Abstract
Novel hybrid approaches for chest wall irradiation show promising outcomes regarding target coverage and sparing organs at risk (OARs). In this systematic review, we compared hybrid volumetric modulated arc therapy (H-VMAT) or hybrid intensity-modulated radiotherapy (H-IMRT) techniques with non-hybrid techniques, such as three-dimensional conformal radiation therapy (3DCRT), field-in-field (FIF), intensity-modulated arc therapy (IMRT), and volumetric modulated arc therapy (VMAT), for breast cancer patients with mastectomy. Our focus was the plan quality and dose distribution to the OARs. Using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist, we performed a systematic review and quality appraisal of primary studies evaluating hybrid therapy to the chest wall and the OARs. An extensive online search of PubMed and Scopus databases was conducted using appropriate keywords. The dose to the OARs (lung, heart, and contralateral breast), planning target volume (PTV), homogeneity index (HI), and conformity index (CI) were extracted. The data were then tabulated and compared for the outcomes between modalities among the studies. Nine studies that met the search criteria were selected to evaluate the PTV coverage and dosimetric results of hybrid and non-hybrid techniques. In terms of 95% PTV coverage, among nine reviewed studies, the largest difference between the two techniques was between VMAT (47.6 Gy) and H-VMAT (48.4 Gy); for the conformity index, the largest difference was noted between 3DCRT (0.58) and H-VMAT (0.79). In both cases, differences were statistically significant (P < 0.005). Two studies showed dose homogeneity improvement within the treatment target in H-VMAT (0.15 and 0.07) compared with 3DCRT (0.41 and 0.12), with a P value of <0.001. Two studies did not report on the homogeneity index, and three others observed no statistical difference. Regarding OARs, in the comparison of H-VMAT and VMAT, the largest significant change was in the volume receiving 5 Gy (V5Gy) of the ipsilateral lung and the V10Gy of the contralateral lung. For the ipsilateral lung, V5Gy was 90.7% with VMAT versus 51.45% with H-VMAT. For the contralateral lung, V10Gy was 54.9% with VMAT versus 50.5% with H-VMAT. In six studies, the mean dose of the contralateral breast was lower in hybrid techniques than in single modalities: VMAT (4.2%, 6.0%, 1.9%, 7.1%, 4.57%) versus H-VMAT (1.4%, 3.4%, 1.8%, 3.5%, 2.34%) and IMRT (9.1%) versus H-IMRT (4.69%). Although most studies did not report on monitor units and treatment time, those that included them showed that hybrids had lower monitor units and shorter treatment times. Hybrid techniques in radiotherapy, such as combining two modalities, can indeed facilitate lower doses to OARs for patients with a high risk of toxicities. Prospective clinical studies are needed to determine the outcomes of breast cancer treated with hybrid techniques.
Keywords: intensity-modulated radiation therapy (imrt), hybrid radiotherapy planning, organs-at-risk, chest wall radiotherapy, vmat radiotherapy
Introduction and background
Radiotherapy is a treatment that uses high-energy radiation or radioactive elements to destroy cancer cells while preserving nearby healthy tissues [1]. External beam radiation therapy (EBRT) is a crucial treatment for breast cancer, especially for post-mastectomy patients. In cases where mastectomy has been performed, the indication for radiation therapy is different from breast-conserving treatment, where radiation therapy is an integral part of the treatment. Thus, for patients who are identified to have high-risk features after mastectomy, EBRT is often recommended to reduce the risk of local recurrence by targeting any cancer cells present in the chest wall or nearby lymph nodes. Treatment planning is a crucial component of breast cancer radiation therapy, ensuring that the radiation dose is accurately targeted to the affected area while minimizing exposure to the surrounding healthy tissues.
Radiation treatment planning of breast cancer can be performed using techniques ranging from three-dimensional conformal radiation therapy (3DCRT) and field-in-field (FIF) to more advanced therapies, such as intensity-modulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT). In conventional 3DCRT, tangential beams are employed with a simple wedge to avoid low-dose zones in the heart and ipsilateral lung or to create “FIF” or “sub-fields” to the main fields using a multileaf collimator (MLC) [1]. However, these approaches are typically linked to substantially worse homogeneity and compliance and potential hot spots beyond the target volume compared to IMRT and VMAT [2]. Dose homogeneity refers to the uniformity of the radiation dose that is administered throughout the intended area of treatment. However, compliance refers to treatment goals and prescribed dose constraints [3]. Compliance with the treatment plan balances the delivery of radiation dose to achieve therapeutic goals while minimizing the risk of adverse effects on healthy tissues [4].
IMRT is a type of radiation therapy that offers several benefits. It improves dose homogeneity within the target area while preserving critical organs, such as the heart and lungs. However, it has also been found to have potential drawbacks. High monitors (MUs) can increase treatment time and the amount of low-dose radiation exposure, which can potentially increase the risk of developing second malignancies [5].
VMAT has features that help reduce delivery time. It utilizes simultaneous optimization, dynamically adjusting the shape, intensity, and gantry speed of the radiation beam as the machine rotates around the patient. Unlike IMRT, where the gantry stops at various angles to deliver the radiation, VMAT’s gantry continuously rotates. Furthermore, VMAT provides the flexibility to adjust parameters, such as the dose rate and MLC speed, enhancing treatment planning and delivery [6].
IMRT and VMAT both increase the target’s dose conformity at the expense of higher low-dose spread to the contralateral lung and contralateral breast, which may increase the risk of secondary malignancy and other complications [7].
The curvature of the chest wall makes radiation therapy planning for postmastectomy patients more challenging, and the thin target volume along the lung interface makes chest wall irradiation harder than whole breast treatment. Furthermore, depending on the planner’s experience level, sophisticated planning procedures require more extended planning periods [8]. Another problem with breast treatment is target motion brought on by breathing [9]. Therefore, to ensure the accuracy driven by adaptive methods, image-guided radiotherapy (i.e., kilovoltage or megavoltage verification imaging) must be implemented with daily treatment [6]. As it minimizes the margin contributed to the planning target volume (PTV), image-guided radiotherapy has demonstrated an increase in daily treatment accuracy [9]. In addition, deep inspiration breath hold (DIBH) has been used, mainly on the left-sided breast or chest wall, and has considerably reduced the dosage to the heart [10].
In contrast to 3DCRT, IMRT and VMAT are more significantly affected by difficult-to-control breathing patterns [8,11]. Although these state-of-the-art therapies are clinically acceptable, new strategies are needed to successfully lower dosages to the heart and lungs. This need has led to the development of techniques known as hybrid IMRT and VMAT (H-IMRT and H-VMAT, respectively), which combine an open beam or FIF with an inversely planned IMRT or VMAT beam with various weightings.
Mayo et al. [12] introduced a novel technique that integrates static and dynamic fields, known as the hybrid technique, in treating breast cancer patients. This approach was specifically designed to address the crucial concern regarding the protection of OARs, while ensuring optimal treatment plan quality. The strategic integration of these modalities offers potential treatment optimization, particularly in cases related to the breast and the chest wall [13,14]. It is important to acknowledge that each modality has inherent advantages and disadvantages. However, integrating and synergizing these two approaches makes it possible to mitigate the limitations, thus presenting a more refined and enhanced alternative solution.
In this systematic review, we aimed to review and synthesize the comparison between H-VMAT or H-IMRT and non-hybrid techniques for breast cancer, focusing on the plan quality in terms of PTV coverage, homogeneity and conformity indexes, MU, treatment time, and OAR dosages for chest wall cancer patients.
Review
Material and methods
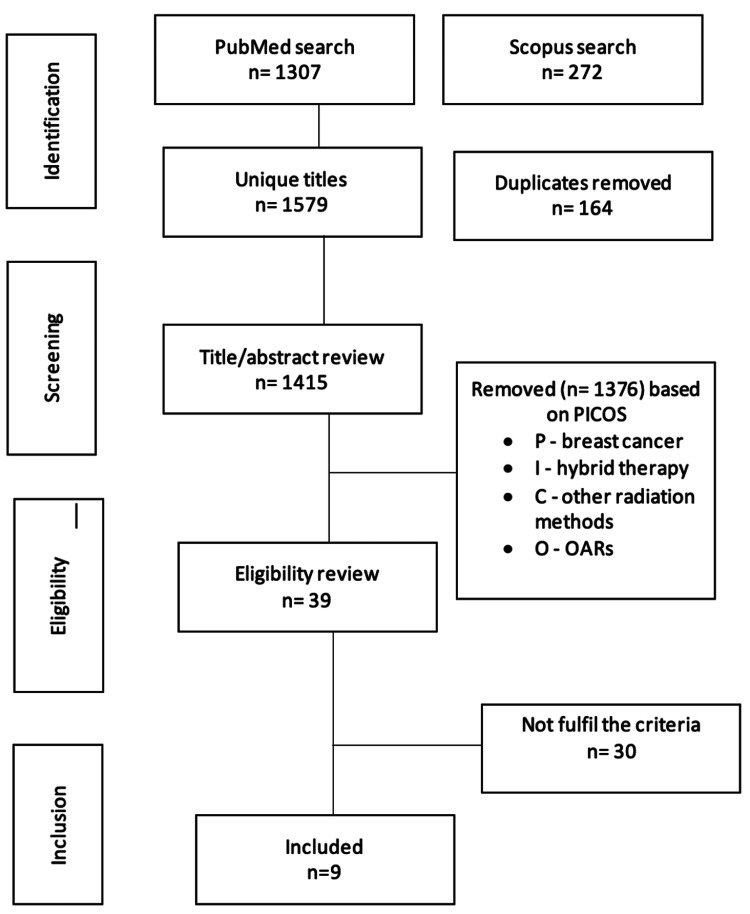
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist was used to guide the design and reporting of this work as a systematic review [15]. The search was conducted in the PubMed and Scopus databases using the population, intervention, control, and outcomes (PICO) framework to establish the search terms (Table 1, Appendix). This type of review is widely used to expand upon the current knowledge base to drive the development of healthcare practice [16-18]. Boolean search phrase combinations were used to guarantee that all pertinent articles were found (Supplementary A). Reference lists were checked for additional studies, and additional manual searches of relevant journals were performed. Following the search, the results were filtered based on the inclusion and exclusion criteria. Duplicates and irrelevant publications were removed from the search by manually filtering the titles and abstracts (Figure 1). The search was further filtered by reading full-text articles to weed out irrelevant publications.
Table 1. Characteristics of the included studies.
Abbreviations: N, number of patients; SCL, supraclavicular; ALN, axillary lymph nodes; IMN, internal mammary node; DIBH, deep inspiration breath hold; G, grade; TPS, treatment planning system; NA, not available; MV, megavolts; H-VMAT, hybrid-volumetric modulated arc therapy; H-IMRT, hybrid-intensity modulated radiation therapy; FIF, field in field.
| Reference | N | Nodes included | Dose prescription (no. of fractions) | Treatment side | Breathing setting | Stage or grade | Energy | TPS | Hybrid technique used | Dose weighting | Type of fields used |
| Balaji et al., 2018 [13] | 20 | SCL | 50.0 Gy (25) | Left | Normal | NA | 6 MV | ECLIPSE | H-VMAT (3DCRT+VMAT) | 90%/10%, 80%/20%, 70%/30%; | Two coplanar open tangential fields + four coplanar partial arcs |
| Dumane et al., 2018 [25] | 10 | SCL, ALN, IMN | 50.4 Gy (28) | 5 Left + 5 Right | Normal | II–IV | 6 MV | ECLIPSE | H-VMAT (3DCRT+VMAT) | NA | 3DCRT + two coplanar arcs |
| Lang et al., 2020 [26] | 11 | SCL, ALN, IMN | 50 Gy (25) | 4 Right + 7 Left | DIBH | Locally advanced | 6 + 10 MV | ECLIPSE | H-VMAT (3DCRT+VMAT) | 80%/20% | Four partial arcs with two additional tangential fields |
| Doi et al., 2020 [27] | 70 | SCL, ALN, IMN | 50 Gy (25) | 35 Left + 35 Right | Normal | G 1, 2, 3 | 6 MV | ECLIPSE | H- VMAT (3DCRT+VMAT) | NA | Four fields of 3DCRT (two main tangential fields and two anterior-posterior field) + two coplanar arcs |
| Cilla et al., 2021 [21] | 25 | SCL, ALN | 50.0 Gy (25) | Left | DIBH | G 3 | 6 MV | PINNACLE | H-IMRT (3CRT+IMRT), H-VMAT (3DCRT+VMAT) | 75%/25% | Two open tangential fields and two IMRT fields, two open tangential fields and two partial arcs |
| Zhang et al., 2022 [23] | 32 | SCL, ALN, IMN | 50 Gy (25) | Left | Normal | G 2, 3 | 6 MV | ECLIPSE | H-VMAT (3DCRT+VMAT) | 70%/30% | Five fields (two tangential fields + two partial arcs + one separate arc) |
| Sathiyaraj et al., 2022 [24] | 15 | SCL | 50 Gy (25) | Left | NA | NA | 6 MV | MONACO | H-VMAT (FIF+VMAT) | 70%/30% | FIF for IMRT and two coplanar partial arc for VMAT |
| Haldar et al., 2023 [22] | 10 | SCL, ALN | 40.5 Gy (15) | Left | NA | NA | 6 MV | ECLIPSE | H-IMRT (3DCRT+IMRT) | 60%/40% | Two tangential beams and two IMRT fields |
| Balaji et al., 2023 [20] | 25 | SCL, IMN | 40.5 Gy (15) | Left | DIBH | Locally advanced | 6, 10, 15 MV | ECLIPSE | H-IMRT (3DCRT+IMRT), H-VMAT (3DCRT+VMAT) (IMRT+VMAT) | 70%/30% | Two tangential (3DCRT) + two tangential IMRT or two partial arcs five IMRT fields + two partial arc |
Figure 1. Search strategy via the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Data Extraction and Synthesis
Authors and year, target, patients, dose prescription, treatment side, breathing setting, hybrid technique, stage, energy, treatment planning system, dose weighting, dose received by 95% (D95Gy) of the PTV in Gray(Gy), homogeneity index (HI), conformity index (CI), dose metrics with significant results, planning techniques used, planning or treatment time, MU, the hybrid technique used, type of fields, and the primary outcome of the study were extracted from the selected articles. The dosimetry of all the approaches, including VMAT, IMRT, H-VMAT, H-IMRT, and 3DCRT, was compared between the studies to explore the change in the dose level with different approaches along with their comparable outcomes.
Inclusion Criteria
Studies that involved patients with either left- or right-sided chest wall malignancies and who were candidates for radiation treatment were included. These studies also included the dose parameters of PTV and OARs to facilitate comparison between different treatment techniques.
Exclusion Criteria
Our review excluded studies that involved patients with metastatic disease and those who had previously undergone radiation therapy at the treatment site, as this could increase the risk of radiation-related complications. In addition, studies were excluded if they involved patients treated with other modalities alongside radiotherapy, such as electron and proton therapies.
Results
Study Characteristics
We initially identified 1,579 articles from the PubMed and Scopus searches, and 39 articles were ultimately selected based on the title and abstract. The results were filtered after the search based on the inclusion and exclusion criteria. Articles including whole-breast irradiation were excluded from this review, with the focus directly solely on chest wall irradiation. In addition, studies involving plan robustness were excluded due to their use of phantoms in the study methodology. This exclusion was made because plan robustness in radiotherapy involves quantifying uncertainties and simulating various errors using phantoms, which may not accurately represent the actual uncertainties and variations in patient anatomy and setup. Finally, nine publications were selected and included in the review.
The characteristics of the chosen research articles, which were published between 2018 and 2023, are summarized in Table 1. The nine reviewed articles have various levels of chest wall irradiation with lymph node inclusion. The left side was covered in six reports [19-24]. The chest wall on both sides was studied in three investigations [25-27]. The prescribed doses for the trials that were included ranged from 40.05 to 50.4 Gy in 15 to 25 fractions; the dose weighting for 3DCRT, IMRT, and VMAT ranged from 20% to 80%, and the energy range varied between 6, 10, and 15 MV. In addition, the current review includes reports with different techniques in terms of chest wall side and breathing patterns.
Plan Quality
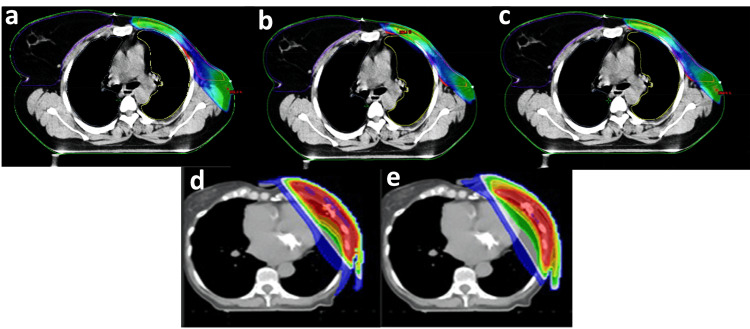
The main findings of the studies comparing the plan quality between hybrid and non-hybrid radiotherapy planning techniques, including MU, treatment time or planning time, HI, and CI, are summarized in Table 2. Various treatment planning strategies and hybrid approaches were used for breast radiotherapy, including 3DCRT, IMRT, VMAT, H-VMAT, and H-IMRT. The dose distribution map for the mentioned techniques is illustrated in Figure 2.
Table 2. Significant results of MU, TT, PTV, CI, and HI.
Abbreviations: AP, automated plan; CI, conformity index; CTV, clinical target volume; Dmin, minimum dose to the PTV; DT, delivery time; FIF, field in field; HI, homogeneity index; MP-VMAT, manual plan-volumetric modulated arc therapy; MU, monitor unit; NA, not available; ns, not statistically significant; PTV(cw), planning target volume for chest wall; PTV, planning target volume; TP, treatment planning; TT, treatment time.
^CTV values.
| Authors | Planning techniques used | MU | TT/TP/DT | PTV(cw)/CTV^ P < 0.05 | CI P < 0.05 | HI P < 0.05 | Conclusion |
| Balaji et al., 2018 [13] | FIF | 442 | NA | D95: 47.4 Gy | 0.58 | 0.12 | H-VMAT is better in CI and HI than FIF and significantly better in PTV coverage than VMAT. |
| H-VMAT | 489 | NA | D95: 48.4 Gy | 0.79 | 0.07 | ||
| VMAT | 524 | NA | D95: 47.6 Gy | 0.87 | 0.10 | ||
| Dumane et al., 2018 [25] | VMAT | NA | NA | V95: 97.0%ns | NA | NA | The difference in PTV coverage is not statistically significant. |
| H-VMAT | NA | NA | V95: 96.4%ns | NA | NA | ||
| Lang et al., 2020 [26] | VMAT | 673ns | NA | V95: 98.4% | 1.15 | 0.069ns | The quality of PTV is maintained compared with VMAT. |
| H-VMAT | 675ns | NA | V95: 97.1% | 1.21 | 0.082ns | ||
| Doi et al., 2020 [27] | 3DCRT | NA | NA | Dmin: 12.3 Gy | 2.1 | 0.41 | H-VMAT is better in PTV coverage and HI than 3DCRT. |
| H-VMAT | NA | NA | Dmin: 21.6 Gy | 1.6 | 0.15 | ||
| Cilla et al., 2021 [21] | H-IMRT | NA | NA | D95: 47.1 Gy | NA | 51.2 | H-IMRT and H-VMAT have the same PTV coverage. H-VMAT is better inhomogeneity than H-IMRT. AP-VMAT is better among all. |
| H-VMAT | NA | NA | D95: 47.1 Gy | NA | 44.8 | ||
| MP-VAMT | NA | NA | D95: 48.1 Gy | NA | 13.5 | ||
| AP-VMAT | NA | NA | D95: 48.5 Gy | NA | 12.4 | ||
| Zhang et al., 2022 [23] | VMAT | 746 | DT: 168.6 s | ^D50: 98.67 Gy | NA | NA | H-VMAT is better in PTV coverage than IMRT. MU delivered by VMAT and H-VMAT is the same but less than three times IMRT. |
| IMRT | 2098 | DT: 365.7 s | ^D50: 96.97 Gy | NA | NA | ||
| H- VMAT | 742 | DT: 169.5 s | ^D50: 98.31 Gy | NA | NA | ||
| Sathiyaraj et al., 2022 [24] | VMAT | NA | NA | D95: 96.9 Gy | 0.972ns | 0.127ns | H-VMAT is better in PTV coverage but has no statistical differences in CI and HI. |
| H-VMAT | NA | NA | D95: 96.2 Gy | 0.97ns | 0.12ns | ||
| Haldar et al., 2023 [22] | FIF | 323 | DT: 32.4 s, | D95: 37.10 Gy | 0.931 | 0.111 | H-IMRT is lower in MU than IMRT and similar in PTV coverage. H-IMRT is better in CI than FIF. FIF is the lowest in MU, DT, and the minimum in PTV coverage among all. IMRT is better than H-IMRT in HI and CI but not significantly different. |
| IMRT | 751 | DT: 75.0 s | D95: 39.32 Gy | 0.981ns | 0.087ns | ||
| H-IMRT | 510 | DT: 51.0 s | D95: 38.39 Gy | 0.970ns | 0.107ns | ||
| Balaji et al., 2023 [20] | 3DCRT+IMRT | 1094 | TT: 4.0 min | NA | 1.03ns | 1.08ns | All hybrids gave the same homogeneity and conformity. 3DCRT+VMAT gave less time and less MU. |
| 3DCRT+VMAT | 579 | TT: 3.2 min | NA | 1.03ns | 1.08ns | ||
| IMRT+VMAT | 831 | TT: 3.8 min | NA | 1.03ns | 1.09ns |
Figure 2. Dose distribution map of a) 3DCRT, b) IMRT, c) H-IMRT, d) VMAT, and e) H-VMAT.
a) 3DCRT, b) IMRT, c) H-IMRT; adopted from Haldar et al. (2023) [22]. d) VMAT and e) H-VMAT; adopted from Cilla et al. (2021) [21].
A combination of modalities produced better PTV coverage [19,22,23,27], lower HI [19,27], higher CI [19,22], lower MU [19,22,23], and shorter treatment time [19,22] than relying on a single modality. The hybrid techniques, H-VMAT or H-IMRT, performed better in PTV coverage than single modalities 3DCRT and VMAT. To illustrate, from two studies [19,22], the PTV coverage at 95% of the single modality 3DCRT was 47.6 Gy and 37.10 Gy, better than H-VMAT with 47.4 Gy and 38.39 Gy, respectively. In addition, the PTV coverage was better between VMAT and H-VMAT (47.6 Gy and 48.4 Gy, respectively) [19].
Moreover, HI and CI were also better in hybrid techniques than in IMRT or VMAT [19,22,27]. Dose homogeneity improvement is derived from the calculation of the homogeneity index, where a homogeneity index closer to 1 indicates a more uniform distribution of dose within the target volume, which is considered better. As the homogeneity index increases above one, it indicates a less uniform distribution of dose within the target volume [3]. For example, the HI and CI values for the single modality were 0.41 and 2.1, respectively, while for the hybrid techniques, they were 0.15 and 1.6 [27]. Other studies did not report or did not find a significant change [21,23,25]. H-VMAT and H-IMRT had lower MUs and less treatment time. From two reviewed studies, the MU decreased from 524 and 746 in VMAT to 489 and 742 in H-VMAT [19,23]. Similarly, the MU for IMRT was 751, with a treatment time of 75 s to 510 MU and 51 s in H-IMRT [22].
Organs at Risks (OARs)
The tabulated dosimetric data concerning OARs, focusing on lung (ipsilateral and contralateral), heart, and contralateral breast doses, is summarized in Table 3. Overall, hybrid techniques have demonstrated a reduction in OAR doses compared to VMAT or IMRT but not when compared to 3DCRT. In three separate studies, the volume receiving 5 Gy (V5Gy) for the ipsilateral lung was notably higher for VMAT compared to H-VMAT (90.7%, 66.6%, 61.47% vs. 51.45%, 52.4%, 48.84%, respectively). In addition, V5Gy for IMRT was higher than for H-IMRT (36.75% vs. 27.64%, respectively) [19,21,24]. Similarly, V5Gy for the contralateral lung was greater for single-modality approaches compared with the hybrid techniques (VMAT: 35.67% vs. H-VMAT: 0.68% and IMRT: 13.3% vs. H-IMRT: 9.93%) [19,22]. Hybrid techniques were found to be superior in reducing the mean dose (Dmean) of the contralateral breast in all studies comparing methods: VMAT (ranging from 4.2 Gy to 7.1 Gy) versus H-VMAT (ranging from 1.4 Gy to 3.5 Gy) and IMRT (9.1 Gy) versus H-IMRT (4.69 Gy) [19,21-24,26].
Table 3. OAR doses to the lungs, heart, and contralateral breast.
Abbreviations: AP, automated plan; CB, contralateral breast; CL, contralateral lung; FIF, field in field; H-IMRT, hybrid-intensity modulated radiation therapy; H-VMAT, hybrid volumetric arc therapy; IL, ipsilateral lung; L, left; MP-VMAT, manual plan volumetric arc therapy; ns, not statistically different; OAR, organ at risk; R, right; T-VMAT, tangential volumetric arc therapy; VxGy, volume receiving x Gy.
| OARs (P < 0.05) | ||||||
| Authors | Techniques | Ipsilateral Lung | Contralateral Lung | Heart | Contralateral Breast | Conclusion |
| Balaji et al., 2018 [13] | FIF | V5Gy: 41.68% | V5Gy: 0.00% | Dmean: 5.41 Gy | Dmean: 0.54 Gy | H-VMAT is lower in V5Gy lungs and Dmean of heart and CB compared with VMAT. FIF is the lowest in all OARs among all techniques. |
| H-VMAT | V5Gy: 51.45% | V5Gy: 0.68% | Dmean: 6.17 Gy | Dmean: 1.36 Gy | ||
| VMAT | V5Gy: 90.7% | V5Gy: 35.67% | Dmean: 11.51 Gy | Dmean: 4.55 Gy | ||
| Dumane et al., 2018 [25] | VMAT | Dmean: 15.3 Gy | Dmean: 3.6 Gy | V5Gy: 39.0 Gyns | Dmean: 4.2 Gy | H-VMAT reduced the dose to the CL and CB compared with VMAT. Heart is not statistically significant. |
| H-VMAT | Dmean: 16.4 Gy | Dmean: 3.2 Gy | V5Gy: 40.2 Gyns | Dmean: 1.4 Gy | ||
| Lang et al., 2020 [26] | VMAT | V10Gy: 10.3% | V10Gy: 54.9% | Dmean: 3.7 Gy | Dmean: 6.0 Gy | H-VMAT is lower in lung (V10Gy), heart (Dmean) and CB (Dmean) compared with VMAT. |
| H-VMAT | V10Gy: 6.9% | V10Gy: 50.5% | Dmean: 3.0 Gy | Dmean: 3.4 Gy | ||
| Doi et al., 2020 [27] | 3DCRT, | V5Gy: 41.0% | V5Gy: 0.0% | Dmean: 11.8 Gyns | NA | V5Gy of IL and CL are higher in H-VMAT compared with 3DCRT. Heart (Dmean) is not statistically significant. |
| H-VMAT | V5Gy: 47.5% | V5Gy: 28.0% | Dmean: 12.0 Gyns | NA | ||
| Cilla et al., 2021 [21] | H-IMRT | V5Gy: 49.7% | NA | V5Gy: 5.3% | Dmean: 1.3 Gy | H-IMRT is lower in lungs, heart and CB when compared with H-VMAT. Both I-IMRT and H-VMAT is lower in lungs, heart, and CB compared with manual plan VMAT. AP-VMAT is lower in heart. |
| H-VMAT | V5Gy: 52.4% | NA | V5Gy: 6.1% | Dmean: 1.8 Gy | ||
| MP-VMAT | V5Gy: 66.6% | NA | V5Gy: 6.6% | Dmean: 1.9 Gy | ||
| AP- VMAT | V5Gy: 55.7% | NA | V5Gy: 4.1% | Dmean: 2.3 Gy | ||
| Zhang et al., 2022 [23] | T-VMAT | V20Gy: 22.2% | V20Gy: 2.77% | V30Gy: 2.13% | Dmean: 7.1 Gy | Only CB is the lowest in H-VMAT among all. |
| IMRT | V20Gy: 29.6% | V20Gy: 0.17% | V30Gy: 7.15% | Dmean: 3.6 Gy | ||
| H- VMAT | V20Gy: 28.81% | V20Gy: 0.18% | V30Gy: 8.53% | Dmean: 3.5 Gy | ||
| Sathiyaraj et al., 2022 [24] | H-VMAT | V5Gy: 48.84% | Dmean: 2.19 Gy | V30Gy: 3.27% | Dmean: 2.34 Gy | H-VMAT is lower in IL (V5Gy), Dmean of CL and CB. Heart is lower in VMAT. |
| VMAT | V5Gy: 61.47% | Dmean: 3.9 Gy | V30Gy: 2.94% | Dmean: 4.57 Gy | ||
| Haldar et al., 2023 [22] | FIF | V5GY: 29.96% | Dmean: 9.7 Gy | V10Gy: 11.94% | Dmax: 3.67 Gy | H-IMRT is lower in V5Gy lungs and V10Gy heart than IMRT. CB is the lowest in FIF among all. |
| IMRT | V5GY: 36.75% | Dmean: 13.3 Gy | V10Gy: 14.22% | Dmax: 9.19 Gy | ||
| H-IMRT | V5GY: 27.64% | Dmean: 9.93 Gy | V10Gy: 10.55% | Dmax: 4.69 Gy | ||
| Balaji et al., 2023 [20] | 3DCRT+IMRT, | V5Gy: 56.5% | V5Gy: 1.6% | V5Gy: 30.4% | V5Gy: 6.0% | 3DCRT+IMRT and 3DCRT+VMAT are lower in IL and heart. IMRT+VMAT is lower in CB. |
| 3DCRT+VMAT, | V5Gy: 57.3% | V5Gy: 0.6% | V5Gy: 30.6% | V5Gy: 4.4% | ||
| IMRT+VMAT | V5Gy: 60.4% | V5Gy: 0.6% | V5Gy: 41.5% | V5Gy: 3.5% | ||
Discussion
This article is the first systematic review to examine hybrid planning techniques for chest wall irradiation and compare them with other hybrid or non-hybrid techniques. We compared the effectiveness of H-VMAT or H-IMRT and non-hybrid techniques (3DCRT, FIF, IMRT, and VMAT), emphasizing the quality of the treatment plan and the dose to the OARs. Although reports on PTV coverage, CI, HI, and doses to OARs are conflicting, hybrid techniques generally provide better PTV coverage than single modality techniques (3DCRT, IMRT, and VMAT) and result in lower doses to OARs, such as the lungs, heart, and contralateral breast.
In the majority of institutions around the world, 3DCRT is the most popular radiation treatment planning technique for breast cancer [1]. The technique is used in many reviewed studies along with post-mastectomy hybrid planning radiotherapy [19-21,23-27]. In those investigations, 3DCRT was used either with two open tangential fields or two tangential FIF [19,22,27]. These tangential beams avoid exposing the ipsilateral lung and heart to low-dose radiation, but they have poor conformance and homogeneity [2]. Due to the target’s conformance, IMRT and VMAT are now frequently recommended approaches over 3DCRT for pelvic malignancies, prostate cancer, and head and neck tumors [6]. With regard to postmastectomy breast radiation, there is considerable discussion on using these methods. The importance of IMRT alone or in combination with other approaches for chest wall irradiation was demonstrated in some studies [20,22]. According to reports, IMRT doubles the likelihood of developing subsequent cancer compared with 3DCRT [28,29]. As a result, several studies used VMAT alone or in combination with other planning modalities [19,20,23-27], possibly due to shorter treatment times and MU, which reduces the total exposure and potentially reduces the risk of radiation-induced secondary tumors [6].
Some institutions are conducting ongoing trials of hybrid techniques, while others are already in operation [21]. This review shows that there are different suggested hybrid techniques for chest wall irradiation, which are a combination of either 3DCRT (OF or FIF) + VMAT [19,20,22-27] or 3DCRT (OF or FIF) + IMRT [20,22,24]; three studies have used IMRT+VMAT [20,23,24].
It is evident from some studies that the H-VMAT (3DCRT+VMAT or FIF+VMAT or IMRT+VMAT) is superior in providing conformity, uniformity, and dose reduction to OARs compared with VMAT alone or FIF [19-24,26]. However, only two studies claimed that the PTV coverage maintained the same quality as VMAT alone [25,27]. One study compared H-IMRT (3DCRT+IMRT) with H-VMAT (3DCRT +VMAT) and H-VMAT (IMRT +VMAT) and concluded that H-VMAT (3DCRT +VMAT) is superior [20]. Another study compared H-IMRT (3DCRT+IMRT) with IMRT alone and 3DCRT and stated that H-IMRT is the best option for homogeneity and dose distributions [22].
IMRT for breast cancer is limited by uncertainties in patient setup and respiratory motion causing unexpected dose deviations [30]. The H-IMRT plan may eliminate the geometrical errors associated with IMRT by combining two opposed tangential open beams with IMRT beams. In terms of robustness against uncertainty and plan quality, H-IMRT outperformed the non-hybrid IMRT [30]. Many challenges in treating the chest wall area must be considered in determining the optimal planning technique. The physical characteristics of patients can vary between individuals, in terms of the size and volume of the PTV, chest wall separation, heart volume and position, and lung volume [19]. In addition, age, breathing motion, and daily setup reproducibility further contribute to the challenges encountered in planning cases involving the chest wall [2].
Beam weighting refers to the process of assigning different weights to the technique involved. It serves as an additional selection criterion after identifying the optimal technique. Balaji et al. [19] demonstrated that H-VMAT with beam weighting (80-90% of 3DCRT and 10-20% of VMAT) is the optimal choice based on its correlation with mean dose, V5Gy, and V20Gy of the heart and lung, as well as the lower incidence of secondary cancers resulting from low-dose irradiation. Furthermore, several other studies [23,25,26] have provided support for the superiority of the beam-weighting methods described by Balaji et al. [19].
This review highlights various suggested techniques for chest wall radiation. Utilizing newer techniques, such as IMRT/VMAT, which aim to achieve good PTV coverage, may increase low-dose irradiation to OARs compared with traditional 3DCRT plans. In addition, when the internal mammary chain is involved in the treatment of the chest wall area, it poses an increased risk to the heart. However, IMRT and VMAT are preferred over other techniques due to their ability to create concave dose distributions for the internal mammary chain [31].
Studies have reported that the risk of coronary artery disease is reduced with doses ≤30 Gy, indicating that V25Gy should be less than 10% [32]. Furthermore, it has been observed that the incidence of coronary events increases by 7.4 per 1 Gy increase in the mean heart dose [33]. In most studies, hybrid techniques (H-VMAT, H-IMRT) had lower heart doses than VMAT or IMRT [13-18,20], but some studies reported no statistically significant difference [25,27]. However, these latter studies included both breast and chest wall patients, which could affect the final result. One study performed an automated plan of VMAT and found statistical differences in the doses to the heart compared with the manual VMAT plan, H-IMRT, and H-VMAT [21]. Radiation-induced pneumonitis can be caused by radiation doses to the lungs on the same side [34]. Achieving optimal lung health requires exceptional care in optimizing both sides of the lungs. With free-breathing or DIBH settings, H-VMAT performs better [19-21,23,24,26]. Two studies of breast mastectomy showed that in a comparison between H-VMAT and H-IMRT, H-IMRT was better in V5Gy [20,21]. Similarly, in a comparison of IMRT with H-IMRT, the V5Gy and V10Gy of ipsilateral lung were smaller in H-IMRT than in IMRT and FIF [22]. The parameters V5Gy, V10Gy, and V20Gy of the ipsilateral lung are known as predictors of radiation-induced pneumonitis, but the most effective predictor among these parameters has been debated in several studies [34]. H-VMAT was shown to be considerably reduced in Dmean, V5Gy, and V20Gy in several investigations [19,23-27].
In addition, it is essential to note that advanced techniques carry a potential risk to the contralateral breast. Ignoring this factor during the planning process may result in radiation-induced carcinogenesis [35]. The Dmean of the contralateral breast is less with the hybrid technique (H-VMAT; either 3DCRT+VMAT or IMRT+VMAT) than with the non-hybrid technique (VMAT) [19,23-26]. Only one study reported no radiation to the contralateral breast when using a hybrid technique as no VMAT was used over the chest area [27]. The Dmean of H-IMRT was reported to be better than that of H-VMAT [21]. Similarly, in comparison with IMRT [22], both H-VMAT and H-IMRT had lower doses to the contralateral breast in comparison with VMAT alone [21].
It has been reported that the more MU delivered to the target, the higher the dose to normal tissues and the greater the incidence of radiation-induced malignancies [6]. Although four of the studies reviewed did not report details on MU, H-VMAT or H-IMRT had a smaller MU than the other techniques [19,20,22,23]. In terms of treatment time, H-VMAT was found to have comparatively less time than IMRT or VMAT [22,36]. The shorter time brought more comfort to the patients, especially in DIBH settings, increasing reproducibility and reducing setup errors.
The dosimetric parameters for both PTV and OARs varied between studies, and the field involvement of hybrid techniques also differed. Some studies only addressed certain combinations of modalities for chest walls and regional nodes. Furthermore, many studies did not report on crucial factors, such as CI, HI, and MU alongside treatment time. Due to these inconsistencies, it is challenging to come to a definitive conclusion.
Maintaining a consistent approach to dose prescription, target volume, and dose constraints is essential when reporting on breast radiotherapy treatment plans. In cases in which both sides of the breast are treated, it is vital to evaluate each side individually or to assess the heart doses if possible. Determining the breathing pattern is highly recommended for the precise evaluation of OAR structures. In addition, a larger population is needed to achieve more accurate and reliable outcomes.
Conclusions
The hybrid planning technique is potentially valuable in the treatment of postmastectomy breast irradiation. However, few comparative dosimetric studies of chest wall volumes and nodal volumes have been addressed in existing research. Further investigation of combining availability modalities is needed with the use of automated plans for chest wall patients. Since the studies did not use flattening filter-free beams for chest wall irradiation, further investigation comparing 3DCRT+IMRT, 3DCRT+VMAT, and IMRT+VMAT is needed. In addition, no long-term clinical outcome studies have been conducted in patients treated with hybrid procedures, necessitating in-depth prospective research to investigate the benefits of the hybrid approaches.
Appendices
Online search of PubMed and Scopus databases
( TITLE-ABS-KEY ( breast AND cancer ) OR TITLE-ABS-KEY ( breast AND carcinoma ) ) AND ( TITLE-ABS-KEY ( radiotherapy ) OR TITLE-ABS-KEY ( radiation AND therapy ) ) AND ( TITLE-ABS-KEY ( hybrid AND plan ) OR TITLE-ABS-KEY ( integrated AND plan ) OR TITLE-ABS-KEY ( combined AND plan ) ) AND ( TITLE-ABS-KEY ( oars ) OR TITLE-ABS-KEY ( organs AND at AND risk ) OR TITLE-ABS-KEY ( lung ) OR TITLE-ABS-KEY ( heart ) OR TITLE-ABS-KEY ( surrounding AND organs ) )
Scopus: 272 documents
Search: ((((breast cancer) OR (breast carcinoma)) AND ((radiotherapy) OR (radiation therapy))) AND (((hybrid plan) OR (Integrated plan)) OR (Combined technique))) AND (((((OARs) OR (Organ at risks)) OR (Surrounding organs)) OR (heart)) OR (lung))
PubMed: 1,307 documents
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Zainab Alsaihaty, Noorazrul Yahya, Hanani Abdul Manan
Acquisition, analysis, or interpretation of data: Zainab Alsaihaty, Noorazrul Yahya, Hanani Abdul Manan, Akmal Sabarudin
Drafting of the manuscript: Zainab Alsaihaty
Critical review of the manuscript for important intellectual content: Zainab Alsaihaty, Noorazrul Yahya, Hanani Abdul Manan, Akmal Sabarudin
Supervision: Noorazrul Yahya
References
- 1.A new three-dimensional conformal radiotherapy (3DCRT) technique for large breast and/or high body mass index patients: evaluation of a novel fields assessment aimed to reduce extra-target-tissue irradiation. Gerardina S, Edy I, Sonia S, et al. Br J Radiol. 2016;89:20160039. doi: 10.1259/bjr.20160039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Radiation therapy for breast cancer: Literature review. Balaji K, Subramanian B, Yadav P, Anu Radha C, Ramasubramanian V. Med Dosim. 2016;41:253–257. doi: 10.1016/j.meddos.2016.06.005. [DOI] [PubMed] [Google Scholar]
- 3.A new homogeneity index definition for evaluation of radiotherapy plans. Yan L, Xu Y, Chen X, Xie X, Liang B, Dai J. J Appl Clin Med Phys. 2019;20:50–56. doi: 10.1002/acm2.12739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dose-volume constraints for organs at risk In radiotherapy (CORSAIR): an ‘all-in-one’ multicenter-multidisciplinary practical summary. Bisello S, Cilla S, Benini A, et al. Curr Oncol. 2022;29:7021–7050. doi: 10.3390/curroncol29100552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Intensity modulated radiation therapy: a review of current practice and future outlooks. . ur Rehman J, Ahmad N, Khalid M, et al. J Radiat Res Appl Sci. 2018;11:361–367. [Google Scholar]
- 6.Volumetric modulated arc therapy: a review of current literature and clinical use in practice. Teoh M, Clark CH, Wood K, Whitaker S, Nisbet A. Br J Radiol. 2011;84:967–996. doi: 10.1259/bjr/22373346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Risk of contralateral breast and ipsilateral lung cancer induction from forward-planned IMRT for breast carcinoma. Mazonakis M, Stratakis J, Lyraraki E, Damilakis J. Phys Med. 2019;60:44–49. doi: 10.1016/j.ejmp.2019.03.021. [DOI] [PubMed] [Google Scholar]
- 8.Planning hybrid intensity modulated radiation therapy for whole-breast irradiation. Farace P, Zucca S, Solla I, et al. Int J Radiat Oncol Biol Phys. 2012;84:0–22. doi: 10.1016/j.ijrobp.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 9.Clinical experience with image-guided radiotherapy in an accelerated partial breast intensity-modulated radiotherapy protocol. Leonard CE, Tallhamer M, Johnson T, et al. Int J Radiat Oncol Biol Phys. 2010;76:528–534. doi: 10.1016/j.ijrobp.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 10.Deep inspiration breath hold technique reduces heart dose from radiotherapy for left-sided breast cancer. Hayden AJ, Rains M, Tiver K. J Med Imaging Radiat Oncol. 2012;56:464–472. doi: 10.1111/j.1754-9485.2012.02405.x. [DOI] [PubMed] [Google Scholar]
- 11.Dosimetric evaluation of breast radiotherapy in a dynamic phantom. Menon G, Pudney D, Smith W. Phys Med Biol. 2011;56:7405–7418. doi: 10.1088/0031-9155/56/23/005. [DOI] [PubMed] [Google Scholar]
- 12.Hybrid IMRT plans--concurrently treating conventional and IMRT beams for improved breast irradiation and reduced planning time. Mayo CS, Urie MM, Fitzgerald TJ. Int J Radiat Oncol Biol Phys. 2005;61:922–932. doi: 10.1016/j.ijrobp.2004.10.033. [DOI] [PubMed] [Google Scholar]
- 13.Ultrasonographic evaluation of skin toxicity following radiotherapy of breast cancer: a systematic review. Hussein FA, Manan HA, Mustapha AW, Sidek K, Yahya N. Int J Environ Res Public Health. 2022;19 doi: 10.3390/ijerph192013439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Automated hybrid volumetric modulated arc therapy (HVMAT) for whole-breast irradiation with simultaneous integrated boost to lumpectomy area : a treatment planning study. Cilla S, Romano C, Macchia G, et al. Strahlenther Onkol. 2022;198:254–267. doi: 10.1007/s00066-021-01873-3. [DOI] [PubMed] [Google Scholar]
- 15.The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Page MJ, McKenzie JE, Bossuyt PM, et al. BMJ. 2021;372:0. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Delta-radiomics-based models for toxicity prediction in radiotherapy: a systematic review and meta-analysis. Tan D, Mohamad Salleh SA, Manan HA, Yahya N. J Med Imaging Radiat Oncol. 2023;67:564–579. doi: 10.1111/1754-9485.13546. [DOI] [PubMed] [Google Scholar]
- 17.Toxicity profile of patients treated with proton and carbon-ion therapy for primary nasopharyngeal carcinoma: a systematic review and meta-analysis. Yahya N, Mohamad Salleh SA, Mohd Nasir NF, Abdul Manan H. Asia Pac J Clin Oncol. 2024;20:240–250. doi: 10.1111/ajco.13915. [DOI] [PubMed] [Google Scholar]
- 18.Role of resting-state functional MRI in detecting brain functional changes following radiotherapy for head and neck cancer: a systematic review and meta-analysis. Voon NS, Manan HA, Yahya N. Strahlenther Onkol. 2023;199:706–717. doi: 10.1007/s00066-023-02089-3. [DOI] [PubMed] [Google Scholar]
- 19.Hybrid volumetric modulated arc therapy for chest wall irradiation: for a good plan, get the right mixture. Balaji K, Yadav P, BalajiSubramanian S, Anu Radha C, Ramasubramanian V. Phys Med. 2018;52:86–92. doi: 10.1016/j.ejmp.2018.06.641. [DOI] [PubMed] [Google Scholar]
- 20.Accelerated hypofractionated radiotherapy for chest wall and nodal irradiation using hybrid techniques. Balaji K, Ramasubramanian V. J Radiother Pract. 2023;22:21. [Google Scholar]
- 21.Challenges in lung and heart avoidance for postmastectomy breast cancer radiotherapy: Is automated planning the answer? Cilla S, Macchia G, Romano C, et al. Med Dosim. 2021;46:295–303. doi: 10.1016/j.meddos.2021.03.002. [DOI] [PubMed] [Google Scholar]
- 22.The feasibility of hybrid IMRT treatment planning for left sided chest wall irradiation: a comparative treatment planning study. Haldar S, Saroj DK, Dixit A, Sarkar B, Yadav S. Iran J Med Phys. 2023;20:31–41. [Google Scholar]
- 23.Evaluation of hybrid VMAT advantages and robustness considering setup errors using surface guided dose accumulation for Internal lymph mammary nodes irradiation of postmastectomy radiotherapy. Zhang Z, Li D, Peng F, et al. Front Oncol. 2022;12:907181. doi: 10.3389/fonc.2022.907181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dosimetric evaluation of hybrid and volumetric-modulated arc therapy plan for left-sided chest wall irradiation in MONACO treatment planning system. Sathiyaraj P, Manikandan PS, Varatharaj C, Ganesh KM, Sathiyan S, Ravikumar M. J Cancer Res Ther. 2022;18:1728–1732. doi: 10.4103/jcrt.JCRT_707_20. [DOI] [PubMed] [Google Scholar]
- 25.Dose to organs in the supraclavicular region when covering the internal mammary nodes (IMNs) in breast cancer patients: a comparison of volumetric modulated arc therapy (VMAT) versus 3D and VMAT. Dumane VA, Bakst R, Green S. PLoS One. 2018;13:0. doi: 10.1371/journal.pone.0205770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dosimetric comparison between volumetric-modulated arc therapy and a hybrid volumetric-modulated arc therapy and segmented field-in-field technique for postmastectomy chest wall and regional lymph node irradiation. Lang K, Loritz B, Schwartz A, et al. Med Dosim. 2020;45:121–127. doi: 10.1016/j.meddos.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 27.Hybrid volumetric-modulated arc therapy for postoperative breast cancer including regional lymph nodes: the advantage of dosimetric data and safety of toxicities. Doi Y, Nakao M, Miura H, Ozawa S, Kenjo M, Nagata Y. J Radiat Res. 2020;61:747–754. doi: 10.1093/jrr/rraa057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Radiation-induced second cancers: the impact of 3D-CRT and IMRT. Hall EJ, Wuu C. Int J Radiat Oncol Biol Phys. 2003;56:83–88. doi: 10.1016/s0360-3016(03)00073-7. [DOI] [PubMed] [Google Scholar]
- 29.Intensity-modulated radiation therapy: a review with a physics perspective. Cho B. Radiat Oncol J. 2018;36:1–10. doi: 10.3857/roj.2018.00122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Evaluation of robustness in hybrid intensity-modulated radiation therapy plans generated by commercial software for automated breast planning. Mizuno N, Yamauchi R, Kawamori J, et al. Sci Rep. 2022;12:1418. doi: 10.1038/s41598-022-05538-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heart sparing radiotherapy techniques in breast cancer: a focus on deep inspiration breath hold. Stowe HB, Andruska ND, Reynoso F, Thomas M, Bergom C. Breast Cancer (Dove Med Press) 2022;14:175–186. doi: 10.2147/BCTT.S282799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Radiation dose-volume effects in the heart. Gagliardi G, Constine LS, Moiseenko V, Correa C, Pierce LJ, Allen AM, Marks LB. Int J Radiat Oncol Biol Phys. 2010;76:0–85. doi: 10.1016/j.ijrobp.2009.04.093. [DOI] [PubMed] [Google Scholar]
- 33.Risk of ischemic heart disease in women after radiotherapy for breast cancer. Darby SC, Ewertz M, McGale P, et al. N Engl J Med. 2013;368:987–998. doi: 10.1056/NEJMoa1209825. [DOI] [PubMed] [Google Scholar]
- 34.A dosimetric comparison of volumetric modulated arc therapy and intensity modulated radiotherapy in patients treated with post-mastectomy radiotherapy. Adeneye S, Akpochafor M, Adedewe N, et al. Eur J Breast Health. 2023;19:92–98. doi: 10.4274/ejbh.galenos.2022.2022-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Intensity-modulated radiation therapy, protons, and the risk of second cancers. Hall EJ. Int J Radiat Oncol Biol Phys. 2006;65:1–7. doi: 10.1016/j.ijrobp.2006.01.027. [DOI] [PubMed] [Google Scholar]
- 36.Multibeam inverse intensity-modulated radiotherapy (IMRT) for whole breast irradiation: a single center experience in China. Yang Z, Zhang L, Chen X, et al. Oncotarget. 2015;6:35063–35072. doi: 10.18632/oncotarget.5278. [DOI] [PMC free article] [PubMed] [Google Scholar]