Abstract
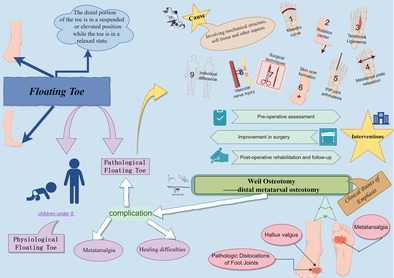
The floating toe deformity is classified as a forefoot deformity wherein the distal portion of the toe does not establish touch with the ground, resulting in a suspended or elevated position while the finger is in a relaxed state. At first, it garnered considerable interest as a complication It is worth noting that this condition is particularly common in children under the age of 8, which usually disappears as the individual reaches maturity. Studies have shown that with the aggravation of floating toe deformity, its adverse effects on patients' gait and overall quality of life also increase. Despite the prevalence of floating toe deformity in clinical settings, there is a lack of comprehensive literature investigating its underlying causes and potential preventive strategies. This scope review follows the preferred reporting items for systematic reviews and meta‐analyses extension for scoping reviews (PRISMA‐ScR) statement guidelines for scope reviews. The literature was obtained from various full‐text databases, including China National Knowledge Infrastructure Database (CNKI), Wanfang Database, PubMed, and Web of Science Database. Our search focused on published literature related to floating toes, Weil osteotomy, and distal metatarsal osteotomy, up until March 1, 2023. The literature search and data analysis are conducted by two independent reviewers. If there are any disagreements, a third researcher will participate in the discussion and negotiate a decision. Furthermore, two experienced foot and ankle surgeons conducted a thorough literature analysis for this review. Sixty‐two articles were included. Through the clinical analysis of the structural changes of the forefoot before and after operation, the classification of floating toe was described, the causes of pathological floating toe were summarized, and the possible intervention measures for the disease were put forward under the advice of foot and ankle surgery experts. We comprehensively summarize the current knowledge system about the etiology of floating toe and put forward the corresponding intervention strategy. We recommend that future studies will focus on the improvement of surgical procedures, such as the combination of Weil osteotomy, proximal interphalangeal (PIP) arthrodesis and flexor tendon arthrodesis.
Keywords: Floating toe, Distal metatarsal osteotomy, Interventions, Surgical complications, Weil osteotomy
The image is drawn by Figdraw software.
Introduction
The condition known as a floating toe is characterized by the inability of the toe's end to maintain contact with the ground in a relaxed state. This results in the toe hovering or floating in the air, leading to an inability to bear pressure, maintain balance, and potentially interfering with normal walking and daily activities. 1 , 2 Numerous research have provided empirical evidence supporting the categorization of floating toes into normal and pathological subtypes. The occurrence of physiological floating toes is prevalent during childhood and tends to diminish progressively as the individual undergoes growth and maturation. The occurrence of pathological floating toes is frequently observed as a prevalent complication of Weil osteotomy, with an incidence rate ranging from 15% to 68% according to various studies 3 , 4 , 5 , 6 , 7 , 8 The Weil osteotomy, a commonly employed surgical technique for addressing forefoot pain and deformity, is a component of the distal metatarsal osteotomy. 9 The technique was initially created in 1985 by American surgeon Lowell Weil for the treatment of patients with central metatarsals, specifically the second through fourth metatarsals. Following its introduction, the technique gained popularity in Europe. 10 In contrast to proximal osteotomies, the Weil osteotomy presents several advantages including a reduced incision size, enhanced stability of the osteotomy plane, and a greater likelihood of accelerated healing. 9 , 11 Nevertheless, these advantages are accompanied by distinct complexities. The prevailing issues usually cited in contemporary clinical practice encompass floating toe, metatarsalgia, and healing difficulties, 8 with floating toe being the most predominant.
Despite the prevalence of floating toes, there is a scarcity of literature that precisely investigates the underlying causes of this condition. 12 , 13 This phenomenon can be attributed to the fact that the Weil osteotomy offers significant benefits in terms of long‐lasting alleviation of metatarsalgia and bunion symptoms, 4 , 14 , 15 and alternative surgical techniques with superior outcomes have not yet been suggested. In addition, it has been observed that the presence of floating toe deformity (FTD) does not have a substantial impact on patient satisfaction or functional outcomes subsequent to undergoing Weil osteotomy, as indicated by the findings of Wagner et al. 8 Nevertheless, the development of a floating toe is a persistent phenomenon, and its effects on an individual's ability to walk and overall quality of life become increasingly noticeable as the condition progresses in severity. Hence, it is imperative to conduct a thorough examination of the potential factors contributing to the occurrence of floating toes, as this investigation may afterwards facilitate advancements in the field of Weil osteotomy. The objective of this article is to provide a concise overview of the potential factors contributing to the occurrence of floating toes in the current stage. Additionally, it seeks to derive insights for implementing interventions that might mitigate the risk of such incidents. Furthermore, the study wants to investigate novel avenues for the advancement of forefoot surgery in the future.
Methods
The Scoping Review Principle
The reporting of this study conforms to the preferred reporting items for systematic reviews and meta‐analyses (PRISMA) statement for scoping review standards or the preferred reporting items for systematic reviews and meta‐analyses extension for scoping reviews (PRISMA‐ScR).
Purpose Statement of the Scoping Review
The purpose of this scope review is to synthesize the possible pathogenesis of FTD supported by existing evidence, and to determine effective intervention measures based on clinical experience and expert opinions to reduce the risk of toe floating. Ultimately, it will explore potential future directions to contribute to the development of forefoot surgery.
Systematic Search Strategy
Identification
The main electronic databases used for evidence retrieval are China National Knowledge Infrastructure Database (CNKI), Wanfang Database, PubMed, and Web of Science Database. Our search strategy is “floating toe,”, “Weil osteotomy,”, “distal metatarsal osteotomy” and their synonyms. We set the restriction of language to be in English or Chinese, searching for literature from the databases until March 1, 2023, and tracing relevant references.
Literature Screening and Data Analysis
Two literature evaluators strictly followed the operation process, independently searching for citation information such as titles and abstracts based on the proposed inclusion and exclusion criteria, conducting preliminary selection, then including qualified literature, reading the entire text in sequence, gradually eliminating articles that did not meet the standards, and cross checking the results. If there was disagreement, a third researcher participated in the discussion and negotiated a decision.
Selection Criteria and Quality Assessment
Any study, both primary and secondary, which examined search strategy was eligible. We included theoretical/clinical studies. Non‐English studies or non‐Chinese studies, studies which lacked sufficient detail for data extraction, protocols, and studies which only referenced but did not describe the subject in detail, were all excluded.
No quality assessment was undertaken for this scoping review as the aim was to summarize existing evidence on the topic to inform future research direction, not to include or exclude studies based on quality.
Results Synthesis
Two experienced foot and ankle surgeons conducted a comprehensive literature analysis on the selected articles and ultimately obtained results on the possible causes and intervention measures of floating toes.
Results
After cross‐screening by three researchers, 60 articles were finally included, while two ankle surgeons included two articles based on specific experience, giving a total of 62 articles. The specific process is shown in the literature screening flow chart (Figure 1). Two ankle surgeons summarized and analyzed the structural changes of the forefoot, described the classification of floating toes, summarized the causes of pathological floating toes, and proposed possible intervention measures.
FIGURE 1.
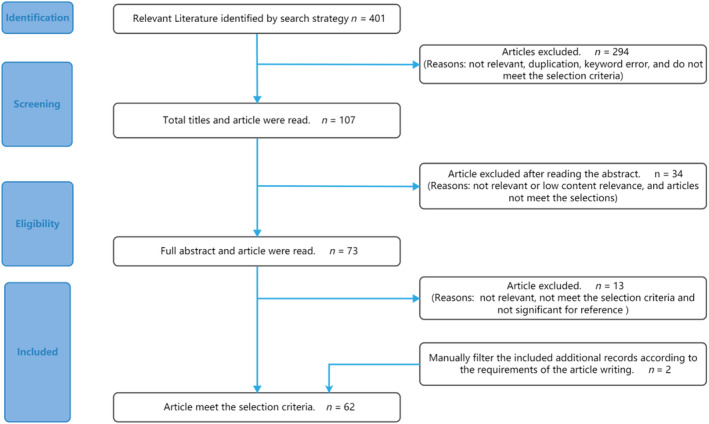
Literature screening flow chart.
Clinical Points of Emphasis
According to a comprehensive analysis of numerous case series documented in the medical literature, it has been established that the customary approach for conducting a Weil osteotomy involves following a certain protocol as outlined by Coughlin in 1997. 16 A longitudinal incision measuring 3–4 mm is performed, extending from the dorsal distal one‐third of the metatarsal to the base of the proximal phalangeal bone. The metatarsophalangeal (MTP) joint capsule is surgically opened while the toe is flexed, followed by an incision of a section of the lateral collateral ligament, and finally, the proximal phalange is moved into a plantar flexion position. The proximal phalanx can be incised to fully expose the metatarsal head. An oblique osteotomy is performed starting from a point 2 mm below the most dorsal part of the articular surface of the metatarsal head. The osteotomy extends from the intra‐articular region to the proximal end, following the direction of the plantar weight‐bearing plane. Typically, this plane is inclined at an angle of approximately 25° to the metatarsal trunk. The proximal end of the osteotomy is usually positioned at the junction between the distal and middle thirds of the metatarsal trunk, specifically at the junction of the metatarsal trunk and the metaphysis. After the completion of the osteotomy procedure, the metatarsal head is displaced proximally, typically resulting in a reduction of 3–5 mm in length. This is done concurrently with the correction of any varus or valgus deformities, in order to establish proper alignment of the foot. Subsequently, the foot is immobilized to maintain its correct position.
This procedure has the potential to induce various changes in the mechanics of the bones. Specifically, it may result in the loss of the original “Maestro parabolic” structure. 17 Additionally, it can lead to alterations in the rotation axis of the MTP joint, causing a downward shift in the rotation center of the joint. 18 Furthermore, the procedure may contribute to joint fibrosis and stiffness due to the opening of the joint capsule. 9 Other effects include laxity of the plantar plate and shortening of the metatarsal bones, which can result in relative lengthening of the flexor tendon, extensor tendon, and ligaments. Moreover, it can lead to reduced tension in the foot aponeurosis and weakened functioning of the windlass mechanism. 7 , 9 , 19 Scar contracture during the recovery process has the potential to cause dorsal pulling of the proximal phalange. 20 Lastly, it is important to note that surgery carries the risk of damaging peripheral nerves and blood vessels.
The Cause of Pathological Floating Toe
Changes in the Mechanical Structure of the Foot Bone
The Weil osteotomy is a frequently employed surgical procedure aimed at addressing forefoot abnormalities, including hallux valgus and associated pain. Nevertheless, it induces alterations in both the location and orientation of the affected metatarsal bones, particularly the first and second metatarsals, hence perturbing the initial “Maestro parabola.” Valley and Reese 21 were among the first researchers to recognize and address the issue at hand. They authored the “Guidelines for reconstructing the metatarsal parabola through the utilization of the shortening osteotomy” technique. This publication has been instrumental in equipping medical professionals with valuable insights to effectively mitigate the numerous complications arising from excessive osteotomy, which can result in the disruption of the parabolic structure. In the year 2003, Maestro et al. 22 conducted a study aimed at standardizing the optimal physiological curve. This involved extensive data measurements and the formulation of a specific specification about the number of surgical osteotomies permissible without disrupting the aforementioned physiological curve. The axis of the second metatarsal traverses the midpoint of the hind foot, whereas the SM4 (is defined as a perpendicular line drawn through the center of the lateral sesamoid bone, perpendicular to the second metatarsal bone.). This line passed through the central part of the fourth metatarsal head in many cases and was termed the SM4 axis. The line is positioned somewhat towards the middle third of the fourth metatarsal, closer to its distal end. Additionally, the first metatarsal exhibits a reduction in length of no more than 10 mm compared to the second metatarsal. The average difference between M2 (second metatarsal length) and M3 (third metatarsal length) is 3.37 mm with a standard deviation of 0.96 mm. Similarly, the average difference between M3 and M4 (fourth metatarsal length) is 6.54 mm with a standard deviation of 1.03 mm, while the average difference between M4 and M5 (fifth metatarsal length) is 12 mm with a standard deviation of 1.91 mm. The relative disparity in length among these four metatarsals can be conceptualized as an isometric series with a constant ratio of 2 (M2‐M3: M3‐M4: M4‐M5 = 3:6:12 or 3.5:7:14) (Figure 2). In a study conducted by Stoupine and Singh 23 at the Barry University School of Podiatric Medicine, it was reaffirmed that focusing on the “Maestro parabola” during osteotomy can effectively mitigate the occurrence of post‐operative complications, specifically floating toe, transfer metatarsalgia, and foot back skin ulcer. This conclusion was reached after an extensive examination of male and female cadavers.
FIGURE 2.
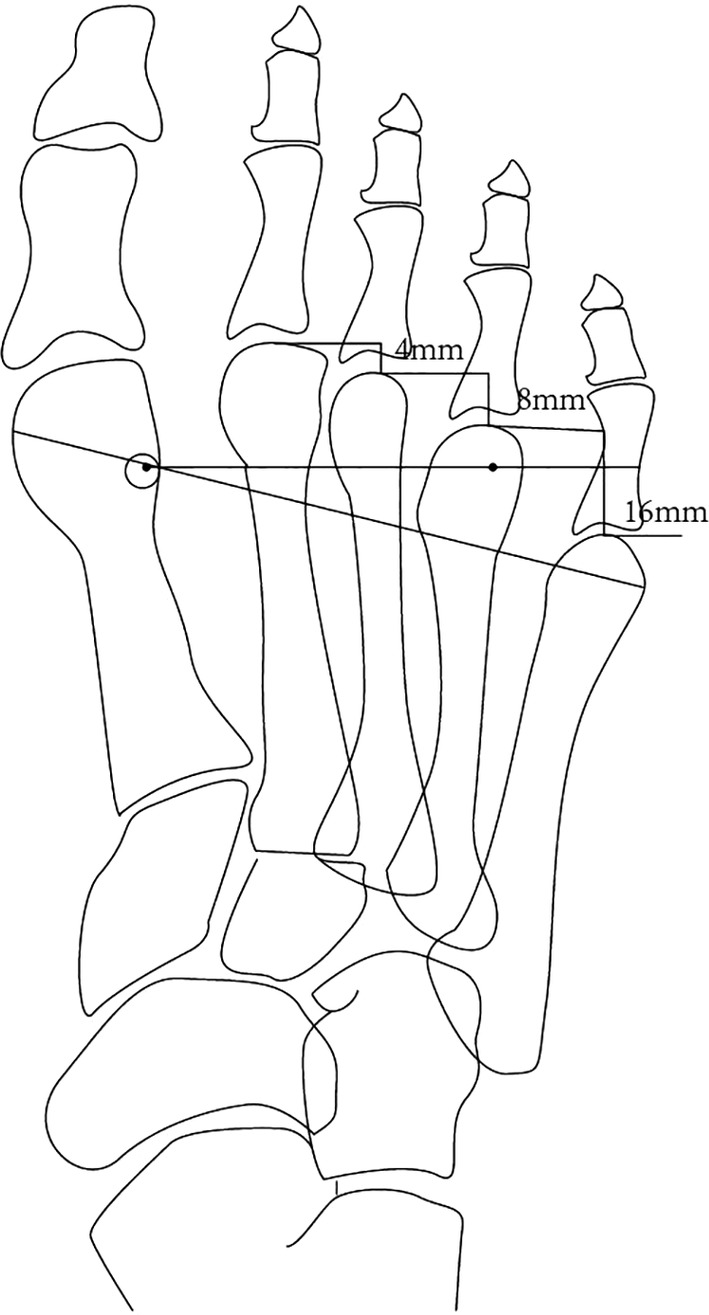
Architectural marks 22 : Pictures for relative differences in four metatarsal lengths that can be conceptualized as an isometric sequence with a constant ratio of 2.
Rotation Center of the MTP Joint Shifted Down
According to Godoy‐Santos et al. 24 the Weil osteotomy is considered the principal surgical intervention for the treatment of floating toes. There is a general consensus among foot and ankle surgeons that the downward displacement of the rotation center of the MTP joint, which occurs during surgery, plays a crucial role in the pathogenesis of floating toes. Bougiouklis and colleagues expand upon the research conducted by Grimes and Coughlin 25 to conduct a comprehensive analysis of the alterations in the center of rotation of the MTP joint following the Weil osteotomy. The findings of the study conducted by Bougiouklis et al. 26 revealed that, following the Weil osteotomy, the rotation center of the MTP joint exhibited a proximal and plantar shift with an average magnitude of 3.5 ± 1.64 mm, as compared to the control group (Figure 3). All of Bougiouklis et al.'s subjects were individuals diagnosed with floating toe. It is postulated that during surgery, the rotation center of the MTP joint is displaced in a downward direction, thereby inducing a collapse of the foot arch. This collapse subsequently causes the proximal phalangeal bone to elevate upwards due to the levering effect, ultimately culminating in the manifestation of a floating toe. In a state of static equilibrium, the toe lacks the capacity to independently bear the body's weight, leading to a concentration of pressure on the grounded portion of the foot. Consequently, this gives rise to an unsteady gait, challenges in maintaining balance, and the occurrence of joint friction accompanied by pain. In instances of heightened severity, this can result in notable problems, including but not limited to arthritis, joint inflammation, and skeletal malformation.
FIGURE 3.
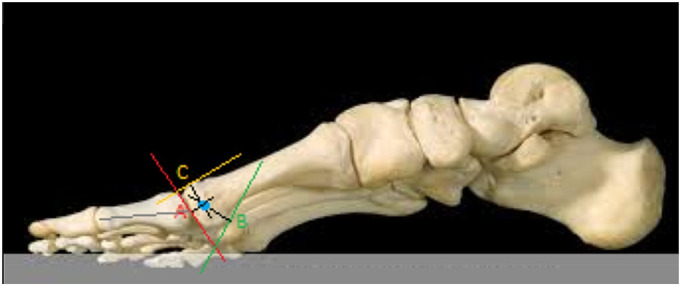
Rotation center of the metatarsophalangeal joint shifted down:26 the determination of the center of rotation of themetatarsophalangeal joint was achieved through the use of three points on the metatarsal head. Point A is the central point of the articular surface of the metatarsal head, in the same straight line as the longitudinal axis of the proximal phalanx. Point B corresponded to the lower (plantar) and more proximal edge of the head before its transition to the plantar surface of the neck. Point C is the dorsal highest point of the metatarsal head.
Relative Lengthening of Tendons, Ligaments
Previous research has indicated that following the Weil osteotomy procedure, there are alterations in the positioning of the ligaments and tendons (specifically, the flexor tendon and extensor tendon) in the foot. These changes occur as a result of the metatarsal head being translated proximally, the metatarsals undergoing shortening and elevation, and the surrounding soft tissues being disrupted. 12 , 27 , 28 Nevertheless, inadequate attention was given to the treatment of ligaments and tendons during the surgical procedure, resulting in a lack of tension in these structures (Figure 4). This particularly affected the flexor tendon, impeding its ability to fulfill its usual function of exerting pulling force. Consequently, the MTP joint, responsible for plantarflexion movements, is unable to execute its regular range of motion and may potentially exhibit a condition known as a floating toe. The flexor tendon has the potential to undergo displacement towards the dorsal side of the MTP joint, assuming the role of the extensor tendon. This displacement results in the upward pulling of the toe, hence contributing to an increased degree of the floating toe. Furthermore, the alteration in the positioning of the tendon of the interosseous muscle around the rotational center of the MTP joint is also a crucial factor in the development of floating toes. 12 The significance of this feature becomes particularly notable when the reduction in length of the metatarsals surpasses 3 mm, as indicated by Migues et al. 4
FIGURE 4.
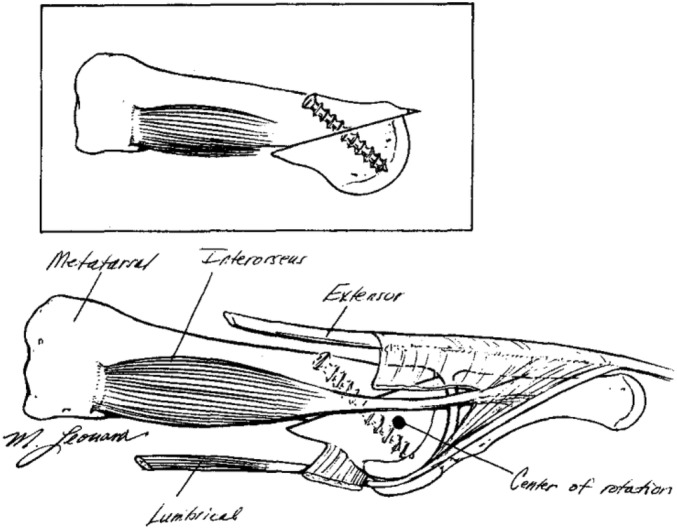
Weil osteotomy anatomic positions. The shortening of the metatarsal bone causes a relative lengthening of the tendon and ligaments. 12
Metatarsal Plate Relaxation, Change in the Windlass Mechanism
Many scholars have proposed that the pathophysiological cause for the occurrence of the floating toe may be attributed to the failure of the plantar structure, specifically the flexor muscle, in addition to the elongation of tendons and ligaments. There exists a suggestion that the occurrence of floating toes is a consequence of the reduction in plantar flexion resulting from metatarsal shortening. This reduction in plantar flexion subsequently leads to a decrease in tension within the plantar aponeurosis, hence causing relaxation of the metatarsal plate and impairing the windlass mechanism. In typical circumstances, the tension produced in the metatarsal plate and the MTP joint during toe elevation facilitates a stable hinge‐like movement. The atypical relaxation of the flexor muscles might potentially result in the prolonged partial dislocation of the metatarsal joint or heightened pressure underneath the metatarsal head. Consequently, this can lead to an augmented looseness of the metatarsal plate and a weakening of the windlass mechanism. Simultaneously, the dorsal extensor tendons maintain their normal tension, thereby leading to a higher occurrence of floating toes. In an effort to tackle this issue, Perez et al. 13 undertook cadaveric tests with the aim of reducing the length of the metatarsal plates. The findings of the study indicated a notable correction of the condition known as floating toe, hence reinforcing the significance of the windlass mechanism in the progression, rectification, and prevention of floating toes. In their study, Weil et al. 29 provided evidence that the occurrence of floating toe was not observed when the potentially loose plantar plate was advanced by the dorsal approach following the Weil osteotomy in patients experiencing post‐operative MTP joint instability. A study conducted by Dohle and Marques 30 examined the application of a dorsal transarticular technique for the reconstruction of the metatarsal plate. Nevertheless, because to the scarcity of such articles and the lack of complete alignment between cadaveric investigations and clinical research, the mechanism in question has not yet been widely acknowledged as a definitive cause, and the precise mechanism continues to be a subject of ongoing discussion.
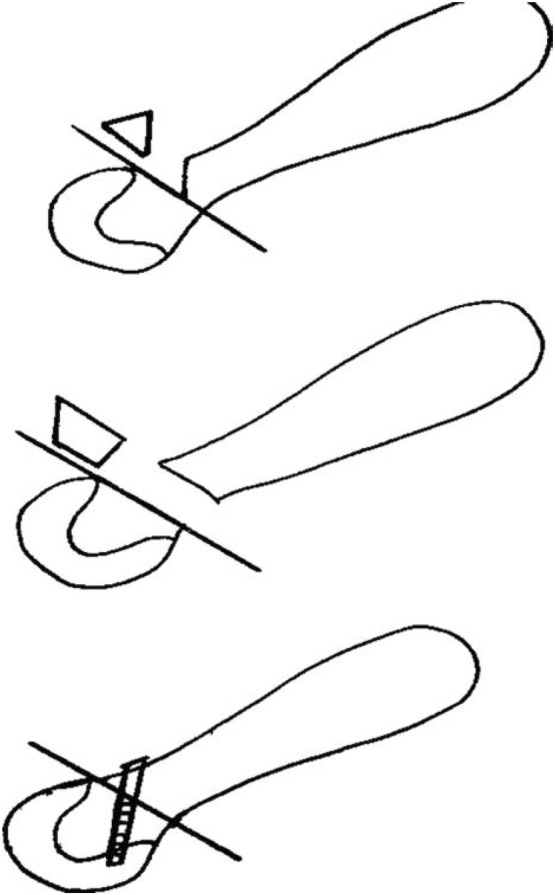
Proximal Interphalangeal (PIP) Joint Arthrodesis
Weil osteotomy indications are often accompanied by hammer and claw toe deformities that require simultaneous surgical correction. The main surgical options for fixing these deformities are PIP joint arthrodesis (Figure 5) and arthroplasty. It has been documented that PIP joint fusion (PIP joint arthrodesis) is significantly associated with an increased incidence of floating toes. 4 Lee et al. 19 suggested that the flexor digitorum brevis tendon (FDB) could be transferred into the PIP joint while maintaining tension, which could indirectly restore the windlass mechanism by generating flexion forces at the MTP joint. The normal windlass mechanism can help prevent the formation of a floating toe, as demonstrated in cadavers. This requires a flexor tenodesis procedure in conjunction with a PIP joint fusion (PIP joint arthrodesis) to prevent the development of a floating toe. Cook et al. 31 also demonstrated that by applying anatomical reconstruction techniques, rebalancing techniques (e.g., capsulotomy and cellulolysis) can significantly improve the occurrence of floating toe complications after Weil osteotomy. Anatomical reconstruction techniques are now being used to reduce the incidence of floating toes. Anatomical reconstruction techniques have been used to reduce the incidence of floating toes. This is certainly good news in that it addresses the risk factors and utilizes them to help reduce the incidence of floating toes in reverse. With further clinical trial studies to evaluate the clinical possibilities of this method and improve it, it may become an actual intervention to reduce the pain caused to patients by secondary surgery in the form of a combination or new procedure.
FIGURE 5.

Proximal interphalangeal (PIP) joint arthrodesis of Toe 2.
Skin Scar Formation
The expected scar formation after the surgical skin incision is also a consideration that should be considered. Current osteotomies generally use a dorsal approach, which allows visualization of the MTP joint and the intact metatarsal bone, facilitating the surgical procedure. The post‐operative scar is not located on the plantar aspect of the foot, facilitating simultaneous post‐operative wound healing and recovery training. This is an improvement on the disadvantages of the previous procedure. However, the location of the dorsal skin incision over the MTP joint may lead to contracture and further increase the probability of floating toes and the degree of elevation. 23
Surgical Techniques
In practical situations, it is difficult to perform an osteotomy parallel to the weight‐bearing surface. 12 , 32 The surgeon must be experienced and skilled in measuring the length and angle of the bones in the foot to determine the amount and position of the bone to be removed according to the patient's particular situation. If too much is removed surgically or the position or angle is incorrect, this may result in severe changes to the foot's mechanics.
Vascular Nerve Injury
Neurological system problems can also lead to the development of floating toes. Neurogenic floating toe is caused by neurological conditions such as cerebral palsy, amyotrophic lateral sclerosis, and multiple sclerosis that result in damage to the motor nerves, causing the toes to curl upwards uncontrollably. The nerves are responsible for sensory and motor control, 33 while the blood vessels are responsible for motor and metabolic support. 34 , 35 , 36 Damage to the blood vessels and nerves during surgery may affect the foot's health and lead to the formation of a floating toe.
Individual Differences and Activity Restrictions
Several studies have confirmed that. 37 , 38 , 39 hallux valgus, one of the best indications for Weil osteotomy, is a condition that has a clear familial tendency to be more common in women than men and is highly susceptible to environmental influences. After a Weil osteotomy, the toe's range of motion is limited for some time; this can lead to a lack of plantar flexion of the toes, preventing the end of the toes from touching the ground. This may result in inadequate plantarflexion of the toe, which may prevent the end of the toe from touching the ground. Also, uncomfortable shoes (e.g., high heels) and improper walking posture may force the proximal phalange into a prolonged dorsiflexion position, increasing the incidence of floating toes.
Physiological Floating Toe
Physiological floating toe occurs when a child walks or stands with one or two toes slightly raised or curved as the weight shifts. This phenomenon is usually harmless, does not require treatment, and will disappear as the child grows and develops. 40 In recent years, the Faculty of Medicine, University of Yamanashi, Chuo‐shi, Yamanashi, Japan; The Faculty of Rehabilitation, Kobe International University, Japan; the Graduate School of Medicine, Kyoto University, Japan; Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Japan Medical and Dental University, Japan, conducted a study on factors associated with floating toes in preschool children up to the age of 8 years. 40 , 41 , 42 , 43 Wako and her team 40 , 41 , 44 concluded that physiological floating toes in children are often caused by:
Underdeveloped nervous system: the immature development of the nervous system in children leads to insufficient coordination between nerves and muscles, resulting in physiological floating toes.
Laxity of the ligaments: in children, the ligaments are relatively lax and do not pull sufficiently on the bones of the toes.
Normal foot growth and development: as the child's foot grows and develops, the ligaments and muscles of the foot gradually develop into a stable structure that becomes the regular foot and ankle structure.
Lighter weight at birth: studies have confirmed that 42 children's lighter weight is significantly associated with physiological floating toes, independent of other factors measured at birth.
In addition, Wako et al. also ruled out several factors that were thought to be possible causes of the formation of physiological floating toes, such as lower limb muscle strength, physical length at birth, physical development, and time to start walking.
Physiological floating toe is not a disease because, in general, it has a natural tendency to heal on its own. And can gradually disappear as the child ages. It should be distinguished from complications resulting from the Weil osteotomy.
Possible Interventions
In response to these possible causes of floating toes, we have reviewed and consolidated a large body of literature and collected recommendations from foot and ankle surgeons specializing in Hallux valgus, transfer metatarsalgia and so on, to list the following possible interventions to reduce the incidence of floating toes.
Pre‐operative Assessment
A thorough pre‐operative assessment, including an evaluation of the structure, function, nerves, and blood vessels of the foot, should be carried out before a decision is made to proceed with a Weil osteotomy. A detailed history of the patient, especially relevant diseases, surgical history, and allergies, can help the surgeon determine whether there are potential health problems affecting the patient's prognosis and whether there are risk factors that may affect the procedure; a meticulous and thorough physical examination: perform a physical examination including foot appearance, palpation and joint mobility to assess the source of pain, swelling or other abnormal symptoms and to determine the appropriate imaging tests. Based on the surgeon's experience, select appropriate imaging tests such as X‐ray, MRI, CT, etc. This can help the surgeon determine the internal condition of the patient's foot, select the best surgical procedure, and reduce the risk of surgical and post‐operative complications. Assess the risk of anesthesia: perform an anesthetic risk assessment to determine the most appropriate type and dose of anesthesia for the patient. Assessing post‐operative rehabilitation and determining the expected recovery time can help to reduce the risk of joint stiffness due to prolonged immobilization at a later stage, which can lead to a floating toe; patient education: providing adequate preoperative education to patients about the procedure and the risks involved can help to reduce patient concerns and anxiety and improve This helps to reduce the patient's concerns and anxiety and increases the level of cooperation from the patient and their family after surgery. In conclusion, a rigorous and comprehensive preoperative assessment can help the surgeon determine the patient's suitability for surgery and reduce the risk of complications such as floating toes in several ways.
Concentration During Surgery
During the Weil osteotomy procedure, it is imperative for the surgeon to adhere to the optimal cutting trajectory in order to maintain stability and equilibrium of the foot bones. Additionally, careful consideration must be given to selecting the appropriate site for osteotomy and determining the extent of resection, as excessive removal may lead to the undesirable outcome of a floating toe. 21 , 23 Furthermore, the surgeon should exercise special caution to safeguard the nerves and blood vessels in the foot, as well as the neurovascular and nerve microcirculation in the toe region. The significance of microcirculation in facilitating post‐operative healing and minimizing post‐operative complications has been widely recognized. 45 In addition, it is imperative to address the management of soft tissues during surgery, including the implementation of appropriate soft tissue repair procedures when necessary. This is crucial in order to prevent complications such as floating toes, which can arise from tendon stretching. It is essential to minimize the excessive stretching of foot muscles and ligaments, as this can lead to elongation of ligamentous tendons. 12 , 32 This necessitates a higher level of skill and expertise from the surgeon conducting the procedure.
Improved Surgical Techniques
Improving surgical techniques may be a worthwhile direction to consider to reduce complications such as floating toes in Weil osteotomy. For example, the traditional Weil osteotomy involves making a longitudinal incision on the dorsal side of the metatarsal bone, and performing an oblique osteotomy 1–2 mm below the dorsal boundary of the articular cartilage, with the direction as parallel as possible to the load‐bearing surface. The degree of shortening is controlled on the dorsal surface of the proximal fragment, and two parallel or crossed Kirschner wires or 2 mm screws are selected for fixation. Surgery can easily cause changes in the mechanical structure of the foot bone; relative lengthening of tendons and ligaments; metatarsal plate relaxation, change in the windlass mechanism; and scar contracture of the dorsal skin, greatly increasing the incidence of floating toes. Therefore, in response to the shortcomings of traditional Weil osteotomy, smaller incisions, more precise osteotomy positions, and more accurate fixation of the bone graft have been proposed to reduce the impact on foot structure and function. can be used to reduce the impact on the structure and function of the foot.
Modified Weil Osteotomy
Metatarsophalangeal joint (MPJ) instability is a prevalent clinical issue encountered by surgeons specializing in foot and ankle conditions. 31 , 46 Numerous studies have provided extensive documentation on this matter. 46 , 47 , 48 , 49 , 50 The aforementioned modified procedure demonstrates efficacy in addressing persistent coronal plane malalignment of the lesser MTP joint (MPJ) when the conventional Weil osteotomy fails to completely restore the anatomical position of the MPJ. In comparison to the conventional Weil osteotomy, the modified Weil osteotomy demonstrates enhancements in various aspects, including the incision location, osteotomy site, resection volume, correction method, and fixation technique. These modifications aim to safeguard the soft tissues and joints of the foot, resulting in reduced trauma, a shorter recovery period, and improved tolerance for alterations in the relative length of the second and third metatarsals (Figure 6). 49 According to Herzog et al. 50 the modified Weil osteotomy has demonstrated a reduced occurrence of floating toes and improved clinical outcomes. During their average follow‐up period of 9.1 months, the post‐operative American Foot and Ankle Association score (AOFAS) increased to 76.7 and the visual analogue scale (VAS) 51 score decreased from 6.7 preoperatively to 1.7 post‐operatively. The Kim team and the Edmondson team reached the similar conclusion: Kim et al. reported that the post‐operative VAS score reduced from 6.2 ± 1.4 to 1.4 ± 1.5, and post‐operative AOFAS score increased to 80.4 ± 5.6, 47 while Edmondson et al. reported a 36‐point increase in the average score after modified surgery. 48
FIGURE 6.

An atomical interpretation of the modified Weil osteotomy. 49
Triple Weil Osteotomy
When the degree of metatarsal shortening exceeds 3 mm, it results in an elevation of metatarsal displacement, thereby leading to a significant and highly prevalent occurrence of floating toes. Consequently, Monteagudo and Maceira devised the triple Weil osteotomy (Figure 7) as a means to achieve a regulated reduction in length, aligned with the metatarsal shaft, and to elevate the metatarsal head in response to metatarsal displacement resulting from a shortening exceeding 3 mm. 10 The triple Weil osteotomy has been identified as an enhancement over the conventional osteotomy in various aspects. 52 , 53 , 54 Initially, in the triple Weil osteotomy procedure, the plantar bone is partitioned into three distinct fragments, which are subsequently excised and individually modified, so facilitating a more intricate manipulation process. Furthermore, the triple Weil osteotomy has been found to provide significant benefits in the enhancement of plantar fascia laxity 53 without the requirement of substantial dorsiflexion of the MTP joint, hence lowering the occurrence of floating toes in many manners. Bougiouklis et al. showed that the average AOFAS score of triple Weil osteotomy increased from 50 points to 93 points, which was significantly better than the 89 points of Weil osteotomy. 52 When the metatarsal bone needs to be shortened by 5 mm or more, the average difference of plantar displacement between Triple Weil osteotomy and Weil osteotomy is 3.7 mm, which proves that triple Weil osteotomy can significantly prevent the plantar displacement of the rotation center of MTP joint. 26
FIGURE 7.
Anatomical interpretation of the triple Weil osteotomy. 52
Secondary or Simultaneous Surgery
The occurrence of complications such as floating toes is not immediate post‐operation, but rather tends to escalate gradually. In many instances, despite the initial procedure yielding favorable outcomes, further issues arising from floating toes tend to manifest over time. Doctors have incorporated a supplementary or adjunctive technique during the primary surgery, such as the flexor tenodesis procedure, in order to address or preempt the difficulties associated with the osteotomy, specifically the occurrence of floating toe. The prevailing consensus among surgeons is that the relative laxity of the tendon, ligaments, and particularly the flexor tendon, is a notable contributing factor to the occurrence of floating toes. De Netto et al. 55 conducted a study to investigate the efficacy of flexor tendon fixation on the metatarsal side of the proximal phalanx. Their findings demonstrated that this approach enables the fixation of both long and short toe flexors to an implant on the metatarsal side of the proximal phalanx, requiring only a minimal surgical incision. This technique effectively addresses and corrects deformities related to sagittal and dorsiflexion of the MTP joint, as well as the condition known as floating toe. The study involved a systematic analysis of three patients with floating toes. Lee et al. 19 demonstrated the successful transfer of the FDB tendon to the PIP joint for the purpose of correcting floating toes. This was achieved through the use of cadaveric research. Over the course of several years, medical professionals have conducted extensive research on the identification of improved sites for tendon transfer or the development of more effective surgical techniques. 56 , 57 , 58 , 59 Various alternative methods have been employed to relocate the attachment point of the flexor hallucis longus tendon, such as the fusion of the flexor hallucis longus tendon with the extensor hallucis longus tendon, among others. By altering the initial attachment site of the (flexor tendon) or suitably shortening the (flexor tendon), the normal tension is reinstated, hence addressing the condition known as floating toe.
It is important to acknowledge that some studies 4 , 60 , 61 have reported that arthrodesis of the PIP joint is associated with joint stiffness and downward displacement of the rotation center of the MTP joint. The downward displacement of the rotation center of the MTP joint results in an elevated occurrence of floating toes. Nevertheless, the integration of PIP fusion alongside the (flexor tenodesis) treatment significantly diminishes the likelihood of experiencing floating toes. 31 This discovery has the potential to pave the way for further investigation into a novel approach or amalgamation of the Weil osteotomy, (flexor tenodesis treatment), and PIP joint arthrodesis. The integration of these novel approaches presents a potential paradigm shift in addressing the prevalent occurrence of floating toes.
Post‐operative Rehabilitation
Post‐operative rehabilitation is the key to reducing complications from Weil's osteotomies. Post‐operative rehabilitation should be personalized to the patient, and we consulted experienced surgeons who have performed Weil osteotomies for many years and obtained the following recommendations:
Wearing the right, comfortable shoes: they can effectively reduce the forces on the foot and avoid pressure and friction, thus reducing the risk of floating toes occurring due to external forces. Post‐operative rehabilitation can help restore function and stability to the foot and prevent complications from occurring.
Keeping your feet healthy: regular foot massage, proper foot stretching, and exercises under the advice of a medical professional can increase flexibility and stability.
Weight control: excessive weight can put excessive pressure on the foot, increasing the weight bearing on the foot and increasing the risk of Arch collapse, leading to floating toes.
Avoid prolonged and intense standing and walking: even if the metatarsal bone is well healed after osteotomy, it is still relatively fragile, and prolonged and strenuous standing or walking can lead to severe complications such as wound rupture, malunion, nonunion of bone and floating toe. It is crucial to reduce foot strain and take appropriate rest during daily work and life.
Avoid foot injuries: injuries can cause secondary damage to the muscles, ligaments, nerves, and bones around the osteotomy site, increasing the risk of poor prognosis and complications, so extra care should be taken concerning foot safety.
Post‐operative Follow‐up (POST‐OP)
Post‐operative follow‐up (POST‐OP) is always emphasized by clinicians and is of great importance. Post‐operative follow‐up at 2 weeks, 4 weeks, 6 weeks, 3 months, 6 months, or 1 year is usually recommended, which helps the surgeon check the structure and function of the foot after surgery, identify and manage complications such as floating toes, and ensure that the surgery results are long‐lasting. Follow‐up visits can include the AOFAS forefoot efficacy score, pain VAS score, tenderness index, skin sensation around the incision, and off section mobility and MTP joint matching degree, foot X‐ray angle measurement, anxiety score, etc.
Discussion
The review summarizes important research information. In addition to the physiological floating toe belongs to the stage phenomenon of the growth process, the occurrence of pathological floating toe is obviously related to Weil osteotomy, and has become one of its common complications. Surgeons have been working hard to investigate the cause of floating toe, and hypotheses have been put forward and verified from the aspects of mechanical structure, rotation center, soft tissue balance and so on. Skin scars and vascular and nerve injuries have also been taken into account. Nevertheless, the occurrence of a floating toe is a result of intricate interactions between several systems and is not only attributed to anatomical alterations generated by surgery, skin scars, and similar factors. Several studies have indicated that the occurrence of floating toes can be significantly influenced by individual variations and lifestyle choices, including regular use of high‐heeled footwear and engaging in prolonged and vigorous physical activities. 62 , 63
There are limitations in the current stage of research. There are many etiological hypotheses, but most of them lack of high‐quality evidence, and there is a lack of review articles that have been agreed by experts. This article will screen and summarize the content supported by relevant evidence in order to facilitate the expert consensus in the future. According to the available evidence, we have proposed a range of potential procedures aimed at mitigating the occurrence of floating toes and emphasized the importance of comprehensive management for floating toes. It is advised to use caution in addressing floating toes, starting from pre‐operative assessment and extending to surgical selection, post‐operative rehabilitation and follow‐up, which are all important. We believe that the change of mechanical structure is the main cause of floating toe after Weil osteotomy. At this stage, with the “Maestro” curve explicitly described, foot and ankle doctors have paid attention to the preservation of parabola when performing Weil osteotomy. However, in the process of oblique osteotomy, because of the downward force of the pendulum saw, the downward of the metatarsal head and the downward movement of the rotation center seem to be inevitable, which is the main reason for the formation of floating toes. we considered releasing the metatarsal soft tissue after Weil osteotomy to reduce the downward traction of the metatarsal head, however, in clinical observation and literature retrieval, the problems of flexor tendon injury and metastatic metatarsalgia (caused by uneven distribution of soft tissue) were found after release. Metatarsalgia is often associated with mallet toe deformity, which requires additional PIP arthrodesis. A Kirschner needle is often used to connect distal the interphalangeal joint, PIP joint and even the MTP joint. In order to ensure the correction effect of hammer toe, a larger dorsal extension angle of MTP joint is often used. Clinically, the Kirschner needle was removed 4 weeks after operation, and the joint stiffness caused by it became a significant factor affecting the aggravation of floating toe. The lack of clinical research on inserting Kirschner needle parallel to the sole of the foot may reduce the incidence of floating toes caused by PIP joint arthrodesis.
Our review has some limitations. There are few separate literatures about floating toe, and most of them are involved in part, so it is difficult to screen and there may be omissions. In addition, in the induction of the etiology of floating toe, there is a compound effect of multiple mechanisms, resulting in the lack of clarity in the analysis. Nevertheless, the advantages of our study include conducting literature screening according to systematic and transparent programmes, ensuring document quality by multiple examiners, and reporting strictly in accordance with PRISMA‐ScR principles.
According to the review results, we recommend that future studies will focus on the improvement of surgical procedures. The combination of PIP joint arthrodesis is frequently observed in conjunction with weil osteotomies. Nevertheless, the occurrence of floating toes is found to be significantly associated with joint arthrodesis. The implementation of the flexor tenodesis fixation surgery, which involves transferring the attachment point of the flexor tendon to allow it to function normally. We believe that a comprehensive assessment of the risk of floating toes and a step‐by‐step decision on whether to perform the Weil osteotomy, PIP joint arthrodesis, and/or flexor tendesis fixation surgery can effectively prevent floating toes from occurring as surgical complications while avoiding unnecessary surgery, and address potential major pathologies.
Conclusion
FTD is included physiological and pathological. After a detailed analysis of the physiology, pathology of the floating toe and the Weil osteotomy, this article provides a comprehensive overview of the current body of knowledge pertaining to the etiology of floating toes, and explores the potential contributing variables associated with the development of this condition and feasible treatments.
Conflict of Interest Statement
All of the authors had no any personal, financial, commercial, or academic conflicts of interest separately.
Ethical Statement
This article is a summary article and does not need ethical approval.
Author Contributions
Ziyan Guo performed the article writing, Binglang Xiong performed the article revision, Longwei Zhang performed the article translation and embellishment, Xuhan Cao performed the literature screening, Xudong Sun performed the literature screening, Weidong Sun coordinated the study and reviewed the manuscript and he is primarily responsible for this article. All authors read and approved the final manuscript.
Funding Information
This study received primary funding and grant support from the National Natural Science Foundation of China (81373802) and Beijing Science and Technology Plan (Z191100006619024).
Acknowledgments
We thank Prof. Weidong Sun of the China Academy of Chinese Medical Sciences for funding and constructive discussion.
References
- 1. McGlamry E. Floating toe syndrome. J Am Podiatr Med Assoc. 1982;72(11):561–568. [DOI] [PubMed] [Google Scholar]
- 2. Fukuyama K, Maruyama H. Occurrence of floating toe from the viewpoint of the structure of foot arch. J Phys Ther Sci. 2011;23(1):33–36. [Google Scholar]
- 3. Vandeputte G, Dereymaeker G, Steenwerckx A, Peeraer L. The Weil osteotomy of the lesser metatarsals: a clinical and pedobarographic follow‐up study. Foot Ankle Int. 2000;21(5):370–374. [DOI] [PubMed] [Google Scholar]
- 4. Migues A, Slullitel G, Bilbao F, Carrasco M, Solari G. Floating‐toe deformity as a complication of the Weil osteotomy. Foot Ankle Int. 2004;25(9):609–613. [DOI] [PubMed] [Google Scholar]
- 5. Ramisetty N, Greiss M. The Weil osteotomy: a seven‐year follow‐up. J Bone Joint Surg Br. 2007;89(2):280. [DOI] [PubMed] [Google Scholar]
- 6. Highlander P, VonHerbulis E, Gonzalez A, Britt J, Buchman J. Complications of the Weil osteotomy. Foot Ankle Spec. 2011;4(3):165–170. [DOI] [PubMed] [Google Scholar]
- 7. Garg R, Thordarson DB, Schrumpf M, Castaneda D. Sliding oblique versus segmental resection osteotomies for lesser metatarsophalangeal joint pathology. Foot Ankle Int. 2008;29(10):1009–1014. [DOI] [PubMed] [Google Scholar]
- 8. Wagner E, O'Connell LA, Radkievich R, Caicedo N, Mococain P, Wagner P. Incidence of and functional significance of floating toe after Weil osteotomy. Foot Ankle Orthop. 2019;4(4):2473011419891956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Reddy VB. Metatarsal osteotomies: complications. Foot Ankle Clin. 2017;23(1):47–55. [DOI] [PubMed] [Google Scholar]
- 10. Monteagudo M, Maceira E. Evolution of the Weil osteotomy: the triple osteotomy. Foot Ankle Clin. 2019;24(4):599–614. [DOI] [PubMed] [Google Scholar]
- 11. Schuh R, Trnka HJ. Metatarsalgia: distal metatarsal osteotomies. Foot Ankle Clin. 2011;16(4):583–595. [DOI] [PubMed] [Google Scholar]
- 12. Trnka H‐J, Nyska M, Parks BG, Myerson MS. Dorsiflexion contracture after the Weil osteotomy: results of cadaver study and three‐dimensional analysis. Foot Ankle Int. 2001;22(1):47–50. [DOI] [PubMed] [Google Scholar]
- 13. Perez HR, Reber LK, Christensen JC. The role of passive plantar flexion in floating toes following Weil osteotomy. J Foot Ankle Surg. 2008;47(6):520–526. [DOI] [PubMed] [Google Scholar]
- 14. O'Kane C, Kilmartin T. The surgical management of central metatarsalgia. Foot Ankle Int. 2002;23(5):415–419. [DOI] [PubMed] [Google Scholar]
- 15. Hofstaetter S, Hofstaetter J, Petroutsas J, Gruber F, Ritschl P, Trnka H‐J. The Weil osteotomy: a seven‐year follow‐up. J Bone Joint Surg Br. 2005;87(11):1507–1511. [DOI] [PubMed] [Google Scholar]
- 16. Coughlin M. Hallux valgus. Instr Course Lect. 1997;46:357–391. [PubMed] [Google Scholar]
- 17. Suh JW, Jang H‐S, Park H‐W. Iatrogenic second transfer metatarsalgia and the first metatarsal shortening and elevation after scarf osteotomy. Foot Ankle Surg. 2022;28(4):464–470. [DOI] [PubMed] [Google Scholar]
- 18. Melamed EA, Schon LC, Myerson MS, Parks BG. Two modifications of the Weil osteotomy: analysis on sawbone models. Foot Ankle Int. 2002;23(5):400–405. [DOI] [PubMed] [Google Scholar]
- 19. Lee LC, Charlton TP, Thordarson DB. Flexor digitorum brevis transfer for floating toe prevention after Weil osteotomy: a cadaveric study. Foot Ankle Int. 2013;34(12):1724–1728. [DOI] [PubMed] [Google Scholar]
- 20. Derner R, Meyr AJ. Complications and salvage of elective central metatarsal osteotomies. Clin Podiatr Med Surg. 2009;26(1):23–35. [DOI] [PubMed] [Google Scholar]
- 21. Valley B, Reese H. Guidelines for reconstructing the metatarsal parabola with the shortening osteotomy. J Am Podiatr Med Assoc. 1991;81(8):406–413. [DOI] [PubMed] [Google Scholar]
- 22. Maestro M, Besse J‐L, Ragusa M, Berthonnaud E. Forefoot morphotype study and planning method for forefoot osteotomy. Foot Ankle Clin. 2003;8(4):695–710. [DOI] [PubMed] [Google Scholar]
- 23. Stoupine A, Singh BN. A cadaveric study of metatarsal length and its function in the metatarsal formula and forefoot pathology. J Am Podiatr Med Assoc. 2018;108(3):194–199. [DOI] [PubMed] [Google Scholar]
- 24. Godoy‐Santos AL, Diniz Fernandes T, Luzo C, Ortiz RT, Sakaki M, Weil L Jr. Effectiveness of the dorsal thermoplastic locking orthosis to prevent floating toes in postoperative follow‐up of Weil osteotomies: pilot study. Foot Ankle Spec. 2014;7(5):356–362. [DOI] [PubMed] [Google Scholar]
- 25. Grimes J, Coughlin M. Geometric analysis of the Weil osteotomy. Foot Ankle Int. 2006;27(11):985–992. [DOI] [PubMed] [Google Scholar]
- 26. Bougiouklis D, Tyllianakis M, Deligianni D, Panagiotopoulos E, Bougiouklis D, Tyllianakis M, et al. Biomechanical analysis of the change of the metatarsophalangeal Joint's Center of Rotation after Weil and Triple Weil Osteotomies: a comparative cadaveric study. Cureus. 2022;14(2):e21866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bobrov D, Slinjakov L, Rigin N. The primary metatarsalgia: pathogenesis, biomechanics and surgical treatment. Vestn Ross Akad Med Nauk. 2017;72(1):53–58. [DOI] [PubMed] [Google Scholar]
- 28. Bennett AJ, McLeod I. An adaptation of Weil's osteotomy of the lesser metatarsal neck. J Foot Ankle Surg. 2009;48(4):516–517. [DOI] [PubMed] [Google Scholar]
- 29. Weil L Jr, Sung W, Weil LS Sr, Malinoski K. Anatomic plantar plate repair using the Weil metatarsal osteotomy approach. Foot Ankle Spec. 2011;4(3):145–150. [DOI] [PubMed] [Google Scholar]
- 30. Dohle J, Marques A. Reconstruction of the plantar plate of the metatarsophalangeal joint using a dorsal transarticular approach. Oper Orthop Traumatol. 2021;33:422–429. [DOI] [PubMed] [Google Scholar]
- 31. Cook JJ, Johnson LJ, Cook EA. Anatomic reconstruction versus traditional rebalancing in lesser metatarsophalangeal joint reconstruction. J Foot Ankle Surg. 2018;57(3):509–513. [DOI] [PubMed] [Google Scholar]
- 32. Sorensen MD, Weil L. Lesser metatarsal osteotomy. Clin Podiatr Med Surg. 2015;32(3):275–290. [DOI] [PubMed] [Google Scholar]
- 33. Moraes MR, Cavalcante MLC, Leite JAD, Ferreira FV, Castro AJO, Santana MG. Histomorphometric evaluation of mechanoreceptors and free nerve endings in human lateral ankle ligaments. Foot Ankle Int. 2008;29(1):87–90. [DOI] [PubMed] [Google Scholar]
- 34. Attinger CE, Evans KK, Bulan E, Blume P, Cooper P. Angiosomes of the foot and ankle and clinical implications for limb salvage: reconstruction, incisions, and revascularization. Plast Reconstr Surg. 2006;117(7S):261S–293S. [DOI] [PubMed] [Google Scholar]
- 35. Petersen W, Lankes J, Paulsen F, Hassenpflug J. The arterial supply of the lesser metatarsal heads: a vascular injection study in human cadavers. Foot Ankle Int. 2002;23(6):491–495. [DOI] [PubMed] [Google Scholar]
- 36. Rath B, Notermans H‐P, Franzen J, Knifka J, Walpert J, Frank D, et al. The microvascular anatomy of the metatarsal bones: a plastination study. Surg Radiol Anat. 2009;31:271–277. [DOI] [PubMed] [Google Scholar]
- 37. Nguyen U‐S, Hillstrom HJ, Li W, Dufour AB, Kiel DP, Procter‐Gray E, et al. Factors associated with hallux valgus in a population‐based study of older women and men: the MOBILIZE Boston study. Osteoarthr Cartil. 2010;18(1):41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Piqué‐Vidal C, Solé MT, Antich J. Hallux valgus inheritance: pedigree research in 350 patients with bunion deformity. J Foot Ankle Surg. 2007;46(3):149–154. [DOI] [PubMed] [Google Scholar]
- 39. Jia J, Li J, Qu H, Li M, Zhang S, Hao J, et al. New insights into hallux valgus by whole exome sequencing study. Exp Biol Med. 2021;246(14):1607–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Fujimaki T, Wako M, Koyama K, Furuya N, Shinohara R, Otawa S, et al. Prevalence of floating toe and its relationship with static postural stability in children: the Yamanashi adjunct study of the Japan environment and Children's study (JECS‐Y). PloS One. 2021;16(3):e0246010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wako M, Fujimaki T, Koyama K, Furuya N, Shinohara R, Otawa S, et al. A cross‐sectional study on the correlations between floating toe, plantar arch posture, and body composition in 8‐year‐old children. Foot Ankle Surg. 2022;28(7):1035–1039. [DOI] [PubMed] [Google Scholar]
- 42. Araki T, Masuda T, Jinno T, Morita S. Incidence of floating toe and its association with the physique and foot morphology of Japanese children. J Phys Ther Sci. 2015;27(10):3159–3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Tasaka S, Matsubara K, Nishiguchi S, Fukutani N, Tashiro Y, Shirooka H, et al. Association between floating toe and toe grip strength in school age children: a cross‐sectional study. J Phys Ther Sci. 2016;28(8):2322–2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wako M, Koyama K, Furuya N, Shinohara R, Otawa S, Kobayashi A, et al. Relationship between floating toes condition and lower limb muscle weight in 8‐year‐old children: the Yamanashi adjunct study of the Japan environment and Children's study (JECS‐Y). J Phys Ther Sci. 2023;35(3):252–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Balasubramanian G, Vas P, Chockalingam N, Naemi R. A synoptic overview of neurovascular interactions in the foot. Front Endocrinol. 2020;11:308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Klinge SA, McClure P, Fellars T, DiGiovanni CW. Modification of the Weil/Maceira metatarsal osteotomy for coronal plane malalignment during crossover toe correction: case series. Foot Ankle Int. 2014;35(6):584–591. [DOI] [PubMed] [Google Scholar]
- 47. Kim J, Choi WJ, Park YJ, Lee JW. Modified Weil osteotomy for the treatment of Freiberg's disease. Clin Orthop Surg. 2012;4(4):300–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Edmondson M, Sherry K, Afolayan J, Armitage A, Skyrme A. Case series of 17 modified Weil's osteotomies for Freiberg's and Köhler's II AVN, with AOFAS scoring pre‐and post‐operatively. Foot Ankle Surg. 2011;17(1):19–24. [DOI] [PubMed] [Google Scholar]
- 49. de César PC, Torres AC, Oliani CHP, de Abreu MR. Influence of the length ratio between second and third metatarsals after modified Weil osteotomy on clinical outcomes. J Foot Ankle Surg. 2022;61(5):1007–1012. [DOI] [PubMed] [Google Scholar]
- 50. Herzog JL, Goforth WD, Stone PA, Paden MH. A modified fixation technique for a decompressional shortening osteotomy: a retrospective analysis. J Foot Ankle Surg. 2014;53(2):131–136. [DOI] [PubMed] [Google Scholar]
- 51. Martin KD, McBride T, Wake J, Van Buren JP, Dewar C . Comparison of visual analog pain score reported to physician vs nurse in nonoperatively treated foot and ankle patients. Foot Ankle Int. 2018;39(12):1444–1448. [DOI] [PubMed] [Google Scholar]
- 52. Bougiouklis D, Tyllianakis M, Deligianni D, Panagiotopoulos E, Bougiouklis D, Tyllianakis M, et al. Comparison of the Weil and triple Weil osteotomies: a clinical retrospective study. Cureus. 2022;14(2):e22220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Espinosa N, Myerson MS, De Retana PF, Maceira E. A new approach for the treatment of metatarsalgia: the triple Weil osteotomy. Techniques Foot Ankle Sur. 2007;6(4):254–263. [Google Scholar]
- 54. Pérez‐Muñoz I, Escobar‐Antón D, Sanz‐Gómez TA. The role of Weil and triple Weil osteotomies in the treatment of propulsive metatarsalgia. Foot Ankle Int. 2012;33(6):501–506. [DOI] [PubMed] [Google Scholar]
- 55. de Cesar NC, Schmidt EL, Lalevee M, Mansur NSB. Correction to: flexor tenodesis procedure in the treatment of lesser toe deformities. Arch Orthop Trauma Surg. 2022;142(11):3139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Landsman A, Cook E, Cook J. Tenotomy and tendon transfer about the forefoot, midfoot and hindfoot. Clin Podiatr Med Surg. 2008;25(4):547–569. [DOI] [PubMed] [Google Scholar]
- 57. Myers SH, Schon LC. Forefoot tendon transfers. Foot Ankle Clin. 2011;16(3):471–488. [DOI] [PubMed] [Google Scholar]
- 58. Nery C, Baumfeld D. Lesser metatarsophalangeal joint instability: treatment with tendon transfers. Foot Ankle Clin. 2018;23(1):103–126. [DOI] [PubMed] [Google Scholar]
- 59. Veljkovic A, Lansang E, Lau J. Forefoot tendon transfers. Foot Ankle Clin. 2014;19(1):123–137. [DOI] [PubMed] [Google Scholar]
- 60. Waizy H, Abbara‐Czardybon M. Arthodesis of the proximal and distal interphalangeal joint. Oper Orthop Traumatol. 2014;26:307–323. [DOI] [PubMed] [Google Scholar]
- 61. Döhner C, Beyerle H, Graw JA, Soost C, Burchard R. Biomechanical comparison of different implants for PIP arthrodesis. Foot Ankle Surg. 2023;29:518–524. [DOI] [PubMed] [Google Scholar]
- 62. Nagamoto H, Kimura R, Hata E, Kumai T. Disabled throwing shoulder/elbow players have high rates of impaired foot function. Res Sports Med. 2023;31(5):679–686. [DOI] [PubMed] [Google Scholar]
- 63. Yanagiya T, Hata K, Takeshita T, Noro H, Yoshida T, Koyama M, et al. Athletic event‐specific characteristics in floating toes during the static standing posture. J Phys Ther Sci. 2020;32(5):342–347. [DOI] [PMC free article] [PubMed] [Google Scholar]


