Abstract
Precision Cut Lung Slices (PCLS) have emerged as a sophisticated and physiologically relevant ex vivo model for studying the intricacies of lung diseases, including fibrosis, injury, repair, and host defense mechanisms. This innovative methodology presents a unique opportunity to bridge the gap between traditional in vitro cell cultures and in vivo animal models, offering researchers a more accurate representation of the intricate microenvironment of the lung. PCLS require the precise sectioning of lung tissue to maintain its structural and functional integrity. These thin slices serve as invaluable tools for various research endeavors, particularly in the realm of airway diseases. By providing a controlled microenvironment, precision-cut lung slices empower researchers to dissect and comprehend the multifaceted interactions and responses within lung tissue, thereby advancing our understanding of pulmonary pathophysiology.
Keywords: Precision cut lung slices, Respiratory therapeutics, Airway physiology in precision cut lung slices
Introduction
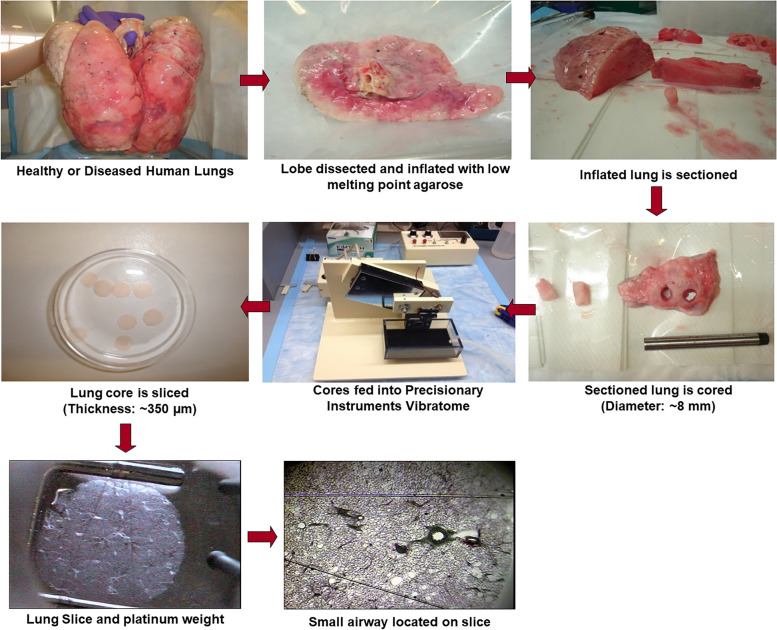
The history of precision-cut lung slices can be traced back to the general development of techniques for preparing and studying tissue slices in general. The development of tissue-slicing techniques began in the late 19th and early 20th centuries when investigators used specialized instruments to cut thin sections of various tissues for microscopic examination, but the use of the microtome for preparation of lung slices was first published in 1944 [1]. The term “precision cut” implies a high degree of accuracy and consistency in the preparation of tissue slices. In the mid-20th century, advances in microtome/vibratome technology and other cutting instruments allowed for the creation of slices with more precision, as depicted in Fig. 1. The application of precision-cut techniques to lung tissue likely followed the general trends in tissue slicing.
Fig. 1.
Generation of human lung slices. The lobes of the lungs from either healthy or diseased donors were inflated with a low melting point agarose, the agarose was allowed to solidify in the lungs, and the lung tissue was sectioned. A tissue punch or coring tool was used to generate columns of tissue containing airways, which are fed into a Precisionary Instruments Vibratome© to generate ~350 µm thick slices. Airways in these slices were identified, and the slices were weighed by platinum weights with nylon threads to assess changes in contraction and relaxation of the airways
Initially, lung slices were employed for toxicology studies to examine cellular survival in the face of exposure to environmental/industrial pollutants [2–5]. Subsequently, the importance of maintaining the physiological composition of the tissue for experiments was recognized, and precision-cut lung slices gained popularity and acceptance (as reviewed in [6]). Concerning respiratory research, PCLS became particularly valuable for studying airway reactivity and lung function, fibrosis, vascular responsiveness, responses to pharmacological agents/therapeutics, and airway immunology. The PCLS platform maintains the architecture of the lung tissue, including the airways, blood vessels, and parenchyma with the study of resident cell types in the context of the whole lung tissue. Over the years, advancements in imaging technologies and tissue preparation methods helped to improve the quality, rigor, and reproducibility of studies conducted using lung slices. Researchers can now study dynamic processes in real-time, such as airway constriction and dilation with greater accuracy, and can expose the slices to various substances to assess their effects on lung function and selective cellular responses, all of which provide insight into drug development and safety evaluation of potential therapeutic. PCLS provides a more realistic simulation of the lung microenvironment to study a variety of lung diseases.
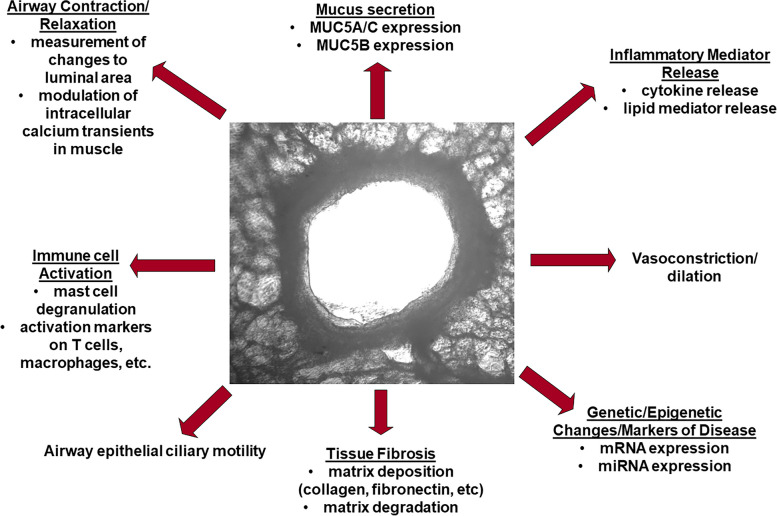
Taken together, PCLS have emerged as a powerful tool to study an array of lung diseases, including asthma, chronic obstructive pulmonary disease, fibrotic lung diseases (idiopathic pulmonary fibrosis, sarcoidosis), diseases of the pulmonary vasculature (pulmonary arterial hypertension and bronchopulmonary dysplasia), acute respiratory distress syndrome, lung cancer, and the consequences of respiratory pathogen exposure. The functional complexity, physiological relevance, and versatility of the platform make PCLS an invaluable asset for the study of the complexities of lung diseases and for advancing therapeutic development. As researchers refine the generation and uses of PCLS, the platform is poised to play a pivotal role in deepening our understanding of lung diseases and ultimately improving clinical outcomes for patients with those diseases. This review will summarize the use of PCLS in examining various lung diseases, and how this platform can foster an understanding of fundamental aspects of lung biology and disease-specific pathobiology, as depicted in Fig. 2. Further, the platform can serve as a tool for novel therapeutic discoveries in lung diseases.
Fig. 2.
The range of processes that can be measured utilizing the PCLS as a model system. A wide variety of endpoints, from changes in gene expression to tissue fibrosis and more, can be studied using this model system. Specific outcomes are noted below each type of outcome measured
Studies in infectious disease
Respiratory pathogen exposure has been extensively studied in primary and immortalized airway cell types; PCLS, however, offers an integrated tissue model to study the consequences of exposure and infection. Responses of the tissue to a variety of respiratory pathogens have been examined including responses to influenza, rhinovirus, respiratory syncytial virus, SARS-CoV2, fungal lung infection, and pathogenic bacterial species like Pseudomonas aeruginosa and Mycobacterium tuberculosis.
An influenza study used PCLS to show that exposure of PCLS downregulated albumin uptake, which impairs protein clearance from the alveolar space during flu-induced acute respiratory distress syndrome [7], and that the combination of influenza A and cigarette smoke exposure diminished responses to bronchodilators used in the treatment of asthma and COPD [8]. Activation of virus-sensing pathways induced by influenza and its competency for replication in PCLS following cigarette or e-cigarette exposure provided the model to report that cigarette exposure of the lung tissue worsened responses to influenza by suppressing the ability of the lung to properly respond to infection [9, 10]. Single cell sequencing of cells derived from PCLS showed that vaping extract amplified influenza-induced inflammatory responses [11]. Studies also examined the effects of specific inhibitors of multiple pathways to treat influenza infection and its effects [12–15], as well as to provide information on fundamental ways in which the lung responds to influenza infection [16–20]. Exposure to some species-specific viruses, including canine distemper virus [21] and murine pneumonia virus [22], have also been examined using PCLS.
The functional consequences of respiratory viruses like rhinovirus (RV) and respiratory syncytial virus (RSV), both of which evoke the development of wheeze and asthma as well as induce asthma exacerbations, have leveraged the use of PCLS. Lung inflammation following exposure to RSV in PCLS [23] identified novel treatment strategies including mucosal application of an RSV vaccine [24] and modulation of an ion channel [25] to attenuate the effects of RSV. Much of the research that has been conducted examining the effects of RV on the airways has focused on examining inflammatory mediator release from monocultures of airway epithelial cells. Interestingly, RV exposure of PCLS can modulate both agonist-induced contraction [26, 27] and relaxation [28] of the airways that both appear to be serotype- and disease state-specific. Inflammatory responses elicited by RV have also been studied in PCLS [29], with the addition of different treatment strategies showing a reduction in RV-induced inflammation [30, 31].
With the SARS-CoV2 pandemic catapulting respiratory virus exposure to the forefront of research efforts for scientists globally, PCLS provided a relevant platform to study aspects of infection and response to infection in the lung. An early study utilized various strains of infectious bronchitis virus, which are avian coronaviruses, to examine infection of the lung with these viruses [32]. An understanding of the mechanisms driving the inflammation associated with SARS-CoV2, as well as replication mechanisms and pathologic features of the disease have been achieved using PCLS [33–35]. Other laboratories identified effective therapeutics that could target SARS-CoV2 infection in PCLS [36–40].
While there has been extensive focus on exposure of lungs to viral pathogens, there are also pathogenic bacteria and fungi that infect the lung causing inflammation and disease. Investigators have used components of bacteria, including lipopolysaccharide (LPS), to stimulate pattern recognition receptors on a variety of cell types in PCLS. LPS induced an upregulation of innate immune responses consistent with endotoxin challenge of patients [41]; LPS had little effect on agonist-induced airway constriction or relaxation [42]; and toll-like receptor 2 (TLR2) activation reduced the ability of bronchodilators to induce relaxation of murine airways [43]. The consequences of exposure to the pathogenic bacteria Pseudomonas aeruginosa has also been examined in PCLS [44–47], with one study showing that some commensal bacteria strains present in the lung of cystic fibrosis patients may protect the host from P. aeruginosa-induced inflammation [46], and another noting a more robust immune/inflammatory response in younger mice compared to older mice of the same strain when exposed to the bacteria [47]. Some bacteria, like Trueperella pyogenes, only appear to infect animals but not humans, with their pathogenic effects having been studied in PCLS [48]. Additional studies in PCLS studied Mycobacterium tuberculosis [49], Mycobacterium abscessus [50], Yersinia pestis [51], and Staphylococcus aureus [52] to understand the pathologic features of infection and agents used to treat these infections. Additionally, co-infection of PCLS with influenza and a Mycobacterium strain showed that the influenza infection increased the susceptibility to Mycobacterium infection by attenuating responses to the bacteria that would otherwise allow the animal to clear the bacteria [53]. Exposure of the lung to fungal pathogens can also occur in healthy patients but tend to be a significant problem for those with underlying lung diseases. Infection of murine PCLS with Pneumocystis murina, a common pathogen that infects immunosuppressed mice and can cause pneumonia, showed colonization of PCLS with the pathogen and that PCLS can serve as a useful model for testing anti-fungal molecules in a moderate-to-high throughput manner [54]. Overall, PCLS can serve as a valuable model to study the pathologic and inflammatory aspects of exposure to bacterial and fungal pathogens, as well as aid in the discovery of novel, effective treatments to combat these pathogens.
Studies in lung cancer
Although considerable research has been done to study lung cancer and both current and potential therapeutics, few studies have used PCLS as a model system. Some studies have utilized lung cancer explants into murine systems and analyzed the PCLS derived from these mice, where others have used cancerous tissue derived from the lungs of patients to generate PCLS. A few studies have utilized PCLS as a preclinical model to test therapeutics in both human and mouse tissues [55–58]. Others have examined lymphocyte migration into lung tumors to try to understand lymphocyte accumulation in the tumors [59], while another study examined changes in macrophage activation and the contribution to lung cancer growth [60]. A proof-of-concept study leveraged molecular imaging of PCLS from non-small cell lung cancer tissue to examine cell-cell and cell-stroma interactions in lung cancer [61]. There have also been studies targeting specific signaling pathways driving some lung cancers that have provided insight into the utility of specifically targeting the lung to treat the cancer [62–68]. Collectively, PCLS use in cancer studies is still evolving, but the model is amenable to moderate to high-throughput drug discovery for cell-targeted therapy to the lungs.
Studies in pulmonary vascular diseases
According to the National Institutes of Health, pulmonary hypertension (PH) has an incidence rate of about 1% globally. However, in over 50% of the cases of PH there is no known cause. PCLS have been used to study vasoconstriction and dilation [69], and to model the consequences of exposures that induce bronchopulmonary dysplasia (BPD) and acute respiratory distress syndrome (ARDS). Studies of endogenous vasoconstrictors and dilators have used PCLS [70–75], along with studies examining the consequences of pharmacologic intervention on these processes [76–83]. Two studies also noted that cigarette smoke enhanced the contraction of vessels in PCLS to endothelin-1 [84, 85], an endogenous vasoconstrictor. One study examined a role for IL-11 in PH, finding that in PH patients IL-11 expression was higher in the vasculature from those patients compared to patients without PH, and that IL-11 treatment of PCLS made the vessels more sensitive to endothelin-1-induced vasoconstriction [86]. Changes elicited by exposure to a hypoxic [87–95] or hypercapnic [96] environment, both of which can cause increased vascular resistance, have been modeled in PCLS. For BPD, the hyperoxia and mechanical ventilation that are necessary for ventilation of premature newborn lungs causes damage to the lungs that can persist long-term. Few studies exist using PCLS to examine mechanisms of pathology of BPD [93, 97–99] or ARDS [100, 101] and even fewer have studied mechanisms of pulmonary hypertension [102, 103]. Despite a lack of extensive studies, PCLS may provide insight into the pathophysiology and discovery of new therapeutic approaches in the treatment of pulmonary vascular diseases.
Studies in fibrotic lung diseases
Idiopathic pulmonary fibrosis (IPF) is a fibrotic disease of the lung tissue surrounding the alveoli that progressively stiffens the lung, making it difficult for the person to breathe. Studies in PCLS have supported a number of different molecules in the pathogenesis of IPF including: a transmembrane protein that can interact with growth factor receptors or extracellular ligands to modulate receptor activation [104]; activation of histone deacetylases [105]; activation of integrins [106]; ion channel activation [107]; a kinase and a signaling microdomain protein [108]; a protein involved in cell fate determination, motility, and organogenesis [109]; and even an miRNA mimic as a potential therapy [110]. Additionally, other pathways have been postulated to be part of specific aspects of the biology of both epithelial cells and fibroblasts that may play a role in the pathology of IPF [111–121]. Studies have utilized PCLS to identify the cell types that drive fibrosis signals and showed the ways in which PCLS can model IPF [122–125]. A number of pharmacologic inhibitors have been used as potential treatments for IPF [126–131], including current therapeutics that are being used in the treatment of IPF, like nintedanib and pirfenidone [132–134]. The contribution of released factors to the development/progression of IPF has also been studied in PCLS [121, 135, 136]. PCLS provides an ex vivo system in which lung tissue derived from IPF patients can be examined for biomarkers, and to ascertain the efficacy of a variety of therapeutic interventions to decrease expression/deposition of the fibrotic proteins that are overproduced in the disease that contribute to the increased stiffness of the lungs.
Sarcoidosis is a systemic inflammatory disease that affects multiple organs of the body. Broadly, sarcoidosis induces granuloma formation in the tissue and in the lungs produces a fibrosis-like phenotype that, like IPF, induces severe, irreversible damage to the lungs. To date, there are no studies examining PCLS derived from the lungs of sarcoidosis patients. PCLS may provide a platform well suited for study of the fibrosis associated with sarcoidosis, allowing for testing of novel therapeutics and identification of biomarkers similarly to how IPF is being studied in PCLS.
Studies of obstructive lung diseases
PCLS models have been used to study the consequences of obstructive lung diseases including asthma and chronic obstructive pulmonary disease (COPD). A study showed that airway constriction and relaxation in PCLS linked internal perimeter of the airways to airway smooth muscle shortening [137]. Additionally, PCLS has enabled investigators to translate their findings to clinically measurable respiratory parameters that are typically measured in obstructive lung diseases like asthma and COPD. For example, the luminal area of the small airways in PCLS correlates with the forced expiratory flow between 25% and 75% (FEF25-75), which serves to predict small airways obstruction that is characteristic of asthma and COPD (as reviewed in [138]).
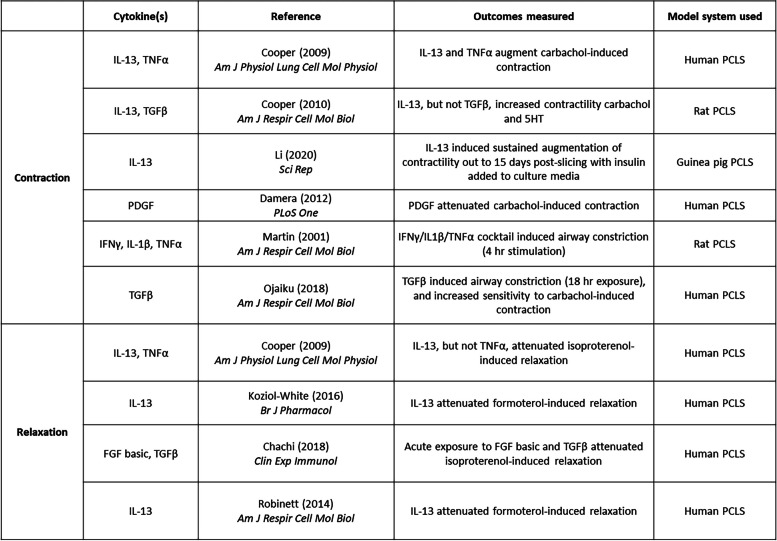
With respect to allergic asthma, studies in both human PCLS and in animal models of allergic airways inflammation have enhanced our understanding of basic mechanisms underlying bronchoconstriction and how an inflammatory milieu affects basal bronchomotor tone. Early studies using human PCLS (hPCLS) demonstrated that allergen sensitization of hPCLS, and subsequent stimulation with allergen, could mimic bronchoconstriction associated with allergic asthma [139, 140]. Since then, human- [141–144], rat- [145], and guinea pig-derived [146, 147] PCLS have been utilized to determine the roles of specific receptor subtypes and signaling molecules downstream of the immunoglobulin E (IgE) receptor in IgE-induced airway constriction. Murine models of allergen exposure, or exposure to proteases found in allergen extracts, showed that release of specific inflammatory mediators [148] increased airway contractility [148–151]. In the context of a Th2 inflammation of the airways, compelling evidence suggests that Interleukin-13 (IL-13) and IL-4, Th2 cytokines, enhanced airway contractility and diminished responsiveness to commonly used bronchodilators in human, rat, and murine PCLS [141, 152–156]. In animal models of allergic airway inflammation, PCLS studies revealed a spectrum of cellular pathways that evoke airway hyperresponsiveness including transcription factor activation in airway cells [157]; asthma-associated genes modulating airway smooth muscle shortening [158]; and increased cholinergic stimulation of nerve-dependent airway constriction following ovalbumin sensitization and challenge [159] following early-life allergen exposure [160]. Stimulation of PCLS with other inflammatory cytokines that are associated with allergic asthma, non-allergic asthma, and asthma exacerbations have been shown to alter contractility of the airways and/or attenuate agonist-induced bronchodilation (specific studies listed in Table 1) [141, 152, 155, 156, 161–165].
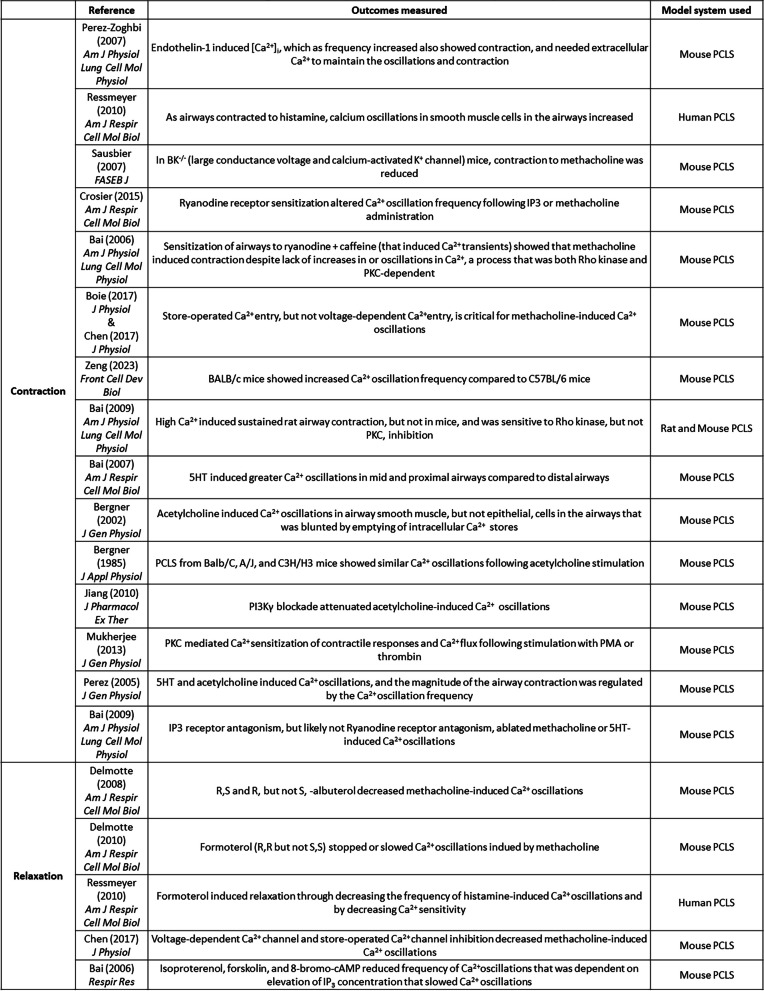
Table 1.
Studies of inflammatory mediator-dependent modulation of airway contraction/relaxation
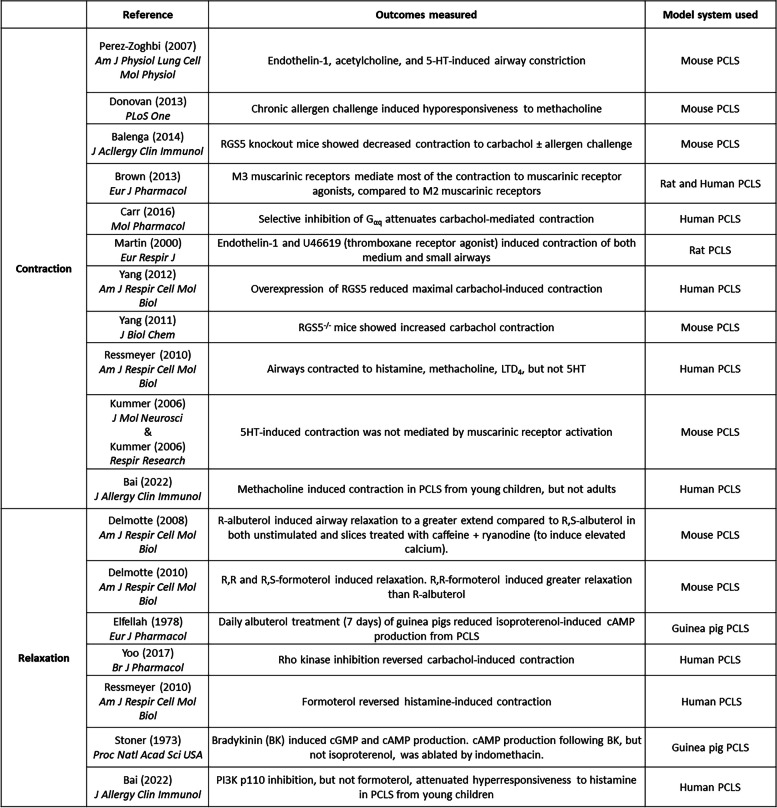
To understand basic mechanisms of airway biology, PCLS can be used to examine mechanisms that underly contraction or relaxation in non-diseased tissue from either human or animal models. The role(s) for numerous signaling molecules in mechanisms of receptor-mediated contraction and relaxation of small airways have been examined by observing narrowing and opening of airways (specific studies listed in Table 2) [75, 151, 166–182], and/or visualization of signaling events occurring simultaneously with airway contraction/relaxation (specific studies listed in Table 3) [75, 158, 169, 170, 175, 183–196]. Airway constriction in PCLS also induced remodeling in guinea pig PCLS [197]. Bronchopulmonary dysplasia can alter the vasculature architecture of the lung, inducing susceptibility for the development of asthma. One study noted that exposure of mouse pups to hyperoxia, that induces a BPD-like phenotype, evoked greater maximal airway contraction in PCLS derived from the hyperoxic mice compared to those in normoxic conditions [198]. PCLS has also had value in modeling of clinically observed phenomena, including desensitization of the β2 adrenergic receptor (β2AR) following agonist stimulation [155, 199–202].
Table 2.
Studies of airway contraction/relaxation
Table 3.
Studies showing visualization of processes associated with airway contraction/relaxation
Despite significant advances in our knowledge of asthma pathogenesis, the search for better bronchodilators is still evolving. Drugs that inhibit pathways underlying contraction promote relaxation of pre-constricted airways [150, 155, 162, 168, 178, 180, 203–207], and testing of selective molecules that either elicit or enhance bronchodilation have been used in PCLS [81, 208–212]. Other non-canonical pathways have also been targeted to reverse, or inhibit, airway contraction (specific studies listed in Table 4) [155, 165, 202, 213–228]. Compounds targeting orphan, or non-β2 receptors, can serve as new classes of bronchodilators, or have been suggested to be useful as add-on therapy for existing therapeutics [164, 165, 214–228]. Overall, PCLS provide a highly useful and versatile platform for drug discovery to modulate both contraction and relaxation of the airways that can serve to increase our understanding of basic mechanisms underlying these processes, and uncover novel therapeutics that may have clinical use in treatment of obstructive lung diseases.
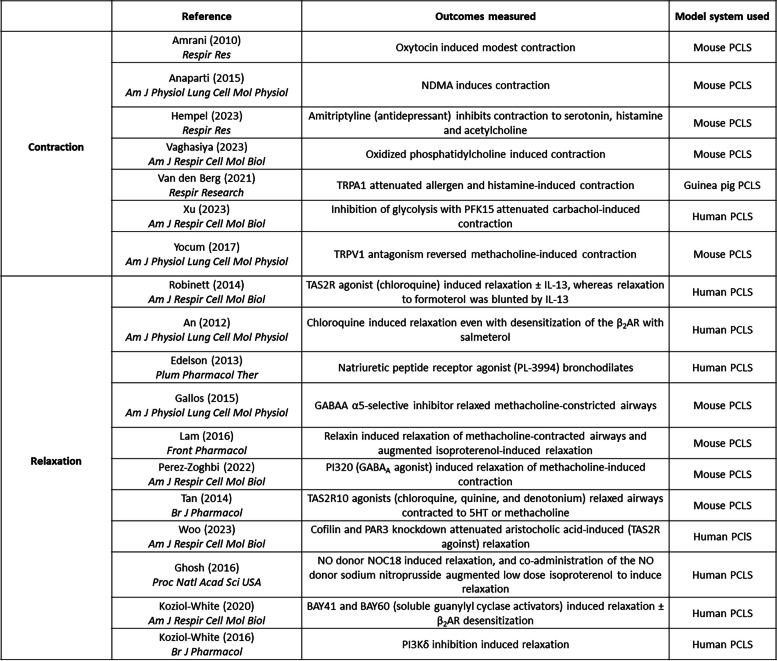
Table 4.
Studies of novel bronchoconstrictors and bronchodilators
Despite considerable research into modeling asthma phenotypes and/or inflammatory milieu associated with asthma, there is a paucity of research into chronic obstructive pulmonary disease (COPD) using PCLS. To date, only four studies examining aspects of COPD pathobiology in hPCLS have been published [229–233]. Van Dijk et al. reported that elastase-induced parenchymal disruption of murine PCLS that would provide an animal model to study COPD [234], and Kim et al. defined the mechanical properties of PCLS derived from lungs from an emphysema patient [235]. Ideally, PCLS derived from patients with COPD would identify biomarkers that could be targeted, thereby aiding in discovery of drugs that would mitigate the inflammation and destruction of the airspace associated with the disease.
Environmental toxicant exposure studies
An early adaption of PCLS for research focused on PCLS use in lung toxicology [2–5]. Since then, an array of other endpoints have been studied to understand how exposure to various toxicants can engender inflammation and even promote airway hyperresponsiveness. Consequences of exposure to noxious gases, including warfare agents like sarin and VX gas, in PCLS showed enhanced airway constriction that could be modulated by anti-muscarinic drugs [236–239]. Chlorine exposure of PCLS increased release of inflammatory mediators from the tissue, decreased airway constriction, and decreased cell viability [240, 241]. Exposure to gases from industrial processes or the use of pesticides induced cytotoxicity in PCLS, as well as inflammatory mediator production and oxidative stress [242, 243]. Interestingly, lipid peroxidation occurs in many disease processes and occurs following toxicant exposure. Recently, a PCLS study detected lipid peroxidation using a biosensor following exposure to nitrogen mustard [244]. Such a biosensor can provide a tool for understanding of toxicity of a variety of environmental compounds. Additionally, another study found that the effects of nitrogen mustard exposure that drive pulmonary toxicity appear to be independent of immune cell trafficking to the lungs [245].
In addition to noxious gases, exposure to environmental cigarette smoke (CS), has been studied in PCLS. CS or CSE (cigarette smoke extract) elicited inflammatory mediator release, induced histologic inflammatory changes and extracellular matrix gene expression, decreased cell viability, increased markers of the unfolded protein response, and increased airway constriction to serotonin but not methacholine [246–249]. Interestingly, menthol-containing e-cigarette condensate decreased airway contraction in PCLS but increased oxidative stress markers [250]. The combination of influenza with CS exposure showed that CS exposure reduced flu-induced inflammatory mediator release, and the combination of the two insults reduced airway relaxation when CS exposure alone had little effect [8]. Using a highly sensitive sensor for cAMP, investigators showed that CS exposure of mouse PCLS attenuated β2AR signaling that was reversed by inhibition of phosphodiesterase 3 (PDE3) and PDE4 [251].
The effects of chemical sensitizers, whether inhaled or dermal sensitizers, have been studied in PCLS where most sensitizers induced inflammatory mediator release from PCLS [252, 253], but only a few increased contractility of the airways [252, 254, 255]. Additionally, the toxicologic effects of various drugs and chemicals have been assessed in PCLS. Exposure of PCLS to an anti-cancer drug that is known to cause pulmonary toxicity showed increased inflammatory mediatory release as well as cellular toxicity [256]. PCLS exposed to the industrial toxins cadmium chloride, ammonium hexachloroplatinate, and zinc chloride showed increased inflammatory mediator release from PCLS [257–259], and when cadmium chloride was combined with Transforming Growth Factor β (TGFβ) there was increased fibrosis of the tissue compared to TGFβ treatment alone [257].
Common environmental exposures that induce a significant number of exacerbations of underlying asthma, including ozone and particulate matter, have also been studied using PCLS. Following exposure to ozone, inflammatory markers were upregulated in PCLS [260–262] and acute exposure to high levels of ozone also induced airway hyperresponsiveness in the absence of influx of immune cells [260]. Interestingly, deletion of microsomal prostaglandin E synthase 1 (PGES-1), an enzyme necessary for the metabolism of arachidonic acid into prostaglandin E2, had little effect on ozone-induced airway hyperresponsiveness and inflammation in a mouse model [262]. Diesel exhaust particle exposure of PCLS induced cell death, oxidative stress, and inflammatory mediator release [263, 264]. Particulate matter, from agricultural dust or the desert, increased airway hyperresponsiveness [265], anti-oxidant gene expression, and inflammatory mediator gene expression [266] in PCLS.
Comparisons of animal versus human models
Animal models provide platforms to study pathophysiology of human disease. Studies of lung diseases have extensively used rodent models, including mice and rats, and many studies have used PCLS derived from these animals. Only a few studies have compared animal-derived to human-derived PCLS. Schleputz et al. performed a study of PCLS from mice, rats, guinea pigs, marmosets, sheep, and humans found that electric field stimulation of neural responses that induced airway constriction in marmosets and guinea pigs was similar to humans, whereas the airways of mice and rats did not respond similarly to human [267]. Zeng et al. noted differences among strains of mice in their responsiveness to methacholine, a muscarinic receptor agonist, and 5-hydroxytryptamine (5-HT), a serotonin receptor agonist, where airway constriction of the small airways (not the tracheas) in PCLS of BALB/c mice to both contractile agonists elicited greater contraction compared to small airways from C57BL/6 [187]. Comparison between human and guinea pig-derived PCLS noted that airways from both contracted to leukotriene D4, thromboxane, histamine and methacholine, but only guinea pig airways contracted to serotonin [268]. A comparison among PCLS from a primate species and humans found that airways from cynomolgus macaques and baboons responded most similarly to human airways with respect to their responsiveness to methacholine, histamine, serotonin, leukotriene D4 (LTD4), and endothelin-1 [269].
In addition to differential responsiveness to bronchoconstrictors, many studies highlight the substantial differences between mice and human lungs in terms of the physiology, anatomy, and immunology of each species. Studies have also highlighted that the preclinical results obtained from mouse studies failed to accurately model airways diseases in humans (as reviewed in [138]). Despite the limitations of mouse models in the study of airways diseases, rodent strains offer the opportunity to genetically modify the animal to assess the function of cell-specific gene deficiency on the development and progression of lung diseases. Two studies have utilized siRNA-mediated knockdown of specific transcripts in human PCLS [225, 270, 271], but the siRNA used in each study was not cell-type specific. Despite the limitations of working with animal model systems, these platforms can augment our understanding of disease pathogenesis when combined with observations using human cells and tissues.
Technologic innovations in PCLS use
With any model system, the broad utility and versatility of the system is what propels it into use on a greater scale, ultimately leading to significant use of the system. PCLS is becoming a platform that demonstrates both broad utility and versatility. Given this, studies by Martin et al. [81, 163, 172, 203, 267, 272, 273] and Sanderson et al. [158, 169, 170, 183–192, 195, 196] paved the way for technologic advances for studying obstructive lung diseases in PCLS with respect to imaging of airway and vascular constriction, but also visualization of cellular processes that underly airway constriction, like calcium oscillations in muscle surrounding the airways. Others have studied the effects of stretch of the tissue that mimics breathing in human lung, examining both mechanical and biological outcomes [274–280]. Utilization of PCLS to generate large data sets, like miRNA and RNAseq data sets, have also been optimized by a few laboratories [281, 282]. To understand how histone modifications alter inflammation of the lung, the histone acetyltransferase inhibitor MG149 was found to attenuate LPS and Interferon γ (IFNγ)-stimulated proinflammatory gene expression [283]. Others have also optimized siRNA-mediated knockdown of multiple gene targets to decrease protein expression [225, 270, 271], with one of the studies also assessing the functional effects of the knockdown [225]. Receptor localization has also been studied in the epithelium of the airways by fluorescent microscopy following adenoviral transduction of hPCLS following desensitization of the β2AR [199]. Investigators have imaged PCLS to visualize migration of live immune cells [284], to define 3D cell-cell interactions in situ [285], and to generate immune responses normally associated with immune responses observed to antigens that the individual has been vaccinated against [286]. Studies have also used electric field stimulation of PCLS and measured airway contraction [273], or exposure to specific wavelengths of light to induce relaxation of muscle in the airways [287]. PCLS have been utilized to examine mucociliary properties of airway epithelial cells [288–292], and the ability of lung tissue to repair itself [293]. A variety of pathologic processes, as well as cellular changes, have been examined using PCLS using a wide array of technologies.
Advantages and challenges of the system
PCLS maintain the native architecture of the lung, including a complement of resident cells like airway smooth muscle, epithelial cells, fibroblasts, and resident immunocytes. This architecture provides the study of physiologic processes including airway constriction and dilation, vasoconstriction and dilation, lung fibrosis, and epithelial ciliary function. In diseased tissues, researchers can examine the reversal of some of the pathologies associated with the disease given experimental interventions. PCLS affords physiologic relevance to the research, as it is an environment that closely mimics the in vivo conditions and retains the 3D structure of the lung, thereby providing meaningful insights into disease mechanisms. Additionally, this system fosters the study of a multitude of outcomes through the interplay among various cell types. PCLS serve as invaluable tool for drug screening and therapeutic development, allowing for testing of both the safety and efficacy of compounds/biologics/etc. to expedite the translation of promising candidates for translation from bench to bedside.
With all the advantages of the system, there are some disadvantages to using PCLS to study lung diseases. The issues with the system are the following: lack of circulation, tissue viability over time, and standardization of derivation/culture/use of the slices between laboratories. While there is a wide array of cell types present in the lung tissue, the consequences of the effects of therapeutic intervention outside the lung on the resident lung cells, or on cell types recruited to the lung, cannot be studied. Only in in vivo systems, like rodent and non-human primate models, are the systemic responses and their effects on the lungs able to be studied in isolated PCLS following a given exposure. For human lung tissue, this simply is not possible. Due to the nature of generation of PCLS, there exists the limitation that exposure to small molecules/pathogens/etc. is non-physiologic as the entire slice, and all cell types contained within the slice, is/are likely exposed to a given stimulus. The use of slices in air-liquid interface cultures and delivery of some types of stimuli into the lumen of the airway directly may mitigate some of the off-target or non-physiological effects of a given exposure. Viability of the tissue over time is also an issue, depending on the outcome(s) being measured. For some assays including measuring ciliary beat or acute progression of induced fibrosis, short-term measurements pose no challenges. However, for other assays like assessment of airway contraction and relaxation, the fidelity and reproducibility of PCLS measurements decreases over time that the slices have been in culture. Baseline viability that is irrespective of therapeutic intervention that may be used to try to reverse the effects of processes like fibrosis also presents a challenge for long-term study of those types of lung pathologies. With respect to the differences in baseline variability, the acceptance criteria for lungs from “healthy” donors that have no history chronic illness can vary between laboratories with respect to things like O2 saturation of the donor near time of death, number of days on a ventilator, etc. Some laboratories use non-diseased resections from donors that have lung cancer, which calls into question whether they can be directly compared with tissue/PCLS from people with no cancer diagnosis. Standardization of a basic set of parameters for acceptance of tissue from “healthy” donors may help in decreasing experimental variability between laboratories.
With respect to the issue of viability of PCLS, groups have examined various outcomes following cryopreservation of PCLS to provide a larger supply of PCLS that can be utilized for more than just short-term culture [259, 294–298]. Bailey et al. showed that embedding PCLS in hydrogel biomaterials can extend the viability of the slices in culture [299]. With respect to cryopreservation, the methods vary from lab to lab, and vary among species that the PCLS were derived from. Watson et al. reported that PCLS were susceptible to zinc chloride-induced damage after cryopreservation [259], suggesting significant variation between freshly prepared and cryopreserved PCLS. Undoubtedly, standardization of the cryopreservation method and fidelity of the data produced in thawed tissue slices become much more difficult to achieve and assess when there is a lack of reproducibility or standard operating procedures. While some outcomes, like inflammatory mediator release, may exhibit less variability before and after cryopreservation, other outcomes like contraction and relaxation of the airways are subject to high variability from donor to donor even before PCLS are cryopreserved, most notably in human PCLS. Despite some successes, significant work is needed assure that outcomes of cryopreserved PCLS mimic those of fresh PCLS.
Other issues concern standardization of experimental conditions among laboratories. Multiple methods-focused papers have been published detailing the processing of mainly murine [66, 300–303] and human lung tissue [258, 304], highlighting both the complexities of generating PCLS and noting that becoming adept at the process of generating the slices can ensure greater reproducibility of results. These and other publications also show the differences in how murine PCLS are generated versus human PCLS, and demonstrate that the method(s) of generation even the same type of lung source (i.e. human lung tissue) can vary greatly between laboratories. Be it lung inflation protocols, tissue slicing protocols, culture media, or culture protocols, there is wide variation between labs that makes comparisons between studies challenging (partially noted in [6, 305]). With respect to culture media, Patel et al. described differences in long-term PCLS culture in a few different media formulations, noting that given certain inflammatory stimulation (LPS or poly(I: C)) that the robustness of cytokine release varied between the air-liquid interface (ALI)-cultured PCLS and submerged cultures as to which culture environment elicited a greater response [305]. The antimicrobial agents used in culture of PCLS vary slightly between studies, but most investigators use penicillin/streptomycin in the presence or absence of an anti-fungal agent to protect their cultures. The components added to a base media, including things like fetal bovine serum, vary between groups and can vary dependent upon the outcome that will be measured or the cell type that the investigators are interested in studying. For example, some groups do not use any serum in their media formulation because there isn’t a need for growth of the structural cells in culture, but rather maintenance of the architecture of the tissue. For study of epithelial cells lining the airways, some groups have used epithelial cell-specific media that is used for monoculture of air-liquid differentiated airway epithelial cells. Others have used media used for the culture of immunocytes, which may not be optimal for the culture of structural cell types.
A discussion of experimental replicates when using PCLS also requires careful attention; some report experimental replicates as those data derived from multiple slices from a single lung donor. This approach fails to account for biological variation across multiple donors. Arguably, technical replicates can refer to serial slices cut from the same core/piece of lung tissue, or may refer to multiple slices derived from a single donor. A designation of biological replicates, however, should only be applied to data derived from separate, distinct donors and should not be published as experimental replicates if they are all derived from a single donor. Other investigators refer to a variant of PCLS in which bronchioles are embedded in agarose and thinly sliced [306–308]. This system is more akin to organ bath systems where bronchiole rings are cut and tethered to a myograph to measure force generation of airway smooth muscle. PCLS can measure an integrated response that incorporates parenchymal tethering of the airway and is more akin to an in situ environment in which airway luminal area is measured. Accordingly, the bronchiole slice model may not equate to PCLS and may serve to measure outcomes disparate from those measured with PCLS. In summary, standardization of protocols for the generation and use of PCLS will improve scientific rigor and reproducibility.
Conclusions and future directions
PCLS provide a multifaceted platform in which studies of several different lung diseases can be studied. The mechanistic insights gained for a range of lung diseases provide novel targets for development of therapeutics that can be used in conjunction with current treatments, or may even serve as replacements to traditional therapeutic strategies. The PCLS platform offers a broadly applicable model for treatment of an array of lung diseases, with the platform providing a solid connection between translational science and clinical utility.
Abbreviations
- PCLS
Precision cut lung slices
- hPCLS
Human precision cut lung slices
- SARS-CoV2
Severe acute respiratory syndrome-related coronavirus
- RV
Rhinovirus
- RSV
Respiratory syncytial virus
- LPS
Lipopolysaccharide
- PH
Pulmonary hypertension
- BPD
Bronchopulmonary dysplasia
- IPF
Idiopathic pulmonary fibrosis
- COPD
Chronic obstructive pulmonary disease
- FEF25-75
Force expiratory flow between 25 and 75%
- IgE
Immunoglobulin E
- IL-13
Interleukin 13
- β2AR
β2 adrenergic receptor
- CS
Cigarette smoke
- CSE
Cigarette smoke extract
- PDE
Phosphodiesterase
- PGES-1
Prostaglandin E synthase 1
- 5-HT
5-hydroxtryptamine
- LTD4
Leukotriene D4
- siRNA
Small interfering ribonucleic acid
- IFN γ
Interferon γ
- TGFβ
Transforming growth factor β
Authors’ contributions
C. Koziol-White: drafting and editing of the manuscript, final approval of the publication. E. Gebski: drafting and editing of the manuscript, final approval of the publication. G. Cao: drafting and editing of the manuscript, final approval of the publication. R. Panettieri: drafting and editing of the manuscript, final approval of the publication.
Funding
This manuscript was funded by grants received by the authors from the NIH (listed on the authors page).
Availability of data and materials
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
There were no research studies conducted where data was included in this manuscript, so there was no need for ethical approval of the studies as this is a literature review.
Consent for publication
N/A as this is a literature review.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.BC SWaR Microtome for preparation of tissue slices for metabolic studies in vitro. J Biol Chem. 1944;154:687–90. doi: 10.1016/S0021-9258(18)71901-7. [DOI] [Google Scholar]
- 2.Boyd MR, Statham CN, Longo NS. The pulmonary clara cell as a target for toxic chemicals requiring metabolic activation; studies with carbon tetrachloride. J Pharmacol Exp Ther. 1980;212:109–14. [PubMed] [Google Scholar]
- 3.Freeman BA, O’Neil JJ. Tissue slices in the study of lung metabolism and toxicology. Environ Health Perspect. 1984;56:51–60. doi: 10.1289/ehp.845651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karl PI, Friedman PA. Competition between paraquat and putrescine for accumulation by rat lung slices. Toxicology. 1983;26:317–23. doi: 10.1016/0300-483X(83)90092-6. [DOI] [PubMed] [Google Scholar]
- 5.Smith LL, Wyatt I, Rose MS. Factors affecting the efflux of paraquat from rat lung slices. Toxicology. 1981;19:197–207. doi: 10.1016/0300-483X(81)90129-3. [DOI] [PubMed] [Google Scholar]
- 6.Alsafadi HN, Uhl FE, Pineda RH, Bailey KE, Rojas M, Wagner DE, Konigshoff M. Applications and approaches for three-Dimensional Precision-Cut lung slices. Disease modeling and Drug Discovery. Am J Respir Cell Mol Biol. 2020;62:681–91. doi: 10.1165/rcmb.2019-0276TR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alberro-Brage A, Kryvenko V, Malainou C, Gunther S, Morty RE, Seeger W, Herold S, Samakovlis C, Vadasz I. Influenza virus decreases albumin uptake and megalin expression in alveolar epithelial cells. Front Immunol. 2023;14:1260973. doi: 10.3389/fimmu.2023.1260973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donovan C, Seow HJ, Bourke JE, Vlahos R. Influenza a virus infection and cigarette smoke impair bronchodilator responsiveness to beta-adrenoceptor agonists in mouse lung. Clin Sci (Lond) 2016;130:829–37. doi: 10.1042/CS20160093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agraval H, Crue T, Schaunaman N, Numata M, Day BJ, Chu HW. Electronic cigarette exposure increases the severity of Influenza a Virus infection via TRAIL dysregulation in Human Precision-Cut lung slices. Int J Mol Sci. 2023;24:4295–4311. doi: 10.3390/ijms24054295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu W, Patel KB, Booth JL, Zhang W, Metcalf JP. Cigarette smoke extract suppresses the RIG-I-initiated innate immune response to influenza virus in the human lung. Am J Physiol Lung Cell Mol Physiol. 2011;300:L821–830. doi: 10.1152/ajplung.00267.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crue T, Lee GY, Peng JY, Schaunaman N, Agraval H, Day BJ, Dimasuay KG, Cervantes D, Nouri H, Nichols T, et al. Single cell RNA-sequencing of human precision-cut lung slices: a novel approach to study the effect of vaping and viral infection on lung health. Innate Immun. 2023;29:61–70. doi: 10.1177/17534259231181029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu R, An L, Liu G, Li X, Tang W, Chen X. Mouse lung slices: an ex vivo model for the evaluation of antiviral and anti-inflammatory agents against influenza viruses. Antiviral Res. 2015;120:101–11. doi: 10.1016/j.antiviral.2015.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meineke R, Stelz S, Busch M, Werlein C, Kuhnel M, Jonigk D, Rimmelzwaan GF, Elbahesh H. FDA-Approved inhibitors of RTK/Raf signaling potently impair multiple steps of in Vitro and Ex vivo Influenza A Virus infections. Viruses. 2022;14:2058–2077. doi: 10.3390/v14092058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meineke R, Stelz S, Busch M, Werlein C, Kuhnel M, Jonigk D, Rimmelzwaan GF, Elbahesh H. FDA-approved Abl/EGFR/PDGFR kinase inhibitors show potent efficacy against pandemic and seasonal influenza a virus infections of human lung explants. iScience. 2023;26:106309. doi: 10.1016/j.isci.2023.106309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neuhaus V, Schwarz K, Klee A, Seehase S, Forster C, Pfennig O, Jonigk D, Fieguth HG, Koch W, Warnecke G, et al. Functional testing of an inhalable nanoparticle based influenza vaccine using a human precision cut lung slice technique. PLoS ONE. 2013;8:e71728. doi: 10.1371/journal.pone.0071728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Delgado-Ortega M, Melo S, Punyadarsaniya D, Rame C, Olivier M, Soubieux D, Marc D, Simon G, Herrler G, Berri M, et al. Innate immune response to a H3N2 subtype swine influenza virus in newborn porcine trachea cells, alveolar macrophages, and precision-cut lung slices. Vet Res. 2014;45:42. doi: 10.1186/1297-9716-45-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fu Y, Tong J, Meng F, Hoeltig D, Liu G, Yin X, Herrler G. Ciliostasis of airway epithelial cells facilitates influenza a virus infection. Vet Res. 2018;49:65. doi: 10.1186/s13567-018-0568-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meng F, Punyadarsaniya D, Uhlenbruck S, Hennig-Pauka I, Schwegmann-Wessels C, Ren X, Durrwald R, Herrler G. Replication characteristics of swine influenza viruses in precision-cut lung slices reflect the virulence properties of the viruses. Vet Res. 2013;44:110. doi: 10.1186/1297-9716-44-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.FitzPatrick M, Royce SG, Langenbach S, McQualter J, Reading PC, Wijburg O, Anderson GP, Stewart A, Bourke J, Bozinovski S. Neonatal pneumococcal colonisation caused by Influenza a infection alters lung function in adult mice. Sci Rep. 2016;6:22751. doi: 10.1038/srep22751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schaunaman N, Cervantes D, Nichols T, Numata M, Ledford JG, Kraft M, Chu HW. Cooperation of immune regulators Tollip and surfactant protein A inhibits influenza a virus infection in mice. Respir Res. 2024;25:193. doi: 10.1186/s12931-024-02820-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chludzinski E, Ciurkiewicz M, Stoff M, Klemens J, Kruger J, Shin DL, Herrler G, Beineke A. Canine distemper virus alters defense responses in an Ex vivo model of pulmonary infection. Viruses. 2023;15:834–852. doi: 10.3390/v15040834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Limkar AR, Percopo CM, Redes JL, Druey KM, Rosenberg HF. Persistent Airway Hyperresponsiveness following recovery from infection with Pneumonia Virus of mice. Viruses. 2021;13:728–740. doi: 10.3390/v13050728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krishnamoorthy N, Walker KH, Bruggemann TR, Tavares LP, Smith EW, Nijmeh J, Bai Y, Ai X, Cagnina RE, Duvall MG, et al. The Maresin 1-LGR6 axis decreases respiratory syncytial virus-induced lung inflammation. Proc Natl Acad Sci U S A. 2023;120:e2206480120. doi: 10.1073/pnas.2206480120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eberlein V, Ahrends M, Bayer L, Finkensieper J, Besecke JK, Mansuroglu Y, Standfest B, Lange F, Schopf S, Thoma M, et al. Mucosal application of a low-energy Electron inactivated respiratory Syncytial Virus Vaccine shows protective efficacy in an animal model. Viruses. 2023;15:1846–1863. doi: 10.3390/v15091846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pearson H, Todd E, Ahrends M, Hover SE, Whitehouse A, Stacey M, Lippiat JD, Wilkens L, Fieguth HG, Danov O, et al. TMEM16A/ANO1 calcium-activated chloride channel as a novel target for the treatment of human respiratory syncytial virus infection. Thorax. 2021;76:64–72. doi: 10.1136/thoraxjnl-2020-215171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kennedy JL, Koziol-White CJ, Jeffus S, Rettiganti MR, Fisher P, Kurten M, Eze A, House S, Sikes JD, Askew E, et al. Effects of rhinovirus 39 infection on airway hyperresponsiveness to carbachol in human airways precision cut lung slices. J Allergy Clin Immunol. 2018;141:1887–e18901881. doi: 10.1016/j.jaci.2017.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parikh V, Scala J, Patel R, Corbi C, Lo D, Bochkov YA, Kennedy JL, Kurten RC, Liggett SB, Gern JE, Koziol-White CJ. Rhinovirus C15 induces Airway Hyperresponsiveness via Calcium mobilization in Airway smooth muscle. Am J Respir Cell Mol Biol. 2020;62:310–8. doi: 10.1165/rcmb.2019-0004OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gebski EB, Parikh V, Lam H, Kim N, Bochkov YA, Cao G, Panettieri RA, Jr, Kurten R, Gern J, An SS, Koziol-White CJ. Rhinovirus C15 attenuates relaxation and cAMP production in Human Airways and smooth muscle. Am J Respir Cell Mol Biol. 2023;69:172–81. doi: 10.1165/rcmb.2021-0526OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wronski S, Beinke S, Obernolte H, Belyaev NN, Saunders KA, Lennon MG, Schaudien D, Braubach P, Jonigk D, Warnecke G, et al. Rhinovirus-induced human lung tissue responses mimic chronic obstructive Pulmonary Disease and Asthma Gene Signatures. Am J Respir Cell Mol Biol. 2021;65:544–54. doi: 10.1165/rcmb.2020-0337OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Danov O, Lasswitz L, Obernolte H, Hesse C, Braun A, Wronski S, Sewald K. Rupintrivir reduces RV-induced T(H)-2 cytokine IL-4 in precision-cut lung slices (PCLS) of HDM-sensitized mice ex vivo. Respir Res. 2019;20:228. doi: 10.1186/s12931-019-1175-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reamon-Buettner SM, Niehof M, Hirth N, Danov O, Obernolte H, Braun A, Warnecke J, Sewald K, Wronski S. Transcriptomic analysis reveals priming of the Host Antiviral Interferon Signaling Pathway by Bronchobini((R)) resulting in Balanced Immune response to Rhinovirus infection in mouse lung tissue slices. Int J Mol Sci. 2019;20:2242–2267. doi: 10.3390/ijms20092242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abd El Rahman S, Winter C, El-Kenawy A, Neumann U, Herrler G. Differential sensitivity of well-differentiated avian respiratory epithelial cells to infection by different strains of infectious bronchitis virus. J Virol. 2010;84:8949–52. doi: 10.1128/JVI.00463-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miura Y, Ohkubo H, Nakano A, Bourke JE, Kanazawa S. Pathophysiological conditions induced by SARS-CoV-2 infection reduce ACE2 expression in the lung. Front Immunol. 2022;13:1028613. doi: 10.3389/fimmu.2022.1028613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ricke-Hoch M, Stelling E, Lasswitz L, Gunesch AP, Kasten M, Zapatero-Belinchon FJ, Brogden G, Gerold G, Pietschmann T, Montiel V, et al. Impaired immune response mediated by prostaglandin E2 promotes severe COVID-19 disease. PLoS ONE. 2021;16:e0255335. doi: 10.1371/journal.pone.0255335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu TT, Travaglini KJ, Rustagi A, Xu D, Zhang Y, Andronov L, Jang S, Gillich A, Dehghannasiri R, Martínez-Colón GJ et al. Interstitial macrophages are a focus of viral takeover and inflammation in COVID-19 initiation in human lung. J Exp Med 2024, 221:e20232192–2144. [DOI] [PMC free article] [PubMed]
- 36.Diesendorf V, Roll V, Geiger N, Fahr S, Obernolte H, Sewald K, Bodem J. Drug-induced phospholipidosis is not correlated with the inhibition of SARS-CoV-2 - inhibition of SARS-CoV-2 is cell line-specific. Front Cell Infect Microbiol. 2023;13:1100028. doi: 10.3389/fcimb.2023.1100028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Geiger N, Diesendorf V, Roll V, Konig EM, Obernolte H, Sewald K, Breidenbach J, Pillaiyar T, Gutschow M, Muller CE, Bodem J. Cell type-specific anti-viral effects of Novel SARS-CoV-2 main protease inhibitors. Int J Mol Sci. 2023;24:3972–3979. doi: 10.3390/ijms24043972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Geiger N, Konig EM, Oberwinkler H, Roll V, Diesendorf V, Fahr S, Obernolte H, Sewald K, Wronski S, Steinke M, Bodem J. Acetylsalicylic acid and salicylic acid inhibit SARS-CoV-2 Replication in Precision-Cut lung slices. Vaccines (Basel) 2022;10:1619–1626. doi: 10.3390/vaccines10101619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Low K, Moller R, Stegmann C, Becker M, Rehburg L, Obernolte H, Schaudien D, Oestereich L, Braun A, Kunz S, Gerold G. Luminescent reporter cells enable the identification of broad-spectrum antivirals against emerging viruses. J Med Virol. 2023;95:e29211. doi: 10.1002/jmv.29211. [DOI] [PubMed] [Google Scholar]
- 40.Zimniak M, Kirschner L, Hilpert H, Geiger N, Danov O, Oberwinkler H, Steinke M, Sewald K, Seibel J, Bodem J. The serotonin reuptake inhibitor Fluoxetine inhibits SARS-CoV-2 in human lung tissue. Sci Rep. 2021;11:5890. doi: 10.1038/s41598-021-85049-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Switalla S, Lauenstein L, Prenzler F, Knothe S, Forster C, Fieguth HG, Pfennig O, Schaumann F, Martin C, Guzman CA, et al. Natural innate cytokine response to immunomodulators and adjuvants in human precision-cut lung slices. Toxicol Appl Pharmacol. 2010;246:107–15. doi: 10.1016/j.taap.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 42.Donovan C, Royce SG, Vlahos R, Bourke JE. Lipopolysaccharide does not alter small airway reactivity in mouse lung slices. PLoS ONE. 2015;10:e0122069. doi: 10.1371/journal.pone.0122069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alkhouri H, Rumzhum NN, Rahman MM, FitzPatrick M, de Pedro M, Oliver BG, Bourke JE, Ammit AJ. TLR2 activation causes tachyphylaxis to beta2 -agonists in vitro and ex vivo: modelling bacterial exacerbation. Allergy. 2014;69:1215–22. doi: 10.1111/all.12449. [DOI] [PubMed] [Google Scholar]
- 44.Cramer N, Nawrot ML, Wege L, Dorda M, Sommer C, Danov O, Wronski S, Braun A, Jonigk D, Fischer S, et al. Competitive fitness of Pseudomonas aeruginosa isolates in human and murine precision-cut lung slices. Front Cell Infect Microbiol. 2022;12:992214. doi: 10.3389/fcimb.2022.992214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kolbe U, Yi B, Poth T, Saunders A, Boutin S, Dalpke AH. Early cytokine induction upon Pseudomonas aeruginosa infection in Murine Precision cut lung slices depends on sensing of bacterial viability. Front Immunol. 2020;11:598636. doi: 10.3389/fimmu.2020.598636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tony-Odigie A, Wilke L, Boutin S, Dalpke AH, Yi B. Commensal Bacteria in the cystic fibrosis airway Microbiome reduce P. Aeruginosa Induced inflammation. Front Cell Infect Microbiol. 2022;12:824101. doi: 10.3389/fcimb.2022.824101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sommer C, Reamon-Buettner SM, Niehof M, Hildebrand CB, Braun A, Sewald K, Dehmel S, Brandenberger C. Age-dependent inflammatory response is altered in an ex vivo model of bacterial pneumonia. Respir Res. 2024;25:15. doi: 10.1186/s12931-023-02609-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Qin L, Meng F, He H, Li S, Zhang H, Sun Y, Zhang W, An T, Cai X, Wang S. Inflammation plays a critical role in damage to the bronchiolar epithelium induced by Trueperella pyogenes in vitro and in vivo. Infect Immun. 2023;91:e0027323. doi: 10.1128/iai.00273-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Carranza-Rosales P, Carranza-Torres IE, Guzman-Delgado NE, Lozano-Garza G, Villarreal-Trevino L, Molina-Torres C, Villarreal JV, Vera-Cabrera L, Castro-Garza J. Modeling tuberculosis pathogenesis through ex vivo lung tissue infection. Tuberculosis (Edinb) 2017;107:126–32. doi: 10.1016/j.tube.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Molina-Torres CA, Flores-Castillo ON, Carranza-Torres IE, Guzman-Delgado NE, Viveros-Valdez E, Vera-Cabrera L, Ocampo-Candiani J, Verde-Star J, Castro-Garza J, Carranza-Rosales P. Ex vivo infection of murine precision-cut lung tissue slices with Mycobacterium abscessus: a model to study antimycobacterial agents. Ann Clin Microbiol Antimicrob. 2020;19:52. doi: 10.1186/s12941-020-00399-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Banerjee SK, Huckuntod SD, Mills SD, Kurten RC, Pechous RD. Modeling Pneumonic Plague in Human Precision-Cut lung slices highlights a role for the Plasminogen activator protease in facilitating type 3 secretion. Infect Immun. 2019;87:e0075–19. (13 pages). [DOI] [PMC free article] [PubMed]
- 52.Brann KR, Fullerton MS, Onyilagha FI, Prince AA, Kurten RC, Rom JS, Blevins JS, Smeltzer MS, Voth DE. Infection of primary human alveolar macrophages alters Staphylococcus aureus Toxin production and activity. Infect Immun 2019, 87:e00167–19. (17 pages). [DOI] [PMC free article] [PubMed]
- 53.Gaudino M, Lion A, Sagne E, Nagamine B, Oliva J, Terrier O, Errazuriz-Cerda E, Scribe A, Sikht FZ, Simon E, et al. The activation of the RIG-I/MDA5 signaling pathway upon influenza D virus infection impairs the pulmonary proinflammatory response triggered by Mycoplasma bovis Superinfection. J Virol. 2023;97:e0142322. doi: 10.1128/jvi.01423-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Munyonho FT, Clark RDE, Lin D, Khatun MS, Pungan D, Dai G, Kolls JK. Precision-cut lung slices as an ex vivo model to study Pneumocystis murina survival and antimicrobial susceptibility. mBio. 2024;15:e0146423. doi: 10.1128/mbio.01464-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Blomberg R, Sompel K, Hauer C, Smith AJ, Pena B, Driscoll J, Hume PS, Merrick DT, Tennis MA, Magin CM. Hydrogel-embedded Precision-Cut lung slices Model Lung Cancer Premalignancy Ex vivo. Adv Healthc Mater. 2024;13:e2302246. doi: 10.1002/adhm.202302246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Davies EJ, Dong M, Gutekunst M, Narhi K, van Zoggel HJ, Blom S, Nagaraj A, Metsalu T, Oswald E, Erkens-Schulze S, et al. Capturing complex tumour biology in vitro: histological and molecular characterisation of precision cut slices. Sci Rep. 2015;5:17187. doi: 10.1038/srep17187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sompel K, Smith AJ, Hauer C, Elango AP, Clamby ET, Keith RL, Tennis MA. Precision Cut lung slices as a preclinical model for Non-small Cell Lung Cancer Chemoprevention. Cancer Prev Res (Phila) 2023;16:247–58. doi: 10.1158/1940-6207.CAPR-23-0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vaira V, Fedele G, Pyne S, Fasoli E, Zadra G, Bailey D, Snyder E, Faversani A, Coggi G, Flavin R, et al. Preclinical model of organotypic culture for pharmacodynamic profiling of human tumors. Proc Natl Acad Sci U S A. 2010;107:8352–6. doi: 10.1073/pnas.0907676107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Salmon H, Franciszkiewicz K, Damotte D, Dieu-Nosjean MC, Validire P, Trautmann A, Mami-Chouaib F, Donnadieu E. Matrix architecture defines the preferential localization and migration of T cells into the stroma of human lung tumors. J Clin Invest. 2012;122:899–910. doi: 10.1172/JCI45817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Karger A, Mansouri S, Leisegang MS, Weigert A, Gunther S, Kuenne C, Wittig I, Zukunft S, Klatt S, Aliraj B, et al. ADPGK-AS1 long noncoding RNA switches macrophage metabolic and phenotypic state to promote lung cancer growth. EMBO J. 2023;42:e111620. doi: 10.15252/embj.2022111620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Azari F, Kennedy GT, Chang A, Low P, Basil M, Planer J, Katzen J, Eruslanov E, Albelda S, Singhal S. Molecular Imaging in Precision-Cut Non-small Cell Lung Cancer slices. Ann Thorac Surg. 2024;117:458–65. doi: 10.1016/j.athoracsur.2023.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dong M, Philippi C, Loretz B, Nafee N, Schaefer UF, Friedel G, Ammon-Treiber S, Griese EU, Lehr CM, Klotz U, Murdter TE. Tissue slice model of human lung cancer to investigate telomerase inhibition by nanoparticle delivery of antisense 2’-O-methyl-RNA. Int J Pharm. 2011;419:33–42. doi: 10.1016/j.ijpharm.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 63.Hu Z, Liu Y, Tang J, Luo R, Qin J, Mo Z, Xie J, Jiang X, Wei S, Lin C. LncRNA HHIP-AS1 suppresses lung squamous cell carcinoma by stabilizing HHIP mRNA. Life Sci. 2023;321:121578. doi: 10.1016/j.lfs.2023.121578. [DOI] [PubMed] [Google Scholar]
- 64.Narhi K, Nagaraj AS, Parri E, Turkki R, van Duijn PW, Hemmes A, Lahtela J, Uotinen V, Mayranpaa MI, Salmenkivi K, et al. Spatial aspects of oncogenic signalling determine the response to combination therapy in slice explants from Kras-driven lung tumours. J Pathol. 2018;245:101–13. doi: 10.1002/path.5059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Prades-Sagarra E, Laarakker F, Dissy J, Lieuwes NG, Biemans R, Dubail M, Fouillade C, Yaromina A, Dubois LJ. Caffeic acid Phenethyl Ester (CAPE), a natural polyphenol to increase the therapeutic window for lung adenocarcinomas. Radiother Oncol. 2024;190:110021. doi: 10.1016/j.radonc.2023.110021. [DOI] [PubMed] [Google Scholar]
- 66.Rosales Gerpe MC, van Vloten JP, Santry LA, de Jong J, Mould RC, Pelin A, Bell JC, Bridle BW, Wootton SK. Use of Precision-Cut lung slices as an Ex vivo Tool for evaluating viruses and viral vectors for Gene and oncolytic therapy. Mol Ther Methods Clin Dev. 2018;10:245–56. doi: 10.1016/j.omtm.2018.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rubio K, Romero-Olmedo AJ, Sarvari P, Swaminathan G, Ranvir VP, Rogel-Ayala DG, Cordero J, Gunther S, Mehta A, Bassaly B, et al. Non-canonical integrin signaling activates EGFR and RAS-MAPK-ERK signaling in small cell lung cancer. Theranostics. 2023;13:2384–407. doi: 10.7150/thno.79493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.van Rijt SH, Bolukbas DA, Argyo C, Datz S, Lindner M, Eickelberg O, Konigshoff M, Bein T, Meiners S. Protease-mediated release of chemotherapeutics from mesoporous silica nanoparticles to ex vivo human and mouse lung tumors. ACS Nano. 2015;9:2377–89. doi: 10.1021/nn5070343. [DOI] [PubMed] [Google Scholar]
- 69.Bai Y, Li G, Yung L, Yu PB, Ai X. Intrapulmonary arterial contraction assay reveals region-specific deregulation of vasoreactivity to lung injuries. Am J Physiol Lung Cell Mol Physiol. 2023;325:L114–24. doi: 10.1152/ajplung.00293.2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Henriquez M, Fonseca M, Perez-Zoghbi JF. Purinergic receptor stimulation induces calcium oscillations and smooth muscle contraction in small pulmonary veins. J Physiol. 2018;596:2491–506. doi: 10.1113/JP274731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Perez JF, Sanderson MJ. The contraction of smooth muscle cells of intrapulmonary arterioles is determined by the frequency of Ca2 + oscillations induced by 5-HT and KCl. J Gen Physiol. 2005;125:555–67. doi: 10.1085/jgp.200409217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rieg AD, Suleiman S, Anker C, Verjans E, Rossaint R, Uhlig S, Martin C. PDGF-BB regulates the pulmonary vascular tone: impact of prostaglandins, calcium, MAPK- and PI3K/AKT/mTOR signalling and actin polymerisation in pulmonary veins of guinea pigs. Respir Res. 2018;19:120. doi: 10.1186/s12931-018-0829-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Springer J, Fischer A. Substance P-induced pulmonary vascular remodelling in precision cut lung slices. Eur Respir J. 2003;22:596–601. doi: 10.1183/09031936.03.00027903. [DOI] [PubMed] [Google Scholar]
- 74.Springer J, Wagner S, Subramamiam A, McGregor GP, Groneberg DA, Fischer A. BDNF-overexpression regulates the reactivity of small pulmonary arteries to neurokinin A. Regul Pept. 2004;118:19–23. doi: 10.1016/j.regpep.2003.10.020. [DOI] [PubMed] [Google Scholar]
- 75.Perez-Zoghbi JF, Sanderson MJ. Endothelin-induced contraction of bronchiole and pulmonary arteriole smooth muscle cells is regulated by intracellular Ca2 + oscillations and Ca2 + sensitization. Am J Physiol Lung Cell Mol Physiol. 2007;293:L1000–1011. doi: 10.1152/ajplung.00184.2007. [DOI] [PubMed] [Google Scholar]
- 76.Maihofer NA, Suleiman S, Dreymuller D, Manley PW, Rossaint R, Uhlig S, Martin C, Rieg AD. Imatinib relaxes the pulmonary venous bed of guinea pigs. Respir Res. 2017;18:32. doi: 10.1186/s12931-017-0514-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rieg AD, Bunting NA, Cranen C, Suleiman S, Spillner JW, Schnoring H, Schroder T, von Stillfried S, Braunschweig T, Manley PW, et al. Tyrosine kinase inhibitors relax pulmonary arteries in human and murine precision-cut lung slices. Respir Res. 2019;20:111. doi: 10.1186/s12931-019-1074-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rieg AD, Rossaint R, Uhlig S, Martin C. Cardiovascular agents affect the tone of pulmonary arteries and veins in precision-cut lung slices. PLoS ONE. 2011;6:e29698. doi: 10.1371/journal.pone.0029698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rieg AD, Rossaint R, Verjans E, Maihofer NA, Uhlig S, Martin C. Levosimendan relaxes pulmonary arteries and veins in Precision-Cut lung slices - the role of KATP-Channels, cAMP and cGMP. PLoS ONE. 2013;8:e66195. doi: 10.1371/journal.pone.0066195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rieg AD, Suleiman S, Bunting NA, Verjans E, Spillner J, Schnoring H, Kalverkamp S, Schroder T, von Stillfried S, Braunschweig T, et al. Levosimendan reduces segmental pulmonary vascular resistance in isolated perfused rat lungs and relaxes human pulmonary vessels. PLoS ONE. 2020;15:e0233176. doi: 10.1371/journal.pone.0233176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rieg AD, Suleiman S, Perez-Bouza A, Braunschweig T, Spillner JW, Schroder T, Verjans E, Schalte G, Rossaint R, Uhlig S, Martin C. Milrinone relaxes pulmonary veins in guinea pigs and humans. PLoS ONE. 2014;9:e87685. doi: 10.1371/journal.pone.0087685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Studley WR, Lamanna E, Martin KA, Nold-Petry CA, Royce SG, Woodman OL, Ritchie RH, Qin CX, Bourke JE. The small-molecule formyl peptide receptor biased agonist, compound 17b, is a vasodilator and anti-inflammatory in mouse precision-cut lung slices. Br J Pharmacol 2023; online ahead of print: 1-15. [DOI] [PubMed]
- 83.Suleiman S, Klassen S, Katz I, Balakirski G, Krabbe J, von Stillfried S, Kintsler S, Braunschweig T, Babendreyer A, Spillner J, et al. Argon reduces the pulmonary vascular tone in rats and humans by GABA-receptor activation. Sci Rep. 2019;9:1902. doi: 10.1038/s41598-018-38267-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Milara J, Gabarda E, Juan G, Ortiz JL, Guijarro R, Martorell M, Morcillo EJ, Cortijo J. Bosentan inhibits cigarette smoke-induced endothelin receptor expression in pulmonary arteries. Eur Respir J. 2012;39:927–38. doi: 10.1183/09031936.00021411. [DOI] [PubMed] [Google Scholar]
- 85.Wright JL, Churg A. Short-term exposure to cigarette smoke induces endothelial dysfunction in small intrapulmonary arteries: analysis using guinea pig precision cut lung slices. J Appl Physiol (1985) 2008;104:1462–9. doi: 10.1152/japplphysiol.00520.2007. [DOI] [PubMed] [Google Scholar]
- 86.Milara J, Roger I, Montero P, Artigues E, Escrivá J, Perez-Vizcaino F, Cortijo J. Targeting IL-11 system as a treatment of pulmonary arterial hypertension. Pharmacol Res. 2023;197:106985. doi: 10.1016/j.phrs.2023.106985. [DOI] [PubMed] [Google Scholar]
- 87.Desireddi JR, Farrow KN, Marks JD, Waypa GB, Schumacker PT. Hypoxia increases ROS signaling and cytosolic ca(2+) in pulmonary artery smooth muscle cells of mouse lungs slices. Antioxid Redox Signal. 2010;12:595–602. doi: 10.1089/ars.2009.2862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dong YN, Hsu FC, Koziol-White CJ, Stepanova V, Jude J, Gritsiuta A, Rue R, Mott R, Coulter DA, Panettieri RA, Jr, et al. Functional NMDA receptors are expressed by human pulmonary artery smooth muscle cells. Sci Rep. 2021;11:8205. doi: 10.1038/s41598-021-87667-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Murtaza G, Paddenberg R, Pfeil U, Goldenberg A, Mermer P, Kummer W. Hypoxia-induced pulmonary vasoconstriction of intra-acinar arteries is impaired in NADPH oxidase 4 gene-deficient mice. Pulm Circ. 2018;8:2045894018808240. doi: 10.1177/2045894018808240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Paddenberg R, Faulhammer P, Goldenberg A, Gries B, Heinl J, Kummer W. Impact of modulators of mitochondrial ATP-sensitive potassium channel (mitoK(ATP)) on hypoxic pulmonary vasoconstriction. Adv Exp Med Biol. 2009;648:361–8. doi: 10.1007/978-90-481-2259-2_41. [DOI] [PubMed] [Google Scholar]
- 91.Paddenberg R, Konig P, Faulhammer P, Goldenberg A, Pfeil U, Kummer W. Hypoxic vasoconstriction of partial muscular intra-acinar pulmonary arteries in murine precision cut lung slices. Respir Res. 2006;7:93. doi: 10.1186/1465-9921-7-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Paddenberg R, Tiefenbach M, Faulhammer P, Goldenberg A, Gries B, Pfeil U, Lips KS, Piruat JI, Lopez-Barneo J, Schermuly RT, et al. Mitochondrial complex II is essential for hypoxia-induced pulmonary vasoconstriction of intra- but not of pre-acinar arteries. Cardiovasc Res. 2012;93:702–10. doi: 10.1093/cvr/cvr359. [DOI] [PubMed] [Google Scholar]
- 93.Shahzad T, Chao CM, Hadzic S, Behnke J, Biebach L, Bottcher-Friebertshauser E, Wilhelm J, Hilgendorff A, Zimmer KP, Morty RE, et al. TRAIL protects the immature lung from hyperoxic injury. Cell Death Dis. 2022;13:614. doi: 10.1038/s41419-022-05072-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Waypa GB, Marks JD, Guzy RD, Mungai PT, Schriewer JM, Dokic D, Ball MK, Schumacker PT. Superoxide generated at mitochondrial complex III triggers acute responses to hypoxia in the pulmonary circulation. Am J Respir Crit Care Med. 2013;187:424–32. doi: 10.1164/rccm.201207-1294OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sucre JMS, Vickers KC, Benjamin JT, Plosa EJ, Jetter CS, Cutrone A, Ransom M, Anderson Z, Sheng Q, Fensterheim BA, et al. Hyperoxia Injury in the developing lung is mediated by mesenchymal expression of Wnt5A. Am J Respir Crit Care Med. 2020;201:1249–62. doi: 10.1164/rccm.201908-1513OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kryvenko V, Wessendorf M, Tello K, Herold S, Morty RE, Seeger W, Vadasz I. Hypercapnia induces inositol-requiring enzyme 1alpha-Driven endoplasmic reticulum-associated degradation of the Na,K-ATPase beta-subunit. Am J Respir Cell Mol Biol. 2021;65:615–29. doi: 10.1165/rcmb.2021-0114OC. [DOI] [PubMed] [Google Scholar]
- 97.Bui CB, Kolodziej M, Lamanna E, Elgass K, Sehgal A, Rudloff I, Schwenke DO, Tsuchimochi H, Kroon M, Cho SX, et al. Interleukin-1 receptor antagonist protects newborn mice against pulmonary hypertension. Front Immunol. 2019;10:1480. doi: 10.3389/fimmu.2019.01480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ragionieri L, Scalera E, Zoboli M, Ciccimarra R, Petracco G, Gazza F, Cacchioli A, Storti M, Catozzi C, Ricci F, Ravanetti F. Preterm rabbit-derived Precision Cut lung slices as alternative model of bronchopulmonary dysplasia in preclinical study: a morphological fine-tuning approach. Ann Anat. 2023;246:152039. doi: 10.1016/j.aanat.2022.152039. [DOI] [PubMed] [Google Scholar]
- 99.Bartman CM, Schiliro M, Nesbitt L, Lee KK, Prakash YS, Pabelick CM. Exogenous hydrogen sulfide attenuates hyperoxia effects on neonatal mouse airways. Am J Physiol Lung Cell Mol Physiol. 2024;326:L52–64. doi: 10.1152/ajplung.00196.2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dutra Silva J, Su Y, Calfee CS, Delucchi KL, Weiss D, McAuley DF, O’Kane C, Krasnodembskaya AD. Mesenchymal stromal cell extracellular vesicles rescue mitochondrial dysfunction and improve barrier integrity in clinically relevant models of ARDS. Eur Respir J. 2021;58:2002978–2996. [DOI] [PMC free article] [PubMed]
- 101.Kryvenko V, Alberro-Brage A, Fysikopoulos A, Wessendorf M, Tello K, Morty RE, Herold S, Seeger W, Samakovlis C, Vadasz I. Clathrin-mediated albumin clearance in alveolar epithelial cells of Murine Precision-Cut lung slices. Int J Mol Sci. 2023;24:2644–2659. doi: 10.3390/ijms24032644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Jandl K, Marsh LM, Mutgan AC, Crnkovic S, Valzano F, Zabini D, Hoffmann J, Foris V, Gschwandtner E, Klepetko W, et al. Impairment of the NKT-STAT1-CXCL9 Axis contributes to Vessel Fibrosis in Pulmonary Hypertension caused by lung fibrosis. Am J Respir Crit Care Med. 2022;206:981–98. doi: 10.1164/rccm.202201-0142OC. [DOI] [PubMed] [Google Scholar]
- 103.Zehendner CM, Valasarajan C, Werner A, Boeckel JN, Bischoff FC, John D, Weirick T, Glaser SF, Rossbach O, Jae N, et al. Long noncoding RNA TYKRIL plays a role in Pulmonary Hypertension via the p53-mediated regulation of PDGFRbeta. Am J Respir Crit Care Med. 2020;202:1445–57. doi: 10.1164/rccm.201910-2041OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Huang Q, Chen Y, Shen S, Wang Y, Liu L, Wu S, Xu W, Zhao W, Lin M, Wu J. Klotho antagonizes pulmonary fibrosis through suppressing pulmonary fibroblasts activation, migration, and extracellular matrix production: a therapeutic implication for idiopathic pulmonary fibrosis. Aging. 2020;12:5812–31. doi: 10.18632/aging.102978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Rubio K, Singh I, Dobersch S, Sarvari P, Gunther S, Cordero J, Mehta A, Wujak L, Cabrera-Fuentes H, Chao CM, et al. Inactivation of nuclear histone deacetylases by EP300 disrupts the MiCEE complex in idiopathic pulmonary fibrosis. Nat Commun. 2019;10:2229. doi: 10.1038/s41467-019-10066-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Decaris ML, Schaub JR, Chen C, Cha J, Lee GG, Rexhepaj M, Ho SS, Rao V, Marlow MM, Kotak P, et al. Dual inhibition of alpha(v)beta(6) and alpha(v)beta(1) reduces fibrogenesis in lung tissue explants from patients with IPF. Respir Res. 2021;22:265. doi: 10.1186/s12931-021-01863-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Knoell J, Chillappagari S, Knudsen L, Korfei M, Dartsch R, Jonigk D, Kuehnel MP, Hoetzenecker K, Guenther A, Mahavadi P. PACS2-TRPV1 axis is required for ER-mitochondrial tethering during ER stress and lung fibrosis. Cell Mol Life Sci. 2022;79:151. doi: 10.1007/s00018-022-04189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Menzel V, Ziegler M, Hante N, Sake JA, Santos-Martinez MJ, Ehrhardt C, Kasper M, Barth K. Fyn-kinase and caveolin-1 in the alveolar epithelial junctional adherence complex contribute to the early stages of pulmonary fibrosis. Eur J Pharm Sci. 2022;175:106236. doi: 10.1016/j.ejps.2022.106236. [DOI] [PubMed] [Google Scholar]
- 109.Cohen ML, Brumwell AN, Che Ho T, Montas G, Golden JA, Jones KD, Wolters PJ, Wei Y, Chapman HA, Le Saux CJ. A fibroblast-dependent TGFbeta1/sFRP2 noncanonical Wnt signaling axis underlies epithelial metaplasia in idiopathic pulmonary fibrosis. bioRxiv. 2023. preprint.
- 110.Chioccioli M, Roy S, Newell R, Pestano L, Dickinson B, Rigby K, Herazo-Maya J, Jenkins G, Ian S, Saini G, et al. A lung targeted miR-29 mimic as a therapy for pulmonary fibrosis. EBioMedicine. 2022;85:104304. doi: 10.1016/j.ebiom.2022.104304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ahmadvand N, Carraro G, Jones MR, Shalashova I, Noori A, Wilhelm J, Baal N, Khosravi F, Chen C, Zhang JS, et al. Cell-Surface Programmed Death Ligand-1 Expression Identifies a Sub-Population of Distal Epithelial Cells Enriched in Idiopathic Pulmonary Fibrosis. Cells. 2022;11:1593–1609. doi: 10.3390/cells11101593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Barnthaler T, Theiler A, Zabini D, Trautmann S, Stacher-Priehse E, Lanz I, Klepetko W, Sinn K, Flick H, Scheidl S, et al. Inhibiting eicosanoid degradation exerts antifibrotic effects in a pulmonary fibrosis mouse model and human tissue. J Allergy Clin Immunol. 2020;145:818–e833811. doi: 10.1016/j.jaci.2019.11.032. [DOI] [PubMed] [Google Scholar]
- 113.Chillappagari S, Schwarz J, Kesireddy V, Knoell J, Korfei M, Hoetzenecker K, Schmitz ML, Behl C, Bellusci S, Guenther A, Mahavadi P. Therapeutic induction of Bcl2-associated athanogene 3-mediated autophagy in idiopathic pulmonary fibrosis. Clin Transl Med. 2022;12:e935. doi: 10.1002/ctm2.935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ji J, Zheng S, Liu Y, Xie T, Zhu X, Nie Y, Shen Y, Han X. Increased expression of OPN contributes to idiopathic pulmonary fibrosis and indicates a poor prognosis. J Transl Med. 2023;21:640. doi: 10.1186/s12967-023-04279-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Khalil N, Xu YD, O’Connor R, Duronio V. Proliferation of pulmonary interstitial fibroblasts is mediated by transforming growth factor-beta1-induced release of extracellular fibroblast growth factor-2 and phosphorylation of p38 MAPK and JNK. J Biol Chem. 2005;280:43000–9. doi: 10.1074/jbc.M510441200. [DOI] [PubMed] [Google Scholar]
- 116.Marchal-Duval E, Homps-Legrand M, Froidure A, Jaillet M, Ghanem M, Lou D, Justet A, Maurac A, Vadel A, Fortas E et al. Identification of paired-related Homeobox Protein 1 as a key mesenchymal transcription factor in pulmonary fibrosis. Elife. 2023;12:e79840–872. [DOI] [PMC free article] [PubMed]
- 117.Ruigrok MJR, El Amasi KEM, Leeming DJ, Sand JMB, Frijlink HW, Hinrichs WLJ, Olinga P. Silencing heat shock protein 47 (HSP47) in Fibrogenic Precision-Cut lung slices: a surprising lack of effects on Fibrogenesis? Front Med (Lausanne) 2021;8:607962. doi: 10.3389/fmed.2021.607962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tsoyi K, Liang X, De Rossi G, Ryter SW, Xiong K, Chu SG, Liu X, Ith B, Celada LJ, Romero F, et al. CD148 Deficiency in fibroblasts promotes the development of Pulmonary Fibrosis. Am J Respir Crit Care Med. 2021;204:312–25. doi: 10.1164/rccm.202008-3100OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wasnick R, Korfei M, Piskulak K, Henneke I, Wilhelm J, Mahavadi P, Dartsch RC, von der Beck D, Koch M, Shalashova I, et al. Notch1 induces defective epithelial surfactant Processing and Pulmonary Fibrosis. Am J Respir Crit Care Med. 2023;207:283–99. doi: 10.1164/rccm.202105-1284OC. [DOI] [PubMed] [Google Scholar]
- 120.Wei Y, Dong W, Jackson J, Ho TC, Le Saux CJ, Brumwell A, Li X, Klesney-Tait J, Cohen ML, Wolters PJ, Chapman HA. Blocking LOXL2 and TGFbeta1 signalling induces collagen I turnover in precision-cut lung slices derived from patients with idiopathic pulmonary fibrosis. Thorax. 2021;76:729–32. doi: 10.1136/thoraxjnl-2020-215745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kortekaas RK, Geillinger-Kastle KE, Borghuis T, Belharch K, Webster M, Timens W, Burgess JK, Gosens R. Interleukin-11 disrupts alveolar epithelial progenitor function. ERJ Open Res. 2023;9:00679–2022. (12 pages). [DOI] [PMC free article] [PubMed]
- 122.Alsafadi HN, Staab-Weijnitz CA, Lehmann M, Lindner M, Peschel B, Konigshoff M, Wagner DE. An ex vivo model to induce early fibrosis-like changes in human precision-cut lung slices. Am J Physiol Lung Cell Mol Physiol. 2017;312:L896–902. doi: 10.1152/ajplung.00084.2017. [DOI] [PubMed] [Google Scholar]
- 123.Cedilak M, Banjanac M, Belamaric D, Paravic Radicevic A, Faraho I, Ilic K, Cuzic S, Glojnaric I, Erakovic Haber V, Bosnar M. Precision-cut lung slices from bleomycin treated animals as a model for testing potential therapies for idiopathic pulmonary fibrosis. Pulm Pharmacol Ther. 2019;55:75–83. doi: 10.1016/j.pupt.2019.02.005. [DOI] [PubMed] [Google Scholar]
- 124.Khan MM, Poeckel D, Halavatyi A, Zukowska-Kasprzyk J, Stein F, Vappiani J, Sevin DC, Tischer C, Zinn N, Eley JD et al. An integrated multiomic and quantitative label-free microscopy-based approach to study pro-fibrotic signalling in ex vivo human precision-cut lung slices. Eur Respir J. 2021;58:2000220–243. [DOI] [PMC free article] [PubMed]
- 125.Lang NJ, Gote-Schniering J, Porras-Gonzalez D, Yang L, De Sadeleer LJ, Jentzsch RC, Shitov VA, Zhou S, Ansari M, Agami A, et al. Ex vivo tissue perturbations coupled to single-cell RNA-seq reveal multilineage cell circuit dynamics in human lung fibrogenesis. Sci Transl Med. 2023;15:eadh0908. doi: 10.1126/scitranslmed.adh0908. [DOI] [PubMed] [Google Scholar]
- 126.Ahangari F, Becker C, Foster DG, Chioccioli M, Nelson M, Beke K, Wang X, Justet A, Adams T, Readhead B, et al. Saracatinib, a selective src kinase inhibitor, blocks fibrotic responses in Preclinical models of Pulmonary Fibrosis. Am J Respir Crit Care Med. 2022;206:1463–79. doi: 10.1164/rccm.202010-3832OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hansen NU, Karsdal MA, Brockbank S, Cruwys S, Ronnow S, Leeming DJ. Tissue turnover of collagen type I, III and elastin is elevated in the PCLS model of IPF and can be restored back to vehicle levels using a phosphodiesterase inhibitor. Respir Res. 2016;17:76. doi: 10.1186/s12931-016-0394-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lofdahl A, Wenglen C, Rydell-Tormanen K, Westergren-Thorsson G, Larsson-Callerfelt AK. Effects of 5-Hydroxytryptamine class 2 receptor antagonists on Bronchoconstriction and Pulmonary remodeling processes. Am J Pathol. 2018;188:1113–9. doi: 10.1016/j.ajpath.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 129.Mercer PF, Woodcock HV, Eley JD, Plate M, Sulikowski MG, Durrenberger PF, Franklin L, Nanthakumar CB, Man Y, Genovese F, et al. Exploration of a potent PI3 kinase/mTOR inhibitor as a novel anti-fibrotic agent in IPF. Thorax. 2016;71:701–11. doi: 10.1136/thoraxjnl-2015-207429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Tatler AL, Barnes J, Habgood A, Goodwin A, McAnulty RJ, Jenkins G. Caffeine inhibits TGFbeta activation in epithelial cells, interrupts fibroblast responses to TGFbeta, and reduces established fibrosis in ex vivo precision-cut lung slices. Thorax. 2016;71:565–7. doi: 10.1136/thoraxjnl-2015-208215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Koudelka A, Cechova V, Rojas M, Mitash N, Bondonese A, St Croix C, Ross MA, Freeman BA. Fatty acid nitroalkene reversal of established lung fibrosis. Redox Biol. 2022;50:102226. doi: 10.1016/j.redox.2021.102226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Hesse C, Beneke V, Konzok S, Diefenbach C, Bulow Sand JM, Ronnow SR, Karsdal MA, Jonigk D, Sewald K, Braun A, et al. Nintedanib modulates type III collagen turnover in viable precision-cut lung slices from bleomycin-treated rats and patients with pulmonary fibrosis. Respir Res. 2022;23:201. doi: 10.1186/s12931-022-02116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Lehmann M, Buhl L, Alsafadi HN, Klee S, Hermann S, Mutze K, Ota C, Lindner M, Behr J, Hilgendorff A, et al. Differential effects of Nintedanib and Pirfenidone on lung alveolar epithelial cell function in ex vivo murine and human lung tissue cultures of pulmonary fibrosis. Respir Res. 2018;19:175. doi: 10.1186/s12931-018-0876-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Maher JM, Zhang R, Palanisamy G, Perkins K, Liu L, Brassil P, McNamara A, Lo A, Hughes AD, Kanodia J, et al. Lung-restricted ALK5 inhibition avoids systemic toxicities associated with TGFbeta pathway inhibition. Toxicol Appl Pharmacol. 2022;438:115905. doi: 10.1016/j.taap.2022.115905. [DOI] [PubMed] [Google Scholar]
- 135.Stancil IT, Michalski JE, Hennessy CE, Hatakka KL, Yang IV, Kurche JS, Rincon M, Schwartz DA. Interleukin-6-dependent epithelial fluidization initiates fibrotic lung remodeling. Sci Transl Med. 2022;14:eabo5254. doi: 10.1126/scitranslmed.abo5254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Stephenson KE, Porte J, Kelly A, Wallace WA, Huntington CE, Overed-Sayer CL, Cohen ES, Jenkins RG, John AE. The IL-33:ST2 axis is unlikely to play a central fibrogenic role in idiopathic pulmonary fibrosis. Respir Res. 2023;24:89. doi: 10.1186/s12931-023-02334-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.James AL, Hogg JC, Dunn LA, Pare PD. The use of the internal perimeter to compare airway size and to calculate smooth muscle shortening. Am Rev Respir Dis. 1988;138:136–9. doi: 10.1164/ajrccm/138.1.136. [DOI] [PubMed] [Google Scholar]
- 138.Calzetta L, Page C, Matera MG, Cazzola M, Rogliani P. Use of human airway smooth muscle in vitro and ex vivo to investigate drugs for the treatment of chronic obstructive respiratory disorders. Br J Pharmacol. 2024;181:610–39. doi: 10.1111/bph.16272. [DOI] [PubMed] [Google Scholar]
- 139.Wohlsen A, Martin C, Vollmer E, Branscheid D, Magnussen H, Becker WM, Lepp U, Uhlig S. The early allergic response in small airways of human precision-cut lung slices. Eur Respir J. 2003;21:1024–32. doi: 10.1183/09031936.03.00027502. [DOI] [PubMed] [Google Scholar]
- 140.Wohlsen A, Uhlig S, Martin C. Immediate allergic response in small airways. Am J Respir Crit Care Med. 2001;163:1462–9. doi: 10.1164/ajrccm.163.6.2007138. [DOI] [PubMed] [Google Scholar]
- 141.Cooper PR, Lamb R, Day ND, Branigan PJ, Kajekar R, San Mateo L, Hornby PJ, Panettieri RA., Jr TLR3 activation stimulates cytokine secretion without altering agonist-induced human small airway contraction or relaxation. Am J Physiol Lung Cell Mol Physiol. 2009;297:L530–537. doi: 10.1152/ajplung.00133.2009. [DOI] [PubMed] [Google Scholar]
- 142.Cooper PR, Zhang J, Damera G, Hoshi T, Zopf DA, Panettieri RA., Jr C-027 inhibits IgE-mediated passive sensitization bronchoconstriction and acts as a histamine and serotonin antagonist in human airways. Allergy Asthma Proc. 2011;32:359–65. doi: 10.2500/aap.2011.32.3460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Duan S, Koziol-White CJ, Jester WF, Jr, Smith SA, Nycholat CM, Macauley MS, Panettieri RA. Jr., Paulson JC: CD33 recruitment inhibits IgE-mediated anaphylaxis and desensitizes mast cells to allergen. J Clin Invest. 2019;129:1387–401. doi: 10.1172/JCI125456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Koziol-White CJ, Jia Y, Baltus GA, Cooper PR, Zaller DM, Crackower MA, Sirkowski EE, Smock S, Northrup AB, Himes BE, et al. Inhibition of spleen tyrosine kinase attenuates IgE-mediated airway contraction and mediator release in human precision cut lung slices. Br J Pharmacol. 2016;173:3080–7. doi: 10.1111/bph.13550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lamb DJ, Wollin SL, Schnapp A, Bischoff D, Erb KJ, Bouyssou T, Guilliard B, Strasser C, Wex E, Blum S, et al. BI 1002494, a Novel Potent and selective oral spleen tyrosine kinase inhibitor, displays Differential Potency in Human basophils and B cells. J Pharmacol Exp Ther. 2016;357:554–61. doi: 10.1124/jpet.116.233155. [DOI] [PubMed] [Google Scholar]
- 146.Folkerts J, Redegeld F, Folkerts G, Blokhuis B, van den Berg MPM, de Bruijn MJW, van Junt IWFJ, Tam T, Galli SY. Butyrate inhibits human mast cell activation via epigenetic regulation of FcepsilonRI-mediated signaling. Allergy. 2020;75:1966–78. doi: 10.1111/all.14254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Khandwala A, Damiani P, Weinryb I. Antigen-induced release of histamine from passively sensitized guinea pig lung slices. I. Optimum conditions for in vitro passive sensitization and challenge with antigen. Int Arch Allergy Appl Immunol. 1979;59:34–44. doi: 10.1159/000232237. [DOI] [PubMed] [Google Scholar]
- 148.Romberger DJ, Heires AJ, Nordgren TM, Souder CP, West W, Liu XD, Poole JA, Toews ML, Wyatt TA. Proteases in agricultural dust induce lung inflammation through PAR-1 and PAR-2 activation. Am J Physiol Lung Cell Mol Physiol. 2015;309:L388–399. doi: 10.1152/ajplung.00025.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Redes JL, Basu T, Ram-Mohan S, Ghosh CC, Chan EC, Sek AC, Zhao M, Krishnan R, Rosenberg HF, Druey KM. Aspergillus Fumigatus-secreted alkaline protease 1 Mediates Airways hyperresponsiveness in severe asthma. Immunohorizons. 2019;3:368–77. doi: 10.4049/immunohorizons.1900046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Madigan LA, Wong GS, Gordon EM, Chen WS, Balenga N, Koziol-White CJ, Panettieri RA, Jr, Levine SJ, Druey KM. RGS4 overexpression in lung attenuates Airway Hyperresponsiveness in mice. Am J Respir Cell Mol Biol. 2018;58:89–98. doi: 10.1165/rcmb.2017-0109OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Donovan C, Royce SG, Esposito J, Tran J, Ibrahim ZA, Tang ML, Bailey S, Bourke JE. Differential effects of allergen challenge on large and small airway reactivity in mice. PLoS ONE. 2013;8:e74101. doi: 10.1371/journal.pone.0074101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Cooper PR, Poll CT, Barnes PJ, Sturton RG. Involvement of IL-13 in tobacco smoke-induced changes in the structure and function of rat intrapulmonary airways. Am J Respir Cell Mol Biol. 2010;43:220–6. doi: 10.1165/rcmb.2009-0117OC. [DOI] [PubMed] [Google Scholar]
- 153.Jiang H, Xie Y, Abel PW, Toews ML, Townley RG, Casale TB, Tu Y. Targeting phosphoinositide 3-kinase gamma in airway smooth muscle cells to suppress interleukin-13-induced mouse airway hyperresponsiveness. J Pharmacol Exp Ther. 2012;342:305–11. doi: 10.1124/jpet.111.189704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kellner J, Gamarra F, Welsch U, Jorres RA, Huber RM, Bergner A. IL-13Ralpha2 reverses the effects of IL-13 and IL-4 on bronchial reactivity and acetylcholine-induced ca + signaling. Int Arch Allergy Immunol. 2007;142:199–210. doi: 10.1159/000097022. [DOI] [PubMed] [Google Scholar]
- 155.Koziol-White CJ, Yoo EJ, Cao G, Zhang J, Papanikolaou E, Pushkarsky I, Andrews A, Himes BE, Damoiseaux RD, Liggett SB, et al. Inhibition of PI3K promotes dilation of human small airways in a rho kinase-dependent manner. Br J Pharmacol. 2016;173:2726–38. doi: 10.1111/bph.13542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Li G, Cohen JA, Martines C, Ram-Mohan S, Brain JD, Krishnan R, Ai X, Bai Y. Preserving Airway smooth muscle contraction in Precision-Cut lung slices. Sci Rep. 2020;10:6480. doi: 10.1038/s41598-020-63225-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Rynne J, Ortiz-Zapater E, Bagley DC, Zanin O, Doherty G, Kanabar V, Ward J, Jackson DJ, Parsons M, Rosenblatt J, et al. The RNA binding proteins ZFP36L1 and ZFP36L2 are dysregulated in airway epithelium in human and a murine model of asthma. Front Cell Dev Biol. 2023;11:1241008. doi: 10.3389/fcell.2023.1241008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Chen J, Miller M, Unno H, Rosenthal P, Sanderson MJ, Broide DH. Orosomucoid-like 3 (ORMDL3) upregulates airway smooth muscle proliferation, contraction, and ca(2+) oscillations in asthma. J Allergy Clin Immunol. 2018;142:207–e218206. doi: 10.1016/j.jaci.2017.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Dragunas G, Woest ME, Nijboer S, Bos ST, van Asselt J, de Groot AP, Vohlidalova E, Vermeulen CJ, Ditz B, Vonk JM, et al. Cholinergic neuroplasticity in asthma driven by TrkB signaling. FASEB J. 2020;34:7703–17. doi: 10.1096/fj.202000170R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Aven L, Paez-Cortez J, Achey R, Krishnan R, Ram-Mohan S, Cruikshank WW, Fine A, Ai X. An NT4/TrkB-dependent increase in innervation links early-life allergen exposure to persistent airway hyperreactivity. FASEB J. 2014;28:897–907. doi: 10.1096/fj.13-238212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Chachi L, Alzahrani A, Koziol-White C, Biddle M, Bagadood R, Panettieri RA, Jr, Bradding P, Amrani Y. Increased beta2-adrenoceptor phosphorylation in airway smooth muscle in severe asthma: possible role of mast cell-derived growth factors. Clin Exp Immunol. 2018;194:253–8. doi: 10.1111/cei.13191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Damera G, Druey KM, Cooper PR, Krymskaya VP, Soberman RJ, Amrani Y, Hoshi T, Brightling CE, Panettieri RA., Jr An RGS4-mediated phenotypic switch of bronchial smooth muscle cells promotes fixed airway obstruction in asthma. PLoS ONE. 2012;7:e28504. doi: 10.1371/journal.pone.0028504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Martin C, Uhlig S, Ullrich V. Cytokine-induced bronchoconstriction in precision-cut lung slices is dependent upon cyclooxygenase-2 and thromboxane receptor activation. Am J Respir Cell Mol Biol. 2001;24:139–45. doi: 10.1165/ajrcmb.24.2.3545. [DOI] [PubMed] [Google Scholar]
- 164.Ojiaku CA, Cao G, Zhu W, Yoo EJ, Shumyatcher M, Himes BE, An SS, Panettieri RA., Jr TGF-beta1 evokes human airway smooth muscle cell shortening and hyperresponsiveness via Smad3. Am J Respir Cell Mol Biol. 2018;58:575–84. doi: 10.1165/rcmb.2017-0247OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Robinett KS, Koziol-White CJ, Akoluk A, An SS, Panettieri RA, Jr, Liggett SB. Bitter taste receptor function in asthmatic and nonasthmatic human airway smooth muscle cells. Am J Respir Cell Mol Biol. 2014;50:678–83. doi: 10.1165/rcmb.2013-0439RC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Balenga NA, Jester W, Jiang M, Panettieri RA, Jr, Druey KM. Loss of regulator of G protein signaling 5 promotes airway hyperresponsiveness in the absence of allergic inflammation. J Allergy Clin Immunol. 2014;134:451–9. doi: 10.1016/j.jaci.2014.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Brown SM, Koarai A, Sturton RG, Nicholson AG, Barnes PJ, Donnelly LE. A role for M(2) and M(3) muscarinic receptors in the contraction of rat and human small airways. Eur J Pharmacol. 2013;702:109–15. doi: 10.1016/j.ejphar.2013.01.054. [DOI] [PubMed] [Google Scholar]
- 168.Carr R, 3rd, Koziol-White C, Zhang J, Lam H, An SS, Tall GG, Panettieri RA, Jr, Benovic JL. Interdicting Gq activation in Airway Disease by receptor-dependent and receptor-independent mechanisms. Mol Pharmacol. 2016;89:94–104. doi: 10.1124/mol.115.100339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Delmotte P, Sanderson MJ. Effects of albuterol isomers on the contraction and Ca2 + signaling of small airways in mouse lung slices. Am J Respir Cell Mol Biol. 2008;38:524–31. doi: 10.1165/rcmb.2007-0214OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Delmotte P, Sanderson MJ. Effects of formoterol on contraction and Ca2 + signaling of mouse airway smooth muscle cells. Am J Respir Cell Mol Biol. 2010;42:373–81. doi: 10.1165/rcmb.2008-0403OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Elfellah MS, Turnbull MJ. Effect of pretreatment with bronchodilator drugs on in vitro responsiveness of guinea pig lung adenylate cyclase. Eur J Pharmacol. 1978;51:211–7. doi: 10.1016/0014-2999(78)90406-5. [DOI] [PubMed] [Google Scholar]
- 172.Martin C, Ullrich V, Uhlig S. Effects of the thromboxane receptor agonist U46619 and endothelin-1 on large and small airways. Eur Respir J. 2000;16:316–23. doi: 10.1034/j.1399-3003.2000.16b21.x. [DOI] [PubMed] [Google Scholar]
- 173.Yang Z, Balenga N, Cooper PR, Damera G, Edwards R, Brightling CE, Panettieri RA, Jr, Druey KM. Regulator of G-protein signaling-5 inhibits bronchial smooth muscle contraction in severe asthma. Am J Respir Cell Mol Biol. 2012;46:823–32. doi: 10.1165/rcmb.2011-0110OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Kummer W, Wiegand S, Akinci S, Wessler I, Schinkel AH, Wess J, Koepsell H, Haberberger RV, Lips KS. Role of acetylcholine and polyspecific cation transporters in serotonin-induced bronchoconstriction in the mouse. Respir Res. 2006;7:65. doi: 10.1186/1465-9921-7-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Ressmeyer AR, Bai Y, Delmotte P, Uy KF, Thistlethwaite P, Fraire A, Sato O, Ikebe M, Sanderson MJ. Human airway contraction and formoterol-induced relaxation is determined by Ca2 + oscillations and Ca2 + sensitivity. Am J Respir Cell Mol Biol. 2010;43:179–91. doi: 10.1165/rcmb.2009-0222OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Sausbier M, Zhou XB, Beier C, Sausbier U, Wolpers D, Maget S, Martin C, Dietrich A, Ressmeyer AR, Renz H, et al. Reduced rather than enhanced cholinergic airway constriction in mice with ablation of the large conductance Ca2+-activated K + channel. FASEB J. 2007;21:812–22. doi: 10.1096/fj.06-7167com. [DOI] [PubMed] [Google Scholar]
- 177.Yang Z, Cooper PR, Damera G, Mukhopadhyay I, Cho H, Kehrl JH, Panettieri RA, Jr, Druey KM. Beta-agonist-associated reduction in RGS5 expression promotes airway smooth muscle hyper-responsiveness. J Biol Chem. 2011;286:11444–55. doi: 10.1074/jbc.M110.212480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Yoo EJ, Cao G, Koziol-White CJ, Ojiaku CA, Sunder K, Jude JA, Michael JV, Lam H, Pushkarsky I, Damoiseaux R, et al. Galpha(12) facilitates shortening in human airway smooth muscle by modulating phosphoinositide 3-kinase-mediated activation in a RhoA-dependent manner. Br J Pharmacol. 2017;174:4383–95. doi: 10.1111/bph.14040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Kummer W, Wiegand S, Akinci S, Schinkel AH, Wess J, Koepsell H, Haberberger RV, Lips KS. Role of acetylcholine and muscarinic receptors in serotonin-induced bronchoconstriction in the mouse. J Mol Neurosci. 2006;30:67–8. doi: 10.1385/JMN:30:1:67. [DOI] [PubMed] [Google Scholar]
- 180.Bai Y, Guedes AGP, Krishnan R, Ai X. CD38 plays an age-related role in cholinergic deregulation of airway smooth muscle contractility. J Allergy Clin Immunol. 2022;149:1643–e16541648. doi: 10.1016/j.jaci.2021.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Kuo JF, Kuo WN. Regulation by beta-adrenergic receptor and muscarinic cholinergic receptor activation of intracellular cyclic AMP and cyclic GMP levels in rat lung slices. Biochem Biophys Res Commun. 1973;55:660–5. doi: 10.1016/0006-291X(73)91195-9. [DOI] [PubMed] [Google Scholar]
- 182.Stoner J, Manganiello VC, Vaughan M. Effects of bradykinin and Indomethacin on cyclic GMP and cyclic AMP in lung slices. Proc Natl Acad Sci U S A. 1973;70:3830–3. doi: 10.1073/pnas.70.12.3830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Croisier H, Tan X, Chen J, Sneyd J, Sanderson MJ, Brook BS. Ryanodine receptor sensitization results in abnormal calcium signaling in airway smooth muscle cells. Am J Respir Cell Mol Biol. 2015;53:703–11. doi: 10.1165/rcmb.2014-0386OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Bai Y, Sanderson MJ. Modulation of the Ca2 + sensitivity of airway smooth muscle cells in murine lung slices. Am J Physiol Lung Cell Mol Physiol. 2006;291:L208–221. doi: 10.1152/ajplung.00494.2005. [DOI] [PubMed] [Google Scholar]
- 185.Boie S, Chen J, Sanderson MJ, Sneyd J. The relative contributions of store-operated and voltage-gated ca(2+) channels to the control of ca(2+) oscillations in airway smooth muscle. J Physiol. 2017;595:3129–41. doi: 10.1113/JP272996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Chen J, Sanderson MJ. Store-operated calcium entry is required for sustained contraction and ca(2+) oscillations of airway smooth muscle. J Physiol. 2017;595:3203–18. doi: 10.1113/JP272694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Zeng Z, Cheng M, Li M, Wang T, Wen F, Sanderson MJ, Sneyd J, Shen Y, Chen J. Inherent differences of small airway contraction and ca(2+) oscillations in airway smooth muscle cells between BALB/c and C57BL/6 mouse strains. Front Cell Dev Biol. 2023;11:1202573. doi: 10.3389/fcell.2023.1202573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Bai Y, Sanderson MJ. Airway smooth muscle relaxation results from a reduction in the frequency of Ca2 + oscillations induced by a cAMP-mediated inhibition of the IP3 receptor. Respir Res. 2006;7:34. doi: 10.1186/1465-9921-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Bai Y, Sanderson MJ. The contribution of Ca2 + signaling and Ca2 + sensitivity to the regulation of airway smooth muscle contraction is different in rats and mice. Am J Physiol Lung Cell Mol Physiol. 2009;296:L947–958. doi: 10.1152/ajplung.90288.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Bai Y, Zhang M, Sanderson MJ. Contractility and Ca2 + signaling of smooth muscle cells in different generations of mouse airways. Am J Respir Cell Mol Biol. 2007;36:122–30. doi: 10.1165/rcmb.2006-0036OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Bergner A, Sanderson MJ. Acetylcholine-induced calcium signaling and contraction of airway smooth muscle cells in lung slices. J Gen Physiol. 2002;119:187–98. doi: 10.1085/jgp.119.2.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Bergner A, Sanderson MJ. Airway contractility and smooth muscle ca(2+) signaling in lung slices from different mouse strains. J Appl Physiol (1985) 2003;95:1325–32. doi: 10.1152/japplphysiol.00272.2003. [DOI] [PubMed] [Google Scholar]
- 193.Jiang H, Abel PW, Toews ML, Deng C, Casale TB, Xie Y, Tu Y. Phosphoinositide 3-kinase gamma regulates airway smooth muscle contraction by modulating calcium oscillations. J Pharmacol Exp Ther. 2010;334:703–9. doi: 10.1124/jpet.110.168518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Mukherjee S, Trice J, Shinde P, Willis RE, Pressley TA, Perez-Zoghbi JF. Ca2 + oscillations, Ca2 + sensitization, and contraction activated by protein kinase C in small airway smooth muscle. J Gen Physiol. 2013;141:165–78. doi: 10.1085/jgp.201210876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Bai Y, Edelmann M, Sanderson MJ. The contribution of inositol 1,4,5-trisphosphate and ryanodine receptors to agonist-induced ca(2+) signaling of airway smooth muscle cells. Am J Physiol Lung Cell Mol Physiol. 2009;297:L347–361. doi: 10.1152/ajplung.90559.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Perez JF, Sanderson MJ. The frequency of calcium oscillations induced by 5-HT, ACH, and KCl determine the contraction of smooth muscle cells of intrapulmonary bronchioles. J Gen Physiol. 2005;125:535–53. doi: 10.1085/jgp.200409216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Oenema TA, Maarsingh H, Smit M, Groothuis GM, Meurs H, Gosens R. Bronchoconstriction induces TGF-beta release and Airway Remodelling in Guinea Pig Lung Slices. PLoS ONE. 2013;8:e65580. doi: 10.1371/journal.pone.0065580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Royce SG, Nold MF, Bui C, Donovan C, Lam M, Lamanna E, Rudloff I, Bourke JE, Nold-Petry CA. Airway Remodeling and Hyperreactivity in a model of Bronchopulmonary Dysplasia and their modulation by IL-1 receptor antagonist. Am J Respir Cell Mol Biol. 2016;55:858–68. doi: 10.1165/rcmb.2016-0031OC. [DOI] [PubMed] [Google Scholar]
- 199.Cooper PR, Kurten RC, Zhang J, Nicholls DJ, Dainty IA, Panettieri RA. Formoterol and Salmeterol induce a similar degree of beta2-adrenoceptor tolerance in human small airways but via different mechanisms. Br J Pharmacol. 2011;163:521–32. doi: 10.1111/j.1476-5381.2011.01257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Cooper PR, Panettieri RA., Jr Steroids completely reverse albuterol-induced beta(2)-adrenergic receptor tolerance in human small airways. J Allergy Clin Immunol. 2008;122:734–40. doi: 10.1016/j.jaci.2008.07.040. [DOI] [PubMed] [Google Scholar]
- 201.FitzPatrick M, Donovan C, Bourke JE. Prostaglandin E2 elicits greater bronchodilation than salbutamol in mouse intrapulmonary airways in lung slices. Pulm Pharmacol Ther. 2014;28:68–76. doi: 10.1016/j.pupt.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 202.Koziol-White CJ, Ghosh A, Sandner P, Erzurum SE, Stuehr DJ, Panettieri RA., Jr Soluble Guanylate Cyclase agonists Induce Bronchodilation in Human Small airways. Am J Respir Cell Mol Biol. 2020;62:43–8. doi: 10.1165/rcmb.2019-0001OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Larsson-Callerfelt AK, Dahlen SE, Kuhl AR, Lex D, Uhlig S, Martin C. Modulation of antigen-induced responses by serotonin and prostaglandin E2 via EP1 and EP4 receptors in the peripheral rat lung. Eur J Pharmacol. 2013;699:141–9. doi: 10.1016/j.ejphar.2012.11.039. [DOI] [PubMed] [Google Scholar]
- 204.Maarsingh H, Oldenburger A, Han B, Zuidhof AB, Elzinga CRS, Timens W, Meurs H, Sopi RB, Schmidt M. Effects of (a Combination of) the Beta(2)-Adrenoceptor Agonist Indacaterol and the Muscarinic Receptor Antagonist Glycopyrrolate on Intrapulmonary Airway Constriction. Cells. 2021;10:1237–1255. doi: 10.3390/cells10051237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Mikami M, Perez-Zoghbi JF, Zhang Y, Emala CW. Attenuation of murine and human airway contraction by a peptide fragment of the cytoskeleton regulatory protein gelsolin. Am J Physiol Lung Cell Mol Physiol. 2019;316:L105–13. doi: 10.1152/ajplung.00368.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Simoen V, Christophe B. Effect of levocetirizine on the contraction induced by histamine on isolated rabbit bronchioles from precision-cut lung slices. Pharmacology. 2006;78:61–5. doi: 10.1159/000095508. [DOI] [PubMed] [Google Scholar]
- 207.Sturton RG, Trifilieff A, Nicholson AG, Barnes PJ. Pharmacological characterization of indacaterol, a novel once daily inhaled 2 adrenoceptor agonist, on small airways in human and rat precision-cut lung slices. J Pharmacol Exp Ther. 2008;324:270–5. doi: 10.1124/jpet.107.129296. [DOI] [PubMed] [Google Scholar]
- 208.Ahn S, Maarsingh H, Walker JK, Liu S, Hegde A, Sumajit HC, Kahsai AW, Lefkowitz RJ. Allosteric modulator potentiates beta2AR agonist-promoted bronchoprotection in asthma models. J Clin Invest. 2023;133:e167337–350. [DOI] [PMC free article] [PubMed]
- 209.Goldklang MP, Perez-Zoghbi JF, Trischler J, Nkyimbeng T, Zakharov SI, Shiomi T, Zelonina T, Marks AR, D’Armiento JM, Marx SO. Treatment of experimental asthma using a single small molecule with anti-inflammatory and BK channel-activating properties. FASEB J. 2013;27:4975–86. doi: 10.1096/fj.13-235176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Jude JA, Dainty I, Karmacharya N, Jester W, Panettieri R. The Bronchoprotective effects of dual pharmacology, muscarinic receptor antagonist and beta(2) adrenergic receptor agonist Navafenterol in Human Small airways. Cells. 2023;12:240–48. doi: 10.3390/cells12020240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Kistemaker LEM, Oenema TA, Baarsma HA, Bos IST, Schmidt M, Facchinetti F, Civelli M, Villetti G, Gosens R. The PDE4 inhibitor CHF-6001 and LAMAs inhibit bronchoconstriction-induced remodeling in lung slices. Am J Physiol Lung Cell Mol Physiol. 2017;313:L507–15. doi: 10.1152/ajplung.00069.2017. [DOI] [PubMed] [Google Scholar]
- 212.Martin C, Goggel R, Dal Piaz V, Vergelli C, Giovannoni P, Ernst M, Uhlig S. Airway relaxant and anti-inflammatory properties of a PDE4 inhibitor with low affinity for the high-affinity rolipram binding site. Naunyn Schmiedebergs Arch Pharmacol. 2002;365:284–9. doi: 10.1007/s00210-001-0525-7. [DOI] [PubMed] [Google Scholar]
- 213.Xu S, Karmacharya N, Woo J, Cao G, Guo C, Gow A, Panettieri RA, Jr, Jude JA. Starving a cell promotes Airway smooth muscle relaxation: inhibition of glycolysis attenuates excitation-contraction coupling. Am J Respir Cell Mol Biol. 2023;68:39–48. doi: 10.1165/rcmb.2021-0495OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Amrani Y, Syed F, Huang C, Li K, Liu V, Jain D, Keslacy S, Sims MW, Baidouri H, Cooper PR, et al. Expression and activation of the oxytocin receptor in airway smooth muscle cells: regulation by TNFalpha and IL-13. Respir Res. 2010;11:104. doi: 10.1186/1465-9921-11-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.An SS, Wang WC, Koziol-White CJ, Ahn K, Lee DY, Kurten RC, Panettieri RA, Jr, Liggett SB. TAS2R activation promotes airway smooth muscle relaxation despite beta(2)-adrenergic receptor tachyphylaxis. Am J Physiol Lung Cell Mol Physiol. 2012;303:L304–311. doi: 10.1152/ajplung.00126.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Anaparti V, Ilarraza R, Orihara K, Stelmack GL, Ojo OO, Mahood TH, Unruh H, Halayko AJ, Moqbel R. NMDA receptors mediate contractile responses in human airway smooth muscle cells. Am J Physiol Lung Cell Mol Physiol. 2015;308:L1253–1264. doi: 10.1152/ajplung.00402.2014. [DOI] [PubMed] [Google Scholar]
- 217.Edelson JD, Makhlina M, Silvester KR, Vengurlekar SS, Chen X, Zhang J, Koziol-White CJ, Cooper PR, Hallam TJ, Hay DW, Panettieri RA., Jr In vitro and in vivo pharmacological profile of PL-3994, a novel cyclic peptide (Hept-cyclo(Cys-His-Phe-d-Ala-Gly-Arg-d-Nle-Asp-Arg-Ile-Ser-Cys)-Tyr-[Arg mimetic]-NH(2)) natriuretic peptide receptor-A agonist that is resistant to neutral endopeptidase and acts as a bronchodilator. Pulm Pharmacol Ther. 2013;26:229–238. doi: 10.1016/j.pupt.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Gallos G, Yocum GT, Siviski ME, Yim PD, Fu XW, Poe MM, Cook JM, Harrison N, Perez-Zoghbi J, Emala CW. Sr.: selective targeting of the alpha5-subunit of GABAA receptors relaxes airway smooth muscle and inhibits cellular calcium handling. Am J Physiol Lung Cell Mol Physiol. 2015;308:L931–942. doi: 10.1152/ajplung.00107.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Hempel P, Klein V, Michely A, Boll S, Rieg AD, Spillner J, Braunschweig T, von Stillfried S, Wagner N, Martin C, et al. Amitriptyline inhibits bronchoconstriction and directly promotes dilatation of the airways. Respir Res. 2023;24:262. doi: 10.1186/s12931-023-02580-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Lam M, Royce SG, Donovan C, Jelinic M, Parry LJ, Samuel CS, Bourke JE. Serelaxin elicits bronchodilation and enhances beta-adrenoceptor-mediated Airway Relaxation. Front Pharmacol. 2016;7:406. doi: 10.3389/fphar.2016.00406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Perez-Zoghbi JF, Sajorda DR, Webb DA, Arnold LA, Emala CW, Yocum GT. Imidazobenzodiazepine PI320 relaxes mouse Peripheral Airways by inhibiting calcium mobilization. Am J Respir Cell Mol Biol. 2022;67:482–90. doi: 10.1165/rcmb.2022-0084OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Tan X, Sanderson MJ. Bitter tasting compounds dilate airways by inhibiting airway smooth muscle calcium oscillations and calcium sensitivity. Br J Pharmacol. 2014;171:646–62. doi: 10.1111/bph.12460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Vaghasiya J, Dalvand A, Sikarwar A, Mangat D, Ragheb M, Kowatsch K, Pandey D, Hosseini SM, Hackett TL, Karimi-Abdolrezaee S, et al. Oxidized phosphatidylcholines trigger TRPA1 and ryanodine receptor-dependent Airway smooth muscle contraction. Am J Respir Cell Mol Biol. 2023;69:649–65. doi: 10.1165/rcmb.2022-0457OC. [DOI] [PubMed] [Google Scholar]
- 224.van den Berg MPM, Nijboer-Brinksma S, Bos IST, van den Berge M, Lamb D, van Faassen M, Kema IP, Gosens R, Kistemaker LEM. The novel TRPA1 antagonist BI01305834 inhibits ovalbumin-induced bronchoconstriction in guinea pigs. Respir Res. 2021;22:48. doi: 10.1186/s12931-021-01638-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Woo JA, Castano M, Kee TR, Lee J, Koziol-White CJ, An SS, Kim D, Kang DE, Liggett SB. A Par3/LIM Kinase/Cofilin pathway mediates human airway smooth muscle relaxation by TAS2R14. Am J Respir Cell Mol Biol. 2023;68:417–29. doi: 10.1165/rcmb.2022-0303OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Yocum GT, Chen J, Choi CH, Townsend EA, Zhang Y, Xu D, Fu XW, Sanderson MJ, Emala CW. Role of transient receptor potential vanilloid 1 in the modulation of airway smooth muscle tone and calcium handling. Am J Physiol Lung Cell Mol Physiol. 2017;312:L812–21. doi: 10.1152/ajplung.00064.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Ghosh A, Koziol-White CJ, Asosingh K, Cheng G, Ruple L, Groneberg D, Friebe A, Comhair SA, Stasch JP, Panettieri RA, Jr, et al. Soluble guanylate cyclase as an alternative target for bronchodilator therapy in asthma. Proc Natl Acad Sci U S A. 2016;113:E2355–2362. doi: 10.1073/pnas.1524398113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Yocum GT, Perez-Zoghbi JF, Danielsson J, Kuforiji AS, Zhang Y, Li G, Rashid Roni MS, Kodali R, Stafford DC, Arnold LA, et al. A novel GABA(A) receptor ligand MIDD0301 with limited blood-brain barrier penetration relaxes airway smooth muscle ex vivo and in vivo. Am J Physiol Lung Cell Mol Physiol. 2019;316:L385–90. doi: 10.1152/ajplung.00356.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Maarsingh H, Bidan CM, Brook BS, Zuidhof AB, Elzinga CRS, Smit M, Oldenburger A, Gosens R, Timens W, Meurs H. Small airway hyperresponsiveness in COPD: relationship between structure and function in lung slices. Am J Physiol Lung Cell Mol Physiol. 2019;316:L537–46. doi: 10.1152/ajplung.00325.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Wu CY, Cilic A, Pak O, Dartsch RC, Wilhelm J, Wujak M, Lo K, Brosien M, Zhang R, Alkoudmani I, et al. CEACAM6 as a Novel Therapeutic Target to boost HO-1-mediated antioxidant defense in COPD. Am J Respir Crit Care Med. 2023;207:1576–90. doi: 10.1164/rccm.202208-1603OC. [DOI] [PubMed] [Google Scholar]
- 231.Yeung-Luk BH, Wally A, Swaby C, Jauregui S, Lee E, Zhang R, Chen D, Luk SH, Upadya N, Tieng E, et al. Epigenetic reprogramming drives epithelial disruption in COPD. Am J Respir Cell Mol Biol. 2023;70:165–177. doi: 10.1165/rcmb.2023-0147OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Uhl FE, Vierkotten S, Wagner DE, Burgstaller G, Costa R, Koch I, Lindner M, Meiners S, Eickelberg O, Konigshoff M. Preclinical validation and imaging of wnt-induced repair in human 3D lung tissue cultures. Eur Respir J. 2015;46:1150–66. doi: 10.1183/09031936.00183214. [DOI] [PubMed] [Google Scholar]
- 233.van der Koog L, Boerrigter MJ, Gorter IC, Gosens R, Nagelkerke A. Lung fibroblast-derived extracellular vesicles and soluble factors alleviate elastase-induced lung injury. Eur J Pharmacol. 2024;974:176612. doi: 10.1016/j.ejphar.2024.176612. [DOI] [PubMed] [Google Scholar]
- 234.Van Dijk EM, Culha S, Menzen MH, Bidan CM, Gosens R. Elastase-Induced Parenchymal disruption and Airway Hyper Responsiveness in Mouse Precision cut lung slices: toward an ex vivo COPD Model. Front Physiol. 2016;7:657. doi: 10.3389/fphys.2016.00657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Kim JH, Schaible N, Hall JK, Bartolak-Suki E, Deng Y, Herrmann J, Sonnenberg A, Behrsing HP, Lutchen KR, Krishnan R, Suki B. Multiscale stiffness of human emphysematous precision cut lung slices. Sci Adv. 2023;9:eadf2535. doi: 10.1126/sciadv.adf2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Golitz F, Herbert J, Worek F, Wille T. AChE reactivation in precision-cut lung slices following organophosphorus compound poisoning. Toxicol Lett. 2024;392:75–83. doi: 10.1016/j.toxlet.2023.12.014. [DOI] [PubMed] [Google Scholar]
- 237.Wigenstam E, Artursson E, Bucht A, Thors L. Supplemental treatment to atropine improves the efficacy to reverse nerve agent induced bronchoconstriction. Chem Biol Interact. 2022;364:110061. doi: 10.1016/j.cbi.2022.110061. [DOI] [PubMed] [Google Scholar]
- 238.Wigenstam E, Artursson E, Bucht A, Thors L. Pharmacological prophylaxis with pyridostigmine bromide against nerve agents adversely impact on airway function in an ex vivo rat precision-cut lung slice model. Toxicol Mech Methods. 2023;33:732–40. doi: 10.1080/15376516.2023.2238060. [DOI] [PubMed] [Google Scholar]
- 239.Wigenstam E, Forsberg E, Bucht A, Thors L. Efficacy of atropine and scopolamine on airway contractions following exposure to the nerve agent VX. Toxicol Appl Pharmacol. 2021;419:115512. doi: 10.1016/j.taap.2021.115512. [DOI] [PubMed] [Google Scholar]
- 240.Agren L, Elfsmark L, Akfur C, Hagglund L, Ekstrand-Hammarstrom B, Jonasson S. N-acetyl cysteine protects against chlorine-induced tissue damage in an ex vivo model. Toxicol Lett. 2020;322:58–65. doi: 10.1016/j.toxlet.2020.01.006. [DOI] [PubMed] [Google Scholar]
- 241.Gustafson A, Elfsmark L, Karlsson T, Jonasson S. N-acetyl cysteine mitigates lung damage and inflammation after chlorine exposure in vivo and ex vivo. Toxicol Appl Pharmacol. 2023;479:116714. doi: 10.1016/j.taap.2023.116714. [DOI] [PubMed] [Google Scholar]
- 242.Agren L, Elfsmark L, Akfur C, Jonasson S. High concentrations of ammonia induced cytotoxicity and bronchoconstriction in a precision-cut lung slices rat model. Toxicol Lett. 2021;349:51–60. doi: 10.1016/j.toxlet.2021.06.001. [DOI] [PubMed] [Google Scholar]
- 243.Tigges J, Worek F, Thiermann H, Wille T. Organophosphorus pesticides exhibit compound specific effects in rat precision-cut lung slices (PCLS): mechanisms involved in airway response, cytotoxicity, inflammatory activation and antioxidative defense. Arch Toxicol. 2022;96:321–34. doi: 10.1007/s00204-021-03186-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Gutierrez B, Aggarwal T, Erguven H, Stone MRL, Guo C, Bellomo A, Abramova E, Stevenson ER, Laskin DL, Gow AJ, Izgu EC. Direct assessment of nitrative stress in lipid environments: applications of a designer lipid-based biosensor for peroxynitrite. iScience. 2023;26:108567. doi: 10.1016/j.isci.2023.108567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Bellomo A, Herbert J, Kudlak MJ, Laskin JD, Gow AJ, Laskin DL. Identification of early events in nitrogen mustard pulmonary toxicity that are independent of infiltrating inflammatory cells using precision cut lung slices. Toxicol Appl Pharmacol. 2024;486:116941. doi: 10.1016/j.taap.2024.116941. [DOI] [PubMed] [Google Scholar]
- 246.Donovan C, Seow HJ, Royce SG, Bourke JE, Vlahos R. Alteration of Airway Reactivity and reduction of ryanodine receptor expression by cigarette smoke in mice. Am J Respir Cell Mol Biol. 2015;53:471–8. doi: 10.1165/rcmb.2014-0400OC. [DOI] [PubMed] [Google Scholar]
- 247.Geraghty P, Baumlin N, Salathe MA, Foronjy RF, D’Armiento JM. Glutathione Peroxidase-1 Suppresses the Unfolded Protein Response upon Cigarette Smoke Exposure. Mediators Inflamm. 2016;2016:9461289. doi: 10.1155/2016/9461289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Lagowala DA, Wally A, Wilmsen K, Kim B, Yeung-Luk B, Choi J, Swaby C, Luk M, Feller L, Ghosh B et al. Microphysiological models of Lung epithelium-alveolar macrophage co-cultures to Study Chronic Lung Disease. Adv Biol (Weinh). 2023:e2300165. online ahead of print. [DOI] [PubMed]
- 249.Obernolte H, Niehof M, Braubach P, Fieguth HG, Jonigk D, Pfennig O, Tschernig T, Warnecke G, Braun A, Sewald K. Cigarette smoke alters inflammatory genes and the extracellular matrix - investigations on viable sections of peripheral human lungs. Cell Tissue Res. 2022;387:249–60. doi: 10.1007/s00441-021-03553-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Herbert J, Kelty JS, Laskin JD, Laskin DL, Gow AJ. Menthol flavoring in e-cigarette condensate causes pulmonary dysfunction and cytotoxicity in precision cut lung slices. Am J Physiol Lung Cell Mol Physiol. 2023;324:L345–57. doi: 10.1152/ajplung.00222.2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Zuo H, Han B, Poppinga WJ, Ringnalda L, Kistemaker LEM, Halayko AJ, Gosens R, Nikolaev VO, Schmidt M. Cigarette smoke up-regulates PDE3 and PDE4 to decrease cAMP in airway cells. Br J Pharmacol. 2018;175:2988–3006. doi: 10.1111/bph.14347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Henjakovic M, Martin C, Hoymann HG, Sewald K, Ressmeyer AR, Dassow C, Pohlmann G, Krug N, Uhlig S, Braun A. Ex vivo lung function measurements in precision-cut lung slices (PCLS) from chemical allergen-sensitized mice represent a suitable alternative to in vivo studies. Toxicol Sci. 2008;106:444–53. doi: 10.1093/toxsci/kfn178. [DOI] [PubMed] [Google Scholar]
- 253.Lauenstein L, Switalla S, Prenzler F, Seehase S, Pfennig O, Forster C, Fieguth H, Braun A, Sewald K. Assessment of immunotoxicity induced by chemicals in human precision-cut lung slices (PCLS) Toxicol Vitro. 2014;28:588–99. doi: 10.1016/j.tiv.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 254.Jude J, Botelho D, Karmacharya N, Cao GY, Jester W, Panettieri RA., Jr Salicylic acid amplifies Carbachol-induced bronchoconstriction in human precision-cut lung slices. Respir Res. 2019;20:72. doi: 10.1186/s12931-019-1034-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Jude J, Koziol-White C, Scala J, Yoo E, Jester W, Maute C, Dalton P, Panettieri R. Jr.: Formaldehyde induces rho-Associated kinase activity to Evoke Airway Hyperresponsiveness. Am J Respir Cell Mol Biol. 2016;55:542–53. doi: 10.1165/rcmb.2015-0254OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Behrsing HP, Furniss MJ, Davis M, Tomaszewski JE, Parchment RE. In vitro exposure of precision-cut lung slices to 2-(4-amino-3-methylphenyl)-5-fluorobenzothiazole lysylamide dihydrochloride (NSC 710305, Phortress) increases inflammatory cytokine content and tissue damage. Toxicol Sci. 2013;131:470–9. doi: 10.1093/toxsci/kfs319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Lin CJ, Yang PC, Hsu MT, Yew FH, Liu TY, Shun CT, Tyan SW, Lee TC. Induction of pulmonary fibrosis in organ-cultured rat lung by cadmium chloride and transforming growth factor-beta1. Toxicology. 1998;127:157–66. doi: 10.1016/S0300-483X(98)00025-0. [DOI] [PubMed] [Google Scholar]
- 258.Neuhaus V, Danov O, Konzok S, Obernolte H, Dehmel S, Braubach P, Jonigk D, Fieguth HG, Zardo P, Warnecke G et al. Assessment of the cytotoxic and Immunomodulatory effects of substances in Human Precision-cut lung slices. J Vis Exp. 2018;9:e57042–56. [DOI] [PMC free article] [PubMed]
- 259.Watson CY, Damiani F, Ram-Mohan S, Rodrigues S, de Moura Queiroz P, Donaghey TC, Rosenblum Lichtenstein JH, Brain JD, Krishnan R, Molina RM. Screening for Chemical toxicity using Cryopreserved Precision Cut Lung slices. Toxicol Sci. 2016;150:225–33. doi: 10.1093/toxsci/kfv320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Cooper PR, Mesaros AC, Zhang J, Christmas P, Stark CM, Douaidy K, Mittelman MA, Soberman RJ, Blair IA, Panettieri RA. 20-HETE mediates ozone-induced, neutrophil-independent airway hyper-responsiveness in mice. PLoS ONE. 2010;5:e10235. doi: 10.1371/journal.pone.0010235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Switalla S, Knebel J, Ritter D, Krug N, Braun A, Sewald K. Effects of acute in vitro exposure of murine precision-cut lung slices to gaseous nitrogen dioxide and ozone in an air-liquid interface (ALI) culture. Toxicol Lett. 2010;196:117–24. doi: 10.1016/j.toxlet.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 262.Wang M, Cooper PR, Jiang M, Zhao H, Hui Y, Yao Y, Tate JC, Damera G, Lawson JA, Jester WF, Jr, et al. Deletion of microsomal prostaglandin E synthase-1 does not alter ozone-induced airway hyper-responsiveness. J Pharmacol Exp Ther. 2010;334:63–8. doi: 10.1124/jpet.110.166678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Le Prieur E, Vaz E, Bion A, Dionnet F, Morin JP. Toxicity of diesel engine exhausts in an in vitro model of lung slices in biphasic organotypic culture: induction of a proinflammatory and apoptotic response. Arch Toxicol. 2000;74:460–6. doi: 10.1007/s002040000138. [DOI] [PubMed] [Google Scholar]
- 264.Maikawa CL, Zimmerman N, Rais K, Shah M, Hawley B, Pant P, Jeong CH, Delgado-Saborit JM, Volckens J, Evans G, et al. Murine precision-cut lung slices exhibit acute responses following exposure to gasoline direct injection engine emissions. Sci Total Environ. 2016;568:1102–9. doi: 10.1016/j.scitotenv.2016.06.173. [DOI] [PubMed] [Google Scholar]
- 265.Cervantes D, Schaunaman N, Downey GP, Chu HW, Day BJ. Desert particulate matter from Afghanistan increases airway obstruction in human distal lungs exposed to type 2 cytokine IL-13. Front Med (Lausanne) 2023;10:1177665. doi: 10.3389/fmed.2023.1177665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Shrestha D, Massey N, Bhat SM, Jelesijevic T, Sahin O, Zhang Q, Bailey KL, Poole JA, Charavaryamath C. Nrf2 activation protects against Organic Dust and Hydrogen Sulfide exposure Induced Epithelial Barrier loss and K. pneumoniae Invasion. Front Cell Infect Microbiol. 2022;12:848773. doi: 10.3389/fcimb.2022.848773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Schleputz M, Rieg AD, Seehase S, Spillner J, Perez-Bouza A, Braunschweig T, Schroeder T, Bernau M, Lambermont V, Schlumbohm C, et al. Neurally mediated airway constriction in human and other species: a comparative study using precision-cut lung slices (PCLS) PLoS ONE. 2012;7:e47344. doi: 10.1371/journal.pone.0047344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Ressmeyer AR, Larsson AK, Vollmer E, Dahlen SE, Uhlig S, Martin C. Characterisation of guinea pig precision-cut lung slices: comparison with human tissues. Eur Respir J. 2006;28:603–11. doi: 10.1183/09031936.06.00004206. [DOI] [PubMed] [Google Scholar]
- 269.Seehase S, Schleputz M, Switalla S, Matz-Rensing K, Kaup FJ, Zoller M, Schlumbohm C, Fuchs E, Lauenstein HD, Winkler C, et al. Bronchoconstriction in nonhuman primates: a species comparison. J Appl Physiol (1985) 2011;111:791–8. doi: 10.1152/japplphysiol.00162.2011. [DOI] [PubMed] [Google Scholar]
- 270.Ruigrok MJR, Xian JL, Frijlink HW, Melgert BN, Hinrichs WLJ, Olinga P. siRNA-mediated protein knockdown in precision-cut lung slices. Eur J Pharm Biopharm. 2018;133:339–48. doi: 10.1016/j.ejpb.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 271.Kandil R, Baldassi D, Böhlen S, Müller JT, Jürgens DC, Bargmann T, Dehmel S, Xie Y, Mehta A, Sewald K, Merkel OM. Targeted GATA3 knockdown in activated T cells via pulmonary siRNA delivery as novel therapy for allergic asthma. J Control Release. 2023;354:305–15. doi: 10.1016/j.jconrel.2023.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Martin C, Uhlig S, Ullrich V. Videomicroscopy of methacholine-induced contraction of individual airways in precision-cut lung slices. Eur Respir J. 1996;9:2479–87. doi: 10.1183/09031936.96.09122479. [DOI] [PubMed] [Google Scholar]
- 273.Schleputz M, Uhlig S, Martin C. Electric field stimulation of precision-cut lung slices. J Appl Physiol (1985) 2011;110:545–54. doi: 10.1152/japplphysiol.00409.2010. [DOI] [PubMed] [Google Scholar]
- 274.Dassow C, Wiechert L, Martin C, Schumann S, Muller-Newen G, Pack O, Guttmann J, Wall WA, Uhlig S. Biaxial distension of precision-cut lung slices. J Appl Physiol (1985) 2010;108:713–21. doi: 10.1152/japplphysiol.00229.2009. [DOI] [PubMed] [Google Scholar]
- 275.Davidovich N, Huang J, Margulies SS. Reproducible uniform equibiaxial stretch of precision-cut lung slices. Am J Physiol Lung Cell Mol Physiol. 2013;304:L210–220. doi: 10.1152/ajplung.00224.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Mondonedo JR, Bartolak-Suki E, Bou Jawde S, Nelson K, Cao K, Sonnenberg A, Obrochta WP, Imsirovic J, Ram-Mohan S, Krishnan R, Suki B. A high-Throughput System for Cyclic stretching of Precision-Cut lung slices during Acute cigarette smoke extract exposure. Front Physiol. 2020;11:566. doi: 10.3389/fphys.2020.00566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Nguyen TM, van der Merwe J, Elowsson Rendin L, Larsson-Callerfelt AK, Deprest J, Westergren-Thorsson G, Toelen J. Stretch increases alveolar type 1 cell number in fetal lungs through ROCK-Yap/Taz pathway. Am J Physiol Lung Cell Mol Physiol. 2021;321:L814–26. doi: 10.1152/ajplung.00484.2020. [DOI] [PubMed] [Google Scholar]
- 278.Ram-Mohan S, Bai Y, Schaible N, Ehrlicher AJ, Cook DP, Suki B, Stoltz DA, Solway J, Ai X, Krishnan R. Tissue traction microscopy to quantify muscle contraction within precision-cut lung slices. Am J Physiol Lung Cell Mol Physiol. 2020;318:L323–30. doi: 10.1152/ajplung.00297.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Rosmark O, Ibanez-Fonseca A, Thorsson J, Dellgren G, Hallgren O, Larsson Callerfelt AK, Elowsson L, Westergren-Thorsson G. A tunable physiomimetic stretch system evaluated with precision cut lung slices and recellularized human lung scaffolds. Front Bioeng Biotechnol. 2022;10:995460. doi: 10.3389/fbioe.2022.995460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Ma B, Sanderson M, Bates JH. Airway-parenchymal interdependence in the lung slice. Respir Physiol Neurobiol. 2013;185:211–6. doi: 10.1016/j.resp.2012.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Niehof M, Reamon-Buettner SM, Danov O, Hansen T, Sewald K. A modified protocol for successful miRNA profiling in human precision-cut lung slices (PCLS) BMC Res Notes. 2021;14:255. doi: 10.1186/s13104-021-05674-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Stegmayr J, Alsafadi HN, Langwinski W, Niroomand A, Lindstedt S, Leigh ND, Wagner DE. Isolation of high-yield and -quality RNA from human precision-cut lung slices for RNA-sequencing and computational integration with larger patient cohorts. Am J Physiol Lung Cell Mol Physiol. 2021;320:L232–40. doi: 10.1152/ajplung.00401.2020. [DOI] [PubMed] [Google Scholar]
- 283.van den Bosch T, Leus NGJ, Wapenaar H, Boichenko A, Hermans J, Bischoff R, Haisma HJ, Dekker FJ. A 6-alkylsalicylate histone acetyltransferase inhibitor inhibits histone acetylation and pro-inflammatory gene expression in murine precision-cut lung slices. Pulm Pharmacol Ther. 2017;44:88–95. doi: 10.1016/j.pupt.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Lyons-Cohen MR, Thomas SY, Cook DN, Nakano H. Precision-cut mouse lung slices to visualize live pulmonary dendritic cells. J Vis Exp. 2017;5:e55465–74. [DOI] [PMC free article] [PubMed]
- 285.Klouda T, Condon D, Hao Y, Tian W, Lvova M, Chakraborty A, Nicolls MR, Zhou X, Raby BA, Yuan K. From 2D to 3D: promising advances in imaging lung structure. Front Med (Lausanne) 2020;7:343. doi: 10.3389/fmed.2020.00343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Temann A, Golovina T, Neuhaus V, Thompson C, Chichester JA, Braun A, Yusibov V. Evaluation of inflammatory and immune responses in long-term cultured human precision-cut lung slices. Hum Vaccin Immunother. 2017;13:351–8. doi: 10.1080/21645515.2017.1264794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Yim PD, Gallos G, Perez-Zoghbi JF, Zhang Y, Xu D, Wu A, Berkowitz DE, Emala CW. Airway smooth muscle photorelaxation via opsin receptor activation. Am J Physiol Lung Cell Mol Physiol. 2019;316:L82–93. doi: 10.1152/ajplung.00135.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Akram KM, Yates LL, Mongey R, Rothery S, Gaboriau DCA, Sanderson J, Hind M, Griffiths M, Dean CH. Live imaging of alveologenesis in precision-cut lung slices reveals dynamic epithelial cell behaviour. Nat Commun. 2019;10:1178. doi: 10.1038/s41467-019-09067-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Delmotte P, Sanderson MJ. Ciliary beat frequency is maintained at a maximal rate in the small airways of mouse lung slices. Am J Respir Cell Mol Biol. 2006;35:110–7. doi: 10.1165/rcmb.2005-0417OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Lehmann M, Hu Q, Hu Y, Hafner K, Costa R, van den Berg A, Konigshoff M. Chronic WNT/beta-catenin signaling induces cellular senescence in lung epithelial cells. Cell Signal. 2020;70:109588. doi: 10.1016/j.cellsig.2020.109588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Sponchiado M, Liao YS, Atanasova KR, Collins EN, Schurmann V, Bravo L, Reznikov LR. Overexpression of substance P in pig airways increases MUC5AC through an NF-kbeta pathway. Physiol Rep. 2021;9:e14749. doi: 10.14814/phy2.14749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Wohlsen A, Hirrle A, Tenor H, Marx D, Beume R. Effect of cyclic AMP-elevating agents on airway ciliary beat frequency in central and lateral airways in rat precision-cut lung slices. Eur J Pharmacol. 2010;635:177–83. doi: 10.1016/j.ejphar.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 293.Pouwels SD, Hesse L, Wu X, Allam V, van Oldeniel D, Bhiekharie LJ, Phipps S, Oliver BG, Gosens R, Sukkar MB, Heijink IH. LL-37 and HMGB1 induce alveolar damage and reduce lung tissue regeneration via RAGE. Am J Physiol Lung Cell Mol Physiol. 2021;321:L641–52. doi: 10.1152/ajplung.00138.2021. [DOI] [PubMed] [Google Scholar]
- 294.Bai Y, Krishnamoorthy N, Patel KR, Rosas I, Sanderson MJ, Ai X. Cryopreserved Human Precision-Cut lung slices as a Bioassay for live tissue banking. A viability study of bronchodilation with bitter-taste receptor agonists. Am J Respir Cell Mol Biol. 2016;54:656–63. doi: 10.1165/rcmb.2015-0290MA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Patel VS, Amin K, Wahab A, Marimoutou M, Ukishima L, Alvarez J, Battle K, Stucki AO, Clippinger AJ, Behrsing HP. Cryopreserved human precision-cut lung slices provide an immune competent pulmonary test system for on-demand use and long-term cultures. Toxicol Sci. 2023;191:253–65. doi: 10.1093/toxsci/kfac136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Preuss EB, Schubert S, Werlein C, Stark H, Braubach P, Hofer A, Plucinski EKJ, Shah HR, Geffers R, Sewald K, et al. The challenge of long-term cultivation of Human Precision-Cut lung slices. Am J Pathol. 2022;192:239–53. doi: 10.1016/j.ajpath.2021.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Tigges J, Eggerbauer F, Worek F, Thiermann H, Rauen U, Wille T. Optimization of long-term cold storage of rat precision-cut lung slices with a tissue preservation solution. Am J Physiol Lung Cell Mol Physiol. 2021;321:L1023–35. doi: 10.1152/ajplung.00076.2021. [DOI] [PubMed] [Google Scholar]
- 298.Rosner SR, Ram-Mohan S, Paez-Cortez JR, Lavoie TL, Dowell ML, Yuan L, Ai X, Fine A, Aird WC, Solway J, et al. Airway contractility in the precision-cut lung slice after cryopreservation. Am J Respir Cell Mol Biol. 2014;50:876–81. doi: 10.1165/rcmb.2013-0166MA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Bailey KE, Pino C, Lennon ML, Lyons A, Jacot JG, Lammers SR, Konigshoff M, Magin CM. Embedding of Precision-Cut lung slices in Engineered Hydrogel Biomaterials supports extended Ex vivo culture. Am J Respir Cell Mol Biol. 2020;62:14–22. doi: 10.1165/rcmb.2019-0232MA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Bai Y, Ai X. Utilizing the Precision-Cut Lung slice to study the Contractile Regulation of Airway and Intrapulmonary arterial smooth muscle. J Vis Exp. 2022:183:e63952. video. [DOI] [PMC free article] [PubMed]
- 301.Klouda T, Kim H, Kim J, Visner G, Yuan K. Precision Cut lung slices as an efficient Tool for ex vivo Pulmonary Vessel structure and Contractility studies. J Vis Exp. 2021;171: e62392. video. [DOI] [PubMed]
- 302.Michalaki C, Dean C, Johansson C. The Use of Precision-Cut lung slices for studying innate immunity to viral infections. Curr Protoc. 2022;2:e505. doi: 10.1002/cpz1.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Paddenberg R, Mermer P, Goldenberg A, Kummer W. Videomorphometric analysis of hypoxic pulmonary vasoconstriction of intra-pulmonary arteries using murine precision cut lung slices. J Vis Exp. 2014;83:e50970. video. [DOI] [PMC free article] [PubMed]
- 304.Koziol-White C. Human Precision-Cut lung slices: generation of and measurement of Contractility and Relaxation of Small airways. Methods Mol Biol. 2022;2506:111–7. doi: 10.1007/978-1-0716-2364-0_8. [DOI] [PubMed] [Google Scholar]
- 305.Patel V, Amin K, Allen D, Ukishima L, Wahab A, Grodi C, Behrsing H. Comparison of Long-Term Human Precision-cut lung slice culture methodology and response to challenge: an argument for standardisation. Altern Lab Anim. 2021;49:209–22. doi: 10.1177/02611929211061884. [DOI] [PubMed] [Google Scholar]
- 306.Calzetta L, Matera MG, Facciolo F, Cazzola M, Rogliani P. Beclomethasone dipropionate and formoterol fumarate synergistically interact in hyperresponsive medium bronchi and small airways. Respir Res. 2018;19:65. doi: 10.1186/s12931-018-0770-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Cazzola M, Calzetta L, Puxeddu E, Ora J, Facciolo F, Rogliani P, Matera MG. Pharmacological characterisation of the interaction between glycopyrronium bromide and indacaterol fumarate in human isolated bronchi, small airways and bronchial epithelial cells. Respir Res. 2016;17:70. doi: 10.1186/s12931-016-0386-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Rogliani P, Matera MG, Facciolo F, Page C, Cazzola M, Calzetta L. Beclomethasone dipropionate, formoterol fumarate and glycopyrronium bromide: synergy of triple combination therapy on human airway smooth muscle ex vivo. Br J Pharmacol. 2020;177:1150–63. doi: 10.1111/bph.14909. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.