Twenty years ago the secretary of state for social services of the last Labour government appointed Sir Douglas Black to chair a working group to review information on inequalities in health and suggest policy and research that should follow from this review.1 The report appeared in 1980 and received a cold reception from the new Conservative government.2 The climate for the reception of the Black report’s successor—the independent inquiry into inequalities in health, chaired by Sir Donald Acheson and published this week3—is hopefully different. How do its findings and recommendations compare?
For 17 years of Conservative government the Labour party made political capital out of the non-implementation of the recommendations of the Black report. The announcement before the 1997 election that, if elected, Labour would commission an independent review into inequalities in health was therefore welcome.4 When launching the inquiry in July 1997 the minister for public health criticised the health strategy of the previous administration for “its excessive emphasis on lifestyle issues” which “cast the responsibility back on to the individual.”5 Given the history of the Black report—released with no press release and only 260 copies—the commitment to publish the new report was encouraging, as was the statement that “its conclusions, based on evidence, will contribute to the development of a new strategy for health.”3 The review’s terms of reference, however, included the stipulation that it must be conducted within the broad framework of the government’s overall financial strategy,3 which placed unclear constraints on what it could say.
The eagerly awaited report marshals evidence from an impressive list of institutional and individual contributors and synthesises this into a comprehensive review of current knowledge on the extent and trends of inequalities in health and the determinants of health.3 This complements the equally impressive work of the Social Exclusion Unit in its recent report on the condition of our poorest neighbourhoods in demonstrating the costs of 20 years of growing social inequality in Britain.6 Indeed, a closer link between the independent inquiry and the Social Exclusion Unit might have increased the influence of the inquiry’s recommendations, given that the latter has committed substantial resources to a long term integrated attack on poverty.
The Black report’s recommendations were not implemented, but it stimulated extensive international research into inequalities in health.2,7 Since the new report should lead to policy rather than further research, its recommendations are key. Interestingly the new inquiry follows the Black report in focusing on early life. The Black committee considered that the “preventive way to attack [inequalities in health] is in childhood and, in the light of massive research, the first years of life.”8 The extensive research on the origins of disease in early life since Black9,10 has reinforced this conclusion.
The contested recommendations of the Black report were centred on a comprehensive antipoverty programme with two key elements: a fairer distribution of resources and the provision of the necessary educational and employment opportunities for active social participation.1 The recommendations were targeted at the fundamental causes of inequalities in health, formulated in considerable detail and costed. In contrast the new independent inquiry advances 39 main recommendations for reducing inequalities in health. These contain some focused policies which should receive wide support and which could be implemented tomorrow—such as nicotine replacement therapy being made available on prescription. However, the format of the recommendations is more like that of a shopping list than of a health strategy. There are several reasons for, and consequences of, this.
Firstly, the recommendations are not presented in any hierarchy, and the key fact that inequalities in health follow closely on inequalities in wealth is underemphasised. The one (of 39) set of recommendations on the need to reduce poverty and income inequalities thus appears to have the same status as the recommendations on curbing traffic. The fundamental role of inequalities in material circumstances in producing the inequalities in other exposures is therefore missed, and it is possible that many of the recommendations could be adopted—at least nominally—without addressing the underlying determinants of health inequalities.
Secondly, some of the recommendations are simply too vague to be useful. Recommending “measures to prevent suicide among young people” or “policies to reduce the fear of crime and violence” would receive universal support but are of little use if it is not specified how these things are to be brought about. For example, the report advocates the development of a high quality affordable public transport system and specifically refers to the large relative increases in rail fares compared with motoring costs, but it fails to make the obvious link with the privatisation of the railways and the deteriorating service and increasing costs which have followed from the elementary logic that the creation of short term profits depends on emptying the purses of those who depend on, or chose, public transport.
Thirdly, the recommendations are not costed and therefore it is impossible to weigh up the costs of their implementation, the predicted social benefits which would follow, and the opportunity costs of not investing in other areas. When the Black report recommendations were rejected for being unaffordable the costing exercise showed that the costs of the central component of abolishing child poverty—£1500m a year—was only 3% of the social services budget8 and that an increase of this order was not unrealistic
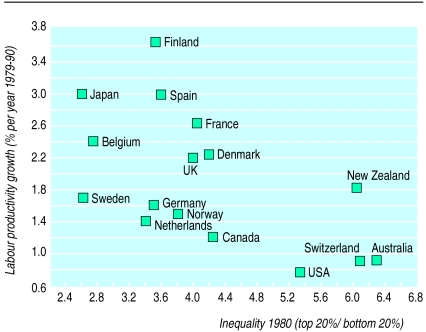
The Black report was commissioned in 1977, when inequalities in income were at a low point. In 1977 7% of the population were on incomes below half of the average after housing costs; in 1995-6 this was 24% and the arresting and then small declines in inequality seen in the early 1990s had ceased, with inequality being again on the increase.11 The same is true for health, with mortality differentials according to poverty having increased up until 1995, the latest date for which data are available.12 Unfortunately the independent inquiry was instructed not to produce targets, but the increase in inequalities in both income and mortality over the past 20 years provide evidence that these are responsive to social policy and therefore could be used for monitoring the effectiveness of policies aimed at lessening inequality. The increasing inequalities in income—which have left the United Kingdom leading the developed world in income inequality and child poverty13—started under the last Labour government, in 1977. The prime minister has declared, “I believe in greater equality. If the Labour government has not raised the living standards of the poorest by the end of its time in office it will have failed.”14 To ensure it does not fail the government should take the independent inquiry’s evidence on the importance and reversibility of health inequalities as a stimulus to introducing redistributive social policies. The government’s overall financial policy emphasises economic growth. Thus as lower levels of income inequality show no tendency to be associated with impaired growth—rather the reverse is the case (figure)15—we can be confident that implementing such an approach would produce all round benefits.
Figure.
Income inequality around 1980 and labour productivity growth from 1979 to 199015
News p 1471
References
- 1.Department of Health and Social Security. Inequalities in health: report of a research working group. London: DHSS; 1980. (Black report). [Google Scholar]
- 2.Townsend P, Davidson N, Whitehead M, editors. Inequalities in health. Harmondsworth: Penguin; 1992. [Google Scholar]
- 3.Independent inquiry into inequalities in health. London: Stationery Office; 1998. [Google Scholar]
- 4.The BMJ’s Question Time. BMJ. 1997;314:1218–1221. [PMC free article] [PubMed] [Google Scholar]
- 5.Department of Health. Public health strategy launched to tackle the root causes of ill health. London: DoH; 1997. (press release 7 July). [Google Scholar]
- 6.Social Exclusion Unit. Bringing Britain together: a national strategy for neighbourhood renewal. London: Stationery Office; 1998. [Google Scholar]
- 7.Davey Smith G, Bartley M, Blane D. The Black report on socioeconomic inequalities in health 10 years on. BMJ. 1990;301:373–377. doi: 10.1136/bmj.301.6748.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morris JN. Equalities and inequalities. BMJ. 1980;281:1003. [PMC free article] [PubMed] [Google Scholar]
- 9.Barker DJP. Mothers, babies and health in later life. Edinburgh: Churchill Livingstone; 1998. [Google Scholar]
- 10.Kuh D, Ben-Shlomo Y. A lifecourse approach to chronic disease epidemiology. Oxford: OUP; 1997. [PubMed] [Google Scholar]
- 11.Department of Social Security. Households below average income 1979-1996/7. London: Stationery Office; 1998. [Google Scholar]
- 12.Davey Smith G, Dorling D, Gordon D, Shaw M. The widening health gap— what are the solutions? Bristol: Townsend Centre for International Poverty Research; 1998. [Google Scholar]
- 13.Lynch JW, Kaplan GA. Understanding how inequality in the distribution of income affects health. J Health Psychol. 1997;2:297–314. doi: 10.1177/135910539700200303. [DOI] [PubMed] [Google Scholar]
- 14.Howarth C, Kenway P, Palmer G, Street C. Key indicators of poverty and social exclusion. York: Joseph Rowntree Foundation; 1998. [Google Scholar]
- 15.Glynn A, Miliband D. Paying for inequality: the economic costs of social injustice. London: Rivers Oran Press; 1994. [Google Scholar]