Abstract
Introduction
Although total knee arthroplasty (TKA) is a very frequent surgery, one in five patients is not completely satisfied. Mechanical alignment (MA) is the most popular technique for implanting TKA. However, to improve clinical outcomes, new techniques that aim to rebuild the native alignment of the knee have been developed.
Objective
The aim of this study is to perform a systematic review of the available clinical trials and observational studies comparing clinical and radiological outcomes of different methods of alignment (kinematic, anatomic, functional) to MA.
Methods
A systematic review is performed comparing results of patient reported outcome measures (PROMs) questionnaires (WOMAC, OKS, KSS, KOOS, FJS), radiological angles (HKA, mLDFA, MPTA, JLOA, femoral rotation and tibial slope) and range of motion (ROM).
Results
Kinematic and functional alignment show a slight tendency to obtain better PROMs compared to mechanical alignment. Complication rates were not significantly different between groups. Nevertheless, these results are not consistent in every study. Anatomic alignment showed no significant differences compared to mechanical alignment.
Conclusion
Kinematic alignment is an equal or slightly better alternative than mechanical alignment for patients included in this study. However, the difference between methods does not seem to be enough to explain the high percentage of dissatisfied patients. Studies implementing lax inclusion and exclusion criteria would be needed to resemble conditions of patients assisted in daily surgical practice. It would be interesting to study patient’s knee phenotypes, to notice if any method of alignment is significantly better for any constitutional deviation.
Keywords: Total knee arthroplasty, mechanical alignment, kinematic alignment, anatomic alignment, functional alignment., knee phenotypes
INTRODUCTION
Total knee arthroplasty (TKA) involves replacing the knee joint with a prosthesis, usually in patients with knee osteoarthritis. Its main goals are to restore normal joint function and alleviate pain.1
Although the number of knee arthroplasties performed is increasing, around 20% of uncomplicated TKA patients remain dissatisfied, a relatively high figure compared to similar interventions like hip arthroplasty.2,3
Multiple factors have been described that could explain this dissatisfaction rate, including patient-related factors (age and outcome expectations), residual pain, residual limitation of knee function and range of motion, and surgical technique. Achieving good long-term clinical and functional outcomes in TKA depends on various factors, with proper implant alignment and balanced soft tissues being notable among them.4
Various methods for aligning the prosthesis with respect to the knee’s mechanical axis were developed when the technique was first introduced. Among them, the mechanical alignment (MA) technique was founded on the theory that aligning the knee to neutral, with a hip-knee-ankle (HKA) angle within 3 degrees of neutral in the coronal plane would ensure longer prosthetic material durability, as it would distribute the load equally across both knee compartments.5
Although MA remains the most popular technique for implanting TKA, in the pursuit of reducing the percentage of dissatisfied patients and considering that MA may alter the native knee anatomy, laxity, and kinematics, new alignment methods have been developed.6
MECHANICAL ALIGNMENT
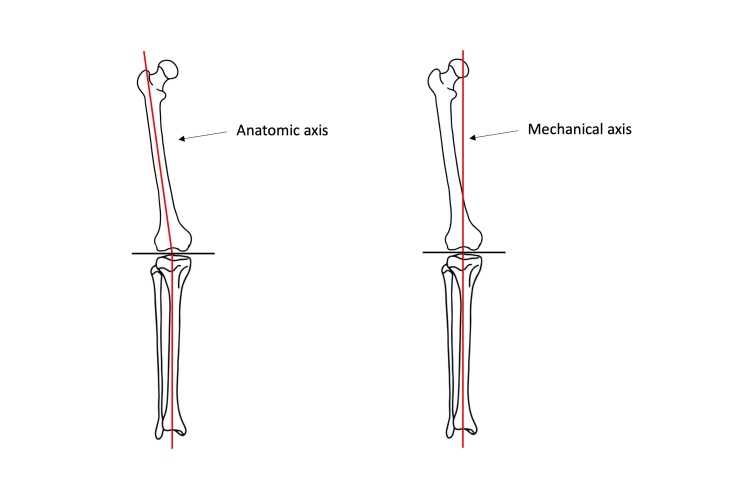
MA (Figure 1) aims to align the femur and tibia components perpendicular to their mechanical axes, modifying internal and external rotation angles of the components to establish parallel extension-flexion gaps for prosthetic knee placement and releasing the medial or lateral collateral ligaments as needed to restore medial and lateral tension balance in the knee.7 This implant positioning was designed to attempt to achieve even distribution of loads between tibial compartments to avoid accelerated polyethylene wear and premature implant loosening.8
Figure 1. Anatomic axis (left) and mechanical axis (right).
As the first developed method, it has a series of advantages: familiarity with the technique, long-term known outcomes, and equitable load distribution. Additionally, commonly used implants are designed for this type of alignment. Nonetheless, limitations have prompted the development of alternative techniques. Firstly, it oversimplifies knee biomechanics, focusing solely on alignment around the mechanical axis. Secondly, challenges may arise in achieving joint space balance throughout flexion and extension. Thirdly, establishing a mechanical axis may lead to soft tissue imbalance, needing tendon and ligament modifications through release or tension increase.7 Fourthly, insufficient resection of the lateral femoral condyle occurs when intervening in varus knees, altering patellar biomechanics and causing flexion overload. Thus, there is a hypothesis that patellar instability influences patient dissatisfaction.8
ADJUSTED MECHANICAL ALIGNMENT
One of the developed techniques involves modifying mechanical alignment for patients with severe coronal plane deformities. The tibial component is aligned mechanically, while the femoral component allows a slight constitutional deformity (maximum of 3°) preservation.8,9
ANATOMIC ALIGNMENT
Anatomic alignment (AA) (Figure 1) was introduced in the 1980s by Hungerford and Krackow.10 It seeks systematic attainment of an oblique joint line, 2-3° valgus relative to the mechanical axis of the limb. With its implementation, prostheses have been developed with a 3° obliquity included in the design, with the surgical procedure being similar to MA.8
KINEMATIC ALIGNMENT
Kinematic alignment (KA) aims to restore the natural joint by preforming a true knee resurfacing. Consequently, femoral and tibial implants are aligned on the knee’s three kinematic axes.11,12
To achieve accurate restoration of the native joint line, precise resection is essential. Several techniques are utilized for this purpose, such as conventional calipered measurements,13 patient-specific instrumentation (PSI),14 computer navigation,15 and robotic-assisted surgery.16 Advocates of KA argue that this approach can enhance pain relief, functionality, and patient satisfaction by reducing gap imbalances and eliminating the necessity for soft tissue release.17,18
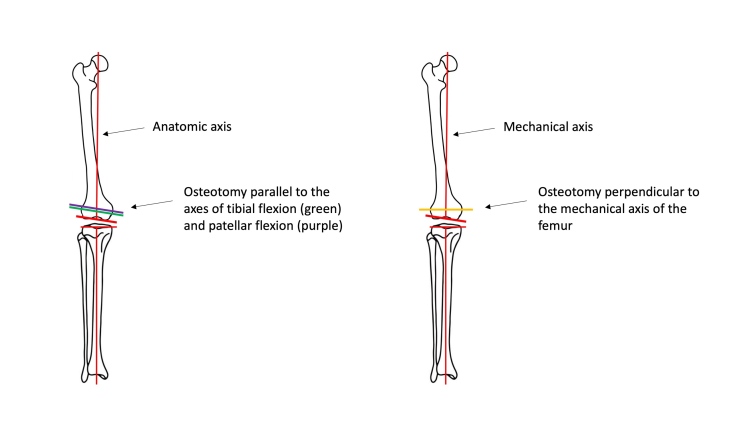
In the Figure 2 we compare the femoral osteotomy in kinematic alignment and mechanical alignment.
Figure 2. Comparison of femoral osteotomy in kinematic alignment (left, parallel to purple and green axes) and mechanical alignment (right, in yellow). Image modified from Hirschmann et al.19.
RESTRICTIVE KINEMATIC ALIGNMENT
Restrictive kinematic alignment (RKA) involves applying KA while maintaining the outcome within a “precaution zone”, before it is clearly known which alignment boundaries are safe.8,20 In rare cases where the deformity extends beyond the precaution zone, corrective osteotomies are performed to subsequently align the prosthesis kinematically.8
FUNCTIONAL ALIGNMENT
Functional alignment (FA) was developed to reduce lateral compartment laxity and attain stability throughout the range of motion.21 It aims to position components to minimize compromise to the soft-tissue envelope, thus restoring the joint’s plane and obliquity as dictated by the soft tissues. Virtual gap balancing can be initiated either from a MA or a KA starting point.9,22 However, starting from a MA point requires greater external rotation of the femoral component to balance the medial flexion-to-extension gap, resulting in a more neutral Joint Line Obliquity (JLO). Conversely, starting from a KA point is more likely to minimize lengthening of the lateral joint line, maintain the stability of the medial collateral ligament to support any medial pivoting, and restore the native JLO.22–24
CLINICAL OUTCOME ASSESSMENT
To objectively assess clinical outcomes after surgery, collected articles used various evaluation scales or Patient-Reported Outcome Measures (PROMs):
Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC).25
Knee Society Score, which comprises two parts: Knee Society Score original (KSS) and Knee Society Score functional (KFS). Combined Knee Society Score (CKSS) sums both scores.26
Oxford Knee Score (OKS).27
Range of motion (ROM), equivalent to the flexion angle’s range.28
The Forgotten Joint Score (FJS): The score is based on patients forgetting about the replaced joint in daily life.29
The Knee Injury and Osteoarthritis Outcome Score (KOOS).30
RADIOLOGICAL OUTCOME ASSESSMENT
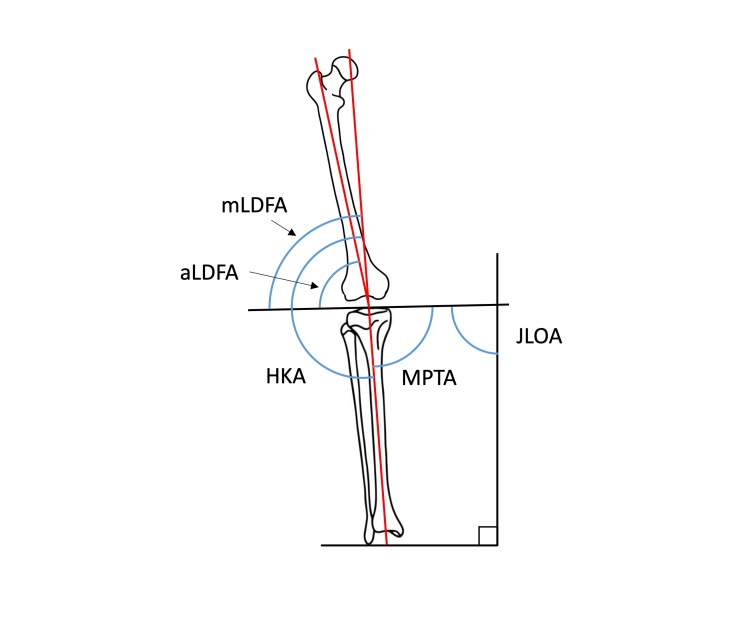
Radiological results were collected through imaging tests such as plain radiography, computed tomography, and magnetic resonance imaging to determine deviations from different limb axes and differences between alignment methods. In the coronal plane (Figure 3)31: Hip-Knee-Ankle angle (HKA), Mechanical Lateral Distal Femoral Angle (mLDFA), Anatomic Lateral Distal Femoral Angle (aLDFA), Medial Proximal Tibial Angle (MPTA) and Joint Line Obliquity Angle (JLOA). In the sagittal plane: Tibial Slope (TS).32 Additionally, some articles reported femoral rotation: rotation of the femoral component relative to the epicondylar axis (negative values indicate internal rotation).
Figure 3. Knee angles in the coronal plane.
JUSTIFICATION
Despite the existence of meta-analyses and systematic reviews comparing KA and MA, no superiority of one technique over the other has been established. Therefore, a systematic review of the current literature was conducted, focusing on recent outcomes without limiting the search to KA and MA exclusively. The PICO (Patient, Intervention, Comparator, and Outcome) strategy was applied to conduct the review.
P: Patients requiring TKA.
I: TKA using alignment methods other than MA.
C: TKA aligned mechanically (the current technique of choice).
O: Clinical outcomes.
OBJECTIVES
Considering the advantages and disadvantages of each technique, the following objectives were investigated:
Comparing implant lifespan between MA and other methods.
Comparing the percentage of dissatisfied patients between MA and other methods.
Comparing the stability of operated knees, including patellar stability.
Comparing radiological results of operated knees.
Whether any alignment method demonstrates sufficient superiority and safety to be considered better than the most common method (MA).
METHODS
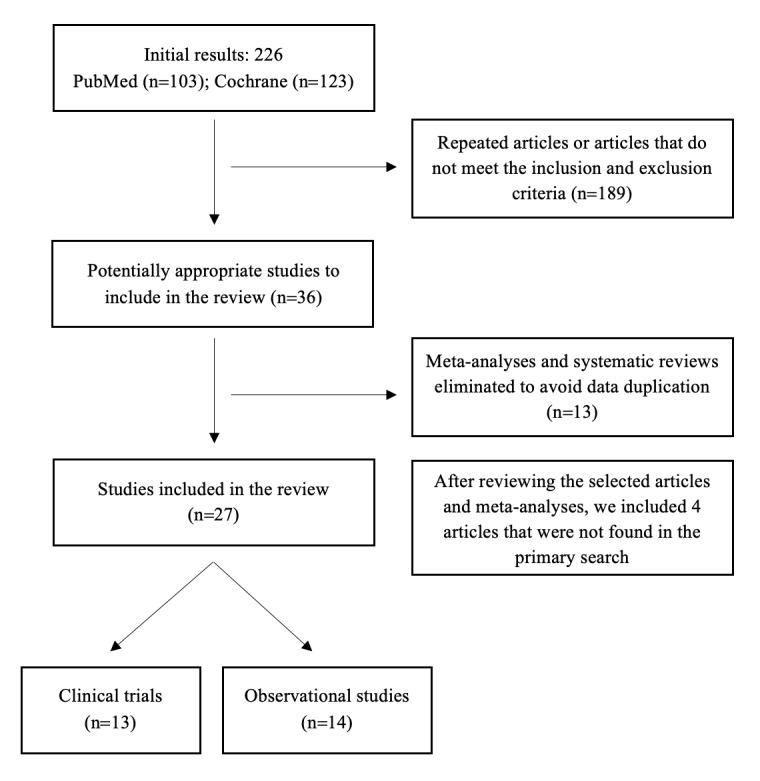
We performed a systematic literature search in keeping with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines. The following combination of thesauri and boolean operators was applied in Pubmed and Cochrane databases, being the final search on the 20th of March 2023: ((((kinematic alignment) OR (mechanical alignment)) OR (functional alignment)) OR (anatomic alignment)) AND (total knee arthroplasty), with the terms present in the article titles. No additional filters were applied to the search. This yielded 226 articles.
Two authors screened the abstracts in order to include articles that matched inclusion and exclusion criteria. Eligibility criteria included articles that provided comparative data between different alignment methods and reported clinical and/or radiological outcomes. Exclusion criteria were duplicates, unpublished results, studies limited to the description of surgical techniques, studies whose results were solely due to robotics, navigation or different brand of implants, cadaver studies, virtually performed surgery studies, letters, and articles whose full text was not written in English or Spanish. Furthermore, meta-analyses and systematic review were excluded to avoid data duplication.
From the primary search in Pubmed, 103 entries were obtained, while from Cochrane, 123 entries were collected, originating from: Embase (n = 53), Pubmed (n = 48), International Clinical Trials Registry Platform (ICTRP, n = 26), National Institute of Health (NIH, n = 19), and CINAHL (n = 2). After applying the inclusion and exclusion criteria and eliminating the duplicated articles, we obtained 23 studies. Additional records identified from meta-analyses were included (n=4), resulting in a total of 27 articles. The article selection strategy is illustrated in the flowchart from Figure 4.
Figure 4. Systematic Review Flowchart.
RESULTS
The results are summarized in the Tables I, II, III, IV, V, VI and VII, which include:
Table I. Demographic data and characteristics of clinical trials comparing kinematic and mechanical alignment.14,33–45.
| Author and year | Follow-up months (average) | Method | Number of knees operated | Average age (years) | Women % | BMI (kg/m2) |
|---|---|---|---|---|---|---|
| Dossett 201233 | 6 | Kinematic + PSI | 41 | 65 ± 8 | 5 | 29 ± 4,2 |
| Mechanical | 41 | 66 ± 8,2 | 15 | 33 ± 6,4 | ||
| Yim 201334 | 24 | Anatomic + PSI | 61 | 69 (58-85) | 93 | 25,7 (18-32,5) |
| Mechanical + PSI | 56 | 66,1 (51-84) | 86 | 26,3 (20-37,2) | ||
| Dossett 201435 | 24 | Kinematic + PSI | 44 | 66 ± 7,7 | 5 | 29 ± 4,1 |
| Mechanical | 44 | 66 ± 8,6 | 12 | 32 ± 4,9 | ||
| Belvedere 201536 | 6 | Kinematic + PSI | 6 | NO | ||
| Mechanical | 11 | |||||
| Waterson 201637 | 12 | Kinematic | 36 | NO | ||
| Mechanical | 35 | |||||
| Calliess 201714 | 12 | Kinematic + PSI | 100 | 67 ± 8 | 61 | 30 ± 4 |
| Mechanical | 100 | 70 ± 8 | 57 | 30 ± 5 | ||
| Matsumoto 201738 | 12 | Kinematic | 30 | 75,3 (55-85) | 88 | 26,9 ± 3,9 |
| Mechanical | 30 | 76,1 (57-86) | 90 | 25,5 ± 3,2 | ||
| Seon 201739 | 96 | Kinematic | 30 | NO | ||
| Mechanical | 30 | |||||
| Young 201740 | 24 | Kinematic + PSI | 49 | 72 ± 6,5 | 51 | 30 ± 4 |
| Navigated mechanical | 50 | 70 ± 7,5 | 52 | 31,5 ± 5 | ||
| Laende 201941 | 24 | Kinematic + PSI | 24 | 64 ± 8 | 67 | 36 ± 5,9 |
| Mechanical | 23 | 63 ± 7 | 74 | 34 ± 7,4 | ||
| Yeo 201942 | 96 | Anatomical | 30 | 72 ± 5,52 | 83 | 26,1 ± 5 |
| Mechanical | 30 | 74 ± 5,16 | 90 | 26,9 ± 2,1 | ||
| McEwen 202043 | 24 | Functional | 41 | 65 (51-78) | NO | 31 (23-39) |
| Mechanical | 41 | |||||
| Young 202044 | 60 | Kinematic | 49 | 72 ± 6,5 | 51 | 30 ± 4 |
| Mechanical | 50 | 70 ± 7,5 | 52 | 31,5 ± 5 | ||
| Sarzaeem 202145 | 3 | Kinematic + PSI | 32 | 62,9 ± 6 | 44 | 27,1 ± 3,4 |
| Mechanical | 32 | 65,3 ± 6,8 | 47 | 26,8 ± 3,4 | ||
Note: “BMI”: Body Mass Index; “NO”: not included, “PSI”: patient-specific instruments.
Table II. Demographic data and characteristics of observational studies.9,17,18,31,46–55.
| Author and year | Study | Follow-up months (average) | Method | Number of knees operated | Average age (years) | Women % | BMI (kg/m2) |
|---|---|---|---|---|---|---|---|
| Blakeney 201917 | Case control study | 33,5 | Kinematic | 18 | 61 ± 8 | 67 | 31 ± 6 |
| Mechanical | 18 | 64 ± 7 | 67 | 32 ± 3 | |||
| An 201918 | Retrospective cohort study | 0 | Kinematic | 90 | 67 ± 12 | 61 | No comparison |
| Mechanical | 120 | 67,9 ± 10,7 | 63 | ||||
| Jeremić 202046 | Case control study | 12 | Kinematic | 24 | 70,7 ± 6,7 | No differences | 30,6 ± 4,5 |
| Mechanical | 24 | 72.5 (5.8) | 30.0 (4) | ||||
| Luceri 202047 | Retrospective cohort study | 3 | Kinematic | 13 | 70 ± 7,1 | 54 | 28,5 ± 4,8 |
| Mechanical | 13 | 69,1 ± 8 | 69 | 27,4 ± 3,4 | |||
| Shelton 2021*48 | Retrospective cohort study | 36 ± 16 | Kinematic | 78 | 70 ± 8 | 73 | 31 ± 6 |
| 120 ± 54 | Mechanical | 78 | NA | 73 | NA | ||
| Abhari 202149 | Retrospective cohort study | 12 | Kinematic (1-5º varus) |
43 | 66 ± 1,5 | 58 | 34 ± 1 |
| Kinematic (6-10º varus) |
56 | 68 ± 1,2 | 36 | 31 ± 0,71 | |||
| Kinematic (11-14º varus) |
16 | 67 ± 2,7 | 44 | 34 ± 1,7 | |||
| Mechanical | 115 | No differences | BMI higher than in KA | ||||
| Alexander 202250 | Retrospective cohort study | 1,5 | Kinematic | 107 | 65 ± 8,6 | 57 | 34,2 ± 8 |
| Mechanical | 223 | 64,5 ± 8,5 | 59 | 32,5 ± 6,6 | |||
| Elbuluk 202251 | Retrospective cohort study | 24 | Kinematic (cutting guide) | 100 | No differences in age, sex, BMI or coronal plane deviation. | ||
| Mechanical (navigated) | 100 | ||||||
| Sappey-Marinier 202231 | Case series | 32 ± 26 | Mechanical | 7 | 70,1 ± 9,3 | 57 | 27 ± 3 |
| Kinematic | 7 | ||||||
| Winnock de Grave 20229 | Retrospective cohort study | 12 | Inverted kinematic | 40 | 69,9 ± 8,3 | 60 | 29,2 ± 4,8 |
| Mechanical (adjusted) | 40 | 67,4 ± 9,5 | 58 | 30 ± 5,3 | |||
| Choi 202252 | Retrospective cohort study | 24 | Functional (robotic) | 60 | 70 ± 5,7 | 78 | 26,7 ± 2,6 |
| Mechanical (manual) | 60 | 70,1 ± 5,7 | 78 | 27,1 ± 3,5 | |||
| Lung 202253 | Retrospective cohort study | 3 | Kinematic | 44 | 68,5 ± 7,5 | 63 | 31 ± 6,6 |
| Mechanical | 57 | 68,2 ± 7,7 | 65 | 32,6 ± 5,6 | |||
| Ma 202254 | Ambispective cohort study | 6 | Restrictive kinematic | 48 | 69,3 | 86 | 27,2 |
| Mechanical | 45 | 67,4 | 78 | 25,2 | |||
| Wen 202355 | Retrospective cohort study | 30,8 | Kinematic | 65 | 70,6 ± 6,4 | 70 | 27,3 ± 3,4 |
| Mechanical | 61 | 71,2 ± 7,1 | 66 | 27,2 ± 3,7 | |||
Note: “BMI”: Body Mass Index; “NA”: Not available. Data with statistically significant differences are shaded in gray.
* Prior primary mechanical alignment total knee arthroplasty (TKA) in the contralateral limb.
Table III. Results of functional assessment scales in clinical trials.14,33–45.
| Author and year | Method | WOMAC | OKS | KSS (Pain) | KSS (Function) | CKSS | KOOS | FJS | ROM FLEXION (º) |
|---|---|---|---|---|---|---|---|---|---|
| Dossett 201233 | Kinematic + PSI | 12 ± 14,8 | 8 ± 9,1 | 90 ± 14,3 | 84 ± 1,9 | 174 ± 31,3 | 120 ± 9,2 | ||
| Mechanical | 28 ± 18,5 | 15 ± 8,9 | 79 ± 18,2 | 70 ± 21 | 149 ± 35,3 | 115 ± 12,3 | |||
| Average difference | 16 (8,4-23) | 7 (3,1-10,9) | 11 (4,6-19) | 14 (4-22) | 25 (10-39,3) | 5 | |||
| Yim 201334 | Anatomical + PSI | 19,3 ± 8,6 | 125 ± 11,5 | ||||||
| Mechanical + PSI | 20,4 ± 6,7 | 129 ± 11,5 | |||||||
| Dossett 201435 | Kinematic + PSI | 15 ± 20,3 | 40 ± 10,2 | 84 ± 17,2 | 77 ± 19,2 | 160 ± 31,9 | 121 ± 10,4 | ||
| Mechanical | 26 ± 22,2 | 33 ± 11,1 | 72 ± 21,2 | 65 ± 21,1 | 137 ± 37,9 | 113 ± 12,5 | |||
| Average difference | 10,7 (1,5-19,8) | 6,2 (1,7-10,7) | 11 (3,1-19,4) | 12 (3,5-20,6) | 23 (8,4-38,1) | 8,5 | |||
| Belvedere 201536 | Kinematic + PSI | 91 ± 12 | 90 ± 15 | ||||||
| Mechanical | 78 ± 20 | 80 ± 23 | |||||||
| Waterson 201637 | Kinematic | 83,5 ± 21,4 | 77,7 ± 20 | 118,5 ± 12 | |||||
| Mechanical | 87,8 ± 15,9 | 76,4 ± 19 | 118,4 ± 9,4 | ||||||
| Average difference | 4,3 | 1,3 | 0,1 | ||||||
| Calliess 201714 | Kinematic + PSI | 13 ± 16 | 190 ± 18 | ||||||
| Mechanical | 26 ± 11 | 178 ± 17 | |||||||
| Matsumoto 201738 | Kinematic | 92,9 ± 4,4 | 68,3 ± 13,6 | 122,3 ± 8,9 | |||||
| Mechanical | 92,5 ± 5,3 | 64 ± 15,9 | 116,8 ± 12,6 | ||||||
| Seon 201739 | Kinematic | NO DIFF | NO DIFF | 83,7 ± 16,7 | NO DIFF | ||||
| Mechanical | 74,8 ± 16,45 | ||||||||
| Young 201740 | Kinematic + PSI | 88 ± 14 | 42 ± 6 | 89 ± 13 | 83 ± 18 | 69 ± 26 | 119 ± 11 | ||
| Mechanical | 85,5 ± 17 | 41 ± 6 | 87 ± 16 | 79,5 ± 24 | 66 ± 26 | 116 ± 11 | |||
| Average difference | -3(-9,1 to 3,2) | -1(-3,5 to 1,4) | -2(-7,8 to3,9) | -4(-12 to 5) | -3 (-13,3 to 7,5) | ||||
| Laende 201941 | Kinematic + PSI | 31 ± 7,8 | |||||||
| Mechanical | 30 ± 8,6 | ||||||||
| Yeo 201942 | Anatomical | 19,3 ± 1,9 | 47,5 ± 5,6 | 90,1 ± 10,5 | 125 ± 11,5 | ||||
| Mechanical | 20,4 ± 1,8 | 47,2 ± 7,5 | 93 ± 9,1 | 129 ± 11,5 | |||||
| McEwen 202043 | Functional | 44,4 ± 4,3 | 89,6 ± 12,9 | 79,9 ± 23,5 | 127 ± 10 | ||||
| Mechanical | 44,1 ± 4,1 | 88,5 ± 13,7 | 79,6 ± 19,4 | 127 ± 11 | |||||
| Young 202044 | Kinematic | 86,1 ± 15,5 | 41,4 ± 7,2 | 74,6 ± 12,2 | 81 ± 18,4 | 68 ± 28,8 | |||
| Mechanical | 89,1 ± 15,3 | 41,7 ± 6,3 | 74,2 ± 9 | 86,7 ± 16,8 | 74,4 ± 23,6 | ||||
| Average difference | -3 (-9,9 a 3,9) | -0,3(-3,2, 2,5) | 0,5 (-6,1 a 7) | -5,7 (-14,5 a 3,1) | -5,7 (-14,5 a 3,1) | ||||
| Sarzaeem 202145 | Kinematic + PSI | 31,2 ± 4,6 | |||||||
| Mechanical | 35,5 ± 5,7 |
Note: “NO DIFF”: the article does not include the specific data but indicates that there are no significant differences; “PSI”: patient-specific instruments. Data with statistically significant differences are shaded in gray. The Young et al article from 2017 used a version of the WOMAC that gives a score from 0 to 100, with 0 being the worst possible score and 100 being the best.
Table IV. Results of functional assessment scales in observational studies.9,17,31,46–53,55.
| Author and year | Method | WOMAC | OKS | KSS (Pain) | KSS (Function) | CKSS | KOOS | FJS | ROM |
|---|---|---|---|---|---|---|---|---|---|
| Blakeney 201917 | Kinematic | 74 ± 17.1 | 54 ± 8,7* | ||||||
| Mechanical | 61 ± 18.1 | 49 ± 8,7* | |||||||
| Jeremić 202046 | Kinematic | 94.0 (79–98) | 67.0 (54–74) | 65.0 (45–75)** | 77 (58–96) | ||||
| Mechanical | 75.0 (61–82) | 60.0 (46–69) | 40.0 (20–55)** | 51 (39–67) | |||||
| Luceri 202047 | Kinematic | 86 ± 3,8 | 93 ± 10,3 | 81 ± 7,1 | |||||
| Mechanical | 76 ± 9,6 | 76 ± 16,2 | ERROR | ||||||
| Shelton 202148 | Kinematic | 43 (39-47) | 75 (51-92) | ||||||
| Mechanical | 42 (33-45) | 60 (29-80) | |||||||
| Abhari 202149 | Restrictive kinematic | 90 ± 1,5 | 93 ± 0,9 | 85 ± 1,6 | 72 ± 2,7 | 120 ± 0,5 | |||
| Mechanical | 85 ± 1,6 | 83 ± 1,1 | 73 ± 1,7 | 61 ± 3,8 | 117 ± 0,7 | ||||
| Alexander 202250 | Kinematic | 114 ± 10,1 | |||||||
| Mechanical | 110 ± 11,9 | ||||||||
| Elbuluk 202251 | Kinematic (cutting guide) | 91 ± 5 | 92 ± 5,3 | ||||||
| Mechanical (navigated) | 84 ± 4 | 78 ± 7,1 | |||||||
| Sappey-Marinier 202231 | Mechanical | 47 ± 7 | 49 ± 20 | 96 ± 23 | 84 ± 35 | ||||
| Difference after reintervention (Mechanical to Kinematic) | 75 ± 27 | 30 ± 23 | |||||||
| Winnock de Grave 20229 | Inverted kinematic | 44,8 ± 3,5 | |||||||
| Mechanical (adjusted) | 42,2 ± 6,3 | ||||||||
| Choi 202252 | Functional (robotic) | 14 ± 12,3 | 95 ± 6,4 | 77 ± 15,1 | 80 ± 30,1 | ||||
| Mechanical (manual) | 19 ± 10,1 | 90 ± 12,9 | 59 ± 1,6 | 35 ± 28,4 | |||||
| Lung 202253 | Kinematic | 77 ± 16,2 | 116 ± 10,8 | ||||||
| Mechanical | 83 ± 12,1 | 114 ± 11,4 | |||||||
| Wen 202355 | Kinematic | 85 ± 8,6 | 81 ± 9,5 | 86 ± 9,7 | |||||
| Mechanical | 78 ± 9,3 | 78 ± 10,6 | 73 ± 13,8 |
Note: The article by Luceri et al in 2020 includes an error in the KOOS data for the mechanically aligned intervention group. In the article by Abhari et al in 2021, although not specified in the text, it is understood that, based on the results presented for WOMAC, the shortened version with values ranging from 0 to 100 (from worse to better) was used, as the result is abnormally high compared to the rest of the functional questionnaires. The article by An et al in 2019 does not include functional results, only radiological ones. The article by Ma et al in 2023 estimates functional outcomes using equations; they are not reported by the patient themselves, so they are not included. The article by Sappey Marinier et al in 2022 is a comparison between patients who have undergone surgery with mechanical alignment, but a reintervention was necessary, and this was performed following a kinematic alignment (using the contralateral knee as the native knee model). Shelton et al in 2019 performed a retrospective study with self-reported outcome measures in patients treated with a calipered kinematic alignment TKA that already had a contralateral mechanically aligned TKA. Data showing statistically significant differences are shaded in gray.
*Blakeney et al in 2018 found statistically significant differences in knee flexion-extension ROM during gait cycle.
**Jeremić et al in 2020 found statistically significant differences in Sport and Recreation Function section of the KOOS.
Table V. Results of stability assessment.14,35,40,43,46,49.
| Author and year | Method | Gap (mm) | Revision for TFJI | Revision for PFJI | Patella instability rate | ||||
|---|---|---|---|---|---|---|---|---|---|
| MEG | LEG | MFG | LFG | ||||||
| Dossett 201435 | Kinematic + PSI | 0% | |||||||
| Mechanical | 2,3% | ||||||||
| Calliess 201714 | Kinematic + PSI | 2% | |||||||
| Mechanical | 1% | ||||||||
| Young 201740 | Kinematic + PSI | 2% | 2% | ||||||
| Navigated mechanical | 2% | 2% | |||||||
| McEwen 202043 | Functional | 1 | 1,1 | 3,2 | 3,5 | ||||
| Mechanical | 1,1 | 1,3 | 3,2 | 3,6 | |||||
| Jeremić 202046 | Kinematic | 0% | 0% | ||||||
| Mechanical | 0% | 0% | |||||||
| Abhari 202149 | Restricted kinematic | 0% | 0% | ||||||
| Mechanical | 0,9% | 0,9% | |||||||
Note: “MEG”: medial extension gap; “LEG”: lateral extension gap; “MFG”: medial flexion gap; “LFG”: lateral flexion gap; “TFJI”: tibiofemoral joint instability; “PFJI”: patellofemoral joint instability.
Table VI. Radiological results of clinical trials.14,33–35,38,40–43.
| Author and year | Method | HKA (º) | mLDFA (º) | MPTA (º) | JLOA (º) | Femoral rotation (º) | Tibial Slope (º) |
|---|---|---|---|---|---|---|---|
| Dossett 201233 | Kinematic + PSI | 0,3 ± 2,8 | 88,6 ± 2 | -2,1 ± 2,1 | 5 ± 5,4 | ||
| Mechanical | 0,0 ± 2,2 | 91 ± 2,6 | 0,0 ± 2,4 | 3 ± 4,7 | |||
| Average difference | 0,3 (-0,9 to 1,3) | -2,4 (-3,4 to -1,4) | -2,1 (-3,1 to -1,1) | 2 (-4,3 to 0,1) | |||
| Yim 201334 | Anatomical + PSI | -0,4 ± 2 | 91,7 ± 1,9 | 87,5 ± 1,7 | 4,6 ± 1,7 | ||
| Mechanical + PSI | -0,7 ± 1,7 | 89,5 ± 0,4 | 90,1 ± 0,4 | 5,9 ± 0,7 | |||
| Dossett 201435 | Kinematic + PSI | 0,1 ± 2,8 | 88,7 ± 2 | 87,8 ± 2,6 | -2 ± 2 | ||
| Mechanical | -0,1 ± 2,5 | 90,8 ± 2,7 | 90 ± 2,1 | -0,1 ± 2,7 | |||
| Average difference | 0,2 (-0,9 to 1,4) | -2,2 (-3,2 to -1,2) | 2,1 (1,1 to 3,1) | -1,9 (-2,9 to -0,9) | |||
| Calliess 201714 | Kinematic + PSI | -1 ± 3 | 88 ± 1 | 88 ± 1 | 4 ± 3,4 | ||
| Mechanical | 1 ± 1 | 89 ± 0 | 89 ± 0 | 4 ± 2 | |||
| Matsumoto 201738 | Kinematic | 1,8 ± 1,5 (-1,5 to 6) | -0,9 ± 2,3 | ||||
| Mechanical | 0,1 ± 1,4 (-3 to 3) | -4,3 ± 1,9 | |||||
| Young 201740 | Kinematic + PSI | 0,4 ± 3,5 | 88 ± 2,5 | 87 ± 3 | -0,5 ± 2,5 | -4 ± 2,5 | |
| Mechanical (navigated) | 0,7 ± 2 | 89,5 ± 1,6 | 89,3 ± 1,8 | 1,5 ± 2,5 | -1,3 ± 2 | ||
| Average difference | -0,3 (-1,4 to 0,8) | -1,6 (-2,5 to -0,7) | -1,9 (-3 to -0,8) | 2 (1 to 3) | 2,3 (1,3 to 3,3) | ||
| Laende 201941 | Kinematic + PSI | 2,3 ± 2,6 | 86,7 ± 2 | ||||
| Mechanical | 2,1 ± 2,1 | 89,2 ± 1,7 | |||||
| Average difference | 0,2 (-1,55 to 1,15) | -2,5 (-3,6 to -1,4) | |||||
| Yeo 201942 | Anatomical | 0,1 ± 2 | 88,3 ± 1,9 | 87,5 ± 1,7 | 7,5 ± 2,8 | ||
| Mechanical | -0,3 ± 1,7 | 90,5 ± 0,4 | 90,1 ± 0,4 | 6,4 ± 1 | |||
| Average difference | 0,4 (-0,5 to 1,34) | -2,2 (-2,9 to -1,5) | -2,6 (-3,2 to -2) | 1,1 (0 to 2,2) | |||
| McEwen 202043 | Functional | 1 ± 2,4 | 91,8 ± 2 | 87,5 ± 1,3 | 0,9 ± 2,6 | -1,3 ± 3,1 | 3,1 ± 1,8 |
| Mechanical | 0,2 ± 2,1 | 89,9 ± 0,6 | 89,7 ± 0,4 | -0,8 ± 2,1 | 1,1 ± 2,5 | 3,2 ± 1,8 | |
| Average difference between knees | 2,1 ± 1,8 | 2,1 ± 1,7 | 2,3 ± 1,3 | 2,7 ± 1,9 | 4 ± 2,8 | 1,5 ± 1,2 |
Note: Data showing statistically significant differences are shaded in gray. The articles by Belvedere et al in 2015, Waterson et al in 2016, Seon et al in 2017, and Sarzaeem et al in 2021 do not include radiological results. Additionally, the radiological results from Young et al in 2020 are the same as those published in 2017, so they are not included in the table to avoid duplicating information.
Table VII. Radiological results of observational studies.9,17,18,31,46,49,52–55.
| Author and year | Method | HKA (º) | mLDFA (º) | MPTA (º) | JLOA (º) | Femoral rotation (º) | Tibial Slope (º) |
|---|---|---|---|---|---|---|---|
| Blakeney 201917 | Kinematic | 0 ± 3.3 | 1 ± 2.8 | ||||
| Mechanical | − 0.5 ± 2.3 | −2 ± 2.0 | |||||
| An 201918 | Kinematic | 1,5 ± 0,2 | |||||
| Mechanical | 0,8 ± 0,2 | ||||||
| Jeremić 202046 | Kinematic | −0.2 ± 3.6 | 88.5◦ ± 3.5 | 88.4 ± 2.1 | |||
| Mechanical | −0.3 ± 2.7 | 89.9 ± 2.8 | 89.0 ± 2.1 | ||||
| Abhari 202149 | Kinematic (1-5º varus) | 2 ± 0,2 | 88 ± 0,12 | ||||
| Kinematic (6-10º varus) | 3 ± 0,2 | 88 ± 0,1 | |||||
| Kinematic (11-14º varus) | 4 ± 0,2 | 87 ± 0,2 | |||||
| Mechanical | NA | ||||||
| Sappey-Marinier 202231 | Mechanical | 1 ± 4 | 90 ± 2 | 90 ± 1 | -0,3 ± 3 | ||
| Difference after reintervention (Mechanical to Kinematic) | -1 ± 2 | 88 ± 3 | 88 ± 2 | 1 ± 3 | |||
| Winnock de Grave 20229 | Inverted kinematic | -1,7 ± 2,1 | 88,8 ± 1,4 | 87,1 ± 1,4 | -0,7 ± 2,1 | 4,2 ± 1,2 | |
| Mechanical (adjusted) | -0,4 ± 1,9 | 90 ± 1,6 | 89,6 ± 0,9 | 2,2 ± 2,5 | 4,1 ± 1,6 | ||
| Choi 202252 | Functional (robotic) | 1,1 ± 1,8 | 83,7 ± 2,1 | 89,2 ± 1 | 2,6 ± 2 | ||
| Mechanical (manual) | -0,2 ± 2,5 | 83,3 ± 2,2 | 89,6 ± 1,7 | 3,1 ± 2,1 | |||
| Lung 202253 | Kinematic | -0,7 ± 3,1 | 88,1 ± 2,6 | 88,6 ± 1,8 | -1,5 ± 2 | ||
| Mechanical | 0,3 ± 4,1 | 90,2 ± 2,2 | 90,3 ± 1,2 | 0,2 ± 1,3 | |||
| Ma 202254 | Restrictive kinematic | 0,8 ± 2,7 | 90,5 ± 1,8 | 89,7 ± 1,9 | |||
| Mechanical | 2 ± 4 | 91,5 ± 3,3 | 89,4 ± 2,5 | ||||
| Wen 202355 | Kinematic | -2,7 ± 1,9 | |||||
| Mechanical | -2,2 ± 1,4 |
Note: Data showing statistically significant differences are shaded in gray. The articles by Luceri et al in 2020, Alexander et al in 2022, and Elbuluk et al in 2022 do not include radiological results. The article by Sappey Marinier et al in 2022 provides results comparing the knees that underwent mechanical alignment intervention with the contralateral non-intervened knee.
Demographic data.
Functional assessment scale outcomes.
Radiological outcomes.
In response to the objectives set at the beginning of the review, the first objective was to assess whether MA improves implants lifespan compared to KA. Articles reviewing patients over extended follow-up periods (Seon et al. 2017, Yeo et al. 2019, and Young et al. 2020, with follow-up times of 8, 8, and 5 years respectively) did not find statistically significant differences in terms of early prosthetic loosening.39,42,44 Furthermore, Laende et al. specifically measured prosthetic component wear two years after the intervention and found no significant differences between patient groups operated on with both methods.41
Regarding patient satisfaction, there were inconclusive results, as reflected in Tables III and IV. However, all articles that found significant differences in functional assessment scales favoured KA or FA over MA, leading to increased satisfaction.
Another theoretical advantage of KA was achieving earlier recovery by respecting the patient’s constitutional biomechanics. Some articles attempted to objectively measure this improvement in recovery speed by calculating the distance patients walked on the hospital floor before discharge. One article found no statistically significant differences between alignment methods,33 but it’s worth noting that two other articles indicated a greater distance walked by kinematically aligned patients.35,53
Another objective was to assess postoperative joint stability (Table V), for which no differences were found between the two groups (MA and KA) in the number of patients reporting instability after surgery9,14,35,38,42,49,54 despite several articles noting that ligament and tendon release was more pronounced in MA than in KA.18,40,41,43 Additionally, three articles reported cases of patellar instability: Two cases were reported by Dossett et al., one in the MA group and one in the KA group; Young et al. also reported one case in each group, and Abhari et al. reported only one case in the MA group. Therefore, no differences in patellofemoral stability can be concluded.33,40,49 Regarding other alignment methods, McEwen at al. found statistically significant differences in lateral extension gap (LEG) in favor of FA.43 In Winnock de Grave et al.’s 2022 study, which compared adjusted mechanical alignment with inverted kinematic alignment (iKA), no soft tissue release was required for any of the patients.9 In Yim et al.’s 2013 study, comparing AA and MA, no results of tendon releases were reported, but postoperative joint laxity was measured, with no differences between the two methods.34
Regarding radiological results, as seen in Tables VI and VII, different alignment methods lead to differences in coronal plane knee angles but not in the sagittal plane (except for the Young et al. 2017 study). All studies met a mean mLDFA > 82° and a mean MTPA > 87°, so the resulting mean alignment from all alignment methods in all studies falls within the “precaution zone”, outside of which early prosthetic component wear is usually observed.56,57
In the two trials comparing AA with MA, radiological results differed between the two methods, but no improvements in functional outcomes were observed for either method.34,42
One study comparing FA with MA showed, in addition to radiological differences, improvements in WOMAC, FJS, and the functional part of the KSS questionnaire in the FA group. However, no differences were found in the KSS questionnaire part related to pain and stability.52
Another article that used the iKA showed radiological differences, but in terms of satisfaction and functional results, superiority of inverted kinematic alignment was demonstrated only in patients with varus deformity (HKA <177°) after multivariate analysis.9
The study comparing RKA with MA showed better functional results for RKA in the WOMAC, KSS, and FJS questionnaires, with no differences in range of motion.49
Ultimately, no significant differences in postoperative complication rates were found among the analysed methods.
DISCUSSION
Regarding implants lifespan, the results observed in this review do not support the theoretical advantage of MA. Therefore, this finding provides reassurance when applying KA, as it was one of the main concerns raised. The maximum follow-up period recorded in the articles of this review is eight years, so future studies with longer follow-up periods are necessary to fully support the idea that component wear is not greater in KA than in MA. However, in this review, this equality of results is observed in terms of prosthetic wear-related consultations. The article that quantitatively measured polyethylene wear did so after two years of follow-up,41 so the evidence provided in this review regarding the equality of component wear between KA and MA is limited, and more long-term quantitative results are needed to confirm it. Moreover, all studies met a mean mLDFA > 82° and a mean MTPA > 87°. These results explain the lack of differences in terms of early prosthetic loosening since other studies defined an increased loosening rate with a tibial varus deviation of more than 3°56 and a femoral valgus deviation of more than 8°.57
Furthermore, the main finding of this review is that, despite conflicting results, there is a trend towards better clinical outcomes in patients with kinematically aligned knee prostheses compared to those using the traditional MA approach, with no differences in complication rates observed. Other reviews and meta-analyses support this finding.58–66 It should be noted that errors have been identified in Liu’s meta-analysis regarding the data from HKA and TS from Yeo et al. 2019, where MA data were mistakenly assigned to AA and vice versa,63 upon comparison with the original article.42
In terms of knee stability, some authors argue that the reduced ligament release in KA leads to less inflammation and faster recovery.18,35 However, inconclusive results are found in the articles included in the review.
Regarding functional alignment, McEwen’s clinical trial found differences in terms of radiological outcomes compared to the MA. Additionally, differences in terms of LEG are described in the stability assessment.43 Choi et al.’s article demonstrates slight functional advantages in FA application. However, the FA group underwent robotic surgery, while the MA group underwent conventional surgery.52 Therefore, in future clinical trials, comparing FA with MA should be conducted under similar intervention conditions to appreciate the potential improvements offered by alignment type and robotic approach separately. In this context, MacDessi et al. propose a protocol for future clinical trials to compare two alignment methods and conventional surgery versus robotic surgery in a factorial manner, allowing the interpretation of alignment method and robotic results independently.67
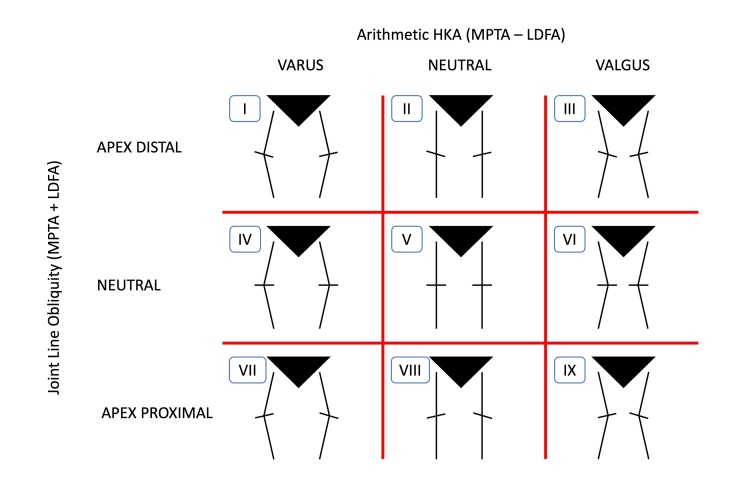
Another important point introduced by Choi et al.’s article is the assessment of patient knee phenotypes. In 2019, Hirschmann et al. described a new classification of knee joint phenotypes, as the conventional classification into varus, neutral, or valgus only considers limb deviation from the frontal plane without accounting for the orientation of the joint line to the ground, which also influences knee and limb mechanics. In addition to considering the angle relative to the mechanical axis (HKA), they consider angles between the femoral axis and the joint line (mLDFA) and between the tibial axis and the joint line (MPTA, also occasionally abbreviated as TMA). In the case of Hirschmann et al., the medial version of mLDFA (Femoral Mechanical Angle, FMA) is used instead of mLDFA.68 As a reference value, RKA considers HKA values of 180° ± 3°, mLDFA 90° ± 5°, and MPTA 90 ± 5° as falling within the “precaution zone”, which are considered neutral values. Any deviation greater than this is considered valgus or varus (although the limits of neutrality vary among authors and there is no definitive consensus). In this way, 27 different phenotypes are described, depending on the combinations of HKA, FMA, and TMA, with all three angles being varus, neutral, or valgus. In summary, 9 phenotypes are considered, considering only limb deviation from the mechanical axis (HKA) and the angle of the joint line relative to the ground (JLOA).69 (Figure 5)
Figure 5. Schematic representation of knee phenotypes based on HKA and JLOA.69.
In the ongoing pursuit of personalized medicine, it is foreseeable that adapting alignment methods to each patient’s characteristics will be implemented if it proves superior to conventional methods. For example, KA could be advantageous in phenotypes I, II, IV, and V, which are varus or neutral deviations supported by clinical trials with KA; RKA could be suitable for phenotypes III and VI, as valgus deviations often lead to exclusion criteria in KA trials,38,42,43,45,49,51,55 going beyond the previously mentioned “precaution zone”; and MA might be indicated for phenotypes VII, VIII, and IX, which are less common in the population and involve more extreme deformities.69
Although recent articles report results based on phenotypes,70 future trials should be designed to compare alignment method results and phenotypes separately, like the previously mentioned MacDessi et al. protocol.67
In addition to the brief follow-up period to determine potential long-term prosthetic wear, another major limitation of this review is the heterogeneity in KA techniques, as some studies use patient-specific instruments, others use conventional methods, and some employ robotic surgery. This limitation is shared with other reviews and meta-analyses.58,59
In conclusion, regarding the comparison of the most used alignment methods, mechanical and kinematic, while not all studies observe functional or patient satisfaction differences, those that do find such differences favor KA. It should be emphasized that these differences have been observed under clinical trial conditions with rigorous inclusion and exclusion criteria. As noted earlier, valgus deformity was an exclusion criterion in 7 articles,38,42,43,45,49,51,55 but patients with deviations of more than 10° in the coronal plane, BMI greater than 40 kg/m2, or prior knee surgeries were also frequently excluded.
It would be interesting to conduct studies with more relaxed inclusion and exclusion criteria, more closely resembling routine surgical practice, and with a longer follow-up period, to fully confirm the advantage of KA in terms of functional outcomes. Furthermore, presenting results based on patients’ knee phenotypes could help determine whether one alignment method is superior for a specific knee phenotype.
CONCLUSION
No greater wear or early loosening of components in kinematically aligned prostheses was observed two years post-surgery compared to mechanically aligned prostheses. To objectively assess component wear equality between both methods, studies analyzing quantitative prosthesis thickness over a longer time period are needed.
KA is superior in certain cases in terms of patient functionality and reduced pain, but it does not seem sufficient to explain the 20% of patients dissatisfied after TKA.
Despite greater ligament and tendon release in MA, this does not translate into differences in consultations for femorotibial or femoropatellar instability following surgical intervention.
Although KA shows superiority in functional and patient satisfaction results in several included studies, it must be considered that study conditions do not accurately mirror real-world surgical conditions. Further studies are necessary to ascertain the reproducibility of the promising clinical outcomes documented by these articles.
CONTRIBUTIONS
Juan Segura-Nuez: main and corresponding author, study design, introduction, literature search, acquisition and analysis of abstracts, result analysis, writing, table design, discussion.
Carlos Martín-Hernández: introduction, study design, literature search, final decision in disagreement, writing, discussion.
Julián Carlos Segura-Nuez: literature search, acquisition and analysis of abstracts, result analysis, figure design, discussion.
Julián Carlos Segura-Mata: study design, introduction, discussion.
DISCLOSURE OF INTEREST
The authors declare no conflicts of interest.
Funding Statement
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- Estudio multicéntrico sobre la incidencia de infección en prótesis de rodilla. Jaén F., Sanz-Gallardo M. I., Arrazola M. P., García de Codes A., De Juanes A., Resines C. 2012Rev Esp Cir Ortop Traumatol. 56(1):38–45. doi: 10.1016/j.recot.2011.08.001. [DOI] [PubMed] [Google Scholar]
- Patients’ expectations impact their satisfaction following total hip or knee arthroplasty. Neuprez A., Delcour J. P., Fatemi F., Gillet P., Crielaard J. M., Bruyère O.., et al. 2016PLoS One. 11(12):1–14. doi: 10.1371/journal.pone.0167911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patients’ expectations and satisfaction with total hip arthroplasty. Mancuso C. A., Salvati E. A., Johanson N. A., Peterson M. G. E., Charlson M. E. Jun;1997 J Arthroplasty. 12(4):387–96. doi: 10.1016/S0883-5403(97)90194-7. [DOI] [PubMed] [Google Scholar]
- Patient satisfaction after total knee arthroplasty. Choi Y. J., Ra H. J. 2016Knee Surg Relat Res. 28(1):1–15. doi: 10.5792/ksrr.2016.28.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tibiofemoral alignment and the results of knee replacement. Tew M, Waugh W. Aug 1;1985 Journal of Bone and Joint Surgery - Series B. 67(4):551–6. doi: 10.1302/0301-620X.67B4.4030849. [DOI] [PubMed] [Google Scholar]
- How Accurately Can Soft Tissue Balance Be Determined in Total Knee Arthroplasty? MacDessi S. J., Gharaibeh M. A., Harris I. A. Feb 1;2019 J Arthroplasty. 34(2):290–294.e1. doi: 10.1016/j.arth.2018.10.003. [DOI] [PubMed] [Google Scholar]
- Alignment in total knee arthroplasty. Correlated biomechanical and clinical observations. Bargren J. H., Blaha J. D., Freeman M. A. R. Mar 1;1983 Clin Orthop Relat Res. 173(173):178–183. doi: 10.1097/00003086-198303000-00024. [DOI] [PubMed] [Google Scholar]
- Alignment options for total knee arthroplasty: A systematic review. Rivière C., Iranpour F., Auvinet E., Howell S., Vendittoli P. A., Cobb J.., et al. 2017Orthopaedics and Traumatology: Surgery and Research. 103(7):1047–1056. doi: 10.1016/j.otsr.2017.07.010. [DOI] [PubMed] [Google Scholar]
- Higher satisfaction after total knee arthroplasty using restricted inverse kinematic alignment compared to adjusted mechanical alignment. Winnock de Grave P., Luyckx T., Claeys K., Tampere T., Kellens J., Müller J.., et al. 2022Knee Surgery, Sports Traumatology, Arthroscopy. 30(2):488–99. doi: 10.1007/s00167-020-06165-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The porous-coated anatomic total knee. Hungerford D. S., Kenna R. V., Krackow K. A. Jan;1982 Orthop Clin North Am. 13(1):103–22. doi: 10.1016/S0030-5898(20)30270-4. [DOI] [PubMed] [Google Scholar]
- Alignment and balance methods in total knee arthroplasty. Jaffe W. L., Dundon J. M., Camus T. 2018Journal of the American Academy of Orthopaedic Surgeons. 26(20):709–716. doi: 10.5435/JAAOS-D-16-00428. [DOI] [PubMed] [Google Scholar]
- Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Howell S.M., Papadopoulos S., Kuznik K.T., Hull M.L. 2013Knee Surgery, Sports Traumatology, Arthroscopy. 21(10):2271–80. doi: 10.1007/s00167-013-2621-x. [DOI] [PubMed] [Google Scholar]
- Calipered Kinematically Aligned Total Knee Arthroplasty: An Accurate Technique That Improves Patient Outcomes and Implant Survival. Howell S.M. Mar 1;2019 Orthopedics. 42(3):126–135. doi: 10.3928/01477447-20190424-02. [DOI] [PubMed] [Google Scholar]
- PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study. Calliess T., Bauer K., Stukenborg-Colsman C., Windhagen H., Budde S., Ettinger M. 2017Knee Surgery, Sports Traumatology, Arthroscopy. 25(6):1743–8. doi: 10.1007/s00167-016-4136-8. [DOI] [PubMed] [Google Scholar]
- Kinematic TKA using navigation: Surgical technique and initial results. Hutt J.R.B., LeBlanc M.A., Massé V., Lavigne M., Vendittoli P.A. Feb 1;2016 Orthop Traumatol Surg Res. 102(1):99–104. doi: 10.1016/j.otsr.2015.11.010. [DOI] [PubMed] [Google Scholar]
- Individualized alignment in total knee arthroplasty using image-based robotic assistance : Video article. Calliess T., Ettinger M., Savov P., Karkosch R., Windhagen H. Oct 1;2018 Orthopade. 47(10):871–9. doi: 10.1007/s00132-018-3637-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinematic alignment in total knee arthroplasty better reproduces normal gait than mechanical alignment. Blakeney W., Clément J., Desmeules F., Hagemeister N., Rivière C., Vendittoli P. A. 2019Knee Surgery, Sports Traumatology, Arthroscopy. 27(5):1410–7. doi: 10.1007/s00167-018-5174-1. [DOI] [PubMed] [Google Scholar]
- Kinematic alignment is bone and soft tissue preserving compared to mechanical alignment in total knee arthroplasty. An V. V. G., Twiggs J., Leie M., Fritsch B. A. 2019Knee. 26(2):466–76. doi: 10.1016/j.knee.2019.01.002. [DOI] [PubMed] [Google Scholar]
- Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Hirschmann M. T., Moser L. B., Amsler F., Behrend H., Leclerq V., Hess S. 2019Knee Surgery, Sports Traumatology, Arthroscopy. 27(5):1394–1402. doi: 10.1007/s00167-019-05509-z. [DOI] [PubMed] [Google Scholar]
- La alineación de la artroplastia de rodilla. Antiguos mitos y nuevas controversias. Hernández-Vaquero D. 2021Rev Esp Cir Ortop Traumatol. 65(5):386–97. doi: 10.1016/j.recot.2021.01.002. [DOI] [Google Scholar]
- Alignment in total knee arthroplasty. Oussedik S., Abdel M. P., Victor J., Pagnano M. W., Haddad F. S. 2020Bone Joint J. 102-B(3):276–9. doi: 10.1302/0301-620X.102B3.BJJ-2019-1729. [DOI] [PubMed] [Google Scholar]
- Functional alignment achieves a more balanced total knee arthroplasty than either mechanical alignment or kinematic alignment prior to soft tissue releases. Clark G., Steer R., Wood D. 2022Knee Surgery, Sports Traumatology, Arthroscopy. doi: 10.1007/s00167-022-07156-3. [DOI] [PMC free article] [PubMed]
- Joint line is restored in robotic-arm-assisted total knee arthroplasty performed with a tibia-based functional alignment. Zambianchi F., Bazzan G., Marcovigi A., Pavesi M., Illuminati A., Ensini A.., et al. Dec 1;2021 Arch Orthop Trauma Surg. 141(12):2175–84. doi: 10.1007/s00402-021-04039-z. [DOI] [PubMed] [Google Scholar]
- The language of knee alignment updated definitions and considerations for reporting outcomes in total knee arthroplasty. MacDessi S.J., Oussedik S., Abdel M.P., Victor J., Pagnano M.W., Haddad F.S. Feb 1;2023 Bone and Joint Journal. 105 B(2):102–8. doi: 10.1302/0301-620X.105B2.BJJ-2022-1345. [DOI] [PubMed] [Google Scholar]
- SEROD: Cuestionarios. Sociedad Española de la Rodilla; [2017]. https://www.serod.org/koos/ [Google Scholar]
- OrthoToolKit: Knee Society Score. https://orthotoolkit.com/knee-society-score/
- Shrewsbury and Telford Hospital . National Health Service. Department of Public Health, University of Oxford; Oxford: https://www.sath.nhs.uk/wp-content/uploads/2016/08/gpinfo_OxfordKneeScore.pdf [Google Scholar]
- Giglio Pedro. Pedrogiglio Ortopedista Especialista em Joelho. Pedro Giglio; São Paulo: [2021]. https://pedrogiglio.com/artrofibrose-do-joelho/ [Google Scholar]
- The “Forgotten Joint” as the Ultimate Goal in Joint Arthroplasty. Validation of a New Patient-Reported Outcome Measure. Behrend H., Giesinger K., Giesinger J. M., Kuster M. S. 2012Journal of Arthroplasty. 27(3):430–6. doi: 10.1016/j.arth.2011.06.035. [DOI] [PubMed] [Google Scholar]
- SEROD: Cuestionarios. Sociedad Española de la Rodilla; https://www.serod.org/womac/ [Google Scholar]
- Kinematic Alignment of Failed Mechanically Aligned Total Knee Arthroplasty Restored Constitutional Limb Alignment and Improved Clinical Outcomes: A Case Report of 7 Patients. Sappey-Mariner E., Wu S. A., Bini S. A. 2022J Pers Med. 12(11):15–20. doi: 10.3390/jpm12111780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ángulo de pendiente tibial posterior “Slope” en prótesis total de rodilla. Diferencias entre alineación Intra o Extramedular y su repercusión sobre el rango de movilidad postoperatorio. Cruzado B., Mifsut D., Silvestre A. 2019Revista Española de Cirugía Osteoarticular. 54:143–8. [Google Scholar]
- Kinematically versus mechanically aligned total knee arthroplasty. Dossett H. G., Swartz G. J., Estrada N. A., Lefevre G. W., Kwasman B. G. 2012Orthopedics. 35(2):160–9. doi: 10.3928/01477447-20120123-04. [DOI] [PubMed] [Google Scholar]
- A comparison of classical and anatomical total knee alignment methods in robotic total knee arthroplasty. Classical and anatomical knee alignment methods in TKA. Yim J. H., Song E. K., Khan M. S., Sun Z. hui, Seon J. K. 2013Journal of Arthroplasty. 28(6):932–7. doi: 10.1016/j.arth.2013.01.013. [DOI] [PubMed] [Google Scholar]
- A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Dossett H. G., Estrada N. A., Swartz G. J., LeFevre G. W., Kwasman B. G. Jul;2014 Bone Joint J. 96-B(7):907–913. doi: 10.1302/0301-620X.96B7.32812. [DOI] [PubMed] [Google Scholar]
- Better joint motion and muscle activity are achieved using kinematic alignment than neutral mechanical alignment in total knee replacement. Belvedere C., Tamarri S., Ensini A., Caravaggi P., Ortolani M., Lullini G.., et al. 2015Gait Posture. 42:19–20. doi: 10.1016/j.gaitpost.2015.07.043. [DOI] [Google Scholar]
- The early outcome of kinematic versus mechanical alignment in total knee arthroplasty: a prospective randomised control trial. Waterson H. B., Clement N. D., Eyres K. S., Mandalia V. I., Toms A. D. Oct;2016 Bone Joint J. 98-B(10):1360–8. doi: 10.1302/0301-620X.98B10.36862. [DOI] [PubMed] [Google Scholar]
- Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Matsumoto T., Takayama K., Ishida K., Hayashi S., Hashimoto S., Kuroda R. 2017Bone and Joint Journal. 99B(5):640–6. doi: 10.1302/0301-620X.99B5.BJJ-2016-0688.R2. [DOI] [PubMed] [Google Scholar]
- Comparison of Outcome and Gait Analysis after Robotic Total Knee Arthroplasty Between Mechanical and Kinematic Knee Alignment Methods with Average 8 Years Follow Up. Seon J. K., Song E. K., Lee D. H., Yeo J. H., Jin C. 2017Arthroscopy: The Journal of Arthroscopic & Related Surgery. 33(10):150–1. doi: 10.1016/j.arthro.2017.08.189. [DOI] [Google Scholar]
- The Chitranjan S. Ranawat Award: No Difference in 2-year Functional Outcomes Using Kinematic versus Mechanical Alignment in TKA: A Randomized Controlled Clinical Trial. Young S.W., Walker M.L., Bayan A., Briant-Evans T., Pavlou P., Farrington B. 2017Clin Orthop Relat Res. 475(1):9–20. doi: 10.1007/s11999-016-4844-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- A randomized controlled trial of tibial component migration with kinematic alignment using patient-specific instrumentation versus mechanical alignment using computer-assisted surgery in total knee arthroplasty. Laende E. K., Richardson C. G., Dunbar M. J. 2019Bone and Joint Journal. 101 B(8):929–40. doi: 10.1302/0301-620X.101B8.BJJ-2018-0755.R3. [DOI] [PubMed] [Google Scholar]
- No difference in outcomes and gait analysis between mechanical and kinematic knee alignment methods using robotic total knee arthroplasty. Yeo J. H., Seon J. K., Lee D. H., Song E. K. 2019Knee Surgery, Sports Traumatology, Arthroscopy. 27(4):1142–7. doi: 10.1007/s00167-018-5133-x. [DOI] [PubMed] [Google Scholar]
- Computer-Assisted Kinematic and Mechanical Axis Total Knee Arthroplasty: A Prospective Randomized Controlled Trial of Bilateral Simultaneous Surgery. McEwen P. J., Dlaska C. E., Jovanovic I. A., Doma K., Brandon B. J. 2020Journal of Arthroplasty. 35(2):443–50. doi: 10.1016/j.arth.2019.08.064. [DOI] [PubMed] [Google Scholar]
- No Difference in 5-year Clinical or Radiographic Outcomes between Kinematic and Mechanical Alignment in TKA: A Randomized Controlled Trial. Young S. W., Sullivan N. P. T., Walker M. L., Holland S., Bayan A., Farrington B. 2020Clin Orthop Relat Res. 478(6):1271–9. doi: 10.1097/CORR.0000000000001150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comparison of pain and Oxford score of patients who underwent TKA with two methods of mechanical and kinematic alignment techniques. Sarzaeem M. M., Rasi A. M., Omrani F. A., Darestani R. T., Barati H., Moghaddam A. N.., et al. 2021Pakistan Journal of Medical and Health Sciences. 15(1):665–670. [Google Scholar]
- Short-term follow-up of kinematically vs. mechanically aligned total knee arthroplasty with medial pivot components: A case-control study. Jeremić D. V., Massouh W. M., Sivaloganathan S., Rosali A. R., Haaker R. G., Rivière C. Sep 1;2020 Orthopaedics & Traumatology: Surgery & Research. 106(5):921–7. doi: 10.1016/j.otsr.2020.04.005. [DOI] [PubMed] [Google Scholar]
- Kinematic versus mechanical alignment in total knee arthroplasty: A preliminary study. Luceri F., Sosio C., Sirtori P., Battistella D., Zuffada M., Ulivi M.., et al. 2020J Biol Regul Homeost Agents. 34(4):139–143. [PubMed] [Google Scholar]
- Outcomes in Patients with a Calipered Kinematically Aligned TKA That Already Had a Contralateral Mechanically Aligned TKA. Shelton T. J., Gill M., Athwal G., Howell S. M., Hull M. L. Jan 1;2021 Journal of Knee Surgery. 34(1):87–93. doi: 10.1055/s-0039-1693000. [DOI] [PubMed] [Google Scholar]
- Patient satisfaction following total knee arthroplasty using restricted kinematic alignment. Abhari S., Hsing T.M., Malkani M.M., Smith A.F., Smith L.S., Mont M.A.., et al. 2021Bone and Joint Journal. 103-B(7):59–66. doi: 10.1302/0301-620X.103B6.BJJ-2020-2357.R1. [DOI] [PubMed] [Google Scholar]
- Influence of Kinematic Alignment on Soft Tissue Releasing and Manipulation Under Anesthesia Rates in Primary Total Knee Arthroplasty. Alexander J. S., Morris M. J., Lombardi, Jr A. V., Berend K. R., Crawford D. A. Surgical Technology Online. 2022:41. doi: 10.52198/22.STI.41.OS1641. [DOI] [PubMed] [Google Scholar]
- Head-to-Head Comparison of Kinematic Alignment Versus Mechanical Alignment for Total Knee Arthroplasty. Elbuluk A. M., Jerabek S. A., Suhardi V. J., Sculco P. K., Ast M. P., Vigdorchik J. M. 2022Journal of Arthroplasty. 37(8):849–51. doi: 10.1016/j.arth.2022.01.052. [DOI] [PubMed] [Google Scholar]
- Functional alignment with robotic arm assisted total knee arthroplasty demonstrated better patient-reported outcomes than mechanical alignment with manual total knee arthroplasty. Choi B. S., Kim S. E., Yang M., Ro D. H., Han H. S. 2022Knee Surgery, Sports Traumatology, Arthroscopy. 31(3):1072–80. doi: 10.1007/s00167-022-07227-5. [DOI] [PubMed] [Google Scholar]
- Kinematic Alignment May Reduce Opioid Consumption and Length of Stay Compared to Mechanically Aligned Total Knee Arthroplasty. Lung B.E., Donnelly M.R., McLellan M., Callan K., Amirhekmat A., McMaster W.C.., et al. 2022Orthop Surg. 15(2):432–9. doi: 10.1111/os.13605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Computer Navigation Assisted Restricted Kinematic Alignment Improves Short-Term Outcomes in Total Knee Arthroplasty: An Ambispective Cohort Study. Ma R., Chen X., Li H., Wang Y., Li S., Li S.., et al. 2022Orthop Surg. 15(2):460–470. doi: 10.1111/os.13603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- An early clinical comparative study on total knee arthroplasty with kinematic alignment using specific instruments versus mechanical alignment in varus knees. Wen L., Wang Z., Ma D., Zhao X. 2023Front Surg. 9(January):1–8. doi: 10.3389/fsurg.2022.1097302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Chetranjan Ranawat Award: Tibial Component Failure Mechanisms in Total Knee Arthroplasty. Berend M. E., Ritter M. A., Meding J. B., Faris P. M., Keating E. M., Redelman R.., et al. 2004Clin Orthop Relat Res. 428(Nov):26–34. doi: 10.1097/01.blo.0000148578.22729.0e. [DOI] [PubMed] [Google Scholar]
- The Effect of Alignment and BMI on Failure of Total Knee Replacement. Ritter M. A., Davis K. E., Meding J. B., Pierson J. L., Berend M. E., Malinzak R. A. Sep 7;2011 Journal of Bone and Joint Surgery. 93(17):1588–1596. doi: 10.2106/JBJS.J.00772. [DOI] [PubMed] [Google Scholar]
- Early Outcomes of Kinematic Alignment in Primary Total Knee Arthroplasty: A Meta-Analysis of the Literature. Courtney P.M., Lee G.C. 2017Journal of Arthroplasty. 32(6):2028–2032.e1. doi: 10.1016/j.arth.2017.02.041. [DOI] [PubMed] [Google Scholar]
- Comparison of kinematic and mechanical alignment techniques in primary total knee arthroplasty. Yoon J.R., Han S.B., Jee M.K., Shin Y.S. 2017Medicine (United States) 96(39):1–9. doi: 10.1097/MD.0000000000008157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Lee Y. S., Howell S. M., Won Y. Y., Lee O. S., Lee S. H., Vahedi H.., et al. 2017Knee Surgery, Sports Traumatology, Arthroscopy. 25(11):3467–79. doi: 10.1007/s00167-017-4558-y. [DOI] [PubMed] [Google Scholar]
- Comparison of Kinematic Alignment and Mechanical Alignment in Total Knee Arthroplasty: A Meta-analysis of Randomized Controlled Clinical Trials. Gao Z. Xiang, Long N. Ji, Zhang S. Yun, Yu W., Dai Y. Xin, Xiao C. 2020Orthop Surg. 12(6):1567–78. doi: 10.1111/os.12826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clinical outcomes of kinematic alignment versus mechanical alignment in total knee arthroplasty: A systematic review. Roussot M. A., Vles G. F., Oussedik S. 2020EFORT Open Rev. 5(8):486–97. doi: 10.1302/2058-5241.5.190093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinematic alignment versus mechanical alignment in primary total knee arthroplasty: an updated meta-analysis of randomized controlled trials. Liu B., Feng C., Tu C. 2022J Orthop Surg Res. 17(1):1–18. doi: 10.1186/s13018-022-03097-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Similar results with kinematic and mechanical alignment applied in total knee arthroplasty. Luo Z., Zhou K., Peng L., Shang Q., Pei F., Zhou Z. 2020Knee Surgery, Sports Traumatology, Arthroscopy. 28(6):1720–1735. doi: 10.1007/s00167-019-05584-2. [DOI] [PubMed] [Google Scholar]
- Kinematic alignment versus mechanical alignment in total knee arthroplasty: An up-to-date meta-analysis. Tian G, Wang L, Liu L, Zhang Y, Zuo L, Li J. 2022Journal of Orthopaedic Surgery. 30(3):1–11. doi: 10.1177/10225536221125952. [DOI] [PubMed] [Google Scholar]
- Kinematic alignment results in clinically similar outcomes to mechanical alignment: Systematic review and meta-analysis. Van Essen J., Stevens J., Dowsey M. M., Choong P. F., Babazadeh S. 2023Knee. 40:24–41. doi: 10.1016/j.knee.2022.11.001. [DOI] [PubMed] [Google Scholar]
- Robotic-assisted surgery and kinematic alignment in total knee arthroplasty (RASKAL study): a protocol of a national registry-nested, multicentre, 2×2 factorial randomised trial assessing clinical, intraoperative, functional, radiographic and survivorship. MacDessi S. J., Wernecke G. C., Bastiras D., Hooper T., Heath E., Lorimer M.., et al. 2022BMJ Open. 12(6):67. doi: 10.1136/bmjopen-2021-051088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Restricted Inverse Kinematic Alignment Better Restores the Native Joint Line Orientation While Achieving Similar Balance, Laxity, and Arithmetic Hip-Knee-Ankle Angle to Gap Balancing Total Knee Arthroplasty. Orsi A. D., Wakelin E., Plaskos C., McMahon S., Coffey S. 2023Arthroplast Today. 19 doi: 10.1016/j.artd.2022.101090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coronal Plane Alignment of the Knee (CPAK) classification a new system for describing knee phenotypes. MacDessi S. J., Griffiths-Jones W., Harris I. A., Bellemans J., Chen D. B. 2021Bone and Joint Journal. 103 B(2):329–37. doi: 10.1302/0301-620X.103B2.BJJ-2020-1050.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clinical and Radiographic Outcomes of Inversed Restricted Kinematic Alignment Total Knee Arthroplasty by Asia Specific (Huang’s) Phenotypes, a Prospective Pilot Study. Hsieh S. L., Lin T. L., Hung C. H., Fong Y. C., Chen H. T., Tsai C. H. 2023J Clin Med. 12(6):2110. doi: 10.3390/jcm12062110. [DOI] [PMC free article] [PubMed] [Google Scholar]