Abstract
Background:
Many recent studies have shown that patients who undergo capsular repair after hip arthroscopy achieve superior clinical outcomes compared with those who do not. However, patients with dysplasia or generalized ligamentous laxity (GLL) were not excluded from most of these studies, which may have affected the outcomes.
Purpose:
To determine whether capsular repair influences the outcomes of hip arthroscopy for patients without dysplasia or GLL.
Study Design:
Systematic review; Level of evidence, 1.
Methods:
Under the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, randomized controlled trials comparing the outcomes of capsulotomy with versus without repair were included, but studies that included patients with dysplasia or GLL were excluded. The study outcomes were patient-reported outcome measures (PROMs) at 6 months and 2 years postoperatively—including the modified Harris Hip Score (mHHS), Hip Outcome Score–Activities of Daily Living (HOS-ADL), and Hip Outcome Score–Sport-Specific Subscale (HOS-SSS)— and were compared between the repair and no-repair groups. A narrative analysis and meta-analysis were performed to integrate and compare the results of the 2 groups. In the meta-analysis of the outcome measures, studies with significant differences in the preoperative scores between the repair and no-repair groups were excluded because previous studies have shown that these can affect the outcomes.
Results:
A total of 761 studies were initially identified, of which 3 were included. Of the 322 included patients, 136 underwent capsular repair, and 186 underwent capsulotomy with no repair. The meta-analysis showed that capsular repair was associated with significantly higher postoperative PROMs: the mHHS at 2 years (P = .03), the HOS-ADL at 6 months (P = .02) and 2 years (P < .0001), and the HOS-SSS at 6 months (P = .02) and 2 years (P = .001).
Conclusion:
Capsular repair after hip arthroscopy was associated with superior clinical outcomes when compared with no capsular repair in patients without dysplasia or GLL.
Keywords: capsule, capsular repair, hip arthroscopy, meta-analysis, systematic review
The hip joint is a ball-and-socket joint consisting of the femoral head and acetabulum, plus accessory structures that include the joint capsule, labrum, ligaments, and surrounding muscles. These structures work together to maintain the stability of the joint. With the development of the arthroscopic technique, hip arthroscopy is increasingly being performed in clinical practice, and many studies have shown that hip arthroscopy achieves very good results.20,36
Previous biomechanical and clinical studies have shown that the hip capsule plays a very important role in maintaining hip stability.16,21,22 However, whether capsular repair should be performed after hip arthroscopy remains controversial. There have been many systematic reviews and meta-analyses comparing the clinical outcomes of patients who had repair with those who did not. Most of these studies have demonstrated superior clinical outcomes in the repaired group.6,27-29,31,33 However, patients with congenital malformations, such as borderline developmental dysplasia of the hip (BDDH), developmental dysplasia of the hip (DDH), or systemic generalized ligamentous laxity (GLL), which may affect the clinical outcomes of the procedure, were not excluded from many of these studies. It is known that such patients require capsular repair to maintain hip stability after arthroscopy. Still, it is less certain whether a hip capsular repair is necessary for patients without dysplasia or GLL. Furthermore, studies other than randomized controlled trials (RCTs) were included in most of the previous systematic reviews and meta-analyses, which would tend to reduce the reliability of the conclusions drawn.
In the present study, a systematic review and meta-analysis of RCTs was performed to determine whether capsular repair influences the clinical outcomes of hip arthroscopy for patients without dysplasia or GLL. We hypothesized that postoperative capsular repair would be superior to no repair.
Methods
Study Registration and Search Strategy
A systematic review and meta-analysis was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines and checklist, 26 and the study protocol was registered with PROSPERO (no. CRD42023406214). 17 The Embase, Cochrane Library, and PubMed databases were searched from their inception to February 2023. The following keywords were used in the search, along with “AND” and “OR” Boolean operators: “hip,”“arthroscopy,”“capsule,”“close,”“capsular,”“repair,”“management,”“closure,” and “arthroscopic.”
Inclusion and exclusion Criteria
Included were studies that met the following criteria: (1) publication in English; (2) patient-reported outcome measures (PROMs) reported after hip arthroscopic surgery; (3) comparison of the outcomes after capsulotomy with versus without repair; and (4) RCT. The exclusion criteria were as follows: (1) surgical indication of dysplasia, borderline dysplasia, central-edge angle <25°, or GLL; (2) significant differences in the preoperative PROM scores between the capsular repair and no-repair groups; (3) cadaveric studies, animal experiments, and biomechanical studies; (4) case reports, systematic reviews, editorial commentaries, and meeting reports; (5) duplicate articles; and (6) abstract-only articles.
Data Extraction
Two authors (L.-Y.S. and Q.-R.L.) independently screened the texts, extracted the data, and reached conformity regarding study inclusion. If there was disagreement, the corresponding author assisted in establishing a consensus. During the screening, the title and abstract of each article were considered first to determine whether to read the full text, which was necessary to decide on the inclusion of the study. The information extracted from all the candidate studies consisted of the author names; year of publication; level of evidence; study design; sample size; the age, sex, and body mass index (BMI) of the participants; and the duration of follow-up.
Outcomes
The study outcomes were 3 PROMs: the modified Harris Hip Score (mHHS), the Hip Outcome Score–Activities of Daily Living (HOS-ADL), and the Hip Outcome Score–Sport-Specific Subscale (HOS-SSS). In the meta-analysis of the mHHS, HOS-ADL, and HOS-SSS data, studies were excluded when the preoperative scores of the repair and no-repair groups significantly differed, as preoperative scores may affect the postoperative outcomes. 29 According to the follow-up periods of the included studies, meta-analyses of the mHHS, HOS-ADL, and HOS-SSS data were performed for the 6-month and 2-year postoperative time points.
Risk-of-Bias and Quality Assessment
The quality of the RCTs was evaluated using the Cochrane risk-of-bias assessment tool, which classifies the following items as having low, high, or an unclear risk of bias based on the following criteria: random sequence generation; allocation concealment; blinding of the participants, care providers, and outcome assessors; incomplete outcome data; selective outcome reporting; and other sources of bias. 10 The MINORS (Methodological Index for Non-Randomized Studies) was used to assess the quality of the studies. The MINORS has 12 criteria for comparative studies, for a total of 24 points: (1) clearly stated aim; (2) inclusion of consecutive patients; (3) prospective collection of data; (4) endpoints appropriate to the aim of the study; (5) unbiased assessment of the study endpoint; (6) follow-up period appropriate to the aim of the study; (7) loss to follow-up <5%; (8) prospective calculation of the study size; (9) adequate control group; (10) contemporary groups; (11) baseline equivalence of groups; and (12) adequate statistical analyses. Scores of 0 to 6 are considered very low, 7 to 12 low, 1 to 18 fair, and 19 to 24 high.
Data Analysis
The statistical analysis was performed using RevMan5.3 software (Cochrane Collaboration). Mean differences (MDs) were used for continuous data, and odds ratios were used for dichotomous data, with 95% CIs quoted for both outcomes. I2 and chi-square tests were used to evaluate the heterogeneity of the selected studies. A random-effects model was used for the meta-analysis if I2 >50%, representing high heterogeneity; otherwise, a fixed-effects model was used. P < .05 was regarded as indicating statistical significance.
Results
Study Selection
Our initial search identified 760 studies, and 1 additional study was identified through other means. After the removal of duplicates, 420 articles remained. After evaluating the abstracts, 379 of the articles were discarded, and a full-text review was performed on the remaining 41; of these, 3 studies1,14,35 were included in the systematic review, but only 2 studies14,35 were included in the meta-analysis because the other study did not involve the stipulated PROMs (Figure 1).
Figure 1.
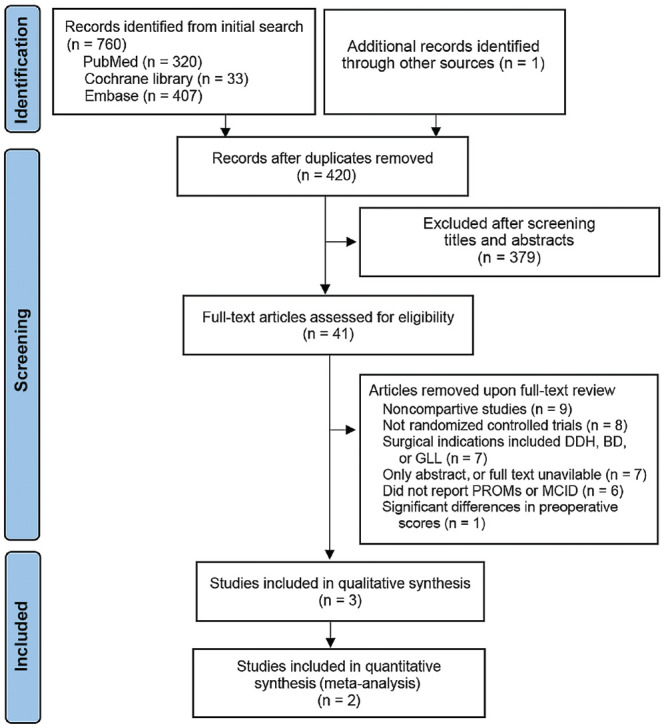
A PRISMA flowchart for the literature review. BDDH, borderline developmental dysplasia of the hip; DDH, developmental dysplasia of the hip; GLL, generalized ligamentous laxity; MCID, minimum clinically important difference; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; PROMs, patient-reported outcome measures.
Study Characteristics
The 3 RCTs included 322 patients who underwent hip arthroscopy, 136 of whom underwent capsular repair and 186 did not. The principal characteristics of the included studies are shown in Table 1.
Table 1.
Characteristics of the Included Studies a
| Author (Year) | LOE | MINORS Score | Follow-Up Times, mo | Sample Size, n | Age, Years | Female Sex, n | BMI, kg/m2 | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No Repair | Repair | No Repair | Repair | No Repair | Repair | No Repair | Repair | ||||
| Bech et al 1 (2023) | 1 | 20 | 3, 12 | 58 | 58 | 35.5 ± 10.4 | 33.5 ± 8.5 | 35 | 39 | 23.1 ± 2.7 | 24.2 ± 2.9 |
| Economopoulos et al 14 (2020) | 2 | 18 | 3, 6, 12, 24 | 100 | 50 | 37.8 ± 13.37 | 35.2 ± 10.9 | 42 | 19 | 26.15 ± 4.26 | 24.8 ± 3.9 |
| Sugarman et al 35 (2021) | 1 | 22 | 6, 24 | 28 | 28 | 33.7 ± 9.7 | 31.8 ± 8.6 | 8 | 22 | 25.7 ± 4.1 | 24.4 ± 4.9 |
Data are reported as absolute values or as mean ± SD. BMI, body mass index; LOE, level of evidence; MINORS, Methodological Index for Non-Randomized Studies.
Study Quality
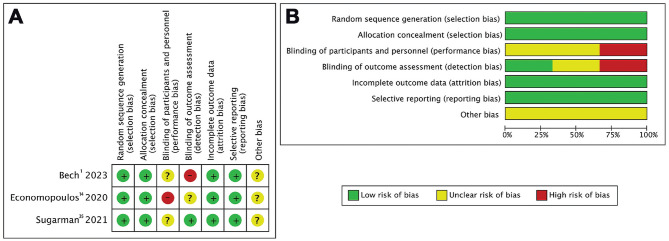
The findings of the standardized assessment of the risk of bias associated with the included RCTs are summarized in Figure 2. The overall risk of bias was deemed to be low. In each article, ≥4 evaluation items were considered to have a low risk of bias. However, 1 study 14 exhibited a high risk of bias in terms of performance bias, and 1 study 1 demonstrated a high risk of bias in terms of detection bias; no study addressed other potential sources of bias. The MINORS scores indicated high quality for 2 of the studies1,35 and fair quality for 1 study (Table 1). 14
Figure 2.
(A) Risk of bias summary of the included studies. (B) The overall risk of bias graph.
Outcomes
Results According to Study
The study by Bech et al 1 included 116 patients, 58 of whom were allocated to the no-repair group, and the remaining 58 patients were allocated to the repair group. The capsulotomy performed was interportal rather than T-shaped in all patients. The PROMs used were pain on a numerical rating scale (NRS) and the Copenhagen Hip and Groin Outcome Score (HAGOS) at the 3- and 12-month follow-up examinations. The authors found no significant differences in the NRS pain or the HAGOS between the repair and no-repair groups, except for the Sports domain of the HAGOS at 3 months. Therefore, they concluded there is no need for the routine closure of the joint capsule at the end of hip arthroscopy.
The study by Economopoulos et al 14 included 150 patients who were randomly assigned to 3 groups at the time of their surgery: T-capsulotomy without closure (TC), interportal capsulotomy without closure (IC), and interportal capsulotomy with closure (CC). The patients completed mHHS, HOS-ADL, and HOS-SSS scores preoperatively and at 3, 6, 12, and 24 months postoperatively. Results showed that the CC group had significantly higher mHHS and HOS-ADL scores at the 2-year time point compared to the IC group and that the CC group had superior mHHS, HOS-ADL, and HOS-SSS scores at the final 2-year time point. In addition, patients who underwent complete capsular closure during hip arthroscopy had superior patient-reported and surgical outcomes to those who underwent TC or IC. Therefore, the authors concluded that repair after capsulotomy may be beneficial.
The study by Sugarman et al 34 included 56 patients, of whom 28 were allocated to the no-repair group, and the remaining 28 were assigned to the repair group. An interportal capsulotomy was performed in all cases. The clinical outcomes of the patients were assessed using the HOS-ADL, HOS-SSS, mHHS, visual analog scale pain, International Hip Outcome Tool, and Veterans RAND 12-Item Health Survey (VR-12). The authors found no significant differences between the repair and no-repair groups concerning any of the evaluated PROMs. A superior outcome in the capsular repair group was identified for the VR-12 Physical subscale at the 2-year time point. Therefore, they concluded that capsular closure had no detrimental effect on functional outcome scores after hip arthroscopy.
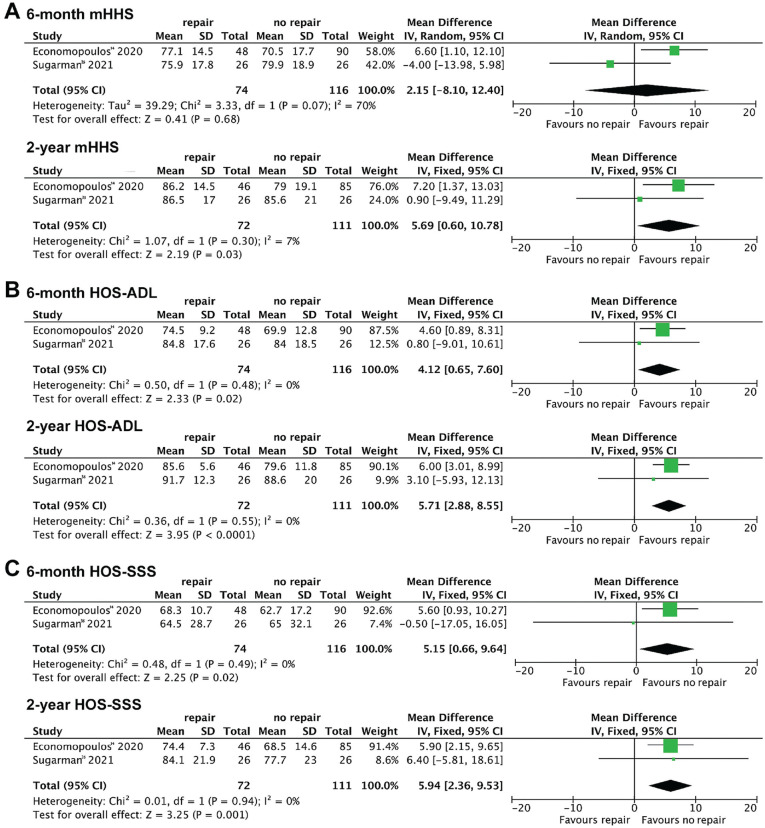
Results According to PROM Scores
Separate meta-analyses were performed for the 6-month and 2-year postoperative time points. Regarding the mHHS, no significant difference was observed in the 6-month outcomes between the repair and no-repair groups (MD, 2.15 [95% CI, -8.10 to 12.40]; I2 = 70%; P = .68). However, a significant difference was found in favor of capsular repair in the 2-year outcomes between groups (MD, 5.69 [95% CI, 0.6 to 10.78]; I2 = 7%; P = .03) (Figure 3A). Regarding the HOS-ADL, a significant difference was found in favor of repair in both the 6-month outcomes between the groups (MD, 4.12 [95% CI, 0.65 to 7.60]; I2 = 0%; P = .02) and the 2-year outcomes (MD, 5.71 [95% CI, 2.88 to 8.55]; I2 = 0%; P < .0001) (Figure 3B). Regarding the HOS-SSS, a significant difference was found in favor of repair in the 6-month outcomes of the groups (MD, 5.15 [95% CI, 0.66 to 9.64]; I2 = 0%; P = .02) as well as the 2-year outcomes (MD, 5.94 [95% CI, 2.36 to 9.53]; I2 = 0%; P = .001) (Figure 3C).
Figure 3.
Forest plots showing the scores for (A) the mHHS, (B) the HOS-ADL, and (C) the HOS-SSS at 6 months and 2 years postoperatively. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SSS, Hip Outcome Score–Sport-Specific Subscale; mHHS, modified Harris Hip Score.
Discussion
The most important finding of the present study was that most of the PROM scores, especially in the medium term, showed a significant advantage in favor of capsular repair in patients who did not have BDDH, DDH, or GLL. These results suggest that capsular repair after hip arthroscopic surgery is associated with superior outcomes for patients who do not have these conditions.
Hip arthroscopy has the advantages of creating less trauma and permitting faster postoperative recovery than standard open joint surgery. 19 In the past, as the result of the difficulty of arthroscopic capsular suturing and the relative stability of the hip joint, capsule repair after hip arthroscopy was not routinely performed. However, recent biomechanical studies have confirmed the role of the capsule in hip joint stability.16,21,22 They have shown that a loose capsule is associated with microinstability of the hip joint, manifesting in significantly greater rotation and translation of the femoral head.16,21 Furthermore, the important role of the joint capsule in the maintenance of hip stability has been recognized, especially in patients with DDH or GLL.24,25 In addition, several studies have demonstrated the microinstability of hip joints after hip arthroscopy, which may be caused by the lack of an intact joint capsule.9,23,34 Nevertheless, the need for hip capsule repair after arthroscopy is controversial. The studies performed to date have yielded differing results: Some have shown no significant difference between groups of patients who undergo capsular repair and those who do not,1,13 while others have shown a significant advantage, in the form of superior postoperative scores, for patients who undergo capsule repair.2,3,15,18
In response to these studies, several systematic reviews and meta-analyses were conducted that compared the clinical outcomes of patients who did or did not undergo capsule repair after hip arthroscopy in several different populations and under various clinical situations. A meta-analysis by Looney et al 29 included 36 studies of 5132 hips. This was the largest meta-analysis to date that evaluated the effect of capsular closure on PROMs, with results showing that repair was associated with significantly higher mean postoperative scores and more marked improvement. In their analysis, the authors controlled for the effects of the preoperative score and surgical indication. Still, all types of patients were included, including those with BDDH and GLL, which may have influenced the results.
In their review, Owens et al 31 included 16 studies (2996 hips) in patients with femoroacetabular impingement (FAI). The medium-term outcomes of these patients suggested that capsular repair was safe and effective in patients without arthritis who underwent hip arthroscopy and that it was associated with superior PROMs to those of patients whose capsulotomies were not repaired. Although they targeted patients with FAI, they did not exclude patients with BDDH, DDH, or GLL. Furthermore, their review included both primary and revision hip arthroscopy studies, which may have limited its generalizability.
Cohen et al 8 included 36 studies (4744 patients) in their meta-analysis and found superior postoperative outcomes in patients who undergo complete capsular closure, regardless of the type of capsulotomy, based on an analysis of postoperative mHHS scores. Thus, their findings may suggest superior postoperative outcomes after the closure of an interportal capsulotomy. However, they included several studies that did not compare groups, and there was significant heterogeneity in the reporting of the capsular management techniques in the included studies.
Lin et al 27 included 12 comparative studies of 1185 hips in their meta-analysis and found that the published evidence was insufficient to confirm the superiority of capsular repair after hip arthroscopy and, therefore, that the routine repair of the capsule during surgery could not be recommended. Their study also had several limitations—including a small sample size, a lack of subgroup or sensitivity analyses, and a lack of accounting for the effects of differences in preoperative scores.
As a result of the findings of these previous reviews and meta-analyses, most scholars support the use of capsular repair after hip arthroscopy. However, patients with forms of hip dysplasia and GLL were not excluded from these analyses, and given that patients with dysplasia or GLL are at a higher risk of hip microinstability, it is generally recognized that capsular repair is necessary for these patients.24,25 Therefore, the authors of these studies may have overestimated the effect of capsular repair in patients who do not have such disorders. Indeed, most patients do not have dysplasia or GLL, but there have been no studies regarding the necessity for capsular repair in these patients. Patients with dysplasia or GLL were excluded from the present study, which renders the findings more applicable to the general population.
Some authors have also reported that patients who undergo capsular repair demonstrate more durable clinical outcomes. Domb et al 12 found that the mHHS, Non-Arthritic Hip Score, and HOS-SSS scores all decreased in patients without capsular repair between 2 years and a minimum of 5 years after surgery. There was a significant decrease in the mHHS from 87.9 at 2 years to 79.3 at >5 years and patient satisfaction decreased from 8.5 at 2 years to 7.7 at >5 years. However, the patients who underwent capsular repair did not show significant decreases in these parameters. Tahoun et al 36 also compared the clinical outcomes of patients between 2 and 5 years postoperatively. They found decreases in some clinical outcome scores in the no-repair group but not in the repair group. Future studies should further evaluate the durability of the clinical outcomes of patients who undergo capsular repair and those who do not.
The conventional methods of capsular dissection include interportal capsulotomy and T-capsulotomy. However, the capsulotomy method was not described clearly in many of the publications, which may have affected the clinical outcomes. Economopoulos et al 14 found that the interportal capsulotomy without repair group had significantly higher mHHS, HOS-ADL, and HOS-SSS scores than the T-capsulotomy without repair group at the 2-year time point. In addition, some authors have proposed using periportal capsulotomy, which causes relatively minor damage to the joint capsule. 7 Chambers et al 7 performed a retrospective study of the outcomes of a limited periportal capsulotomy without capsular closure for the arthroscopic treatment of 142 patients with FAI. They found that periportal capsulotomy provided safe and sufficient access to the hip joint for the arthroscopic treatment of this condition without the need for capsular closure. This technique showed significant clinical improvement, and no postoperative instability was present 1 and 2 years postoperatively. However, they did not compare the outcomes with the alternative approach; thus, it is unclear whether capsular repair is superior to no repair for patients who undergo periportal capsulotomy. Furthermore, previous biomechanical studies have shown that the repair method affects the stability of the capsule.11,30 However, the effects of the suturing method used and the number of sutures placed were not evaluated in the present study. These factors may affect the degree of capsular closure and even the final clinical outcomes; therefore, further studies of these parameters are needed.
The existing research evidence suggests that capsular repair is superior to no repair. However, some authors have stated that capsulectomy may represent a viable treatment option in cases of hip joint stiffness or poor capsular compliance.4,5,32 However, whether patients with preoperative stiffness or adhesive capsulitis may benefit from not repairing their hip joint capsule requires further study.5,32
In general, capsular repair after hip arthroscopy is recommended to restore the original anatomy, which is likely beneficial for patients without dysplasia or GLL. However, the exact suturing method used, the number of sutures placed, and the optimal tightness of the capsule require further investigation in various patient populations and under different clinical conditions. Further research should focus on comparing the effects of the type of capsulotomy performed and the type of suturing method.
Strengths and Limitations
The greatest strength of the present study is that patients with hip dysplasia or GLL were excluded. In addition, only RCTs were included, which increases the reliability of the conclusions drawn. Studies in which treatment groups significantly differed in their preoperative scores were excluded from the meta-analysis of the PROMs to further improve the reliability of the conclusions. The heterogeneity among the studies was also relatively low. Last, subgroup analyses of PROMs were conducted according to the timing of the follow-up examination.
The study also had some limitations. First, the type of capsulotomy performed and the number of sutures placed were not controlled for owing to limitations in the source data. Second, sensitivity analyses were not performed. Third, the sample size was small, and the follow-up periods were short. Further RCTs should be performed to strengthen the evidence base. Nevertheless, our findings demonstrate a significant advantage of capsular repair in patients without dysplasia or GLL.
Conclusion
This systematic review and meta-analysis indicated that capsular repair after hip arthroscopic surgery was associated with superior clinical outcomes when compared with no capsular repair in patients without dysplasia or GLL.
Footnotes
Final revision submitted September 5, 2023; accepted November 14, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was supported by a grant awarded to Hong-Yun Li from the National Key Research and Development Program of China (2020YFC20070405). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Bech NH, Sierevelt IN, de Waard S, et al. Capsular closure versus unrepaired interportal capsulotomy after hip arthroscopy in patients with femoroacetabular impingement: results of a patient-blinded randomised controlled trial. Hip Int. 2023;33(1):94-101. [DOI] [PubMed] [Google Scholar]
- 2. Beck EC, Nwachukwu BU, Chahla J, et al. Complete capsular closure provides higher rates of clinically significant outcome improvement and higher survivorship versus partial closure after hip arthroscopy at minimum 5-year follow-up. Arthroscopy. 2021;37(6):1833-1842. [DOI] [PubMed] [Google Scholar]
- 3. Bolia IK, Fagotti L, Briggs KK, Philippon MJ. Midterm outcomes following repair of capsulotomy versus nonrepair in patients undergoing hip arthroscopy for femoroacetabular impingement with labral repair. Arthroscopy. 2019;35(6):1828-1834. [DOI] [PubMed] [Google Scholar]
- 4. Byrd JWT, Jones KS. Adhesive capsulitis of the hip. Arthroscopy. 2006;22(1):89-94. [DOI] [PubMed] [Google Scholar]
- 5. Byrd JWT, Jones KS. Hip arthroscopy for labral pathology: prospective analysis with 10-year follow-up. Arthroscopy. 2009;25(4):365-368. [DOI] [PubMed] [Google Scholar]
- 6. Carbone AD, Prabhavalkar O, Chishti Z, et al. Hip capsular repair results in improved patient-reported outcomes and survivorship: a systematic review of the literature. Arthroscopy. 2023;39(2):488-497. [DOI] [PubMed] [Google Scholar]
- 7. Chambers CC, Monroe EJ, Flores SE, Borak KR, Zhang AL. Periportal capsulotomy: technique and outcomes for a limited capsulotomy during hip arthroscopy. Arthroscopy. 2019;35(4):1120-1127. [DOI] [PubMed] [Google Scholar]
- 8. Cohen D, Comeau-Gauthier M, Khan A, et al. A higher proportion of patients may reach the MCID with capsular closure in patients undergoing arthroscopic surgery for femoroacetabular impingement: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2022;30(7):2425-2456. [DOI] [PubMed] [Google Scholar]
- 9. Cohen D, Jean PO, Patel M, et al. Hip microinstability diagnosis and management: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2023;31(1):16-32. [DOI] [PubMed] [Google Scholar]
- 10. Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10(10):ED000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. De Giacomo AF, Lu Y, Suh DH, et al. Biomechanical comparison of capsular repair, capsular shift, and capsular plication for hip capsular closure: is a single repair technique best for all? Orthop J Sports Med. 2021;9(10):23259671211040098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Domb BG, Chaharbakhshi EO, Perets I, et al. Patient-reported outcomes of capsular repair versus capsulotomy in patients undergoing hip arthroscopy: minimum 5-year follow-up—a matched comparison Study. Arthroscopy. 2018;34(3):853-863.e1. [DOI] [PubMed] [Google Scholar]
- 13. Domb BG, Stake CE, Finley ZJ, Chen T, Giordano BD. Influence of capsular repair versus unrepaired capsulotomy on 2-year clinical outcomes after arthroscopic hip preservation surgery. Arthroscopy. 2015;31(4):643-650. [DOI] [PubMed] [Google Scholar]
- 14. Economopoulos KJ, Chhabra A, Kweon C. Prospective randomized comparison of capsular management techniques during hip arthroscopy. Am J Sports Med. 2020;48(2):395-402. [DOI] [PubMed] [Google Scholar]
- 15. Frank RM, Lee S, Bush-Joseph CA, et al. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42(11):2634-2642. [DOI] [PubMed] [Google Scholar]
- 16. Han S, Alexander JW, Thomas VS, et al. Does capsular laxity lead to microinstability of the native hip? Am J Sports Med. 2018;46(6):1315-1323. [DOI] [PubMed] [Google Scholar]
- 17. Harris JD, Quatman CE, Manring MM, Siston RA, Flanigan DC. How to write a systematic review. Am J Sports Med. 2014;42(11):2761-2768. [DOI] [PubMed] [Google Scholar]
- 18. Hassebrock JD, Makovicka JL, Chhabra A, et al. Hip arthroscopy in the high-level athlete: does capsular closure make a difference? Am J Sports Med. 2020;48(10):2465-2470. [DOI] [PubMed] [Google Scholar]
- 19. Jamil M, Dandachli W, Noordin S, Witt J. Hip arthroscopy: indications, outcomes and complications. Int J Surg. 2018;54(Pt B):341-344. [DOI] [PubMed] [Google Scholar]
- 20. Jimenez AE, Lee MS, Owens JS, et al. Competitive athletes who underwent hip arthroscopy with capsular repair showed greater improvement in patient-reported outcome scores compared with those who did not undergo repair. Arthroscopy. 2022;38(11):3030-3040. [DOI] [PubMed] [Google Scholar]
- 21. Johannsen AM, Behn AW, Shibata K, et al. The role of anterior capsular laxity in hip microinstability: a novel biomechanical model. Am J Sports Med. 2019;47(5):1151-1158. [DOI] [PubMed] [Google Scholar]
- 22. Johannsen AM, Ejnisman L, Behn AW, et al. Contributions of the capsule and labrum to hip mechanics in the context of hip microinstability. Orthop J Sports Med. 2019;7(12):2325967119890846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kalisvaart MM, Safran MR. Microinstability of the hip-it does exist: etiology, diagnosis and treatment. J Hip Preserv Surg. 2015;2(2):123-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Larson CM, Ross JR, Stone RM, et al. Arthroscopic management of dysplastic hip deformities: predictors of success and failures with comparison to an arthroscopic FAI cohort. Am J Sports Med. 2016;44(2):447-453. [DOI] [PubMed] [Google Scholar]
- 25. Larson CM, Stone RM, Grossi EF, Giveans MR, Cornelsen GD. Ehlers-Danlos syndrome: arthroscopic management for extreme soft-tissue hip instability. Arthroscopy. 2015;31(12):2287-2294. [DOI] [PubMed] [Google Scholar]
- 26. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1-e34. [DOI] [PubMed] [Google Scholar]
- 27. Lin Y, Li T, Deng X, et al. Repaired or unrepaired capsulotomy after hip arthroscopy: a systematic review and meta-analysis of comparative studies. Hip Int. 2020;30(3):256-266. [DOI] [PubMed] [Google Scholar]
- 28. Liu L, Zhang Y, Gui Q, et al. Effect of capsular closure on outcomes of hip arthroscopy for femoroacetabular impingement: a systematic review and meta-analysis. Orthop Surg. 2020;12(4):1153-1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Looney AM, McCann JA, Connolly PT, et al. Routine capsular closure with hip arthroscopic surgery results in superior outcomes: a systematic review and meta-analysis. Am J Sports Med. 2022;50(7):2007-2022. [DOI] [PubMed] [Google Scholar]
- 30. Murata Y, Fukase N, Brady AW, et al. Biomechanical evaluation of 4 suture techniques for hip capsular closure. Orthop J Sports Med. 2022;10(6):23259671221089946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Owens JS, Jimenez AE, Shapira J, et al. Capsular repair may improve outcomes in patients undergoing hip arthroscopy for femoroacetabular impingement: a systematic review of comparative outcome studies. Arthroscopy. 2021;37(9):2975-2990. [DOI] [PubMed] [Google Scholar]
- 32. Philippon MJ, Stubbs AJ, Schenker ML, et al. Arthroscopic management of femoroacetabular impingement: osteoplasty technique and literature review. Am J Sports Med. 2007;35(9):1571-1580. [DOI] [PubMed] [Google Scholar]
- 33. Riff AJ, Kunze KN, Movassaghi K, et al. Systematic review of hip arthroscopy for femoroacetabular impingement: the importance of labral repair and capsular closure. Arthroscopy. 2019;35(2):646-656.e3. [DOI] [PubMed] [Google Scholar]
- 34. Safran MR. Microinstability of the hip-gaining acceptance. J Am Acad Orthop Surg. 2019;27(1):12-22. [DOI] [PubMed] [Google Scholar]
- 35. Sugarman EP, Birns ME, Fishman M, et al. Does capsular closure affect clinical outcomes in hip arthroscopy? A prospective randomized controlled trial. Orthop J Sports Med. 2021;9(5):2325967120963110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tahoun MF, Lizano-Díez X, Soler BC, Pons MT. Superior outcomes after arthroscopic treatment of femoroacetabular impingement and labral tears with closed versus open capsule. Knee Surg Sports Traumatol Arthrosc. 2023;31(10):4501-4509. [DOI] [PubMed] [Google Scholar]