The 2F inclusion Ross technique.
Central Message.
Herein, we present a novel approach of the Dacron tube inclusion Ross procedure, widely inspired by the David I procedure and the Medtronic 3F stentless aortic valve implantation.
Since its introduction in 1967, the Ross procedure has been subject to numerous variations, most particularly the Dacron tube inclusion to prevent the autograft from further dilation.1 Yet, some authors argue that an inclusion technique could originate with autograft failure due to geometric issues. In addition, the autograft is often too short to replace the entire aorta; therefore, an additional Dacron graft is needed in between the autograft and the distal aorta. Finally, the reimplantation of the coronary ostia on the autograft needs large-scale windows on the inclusion tube and is sometimes tricky. Herein, we present a novel approach that could address all these issues.
Surgical Technique
After harvesting, excess fat and muscle of the pulmonary autograft are trimmed (Figure 1). The pulmonary artery wall is resected, leaving 3 mm of remnant, the leaflets' coaptation is checked (Figure 2), and the autograft is sized using Hegar measurers. A straight Dacron tube oversized by 2 mm is used. Three 5/0 stiches are positioned in the middle of the 3 subcommisural triangles and running sutures secure the muscle of the autograft to the Dacron tube (Figure 3). Then, each commissure is attached to the Dacron tube using a Teflon felt 4/0 polypropylene U-stich and the proximal end of the tube is attached to the aortic annulus with three 4/0 polypropylene running sutures (Figure 4). Reimplantation of the coronary ostia is performed directly on the Dacron. The pulmonary conduit is then the distal anastomosis in between the tube and the aorta done. Patients’ pre- and postoperative data are presented in the Table 1.
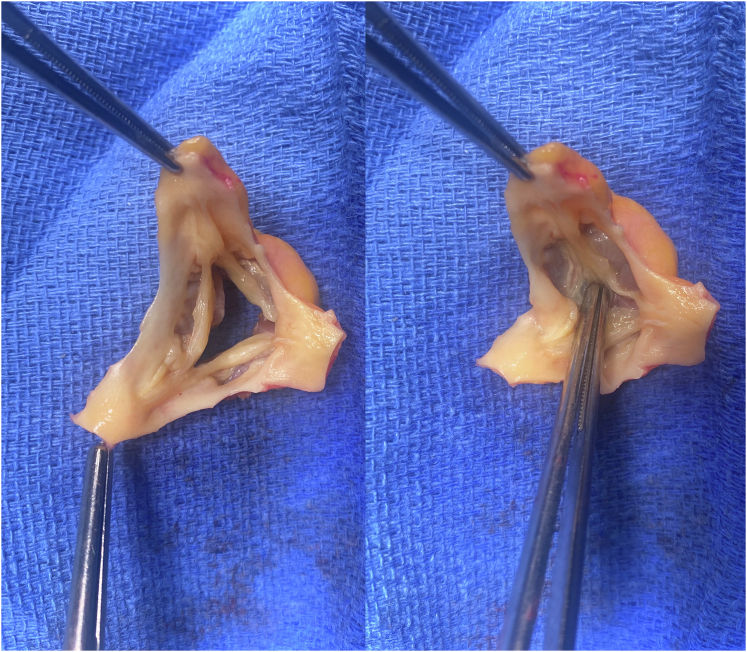
Figure 1.
View from the proximal side of the autograft. The muscle and the excess fat are trimmed to leave about 3 mm of remaining tissue.
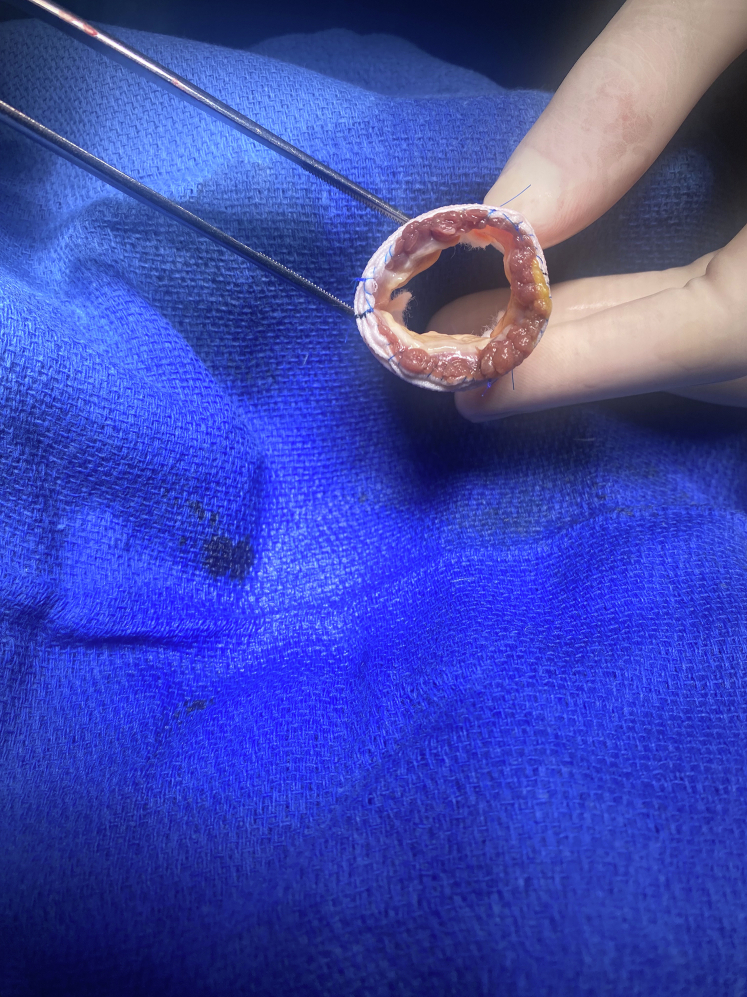
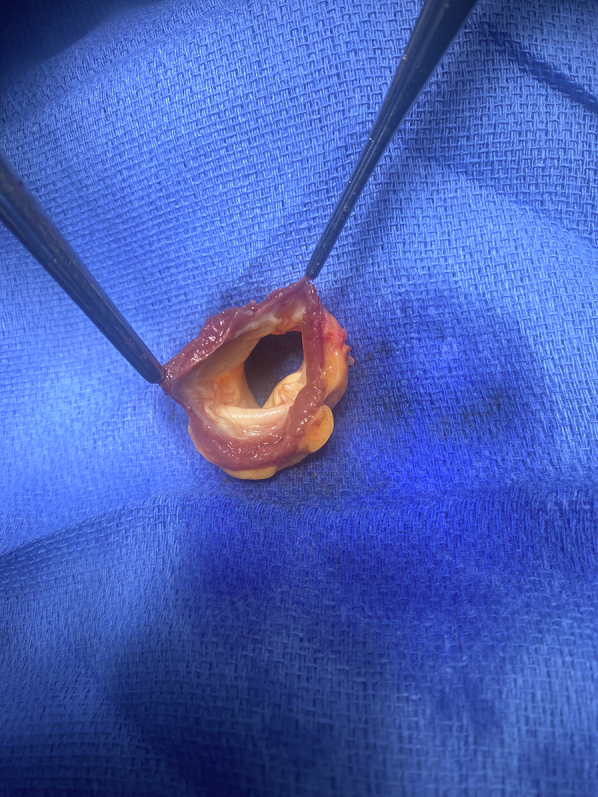
Figure 2.
The pulmonary artery wall is resected, leaving 3 mm of remnants after the leaflets, same as what performed in a David approach (left), then the coaptation of the 3 leaflets is checked (right).
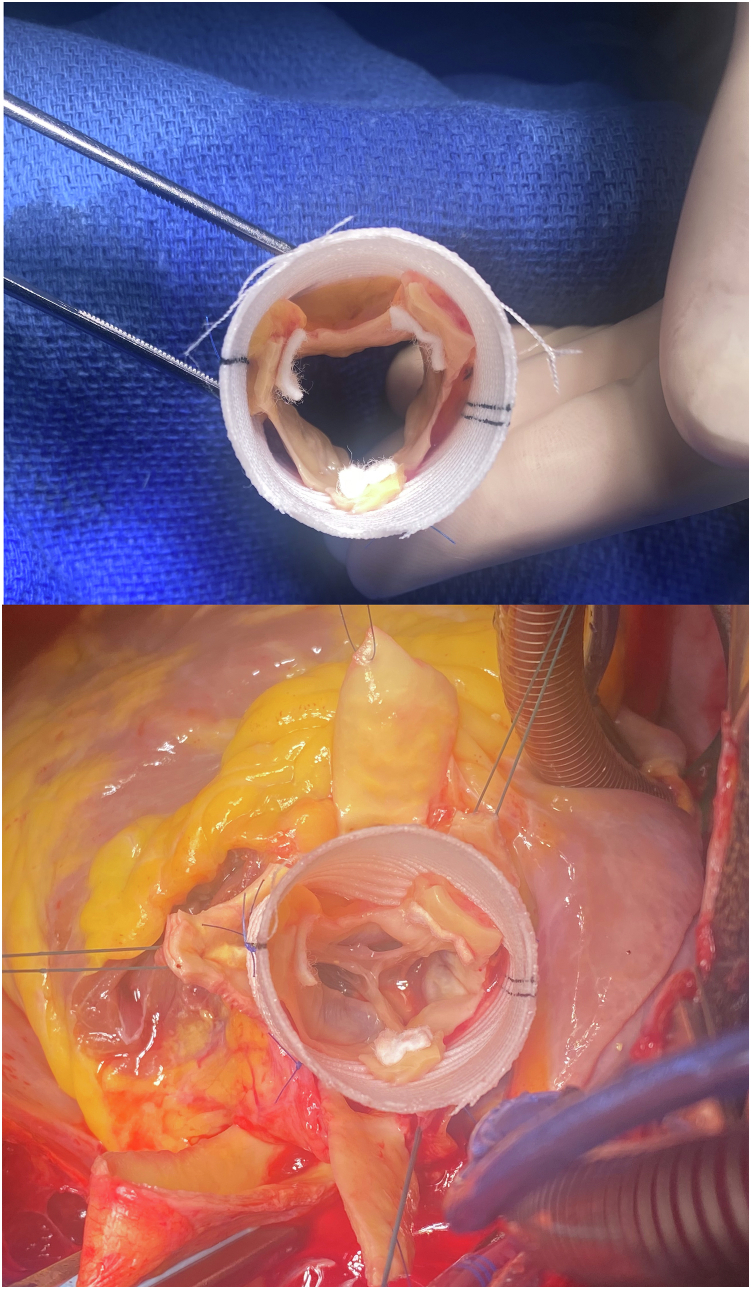
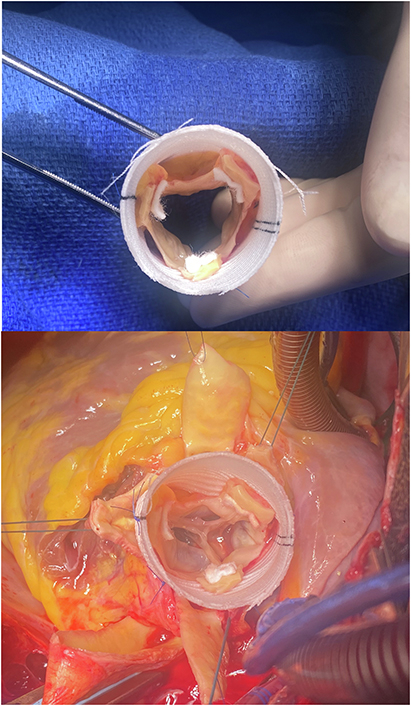
Figure 3.
The muscle below the leaflets is attached to the inclusion Dacron tube using three 5/0 polypropylene running suture after a careful assessment of the annulus geometry.
Figure 4.
Surgical view of the 2F inclusion technique before and after implantation on the aortic annulus. Note that the commissures are fare below the distal end of the Dacron tube without any difficulty to attach with Teflon felt U-stitches.
Table 1.
Pre- and postoperative patient data
| N = 6 | Preoperative | Postoperative | |
|---|---|---|---|
| Gender | |||
| Male | 4 | ||
| Female | 2 | ||
| Age, y | 52.5 (43-58) | ||
| LVEF | 62.5 (55-71) | 59.7 (50-65) | |
| AI 0/I | 5/1 | ||
| Crossclamping time, min | 102 (95-115) | ||
| CPB time, min | 121 (115-132) | ||
| Postoperative autograft valve gradient | 5.7 (4-8) | ||
| Postoperative hospital stay, d | 9.8 (7-13) |
LVEF, Left ventricular ejection fraction; AI, aortic insufficiency; CPB, cardiopulmonary bypass. Ranges are it between brackets.
Discussion
The Ross procedure has been recently the subject of significant research interest. Yokoyama and colleagues2 compared outcomes of the Ross procedure with mechanical aortic valve replacement (M-AVR) and bioprosthetic (B-AVR) valves. Their research involved studies including 4812 patients. All-cause mortality was lower in the Ross procedure compared with M-AVR and B-AVR. Major bleeding rate was lower after the Ross procedure compared with M-AVR, whereas long-term stroke rate was lower following the Ross procedure compared with M-AVR and B-AVR.
El-Hamamsy2 underscored the importance of concentrating care in specialized centers with surgical expertise, allowing the extension of the procedure to patients up to 55 years and not only younger patients. Lastly, the article by Tanaka and colleagues3 discusses strategies for supporting pulmonary autografts while preserving root physiology during the Ross procedure. Juthier and colleagues1 have introduced the use of a Valsalva-shaped tube to prevent dilatation and subsequently valve insufficiency or root aneurysm. We decided to use a straight tube instead of a Valsalva-shaped one to avoid positioning issues inside the bulged segment of the Dacron.
Our approach is designed to deal with 2 of the issues of the Ross procedure when included in a Dacron tube, which are the lack of length of the autograft to allow the replacement of the entire ascending aorta (needing at that point an additional graft) and the difficulty of reimplantation of the coronary ostia on the autograft through large windows on the Dacron. Our approach is a combination of 2 well-known techniques, the David procedure with the resection of the vessel wall, leaving only 3 mm of remnants and subsequently allowing the implantation of the coronary ostia directly to the tube, and the Medtronic 3F stentless valve implantation technique with the attachment of the 3 commissures on the aortic wall (here a Dacron tube) using U stiches. Both techniques have proven an excellent long-term durability. Concerning the replacement of the entire aorta, Tweddell and O'Donnell4 have previously described the inclusion of the autograft into a longer Dacron tube to allow the replacement of the entire aorta without need for an additional tube. Yet, they have to perform a time-consuming distal suture of the autograft inside the Dacron to achieve hemostasis. In our approach, only a suspension of the commissures by three stitches is performed.
The last point of concern is the one rising from the use of the straight Dacron tube instead of a Valsalva-shaped one. Shrestha and colleagues5 have recently reported a series of 677 patients over 27 years using a David I technique with a straight tube, with excellent long-term results.
Conclusions
The 2F technique seems to be a promising approach to simplify the Ross procedure. It is reproducible, and deals with issues faced with the classical technique, such as the lack of length of the autograft and the reimplantation of the coronary ostia on the autograft through large windows on the Dacron tube. However, long-term results are still to be analyzed.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
References
- 1.Juthier F., Banfi C., Vincentelli A., et al. Modified Ross operation with reinforcement of the pulmonary autograft: six-year results. J Thorac Cardiovasc Surg. 2010;139:1420–1423. doi: 10.1016/j.jtcvs.2010.01.032. [DOI] [PubMed] [Google Scholar]
- 2.Yokoyama Y., Kuno T., Toyoda N., et al. Ross procedure versus mechanical versus bioprosthetic aortic valve replacement: a network meta-analysis. J Am Heart Assoc. 2023;12 doi: 10.1161/JAHA.122.027715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanaka D., Mazine A., Ouzounian M., El-Hamamsy I. Supporting the Ross procedure: preserving root physiology while mitigating autograft dilatation. Curr Opin Cardiol. 2022;37:180–190. doi: 10.1097/HCO.0000000000000949. [DOI] [PubMed] [Google Scholar]
- 4.Tweddell J., O’Donnell A. The external-supported Ross procedure with Konno aortoventriculoplasty. Op Tech Thor Cardiovasc Surg. 2021;26:487–509. [Google Scholar]
- 5.Shrestha M., Boethig D., Krüger H., et al. Valve-sparing aortic root replacement using a straight tube graft (David I procedure) J Thorac Cardiovasc Surg. 2022;166:1387–1397.e10. doi: 10.1016/j.jtcvs.2022.01.061. [DOI] [PubMed] [Google Scholar]