Abstract
Introduction
Technical advances and the increasing role of interdisciplinary decision-making may warrant formal definitions of expertise in surgical neuro-oncology.
Research question
The EANS Neuro-oncology Section felt that a survey detailing the European neurosurgical perspective on the concept of expertise in surgical neuro-oncology might be helpful.
Material and methods
The EANS Neuro-oncology Section panel developed an online survey asking questions regarding criteria for expertise in neuro-oncological surgery and sent it to all individual EANS members.
Results
Our questionnaire was completed by 251 respondents (consultants: 80.1%) from 42 countries. 67.7% would accept a lifetime caseload of >200 cases and 86.7% an annual caseload of >50 as evidence of neuro-oncological surgical expertise. A majority felt that surgeons who do not treat children (56.2%), do not have experience with spinal fusion (78.1%) or peripheral nerve tumors (71.7%) may still be considered experts. Majorities believed that expertise requires the use of skull-base approaches (85.8%), intraoperative monitoring (83.4%), awake craniotomies (77.3%), and neuro-endoscopy (75.5%) as well as continuing education of at least 1/year (100.0%), a research background (80.0%) and teaching activities (78.7%), and formal interdisciplinary collaborations (e.g., tumor board: 93.0%). Academic vs. non-academic affiliation, career position, years of neurosurgical experience, country of practice, and primary clinical interest had a minor influence on the respondents’ opinions.
Discussion and conclusion
Opinions among neurosurgeons regarding the characteristics and features of expertise in neuro-oncology vary surprisingly little. Large majorities favoring certain thresholds and qualitative criteria suggest a consensus definition might be possible.
Keywords: Expertise, Surgical neuro-oncology, EANS, CNS tumors
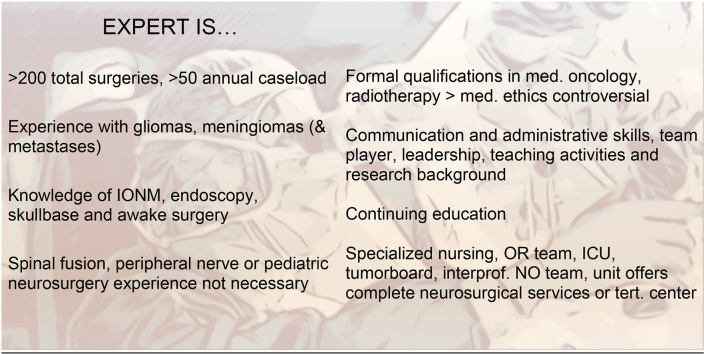
Graphical abstract
Features of an expert in surgical neuro-oncology. IONM, intraoperative neuromonitoring; OR, operating room; ICU, intensive care unit; NO team, neuro-oncology team.
Highlights
-
•
Opinions on expertise in surgical neuro-oncology vary little among neurosurgeons.
-
•
Expertise requires certain operative caseloads (e.g. >200 tumors overall, 50/year).
-
•
Experience with monitoring, awake, skullbase and endoscopic surgery is necessary.
-
•
Other requirements: interdisciplinary collaborations, teaching, research background.
1. Introduction
Experts in surgery have been defined as experienced surgeons with consistently better outcomes than non-experts (Schaverien, 2010). The basic idea that experience translates into expertise seems often confirmed in everyday neurosurgical practice, including brain tumor surgery. Neurosurgery relies heavily on technical skills, and it is not surprising that quite a few researchers have investigated how technical competency can be assessed and taught (Gelinas-Phaneuf and Del Maestro, 2013; Kirsch et al., 2022; Davids et al., 2021). More recently, some groups have investigated a potential role for modern computer-based techniques such as virtual reality simulation and machine learning or virtual communities in this field (Winkler-Schwartz et al., 2019; Titov et al., 2023; Gandamihardja, 2014; Bonrath et al., 2015; Issenberg et al., 2005; Ledwos et al., 2022).
However, more experience does not necessarily equal superior skills; thus, an experienced surgeon is not necessarily an expert (Carnduff and Place, 2022). Expert surgeons typically gain their relevant experience over a relatively short period of time as opposed to surgeons who perform the same number of procedures but over many years. Although a higher volume of performed surgeries and more years of experience have been linked to enhanced technical skills (Hardre et al., 2016), further quantitative and qualitative factors besides hours of experience may play an even more significant role in developing expertise (Carnduff and Place, 2022).
Research involvement is a well-established indicator of expertise, as measured by the number and impact of publications on a specific subject of interest. Engaging in academic teaching, mentoring trainees, and participating in conferences can be viewed as an advanced level of expertise, as teaching someone requires a deep understanding of the subject (Hardre et al., 2016). Personal qualifications and professional attributes, like in-depth medical knowledge, adaptability, communication skills, or leadership, may also contribute to developing surgical expertise (Hardre et al., 2016; Sachdeva, 2020). Other person-independent factors, such as the institutional environment, interdisciplinary work and collaborations, surgical teams, and facilities, may influence an individual's level of expertise (Rethans et al., 2002).
Attitudes and opinions on expertise in neurosurgery, mainly surgical neuro-oncology, will have significant implications in clinical practice. Subspecialization and corresponding certification efforts are underway in Europe and elsewhere. The overall issue is of great interest to all neurosurgeons practicing in this field. Still, opinions regarding the underlying concepts and the figures used to define expertise in neuro-oncology may vary between neurosurgeons but also countries reflecting, e.g., different systems of medical care provision. The EANS Neuro-oncology Section is a platform that brings together all individual EANS members with a specific interest in neuro-oncology research as well as clinical practice. Its panel felt that addressing the expertise issue is of great interest to all section members and the neurosurgical community. To this end, the panel designed the online survey ‘Expertise in surgical Neuro-oncology’ to collect the opinions of fellow neurosurgeons in Europe (and beyond). We were interested in characterizing a potential “common ground” of the various views and approaches.
2. Material and Methods
A questionnaire detailing features and criteria potentially required for surgical neuro-oncology expertise was designed by KG and MS together with the EANS Neuro-oncology Section Panel (Table 1). The survey specified caseloads for certain tumor surgeries. It proposed different clinical skills and surgical experience levels, specific personal qualifications and attributes, as well as distinct practice environments as parameters that describe expertise.
Table 1.
Questionnaire.
| Operative experience | |
|---|---|
| How can expert surgical skills be measured? | |
| Total number of tumor surgeries of the CNS | >50-100 |
| >100-200 | |
| >200-500 | |
| >500 | |
| Annual caseload | >10-20 |
| >20-50 | |
| >50-100 | |
| >100 | |
| The number of procedures performed for certain histologies | Gliomas yes/no |
| Meningiomas yes/no | |
| Metastases yes/no | |
| Other (please specify) | |
| The number of procedures using certain surgical adjuncts and techniques | IONM/mapping yes/no |
| Awake craniotomy yes/no | |
| Endoscopy yes/no | |
| Skull base approaches yes/no | |
| Is experience with both resections and stereotactic biopsies required? | Yes |
| Resection only is enough | |
| Stereotactic biopsy only is enough | |
| Experience with spinal and nerve tumors is required | Spinal tumors (extramed.) yes/no |
| Spinal tumors (intramed.) yes/no | |
| Spinal tumors (epidural) yes/no | |
| Spinal fusion yes/no | |
| Peripheral nerve tumors yes/no | |
| Neuro-oncology expertise includes experience with the following tumors or tumor locations | Pituitary yes/no |
| Vestibular schwannoma yes/no | |
| Other skull base yes/no | |
| Pediatric yes/no | |
| Please define the number of surgeries which define surgical expertise with a certain tumor type |
Number of intrinsic brain tumors |
| >50 | |
| >100 | |
| >200 | |
| Other (please specify) | |
| Number of metastases | |
| >50 | |
| >100 | |
| >200 | |
| Other (please specify) | |
| Number of meningiomas | |
| >50 | |
| >100 | |
| >200 | |
| Other (please specify) | |
|
Other personal skills & qualifications | |
| The following skills are necessary | Communication skills yes/no |
| Team player yes/no | |
| Leadership yes/no | |
| Administrative skills | |
| Teaching activities yes/no | |
| Research background yes/no | |
| Other (please specify) | |
| The following formal qualifications (at least observership/hospitation) are necessary | Medical oncology (chemotherapy) background yes/no |
| Radiotherapy/-surgery yes/no | |
| Medical ethics background yes/no | |
| Medicolegal, regulations, economics yes/no | |
| Other (please specify) | |
| Required continuing education: conference attendance | at least bi-annually |
| ≥1/yr. | |
| Other (please specify) | |
| Necessary publication/research activities |
No activities required |
| Conference abstracts/talks | |
| Publications in scientific journals | |
|
Institution & workplace | |
| The following resources are required | Specialized nursing yes/no |
| Specialized OR team yes/no | |
| Specialized ICU (NICU) yes/no | |
| Specialized tumor board yes/no | |
| Specialized interprofessional neuro-oncology team yes/no | |
| More than one dedicated neuro-oncological surgeon yes/no | |
| Interdisciplinary neuro-oncology | Expert neuro-oncological surgery services rely heavily on in-house collaborations |
| Allied disciplines do not have to be in-house, but formal collaborations and an interdisciplinary tumor board are necessary | |
| “Stand-alone” expert neuro-oncological surgery services are possible | |
| The optimal performance of an expert | requires working in a tertiary center |
| is possible in any neurosurgical unit or department offering complete neurosurgery services and resident training | |
| is possible in any neurosurgical unit or department | |
| is possible in a (private) practice setting | |
A link to the survey was made available to all EANS individual members online via email on the 5th of December 2022. Publication of the survey was accompanied by a letter describing the project and its aims and inviting all addressees to participate. A reminder was sent on the 6th of February 2023. The survey was closed on the February 13, 2023. Participation in the survey was voluntary. We listed every respondent as a study group member if they wished so. All answers were entered into a computer-based database. Further details together with a description and quality assessment of the survey according to modified CHERRIES guidelines can be found in Supplemental Table 1 (Eysenbach, 2004; Turk et al., 2018).
Data were first analyzed descriptively, followed by logistic regression models for the more controversial outcomes (<80% agreement) and questions regarding surgical caseloads while adjusting for potential confounders (years of neurosurgical practice, practice setting, position, interest in neuro-oncology, country of practice). Specifically, the following items were investigated using regression analysis: lifetime and annual caseload, the required number of surgeries for intrinsic tumors, meningiomas, metastases, experience with spinal (extra- and intramedullary, epidural) tumors and spinal fusion, skull base but also pediatric and peripheral nerve tumors, requirements for formal qualifications in medical oncology, radiotherapy/radiosurgery, medical ethics, medicolegal regulations, and economics, academic and educational activities (teaching and publication activities, continuing education), and institutional requirements (specialized nursing and ICU facilities, interprofessional collaborations).
For statistical analysis, countries were grouped into five regions based on the United Nations geoscheme for Europe as follows: i.e., Northern Europe (Denmark, Finland, Ireland, Lithuania, Norway, Sweden, United Kingdom), Western Europe (Austria, Belgium, France, Germany, Netherlands, Switzerland), Southern Europe (Albania, Bosnia and Herzegovina, Greece, Italy, Portugal, Serbia, Spain), Eastern Europe (Belarus, Czech Republic, Poland, Romania, Russian Federation, Slovakia, Ukraine) and all other countries (Afghanistan, Armenia, Australia, Brazil, Canada, Cyprus India, Iraq, Israel, Jordan, Mexico, Pakistan, Saudi Arabia, Singapore, Turkey) (U. Nations). We acknowledge that this will not allow for an analysis of the role of specific organizational aspects of the respective health care systems (such as centralization etc.), which will vary very much between countries even within geographically defined regions.
3. Results
3.1. Participants
The 251 survey participants work in 42 countries (Northern Europe: N = 36, Western Europe: N = 109, Southern Europe: N = 66, Eastern Europe: N = 19; other countries: N = 21).
Ninety-three (37.1%) and 68 (27.1%) of our respondents reported 11–20 and 5–10 years of neurosurgical experience, respectively. 173 (68.9%) of the survey participants were affiliated with a university or university-affiliated hospital, 61 (24.3%) at non-academic hospitals, and 17 (6.8%) were working in a private practice setting. 93 (37.1%) were early career consultants (first ten years post-residency), 67 (26.7%) senior consultants (> ten years post-residency), and 41 (16.3%) department chairs. Neuro-oncology was the main clinical interest in 200 (79.7%) of our respondents. 132 (52.6%) reported skull-base surgery, 92 (36.7%) cerebrovascular neurosurgery, and 81 (32.3%) spinal surgery as (additional) main clinical interests. A baseline table of the participants is provided by our Supplemental Table 2.
3.2. Caseloads and specific operative skills or experiences
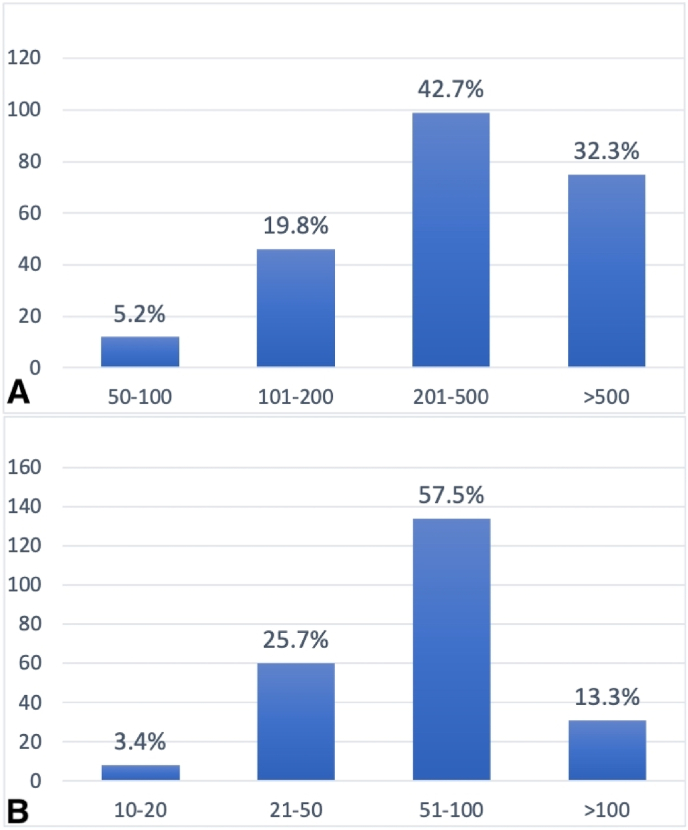
Expert skills were felt to require having performed overall <200 by 58 (25.0%) and >200–500 CNS tumor surgeries by 99 (42.7%) respondents (>500: N = 75, 32.3%), and an annual caseload of ≤50 by 68 (29.2%) and >50–100 by 134 (57.5%) (>100: N = 31, 13.3%), i.e., 157 (67.7%) would accept a lifetime caseload of >200 cases and 202 (86.7%) an annual caseload of >50 as evidence of neuro-oncological surgical expertise (Fig. 1A and B).
Fig. 1.
A) overall and B) annual caseload required to be considered an expert in surgical neuro-oncology.
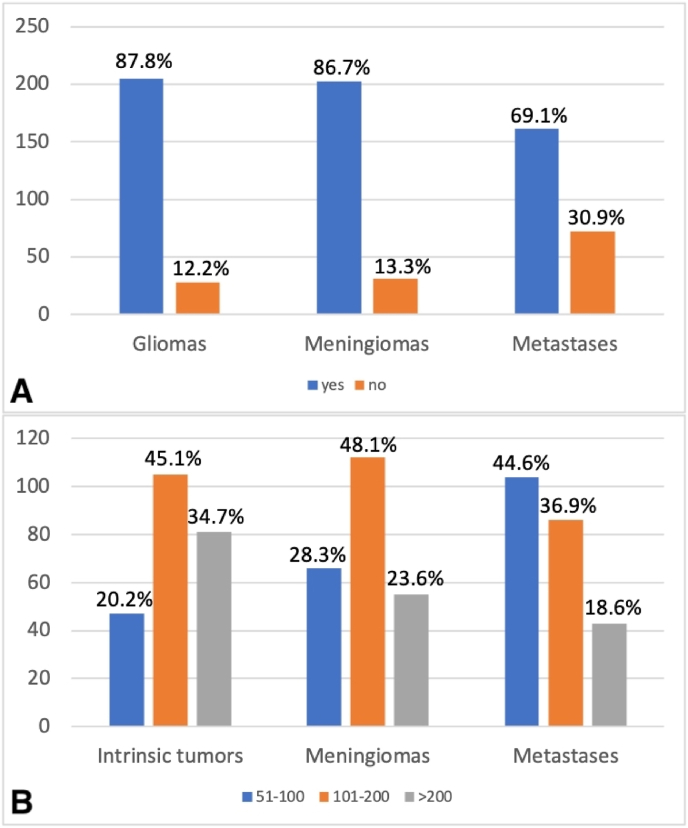
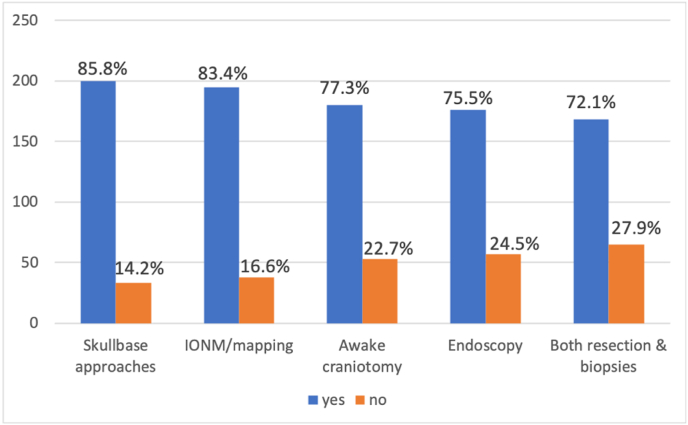
Large or at least solid majorities considered the number of procedures performed for gliomas (N = 205, 87.8%), meningiomas (N = 202, 86.7%) and metastases (N = 161, 69.1%) (Fig. 2A) as well as the use of specific techniques (N = 200, skull-base approaches: 85.8%; intraoperative monitoring: N = 195, 83.4%; awake craniotomies: N = 180, 77.3%; neuro-endoscopy: N = 176, 75.5%) as suitable measures of expertise (Fig. 3). 168 (72.1%) of the respondents also felt that neuro-oncological surgical expertise requires experience with both resections and stereotactic biopsies (Fig. 3). The specific number of procedures for certain tumor entities thought by a majority to define neuro-oncological surgical expertise was >100 intrinsic tumors (N = 186, 79.8%), >100 meningiomas (N = 167, 71.7%), and >100 metastases (N = 129, 56.4%) (Fig. 2B).
Fig. 2.
A) Glioma and meningioma caseloads are considered good indicators of surgical neuro-oncology expertise by more respondents than brain metastases caseload. B) Specific lifetime caseloads for intrinsic tumors, meningiomas, and brain metastases are needed to characterize an expert. 20.2% and 28.3% vs. 44.6% of our participants feel that surgical neuro-oncology expertise requires an overall caseload of 51–100 intrinsic tumors and meningiomas vs. brain metastases.
Fig. 3.
The use of certain surgical adjuncts and techniques is considered by large majorities as a feature of neurosurgical oncology expertise. IONM, intraoperative neuromonitoring.
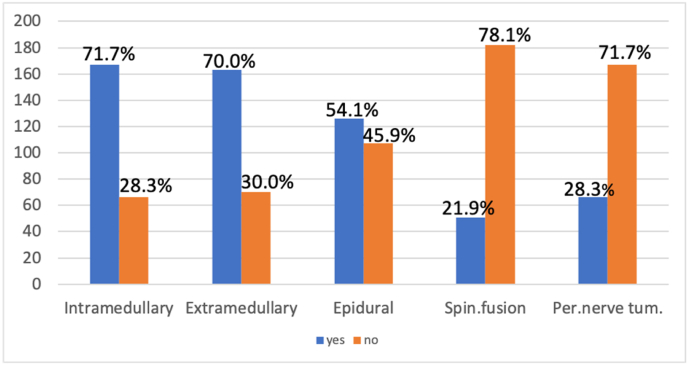
Experience with extramedullary (N = 163, 70.0%) and intramedullary tumors (N = 167.7%, 71.7%) was deemed necessary by large majorities. Opinions concerning surgery for epidural tumors were more divided (in favor: N = 126, 54.1%), and the majority felt that experience with spinal fusion techniques was not a requirement (N = 182, 78.1%) (Fig. 4).
Fig. 4.
Surgical neuro-oncology expertise & spinal and peripheral nerve tumor (Per.nerve tum.) surgery. Mastering intra- and extramedullary tumors is considered an important qualification of a neurosurgical oncology expert, whereas experience with spinal fusion (Spin.fusion) and peripheral nerve tumor surgery is not.
Somewhat mixed responses were also obtained when asking if surgical neuro-oncology expertise includes experience with vestibular schwannoma (in favor: N = 151, 64.8%), other skull base tumors (in favor: N = 152, 65.2%), and pituitary surgeries (in favor: N = 119, 51.1%). Most felt that surgeons who do not treat children (N = 131, 56.2%) or do not have experience with peripheral tumor neurosurgery (N = 167, 71.7%) may still be considered experts in neuro-oncological surgery. (Fig. 4).
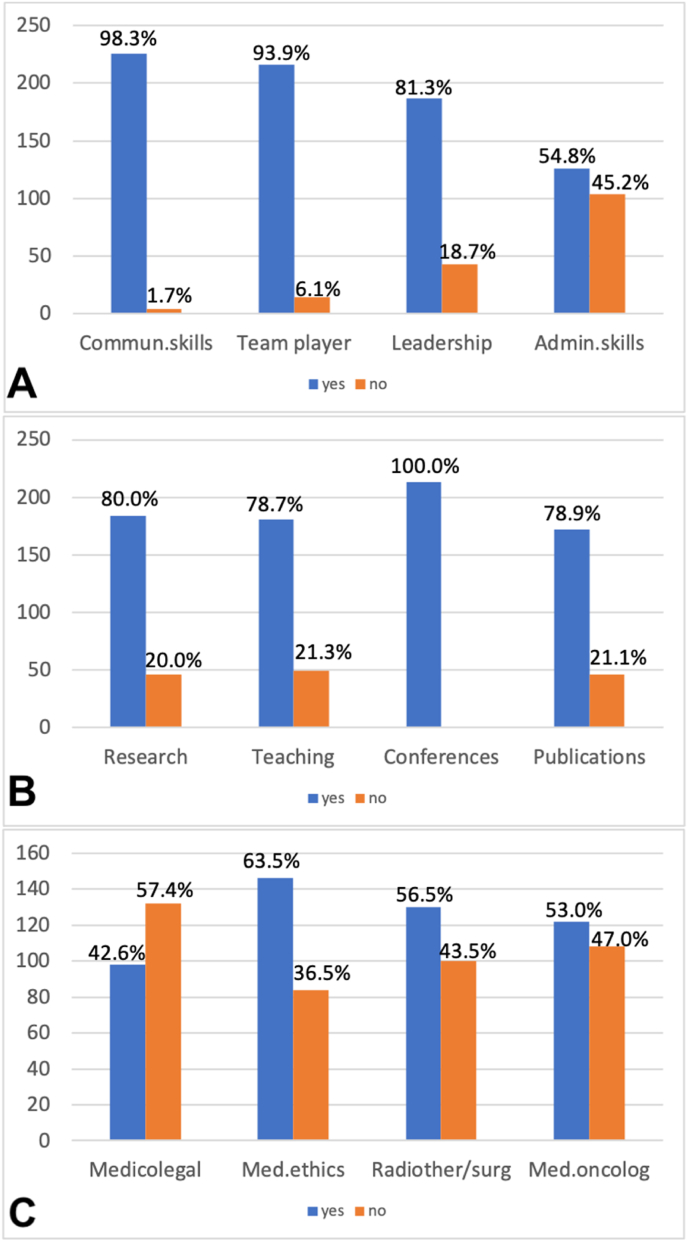
3.3. Non-operative skills and experience
Large majorities believed that expertise requires attending scientific conferences for continuing education (at least bi-annually: N = 110, 51.6%; once/yr.: N = 103, 48.4%), communication skills (N = 226, 98.3%), being a team player (N = 216, 93.9%), leadership (N = 187, 81.3%), a research background (N = 184, 80.0%) and teaching activities (N = 181, 78.7%). Administrative skills were also deemed necessary, but only by a small majority (N = 126, 54.8%). A majority (N = 134, 61.5%) considered publications in scientific journals essential (Fig. 5). Experts are supposed to have some formal medical qualifications outside neurosurgery (at least observerships or hospitations), in medical ethics (N = 146, 63.5%), radiotherapy/radiosurgery (N = 130, 56.5%) and medical oncology (N = 122, 53.1%) by small majorities each, but not necessarily in the fields of medicolegal issues, regulations and business/health care economics (N = 98, 42.6%) (Fig. 5).
Fig. 5.
Non-operative skills and qualifications of an expert in neurooncological surgery. Opinions on A) social competence, B) academic activities, and C) related medical knowledge. Med. ethics, medical ethics; Radiother/surg, radiotherapy/radiosurgery; Med.oncolog, medical oncology.
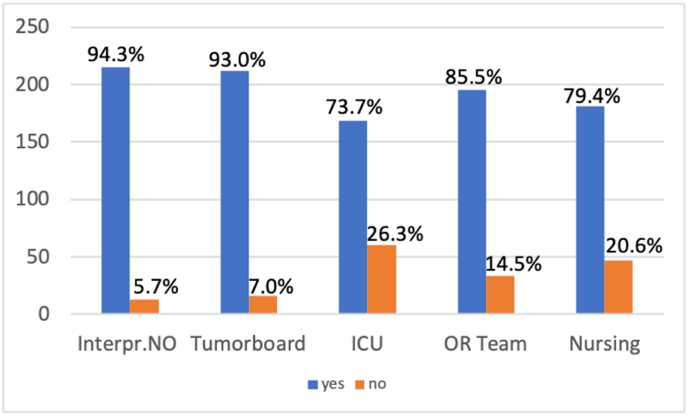
3.4. Institutional requirements
Almost all respondents felt that the optimal institutional setting requires a specialized interprofessional neuro-oncology team (N = 215, 94.3%) and a tumor board (N = 212, 93%). Very large majorities answered that expert neurooncological surgery services require more than one dedicated neuro-oncological surgeon (N = 198, 86.8%), a specialized OR (operating room) team (N = 195, 85.5%), and specialized nursing (N = 181, 79.4%) as well as intensive care facilities (N = 168, 73.7%) (Fig. 6).
Fig. 6.
Institutional and workplace characteristics believed to be required for expert neurosurgical oncology services. Interpr.NO, interprofessional neuro-oncology team; ICU, specialized intensive care unit; OR team, specialized operating room team; Nursing, specialized nursing.
According to 81.1% (N = 185) of our study participants, stand-alone expert neuro-oncological surgery is impossible. In-house collaborations with allied disciplines are essential (N = 197, 86.4%) but not necessarily required as long as formal interdisciplinary cooperations exist (N = 180, 79.0%). The respondents believe that the optimal performance of an expert is possible in all neurosurgical units offering complete services and resident training (N = 113, 49.6%) and, of course, in a tertiary center (N = 84, 36.8%).
3.5. Regression analyses for differences of opinion
As detailed above, answers to the questions and opinions on the items addressed in the survey varied surprisingly little among respondents. Nevertheless, there were some differences of opinion. In order to better understand this variation, we performed logistic regression analyses for all questions whenever there was <80% agreement (and/or when questions addressed caseloads). We studied professional experience (≤10 vs. >10 years), position (senior consultant/department chair vs. resident/junior consultant), practice setting (academic/university affiliated vs. non), main clinical interest in neuro-oncology, and region of practice as potential confounders. Results are shown in Table 2, Table 3, Table 4 and Supplemental Tables 3–6.
Table 2.
Logistic regression analysis for minimum lifetime and annual caseloads. None of the confounders analyzed correlated significantly with responding that experience with >200 cases is necessary to be an expert. Academic affiliation and <10 years of professional expertise significantly predicted voting for higher (>50) annual caseloads as a criterion for expertise.
| Covariate | Lifetime caseload >200 |
Annual caseload >50 |
||
|---|---|---|---|---|
| Odds Ratio (95%-CI) | p-Value | Odds Ratio (95%-CI) | p-Value | |
| ≥10 vs. <10 years of neurosurgical practice | 0.787 [0.373; 1.660] | 0.5287 | 0.380 [0.175; 0.826] | 0.0145 |
| Academic affiliation vs. non-academic | 1.664 [0.864; 3.206] | 0.1280 | 2.676 [1.405; 5.100] | 0.0028 |
| Senior consultant/department chair vs. resident/junior consultant | 1.597 [0.766; 3.331] | 0.2117 | 1.172 [0.572; 2.399] | 0.6649 |
| Main interest neuro-Oncology: Yes vs. No | 1.072 [0.521; 2.206] | 0.8505 | 1.149 [0.544; 2.428] | 0.7165 |
| Country of Practice: West vs. Other | 1.915 [0.579; 6.331] | 0.2869 | 0.620 [0.198; 1.947] | 0.4134 |
| Country of Practice: North vs. Other | 2.251 [0.589; 8.606] | 0.2358 | 0.348 [0.094; 1.281] | 0.1124 |
| Country of Practice: South vs. Other | 1.793 [0.518; 6.213] | 0.3569 | 0.950 [0.284; 3.184] | 0.9340 |
| Country of Practice: East vs. Other | 2.889 [0.629; 13.271] | 0.1726 | 1.106 [0.227; 5.388] | 0.9003 |
Table 3.
Logistic regression analysis for the use of adjunct and operative techniques. Opinions on the use of endoscopy and awake craniotomy vary based on practice location, professional position, and academic affiliation.
| Covariate | Both resections and stereotactic biopsies |
Endoscopy |
Awake craniotomy |
|||
|---|---|---|---|---|---|---|
| Odds Ratio (95%-CI) | p-Value | Odds Ratio (95%-CI) | p-Value | Odds Ratio (95%-CI) | p-Value | |
| ≥10 vs. <10 years of neurosurgical practice | 1.196 [0.573; 2.499] | 0.6336 | 1.007 [0.445; 2.278] | 0.9861 | 2.361 [0.942; 5.918] | 0.0668 |
| Academic affiliation vs. non-academic | 1.155 [0.608; 2.193] | 0.6599 | 1.886 [0.960; 3.702] | 0.0654 | 2.145 [1.087; 4.232] | 0.0278 |
| Senior consultant/department chair vs. resident/junior consultant | 1.125 [0.535; 2.366] | 0.7551 | 0.726 [0.327; 1.609] | 0.4302 | 0.276 [0.111; 0.685] | 0.0055 |
| Main interest neuro-Oncology: Yes vs. No | 1.001 [0.479; 2.093] | 0.9969 | 0.530 [0.213; 1.316] | 0.1713 | 1.278 [0.586; 2.786] | 0.5381 |
| Country of Practice: West vs. Other | 0.783 [0.235; 2.609] | 0.6906 | 0.101 [0.013; 0.811] | 0.0310 | 0.574 [0.160; 2.059] | 0.3941 |
| Country of Practice: North vs. Other | 0.698 [0.175; 2.795] | 0.6119 | 0.212 [0.022; 2.052] | 0.1806 | 0.776 [0.164; 3.677] | 0.7496 |
| Country of Practice: South vs. Other | 0.467 [0.136; 1.597] | 0.2247 | 0.197 [0.023; 1.671] | 0.1365 | 0.444 [0.118; 1.676] | 0.2308 |
| Country of Practice: East vs. Other | 0.452 [0.100; 2.045] | 0.3024 | 0.091 [0.009; 0.883] | 0.0387 | 0.443 [0.087; 2.260] | 0.3272 |
Table 4.
Logistic regression analysis. Opinions on the role of non-neurosurgical (neuro)oncology training and knowledge concerning healthcare economics, regulations, and medicolegal issues vary with country of practice. RT/RS, radiotherapy/radiosurgery.
| Covariate | Formal qualifications |
|||||||
|---|---|---|---|---|---|---|---|---|
| Medical oncology |
RT/RS |
Medical ethics |
Medicolegal, regulations, economics |
|||||
| Odds Ratio (95%-CI) | p-Value | Odds Ratio (95%-CI) | p-Value | Odds Ratio (95%-CI) | p-Value | Odds Ratio (95%-CI) | p-Value | |
| ≥10 vs. <10 years of neurosurgical practice | 0.906 [0.454; 1.809] | 0.7798 | 1.094 [0.550; 2.179] | 0.7975 | 0.834 [0.408; 1.707] | 0.6195 | 0.937 [0.460; 1.907] | 0.8577 |
| Academic affiliation vs. non-academic | 1.660 [0.909; 3.030] | 0.0988 | 1.755 [0.960; 3.208] | 0.0677 | 1.021 [0.544; 1.916] | 0.9484 | 0.849 [0.462; 1.563] | 0.5997 |
| Senior consultant/department chair vs. resident/junior consultant | 1.147 [0.577; 2.279] | 0.6956 | 1.254 [0.630; 2.494] | 0.5195 | 1.304 [0.643; 2.645] | 0.4619 | 1.407 [0.697; 2.838] | 0.3405 |
| Main interest neuro-Oncology: Yes vs. No | 0.961 [0.479; 1.928] | 0.9105 | 0.779 [0.385; 1.577] | 0.4879 | 0.867 [0.421; 1.784] | 0.6978 | 0.531 [0.263; 1.074] | 0.0781 |
| Country of Practice: West vs. Other | 0.558 [0.193; 1.611] | 0.2805 | 0.915 [0.324; 2.583] | 0.8674 | 0.456 [0.139; 1.491] | 0.1937 | 0.367 [0.127; 1.059] | 0.0637 |
| Country of Practice: North vs. Other | 0.110 [0.030; 0.407] | 0.0010 | 0.197 [0.057; 0.686] | 0.0107 | 0.260 [0.069; 0.984] | 0.0474 | 0.149 [0.040; 0.550] | 0.0043 |
| Country of Practice: South vs. Other | 0.456 [0.152; 1.370] | 0.1617 | 0.715 [0.243; 2.100] | 0.5414 | 0.357 [0.106; 1.207] | 0.0976 | 0.299 [0.099; 0.905] | 0.0326 |
| Country of Practice: East vs. Other | 0.617 [0.152; 2.495] | 0.4977 | 0.655 [0.166; 2.587] | 0.5463 | 4.055 [0.401; 41.040] | 0.2358 | 1.106 [0.257; 4.758] | 0.8921 |
We obtained several interesting results. Firstly, reporting surgical neuro-oncology as a primary clinical interest did not significantly influence the answers to the questions studied. Secondly, none of the confounders analyzed was found to be significantly associated with the following outcomes: total (lifetime) caseload, brain metastases caseload as an indicator of expertise, the importance of both stereotactic and resective surgery, importance of extramedullary spinal tumor surgeries, spinal fusion and PNS operations, importance of continuous medical education (conference attendance), medical ethics background, role of specialized nursing and ICU facilities, and optional but not in-house interdisciplinary collaborations.
Thirdly, increasing professional experience, a higher (hierarchical) position, and academic affiliation did have a significant impact on the answers to some questions asked, however, not always pointing into the same directions. E.g. a higher annual caseload was favored by respondents with an academic background, but also participants with lesser years of neurosurgical practice. An academic affiliation correlated with considering awake craniotomies a good measure of expertise, while a senior hierarchical position did not.
Finally, country of practice (assessed using the UN geoscheme) was significantly associated with some of the variation in opinions observed. These effects were seen when analyzing the role of skull base and pituitary operative experience (country of practice/north vs. other - experience with X is important; vestibular schwannoma [OR: 0.130, 95%CI: 0.034–0.492, P = 0.0027], pituitary [OR: 0.270, 95%CI: 0.076–0.961, P = 0.0432], other skullbase surgery [OR: 0.157, 95%CI: 0.042–0.582, P = 0.0057]), neurosurgical endoscopy (country of practice/west vs. other & east vs. other - experience important; OR: 0.101, 95%CI: 0.013–0.811, P = 0.0310 & OR: 0.091, 95%CI: 0.009–0.883, P = 0.0387), and the number of meningioma surgeries considered necessary for neuro-oncology expertise (country of practice/north vs. other & east vs. other - >100 cases necessary; OR: 0.106, 95%CI: 0.012–0.937, P = 0.0435 & OR: 0.076, 95%CI: 0.008–0.732, P = 0.0257). Region of practice also correlated significantly with the responses to questions regarding the importance of teaching (country of practice/north vs. other & west vs. other; OR: 0.098, 95%CI: 0.011–0.901, P = 0.04020 & OR: 0.118, 95%CI: 0.015–0.957, P = 0.0454) and publication activities (country of practice/east vs. other; OR: 0.185, 95%CI: 0.039–0.868, P = 0.0324), medicolegal, regulations, and economics background (country of practice/north vs. other & south vs. other; OR: 0.149, 95%CI: 0.040–0.550, P = 0.0043 & OR: 0.299, 95%CI: 0.099, 95%CI: 0.905-0.0326), but also aspects of the organization of neurosurgical oncology care, i.e., the importance of medical oncology (country of practice/north vs. other; OR: 0.110, 95%CI: 0.030–0.407, P = 0.0010) and radiosurgery/radiotherapy training (country of practice/north vs. other; OR: 0.197, 95%CI: 0.057–0.686, P = 0.0107; see also Table 2, Table 3, Table 4 and Supplemental Tables 3–6).
4. Discussion
Experts have special knowledge and abilities beyond the average person, and experts know when and how to use them. Others will therefore often rely on experts for the management of issues and situations in which such expertise is deemed beneficial and relevant. Every day neurosurgical experience seems to confirm the basic tenet of an intimate relation between experience and outcomes, referred to as expertise. In addition, expertise draws heavily on skills and experiences beyond the operating room. A person's motivation, intellect, emotional intelligence, and innate skills such as advanced pattern recognition, high levels of declarative and procedural knowledge, automaticity in performance, metacognition, and high degree of contextual adaptability play a crucial role in the development of expert performance (Sachdeva, 2020; Dunphy and Williamson, 2004; Ericsson, 2008). Kamp and Selden et al. recently proposed several qualifications that should be achieved during training in surgical neuro-oncology (Kamp et al., 2021; Selden et al., 2013). Expert care probably relies profoundly on organizational and institutional aspects, including non-neurosurgical personnel and other resources (Rethans et al., 2002).
The EANS Tumour Section conducted the present survey to address this topic by detailing the views and opinions of neurosurgeons in Europe (and beyond; the EANS has a substantial number of members who practice outside Europe). We feel that approaching the question of what constitutes surgical neuro-oncology expertise by canvassing the potential experts themselves might be a useful undertaking. Indeed, we were able to collect a sizable number of responses from many colleagues practicing all over Europe and in the Americas, Asia, and Australia, which we feel allows, to some degree, for sketching the neurosurgical perspective on the surgical neuro-oncology expertise issue. Our sample size does not compare unfavorably with other recent international questionnaire-based tumor neurosurgery surveys addressing, e.g., intraoperative tissue sampling strategies during meningioma surgery to assess CNS invasion (Behling et al., 2023) or surgical modality selection in glioblastoma patients (Gerritsen et al., 2022).
The opinions of the survey respondents varied surprisingly little. The possibly most important result of our survey was that it is apparently possible to provide answers to many key questions regarding criteria and even minimum caseload figures on which large majorities in the neurosurgical community would agree. A surgical neuro-oncology expert has performed >200 tumor surgeries (75.0 % agreement), their annual caseload is > 50 (70.8 %), and they have experience with both tumor resections and stereotactic biopsies (72.1%). Experts have communication skills (98.3%), are team players (93.9%), provide leadership (81.30%), engage in teaching activities (78.7%), have some research background (80.0%), and regularly attend scientific conferences (100.0 %). Publication activities (at least talks or abstract presentations, 78.9%) are also required. Personal expertise can be assessed by the number of procedures performed for glioma (88.0%), meningioma (86.7%) and possibly also brain metastases (69.1%), and the number of operations using intraoperative monitoring (83.7%), awake craniotomies (77.3%), neuro-endoscopy (75.5%) and the number of skull base surgeries (85.8%). Institutional requirements include more than one dedicated neuro-oncological surgeon (86.8%), a specialized interprofessional team (94.3%) and nursing (79.4%), a specialized OR team (85.5%) and ICU (73.7%), a specialized tumor board (93.0%) and not necessarily in-house but at least formal interdisciplinary collaborations (79.0%). Our graphical abstract summarizes the features of an expert in surgical neuro-oncology according to the results of our survey (Graphical abstract).
However, we also identified certain more controversial issues. Most notably, opinions varied with respect to the role of experience with surgery for tumors other than gliomas, meningiomas, and metastases. Between 51.1 and 65.2% of respondents felt that neuro-oncology expertise includes experience with pituitary and skull base surgery but not with pediatric brain tumors. Experience with surgery for extra- and intramedullary spinal tumors was considered as a requirement by 70.0 and 71.7%, respectively, while opinions with respect to epidural (i.e. spinal metastases) surgeries were divided, and solid majorities voted against experience with spinal fusion techniques and peripheral nerve tumor surgeries as necessary criteria for surgical neuro-oncology expertise. It is also noteworthy that opinions were somewhat divided with respect to the necessity of having received some formal radio-oncology, radiosurgery and medical oncology training.
We tried to delineate factors contributing to the differences of opinions observed by studying potential confounders. Most notably, a primary clinical neuro-oncology focus did not significantly influence the respondents' answers to any of the questions asked. In addition, for many items, none of the confounders studied accounted significantly for the variation of opinions observed. Academic affiliation, years of neurosurgical experience, and career position had some influence. However, no clear and consistent picture emerged. A higher annual caseload was favored by respondents with an academic background and by participants with a lower hierarchical position (junior consultant/resident). An academic affiliation correlated with considering awake craniotomies a good measure of expertise, while a senior hierarchical position did not. It seems likely that professional experience, career position, and academic affiliation influence one's view of the surgical neuro-oncology expertise issue in somewhat different ways. Country (or better region) of practice also significantly impacted the respondents' opinions of the various issues addressed. This may reflect variations in practice settings throughout Europe, e.g., skull base specialists perform certain skull base surgeries in some countries and as part of the general neurooncological surgery workload in others. Controversial opinions, of course, negatively impact any attempts at arriving at some kind of consensus. Our data indicate that the role of any systematic influence of experience, hierarchical position, academic perspective, primary clinical neuro-oncology interest, and region of practice seems limited, which should positively impact any consensus-building effort. Even though a potential future consensus opinion will have to be restricted to those items of our survey that were agreed upon by large majorities,
Of note, the opinions and views expressed by the survey respondents are in part reflected in the recommendations that can be found in current (European) neuro-oncology guidelines (EANO glioma, EANO-ESMO brain mets, EANO meningioma, EANO vestibular schwannoma) (Goldbrunner et al., 2020, 2021; Le et al., 2021; Weller et al., 2021). All guidelines stress interdisciplinarity, and there was also almost a consensus among survey participants with respect to the importance of an interdisciplinary setting. Opinions only varied on the necessity of formal radio-oncology and medical oncology training of a surgical neuro-oncology expert. The EANO adult glioma guideline explicitly comments on the pertinent role of intraoperative monitoring and awake surgery as well as bioptic surgery which fits well with the importance of these issues attributed to the characterization of surgical neuro-oncology expertise by the survey respondents (EANO glioma). However, guidelines do not comment on the expertise issue in general and also not on specifics such as required qualifications and experience with certain pathologies.
Our analysis certainly has important shortcomings. First of all, the overall approach of performing a survey of opinions and views when addressing the issue of neuro-surgical oncology expertise has inherently very relevant and obvious limitations. Our questionnaire did not address general or interdisciplinary neuro-oncology expertise. It missed specific questions about the relevance of knowledge of principles of neuro-oncology, neuropathology, radiation oncology and other specialties outside neurosurgery relevant for the management of neuro-oncological patients. While we collected a sizable number of responses, our sample may not necessarily have been representative. The response rate varied between regions, likely reflecting, e.g., the variable numbers of EANS individual members in the various countries. A large majority of our respondents reported working at university or university-affiliated institutions. However, despite a probable role for these and other confounders, the overall picture was of agreement between survey participants concerning many items and questions.
5. Conclusions
In conclusion, our survey describes the opinions among neurosurgeons in Europe (and beyond) regarding the features and characteristics of expertise in neuro-oncology that vary surprisingly little. Large majorities favoring certain thresholds and qualitative criteria suggest a consensus definition might be possible.
Authors’ contribution
KG and MS designed and conceptualized the survey; KG, LM, and MS performed literature research, AH conducted the statistical analysis, KG and MS drafted the manuscript for important intellectual content; JB, MB, EC, NF, CF, RG, CJ, PM, DN, RR, PS, CS, FS, AJPEV, LAM, AH, KG and MS revised the manuscript critically for important intellectual content and approved the final version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgments
The authors express their gratitude to the fellow neurosurgeons who agreed to participate in this survey and high gratitude to the staff of the EANS Prodromos Nikolaidis and Anna Rek for launching the survey through EANS platform.
Handling Editor: W Peul
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bas.2024.102822.
Contributor Information
K. Gousias, Email: k.gousias@iatriko.gr.
A. Hoyer, Email: annika.hoyer@uni-bielefeld.de.
L.A. Mazurczyk, Email: mazurczyk.luc@live.unic.ac.cy.
J. Bartek, Jr., Email: jiri.bartek@regionstockholm.se.
M. Bruneau, Email: Michael.Bruneau@uzbrussel.be.
E. Celtikci, Email: drceltikci@gmail.com.
N. Foroglou, Email: nforoglou@auth.gr.
C. Freyschlag, Email: christian.freyschlag@tirol-kliniken.at.
R. Grossman, Email: rachelyg@hotmail.com.
C. Jungk, Email: Christine.Jungk@med.uni-heidelberg.de.
P. Metellus, Email: philippe.metellus@outlook.fr.
D. Netuka, Email: netuka.david@gmail.com.
R. Rola, Email: rola.radoslaw@gmail.com.
P. Schucht, Email: Philippe.Schucht@insel.ch.
C. Senft, Email: Christian.Senft@med.uni-jena.de.
F. Signorelli, Email: signorelli2007@gmail.com.
A.J.P.E. Vincent, Email: a.vincent@erasmusmc.nl.
M. Simon, Email: Matthias.Simon@evkb.de.
for the EANS Surgical Neuro-oncology Expertise Survey working group:
Rachit Agrawal, Luigi Albano, George A. Alexiou, Amanj Ali, Rafid Al-Mahfoudh, Michael Amoo, Christos Anagnostopoulos, Sven Bamps, Soham Bandyopadhyay, Damiano G. Barone, Fabio Barone, Sami Barrit, Felix Behling, Alin Blaga, Alexandros Boukas, Paul Brennan, Vicki M. Butenschoen, Mauro Campello, Areda Cara, Salvatore Chibbaro, Robert Chrenko, Pere J. Cifre Serra, Hans Clusmann, Alba Corell, Jan F. Cornelius, Marcello D'Andrea, Andreas K. Demetriades, Steven De Vleeschouwer, Richard Drexler, Johnny Duerinck, Ruben V. Fanarjyan, Alejandro Fernandez-Coello, Kostas Fountas, Thomas M. Freiman, Vadim Gadzhiagaev, Miltiadis Georgiopoulos, Nathalie Gilis, Jagos Golubovic, Eric Goulin Lippi Fernandes, Giovanni Grasso, Francesco Guerrini, Beste Gulsuna, Ciaran S. Hill, Julius Höhne, Markus Holling, Ievgenii Iarmoliuk, Florian Ioan-Alexandru, Tamara Ius, Kestutis Jacikevicius, Asgeir S. Jakola, Paweł Jakubowski, Georgios Kalantzis, Konstantina Karabatsou, Ramez Kirollos, Ralph König, Danil A. Kozyrev, Dietmar Krex, Barbara Ladisich, Ruth Lau, Yauhen Lizunou, Arnaud Lombard, Hu Liang Low, José Luís Alves, Yazid Maghrabi, Marco Mammi, Ala Marji, Luca Massimi, Ioannis Mavridis, Aaron Lawson McLean, Anna C. Lawson McLean, Bernhard Meyer, Malte Mohme, Pedro Moura Branco, Michael Müther, Issam Musleh, Danial Nasiri, Ramon Navarro, Ibrahim Omerhodzic, Marvin Darkwah Oppong, Nikolaos A. Paidakakos, Zoi Pantera, Mohammed A. Patel, Mateusz Pawlowski, Athanasios Petridis, Adrian J. Praeger, Stephen Price, Franz Ricklefs, Luigi Rigante, Florian Ringel, Pierre A. Robe, Karl Rössler, Eduarda Sá-Marta, Jose L. Sanmillan, Alba Scerrati, Matthias Schneider, Henry W.S. Schroeder, Michael Schwake, Mohamed Shoaib, Octavian Mihai Sirbu, Iñigo L. Sistiaga, Tomasz J. Skajster, Albertas Sliauzys, Vitaly Sokotukhin, Jehuda Soleman, Veit M. Stoecklein, Eric Suero Molina, Wojciech Świątnicki, Νikolaos Syrmos, Graziano Taddei, Avin Taher, Martin Tamarit, Mark ter Laan, Theocharis Theocharous, Dieter Thijs, Leonidas Trakolis, Monica Truffelli, Miriam Weiss, Eberhard Uhl, Laura Grazia Valentini, Dimitri Vanhauwaert, Bassel Zebian, Bojana Zivkovic, and Matteo Zoli
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- Behling F., Bruneau M., Honegger J., Berhouma M., Jouanneau E., Cavallo L., Cornelius J.F., Messerer M., Daniel R.T., Froelich S., Mazzatenta D., Meling T., Paraskevopoulos D., Roche P.H., Schroeder H.W.S., Zazpe I., Voormolen E., Visocchi M., Kasper E., Schittenhelm J., Tatagiba M. Differences in intraoperative sampling during meningioma surgery regarding CNS invasion - results of a survey on behalf of the EANS skull base section. Brain Spine. 2023;3 doi: 10.1016/j.bas.2023.101740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonrath E.M., Dedy N.J., Gordon L.E., Grantcharov T.P. Comprehensive surgical Coaching Enhances surgical skill in the operating room: a Randomized Controlled trial. Ann. Surg. 2015;262:205–212. doi: 10.1097/SLA.0000000000001214. [DOI] [PubMed] [Google Scholar]
- Carnduff M., Place R. The relation of surgical volume to competence: when is Enough, Enough? Mil. Med. 2022;187:64–67. doi: 10.1093/milmed/usab356. [DOI] [PubMed] [Google Scholar]
- Davids J., Manivannan S., Darzi A., Giannarou S., Ashrafian H., Marcus H.J. Simulation for skills training in neurosurgery: a systematic review, meta-analysis, and analysis of progressive scholarly acceptance. Neurosurg. Rev. 2021;44:1853–1867. doi: 10.1007/s10143-020-01378-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunphy B.C., Williamson S.L. In pursuit of expertise. Toward an educational model for expertise development. Adv Health Sci Educ Theory Pract. 2004;9:107–127. doi: 10.1023/B:AHSE.0000027436.17220.9c. [DOI] [PubMed] [Google Scholar]
- Ericsson K.A. Deliberate practice and acquisition of expert performance: a general overview. Acad. Emerg. Med. 2008;15:988–994. doi: 10.1111/j.1553-2712.2008.00227.x. [DOI] [PubMed] [Google Scholar]
- Eysenbach G. Improving the quality of web surveys: the Checklist for reporting results of Internet E-surveys (CHERRIES) J. Med. Internet Res. 2004;6:e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandamihardja T.A. The role of communities of practice in surgical education. J. Surg. Educ. 2014;71:645–649. doi: 10.1016/j.jsurg.2014.03.006. [DOI] [PubMed] [Google Scholar]
- Gelinas-Phaneuf N., Del Maestro R.F. Surgical expertise in neurosurgery: integrating theory into practice. Neurosurgery. 2013;73(Suppl. 1):30–38. doi: 10.1227/NEU.0000000000000115. [DOI] [PubMed] [Google Scholar]
- Gerritsen J.K.W., Broekman M.L.D., De Vleeschouwer S., Schucht P., Jungk C., Krieg S.M., Nahed B.V., Berger M.S., Vincent A. Decision making and surgical modality selection in glioblastoma patients: an international multicenter survey. J. Neuro Oncol. 2022;156:465–482. doi: 10.1007/s11060-021-03894-5. [DOI] [PubMed] [Google Scholar]
- Goldbrunner R., Weller M., Regis J., Lund-Johansen M., Stavrinou P., Reuss D., Evans D.G., Lefranc F., Sallabanda K., Falini A., Axon P., Sterkers O., Fariselli L., Wick W., Tonn J.C. EANO guideline on the diagnosis and treatment of vestibular schwannoma. Neuro Oncol. 2020;22:31–45. doi: 10.1093/neuonc/noz153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldbrunner R., Stavrinou P., Jenkinson M.D., Sahm F., Mawrin C., Weber D.C., Preusser M., Minniti G., Lund-Johansen M., Lefranc F., Houdart E., Sallabanda K., Le Rhun E., Nieuwenhuizen D., Tabatabai G., Soffietti R., Weller M. EANO guideline on the diagnosis and management of meningiomas. Neuro Oncol. 2021;23:1821–1834. doi: 10.1093/neuonc/noab150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardre P.L., Nihira M., LeClaire E., Moen M. Defining expertise in Gynecologic surgery: Perspectives of expert Gynecologic surgeons. Female Pelvic Med. Reconstr. Surg. 2016;22:399–403. doi: 10.1097/SPV.0000000000000336. [DOI] [PubMed] [Google Scholar]
- Issenberg S.B., McGaghie W.C., Petrusa E.R., Lee Gordon D., Scalese R.J. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med. Teach. 2005;27:10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]
- Kamp M.A., Malzkorn B., von Sass C., DiMeco F., Hadjipanayis C.G., Senft C., Rapp M., Gepfner-Tuma I., Fountas K., Krieg S.M., Neukirchen M., Florian I.S., Schnell O., Mijderwijk H.J., Perin A., Baumgarten P., van Lieshout J.H., Thon N., Renovanz M., Kahlert U., Spoor J.K.H., Hanggi D., McLean A.L., Maurer M., Sarrubbo S., Freyschlag C.F., Schmidt N.O., Vergani F., Jungk C., Stein M., Forster M.T., Weinberg J.S., Sinclair J., Belykh E., Bello L., Mandonnet E., Moiyadi A., Sabel M. Proposed definition of competencies for surgical neuro-oncology training. J. Neuro Oncol. 2021;153:121–131. doi: 10.1007/s11060-021-03750-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirsch E.P., Suarez A., McDaniel K.E., Dharmapurikar R., Dunn T., Lad S.P., Haglund M.M. Construct validity of the Surgical Autonomy Program for the training of neurosurgical residents. Neurosurg. Focus. 2022;53:E8. doi: 10.3171/2022.5.FOCUS22166. [DOI] [PubMed] [Google Scholar]
- Ledwos N., Mirchi N., Yilmaz R., Winkler-Schwartz A., Sawni A., Fazlollahi A.M., Bissonnette V., Bajunaid K., Sabbagh A.J., Del Maestro R.F. Assessment of learning curves on a simulated neurosurgical task using metrics selected by artificial intelligence. J. Neurosurg. 2022:1–12. doi: 10.3171/2021.12.JNS211563. [DOI] [PubMed] [Google Scholar]
- Rethans J.J., Norcini J.J., Baron-Maldonado M., Blackmore D., Jolly B.C., LaDuca T., Lew S., Page G.G., Southgate L.H. The relationship between competence and performance: implications for assessing practice performance. Med. Educ. 2002;36:901–909. doi: 10.1046/j.1365-2923.2002.01316.x. [DOI] [PubMed] [Google Scholar]
- Sachdeva A.K. Acquiring and maintaining lifelong expertise in surgery. Surgery. 2020;167:787–792. doi: 10.1016/j.surg.2019.08.023. [DOI] [PubMed] [Google Scholar]
- Schaverien M.V. Development of expertise in surgical training. J. Surg. Educ. 2010;67:37–43. doi: 10.1016/j.jsurg.2009.11.002. [DOI] [PubMed] [Google Scholar]
- Selden N.R., Abosch A., Byrne R.W., Harbaugh R.E., Krauss W.E., Mapstone T.B., Sagher O., Zipfel G.J., Derstine P.L., Edgar L. Neurological surgery milestones. J Grad Med Educ. 2013;5:24–35. doi: 10.4300/JGME-05-01s1-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov O., Bykanov A., Pitskhelauri D. Neurosurgical skills analysis by machine learning models: systematic review. Neurosurg. Rev. 2023;46:121. doi: 10.1007/s10143-023-02028-x. [DOI] [PubMed] [Google Scholar]
- Turk T., Elhady M.T., Rashed S., Abdelkhalek M., Nasef S.A., Khallaf A.M., Mohammed A.T., Attia A.W., Adhikari P., Amin M.A., Hirayama K., Huy N.T. Quality of reporting web-based and non-web-based survey studies: what authors, reviewers and consumers should consider. PLoS One. 2018;13 doi: 10.1371/journal.pone.0194239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U. Nations.
- Weller M., van den Bent M., Preusser M., Le Rhun E., Tonn J.C., Minniti G., Bendszus M., Balana C., Chinot O., Dirven L., French P., Hegi M.E., Jakola A.S., Platten M., Roth P., Ruda R., Short S., Smits M., Taphoorn M.J.B., von Deimling A., Westphal M., Soffietti R., Reifenberger G., Wick W. EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat. Rev. Clin. Oncol. 2021;18:170–186. doi: 10.1038/s41571-020-00447-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkler-Schwartz A., Yilmaz R., Mirchi N., Bissonnette V., Ledwos N., Siyar S., Azarnoush H., Karlik B., Del Maestro R. Machine learning Identification of surgical and operative factors associated with surgical expertise in virtual reality simulation. JAMA Netw. Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.8363. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.