Abstract
AIM
To evaluate the effect of low-degree astigmatism on objective visual quality through the Optical Quality Analysis System (OQAS).
METHODS
This study enrolled 46 participants (aged 23 to 30y, 90 eyes) with normal or corrected-to-normal vision. The cylindrical lenses (0, 0.5, 0.75, 1.0, and 1.25 D) were placed at the axial direction (180°, 45°, 90°, and 135°) in front of the eyes with the best correction to form 16 types of regular low-degree astigmatism. OQAS was used to detect the objective visual quality, recorded as the objective scattering index (OSI), OQAS values at contrasts of 100%, 20%, and 9% predictive visual acuity (OV100%, OV20%, and OV9%), modulation transfer function cut-off (MTFcut-off) and Strehl ratio (SR). The mixed effect linear model was used to compare objective visual quality differences between groups and examine associations between astigmatic magnitude and objective visual quality parameters.
RESULTS
Apparent negative relationships between the magnitude of low astigmatism and objective visual quality were observed. The increase of OSI per degree of astigmatism at 180°, 45°, 90°, and 135° axis were 0.38 (95%CI: 0.35, 0.42), 0.50 (95%CI: 0.46, 0.53), 0.49 (95%CI: 0.45, 0.54) and 0.37 (95%CI: 0.34, 0.41), respectively. The decrease of MTFcut-off per degree of astigmatism at 180°, 45°, 90°, and 135° axis were -10.30 (95%CI: -11.43, -9.16), -12.73 (95%CI: -13.62, -11.86), -12.75 (95%CI: -13.79, -11.70), and -9.97 (95%CI: -10.92, -9.03), respectively. At the same astigmatism degree, OSI at 45° and 90° axis were higher than that at 0° and 135° axis, while MTFcut-off were lower.
CONCLUSION
Low astigmatism of only 0.50 D can significantly reduce the objective visual quality.
Keywords: low-degree astigmatism, objective visual quality, Optical Quality Analysis System
INTRODUCTION
With the continuous improvement of ophthalmic surgery technology and advances in measurement equipment, cataract surgery has gradually developed from initial vision surgery to refractive cataract surgery for better visual quality. However, the residual postoperative astigmatism will still affect the postoperative vision and visual quality[1]–[2].
Human eye astigmatism mainly comes from the cornea and lens[3]–[4]. Previous studies have found that about 86.6% of cataract patients had preoperative corneal astigmatism, among whom about 40% had preoperative corneal astigmatism ≥1.0 D and about 20% had preoperative corneal astigmatism ≥1.5 D[5]. Low-degree astigmatism of 0.50-0.99 D is the most common distribution range of corneal astigmatism before cataract surgery, with a proportion up to 30.08%[6]. Most studies believe that for high-degree regular corneal astigmatism, implantation of astigmatism corrective intraocular lens can significantly improve postoperative vision[7]–[8]. However, there is still a controversial argument about whether patients with low astigmatism need to correct corneal astigmatism by astigmatism intraocular lens implantation. Most ophthalmologists suggest that cataract patients with regular corneal astigmatism of 0.50 D or less may not require correction. Still, those with regular corneal astigmatism of 1.00 D or more and value glasses independence may consider using Toric intraocular lenses to correct[9]–[11]. Recent studies have found that for cataract patients with preoperative low-degree astigmatism (0.10 to 0.75 D), the use of low astigmatism intraocular lens has lower postoperative residual astigmatism and better uncorrected visual acuity than non-astigmatism intraocular lens, particularly with against-the-rule (ATR) astigmatism[12]–[14]. Previous studies on the impact of low-degree astigmatism on objective visual quality are mostly limited to patients after cataract surgery. The effects of the operation, such as surgical incision and duration, on visual quality cannot be excluded entirely. In addition, there has not been a large sample size study on the effect of low-degree astigmatism with different degrees and axes on objective visual quality.
This study aims to evaluate the objective effects of low-degree astigmatism on visual quality through the Objective Visual Quality Detection System (OQAS) by placing cylindrical lenses (0, 0.5, 0.75, 1.0, and 1.25 D) at the axial direction (180°, 45°, 90°, and 135°) in front of the eyes to simulate the state of low-degree astigmatism.
SUBJECTS AND METHODS
Ethical Approval
This clinical study followed the principles of the Declaration of Helsinki and was approved by the Ethical Review Board of the Optometry Hospital Affiliated with Wenzhou Medical University (Batch No.2023-096-K-81). Each participant signed a written informed agreement before the study.
This is an observational and cross-sectional study. Participants were enrolled from patients presenting to the Optometry Hospital affiliated with Wenzhou Medical University from July to October 2020. The inclusion criteria were: 1) aged 18-30 years old; 2) emmetropia or low to moderate refractive errors (spherical diopters: -5.0 to +0.50 D, cylindrical diopters: -1.50 to 0 D); 3) the best corrected visual acuity (BCVA) was 20/20 or better. The exclusion criteria were: 1) patients with high myopia, high hypermetropia, or anisometropia; 2) previous history of ocular surgery or lesions, including cataracts, glaucoma, or other ocular surface diseases; 3) poor fixation or unable to cooperate.
All participants underwent detailed ophthalmological examination, including subjective refraction, slit lamp examination, tear film break-up time (BUT), and fundoscopy. BCVA was tested by tumbling the “E” chart. The spherical equivalent refraction (SE) was calculated as the sum of the spherical diopters and half of the cylindrical diopters. The double-pass OQAS (Visiometrics S.L., Tarrasa, Spain) was applied to measure the objective visual quality, recorded as the objective scattering index (OSI), modulation transfer function cut-off (MTFcut-off), Strehl ratio (SR), OQAS values (OV: OV100%, OV20%, and OV9%). OSI was calculated by the ratio of the peripheral light energy to the central light energy of the retinal image. The higher OSI value indicated worse ocular scattering. MTFcut-off, SR, and OV values were parameters related to MTF, which can be directly computed from the acquired retinal images. MTFcut-off referred to the intercept between the MTF curve and the X-axis, indicating the highest spatial frequency under the condition of the lowest contrast. Generally, when the MTFcut-off value is 30 cycles/degree, the corresponding visual acuity is 20/20. SR was the ratio of the area under the MTF curve of the measured eye to the ideal aberration-free eye. OV values (OV100%, OV20%, and OV9%) represented the predictive visual acuity at contrasts of 100%, 20%, and 9%, as three spatial frequencies responding to the MTF divided by 30 cycles/degree for three contrast levels. The lower values of MTFcut-off, SR, OV100%, OV20%, and OV9% indicated worse optical visual quality. All measurements were performed by an experienced ophthalmologist. To obtain the mean value, twice measurements (six consecutively collecting each time) were performed for each parameter of both eyes.
The built-in refractor of OQAS can correct the refractive error of -8 to 6 D and the astigmatism degree of 0.50 D or less. A cylindrical lens should be added to correct patients with astigmatism degrees greater than 0.50 D. All eyes with the best correction were set as the control group without astigmatism for comparison. Based on this, regular astigmatism was formed by placing cylindrical lenses of four magnitudes (0.50, 0.75, 1.0, 1.25 D) and four axis orientations (180°, 45°, 90°, 135°) in front of the eyes, i.e., 16 combinations of astigmatic magnitude and axis orientation. This design enables a comprehensive evaluation by simulating varying degrees and axes of low-degree astigmatism, with a control group that does not have astigmatism for comparison. During the dark phase, all eye pupils were larger than 4.0 mm, and the examinations were conducted using a 4.0-mm artificial pupil. During the measurement, volunteers were instructed to fixate on the built-in visual target of the OQAS. All measurements were performed by an experienced ophthalmologist in a dark room. All eyes were asked to fixate on the built-in visual target of the OQAS and have 30s of rest before each scan to ensure accuracy and reproducibility. Twice measurements were performed for each parameter of both eyes consecutively to obtain the mean value.
All statistical analyses were conducted by SAS software version 9.1.4 (SAS Institute Inc., Cary, NC, USA) and RStudio (Copyright©2009-2019 RStudio, Inc.). Normally distributed variables were described as mean±standard deviation, while skewed data would be expressed as median (1st quartile, 3rd quartile). The correlation between variables was performed by Spearman analysis. Since we included binocular data of the same person (two eyes of one person were related generally), the mixed effect linear model was applied to compare differences in objective visual quality between groups and investigate associations between astigmatic magnitude and objective visual quality parameters. All tests were two-sided, and the significance level was P<0.05.
RESULTS
A total of 90 eyes of 46 participants [aged from 23 to 30y, 25.0 (24.0, 25.0)] were included. All the eyes were divided into three groups by refractive error: emmetropia (+0.50≥SE≥-0.25 D, 17 eyes), mild myopia (-0.25>SE≥-3.00 D, 48 eyes), and moderate myopia (-3.00 D>SE≥-6.00 D, 25 eyes). The BUT and objective visual quality of all eyes with the best correction are shown in Table 1.
Table 1. The characteristics of the objective visual quality of all eyes with the best correction.
| Variables | ALL (n=90) | Emmetropia (n=17) | Mild myopia (n=48) | Moderate myopia (n=25) | P a |
| BUT (s) | 5.00 (5.00, 6.00) | 5.00 (5.00, 5.00) | 5.00 (5.00, 6.00) | 5.00 (5.00, 6.00) | 0.3486 |
| OSI | 0.38 (0.25, 0.60) | 0.30 (0.25, 0.40) | 0.40 (0.25, 0.55) | 0.55 (0.30, 0.75) | 0.0603 |
| MTFcut-off | 44.66 (38.8, 50.01) | 43.04 (38.80, 49.09) | 44.66 (39.17, 49.22) | 45.07 (36.33, 51.21) | 0.9897 |
| SR | 0.24±0.05 (0.12-0.33) | 0.25±0.05 (0.15-0.31) | 0.25±0.05 (0.14-0.33) | 0.23±0.05 (0.12-0.33) | 0.3307 |
| OV100% | 1.50 (1.30, 1.65) | 1.45 (1.30, 1.65) | 1.48 (1.30, 1.65) | 1.50 (1.20, 1.70) | 0.9572 |
| OV20% | 1.10±0.25 (0.60-1.55) | 1.11±0.25 (0.65-1.50) | 1.11±0.25 (0.60-1.55) | 1.07±0.27 (0.60-1.45) | 0.8022 |
| OV9% | 0.67±0.17 (0.30-1.00) | 0.69±0.15 (0.40-0.90) | 0.68±0.17 (0.30-1.00) | 0.63±0.18 (0.30-0.90) | 0.5066 |
aThe mixed effect linear model was applied to compare the difference among the three groups: emmetropia (+0.50≥SE≥-0.25 D), mild myopia (-0.25>SE≥-3.00 D), and moderate myopia (-3.00>SE≥-6.00 D). BUT: Break-up time; OSI: Scattering index; MTFcut-off: Modulation transfer function cut-off; SR: Strehl ratio; OV100%: The predictive visual acuity at contrasts of 100%; OV20%: The predictive visual acuity at contrasts of 20%; OV9%: The predictive visual acuity at contrasts of 9%; SE: Spherical equivalent refraction. Normally distributed variables were described as mean±standard deviation (range), while skewed data was expressed as median (1st quartile, 3rd quartile).
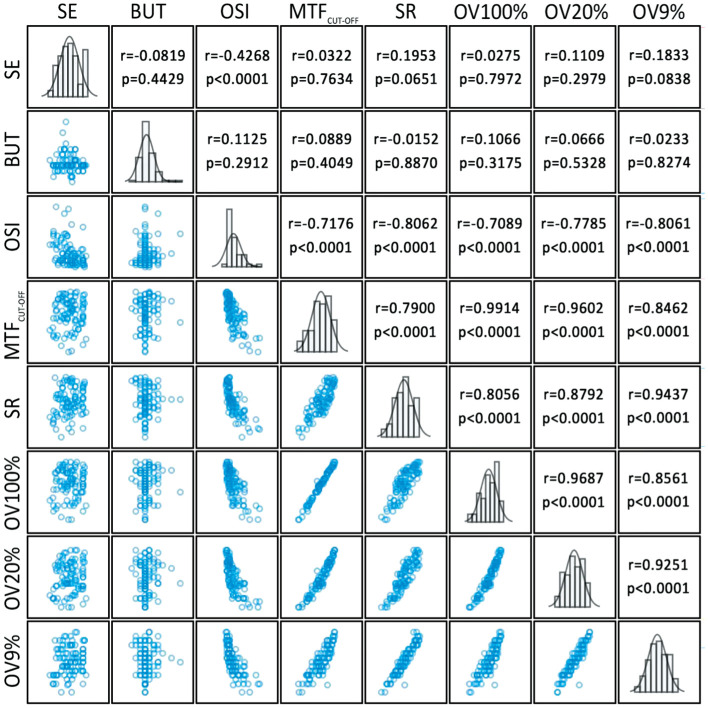
The difference of BUT, OSI, MTFcut-off, SR, OV100%, OV20%, and OV9% among the three groups was not significant (P>0.05). A scatterplot matrix was drawn to show the correlation between these analyzed variables in Figure 1. Tear film BUT did not significantly correlate with the six objective visual quality parameters.
Figure 1. Scatterplot matrix showing the associations between SE, BUT, and parameters of objective visual quality.
SE: Spherical equivalent refraction; BUT: Break-up time; OSI: Scattering index; MTFcut-off: Modulation transfer function cut-off; SR: Strehl ratio; OV100%: The predictive visual acuity at contrasts of 100%; OV20%: The predictive visual acuity at contrasts of 20%; OV9%: The predictive visual acuity at contrasts of 9%.
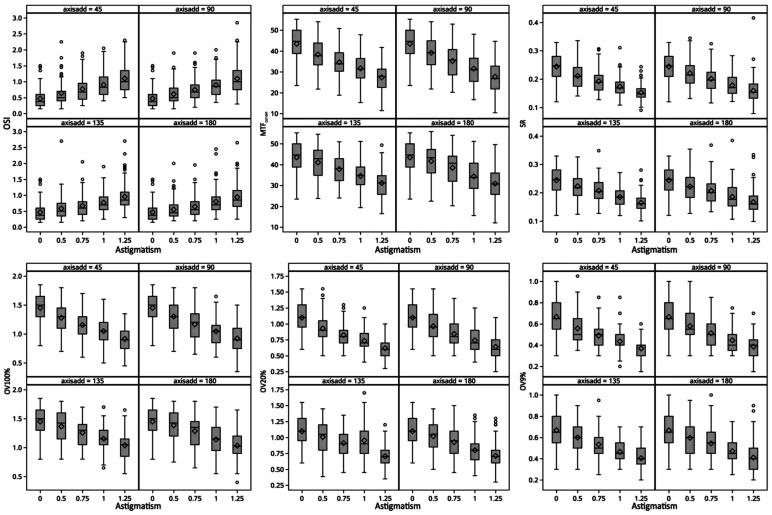
The objective visual quality parameters of 16 types of regular low-degree astigmatism are shown in Table 2 and Figure 2. Apparent negative relationships between the magnitude of low astigmatism and objective visual quality were observed. While astigmatic magnitude had significant main effects on all six objective visual quality parameters (OSI, MTFcut-off, SR, OV100%, OV20%, and OV9%; all P<0.001), astigmatic orientation showed a significant impact on three objective visual quality parameters (MTFcut-off, OV100%, and OV20%; all P<0.05). There was no significant difference in MTFcut-off for the axis oriented at 45° vs 90° and 135° vs 180° (0.50 D: P=0.4921 and P=0.6016; 0.75 D: P=0.5904 and P=0.5410; 1.00 D: P=0.8932 and P=0.8159; 1.25 D: P=0.7768 and P=0.8065); and the difference of MTFcut-off between the remaining axes was statistically significant (45° vs 135°, 45° vs 180°, 90° vs 135°, and 90° vs 180°, all P<0.05). When the astigmatic magnitude was 0.50 D or 0.75 D, astigmatic orientation had no statistically significant effect on OSI (P=0.3864 or P=0.0558). When the astigmatic magnitude was 1.00 D or 1.25 D, astigmatic orientation showed a statistically significant impact on OSI (P=0.0355 or P=0.0201).
Table 2. The objective visual quality parameters of 16 types of regular low-degree astigmatism.
| Variables | 45° | 90° | 135° | 180° | P a |
| OSI | |||||
| 0.50 D | 0.50 (0.40, 0.70) | 0.50 (0.40, 0.80) | 0.50 (0.35, 0.75) | 0.45 (0.35, 0.70) | 0.3864 |
| 0.75 D | 0.68 (0.45, 0.95) | 0.68 (0.50, 0.90) | 0.60 (0.40, 0.80) | 0.55 (0.40, 0.80) | 0.0558 |
| 1.00 D | 0.83 (0.60, 1.15) | 0.85 (0.60, 1.05) | 0.70 (0.55, 0.95) | 0.70 (0.55, 0.95) | 0.0355 |
| 1.25 D | 1.00 (0.75, 1.35) | 1.00 (0.75, 1.35) | 0.85 (0.70, 1.10) | 0.85 (0.65, 1.15) | 0.0201 |
| P | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |
| MTFcut-off | |||||
| 0.50 D | 37.73 (33.39, 43.87) | 39.22 (33.46, 44.94) | 42.88 (34.84, 46.93) | 43.32 (36.03, 47.30) | 0.0115 |
| 0.75 D | 33.86 (30.33, 39.20) | 35.71 (28.58, 40.74) | 38.09 (32.35, 42.90) | 40.67 (32.03, 44.07) | 0.0004 |
| 1.00 D | 31.34 (27.09, 36.39) | 31.02 (25.44, 36.54) | 34.79 (30.41.38.87) | 33.86 (28.59, 40.70) | 0.0024 |
| 1.25 D | 27.83 (22.54, 31.33) | 26.79 (21.80, 32.77) | 31.25 (25.74, 34.71) | 30.72 (25.72, 35.98) | 0.0001 |
| P | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |
| SR | |||||
| 0.50 D | 0.21±0.05 (0.14-0.34) | 0.22±0.05 (0.13-0.34) | 0.22±0.05 (0.12-0.33) | 0.22±0.05 (0.13-0.35) | 0.2851 |
| 0.75 D | 0.19±0.04 (0.13-0.31) | 0.20±0.04 (0.12-0.33) | 0.21±0.04 (0.13-0.35) | 0.21±0.05 (0.13-0.37) | 0.0695 |
| 1.00 D | 0.17±0.03 (0.11-0.31) | 0.18±0.04 (0.12-0.28) | 0.19±0.03 (0.12-0.27) | 0.19±0.05 (0.11-0.38) | 0.1032 |
| 1.25 D | 0.15±0.03 (0.09-0.24) | 0.16±0.04 (0.08-0.42) | 0.16±0.03 (0.10-0.28) | 0.17±0.04 (0.10-0.33) | 0.0511 |
| P | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |
| OV100% | |||||
| 0.50 D | 1.30 (1.10, 1.45) | 1.30 (1.10, 1.50) | 1.42 (1.15, 1.60) | 1.42 (1.20, 1.60) | 0.0206 |
| 0.75 D | 1.15 (1.00, 1.30) | 1.20 (0.95, 1.35) | 1.30 (1.05, 1.40) | 1.35 (1.05, 1.45) | 0.0003 |
| 1.00 D | 1.05 (0.90, 1.20) | 1.05 (0.85, 1.15) | 1.15 (1.05.1.30) | 1.15 (0.95, 1.35) | 0.0016 |
| 1.25 D | 0.90 (0.75, 1.05) | 0.90 (0.75, 1.10) | 1.05 (0.85, 1.15) | 1.03 (0.90, 0.20) | <0.0001 |
| P | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |
| OV20% | |||||
| 0.50 D | 0.93±0.23 (0.50-1.55) | 0.96±0.25 (0.50-1.55) | 1.01±0.23 (0.39-1.45) | 1.02±0.24 (0.50-1.45) | 0.0413 |
| 0.75 D | 0.82±0.18 (0.50-1.30) | 0.84±0.22 (0.50-1.40) | 0.91±0.19 (0.45-1.35) | 0.93±0.22 (0.45-1.50) | 0.0012 |
| 1.00 D | 0.74±0.17 (0.40-1.25) | 0.74±0.19 (0.40-1.25) | 0.95±0.25 (0.45-1.70) | 0.80±0.21 (0.40-1.35) | <0.0001 |
| 1.25 D | 0.62±0.14 (0.30-1.00) | 0.64±0.18 (0.25-1.10) | 0.70±0.17 (0.35-1.20) | 0.71±0.21 (0.30-1.30) | 0.0005 |
| P | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |
| OV9% | |||||
| 0.50 D | 0.56±0.14 (0.35-1.05) | 0.58±0.16 (0.30-1.00) | 0.60±0.14 (0.30-0.90) | 0.60±0.15 (0.30-0.95) | 0.2001 |
| 0.75 D | 0.49±0.11 (0.30-0.85) | 0.51±0.13 (0.30-0.85) | 0.53±0.13 (0.25-0.95) | 0.54±0.14 (0.30-1.00) | 0.0202 |
| 1.00 D | 0.43±0.11 (0.20-0.85) | 0.45±0.12 (0.30-0.75) | 0.46±0.09 (0.30-0.70) | 0.47±0.13 (0.25-0.75) | 0.0992 |
| 1.25 D | 0.37±0.09 (0.15-0.60) | 0.39±0.11 (0.15-0.70) | 0.40±0.10 (0.20-0.70) | 0.41±0.13 (0.20-0.90) | 0.0401 |
| Pa | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
aThe mixed effect linear model was applied to compare the difference among groups. OSI: Objective scatter index; MTF: Modulation transfer function; SR: Strehl ratio; OV: Optical quality analysis system value.
Figure 2. Boxplot panels showing the objective visual quality parameters of 16 types of regular low-degree astigmatism and without astigmatism.
OSI: Objective scatter index; MTF: Modulation transfer function; SR: Strehl ratio; OV: Optical quality analysis system value.
Table 3 shows the associations between astigmatic magnitude and objective visual quality parameters with axis at 180°, 135°, 90°, and 45°. The increase of OSI per degree of astigmatism at 180°, 135°, 90°, and 45° axis were 0.38 (95%CI: 0.35, 0.42), 0.37 (95%CI: 0.34, 0.41), 0.49 (95%CI: 0.45, 0.54), and 0.50 (95%CI: 0.46, 0.53). The decrease of MTFcut-off per degree of astigmatism at 180°, 45°, 90°, and 135° axis were -10.30 (95%CI: -11.43, -9.16), -12.73 (95%CI: -13.62, -11.86), -12.75 (95%CI: -13.79, -11.70), and -9.97 (95%CI: -10.92, -9.03 respectively.
Table 3. The associations between astigmatic magnitude and objective visual quality parameters with axis at 180°, 135°, 90°, and 45°.
| Parameters | OSI |
MTF |
SR |
OV100% |
OV20% |
OV9% |
||||||
| β (95%CI) | P | β (95%CI) | P | β (95%CI) | P | β (95%CI) | P | β (95%CI) | P | β (95%CI) | P | |
| 180° | ||||||||||||
| 0.00 D | ref. | ref. | ref. | ref. | ref. | ref. | ||||||
| 0.50 D | 0.09 (0.04. 0.13) | 0.0002 | -1.79 (-3.28, -0.31) | 0.0181 | -0.02 (-0.03, -0.01) | <0.0001 | -0.07 (-0.12, -0.02) | 0.0109 | -0.08 (-0.12, -0.04) | 0.0005 | -0.07 (-0.10, -0.04) | <0.0001 |
| 0.75 D | 0.18 (0.13, 0.22) | <0.0001 | -4.96 (-6.44, -3.48) | <0.0001 | -0.04 (-0.05, -0.03) | <0.0001 | -0.16 (-0.21, -0.11) | <0.0001 | -0.17 (-0.22, -0.13) | <0.0001 | -0.12 (-0.15, -0.09) | <0.0001 |
| 1.00 D | 0.33 (0.29, 0.38) | <0.0001 | -9.11 (-10.59, -7.63) | <0.0001 | -0.06 (-0.07, -0.05) | <0.0001 | -0.31 (-0.36, -0.26) | <0.0001 | -0.30 (-0.34, -0.26) | <0.0001 | -0.20 (-0.23, -0.17) | <0.0001 |
| 1.25 D | 0.47 (0.43, 0.52) | <0.0001 | -12.56 (-14.04, -11.08) | <0.0001 | -0.08 (-0.09, -0.07) | <0.0001 | -0.42 (-0.47, -0.37) | <0.0001 | -0.39 (-0.43, -0.34) | <0.0001 | -0.26 (-0.29, -0.23) | <0.0001 |
| per 1 D | 0.38 (0.35, 0.42) | <0.0001 | -10.30 (-11.43, -9.16) | <0.0001 | -0.06 (-0.07, -0.06) | <0.0001 | -0.34 (-0.38, -0.31) | <0.0001 | -0.32 (-0.35, -0.29) | <0.0001 | -0.21 (-0.23, -0.18) | <0.0001 |
| 135° | ||||||||||||
| 0.00 D | ref. | ref. | ref. | ref. | ref. | ref. | ||||||
| 0.50 D | 0.12 (0.07, 0.16) | <0.0001 | -2.39 (-3.63, -1.15) | 0.0002 | -0.02 (-0.03, -0.01) | <0.0001 | -0.08 (-0.13, -0.04) | <0.0001 | -0.09 (-0.14, -0.05) | 0.0001 | -0.07 (-0.10, -0.04) | <0.0001 |
| 0.75 D | 0.20 (0.16, 0.25) | <0.0001 | -5.62 (-6.86, -4.38) | <0.0001 | -0.04 (-0.05, -0.03) | <0.0001 | -0.19 (-0.23, -0.15) | <0.0001 | -0.19 (-0.23, -0.14) | <0.0001 | -0.13 (-0.16, -0.11) | <0.0001 |
| 1.00 D | 0.30 (0.26, 0.35) | <0.0001 | -8.86 (-10.10, -7.62) | <0.0001 | -0.06 (-0.07, -0.05) | <0.0001 | -0.30 (-0.34, -0.26) | <0.0001 | -0.15 (-0.19, -0.10) | <0.0001 | -0.20 (-0.23, -0.18) | <0.0001 |
| 1.25 D | 0.49 (0.44, 0.53) | <0.0001 | -12.30 (-13.54, -11.06) | <0.0001 | -0.08 (-0.09, -0.07) | <0.0001 | -0.41 (-0.45, -0.37) | <0.0001 | -0.40 (-0.44, -0.35) | <0.0001 | -0.26 (-0.29, -0.24) | <0.0001 |
| per 1 D | 0.37 (0.34, 0.41) | <0.0001 | -9.97 (-10.92, -9.03) | <0.0001 | -0.06 (-0.07, -0.06) | <0.0001 | -0.33 (-0.36, -0.30) | <0.0001 | -0.37 (-0.31, -0.24) | <0.0001 | -0.21 (-0.23, -0.19) | <0.0001 |
| 90° | ||||||||||||
| 0.00 D | ref. | ref. | ref. | ref. | ref. | ref. | ||||||
| 0.50 D | 0.14 (0.09, 0.20) | <0.0001 | -4.33 (-5.72, -2.94) | <0.0001 | -0.02 (-0.03, -0.01) | <0.0001 | -0.15 (-0.19, -0.10) | <0.0001 | -0.14 (-0.18, -0.09) | 0.0005 | -0.09 (-0.11, -0.06) | <0.0001 |
| 0.75 D | 0.28 (0.22, 0.33) | <0.0001 | -8.22 (-9.62, -6.83) | <0.0001 | -0.04 (-0.05, -0.03) | <0.0001 | -0.28 (-0.33, -0.24) | <0.0001 | -0.26 (-0.30, -0.21) | <0.0001 | -0.15 (-0.18, -0.13) | <0.0001 |
| 1.00 D | 0.42 (0.37, 0.48) | <0.0001 | -11.92 (-13.32, -10.53) | <0.0001 | -0.07 (-0.08, -0.06) | <0.0001 | -0.40 (-0.45, -0.36) | <0.0001 | -0.36 (-0.40, -0.32) | <0.0001 | -0.22 (-0.25, -0.19) | <0.0001 |
| 1.25 D | 0.63 (0.57, 0.68) | <0.0001 | -15.76 (-17.15, -14.37) | <0.0001 | -0.09 (-0.09, -0.08) | <0.0001 | -0.52 (-0.57, -0.48) | <0.0001 | -0.46 (-0.50, -0.42) | <0.0001 | -0.28 (-0.31, -0.25) | <0.0001 |
| per 1 D | 0.49 (0.45, 0.54) | <0.0001 | -12.75 (-13.79, -11.70) | <0.0001 | -0.07 (-0.08, -0.06) | <0.0001 | -0.43 (-0.46, -0.39) | <0.0001 | -0.37 (-0.40, -0.34) | <0.0001 | -0.23 (-0.25, -0.21) | <0.0001 |
| 45° | ||||||||||||
| 0.00 D | ref. | ref. | ref. | ref. | ref. | ref. | ||||||
| 0.50 D | 0.17 (0.13, 0.21) | 0.0002 | -5.12 (-6.31, -3.94) | <0.0001 | -0.03 (-0.04, -0.03) | <0.0001 | -0.17 (-0.21, -0.13) | <0.0001 | -0.17 (-0.21, -0.13) | <0.0001 | -0.11 (-0.14, -0.08) | <0.0001 |
| 0.75 D | 0.30 (0.26, 0.34) | <0.0001 | -8.80 (-9.99, -7.62) | <0.0001 | -0.05 (-0.06, -0.04) | <0.0001 | -0.29 (-0.33, -0.25) | <0.0001 | -0.27 (-0.31, -0.24) | <0.0001 | -0.18 (-0.20, -0.15) | <0.0001 |
| 1.00 D | 0.44 (0.40, 0.48) | <0.0001 | -11.78 (-12.96, -10.60) | <0.0001 | -0.07 (-0.08, -0.06) | <0.0001 | -0.40 (-0.44, -0.36) | <0.0001 | -0.36 (-0.40, -0.33) | <0.0001 | -0.23 (-0.26, -0.21) | <0.0001 |
| 1.25 D | 0.63 (0.59, 0.67) | <0.0001 | -16.06 (-17.24, -14.88) | <0.0001 | -0.09 (-0.10, -0.08) | <0.0001 | -0.54 (-0.58, -0.50) | <0.0001 | -0.48 (-0.52, -0.44) | <0.0001 | -0.30 (-0.32, -0.27) | <0.0001 |
| per 1 D | 0.50 (0.46, 0.53) | <0.0001 | -12.73 (-13.62, -11.86) | <0.0001 | -0.07 (-0.08, -0.07) | <0.0001 | -0.43 (-0.46, -0.40) | <0.0001 | -0.38 (-0.41, -0.35) | <0.0001 | -0.24 (-0.26, -0.22) | <0.0001 |
OSI: Objective scatter index; MTF: Modulation transfer function; SR: Strehl ratio; OV: Optical quality analysis system value.
DISCUSSION
This study assessed the effect of different astigmatism degrees or axial directions on objective visual quality by placing an astigmatism lens in front of the volunteers and by OQAS. Astigmatism's influence on visual quality increases with the astigmatism degree, and low astigmatism of 0.50 D can impact visual quality and quantify the effect of astigmatic magnitude on objective visual quality for the first time. For the same astigmatism degree, astigmatism of 45° and 90° axis have a more significant effect on visual quality parameters than 180° and 135° axis.
Previous studies have shown that implantation of Toric intraocular lens (IOL) is the preferred option for the correction of high astigmatism[15]–[16]. However, the correction of low-degree astigmatism is still controversial. Some scholars believe that the near vision of patients with astigmatism less than 0.50 D can be improved by increasing focal depth, so it is not recommended to have a surgical correction for corneal astigmatism lower than 0.5 D[17]. Some studies have also found that an astigmatism of 0.50 D can cause significant visual loss. Guo and Atchison[18] found that astigmatism of 0.28 D could cause visual loss in volunteers. However, the astigmatism correction of 0.5-0.75 D after cataract surgery can significantly improve their reading speed and contrast sensitivity[19]. Therefore, further research is still needed to determine what extent of low-degree astigmatism needs to be corrected. Previous studies mostly evaluated the effect of astigmatism correction by visual acuity and could not reflect the quality of imaging in the astigmatism state. Based on the principle of dual-channel technology, OQAS can objectively and quantitatively analyze the visual quality through the point spread function and modulation transfer function. In this study, OQAS was used to evaluate the objective visual quality parameters under astigmatism, and it was found that 0.50 D astigmatism could cause a significant increase in OSI and a significant decrease in MTF, SR, and OV under each contrast. Based on the results of this study, the corrected preoperative corneal astigmatism by 0.50 D is likely to improve the postoperative visual quality in cataract patients.
Regular astigmatism can be divided into astigmatism ATR (90°±30°), astigmatism with-the-rule (WTR, 180°±30°), and oblique astigmatism (30°-60° or 120°-150°). In previous studies, the effect of astigmatism axial direction on naked-eye vision is still controversial. Vinas et al[20] found that for individuals without astigmatism, 0° and 45° axis additional astigmatism had a more obvious effect on visual acuity than 90°. The results of Mimouni et al[21] are similar; ATR and oblique astigmatism have more noticeable impact on naked-eye vision than astigmatism WTR. Kordić et al[22] found that the uncorrected near vision of patients with residual astigmatism ATR was better than that of patients with astigmatism WTR. Kobashi et al[23] found that oblique astigmatism had a greater effect on far vision and reading speed than WTR or ATR astigmatism, while there was no obvious difference between WTR and ATR astigmatism. Some studies also found that there is no obvious difference in the effect of different astigmatism axial direction on vision under the same astigmatism, and the fuzzy effect of astigmatism mainly depends on the size of astigmatism rather than the axial direction. In this study, at the same astigmatism, 45° and 90° axial directions had more obvious effects on each visual quality parameter than 0° and 135°, with the 45° axis direction being the most obvious. This result is consistent with most previous studies that oblique astigmatism and ATR astigmatism have more obvious effect on visual acuity than WTR astigmatism. Therefore, it is speculated that the correction of astigmatism in patients with astigmatism greater than or equal to 0.50 D, especially axial at 45° or 90°, may be meaningful to improve the postoperative visual quality of cataract patients. However, it is the first time to find that oblique astigmatism varies between the 45° and 135° axis, and it is also in keeping with the result when divided into right eye group and left group. Further studies are needed to find the underline mechanism.
Previous research found that tear film could affect the optical quality and dry eye (BUT shorter than 5s) had lower optical quality than normal eyes[24]. Although we included 18 dry eyes in present study, the difference of objective visual quality between dry eyes and others were not significant. We suggest that this may be due to the fact that the individual had time to rest by closing their eyes and the measurement was taken quickly in our present study.
The purpose of this study is to evaluate the impact of low-degree astigmatism on objective visual quality. For cataract cases, we discuss the use of Toric IOLs to correct low degrees of corneal astigmatism, however it is not the only resolution. Low-degree corneal astigmatism could be, otherwise, corrected by laser vision correction or limbal relaxing incisions[25]–[28]. further research is needed to evaluate the accuracy of each resolution. And our discussion mainly base on the objective data, however, the subjective aspect should not be neglected. Subjective questionnaire survey should be added in future researches. Furthermore, we believe that the results can not only apply for cataract patients, but also provide a reference for ametropic patients combined with astigmatism whether low astigmatism needs to be corrected when wear glasses.
The sample size of this study is larger than that of previous clinical studies of low-degree astigmatism. Still, this study also has its limitations: it shows that 0.5 D astigmatism can impact objective visual quality. It is speculated that it may improve visual quality after correction. However, the lower degree of astigmatism correction has higher requirements for preoperative evaluation and surgical skills. The same amount of postoperative residual astigmatism of 0.5 D may mean successful correction in patients with preoperative corneal astigmatism 2.5 D and failure in patients with preoperative corneal astigmatism 0.5 D. How to more precisely control postoperative astigmatism to reduce the postoperative residual astigmatism remains to be further studied and explored. In addition, the investigated individuals included in this study are young to middle-aged people, and the study results may not apply to the elderly population. Several researches reported that the astigmatism axis shifts from WTR to ATR with age[2],[29]. However, elderly people usually have more complicated ocular conditions, and the existence of interfering factors such as cataracts may affect the outcomes of objective visual quality. The more elderly population with healthy ocular condition will be needed to explore further the impact of low-degree astigmatism on the visual quality of the elderly population. Moreover, our study doesn't include hyperopia because hyperopia is less common in young to middle-aged people, further researches are needed for hyperopic patients with astigmatism.
Footnotes
Conflicts of Interest: Ye LY, None; Li SF, None; Zuo JJ, None; Li J, None; Ma HX, None.
REFERENCES
- 1.Zhong H, Qin H, Wang HJ, Wang ZY. Objective visual quality one year after toric IOL implantation for correction of moderate and high corneal astigmatism. Int J Ophthalmol. 2021;14(2):245–249. doi: 10.18240/ijo.2021.02.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rajabpour M, Kangari H, Pesudovs K, Khorrami-Nejad M, Rahmani S, Mohaghegh S, Moradnejad S. Refractive error and vision related quality of life. BMC Ophthalmol. 2024;24(1):83. doi: 10.1186/s12886-024-03350-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keshav V, Henderson BA. Astigmatism management with intraocular lens surgery. Ophthalmology. 2021;128(11):e153–e163. doi: 10.1016/j.ophtha.2020.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Namba H, Sugano A, Murakami T, Utsunomiya H, Nishitsuka K, Ishizawa K, Kayama T, Yamashita H. Age-related changes in astigmatism and potential causes. Cornea. 2020;39(Suppl 1):S34–S38. doi: 10.1097/ICO.0000000000002507. [DOI] [PubMed] [Google Scholar]
- 5.Wu Z, Liu C, Chen Z. Prevalence and age-related changes of corneal astigmatism in patients undergoing cataract surgery in Northern China. J Ophthalmol. 2020;2020:6385098. doi: 10.1155/2020/6385098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lake JC, Victor G, Clare G, Porfírio GJ, Kernohan A, Evans JR. Toric intraocular lens versus limbal relaxing incisions for corneal astigmatism after phacoemulsification. Cochrane Database Syst Rev. 2019;12(12):CD012801. doi: 10.1002/14651858.CD012801.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goggin M. Toric intraocular lenses: evidence-based use. Clin Exp Ophthalmol. 2022;50(5):481–489. doi: 10.1111/ceo.14106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pang YL, Yuan L, Cao XG, Hou XR, Bao YZ. Characteristics and analysis of corneal astigmatism in age-related cataract patients over 50y old. Zhonghua Yan Ke Za Zhi. 2020;56(5):349–355. doi: 10.3760/cma.j.cn112142-20190618-00323. [DOI] [PubMed] [Google Scholar]
- 9.Logothetis HD, Feder RS. Which intraocular lens would ophthalmologists choose for themselves? Eye (Lond) 2019;33(10):1635–1641. doi: 10.1038/s41433-019-0460-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yoo YS, Paik DW, Lim DH, Chung TY. One-year long-term clinical outcomes following diffractive trifocal toric intraocular lens implantation: retrospective observational case series study. Ann Transl Med. 2022;10(21):1159. doi: 10.21037/atm-22-1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hayashi K, Manabe S, Yoshida M, Hayashi H. Effect of astigmatism on visual acuity in eyes with a diffractive multifocal intraocular lens. J Cataract Refract Surg. 2010;36(8):1323–1329. doi: 10.1016/j.jcrs.2010.02.016. [DOI] [PubMed] [Google Scholar]
- 12.Gundersen KG, Potvin R. Comparing visual acuity, low contrast acuity and refractive error after implantation of a low cylinder power toric intraocular lens or a non-toric intraocular lens. Clin Ophthalmol. 2020;14:3661–3666. doi: 10.2147/OPTH.S281178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang LM, Shen WQ, Shen JY, Wang M, Ni S, Guo HK, Yang J. Effect of postoperative residual astigmatism on visual outcomes after trifocal intraocular lens implantation. Front Med. 2023;10:1202793. doi: 10.3389/fmed.2023.1202793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Núñez MX, Henriquez MA, Escaf LJ, Ventura BV, Srur M, Newball L, Espaillat A, Centurion VA. Consensus on the management of astigmatism in cataract surgery. Clin Ophthalmol. 2019;13:311–324. doi: 10.2147/OPTH.S178277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu JM, Wang SN, Zhao T, Li MQ. Clinical observation of Toric intraocular lens for correcting low and moderate corneal regular astigmatism in cataract patients. Ophthalmology in China. 2018;27:433–437. [Google Scholar]
- 16.Villegas EA, Alcón E, Artal P. Minimum amount of astigmatism that should be corrected. J Cataract Refract Surg. 2014;40(1):13–19. doi: 10.1016/j.jcrs.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 17.Chen XY, Xie MY, Zhang D, Zhang C. Bibliometric analysis of research relating to refractive cataract surgery over a 20-year period: from 2003 to 2022. Int J Ophthalmol. 2023;16(10):1692–1701. doi: 10.18240/ijo.2023.10.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guo HQ, Atchison DA. Subjective blur limits for cylinder. Optom Vis Sci. 2010;87(8):E549–E559. doi: 10.1097/OPX.0b013e3181e61b8f. [DOI] [PubMed] [Google Scholar]
- 19.Lehmann RP, Houtman DM. Visual performance in cataract patients with low levels of postoperative astigmatism: full correction versus spherical equivalent correction. Clin Ophthalmol. 2012;6:333–338. doi: 10.2147/OPTH.S28241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vinas M, de Gracia P, Dorronsoro C, Sawides L, Marin G, Hernández M, Marcos S. Astigmatism impact on visual performance: meridional and adaptational effects. Optom Vis Sci. 2013;90(12):1430–1442. doi: 10.1097/OPX.0000000000000063. [DOI] [PubMed] [Google Scholar]
- 21.Mimouni M, Nemet A, Pokroy R, Sela T, Munzer G, Kaiserman I. The effect of astigmatism axis on visual acuity. Eur J Ophthalmol. 2017;27(3):308–311. doi: 10.5301/ejo.5000890. [DOI] [PubMed] [Google Scholar]
- 22.Kordić R, Kalauz M, Kuzman T, Masnec S, Skegro I, Vidović T, Suić-Popović S, Cerovski B, Rezaković S, Kutija MB. Effect of the against the rule myopic astigmatism on the near vision of the elderly. Coll Antropol. 2014;38(4):1223–1224. [PubMed] [Google Scholar]
- 23.Kobashi H, Kamiya K, Shimizu K, Kawamorita T, Uozato H. Effect of axis orientation on visual performance in astigmatic eyes. J Cataract Refract Surg. 2012;38(8):1352–1359. doi: 10.1016/j.jcrs.2012.03.032. [DOI] [PubMed] [Google Scholar]
- 24.Yu AY, Lu T, Pan AP, Lin DR, Xu CC, Huang JH, Bao FJ. Assessment of tear film optical quality dynamics. Invest Ophthalmol Vis Sci. 2016;57(8):3821–3827. doi: 10.1167/iovs.15-18985. [DOI] [PubMed] [Google Scholar]
- 25.Hu ZX, Sima J, Cao JG, Ke Y, Zhang YY, Guo QT, He YP, Liao HX, Tan X, Qin B, Li L. Symmetrical femtosecond laser arc incision in correcting corneal astigmatism in cataract patients. Int J Ophthalmol. 2023;16(12):1996–2003. doi: 10.18240/ijo.2023.12.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhong ST, Zhang Z, Liu XH. The research progress of femtosecond laser-assisted arcuate keratotomy for correction of corneal astigmatism in cataract surgery. Zhonghua Yan Ke Za Zhi. 2024;60(2):200–205. doi: 10.3760/cma.j.cn112142-20231010-00127. [DOI] [PubMed] [Google Scholar]
- 27.Cohen KL, Patel NK. Using total corneal astigmatism with femtosecond laser cataract surgery and arcuate keratotomy(ies) to treat low amounts of astigmatism. Cornea. 2024 doi: 10.1097/ICO.0000000000003482. [DOI] [PubMed] [Google Scholar]
- 28.Yang K, Li J, Zhang W, Liu Z, Song C, Zhao Y. Implanting toric implantable collamer lens displays better astigmatism correction than implantable collamer lens combined with manually limbal relaxing incision. BMC Ophthalmol. 2023;23(1):198. doi: 10.1186/s12886-023-02941-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shao X, Zhou KJ, Pan AP, Cheng XY, Cai HX, Huang JH, Yu AY. Age-related changes in corneal astigmatism. J Refract Surg. 2017;33(10):696–703. doi: 10.3928/1081597X-20170718-04. [DOI] [PubMed] [Google Scholar]