Sexual problems present in various ways, many indirect or covert. Patients do not like to come straight to the point. They fear looking stupid by using wrong words, or giving offence by being too explicit, or they have no way of conceptualising what it is that is wrong. A doctor can find himself or herself fumbling around in a slightly mad conversation in which nobody understands what is being said. A common language needs to be established first, particularly in sexual medicine, followed by a good history and a careful examination, if appropriate, before an assessment of relevant management can be made. Recurrent gynaecological or urological complaints, insomnia, depression, joint pains, and other symptoms have all been used as covert presentations of sexual problems.
Useful guides
Videos
The mature couple’s guide to love and intimacy. In the series Sex, a lifelong pleasure. London: Visual Corporation (tel: 01371 873 138)
Lovers’ guide (a series introduced by Dr Andrew Stanway). London: Pickwick Video (tel: 0181 200 7000)
Books
Zilbergeld B. Men and sex: a guide to sexual fulfilment. London: Fontana, 1986
Brown P, Faulder C. Treat yourself to sex. London: Penguin, 1989
Litvinoff S. Relate guide to loving relationships. London: Ebury Press, 1992
Eid JF, Pearce CA. Making love again. Regaining sexual potency through the new injection treatment. New York: Brunner Maazel, 1993
Quilliam S. Your sexual self. London: Cassell, 1997
Once the presence of a sexual problem has been established, its severity and importance to the patient need to be understood before the most appropriate course of management can be offered. This can vary from straightforward education, by simply giving accurate information, to referral for psychiatric assessment (fortunately very rare). History taking is therefore the paramount skill underpinning decisions about management, along with forming a positive alliance with the patient. Any course of action has to have complete cooperation. Without that, the best treatment in the world may be useless.
Overall management
It is worth bearing in mind that, however obviously physical the cause of a sexual problem, there may well be psychological sequelae, if not for the patient then for his or her partner if there is one. Conversely, when the cause seems to be entirely psychological there may be hidden organic factors at work, and it would be irresponsible to miss them. Thus overall management has to take account of both aspects (exclusion of organic factors is covered later in the series).
Psychological approaches
Giving accurate information
It is useful to give accurate and relevant information. Various books and videos are available that patients may find helpful.
Some sexual problems can be solved with an in vivo anatomy lesson, especially if the patient lacks a knowledge of the basics of sexual anatomy and physiology and the normal changes of ageing. It can be particularly invaluable to a woman who has never examined herself or to a man worried about the size of his genitals.
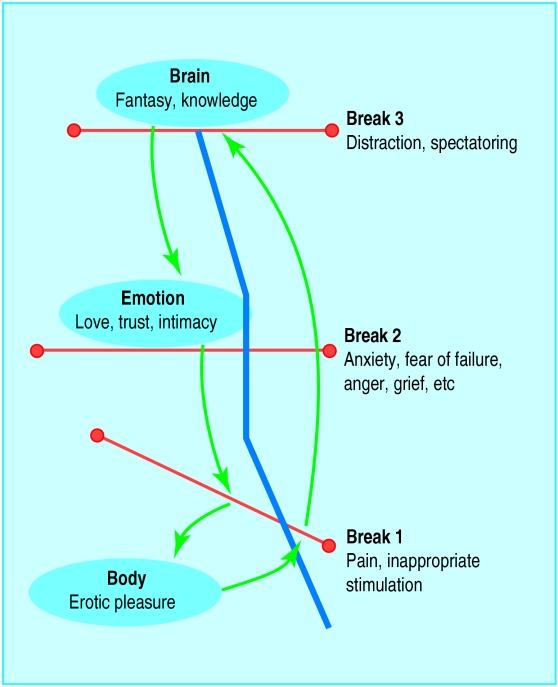
The sexual arousal circuit
A challenge to clinicians is to enable patients to understand that sexual problems happen in response to something and are not usually located solely in the genitals. Relationships, early learning about sex, trauma, and life stresses can all contribute. A diagram of the sexual arousal circuit is beneficial to show how these factors may all be linked to a sexual problem.1 When explained to patients, it can help them understand the possible roots of their problem, and thus the appropriate choices for its management.
At its simplest, sexual arousal is a straightforward spinal reflex triggered by appropriate stimulation of the body, often, but not necessarily, the genital area. This is interpreted in the brain and moderated by the emotions, so that events in those two arenas will exert a powerful influence over that reflex. Sexual response can be described as an electrical circuit that can start anywhere—mind, body, or emotion—but which also has three break points, one in each area.
The first break point occurs when there is inappropriate stimulation or pain. Pain can automatically cancel any possibility of response. Common problems are inappropriate stimulation of the clitoris and, in particular, insufficient stimulation of the penis as men get older, a point not widely appreciated.
The second break point (and probably the most powerful) occurs in the emotional arena, and a patient can be paralysed by fear of failure, anxiety, and pressure to perform. Other negative emotions important in this context include anger, unresolved conflict (in any area of life), undisclosed resentment, and grief.
The third break point occurs when the mind is too busy for the individual to relax and become aroused. An example of this, common in men with erectile dysfunction, is “spectatoring,” when the mind is focused on observing the performance of the penis to the exclusion of almost everything else. Others include distraction caused by worries about work, memories of negative experiences, expectations of failure, and uncertainty of how to behave.
General counselling
Counselling can uncover and help resolve hidden conflicts or the emotions of anger and grief long denied. Any issues about relationships may also be explored in this context, and communication between partners, often difficult in the presence of sexual problems, can be facilitated. An environment of emotional support and understanding can help patients work out their own solutions, with establishment of realistic goals and support for any changes in lifestyle.
Psychosexual therapy
The assumption underlying this therapy is that the relationship between therapist and patient provides a mirror of the relationship the patient has with his or her partner. It enables understanding of any disturbed interaction with the partner and any hidden conflicts in the patient. Initially, the doctor asks questions only when necessary, to minimise leading the patient. Medical investigations and questioning can sometimes be a way of avoiding painful and important emotional matters that the patient or the doctor may be afraid to face.
It is most important to be aware of the feelings evoked in the doctor as well as the patient as the patient’s story unfolds and the physical examination takes place. These feelings need to be discussed with the patient and can be used to inform him or her of the inner conflicts causing the difficulties. Treatment is tailored to a patient’s individual needs to enable an understanding of the unique unconscious blocks hindering sexual fulfilment.
This technique has been developed to be useful in a relatively short interview and so does not necessarily require any commitment to regular therapy sessions. Many general practitioners and some practice nurses have been trained in this approach, which lends itself well to the setting of a general practice or family planning clinic.
Behavioural approach
A man with premature ejaculation can learn to delay his ejaculation by means of a programme of graded masturbatory exercises (the squeeze technique), with or without drug treatment. The aim of the exercises is to enable the patient to recognise the feelings in his penis at different levels of arousal and, by modifying the stimulation, to learn to slow his response.
Vaginismus can also be dealt with behaviourally (see later article in this series). Patients with compulsive sexual behaviour or paraphilia are likely to be most effectively treated with a programme of behaviour modification under supervision (see later article). The behavioural approach would not ordinarily address any underlying psychological factors, but this is not always so.
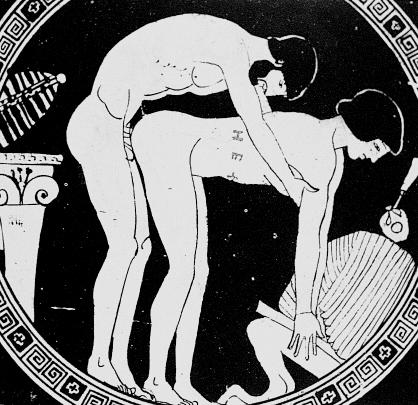
Sexual and relationship therapy
This integrated therapy incorporates psychodynamic, behavioural, cognitive, and systemic principles. The relationship may be viewed as “the patient,” rather than either partner as an individual. After thorough assessment of physical, psychological, and, particularly if a couple comes together, relationship factors, a therapeutic contract is made, with clearly stated goals if possible and sometimes a limited number of sessions. The patient or couple may agree to homework tasks to facilitate and maintain changes. Family influences and cultural and gender issues may also be seen as important, and communication between partners is often fundamental in this approach. With a sexual problem, the relationship will inevitably be affected, but this can commonly offer the very vehicle to ameliorate the situation.
Once communication between partners is open and constructive, therapeutic tasks can be assigned to them to enable them to resolve their difficulties in the privacy of their own home and at times to suit their lifestyle. It is the job of the therapist to work out with them what would be most helpful. The feedback from these tasks, together with the appropriate management of any important emotional material arising from them, provides the route whereby many sexual problems can be resolved.
Sensate focus
This is a programme of tasks, first described by Masters and Johnson in 1970,2 that a couple can undertake in their own time at home. Underlying the programme is a ban on sexual intercourse or any genital contact until anxiety about performance and fear of failure have subsided and trust between the couple has been established. This ban ensures that physical intimacy will not lead to sexual intimacy. The tasks involve the couple setting aside time to explore each other’s bodies in turn by touching, stroking, caressing, and massaging— gradually introducing sensual, then erotic, and then sexual touch over a period of time.
Sensate focus
Stage 1
1—Taking plenty of time, each person explores the other’s naked (if possible) body, avoiding breasts and genitals, avoiding trying to give pleasure, and concentrating on feelings and sensations experienced in both “active” and “passive” roles
2—After 2 weeks or 4 sessions of this, some familiarity and trust should allow inclusion of breasts and experimentation with a variety of touches, such as with body oils, talcum powder, feathers, fabrics, etc
3—As above but adding the making of specific requests for preferred types of touch and the use of a back to front position to enable the person being touched to guide the partner’s hand
Stage 2
1—Maintain the ban on intercourse, but include genital touching as part of the established exercises, so there are now no forbidden areas
2—While continuing all the above, concentrate more on the genitals to discover the sensations resulting from different pressures in different areas
3—This is an optional stage for mutual masturbation to orgasm
Stage 3
1—While continuing all the above and maintaining the ban on full intercourse, the next step is containment without movement, allowing the penis to be accepted and contained by the vagina (modified for homosexual couples). Couples should progress at their preferred pace
2—Containment with gentle thrusting and rotating movement
3—Thrusting to orgasm
The couple need to be monitored, to agree the ground rules and the staged tasks, to deal with any issues that may arise as a result of the tasks, to support positive changes and prevent relapse in the early stages.
Suggested ground rules are
• Agree a ban on sexual intercourse and genital touching
Set up twice weekly times to spend on this homework, increasing from 20 minutes to 60 minutes over 4 weeks
During these times, speak only if the partner’s touch is painful or unacceptable. Otherwise it is assumed that what is being done is all right. Conversation will prevent concentration on the task and render it pointless
Attention should be focused on personal experience, not on pleasing the partner
This is a learning exercise above all
Physical remedies
Pharmacological and surgical treatment will be covered in later articles.
Lubricants—KY Jelly and Senselle are generally well tolerated by both men and women and are available in high street stores. Carrier oils as used in aromatherapy, such as peach kernel and sweet almond oils, can be an excellent substitute for those who find water based lubricants are an irritant or messy.
Tension rings—These are useful when an adequate erection can be obtained but not sustained. A tight rubber band at the base of the penis maintains an erection for up to 30 minutes.
Vacuum pumps—These promote an erection, which a tension ring can then sustain. Pumps are available in both battery and manual forms.
Vibrators—These are available from sex shops and catalogues. The Clairol Heat Massager is obtainable from high street stores and has the advantage of being useful in other contexts. It is mains operated, which may be a further advantage.
Use of surrogates
Masters and Johnson used surrogate partners for patients who presented with sexual dysfunction but who had no partner, and Cole has described the use of surrogates in Britain.3 With a surrogate, a man might gain a sexual confidence that he could take into another relationship, but all relationships have their own chemistry and dynamic, and the erection might well not be portable. The practice was later abandoned by these workers, as complex legal, contractual, and ethical issues are raised. For example, where would responsibility lie if a patient were or became infected with HIV?
Referral onwards
Most patients with sexual problems expect to be referred on or at least investigated medically. It is very useful if the referrer has some personal knowledge or contact with the next clinician.
A list of therapists can be obtained from the Institute of Psychosexual Medicine (11 Chandos Street, London W1M 9DE) or the British Association for Sexual and Marital Therapy (PO Box 13686, London SW20 9HZ). Relate-Marriage Guidance also gives further specialised training in sexual therapy (a list of local centres can be obtained from its office at Herbert Gray College, Little Church Street, Rugby CV21 3AP).
Figure.
Man, Woman and Fish by Emily Young
Figure.
The sexual arousal circuit, a schematic representation of the factors that can positively or negatively affect the sexual response in the body, the mind, and the emotions
Figure.
The third break point in the sexual arousal circuit occurs when the mind is too busy for the individual to relax and become aroused
Figure.
Counselling can uncover and help resolve hidden conflicts or long denied anger and grief
Figure.
By modifying the stimulation in masturbatory exercises, a man with premature ejaculation can learn to slow his response. (Studies of masturbation from Love (1911) by Mihaly von Zichy)
Figure.
Partners can be assigned tasks to enable them to resolve their difficulties in the privacy of their own home (Athenian cup painting by Douris, 500-460 bc)
Figure.
In sensate focus the couple explore each other’s bodies by touching, stroking, and caressing. (Antoine et Cleopatre (c. 1602) by Agostino Carracci)
Figure.
Tension rings can maintain an erection for up to 30 minutes when placed at the base of the penis
Figure.

Carrier oils, as used in aromatherapy and massage, can be used as an alternative to water based lubricants for facilitating sexual intercourse
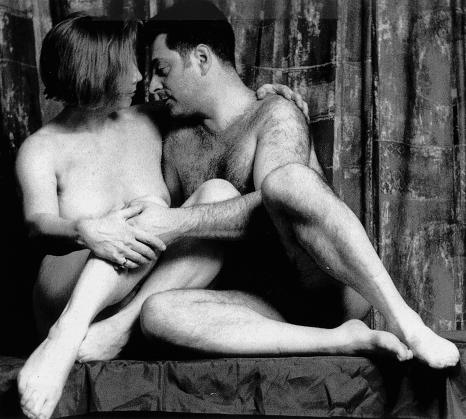
Figure.
With a surrogate partner, a man might gain sexual confidence. (Picture reproduced with subjects’ written permission)
Acknowledgments
The picture of Man, Woman and Fish is reproduced with permission of Emily Young, courtesy of the Thackeray Gallery, London (private collection). The cartoon “Sam, the ceiling needs painting” is by Neville Spearman. The photograph of the couple lying in bed is reproduced with permission of Tony Stone. The engraving by Zichy is reproduced with permission of the Bridgeman Art Library Stapleton Collection.
1 Stanley E. Principles of managing sexual problems. BMJ 1981;282:1200-2.
2 Masters WH, Johnson VE. Human sexual inadequacy. London: Churchill, 1970.
3 Cole M. Sex therapy for individuals. In: Cole M, Dryden W, eds. Sex therapy in Britain. Milton Keynes: Open University Press, 1988.
Footnotes
Margaret Ramage is tutor in human sexuality, St George’s Hospital, London, and psychosexual therapist, Wandsworth and Lambeth health authorities.
The ABC of sexual health is edited by John Tomlinson, physician at the Men’s Health Clinic, Winchester and London Bridge Hospital, and formerly general practitioner in Alton and honorary senior lecturer in primary care at University of Southampton.