the importance of lifestyle management and precautions at the initiation of smoking cessation, as well as to actively promote smoking cessation.
5. Conclusion
In the early stages of smoking cessation, an increased risk of MS compared to active smoking. As the longer the duration of smoking cessation, the risk of MS becomes less significant. Therefore, smoking cessation should be initiated immediately.
Acknowledgments
This work was supported by the grant from the Research Institute of Medical Science, Daegu Catholic University (2017).
Author contributions
Conceptualization: Yoon Jeong Cho.
Data curation: Hyun Ji Kim, Yoon Jeong Cho.
Formal analysis: Hyun Ji Kim, Yoon Jeong Cho.
Investigation: Hyun Ji Kim, Yoon Jeong Cho.
Methodology: Hyun Ji Kim, Yoon Jeong Cho.
Project administration: Hyun Ji Kim, Yoon Jeong Cho.
Resources: Hyun Ji Kim.
Software: Hyun Ji Kim, Yoon Jeong Cho.
Supervision: Yoon Jeong Cho.
Validation: Hyun Ji Kim, Yoon Jeong Cho.
Visualization: Hyun Ji Kim.
Writing – original draft: Hyun Ji Kim.
Writing – review & editing: Hyun Ji Kim, Yoon Jeong Cho.
Abbreviations:
- CI
- confidence interval
- CVD
- cardiovascular disease
- DM
- diabetes mellitus
- MS
- metabolic syndrome
- NCEP III
- National Cholesterol Education Program’s Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults
- NOS
- Newcastle–Ottawa Quality Assessment Scale
- OR
- odds ratio
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RR
- relative risk.
The authors have no funding and conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
How to cite this article: Kim HJ, Cho YJ. Smoking cessation and risk of metabolic syndrome: A meta-analysis. Medicine 2024;103:22(e38328).
References
- [1].Wilson PW, D’Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112:3066–72. [DOI] [PubMed] [Google Scholar]
- [2].Facchini FS, Hollenbeck CB, Jeppesen J, Chen Y-DI, Reaven G. Insulin resistance and cigarette smoking. Lancet. 1992;339:1128–30. [DOI] [PubMed] [Google Scholar]
- [3].Nakanishi N, Takatorige T, Suzuki K. Cigarette smoking and the risk of the metabolic syndrome in middle-aged Japanese male office workers. Ind Health. 2005;43:295–301. [DOI] [PubMed] [Google Scholar]
- [4].Geslain-Biquez C, Tichet J, Caradec A, D’Hour A, Balkau B, Group DS. The metabolic syndrome in smokers. The DESIR study. Diabetes Metab. 2003;29:226–34. [DOI] [PubMed] [Google Scholar]
- [5].Williamson DF, Madans J, Anda RF, Kleinman JC, Giovino GA, Byers T. Smoking cessation and severity of weight gain in a national cohort. N Engl J Med. 1991;324:739–45. [DOI] [PubMed] [Google Scholar]
- [6].Stein JH, Asthana A, Smith SS, et al. Smoking cessation and the risk of diabetes mellitus and impaired fasting glucose: three-year outcomes after a quit attempt. PLoS One. 2014;9:e98278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Yeh H-C, Duncan BB, Schmidt MI, Wang N-Y, Brancati FL. Smoking, smoking cessation, and risk for type 2 diabetes mellitus: a cohort study. Ann Intern Med. 2010;152:10–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kar D, Gillies C, Zaccardi F, et al. Relationship of cardiometabolic parameters in non-smokers, current smokers, and quitters in diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol. 2016;15:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Song Y-M, Chang W-D, Hsu H-Y, Chen M-D. A short-term smoking cessation may increase the risk of developing metabolic syndrome. Diabetes Metab Syndr. 2015;9:135–7. [DOI] [PubMed] [Google Scholar]
- [10].Shin HS, Oh JE, Cho YJ. The association between smoking cessation period and metabolic syndrome in Korean men. Asia Pac J Public Health. 2018;30:415–24. [DOI] [PubMed] [Google Scholar]
- [11].Page MJ, Moher D. Evaluations of the uptake and impact of the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) Statement and extensions: a scoping review. Syst Rev. 2017;6:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- [13].Stang A. Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5. [DOI] [PubMed] [Google Scholar]
- [14].Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- [15].Macaskill P, Walter SD, Irwig L. A comparison of methods to detect publication bias in meta-analysis. Stat Med. 2001;20:641–54. [DOI] [PubMed] [Google Scholar]
- [16].Egger M, Smith GD. Meta-analysis bias in location and selection of studies. Bmj. 1998;316:61–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Park HS, Oh SW, Cho SI, Choi WH, Kim YS. The metabolic syndrome and associated lifestyle factors among South Korean adults. Int J Epidemiol. 2004;33:328–36. [DOI] [PubMed] [Google Scholar]
- [18].Tonstad S, Svendsen M. Premature coronary heart disease, cigarette smoking, and the metabolic syndrome. Am J Cardiol. 2005;96:1681–5. [DOI] [PubMed] [Google Scholar]
- [19].Wannamethee SG, Shaper AG, Whincup PH. Modifiable lifestyle factors and the metabolic syndrome in older men: effects of lifestyle changes. J Am Geriatr Soc. 2006;54:1909–14. [DOI] [PubMed] [Google Scholar]
- [20].Wada T, Urashima M, Fukumoto T. Risk of metabolic syndrome persists twenty years after the cessation of smoking. Intern Med. 2007;46:1079–82. [DOI] [PubMed] [Google Scholar]
- [21].Chen CC, Li TC, Chang PC, et al. Association among cigarette smoking, metabolic syndrome, and its individual components: the metabolic syndrome study in Taiwan. Metabolism. 2008;57:544–8. [DOI] [PubMed] [Google Scholar]
- [22].Al-Daghri NM. Acute post cessation smoking. A strong predictive factor for metabolic syndrome among adult Saudis. Saudi Med J. 2009;30:267–71. [PubMed] [Google Scholar]
- [23].Hishida A, Koyama A, Tomota A, Katase S, Asai Y, Hamajima N. Smoking cessation, alcohol intake and transient increase in the risk of metabolic syndrome among Japanese smokers at one health checkup institution. BMC Public Health. 2009;9:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Kim BJ, Kim BS, Sung KC, Kang JH, Lee MH, Park JR. Association of smoking status, weight change, and incident metabolic syndrome in men: a 3-year follow-up study. Diabetes Care. 2009;32:1314–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Wan C-J, Lin L-Y, Yu T-H, Sheu WH-H. Metabolic syndrome associated with habitual indulgence and dietary behavior in middle-aged health-care professionals. J Diabetes Investig. 2010;1:259–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Zhu Y, Zhang M, Hou X, et al. Cigarette smoking increases risk for incident metabolic syndrome in Chinese men-Shanghai diabetes study. Biomed Environ Sci. 2011;24:475–82. [DOI] [PubMed] [Google Scholar]
- [27].Calo W, Ortiz A, Suárez E, Guzmán M, Pérez C, Pérez C. Association of cigarette smoking and metabolic syndrome in a Puerto Rican adult population. J Immigr Minor Health. 2013;15:810–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Kim S, So WY. Prevalence and correlates of metabolic syndrome and its components in elderly Korean adults. Exp Gerontol. 2016;84:107–12. [DOI] [PubMed] [Google Scholar]
- [29].Udo T, White MA, Barnes RD, et al. Psychosocial and metabolic function by smoking status in individuals with binge eating disorder and obesity. Addict Behav. 2016;53:46–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Heggen E, Svendsen M, Tonstad S. Smoking cessation improves cardiometabolic risk in overweight and obese subjects treated with varenicline and dietary counseling. Nutr Metab Cardiovasc Dis. 2017;27:335–41. [DOI] [PubMed] [Google Scholar]
- [31].Saffar Soflaei S, Darroudi S, Tayefi M, et al. Hookah smoking is strongly associated with diabetes mellitus, metabolic syndrome and obesity: a population-based study. Diabetol Metab Syndr. 2018;10:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Solak I, Duran C, Demirtepe I, Pekgor S, Eryilmaz MA. The effects of short-term smoking cessation on metabolic syndrome parameters. Acta Med Mediterranea. 2018;34:2037–44. [Google Scholar]
- [33].Kim K, Choi S, Lee JK, et al. Weight change after smoking cessation and incident metabolic syndrome in middle-aged Korean men: an observational study. Sci Rep. 2019;9:3103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Oh SS, Jang J-E, Lee D-W, Park E-C, Jang S-I. Cigarette type or smoking history: Which has a greater impact on the metabolic syndrome and its components? Sci Rep. 2020;10:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Park MB, Kang CK, Choi JK. Smoking cessation is related to change in metabolic syndrome onset: a rural cohort study. Tob Induc Dis. 2020;18:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kim SW, Kim HJ, Min K, et al. The relationship between smoking cigarettes and metabolic syndrome: a cross-sectional study with non-single residents of Seoul under 40 years old. PLoS One. 2021;16:e0256257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Park S, Han K, Lee S, et al. Smoking, development of or recovery from metabolic syndrome, and major adverse cardiovascular events: a nationwide population-based cohort study including 6 million people. PLoS One. 2021;16:e0241623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Suutari-Jääskö A, Ylitalo A, Ronkaine J, Huikuri H, Kesäniemi YA, Ukkola OH. Smoking cessation and obesity-related morbidities and mortality in a 20-year follow-up study. PLoS One. 2022;17:e0279443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001;285:2486–97. [DOI] [PubMed] [Google Scholar]
- [40].Alberti G, Zimmet P, Shaw J, Grundy SM. The IDF consensus worldwide definition of the metabolic syndrome. Brussels: International Diabetes Federation; 2006;23:469–80. [DOI] [PubMed] [Google Scholar]
- [41].Teramoto T, Sasaki J, Ueshima H, et al. Metabolic syndrome. J Atheroscler Thromb. 2008;15:1–5. [DOI] [PubMed] [Google Scholar]
- [42].Sun K, Liu J, Ning G. Active smoking and risk of metabolic syndrome: a meta-analysis of prospective studies. PLos One. 2012;7:e47791.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Campbell SC, Moffatt RJ, Stamford BA. Smoking and smoking cessation: the relationship between cardiovascular disease and lipoprotein metabolism: a review. Atherosclerosis. 2008;201:225–35. [DOI] [PubMed] [Google Scholar]
- [44].Yoon C, Goh E, Park SM, Cho B. Effects of smoking cessation and weight gain on cardiovascular disease risk factors in Asian male population. Atherosclerosis. 2010;208:275–9. [DOI] [PubMed] [Google Scholar]
- [45].Gami AS, Witt BJ, Howard DE, et al. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49:403–14. [DOI] [PubMed] [Google Scholar]
- [46].Zhang L, Guo Z, Wu M, Hu X, Xu Y, Zhou Z. Interaction of smoking and metabolic syndrome on cardiovascular risk in a Chinese cohort. Int J Cardiol. 2013;167:250–3. [DOI] [PubMed] [Google Scholar]
- [47].Duncan MS, Freiberg MS, Greevy RA, Kundu S, Vasan RS, Tindle HA. Association of smoking cessation with subsequent risk of cardiovascular disease. JAMA. 2019;322:642–50. [DOI] [PMC free article] [PubMed] [Google Scholar]