Abstract
Purpose:
The purpose of this study is to assess clinical and functional outcomes in separate cohorts of operatively and nonoperatively managed pediatric patella fractures.
Methods:
A retrospective review was completed for patients aged 5–19 years treated for a unilateral patella fracture at a single pediatric level-1 trauma center. Patients were excluded for osteochondral fracture associated with patellar dislocation, polytrauma presentation with additional fractures, or <3 months of clinical follow-up. Functional outcomes were assessed via the Pediatric International Knee Documentation Committee form and the Marx Knee Activity Scale.
Results:
A total of 53 patients met inclusion criteria; 30 patients were treated operatively and 23 patients were treated nonoperatively. Patients with patellar sleeve/pole fractures were significantly younger by 5.2 years (p < 0.01) and presented with greater variability in mechanism of injury (p < 0.01). The nonoperative cohort achieved bony healing and returned to sports at a median (interquartile range) of 1.7 (1.2–2.3) months and 2.8 (2.3–3.3) months, respectively, post-injury. The operative group achieved bony healing and returned to sports at 2.8 (2.1–3.5) months and 5.9 (4.0–7.1) months, respectively, following surgery. Median (interquartile range) Pediatric International Knee Documentation Committee and Marx scores were 98 (89–100) and 14 (10–16), respectively, for the nonoperative group, and 92 (84–99) and 13 (12–16), respectively, for the operative group. No significant differences in patient-reported outcomes were observed between fracture patterns or treatment cohorts.
Conclusion:
Pediatric and adolescent patients sustaining patella fractures reported long-term functional outcomes comparable to normative values, across multiple fracture patterns and with appropriate operative and nonoperative treatment. Fractures requiring surgery were expectedly associated with slower healing and return to sport timelines.
Level of evidence:
Therapeutic Level III.
Keywords: Patella, fracture, knee, pediatric, patient-reported outcomes
Introduction
In children and adolescents, patella fractures are rare, accounting for less than 1% of all pediatric fractures.1,2 However, given the clinical anatomy and biomechanics of the patella, such fractures can be debilitating. 3 Patella fractures may be classified as nondisplaced versus displaced, which generally denotes a cortical or subchondral bony step-off or fracture gap of ≥2 mm. Classification by fracture morphology is also typical, and a common descriptive construct includes transverse, vertical, comminuted/stellate, or patellar pole/sleeve (upper or lower) fractures. 1 Inciting injuries are generally either direct blunt-force trauma to the anterior knee (e.g. dashboard injury, fall onto flexed knee, fall from elevated surface) or an indirect force from sudden eccentric quadriceps contraction (e.g. landing on one’s feet after jumping from a moderate height, sudden deceleration from a full sprint).1,3,4 An important consideration specifically for the pediatric population is the “patellar sleeve” fracture, so named because the deep portion of the distal fracture fragment consists of a cartilage “sleeve” that has separated from the main ossific nucleus of the patella in skeletally immature patients. While the incidence of sleeve fractures is rare overall, one study suggested they may account for >50% of pediatric patella fractures. 5
Given the rarity of patella fractures in both the adult and pediatric population, there is a significant lack of higher-level evidence regarding outcomes of the various treatment interventions. In adult studies, nonoperative management consisting of knee immobilization in extension has been associated with excellent outcomes, given the proper indications. 6 Conversely, there is a suggestion of greater long-term immobility and activity limitation following patella fracture surgery, in part due to hardware-related symptoms and secondary surgeries.1,4 However, the pediatric literature remains devoid of a clear picture of the clinical course, return to activities, and patient-reported functional outcomes following patellar fractures, regardless of treatment. The purpose of this study was therefore to assess the demographics, radiographic features, treatment approaches, clinical course, and functional outcomes in a larger series of patella fractures in children and adolescents.
Materials and methods
Retrospective assessment
Following institutional review board approval, a retrospective chart review was conducted for all cases of isolated unilateral patella fractures in patients aged 5–19 years old presenting to a single pediatric tertiary-care center over a 10-year period. Osteochondral fractures associated with patellofemoral instability, knee dislocations, and polytrauma presentations with multiple fractures were excluded. Mechanism of injury was classified as either “direct blow,” “jumping/landing,” or “twisting.” Assessment of radiographic classification, which was performed by a pediatric orthopedic surgery fellow and a senior orthopedic surgery resident, included descriptive fracture morphology, displacement, and presence of joint effusion or soft tissue swelling. Based on prior studies in adult patients, morphologic descriptors included vertical, patellar sleeve/pole, transverse, or comminuted/stellate fractures (Figure 1(a)–(h)). 1 Disagreement between the two readers was resolved with decisions by the senior attending orthopedic surgeon author. Charts were further reviewed for any incidence of infection, residual pain or stiffness reported in post-injury clinic visits, subsequent surgeries, including planned or unplanned hardware removal, and any other complications. Clinical outcomes recorded included time to radiographic healing as specified by the treating provider or the senior author, if clear healing parameters or descriptors were not included in the record, time to return-to-sport, final descriptions of knee range of motion, and any noted persistence of a “residual extensor lag” at the time of final follow-up. Residual extensor lag was defined as ≥5 degree active extension deficit from the contralateral side with attempted straight leg raise, which was easily corrected with passive extension to equal or exceed the contralateral side. “Residual stiffness” was instead defined as a ≥5 degree deficit from the contralateral side, in terms of flexion or extension, which could not be corrected passively.
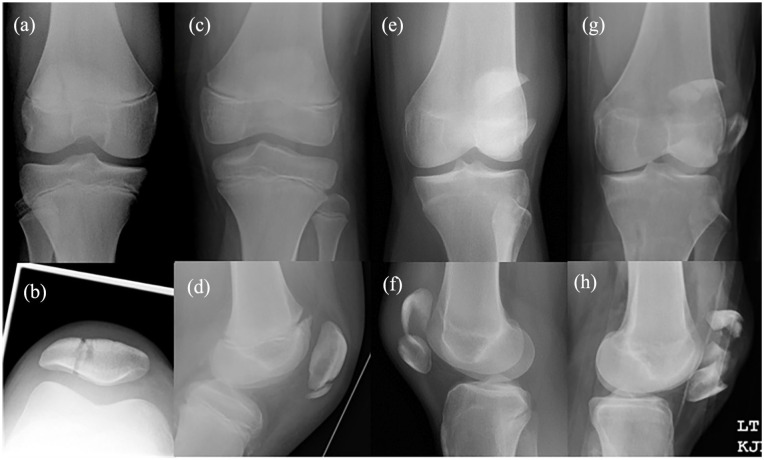
Figure 1.
Fracture pattern classification according to the descriptive morphology used in this study: (a) and (b) vertical, (c) and (d) sleeve/pole, (e) and (f) transverse, and (g) and (h) comminuted.
Prospective functional outcome assessment
All patients included in the retrospective portion of the study were sent, by mail, two patient-reported outcome (PRO) questionnaires: the Pediatric International Knee Documentation Committee (Pedi-IKDC) form and the Marx Activity Scale. Pre-operative PROs were not obtained. The Pedi-IKDC is a knee-specific, outcome instrument which was modified from its adult form and validated for the pediatric and adolescent population by Kocher et al. 7 It is a 13-item questionnaire that is scored on a 0-to-100-point scale, and it can be used to measure a patient’s current subjective and objective knee symptoms and function. The Marx activity scale is a short, four-item questionnaire that more specifically quantifies the frequency and intensity of an individual’s athletic activity. 8 Each question is scored on a 0-to-4-point scale, for a maximum value of 16. While it has not been explicitly validated for the pediatric and adolescent population in the same manner as the Pedi-IKDC, it has been shown to be reliable, although with a significant ceiling effect. 9
Statistical analysis
Patient, injury, treatment, and outcome characteristics were summarized for all subjects. Categorical variables were summarized by frequency and percent. Continuous variables were summarized by median and interquartile range (IQR, 25th–75th percentile). Patient and injury characteristics were compared across treatment groups (operative vs conservative) and fracture patterns using Fisher’s exact test or the Mann–Whitney U-test, as appropriate. Time to healing, return to sport, Pedi-IKDC score, and Marx scale score were compared across treatment groups using the Mann–Whitney U-test. Statistical analyses were performed using SPSS software v.28.0.1.1 (14) (IBM Corp., Armonk, NY, USA).
Results
Over the 10-year study period, 53 patients met inclusion criteria. All fractures were closed injuries, with 23 patients treated nonoperatively and 30 patients treated operatively. At the time of injury, 34 (64%) patients had open physes, 12 (23%) patients had closing physes, and 7 (13%) were closed. Demographic information and clinical outcomes for the entire study group are presented in Table 1. Individual patient-level data are presented in Supplemental Table 1.
Table 1.
Demographics, clinical data, and functional outcomes for the entire study cohort.
| N | n (%N) | Median (IQR) | |
|---|---|---|---|
| Baseline characteristics | |||
| Age at diagnosis | 53 | – | 12.1 (10.1–15.1) |
| Sex (% male) | 53 | 35 (66%) | – |
| Mechanism of injury | |||
| Direct blow | 53 | 37 (70%) | – |
| Jumping/landing | 53 | 10 (19%) | – |
| Twisting | 53 | 6 (11%) | – |
| Fracture pattern | |||
| Vertical | 53 | 4 (7%) | – |
| Sleeve/pole | 53 | 28 (53%) | – |
| Transverse | 53 | 9 (17%) | |
| Comminuted | 53 | 12 (23%) | – |
| Fracture displacement | |||
| Displaced | 53 | 29 (55%) | – |
| Nondisplaced | 53 | 24 (45%) | – |
| Physical exam findings | |||
| Effusion | 53 | 49 (92%) | – |
| Soft tissue swelling | 53 | 53 (100%) | – |
| Post-treatment outcomes and complications | |||
| Clinical follow-up (months) | 53 | – | 8 (4–22) |
| Time to healing (months) | 53 | – | 2.2 (1.6–3.4) |
| Return to sports (months) | 50 | – | 3.9 (2.9–6.4) |
| Residual stiffness | 53 | 3 (6%) | – |
| Residual extensor lag | 53 | 4 (7%) | – |
| PRO follow-up (years) | 21 | – | 4.8 (3.5–7.6) |
| Pedi-IKDC | 21 | – | 92 (84–100) |
| Marx | 21 | – | 13 (12–16) |
IQR: interquartile range; PRO: patient-reported outcome; Pedi-IKDC: Pediatric International Knee Documentation Committee.
Treatment approach was relatively evenly distributed within three of the four described fracture pattern cohorts. Comminuted fractures underwent surgery in 11 of 12 cases. Analysis of the study cohort by fracture pattern is presented in Table 2, and direct comparison of outcomes between the operative and nonoperative cohorts is presented in Table 3. Finally, an analysis comparing all demographics and retrospectively collected clinical outcomes between subjects who responded to PROs and those who did not is presented in Table 4.
Table 2.
Analysis of the study cohort by fracture pattern.
| Comminuted/transverse/vertical | Sleeve/pole | p | |||||
|---|---|---|---|---|---|---|---|
| N | n (%N) | Median (IQR) | N | n (%N) | Median (IQR) | ||
| Baseline characteristics | |||||||
| Age at diagnosis | 25 | – | 14.9 (11.7–16.1) | 28 | – | 11.0 (9.9–13.1) | <0.01 |
| Sex (% male) | 25 | 15 (60%) | – | 28 | 20 (71%) | – | 0.40 |
| Mechanism of injury | <0.01 | ||||||
| Direct blow | 25 | 23 (92%) | – | 28 | 14 (50%) | – | |
| Jumping/landing | 25 | 1 (4%) | – | 28 | 9 (32%) | – | |
| Twisting | 25 | 1 (4%) | – | 28 | 5 (18%) | – | |
| Fracture displacement | 0.27 | ||||||
| Displaced | 25 | 16 (64%) | – | 28 | 13 (46%) | – | |
| Effusion | 25 | 25 (100%) | – | 28 | 24 (86%) | – | 0.11 |
| Operative versus nonoperative | 0.17 | ||||||
| Operative | 25 | 17 (68%) | – | 28 | 13 (46%) | – | |
| Nonoperative | 25 | 8 (32%) | – | 28 | 15 (54%) | – | |
| Removal of hardware | 17 | 12 (71%) | – | 13 | 5 (38%) | – | 0.04 |
| Post-treatment outcomes and complications | |||||||
| Time to healing (months) | 25 | – | 2.4 (1.6–3.4) | 28 | – | 2.2 (1.7–3.4) | 0.75 |
| Return to sports (months) | 25 | – | 5.0 (3.0–6.3) | 28 | – | 3.7 (2.7–6.5) | 0.65 |
| Residual stiffness | 25 | 1 (4%) | – | 28 | 2 (7%) | – | 1.00 |
| Residual extensor lag | 25 | 0 (0%) | – | 28 | 4 (14%) | – | 0.11 |
| Pedi-IKDC | 13 | – | 95 (84–100) | 8 | – | 91 (85–97) | 0.58 |
| Marx | 13 | – | 12 (10–15) | 8 | – | 16 (13–16) | 0.03 |
IQR: interquartile range; Pedi-IKDC: Pediatric International Knee Documentation Committee. Bolded p-values signify statistically significant differences.
Table 3.
Analysis of the cohort by operative versus nonoperative treatment.
| Operative | Nonoperative | p | |||||
|---|---|---|---|---|---|---|---|
| N | n (%N) | Median (IQR) | N | n (%N) | Median (IQR) | ||
| Baseline characteristics | |||||||
| Age at diagnosis | 30 | – | 14.2 (10.3–15.9) | 23 | – | 11.5 (9.7–13.2) | 0.01 |
| Sex (% male) | 30 | 22 (73%) | – | 23 | 13 (57%) | – | 0.25 |
| Mechanism of injury | 0.62 | ||||||
| Direct blow | 30 | 19 (64%) | – | 23 | 18 (78%) | – | |
| Jumping/landing | 30 | 7 (23%) | – | 23 | 3 (13%) | – | |
| Twisting | 30 | 4 (13%) | – | 23 | 2 (9%) | – | |
| Fracture pattern | 0.03 | ||||||
| Vertical | 30 | 2 (7%) | – | 23 | 2 (9%) | – | |
| Sleeve/pole | 30 | 13 (43%) | – | 23 | 15 (65%) | – | |
| Transverse | 30 | 4 (13%) | – | 23 | 5 (22%) | – | |
| Comminuted | 30 | 11 (37%) | – | 23 | 1 (4%) | – | |
| Fracture displacement | <0.01 | ||||||
| Displaced | 30 | 29 (97%) | – | 23 | 0 (0%) | – | |
| Effusion | 30 | 30 (100%) | – | 23 | 19 (83%) | – | 0.03 |
| Post-treatment outcomes and complications | |||||||
| Clinical follow-up (months) | 30 | – | 14 (7–31) | 23 | – | 4 (3–8) | <0.01 |
| Time to healing (months) | 30 | – | 2.8 (2.1–3.5) | 23 | – | 1.7 (1.2–2.3) | <0.01 |
| Return to sports (months) | 30 | – | 5.9 (4.0–7.1) | 20 | – | 2.8 (2.3–3.3) | <0.01 |
| Residual stiffness | 30 | 3 (10%) | – | 23 | 0 (0%) | – | 0.25 |
| Residual extensor lag | 30 | 4 (13%) | – | 23 | 0 (0%) | – | 0.12 |
| PRO follow-up (years) | 15 | – | 4.7 (2.5–7.9) | 6 | – | 5.3 (4.0–7.1) | 0.73 |
| Pedi-IKDC | 15 | – | 92 (84–99) | 6 | – | 98 (89–100) | 0.11 |
| Marx | 15 | – | 13 (12–16) | 6 | – | 14 (10–16) | 1.00 |
IQR: interquartile range; PRO: patient-reported outcome; Pedi-IKDC: Pediatric International Knee Documentation Committee.
Table 4.
Comparison of baseline characteristics and retrospectively collected clinical outcomes between those who responded to patient-reported outcome (PRO) surveys and those who did not.
| PROs obtained | PROs not obtained | p | |||||
|---|---|---|---|---|---|---|---|
| N | n (%N) | Median (IQR) | N | n (%N) | Median (IQR) | ||
| Baseline characteristics | |||||||
| Age at diagnosis | 21 | – | 13.2 (11.0–15.3) | 32 | – | 11.4 (9.7–13.3) | 0.22 |
| Sex (% male) | 21 | 14 (67%) | – | 32 | 21 (66%) | – | 1.00 |
| Mechanism of injury | 0.71 | ||||||
| Direct blow | 21 | 16 (76%) | – | 32 | 21 (66%) | – | |
| Jumping/landing | 21 | 3 (14%) | – | 32 | 7 (22%) | – | |
| Twisting | 21 | 2 (10%) | – | 32 | 4 (12%) | – | |
| Fracture pattern | 0.21 | ||||||
| Vertical | 21 | 3 (14%) | – | 32 | 1 (3%) | – | |
| Sleeve/pole | 21 | 8 (38%) | – | 32 | 20 (63%) | – | |
| Transverse | 21 | 5 (24%) | – | 32 | 4 (12%) | – | |
| Comminuted | 21 | 5 (24%) | 32 | 7 (22%) | |||
| Fracture displacement | 0.17 | ||||||
| Displaced | 21 | 14 (67%) | – | 32 | 15 (47%) | – | |
| Nondisplaced | 21 | 7 (33%) | 17 (53%) | ||||
| Effusion | 21 | 21 (100%) | – | 32 | 28 (88%) | – | 0.14 |
| Treatment | 0.10 | ||||||
| Operative | 21 | 15 (71%) | – | 32 | 15 (47%) | – | |
| Nonoperative | 21 | 6 (29%) | – | 32 | 17 (53%) | – | |
| Post-treatment outcomes and complications | |||||||
| Clinical follow-up (months) | 21 | – | 8 (4–24) | 32 | – | 5 (3–9) | 0.72 |
| Time to healing (months) | 21 | – | 2.2 (1.4–3.3) | 32 | – | 2.2 (1.7–3.6) | 0.51 |
| Return to sports (months) | 20 | – | 4.5 (2.8–6.4) | 30 | – | 3.7 (2.9–6.4) | 0.71 |
| Residual stiffness | 21 | 2 (10%) | – | 32 | 1 (3%) | – | 0.56 |
| Residual extensor lag | 21 | 1 (5%) | – | 32 | 3 (9%) | – | 1.00 |
PROs: patient-reported outcomes; IQR: interquartile range.
Operative technique and fixation construct were individualized based on fracture pattern and surgeons’ preference at the time of injury. Fixation techniques were characterized as open reduction internal fixation (ORIF) with K-wires, cerclage wires, screws, sutures, or hybrid constructs with several of the aforementioned. Nonoperative management consisted of casting in extension, bracing in extension, or a combination of both.
There were no cases of residual stiffness, extensor lag, or any other complication in the nonoperative group. In the operative group, the most common complication necessitating return to the operating room (OR) was symptomatic retained hardware, with 17/30 (57%) patients undergoing hardware removal. In addition, four operative patients (13%) sustained further complications requiring other procedures. One patient underwent revision ORIF 2 months after her initial surgery as she unfortunately sustained a re-fracture through her combined screw/K-wire construct after slipping on ice and falling directly onto her anterior knee. One patient experienced wound dehiscence, for which he was brought back to the OR for irrigation and debridement (I&D) and complex wound closure. He later underwent arthroscopic lateral release and open medial retinacular plication with vastus medialis obliquus (VMO) advancement 2 years following his patella ORIF due to residual pain and patellofemoral dysfunction. He had no further complications, and he was able to return to baseball (as a catcher), football, lacrosse, and golf. One patient underwent hardware repositioning and loose body removal 2 days following ORIF after a post-operative computed tomography (CT) scan revealed K-wires impinging on the chondral surface of the patella, as well as a loose body in the lateral gutter. One patient developed methicillin-resistant Staphylococcus aureus (MRSA) skin infection at the ankle of the operative leg that was theorized to seed the operative site, leading to osteomyelitis of the operative knee. He was treated with intravenous clindamycin and taken to the OR three times over the course of a 19-day admission: twice for I&D of the knee and ankle and once for flap reconstruction at the ankle by plastic surgery.
Ultimately, 90% of the operative cohort recovered with full range of motion documented at the time of final follow-up, but four patients (13%) healed with an extensor lag, three of which were mild (documented in clinic notes as 5 degrees). Of note, each of these patients had sustained a patellar sleeve fracture. The previously mentioned patient with osteomyelitis was documented to have a 20 degree extension lag, the ultimate treatment of which was unclear, as he was lost to follow-up approximately 2 months following the last described operative intervention.
Patient-reported functional outcomes were obtained for 21 (40%) patients: 15 operative (50% of operative cohort) and 6 nonoperative (26% of nonoperative cohort), and there were no baseline differences between the patients who responded to PRO surveys and those who did not (Table 4). The median time to outcome assessment was 4.8 years (3.5–7.6) post-surgery. Overall, PROs demonstrated good levels of knee function, with values consistent with normative age-based values for the Pedi-IKDC. 10 The only significant difference observed between any of the cohorts or sub-cohorts analyzed in this study was that of higher levels of activity reported by patients who had sustained a patellar sleeve/pole fracture (Table 2).
Discussion
Isolated fractures of the patella in the pediatric and adolescent population are rare, with the current literature consisting primarily of only several case reports11,12 and small case series.13,14 No studies to date have comprehensively analyzed features or outcomes of fractures treated operatively in comparison to those treated nonoperatively, nor have previous studies examined cohorts of different fracture patterns. This study was designed to provide a broad perspective on the gamut of patellar fractures sustained specifically within this age group, as well as the natural history following two distinct categories of treatment. While comparisons between the groups were made to provide perspective on the two cohorts, relative to each other, the cohorts were expectedly different, due to having different indications for the two treatment types. Therefore, this study was not designed to elucidate the possibility of a superior treatment for a given fracture, rather to assess potentially descriptive differences and explore the clinical course associated with different treatments for distinct types of patients.
When examining this study cohort based on fracture pattern, there were significant differences in age (p < 0.01), mechanism of injury (p < 0.01), removal of hardware (p = 0.04), and long-term activity levels based on Marx scores (p = 0.03). Patients treated for a patellar sleeve/pole fracture were approximately 4 years younger than those treated for other fracture patterns. This finding potentially speaks to the unique anatomic changes the patella undergoes in the pre-adolescent phase of skeletal development, which predispose the bone to this fracture pattern. 15 In addition, the patellar sleeve patients in this study presented with greater variety in their mechanisms of injury when compared to the patients sustaining fracture patterns, 92% of whom sustained their fracture following a direct blow to the knee. The observed age discrepancies, based on fracture pattern, are consistent with the small number of prior studies on the subject,5,11,12,14 and they coincide with the differences seen in mechanism of injury. These differences may also be a product of older, post-pubertal children being bigger, stronger, faster, and more likely to experience a high-energy traumatic blow to the knee through sports, recreational activity, or other lifestyle factors, such as sitting in the front seat of the car and predisposing themselves to a dashboard injury. Caregivers of pediatric and adolescent age groups should be aware of this array of differences to avoid minimizing patellar or infrapatellar knee pain, or misdiagnosing the etiology, in a pre-adolescent child who may not necessarily have sustained a high-energy mechanism of injury, as delayed presentation and treatment of patellar sleeve fractures may result in notably worse outcomes. 13 Indeed, two patients with sleeve fractures from this study had delayed diagnoses (>1 week from injury) due to their injuries being missed on initial X-rays. However, neither sustained any persistent complications from their injury. Furthermore, patients with patellar sleeve/pole fractures demonstrated a significantly lower rate of hardware removal and still went on to participate in higher levels of activity.
When examining this study’s cohorts of operatively treated versus nonoperatively treated patients (Table 3), the observed discrepancies in time to healing, time to return-to-sport, and total follow-up time are, in all likelihood, attributable to the inherent differences in management of displaced fractures with ORIF, compared to management of nondisplaced fractures with conservative measures. The significant difference in fracture displacement follows the current standard of care, with 97% of operatively treated patients having fractures with >2 mm of displacement and no cases of fractures with that much displacement in the nonoperative group. The significant differences in age, fracture pattern, and radiographic effusion between operatively and nonoperatively treated patients are due to those who sustained comminuted fractures, as each of these relationships becomes nonsignificant when controlling for the comminuted fracture pattern.
Four patients were found to have an extensor lag at final follow-up. While one patient had a 20 degree extension lag, the associated factor of patellar osteomyelitis likely represents a confounder to any clinically meaningful takeaways regarding risk factors for this complication, other than the finding of being more likely in patellar sleeve fractures. In addition, because the other three patients exhibited extensor lags of 5 degrees or less, such lags may be minor, should they arise. However, the presence of such a phenomenon in multiple patients with the same fracture pattern should prompt awareness from caregivers, both in the technical performance of surgery for patellar sleeve fractures, in terms of optimizing the reduction in full extension, and in the rehabilitative phase, in terms of optimizing quad strengthening at the appropriate time.
Perhaps the most noteworthy of the current findings was that of no statistically significant difference in post-operative functional outcome measures, regardless of treatment method (Table 3). In addition, the outcomes in our cohort are encouraging when compared to the established population normative values for both the Pedi-IKDC and the Marx score. Nasreddine et al. 10 reported the population median Pedi-IKDC score as 94.6, as well as the median (interquartile range) score for those with prior knee surgery as 70.7 (55.4–89.1). In all groups analyzed in our study, the median Pedi-IKDC score was greater than 90. While investigating the reliability of the Marx scale in pediatric patients, Shirazi et al. 9 found a mean score of 13.71 (standard deviation (SD) = 3.7) in 62 patients (mean age = 14.6 years) presenting to their clinic with a knee injury. The lowest median Marx score found in our study was 12, which was reported in the group of patients who sustained comminuted, transverse, or vertical fractures (Table 2). All other groups had median scores of 13 or greater. Nevertheless, there were significantly higher levels of activity reported by the patients who had sustained sleeve/pole fractures when compared to other fracture patterns based on Marx scores (Table 2). However, because the mean time of PRO completion was nearly 5 years post-injury, relatively minor differences in Marx score may be reflective of a decreased activity level in later adolescent or young adult respondents. While these long-term functional outcomes are encouraging, it should nevertheless be highlighted that 57% of operative patients required a second surgery for hardware removal, and 4 (13%) of the operative patients required unplanned returns to the OR for additional procedures, including two revision ORIF cases. Furthermore, patients sustaining a comminuted, transverse, or vertical fracture were significantly more likely to undergo removal of hardware (p = 0.04). In several adult studies, the rates of reoperation for symptomatic hardware removal have been cited as 18%–52%.16 –18 The higher instance of hardware removal in this study is likely due to the small number of patients as well as kids having increased activity levels, predisposing the patellar fixation constructs to be more symptomatic. In addition, due to their much more robust healing ability and minimal medical comorbidities, pediatric orthopedic surgeons may have a much lower threshold for removing patella hardware than orthopedic trauma surgeons do for an adult population. The rates of infection (3%) and fixation failure (6%) in our cohort are similar to those reported in the adult literature.16,18
In contrast to the reassuring functional outcome data seen in our cohort, several recent studies have shown that outcomes in adults following surgically treated patella fractures are not as favorable. For example, in a study with a similar design to the current one, Lazaro et al. 19 reviewed prospectively collected data from 30 adults (mean age = 60.2 years) who underwent ORIF for an isolated unilateral patella fracture. At final follow-up, patients continued to exhibit functional impairment, with a mean Activities of Daily Living Scale of the Knee Outcome Survey (ADLS-KOS) score of 75/100, a mean Lower Extremity Functional Scale (LEFS) score of 70/100, and 80% of patients reporting anterior knee pain during activities of daily living. In another study, Lebrun et al. 20 enrolled 40 patients (mean age = 46 years at time of surgery) who underwent surgery for an isolated, unilateral patella fracture in a prospective case series. At a median follow-up time of 6.5 years, the physical component score of the SF-36 and all Knee Injury and Osteoarthritis Outcome Score (KOOS) components were significantly lower than established population normative values. Thus, despite the greater activity level of the young population in this study, similar fracture patterns to those sustained in adults appear to be better tolerated in pediatric and adolescent patients, with greater likelihood of return to baseline or normal knee function.
This study is subject to the limitations and biases inherent to any retrospective investigation with a relatively small overall sample size, despite being larger in size than previous efforts on the same topic. The smaller group of patients precluded robust sub-stratified statistical analyses and conclusions, specifically regarding the functional outcome questionnaire data. While the survey response rate from our operative cohort may be acceptable for a retrospective study investigating a geographically mobile and unstable trauma population, the response rate from the nonoperative cohort was nearly half that of the operative cohort, and our overall response rate was 40% (21/53 patients). In addition, evaluation of physical exam endpoints of this study, most notably extensor lag, may be limited by instances of shorter clinical follow-up. Future comparative investigations with larger numbers of patients as well as more effective systems in place to improve the follow-up of pediatric acute trauma patients are necessary to further support these results.
Conclusion
Based on the current retrospective analysis of 53 pediatric patients treated for isolated, unilateral patella fractures with associated PROs, children and adolescents achieve good function and high activity level in the years following treatment, both of which are similar to that of the normal population. However, surgically treated patients, who are treated for displaced fractures, expectedly take longer to achieve radiographic union and to return to sports than nondisplaced fractures treated nonoperatively. More than half (57%) of operative patients required implant removal surgery, with some risk for additional procedures in all fracture types and a persistent minor extensor lag in approximately 10% of patients with patellar sleeve fractures. Such information is helpful in allowing pediatric providers to have better informed discussions with patients and families regarding diagnosis, treatment, and outcomes of these injuries.
Supplemental Material
Supplemental material, sj-docx-1-cho-10.1177_18632521241232301 for Outcomes of treatment of patella fractures in children and adolescents by Evan W. Beatty, Mathilde Hupin, Dennis E. Kramer, Benjamin J. Shore and Benton E. Heyworth in Journal of Children’s Orthopaedics
Supplemental material, sj-pdf-2-cho-10.1177_18632521241232301 for Outcomes of treatment of patella fractures in children and adolescents by Evan W. Beatty, Mathilde Hupin, Dennis E. Kramer, Benjamin J. Shore and Benton E. Heyworth in Journal of Children’s Orthopaedics
Acknowledgments
The authors acknowledge Patricia Miller, MS, Michael Kozanek, MD, PhD, and Kyna Donohue, MD
Footnotes
Author contributions: E.B. contributed to study design, data collection, data analysis, and manuscript preparation. M.H. contributed to study design, data collection, and data analysis. D.K. contributed to surgical treatment of patients included in study and study design. B.S. contributed to surgical treatment of patients included in study and study design. B.H. contributed to surgical treatment of patients included in study, study design, data analysis, and manuscript preparation.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Benton E. Heyworth has the following disclosures:
- Consultant and stock options owner of Imagen Technologies, Inc.
- Educational Consultant and received educational fees (2019) from Arthrex, Inc. and Kairos Surgical, Inc.
- Member of the Research in OsteoChonditis of the Knee (ROCK) Study Group, which has received unrestricted educational grant funding from Allosource, Inc. and Vericel, Inc.
- Receives Royalties (textbook-related) from Springer Science & Business Media.
Ethical approval: This study received ethical approval from the Boston Children’s Hospital Institutional Review Board (IRB) (IRB-AR00009805-10) on 30 September 2014. This is an IRB-approved retrospective study; all patient information was de-identified and patient consent was not required.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental material: Supplemental material for this article is available online.
References
- 1. Melvin JS, Mehta S. Patellar fractures in adults. J Am Acad Orthop Surg 2011; 19(4): 198–207. [DOI] [PubMed] [Google Scholar]
- 2. Gage BE, McIlvain NM, Collins CL, et al. Epidemiology of 6.6 million knee injuries presenting to United States emergency departments from 1999 through 2008. Acad Emerg Med 2012; 19(4): 378–385. [DOI] [PubMed] [Google Scholar]
- 3. Thompson JC. Leg/knee. In: Thompson JC. (ed.) Netter’s concise orthopedic anatomy. 2nd ed. Philadelphia, PA: Elsevier, 2010, pp. 285–336. [Google Scholar]
- 4. Sayum Filho J, Lenza M, Tamaoki MJ, et al. Interventions for treating fractures of the patella in adults. Cochrane Database Syst Rev 2021; 2: CD009651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Maguire JK, Canale ST. Fractures of the patella in children and adolescents. J Pediatr Orthop 1993; 13(5): 567–571. [PubMed] [Google Scholar]
- 6. Braun W, Wiedemann M, Rüter A, et al. Indications and results of nonoperative treatment of patellar fractures. Clin Orthop Relat Res 1993; 289: 197–201. [PubMed] [Google Scholar]
- 7. Kocher MS, Smith JT, Iversen MD, et al. Reliability, validity, and responsiveness of a modified International Knee Documentation Committee Subjective Knee Form (Pedi-IKDC) in children with knee disorders. Am J Sports Med 2011; 39(5): 933–939. [DOI] [PubMed] [Google Scholar]
- 8. Marx RG, Stump TJ, Jones EC, et al. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med 2001; 29(2): 213–218. [DOI] [PubMed] [Google Scholar]
- 9. Shirazi CP, Israel HA, Kaar SG. Is the Marx activity scale reliable in patients younger than 18 years? Sports Health 2016; 8(2): 145–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nasreddine AY, Connell PL, Kalish LA, et al. The Pediatric International Knee Documentation Committee (Pedi-IKDC) subjective knee evaluation form: normative data. Am J Sports Med 2017; 45(3): 527–534. [DOI] [PubMed] [Google Scholar]
- 11. Siddiqui R, Singh A, Cullinan C. Superior pole sleeve fracture of the patella in an adolescent: a case report. JBJS Case Connect 2020; 10(3): e2000007. [DOI] [PubMed] [Google Scholar]
- 12. Boushnak MO, Moussa MK, Abed Ali AA, et al. Patellar sleeve fracture in an eight-year-old girl. Cureus 2020; 12(9): e10345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sousa PL, Stuart MJ, Prince MR, et al. Nonoperative management of minimally displaced patellar sleeve fractures. J Knee Surg 2021; 34(3): 242–246. [DOI] [PubMed] [Google Scholar]
- 14. Gao GX, Mahadev A, Lee EH. Sleeve fracture of the patella in children. J Orthop Surg 2008; 16(1): 43–46. [DOI] [PubMed] [Google Scholar]
- 15. Pennock AT, Bomar JD, Manning JD. The creation and validation of a knee bone age atlas utilizing MRI. J Bone Joint Surg Am 2018; 100(4): e20. [DOI] [PubMed] [Google Scholar]
- 16. Petrie J, Sassoon A, and Langford J. Complications of patellar fracture repair: treatment and results. J Knee Surg 2013; 26(5): 309–312. [DOI] [PubMed] [Google Scholar]
- 17. Kadar A, Sherman H, Glazer Y, et al. Predictors for nonunion, reoperation and infection after surgical fixation of patellar fracture. J Orthop Sci 2015; 20(1): 168–173. [DOI] [PubMed] [Google Scholar]
- 18. Dy CJ, Little MT, Berkes MB, et al. Meta-analysis of re-operation, nonunion, and infection after open reduction and internal fixation of patella fractures. J Trauma Acute Care Surg 2012; 73(4): 928–932. [DOI] [PubMed] [Google Scholar]
- 19. Lazaro LE, Wellman DS, Sauro G, et al. Outcomes after operative fixation of complete articular patellar fractures: assessment of functional impairment. J Bone Joint Surg Am 2013; 95-A(14): e96. [DOI] [PubMed] [Google Scholar]
- 20. LeBrun CT, Langford JR, Sagi HC. Functional outcomes after operatively treated patella fractures. J Orthop Trauma 2012; 26(7): 422–426. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-cho-10.1177_18632521241232301 for Outcomes of treatment of patella fractures in children and adolescents by Evan W. Beatty, Mathilde Hupin, Dennis E. Kramer, Benjamin J. Shore and Benton E. Heyworth in Journal of Children’s Orthopaedics
Supplemental material, sj-pdf-2-cho-10.1177_18632521241232301 for Outcomes of treatment of patella fractures in children and adolescents by Evan W. Beatty, Mathilde Hupin, Dennis E. Kramer, Benjamin J. Shore and Benton E. Heyworth in Journal of Children’s Orthopaedics