Abstract
Acetabular cartilage delamination is commonly seen in patients with femoroacetabular impingement (FAI), especially ones with the cam deformity. However, the definition and classification of acetabular cartilage injuries caused by FAI to guide clinical treatment remain controversial. Moreover, treatment of acetabular cartilage damage always causes a dilemma for surgeon during surgery. We believe a reliable repair of the acetabular cartilage delamination will lead to a better long-term outcome for patients with FAI. In this Technical Note, we introduce the chondral nail fixation under hip arthroscopy for treating acetabular cartilage delamination in patients with FAI. This technique contributes to eliminating intra-articular unstable factors, preserving native cartilage as much as possible, and restoring cartilage surface intact at best.
Technique Video
Acetabular cartilage injury is commonly caused by impingement induced by cam/pincer lesions in patients with femoroacetabular impingement (FAI) and will lead to a cartilage wear or tear over time1 (Fig 1 A and B). Approximately 44% of patients with FAI are diagnosed with acetabular cartilage delamination (ACD) from the subchondral bone during arthroscopic inspection.2, 3, 4, 5 The definition and classification of acetabular cartilage injuries caused by FAI to guide clinical treatment remain controversial.2,6, 7, 8, 9 Moreover, treatment of acetabular cartilage damage always creates a dilemma for the surgeon during surgery.10 Several repair procedures have been tried,11, 12, 13, 14, 15 and sometimes surgeons have to remove the chondral flap to ensure that it will not form a loose body and cause hip pain after surgery.
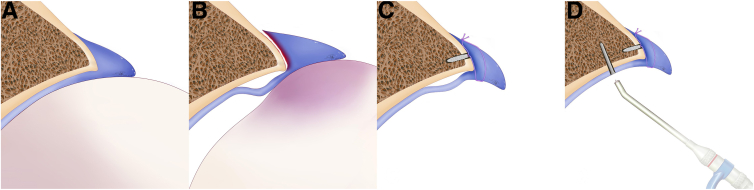
Fig 1.
Schematic diagrams of acetabular cartilage delamination and chondral nail fixation. (A) Normal hip anatomy. (B) Acetabular cartilage delamination caused by femoroacetabular impingement. The acetabular cartilage becomes detached from the subchondral bone because of the shear-force and outside-in abrasion induced by cam deformity. (C) The acetabular cartilage delamination persists after the labrum repair. (D) Chondral nail fixation of the acetabular cartilage delamination. The detached cartilage is pressed back to the subchondral bone by inserting an absorbable chondral nail. The smoothness of joint surface is restored.
We believe a reliable repair of the acetabular cartilage will lead to a better long-term outcome for patients with FAI.16 Based on our previous clinical experience of using biochondral nails for cartilage repair in the knee joint, we have performed acetabular cartilage fixation with chondral nails in patients with FAI during the past 2 years. (Fig 1 C and D) We introduce this technique and share our clinical experiences in this Technical Note.
Surgical Technique (With Video Illustration)
The patient is positioned supine on a traction table (Smith & Nephew, Andover, MA) and is prepared and draped in the standard fashion. The greater trochanter and anterior superior iliac spine are outlined for anatomic landmarks. The anterolateral portal (ALP) is created first. With the inspection using a 30° arthroscope from the ALP, the midanterior portal (MAP) is established. The distal anterolateral accessory portal and proximal MAP are established for placement of the suture anchors and for management of suture wires, respectively. We have described the surgical procedures of evaluation and suture repair of the labrum in our previous studies,17 so we have omitted the details of this part in the present article. The ALP and MAP are set to incise the joint capsule from 10 to 3 o`clock. The labral tear is repaired using a common surgical technique with suture anchors. Before suture repair of the labrum, inspection of ACD is performed by a probe (Fig 2A).
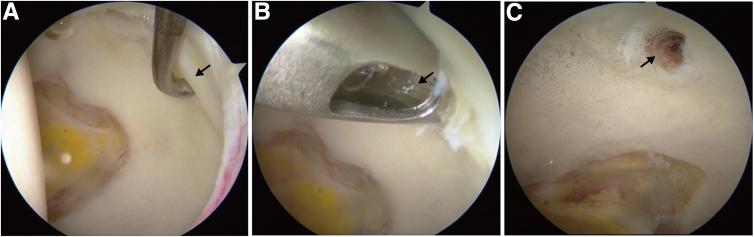
Fig 2.
Arthroscopic view of acetabular cartilage delamination and chondral nail fixation (right hip). (A) Probing of the acetabular cartilage injury; black arrow points to wave sign. (B) The curved guide is set in-place stably; black arrow points to the absorbable chondral nail being inserted. (C) Inspection after the chondral nail fixation; black arrow points to the chondral nail head.
Damage to the acetabular cartilage usually occurs in the transition area of the labrum and cartilage. Estimation of the shape, size, and depth of cartilage injury under arthroscopic inspection is necessary before deciding on surgical treatment (Fig 2A). First, we evaluate the shape and size of cartilage damage under arthroscopy, as well as the depth of cartilage injury according to the International Cartilage Regeneration & Joint Preservation Society grading system, to decide the observing portal and working portal, whereas, in general cases, we only needed to establish AL, MAP, and distal anterolateral accessory for the treatment of acetabular cartilage injury. The chondral nail we use has a diameter of 1.5 mm, a length of 15 mm, and with an absorption time of approximately 2 years. A curved drilling guide is applied for the fixation of the cartilage flap after reduction, and the front of our drilling guide is arc-shaped to ensure the angle of nail insertion is perpendicular to the cartilage surface (Fig 1D). Once the insertion is placed, we check whether the guide is stable, because the conjunction area of the acetabular cartilage and the labrum is a slope, so it is easy for the guide to slide while drilling. The top of the guide is a serrated shape, which provides a reliable grip. The front part of the drill is designed to be spring structure, making the drill more flexible to match the bending angle of the guide, which is more conducive to intraoperative operation. The drilling is monitored under arthroscopy to ensure that it does not pass through the cartilage surface and to keep the articular surface intact. During the insertion of the chondral nail, we use a pusher, not a hammer, because the strength of the chondral nail is relatively low and easy to be compressed or bent under huge vertical pressure, resulting in failure of fixation (Fig 2B). The length of the nail is 15 mm, so the cartilage should be well fixed with subchondral bone. It should be confirmed again after the placement of the chondral nail that the nail did not pass through the articular surface (Fig 2C). After the repair and fixation is completed, we perform cam-osteoplasty of the junction of the femoral head and neck to protect the repaired labrum and fixed cartilage from impingement, thereby reducing the probability of secondary cartilage damage.
Video 1 shows the main surgical procedures of the chondral nail fixation technique. In our surgical protocol, there are some important points to note: (1) Strictly select patients according to the indications and carry out a comprehensive preoperative assessment (Table 1); (2) the guide must be firmly fixed to prevent slipping during the operation; (3) adjust the position and angle of the chondral nails to prevent them from touching with the labrum anchors; (4) the insertion depth of the chondral nail should be appropriate, as it not only sustains a solid fixation to the subchondral bone but also keeps the articular surface smooth and flat (Fig 1D); and (5) The operation should be performed carefully and iatrogenic injury should be avoided (Table 2).
Table 1.
Indications and Contradictions of the Technique
| Indications | Contradictions |
|---|---|
| (1) Patients with FAI without improvement after 6-month nonsurgical treatment | (1) Tönnis grade >1 (2) Partial- or full-thickness acetabular cartilage defect |
| (2) Preoperative MRI signs of ACD injury. To illustrate, at least 2 consecutive slices in the same plane or in the same location in 2 different planes show focal discontinuity of cartilage and fluid located between the acetabular cartilage and subchondral bone plate; in addition, the area of delaminated cartilage is not completely detached from the adjacent cartilage; | (3) Rupture of the acetabular cartilage, exposure of the subchondral bone |
| (3) Tönnis grade ≤1 and no intra-articular loose body | |
| (4) Arthroscopic inspection of an area of degenerated cartilaginous surface at the chondrolabral junction, or a partial detachment of the articular cartilage from the subchondral bone without exposing it, with no interruption of the articular surface |
ACD, acetabular cartilage delamination; FAI, femoroacetabular impingement; MRI, magnetic resonance imaging.
Table 2.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| (1) Strictly select patients according to the indications and carry out a comprehensive preoperative assessment. (2) The guide must be firmly fixed to prevent slipping during the operation. (3) Adjust the position and angle of the chondral nails to prevent them from touching the labrum anchors. (4) The insertion depth of the chondral nail should be appropriate; it not only sustains a solid fixation to the subchondral bone but also keeps the articular surface smooth and flat. |
(1) The flexible drill has a limited lifespan, with risk of snapping. (2) The position and angle of nail-inserting is difficult to handle, which requires certain clinical expertise regarding hip arthroscopy. (3) Close follow-up is performed in case of nail loosening, displacement, and foreign body reaction. |
Discussion
Acetabular cartilage injury is a common complication of FAI, yet there is currently no clear injury classification or arthroscopic established fixation method for this type of injury.18 Due to the unique anatomical character of the acetabular cartilage, the widely used Outerbridge or the International Cartilage Regeneration & Joint Preservation Society grading systems are not applicable to the hip joint.18 From an imaging perspective, the “carpet phenomenon,” “wave sign,” and “inverted Oreo cookie sign,” all contribute to preoperative assessment.5,19,20
Based on biomechanical studies, ACD is believed to be caused by shear and compressive forces stemming from femoral acetabular impingement (Fig 1A and B).21 Cam deformity typically results in cartilage damage in the superior quarter of the anterior acetabulum, whereas pincer leads to a more circumferential and extensive area on the acetabular side.22 ACD often coexists with labral tear, a combined injury typically occurring during flexion rotation of the hip joint (Fig 1A and B).21
Various attempts have been made to treat hip cartilage injuries, including arthroscopic debridement and microfracture, which are the most common surgical options. Arthroscopic debridement is suitable for low-grade, non–full-thickness cartilage injuries, which implies the removal of detached cartilage flaps under arthroscopy.23 Using microfracture for treatment of hip acetabular cartilage injury has limited documentation, but reported with fibrocartilage formation in the defect area.8,24, 25, 26, 27, 28, 29, 30, 31
However, Meulenkamp et al.32 revealed that chondrocyte viability within the detached cartilage flap exceeds 50%, suggesting that such unstable but healthy cartilage tissue held considerable repair value. Some studies reported fibrin glue or suture technique for cartilage fixation, but these methods were challenging to perform under arthroscopy and unreliable for cartilage fixation, especially with weight-bearing.12,33, 34, 35 Based on our experience treating knee osteochondral injuries,36 we propose using absorbable chondral nails for fixation of ACD. By reaching the subchondral bone with 15 mm depth of nail, the reliability of fixation is ensured. This method maximizes the protection of cartilage tissue and restores the joint surface integrity, ultimately promoting cartilage injury healing (Fig 3). This cartilage repair technique has provided satisfactory clinical results over the past 2 years of our clinical practice.
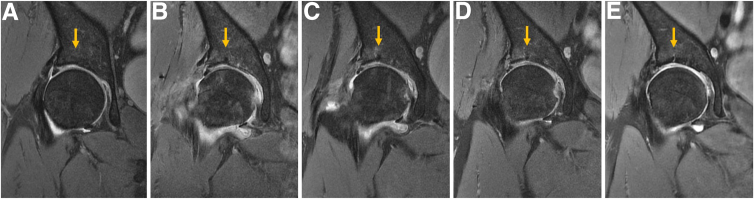
Fig 3.
Pre- and postoperative magnetic resonance images of acetabular cartilage delamination in right hip of 53-year-old female patient in the oblique coronal plane. The yellow arrows point to the site of chondral nail. (A) Preoperation, (B) 3 months after operation, (C) 5 months after operation, (D) 7 months after operation, and (E) 23 months after operation. The nail is gradually absorbed in place without displacement or foreign body reaction.
We consider arthroscopic biopsy as the gold standard for diagnosing ACD. Surgical treatment decisions should be made based on location, size, and depth of the cartilage injury. The technique of absorbable chondral nail for fixation of acetabular cartilage lesion has distinct advantages. We use a curved drill guide, allowing the nail insertion angle to be perpendicular to the articular surface, suiting the dome-like structure of the acetabulum and overcoming the limited space for arthroscopic operation in the hip. A spiral spring structure bending with drill provides some flexibility for the insertion angle. The guide handle helps us accurately adjust the position and insertion angle intraoperatively, to protect from touching with the suture anchors for labral repair.
Nail surface features a grooved design, allowing bone marrow stem cells from the medullary cavity to reach the cartilage and subchondral bone via this groove, promoting cartilage repair and regeneration. In our experience, this technique effectively combines cartilage fixation and microfracture surgery. Furthermore, the implantation of the chondral nail does not affect the patient’s postoperative rehabilitation plan or any extension of weight-bearing time.
However, we also note some limitations to this technique. For instance, the lifespan of the spring drill is limited, leading to a risk of breakage during surgery. The long soft-tissue tunnel of the hip arthroscopy and the requirement for the surgeon’s surgical technique and proficiency pose a greater demand on the surgical learning curve. In addition, the long-term absorption process of the chondral nail and clinical evaluation require further clinical follow-up studies (Table 3). In this Technical Note, we aimed to eliminate intra-articular unstable factors, preserve native cartilage as much as possible, and restore cartilage surface intact at best.
Table 3.
Advantages and Limitations of the Technique
| Advantages | Limitations |
|---|---|
| (1) We use a curved drill guide, allowing the nail insertion angle to be perpendicular to the articular surface, suiting the dome-like structure of the acetabulum and overcoming the limited space for arthroscopic operation in the hip. (2) A spiral spring structure bending with drill provides some flexibility for the insertion angle. (3) The guide handle helps us accurately adjust the position and insertion angle intraoperatively, to protect from touching with the suture anchors for labral repair. (4) Nail surface features a grooved design, allowing bone marrow stem cells from the medullary cavity to reach the cartilage and subchondral bone via this groove, promoting cartilage repair and regeneration. (5) The implantation of the chondral nail does not affect the patient’s postoperative rehabilitation plan or any extension of weight-bearing time. |
(1) The lifespan of the spring drill is limited, leading to a risk of breakage during surgery. (2) The long soft-tissue tunnel of the hip arthroscopy and the requirement for the surgeon's surgical technique and proficiency pose a greater demand for the surgical learning curve. (3) The long-term absorption process of the chondral nail and clinical evaluation require further clinical follow-up studies. |
ACD, acetabular cartilage delamination; FAI, femoroacetabular impingement.
Disclosures
The authors report the following potential conflicts of interest or sources of funding: The study was supported by Clinical Cohort Construction Project of Peking University Third Hospital (BYSYDL2021024), Beijing, China. All authors (H.D., K.T., G.G., R.L., S.Z., Z.L., Y.X.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Footnotes
Hanmei Dong, and M.D. and Kang Tian, M.D., equally contributed to this work and share the first authorship.
Supplementary Data
Acetabular cartilage delamination is commonly seen in patients with FAI, especially ones with the cam deformity. The definition, classification, and treatment of acetabular cartilage injury caused by FAI remain controversial to guide clinical work. We believe a reliable repair of the acetabular cartilage delamination will lead to a better long-term outcome for patients with FAI. Here, we introduce the absorbable chondral nail fixation under hip arthroscopy for treating acetabular cartilage delamination in patients with FAI. This technique contributes to eliminating intra-articular unstable factors, preserving native cartilage as much as possible, and restoring cartilage surface intact at best. In this video, we will describe the surgical procedures of the chondral nail fixation technique in detail. (FAI, femoroacetabular impingement.)
References
- 1.Volpon J.B. Femoroacetabular impingement. Rev Bras Ortop. 2016;51:621–629. doi: 10.1016/j.rboe.2016.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jannelli E., Parafioriti A., Acerbi A., Ivone A., Fioruzzi A., Fontana A. Acetabular delamination: Epidemiology, histological features, and treatment. Cartilage. 2019;10:314–320. doi: 10.1177/1947603518768096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson L.A., Peters C.L., Park B.B., Stoddard G.J., Erickson J.A., Crim J.R. Acetabular cartilage delamination in femoroacetabular impingement. Risk factors and magnetic resonance imaging diagnosis. J Bone Joint Surg Am. 2009;91:305–313. doi: 10.2106/JBJS.G.01198. [DOI] [PubMed] [Google Scholar]
- 4.Konstantinidis G., Mitchell M., Boyd G., Coady C., Ghosh S., Wong I. Poor sensitivity of magnetic resonance arthrography to detect hip chondral delamination: A retrospective follow-up of 227 FAI-operated patients. Cartilage. 2021;12:162–168. doi: 10.1177/1947603518816453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beck M., Kalhor M., Leunig M., Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: Femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 6.Mygind-Klavsen B., Gronbech Nielsen T., Maagaard N., et al. Danish Hip Arthroscopy Registry: An epidemiologic and perioperative description of the first 2000 procedures. J Hip Preserv Surg. 2016;3:138–145. doi: 10.1093/jhps/hnw004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Konan S., Rayan F., Meermans G., Witt J., Haddad F.S. Validation of the classification system for acetabular chondral lesions identified at arthroscopy in patients with femoroacetabular impingement. J Bone Joint Surg Br. 2011;93:332–336. doi: 10.1302/0301-620X.93B3.25322. [DOI] [PubMed] [Google Scholar]
- 8.Dhillon J., Orozco E., Keeter C., Scillia A.J., Harris J.D., Kraeutler M.J. Microfracture of acetabular chondral lesions is not superior to other cartilage repair techniques in patients with femoroacetabular impingement syndrome: A systematic review. Arthroscopy. 2024;40:602–611. doi: 10.1016/j.arthro.2023.05.034. [DOI] [PubMed] [Google Scholar]
- 9.Serong S., Fickert S., Niemeyer P., et al. Outcome-affecting parameters of hip arthroscopy for femoroacetabular impingement with concomitant cartilage damage—data analysis from the German Cartilage Registry. J Clin Med. 2022;11:1532. doi: 10.3390/jcm11061532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hernigou J., Verdonk P., Homma Y., Verdonk R., Goodman S.B., Hernigou P. Nonoperative and operative bone and cartilage regeneration and orthopaedic biologics of the hip: An Orthoregeneration Network (ON) Foundation Hip Review. Arthroscopy. 2022;38:643–656. doi: 10.1016/j.arthro.2021.08.032. [DOI] [PubMed] [Google Scholar]
- 11.Jannelli E., Fontana A. Arthroscopic treatment of chondral defects in the hip: AMIC, MACI, microfragmented adipose tissue transplantation (MATT) and other options. SICOT J. 2017;3:43. doi: 10.1051/sicotj/2017029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tzaveas A.P., Villar R.N. Arthroscopic repair of acetabular chondral delamination with fibrin adhesive. Hip Int. 2010;20:115–119. doi: 10.1177/112070001002000117. [DOI] [PubMed] [Google Scholar]
- 13.Mardones R., Larrain C. Cartilage restoration technique of the hip. J Hip Preserv Surg. 2016;3:30–36. doi: 10.1093/jhps/hnv061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fontana A., Bistolfi A., Crova M., Rosso F., Massazza G. Arthroscopic treatment of hip chondral defects: Autologous chondrocyte transplantation versus simple debridement—a pilot study. Arthroscopy. 2012;28:322–329. doi: 10.1016/j.arthro.2011.08.304. [DOI] [PubMed] [Google Scholar]
- 15.Luo T.D., Beck E.C., Trammell A.P., et al. Hip arthroscopic microfracture augmented with platelet-rich plasma-infused micronized cartilage allograft significantly improves functional outcomes. Arthroscopy. 2022;38:2819–2826 e2811. doi: 10.1016/j.arthro.2022.02.021. [DOI] [PubMed] [Google Scholar]
- 16.Carreira D.S., Shaw D.B., Ueland T.E., et al. Acetabular cartilage lesions predict inferior mid-term outcomes for arthroscopic labral repair and treatment of femoroacetabular impingement syndrome. Arthroscopy. 2022;38:3152–3158. doi: 10.1016/j.arthro.2022.05.013. [DOI] [PubMed] [Google Scholar]
- 17.Tian K., Gao G., Dong H., Zhang S., Zhang W., Wang J., et al. Arthroscopic capsular suture-lifting technique for treating femoroacetabular impingement patients with a high risk of postoperative anterior instability. Arthrosc Tech. 2023;12:e307–e312. doi: 10.1016/j.eats.2022.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ellermann J.M., Donald B., Rohr S., et al. Magnetic resonance imaging of osteochondritis dissecans: validation study for the ICRS classification system. Acad Radiol. 2016;23:724–729. doi: 10.1016/j.acra.2016.01.015. [DOI] [PubMed] [Google Scholar]
- 19.Beaule P.E., Zaragoza E.J. Surgical images: musculoskeletal acetabular cartilage delamination demonstrated by magnetic resonance arthrography: Inverted "Oreo" cookie sign. Can J Surg. 2003;46:463–464. [PMC free article] [PubMed] [Google Scholar]
- 20.Onggo J.D., Onggo J.R., Nambiar M., et al. The 'wave sign' in hip arthroscopy: A systematic review of epidemiological factors, current diagnostic methods and treatment options. J Hip Preserv Surg. 2020;7:410–422. doi: 10.1093/jhps/hnaa058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ganz R., Parvizi J., Beck M., Leunig M., Notzli H., Siebenrock K.A. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 22.Logan Z.S., Redmond J.M., Spelsberg S.C., Jackson T.J., Domb B.G. Chondral lesions of the hip. Clin Sports Med. 2016;35:361–372. doi: 10.1016/j.csm.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Yen Y.M., Kocher M.S. Chondral lesions of the hip: microfracture and chondroplasty. Sports Med Arthrosc Rev. 2010;18:83–89. doi: 10.1097/JSA.0b013e3181de1189. [DOI] [PubMed] [Google Scholar]
- 24.Domb B.G., Redmond J.M., Dunne K.F., Stake C.E., Gupta A. A matched-pair controlled study of microfracture of the hip with average 2-year follow-up: Do full-thickness chondral defects portend an inferior prognosis in hip arthroscopy? Arthroscopy. 2015;31:628–634. doi: 10.1016/j.arthro.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 25.Domb B.G., Gupta A., Dunne K.F., Gui C., Chandrasekaran S., Lodhia P. Microfracture in the hip: Results of a matched-cohort controlled study with 2-year follow-up. Am J Sports Med. 2015;43:1865–1874. doi: 10.1177/0363546515588174. [DOI] [PubMed] [Google Scholar]
- 26.Karthikeyan S., Roberts S., Griffin D. Microfracture for acetabular chondral defects in patients with femoroacetabular impingement: Results at second-look arthroscopic surgery. Am J Sports Med. 2012;40:2725–2730. doi: 10.1177/0363546512465400. [DOI] [PubMed] [Google Scholar]
- 27.Crawford K., Philippon M.J., Sekiya J.K., Rodkey W.G., Steadman J.R. Microfracture of the hip in athletes. Clin Sports Med. 2006;25:327–335. doi: 10.1016/j.csm.2005.12.004. x. [DOI] [PubMed] [Google Scholar]
- 28.Haughom B.D., Erickson B.J., Rybalko D., Hellman M., Nho S.J. Arthroscopic acetabular microfracture with the use of flexible drills: A technique guide. Arthrosc Tech. 2014;3:e459–463. doi: 10.1016/j.eats.2014.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Byrd J.W., Jones K.S. Osteoarthritis caused by an inverted acetabular labrum: Radiographic diagnosis and arthroscopic treatment. Arthroscopy. 2002;18:741–747. doi: 10.1053/jars.2002.32837. [DOI] [PubMed] [Google Scholar]
- 30.Philippon M.J., Schenker M.L., Briggs K.K., Maxwell R.B. Can microfracture produce repair tissue in acetabular chondral defects? Arthroscopy. 2008;24:46–50. doi: 10.1016/j.arthro.2007.07.027. [DOI] [PubMed] [Google Scholar]
- 31.Byrd J.W., Jones K.S. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:739–746. doi: 10.1007/s11999-008-0659-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meulenkamp B., Gravel D., Beaule P.E. Viability assessment of the chondral flap in patients with cam-type femoroacetabular impingement: A preliminary report. Can J Surg. 2014;57:44–48. doi: 10.1503/cjs.003513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stafford G.H., Bunn J.R., Villar R.N. Arthroscopic repair of delaminated acetabular articular cartilage using fibrin adhesive. Results at one to three years. Hip Int. 2011;21:744–750. doi: 10.5301/HIP.2011.8843. [DOI] [PubMed] [Google Scholar]
- 34.Sekiya J.K., Martin R.L., Lesniak B.P. Arthroscopic repair of delaminated acetabular articular cartilage in femoroacetabular impingement. Orthopedics. 2009;32(9) doi: 10.3928/01477447-20090728-44. [DOI] [PubMed] [Google Scholar]
- 35.Lim B.H., Jang S.W., Park Y.S., Lim S.J. Open repair and arthroscopic follow-up of severely delaminated femoral head cartilage associated with traumatic obturator fracture-dislocation of the hip. Orthopedics. 2011;34:199. doi: 10.3928/01477447-20110427-26. [DOI] [PubMed] [Google Scholar]
- 36.Theodorides A.A., Williams A., Guthrie H., Church S. Diagnosis and management of chondral delamination injuries of the knee. Knee. 2019;26:647–652. doi: 10.1016/j.knee.2019.04.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Acetabular cartilage delamination is commonly seen in patients with FAI, especially ones with the cam deformity. The definition, classification, and treatment of acetabular cartilage injury caused by FAI remain controversial to guide clinical work. We believe a reliable repair of the acetabular cartilage delamination will lead to a better long-term outcome for patients with FAI. Here, we introduce the absorbable chondral nail fixation under hip arthroscopy for treating acetabular cartilage delamination in patients with FAI. This technique contributes to eliminating intra-articular unstable factors, preserving native cartilage as much as possible, and restoring cartilage surface intact at best. In this video, we will describe the surgical procedures of the chondral nail fixation technique in detail. (FAI, femoroacetabular impingement.)