Abstract
Background:
There is a paucity of aggregate data documenting mid- to long-term outcomes of patients after hip arthroscopy with labral reconstruction.
Purpose:
To report mid- to long-term outcomes in patients after undergoing either primary or revision hip arthroscopy with labral reconstruction for the treatment of irreparable labral tears.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review of the PubMed, Cochrane, and Scopus databases in May 2022 was conducted with the following keywords: “hip arthroscopy,”“labral reconstruction,”“irreparable,”“labrum,”“reconstruction,”“five-year,”“midterm,”“5 year,”“long-term,”“10 year,” ten-year,” and “femoroacetabular impingement” using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses criteria. Midterm was defined as mean 5-year follow-up, and long-term was defined as mean 10-year or longer follow-up. For each included article, the demographic, radiographic, intraoperative, and surgical variables, as well as patient-reported outcomes (PROs), psychometric thresholds, and secondary surgeries were recorded. Forest plots were created for PROs that were reported in ≥3 studies; heterogeneity was assessed using I2 values.
Results:
Out of 463 initial articles, 5 studies including 178 hips with primary and 41 hips with revision surgeries were included. One study had an average 5-year follow-up, three studies had a minimum 5-year follow-up and one study had a minimum 10-year follow-up. The most common indications for hip arthroscopy with labral reconstruction were irreparable labral tears. The most common PRO was the modified Harris Hip Score (mHHS), which was reported in all 5 studies. The mean preoperative mHHS ranged from 58.9 to 66, and the mean postoperative mHHS at minimum 5-year follow-up ranged from 80.2 to 89. The preoperative and postoperative mHHSs for the single long-term follow-up study were 60 and 82, respectively. All 5 studies demonstrated significant improvements in reported PROs. All 5 studies reported secondary surgery rates, with 1 study reporting rates at both 5- and 10-year follow-up. Conversion to total hip arthroplasty ranged from 0% to 27%, while overall secondary surgery rates ranged from 0% to 36%.
Conclusion:
Findings demonstrated that patients undergoing primary and revision hip arthroscopy with labral reconstruction experienced favorable outcomes and high rates of clinical benefit and survivorship at mid- to long-term follow-up.
Keywords: hip arthroscopy, labral reconstruction, outcomes
Hip arthroscopy has become an increasingly popular method to address femoroacetabular impingement syndrome and labral tears.1,3,5,7,9 The acetabular labrum plays an important role in hip function, mobility, and stability. In addition, the intra-articular fluid pressurization protects the cartilage and decreases friction between the femur and the acetabulum. A cadaver study by Nepple et al 32 showed that, after a labral tear, subsequent repair or reconstruction resulted in a restoration of the critical pressurization. Labral repair has been identified as the preferred treatment when addressing acetabular labral tears.12,18,36 Patients have achieved favorable outcomes at short-, mid-, and long-term follow-ups in a variety of populations, including athletes, those with borderline dysplasia, and adolescents.3,4,8,11,13,31 However, some labral tears may be irreparable due to nonviable tissues, complex labral tearing, or calcified labra.6,24 In light of this dilemma, labral reconstruction has recently emerged as a proven and successful technique in restoring the labrum and the suction seal.26,32
Previous studies have demonstrated its efficacy in short-term outcomes in the primary general and active populations.10,20 Geyer et al 20 reported on 76 hips that underwent primary hip arthroscopy with labral reconstruction in the general population with a mean follow-up of 49 months. They reported that the cohort experienced significant improvement (P < .05) on the modified Harris Hip Score (mHHS), Hip Outcome Score-Activities of Daily Living (HOS-ADL), and Hip Outcome Score-Sports Specific Subscale (HOS-SSS) as well as a high median satisfaction score of 8 out of 10. 20 The trend for favorable outcomes is further seen in the highest level of athletes, whose physical demands on their body greatly exceed those of the general population. Boykin et al 10 reported on 21 elite athletes undergoing primary hip arthroscopy with labral reconstruction and found that 85.7% returned to play, with 81% returning to a similar preinjury level. These patients also reported significant improvement (P < .05) in the mHHS and HOS-SSS. 10
Several studies have previously reported midterm outcomes on patients undergoing hip arthroscopy with labral reconstruction.16,28,29 For long-term outcomes, Philippon et al 33 showed 61% survivorship from total hip arthroplasty (THA) or revision surgery and statistically significant increases in the mHHS, HOS-ADL, and HOS-SSS, with high rates of achievement on psychometric thresholds including the minimal clinically important difference (MCID) and Patient Acceptable Symptom State (PASS). Although these studies overall demonstrated improved outcomes and high patient satisfaction, there have been no aggregate data summarizing these results. Comprehending the mid- to long-term results, such as frequency of revision arthroscopy and conversion to THA, would aid in selecting patients and counseling patients on the durability of the procedure.
The purpose of this study was to report mid- to long-term outcomes in patients undergoing either primary or revision hip arthroscopy with labral reconstruction for the treatment of irreparable labral tears. We hypothesized that patients would demonstrate favorable outcomes with high survivorship and clinical benefit achievement rates at mid- and long-term follow-up.
Methods
Study Search and Identification
A systematic review of the literature was conducted with the following keywords: “hip arthroscopy,”“labral reconstruction,”“irreparable,”“labrum,”“reconstruction,”“five-year,”“midterm,”“5 year,”“long-term,”“10 year,” ten-year,” and “femoroacetabular impingement” in PubMed, Cochrane, and Scopus in May 2022 using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) criteria. 27 Searches for the 3 databases with Boolean operators are presented in Table 1. Two authors (S.F. and J.S.) performed the search and reached a consensus for all articles included in the study. If the reviewers did not agree after initial evaluation, articles underwent re-review and discussion until agreement was made. Included in the review were any articles with evidence Levels 1 to 4 that reported average 5-year or longer patient-reported outcomes (PROs) after primary or revision hip arthroscopy with labral reconstruction. Midterm was defined as an average 5-year follow-up according to the literature, 22 and long-term was defined as a mean 10-year or longer follow-up.25,33 Only articles in English were included in the review. Articles defined as case reports, reviews, technical notes, or opinions were excluded from the study. References from the included articles were analyzed to determine whether further studies met inclusion criteria and could be included in the review.
Table 1.
Article Searches in PubMed, Cochrane, and Scopus a
| Database | Specific Search |
|---|---|
| PubMed | (hip arthroscopy[Title/Abstract] OR femoroacetabular impingement[Title/Abstract]) AND (labral reconstruction[Title/Abstract] OR irreparable [Title/Abstract] OR labrum[Title/Abstract] OR reconstruction[Title/Abstract]) AND (five-year[Title/Abstract] OR midterm[Title/Abstract] OR 5 year [Title/Abstract] OR long-term[Title/Abstract] OR 10 year[Title/Abstract] OR ten-year[Title/Abstract]) |
| Cochrane | (hip arthroscopy[Title/Abstract/Key] OR femoroacetabular impingement[Title/Abstract/Key]) AND (labral reconstruction[Title/Abstract/Key] OR irreparable [Title/Abstract/Key] OR labrum[Title/Abstract/Key] OR reconstruction[Title/Abstract/Key]) AND (five-year[Title/Abstract/Key] OR midterm[Title/Abstract/Key] OR 5 year [Title/Abstract/Key] OR long-term[Title/Abstract/Key] OR 10 year[Title/Abstract/Key] OR ten-year[Title/Abstract/Key]) |
| Scopus | (hip arthroscopy[Title/Abstract/Key] OR femoroacetabular impingement[Title/Abstract/Key]) AND (labral reconstruction[Title/Abstract/Key] OR irreparable [Title/Abstract/Key] OR labrum[Title/Abstract/Key] OR reconstruction[Title/Abstract/Key]) AND (five-year[Title/Abstract/Key] OR midterm[Title/Abstract/Key] OR 5 year [Title/Abstract/Key] OR long-term[Title/Abstract/Key] OR 10 year[Title/Abstract/Key] OR ten-year[Title/Abstract/Key]) |
Key, keywords.
The initial search resulted in 463 articles. After removal of duplicates, 328 articles underwent title and abstract review. After full-text review, 5 articles were included in the review.16,28,29,33,37 The article selection process is shown in Figure 1.
Figure 1.
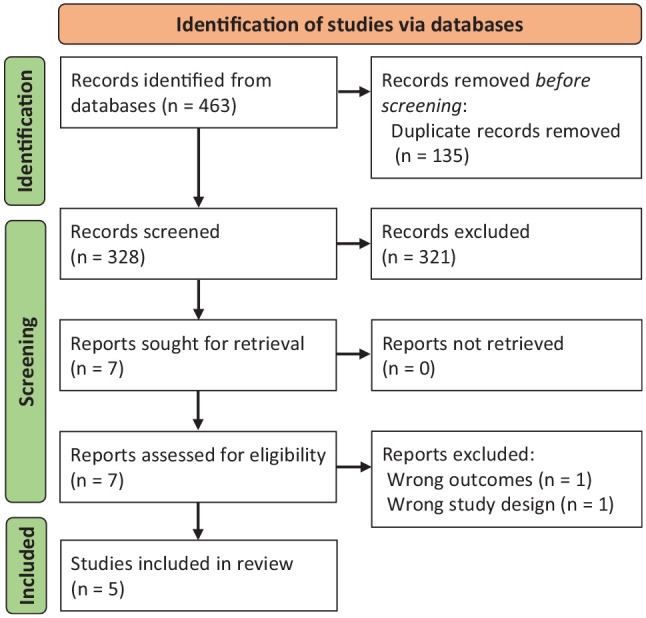
PRISMA flowchart of article selection and screening. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Quality Assessment
The Methodologic Index for Non-Randomized Studies (MINORS) criteria were used to grade all articles included in the review. 39 Two authors (S.F. and J.S.) scored the articles, re-reviewing articles with different initial scores until a consensus was met. The level of evidence of the included articles was established using the criteria set by Hohmann et al. 23
Data Extraction and Statistical Analysis
The following data were recorded from each study: title, author, publication date, study design, patient characteristics, number of hips, follow-up time, study period, indications for hip arthroscopy, PRO scores, radiographic imaging (alpha angle [angle between the center of the femoral neck and point where femoral head loses its sphericity] and lateral center-edge angle [angle between a vertical line through the femoral head and lateral edge of the acetabulum]),21,41 surgical procedures, psychometric thresholds (MCID, maximum outcome improvement [MOI], PASS, and substantial clinical benefit [SCB]), rates of secondary arthroscopies, and conversion to THA. Survivorship was defined as a nonconversion to THA. All extracted data were recorded in Microsoft Word (Microsoft Office 2011).
Forest plots were created for PROs that were reported in ≥3 or studies. Preoperative and postoperative PRO scores were compared using Cochrane's Reviewer Manager web application (RevMan; Version 5.4, The Cochrane Collaboration). Heterogeneity was assessed using the I2 statistic, which was interpreted as follows based on the Cochrane Handbook 15 : I2 between 0% and 40% indicated minimal heterogeneity, between 30% and 60% indicated moderate heterogeneity, between 50% and 90% denoted substantial heterogeneity, and between 75% and 100% denoted considerable heterogeneity.
Results
Study Characteristics
Of the 5 studies (n = 219 hips) included in the review,16,28,29,33,37 4 had Level 3 evidence,16,28,29,37 and 1 had Level 4 evidence. 33 Three studies were cohort studies,16,29,37 and 2 studies were case series.28,33 Article information, including the author, study type, study period, MINORS score, and follow-up, is included in Table 2. There were 178 hips with primary surgeries from all studies and 41 hips with revision surgeries from the Philippon et al 33 study. One study had an average 5-year follow-up, 28 3 studies had a minimum 5-year follow-up,16,29,37 and 1 study had a minimum 10-year follow-up. 33 Irreparable labral tear was a surgical indication in all 5 studies and the most common indication for the surgery. Four studies included only primary labral reconstruction,16,28,29,37 whereas 1 study included both primary and revision surgeries. 33 Surgical indications, radiographic findings, and surgical procedures are listed in Table 3.
Table 2.
Characteristics of Included Studies a
| Lead Author (Year) | Study Type; LOE | Study Period | MINORS Score | No. of Hips | Sex, F/M, No. | Follow-up, mo | Timeline of Follow-up | Age, y | Graft Type | Reconstruction Type | Primary or Revision |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Maldonado 29 (2022) | Cohort study; 3 | 2010-2015 | 15 | 41 | 18/23 | 64.4 ± 24.1 [57-71.8] | Minimum 5 y | 37.5 ± 10.4 [34.4-40.7] | Hamstring tendon autograft, hamstring allograft | Segmental | Primary |
| Domb 16 (2019) | Cohort study; 3 | 2008-2013 | 16 | 23 | 11/12 | 67.2 ± 7.7 (60-89.3) | Minimum 5 y | 35.2 ± 11.9 (15.5-61.9) | NR | Segmental | Primary |
| Scanaliato 37 (2022) | Cohort study; 3 | 2015 | 16 | 62 | 39/23 | 60.37 ± 1.51 | Minimum 5 y | 38.3 (22-70) | Tensor fascia lata allograft | Circumferential | Primary |
| Locks 28 (2017) | Case series; 3 | 2005-2012 | 12 | 11 | 5/6 | 65 (12-120) | Average 5 y | 35 (20-51) | Autologous capsule tissue, indirect head of rectus tendon | Segmental | Primary |
| Philippon 33 (2020) | Case series; 4 | 2006-2008 | 10 | 82 b | 31/51 | NR | Minimum 10 y | 38.7 ± 11.4 (18-65) | Iliotibial band autograft | NR | 41 primary, 41 revision |
Data are reported as mean ± SD (range) or [95% CI] unless otherwise indicated. F, female; LOE, level of evidence; M, male; MINORS, Methodologic Index for Non-Randomized Studies; NR, not reported; PRO, patient-reported outcome.
60 hips with PRO scores.
Table 3.
Indications, Radiographic Findings, and Surgical Treatments a
| Lead Author (Year) | Indications | Radiographic Findings | Surgical Treatment, No. of Hips | Graft Type | |
|---|---|---|---|---|---|
| LCEA | AA | ||||
| Maldonado 29 (2022) | • Failure after 3 mo of nonoperative treatment including rest, physical therapy, NSAIDs, and intra-articular ultrasound-guided injections • Irreparable labral tear • FAIS |
34.5 ± 7.6 [32.2-36.8] | 64.3 ± 10.9 [61-67.7] | • Capsular repair, 16 (39%) • Femoroplasty, 39 (95.1%) • Acetabuloplasty, 40 (97.6%) • Acetabular microfracture, 7 (17.1%) • Femoral head microfracture, 0 (0.0%) • LT debridement, 5 (12.2%) |
Hamstring graft |
| Domb 16 (2019) | • Failure after 3 mo of nonoperative management • Irreparable labral tear • FAI |
NR | — | • Labral reconstruction, 23 (100%) • Capsular repair, 10 (43.5%) • Capsular release, 13 (56.5%) • Acetabuloplasty, 23 (100%) • Femoroplasty, 18 (78.3%) • Acetabular microfracture, 2 (8.7%) • LT debridement, 7 (30.4%) • Iliopsoas fractional lengthening, 12 (52.2%) • Trochanteric bursectomy, 1 (4.3%) |
NR |
| Scanaliato 37 (2022) | • Failure after at least 6 mo of nonoperative treatment • FAI |
33.97 ± 8.2 | 64.12 ± 12.9 | • Cam osteoplasty, 60 (96.8%) • Pincer osteoplasty, 46 (74.2%) • Acetabular chondroplasty, 56 (88.9%) |
Tensor fascia lata allograft |
| Locks 28 (2017) | Labral defects <1 cm in nondysplastic patients | 42 (40-86) | 67 (40-86) | NR | Capsule or indirect head of rectus tendon |
| Philippon 33 (2020) | • Deficient labrum (<5 mm–wide labrum) • If suction seal could not be established during arthroscopic dynamic examination • Irreparable labral tear • Persistent hip pain • Failed physical therapy • FAI |
NR | — | • Cam and pincer decompression, 65 • Cam decompression, 11 • Pincer decompression, 5 • Microfracture, 16 • LT debridement, 60 |
Iliotibial band autograft |
Data are reported as mean ± SD (range) or [95% CI] unless otherwise indicated. AA, alpha angle; FAI, femoroacetabular impingement; FAIS, femoroacetabular impingement syndrome; LCEA, lateral center-edge angle; LT, ligamentum teres; NR, not reported; NSAIDs, nonsteroidal anti-inflammatory drugs.
Surgical Outcomes
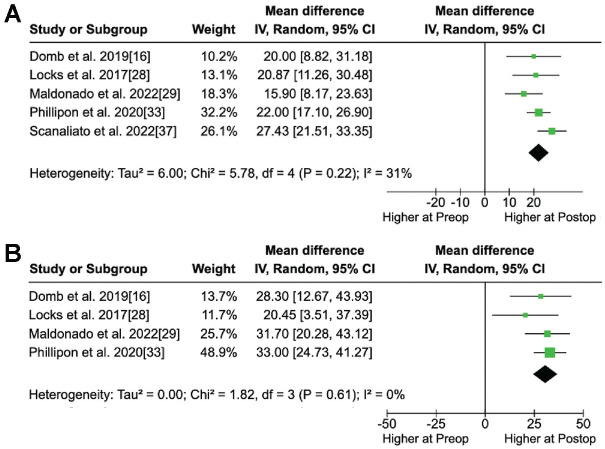
The most common PRO was the mHHS, which was reported in all studies. The mean preoperative mHHS ranged from 58.9 to 66,37,29 and the mean postoperative mHHS at a minimum 5-year follow-up ranged from 80.2 to 89.16,28 The second most common PRO was the HOS-SSS, which was reported in 4 studies.16,28,29,33 The preoperative and minimum 5-year postoperative scores for HOS-SSS ranged from 37.3 to 52 and 65.5 to 79, respectively.16,28 In 4 of the studies,16,28,29,33 patients experienced significant improvement after hip arthroscopy with labral reconstruction (P < .05), as shown in Table 4. Scanaliato et al 37 did not provide P values but reported statistically significant outcomes (P < .05) in outcome scores at a minimum 5-year follow-up. Forest plots of the studies that included mHHS and HOS-SSS scores are shown in Figure 2.
Table 4.
PRO Scores Preoperatively and at Latest Follow-up a
| Outcome Measure | Preoperative | Postoperative | P |
|---|---|---|---|
| Maldonado 29 (2022) | |||
| mHHS | 65.5 ± 17.5 [60.1-70.8] | 81.4 ± 18.2 [75.9-87.0] | <.0001 |
| HOS-SSS | 38.9 ± 23.1 [31.8-45.9] | 70.6 ± 29.3 [61.6-79.6] | <.0001 |
| VAS pain | 5.2 ± 2.2 [4.5-5.9] | 2.8 ± 2.5 [2.0-3.5] | <.0001 |
| NAHS | 61.2 ± 19.4 [55.2-67.1] | 81 ± 19.7 [74.9-87] | <.0001 |
| iHOT-12 | NR | 7.6 ± 2.8 [6.7-8.4] | NR |
| Domb 16 (2019) | |||
| mHHS | 60.2 ± 19.6 (14-96) | 80.2 ± 19.1 (28-100) | .0017 |
| HOS-SSS | 37.3 ± 24.2 (5.6-83) | 65.5 ± 29.6 (2.8-100) | .003 |
| VAS pain | 6 ± 2.7 (0-10) | 2.7 ± 2.7 (0-10) | .0005 |
| NAHS | 55.2 ± 17.3 (22.5-84) | 78.8 ± 21.6 (17.5-100) | .0003 |
| iHOT-12 | NR | 67.1 ± 28.8 (5.3-100) | NR |
| Scanaliato 37 (2022) | |||
| mHHS | 58.85 ± 17.4 | 86.28 ± 16.2 | NR |
| iHOT-12 | 32.84 ± 13.5 | 79.52 ± 18.3 | NR |
| VAS pain | 47.67 ± 17.1 | 26.07 ± 16.8 | NR |
| VAS satisfaction | NR | 85.14 ± 17.4 | NR |
| Locks 28 (2017) | |||
| HOS-ADL | 73 | 89 | <.05 |
| HOS-SSS | 52 | 79 | <.05 |
| mHHS | 66 | 89 | <.05 |
| Satisfaction | NR | 9 (3-10) | NR |
| Philippon 33 (2020) | |||
| HOS-ADL | 69 ± 17 | 90 ± 17 | .004 |
| HOS-SSS | 43 ± 26 | 76 ± 28 | .001 |
| mHHS | 60 ± 16 | 82 ± 16 | .001 |
| WOMAC | 33 ± 18 | 12 ± 15 | <.01 |
| SF-12 MCS | 54 ± 9 | 54 ± 7 | .83 |
| SF-12 PCS | 44 ± 10 | 51 ± 10 | .014 |
Data are reported as the mean value, with ± SD, [95% CI], or (range). HOS-ADL, Hip Outcome Score-Activities of Daily Living; HOS-SSS, Hip Outcome Score-Sports Specific Subscale; iHOT-12, International Hip Outcome Tool-12; mHHS, modified Harris Hip Score; NAHS, Non-Arthritic Hip Score; NR, not reported; PRO, patient-reported outcome; SF-12 MCS, 12-Item Short Form Health Survey-Mental Component Score; SF-12 PCS, 12-Item Short Form Health Survey-Physical Component Score; VAS, visual analog scale; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Score.
Figure 2.
Forest plots of the studies that included preoperative and postoperative data for the (A) mHHS (heterogeneity, I2 = 31%) and (B) HOS-SSS (heterogeneity, I2 = 0%). HOS-SSS, Hip Outcome Score-Sports Specific Subscale; IV, inverse variance; mHHS, modified Harris Hip Score; Preop, preoperative; Postop, postoperative.
Four studies reported clinical benefit in the form of psychometric thresholds, including MCID, PASS, MOI, and SCB.16,29,33,37 All 4 studies reported that patients undergoing hip arthroscopy and labral reconstruction achieved at least 1 psychometric threshold, at a rate ranging from 66.7% to 100%.16,37 The most commonly reported psychometric tools were MCID and PASS, which ranged from 72% to 100% and 66.7% to 96.7%, respectively.16,29,33,37 Table 5 lists the rates of achievement of psychometric threshold for each study.
Table 5.
Achievement Rates of Psychometric Thresholds a
| Psychometric Threshold | Achievement Rate |
|---|---|
| Maldonado 29 (2022) | |
| MCID | |
| mHHS | 23 (76.7) |
| VAS | 26 (86.7) |
| NAHS | 28 (93.3) |
| PASS | |
| mHHS | 29 (96.7) |
| iHOT-12 | 24 (80) |
| Domb 16 (2019) | |
| MIC for mHHS | 11 (73.3) |
| MCID for HOS-SSS | 12 (73.3) |
| PASS | |
| mHHS | 10 (66.7) |
| HOS-SSS | 7 (66.7) |
| Scanaliato 37 (2022) | |
| MCID | |
| iHOT-12 | 62 (100) |
| mHHS | 62 (100) |
| PASS | |
| iHOT-12 | 45 (72.58) |
| mHHS | 49 (79.03) |
| MOI | |
| iHOT-12 | 43 (69.4) |
| mHHS | 44 (71) |
| SCB | |
| iHOT-12 | 33 (53.23) |
| mHHS | 25 (40.32) |
| Philippon 33 (2020) b | |
| MCID | |
| HOS-ADL | 80% |
| HOS-SSS | 86% |
| mHHS | 72% |
| PASS | |
| HOS-ADL | 87% |
| HOS-SSS | 92% |
| mHHS | 87% |
Data are reported as mean (%) unless otherwise indicated. HOS-ADL, Hip Outcome Score-Activities of Daily Living; HOS-SSS, Hip Outcome Score-Sports Specific Subscale; iHOT-12, International Hip Outcome Tool-12; MCID, minimal clinically important difference; mHHS, modified Harris Hip Score; MIC, minimal important change; MOI, maximum outcome improvement; NAHS, Non-Arthritic Hip Score; PASS, Patient Acceptable Symptom State; SCB, substantial clinical benefit; THA, total hip arthroplasty;VAS, visual analog scale.
For patients who did not undergo conversion to THA or revision arthroscopy (n = 50).
Survivorship
All 5 studies reported secondary surgery rates. The conversion to THA ranged from 0% to 27%,28,33 whereas the overall secondary surgery rates ranged from 0% to 36%.28,33 The rates of conversion to THA were 0%, 28 1.61%, 37 13%, 16 17%, 29 and 27%, 33 where the 27% was reported for the cohort with a minimum 10-year follow-up. 33 Further, Philippon et al 33 reported overall secondary surgery rates at both 5-year and minimum 10-year follow-up. The secondary surgery rates were 0%, 28 6.45%, 37 24.8%, 16 26.8%, 29 30%, 33 and 36%, 33 where the reported 36% was for the minimum 10-year follow-up cohort. Survivorship is presented in Table 6.
Table 6.
Summary of Survivorship Rates a
| Lead Author (Year) | Follow-up Time | Secondary Hip Preservation Procedure, % | Time to Secondary Hip Preservation Procedure, mo | Conversion to THA, % | Time to Conversion, mo | Overall Secondary Surgery Rate, % |
|---|---|---|---|---|---|---|
| Maldonado 29 (2022) | 64.4 ± 24.1 [57-71.8] mo | 9.8 | 19 ± 1.8 | 17 | 32.3 ± 18.5 | 26.8 |
| Domb 16 (2019) | 67.2 ± 7.7 (60-89.3) mo | 11.8 | 18.7 ± 18.2 | 13 | NR | 24.8 |
| Scanaliato 37 (2022) | 60.37 ± 1.51 mo | 4.84 | NR | 1.61 | NR | 6.45 |
| Locks 28 (2017) | 65 (12-120) mo | 0 | - | 0 | - | 0 |
| Philippon 33 (2020) | 5 y | NR | NR | NR | NR | 30 |
| Minimum 10 y | 9 | 31 | 27 | 38.4 ± 31.3 (5-102) | 36 |
Data are reported as the mean value, with ± SD, (range), or [95% CI] unless otherwise indicated. Dashes indicate areas not applicable. NR, not reported; THA, total hip arthroplasty.
Discussion
The main finding of this review was that, at mid- to long-term follow-up, patients undergoing either primary or revision hip arthroscopy with labral reconstruction, in the context of irreparable labral tears, demonstrated satisfactory outcomes and low-to-moderate rates of undergoing secondary surgery (ranging from 0% to 36%). We found that, at a minimum of 5-year follow-up, patients undergoing primary and revision hip arthroscopy with labral reconstruction reported favorable clinical outcomes with significant improvements in PROs across all 5 reviewed studies.16,28,29,33,37 The methodologies of the included studies varied with respect to surgical technique, graft source, graft selection, and indications for hip arthroscopy with labral reconstruction.
Since the first study published on labral reconstruction by Sierra and Trousdale in 2009, 38 many additional studies have reported on significantly improved outcomes with labral reconstruction using different techniques and graft sources.28,29,37 Scanaliato et al 37 studied long-term outcomes for patients who underwent primary arthroscopic treatment of hip labral pathology and found similar outcomes for patients who underwent reconstruction versus primary labral repair. In addition, they found that even though the reconstruction group had older patients, more severe labral tears, and worse chondral damage, the group still had outcomes comparable with those of the repair cohort. 37 The literature largely suggests that additional factors such as female sex, age >45 years, increased body mass index, and labral debridement can be predictive of negative outcomes after hip arthroscopy. 40 Further research on the demographic and comorbidity differences and their effect on labral reconstruction will be helpful in provider decision-making.
Many different types of grafts have been used for labral reconstruction in the literature with generally favorable outcomes. 6 Studies in the literature found iliotibial band, gracilis, anterior tibialis, and semitendinosus autografts to have biomechanical properties similar to those of the native labrum. 19 To date, however, there has not been consensus on graft choice.6,17,29,30 Studies by Amar et al 2 and Rathi and Mazek 35 investigated the use of the indirect head of the rectus femoris and found significant improvement in mHHS. Locks et al 28 also studied the use of the indirect of the head of the rectus femoris in addition to capsule tissue and similarly found improvement in mHHS with no complications, need for revision arthroscopy, or conversion to THA in the follow-up period.
Several studies have compared the use of allograft versus autograft for reconstruction of irreparable labral tears.14,22,34 Allografts have the disadvantages of restricted availability, higher costs, and delayed incorporation. On the other hand, autografts may have increased morbidity for the patient and cause additional graft-site pain, nerve injury, risk of infection, and wound healing complications. One of the studies included in the current review, Maldonado et al, 29 found that the outcomes of acetabular arthroscopic segmental labral reconstruction using allograft or autograft were similar in terms of patient satisfaction, PROs, and rates of achieving MCID and PASS. Similarly, Cooper et al 14 found no difference in patient satisfaction and PROs between patients undergoing hip arthroscopy and labral reconstruction with autograft as compared with allograft; however, there was a higher revision rate noted for the allograft group compared with the autograft group (23.6% vs 7.3%; P = .001). As a result, more data in the future will be needed to further elucidate these differences.
We found consistent improvement in postoperative PROs across all studies in this review; however, THA rates varied from study to study ranging from 0% to 27%.28,33 Philippon et al, 33 who recorded the highest rate, however, also reported a 10-year THA rate of just 10% for those with >2 mm of joint space. This finding is consistent with a study after labral reconstructions in 76 hips by Geyer et al, 20 who reported ≤2 mm joint space as a statistically significant risk factor for THA using a Cox proportional hazards model. On the contrary, Locks et al, 28 who recorded the lowest THA conversion rate in this review, reported just 1 of 11 hips with ≤2 mm joint space and exclusively treated small labral defects (<1 cm). The selection used by Locks et al 28 for healthier hips may have contributed to their improved midterm outcomes. With that, the findings from this review reinforce the importance of patient selection in labral reconstructions and support the need for more research focused on better defining surgical indications and guidelines. Ultimately, data from this review show that patients can still do well with labral reconstructions in the absence of these specific guidelines, as long as they have irreparable labral tears and symptoms refractory to conservative treatment.
Limitations
This review has several limitations that must be acknowledged. First, we included patients undergoing labral reconstruction with a variety of surgical techniques, graft choices, and size of reconstruction, which may confound outcomes. Second, the wide study period of some studies may have failed to capture trends of improving surgical techniques, including capsular closure, which could have influenced patient outcomes. Third, we included patients who underwent both primary and revision hip arthroscopy, which added to the heterogeneity of the group studied. Fourth, multiple studies from the same institution were included, and the same patients may have been included in multiple studies. Fifth, this review incorporated nonrandomized studies, which limited external validity and introduced selection bias into the study. Sixth, the number of articles screened for inclusion in this review were constrained by the comprehensive but finite set of search terms used. Finally, we did not report complication rates, which was influenced by the limited data and lack of emphasis on operative complications in the studies reviewed.
Conclusion
Our systematic review demonstrated that patients undergoing primary and revision hip arthroscopy with labral reconstruction experience favorable outcomes and high rates of clinical benefit and survivorship at mid- to long-term follow-up.
Footnotes
Final revision submitted June 14, 2023; accepted August 16, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: D.R.M. has received a grant from Arthrex; education payments from Arthrex, Micromed, and Smith & Nephew; and nonconsulting fees from Arthrex. A.E.J. has received a grant from Arthrex and education payments from Arthrex, Medwest Associates, and Gotham Surgical Solutions & Devices. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Akpinar B, Lin LJ, Bloom DA, Youm T. Hip arthroscopy for femoroacetabular impingement: 1-year outcomes predict 5-year outcomes. Am J Sports Med. 2021;49(1):104-111. [DOI] [PubMed] [Google Scholar]
- 2. Amar E, Sampson TG, Sharfman ZT, et al. Acetabular labral reconstruction using the indirect head of the rectus femoris tendon significantly improves patient reported outcomes. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2512-2518. [DOI] [PubMed] [Google Scholar]
- 3. Beals T, Soares R, Briggs K, Day H, Philippon M. Ten-year outcomes after hip arthroscopy in patients with femoroacetabular impingement and borderline dysplasia. Am J Sports Med. 2022;50(3):739-745. [DOI] [PubMed] [Google Scholar]
- 4. Beck EC, Drager J, Nwachukwu BU, et al. Patients with borderline hip dysplasia achieve clinically significant improvement after arthroscopic femoroacetabular impingement surgery: a case-control study with a minimum 5-year follow-up. Am J Sports Med. 2020;48(7):1616-1624. [DOI] [PubMed] [Google Scholar]
- 5. Bedi A, Chen N, Robertson W, Kelly BT. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy. 2008;24(10):1135-1145. [DOI] [PubMed] [Google Scholar]
- 6. Bessa FS, Williams BT, Polce EM, et al. Indications and outcomes for arthroscopic hip labral reconstruction with autografts: a systematic review. Front Surg. 2020;7:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bharam S. Labral tears, extra-articular injuries, and hip arthroscopy in the athlete. Clin Sports Med. 2006;25(2):279-292. [DOI] [PubMed] [Google Scholar]
- 8. Bolia IK, Fagotti L, Briggs KK, Philippon MJ. Midterm outcomes following repair of capsulotomy versus nonrepair in patients undergoing hip arthroscopy for femoroacetabular impingement with labral repair. Arthroscopy. 2019;35(6):1828-1834. [DOI] [PubMed] [Google Scholar]
- 9. Bonazza NA, Homcha B, Liu G, Leslie DL, Dhawan A. Surgical trends in arthroscopic hip surgery using a large national database. Arthroscopy. 2018;34(6):1825-1830. [DOI] [PubMed] [Google Scholar]
- 10. Boykin RE, Patterson D, Briggs KK, Dee A, Philippon MJ. Results of arthroscopic labral reconstruction of the hip in elite athletes. Am J Sports Med. 2013;41(10):2296-2301. [DOI] [PubMed] [Google Scholar]
- 11. Bryan AJ, Krych AJ, Pareek A, Reardon PJ, Berardelli R, Levy BA. Are short-term outcomes of hip arthroscopy in patients 55 years and older inferior to those in younger patients? Am J Sports Med. 2016;44(10):2526-2530. [DOI] [PubMed] [Google Scholar]
- 12. Byrd JWT, Jones KS. Arthroscopic acetabular labral repair in patients over the age of 60 years: a matched case-control study. Arthroscopy. 2019;35(5):1406-1410. [DOI] [PubMed] [Google Scholar]
- 13. Byrd JWT, Jones KS. Hip arthroscopy in athletes: 10-year follow-up. Am J Sports Med. 2009;37(11):2140-2143. [DOI] [PubMed] [Google Scholar]
- 14. Cooper JD, Dekker TJ, Ruzbarsky JJ, Pierpoint LA, Soares RW, Philippon MJ. Autograft versus allograft: the evidence in hip labral reconstruction and augmentation. Am J Sports Med. 2021;49(13):3575-3581. [DOI] [PubMed] [Google Scholar]
- 15. Deeks JJ, Higgins JPT, Altman DG. Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, eds. Cochrane Handbook for Systematic Reviews of Interventions. Version 6.3. Updated February 2022. Cochrane; 2022. http://www.training.cochrane.org/handbook
- 16. Domb BG, Battaglia MR, Perets I, et al. Minimum 5-year outcomes of arthroscopic hip labral reconstruction with nested matched-pair benchmarking against a labral repair control group. Am J Sports Med. 2019;47(9):2045-2055. [DOI] [PubMed] [Google Scholar]
- 17. Domb BG, Kyin C, Rosinsky PJ, et al. Circumferential labral reconstruction for irreparable labral tears in the primary setting: minimum 2-year outcomes with a nested matched-pair labral repair control group. Arthroscopy. 2020;36(10):2583-2597. [DOI] [PubMed] [Google Scholar]
- 18. Domb BG, Yuen LC, Ortiz-Declet V, Litrenta J, Perets I, Chen AW. Arthroscopic labral base repair in the hip: 5-year minimum clinical outcomes. Am J Sports Med. 2017;45(12):2882-2890. [DOI] [PubMed] [Google Scholar]
- 19. Ferro FP, Philippon MJ, Rasmussen MT, Smith SD, LaPrade RF, Wijdicks CA. Tensile properties of the human acetabular labrum and hip labral reconstruction grafts. Am J Sports Med. 2015;43(5):1222-1227. [DOI] [PubMed] [Google Scholar]
- 20. Geyer MR, Philippon MJ, Fagrelius TS, Briggs KK. Acetabular labral reconstruction with an iliotibial band autograft: outcome and survivorship analysis at minimum 3-year follow-up. Am J Sports Med. 2013;41(8):1750-1756. [DOI] [PubMed] [Google Scholar]
- 21. Hanson JA, Kapron AL, Swenson KM, Maak TG, Peters CL, Aoki SK. Discrepancies in measuring acetabular coverage: revisiting the anterior and lateral center edge angles. J Hip Preserv Surg. 2015;2(3):280-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hevesi M, Hartigan DE, Wu IT, Levy BA, Domb BG, Krych AJ. Are results of arthroscopic labral repair durable in dysplasia at midterm follow-up? A 2-center matched cohort analysis. Am J Sports Med. 2018;46(7):1674-1684. [DOI] [PubMed] [Google Scholar]
- 23. Hohmann E, Feldman M, Hunt TJ, Cote MP, Brand JC. Research Pearls: How Do We Establish the Level of Evidence? Arthroscopy. 2018. Dec;34(12):3271-3277. [DOI] [PubMed] [Google Scholar]
- 24. Jimenez A, Lee M, Owens J, et al. Revision hip arthroscopy with labral reconstruction for irreparable labral tears in athletes: minimum 2-year outcomes with a benchmark control group. Am J Sports Med. 2022;50(6):1571-1581. [DOI] [PubMed] [Google Scholar]
- 25. Lapner P, Li A, Pollock JW, et al. A multicenter randomized controlled trial comparing single-row with double-row fixation in arthroscopic rotator cuff repair: long-term follow-up. Am J Sports Med. 2021;49(11):3021-3029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lee S, Wuerz TH, Shewman E, et al. Labral reconstruction with iliotibial band autografts and semitendinosus allografts improves hip joint contact area and contact pressure: an in vitro analysis. Am J Sports Med. 2015;43(1):98-104. [DOI] [PubMed] [Google Scholar]
- 27. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1-e34. [DOI] [PubMed] [Google Scholar]
- 28. Locks R, Chahla J, Bolia IK, Briggs KK, Philippon MJ. Outcomes following arthroscopic hip segmental labral reconstruction using autologous capsule tissue or indirect head of the rectus tendon. J Hip Preserv Surg. 2017;5(1):73-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Maldonado D, Kyin C, Simpson J, et al. Minimum 5-year outcomes after primary segmental labral reconstruction for irreparable labral tears in the hip with hamstring grafts: with a subanalysis comparing autograft versus allograft. Am J Sports Med. 2022;50(7):1876-1887. [DOI] [PubMed] [Google Scholar]
- 30. Maldonado DR, Lall AC, Laseter JR, et al. Primary hip arthroscopic surgery with labral reconstruction: is there a difference between an autograft and allograft? Orthop J Sports Med. 2019;7(3):2325967119833715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Menge TJ, Briggs KK, Rahl MD, Philippon MJ. Hip arthroscopy for femoroacetabular impingement in adolescents: 10-year patient-reported outcomes. Am J Sports Med. 2021;49(1):76-81. [DOI] [PubMed] [Google Scholar]
- 32. Nepple JJ, Philippon MJ, Campbell KJ, et al. The hip fluid seal - Part II: the effect of an acetabular labral tear, repair, resection, and reconstruction on hip stability to distraction. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):730-736. [DOI] [PubMed] [Google Scholar]
- 33. Philippon MJ, Arner JW, Crawford MD, Bolia IK, Briggs KK. Acetabular labral reconstruction with iliotibial band autograft: outcome and survivorship at a minimum 10-year follow-up. J Bone Joint Surg Am. 2020;102(18):1581-1587. [DOI] [PubMed] [Google Scholar]
- 34. Rahl MD, LaPorte C, Steinl GK, O’Connor M, Lynch TS, Menge TJ. Outcomes after arthroscopic hip labral reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2020;48(7):1748-1755. [DOI] [PubMed] [Google Scholar]
- 35. Rathi R, Mazek J. Arthroscopic acetabular labral reconstruction with rectus femoris tendon autograft: our experiences and early results. J Orthop. 2018;15(3):783-786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Riff AJ, Kunze KN, Movassaghi K, et al. . Systematic review of hip arthroscopy for femoroacetabular impingement: the importance of labral repair and capsular closure. Arthroscopy. 2019;35(2):646-656. [DOI] [PubMed] [Google Scholar]
- 37. Scanaliato JP, Green CK, Salfiti CE, Patrick CM, Wolff AB. Primary arthroscopic labral management: labral repair and complete labral reconstruction both offer durable, promising results at minimum 5-year follow-up. Am J Sports Med. 2022;50(10):2622-2628. [DOI] [PubMed] [Google Scholar]
- 38. Sierra RJ, Trousdale RT. Labral reconstruction using the ligamentum teres capitis: report of a new technique. Clin Orthop Relat Res. 2009;467(3):753-759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712-716. [DOI] [PubMed] [Google Scholar]
- 40. Sogbein OA, Shah A, Kay J, et al. Predictors of outcomes after hip arthroscopic surgery for femoroacetabular impingement: a systematic review. Orthop J Sports Med. 2019;7(6):2325967119848982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Youngman TR, Wagner KJ, III, Montanez B, et al. The association of α angle on disease severity in adolescent femoroacetabular impingement. J Pediatr Orthop. 2021;41(2):88-92. [DOI] [PMC free article] [PubMed] [Google Scholar]