Abstract
Introduction
The incidence of type 2 diabetes is increasing globally. Recent research suggests that loneliness could be a potential risk factor for the development of type 2 diabetes. We aimed to investigate the association between loneliness and type 2 diabetes and the modifying effect of mental disorders.
Research design and methods
We conducted a prospective study including 465 290 adults (aged ≥16 years) who participated in either the Danish Health and Morbidity Survey or the Danish National Health Survey between 2000 and 2017. Loneliness was based on self-report, while type 2 diabetes was measured using an algorithm combining several health registers including type 2 diabetes patients treated both within the hospital sector and general practice. Cox proportional hazards regressions were used to estimate hazard ratios (HRs) and 95% confidence intervals (95% CIs).
Results
During a mean follow-up time of 6.3 years, 13 771 individuals (3%) developed type 2 diabetes. Feeling lonely once in a while was associated with a 14% increased risk of type 2 diabetes (95% CI 1.09 to 1.20), while feeling lonely often was associated with a 24% increased risk (95% CI 1.14 to 1.34), independent of sociodemographic factors and body mass index. The association was stronger among individuals without a mental disorder (HR 1.21, 95% CI 1.10 to 1.34 among those feeling lonely often) compared with those with a mental disorder (HR 1.07, 95% CI 0.93 to 1.23).
Conclusions
Loneliness independently increased the risk of type 2 diabetes. The effect was more pronounced in individuals without a mental disorder, as having a mental disorder itself likely increases the risk of type 2 diabetes. These findings emphasize the importance of addressing loneliness as a modifiable risk factor in preventing type 2 diabetes.
Keywords: Diabetes Mellitus, Type 2; Epidemiology; Mental Disorders
WHAT IS ALREADY KNOWN ON THIS TOPIC
The global incidence of type 2 diabetes is on the rise, and in Denmark there is a concurrent increase in the prevalence of individuals experiencing loneliness.
Studies suggest that loneliness may constitute a potential risk factor in the development of type 2 diabetes. However, there is currently a lack of studies investigating the modifying effect of mental disorders.
WHAT THIS STUDY ADDS
This study adds to the growing body of evidence showing that loneliness increased the risk of incident type 2 diabetes.
The association was stronger among individuals without a mental disorder compared with those with a mental disorder.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE, OR POLICY
The study findings highlight the importance of addressing loneliness as a modifiable risk factor in the prevention of type 2 diabetes.
Introduction
Loneliness has been associated with adverse physical and psychological health outcomes such as depression and anxiety,1 2 cardiovascular disease,3 and all-cause mortality.4 5 Additionally, previous studies have consistently found an association between loneliness and type 2 diabetes.6–12
Several mechanisms underlying the association between loneliness and adverse health outcomes have been suggested comprising three pathways: a biological, a behavioral, and a psychological pathway.13 The biological pathway is related to metabolic mechanisms increasing the risk of obesity and the metabolic syndrome, both of which are associated with loneliness14 and type 2 diabetes.15 The second pathway suggested is through adverse health behaviors, although research related to loneliness has yielded inconsistent results.8 16–18 Lastly, the third pathway is the psychological pathway. Previous research suggests that perceived stress, depression, and anxiety may have a notable impact on the association between loneliness and type 2 diabetes.7 Furthermore, the association between loneliness and psychological conditions such as depression appear to be bidirectional.19 20 Thus, psychological conditions are important to consider when investigating the association between loneliness and type 2 diabetes.
Despite a growing body of literature demonstrating an association between loneliness and type 2 diabetes, the current evidence is limited by several methodological shortcomings. Some studies are cross-sectional,8–10 which may induce temporality issues. Other studies focus exclusively on older age groups6 9 12 or particular ethnic minority groups,10 potentially limiting the generalizability of the findings. Most importantly, the majority of studies have important methodological limitations concerning the measurement of type 2 diabetes, as most studies rely on self-reported data6 8 9 or data from administrative hospitals registers.7 However, both approaches have their limitations. Self-reported data may lead to misclassification, while data from administrative hospital registers only cover patients treated within the secondary sector. This is problematic, considering that the majority (80%) of all type 2 diabetes patients are treated within general practice.21
Therefore, the first aim of this study was to investigate the prospective association between loneliness and incident type 2 diabetes in a representative sample of individuals aged 16 years or older, including type 2 diabetes patients treated both within the hospital sector and general practice. The second aim was to investigate whether the presence of a mental disorder modifies the association.
Research design and methods
In this prospective study, all included individuals were followed from survey response until date of incident type 2 diabetes, emigration, death, or 31 December 2018, whichever occurred first.
Study population
The study population comprised individuals who participated in the Danish Health and Morbidity Surveys from 2000 (n=16 688, response proportion 74.2%) or 2005 (n=14 566, response proportion 66.7%),22 or in the Danish National Health Surveys from 2010 (n=1 77 639, response proportion 59.5%), 2013 (n=1 62 283, response proportion 54.0%), or 2017 (n=1 83 372, response proportion 58.7%).23 The Danish Health and Morbidity Survey has been conducted regularly since 1987, focusing on health and morbidity trends in the adult Danish population (aged 16 years or older).22 Since 2010, the Danish Health and Morbidity Survey has been incorporated into the Danish National Health Survey, which is based on six mutually exclusive subsamples: one from each of the five Danish regions and one national sample, the latter being the Danish Health and Morbidity Survey.23 Some individuals participated in multiple surveys, and to avoid duplicates only their responses to the first survey were included, excluding responses from later survey participation (n=44 492). Thus, a total of 510 056 individuals responded to the questionnaires.
Measures
Exposure: loneliness
The question “Does it ever happen that you are alone, even though you would prefer to be together with other people?” was used as a proxy measure of loneliness, and was obtained the year of baseline (2000, 2005, 2010, 2013, and 2017). Response options were ‘Yes, often’, ‘Yes, once in a while’, ‘Yes, but rarely’, and ‘No’. These were categorized into three groups reflecting those who feel lonely often (‘Yes, often’), once in a while (‘Yes, once in a while’), and those who do not feel lonely (‘Yes, but rarely’ and ‘No’).
Recognizing the importance of considering different dimensions of loneliness, we also used the Three-Item Loneliness Scale (T-ILS) as a comprehensive measure of loneliness. The Danish National Health Survey consists of a mandatory standard questionnaire, which can be supplemented with specific questions on topics of specific interest by each region. The North Denmark Region, Region Zealand, and the Capital Region of Denmark added T-ILS to the 2017 survey, which is a validated and short version of the UCLA Loneliness Scale.24 T-ILS contains the following three questions: (1) “How often do you feel isolated from others?”, (2) “How often do you feel you lack companionship?”, and (3) “How often do you feel left out?”. Each item is rated on a three-point Likert scale. Thus, the sum of the items ranges from 3 to 9, where higher scores indicate greater loneliness. T-ILS was classified using the trichotomous classification dividing respondents into not lonely (scores of 3–4), moderately lonely (scores of 5–6), and severely lonely (scores of 7–9). We used T-ILS as a measure of loneliness in a subsample (n=74 755), while ‘unwanted alone’ served as our primary measure to accommodate a larger and representative study population.
Outcome: type 2 diabetes
We utilized the algorithm developed by Carstensen et al 25 to identify type 2 diabetes patients. Hence, type 2 diabetes was defined from several health registers as the earliest occurrence of any of the following: the date of first diabetes diagnosis in the Danish National Patient Register (International Classification of Diseases 10th Revision (ICD-10) code E11),26 the date of the first filled prescription of any antidiabetic drug (Anatomical Therapeutic Chemical (ATC) Classification System group A10A; insulins or A10B; oral antidiabetics) in the Danish National Prescription Registry,27 the date of first use of podiatry for patients with diabetes in the Danish National Health Service Register,28 the date of the first type 2 diabetes diagnosis in the Danish Adult Diabetes Database,21 or the date of the first eye screening in the Danish Registry of Diabetic Retinopathy.29
The Danish healthcare system is universal and ensures free access to healthcare services both within the hospital sector and general practice. In addition, prescribed medication is partially reimbursed for all residents. This allows for a comprehensive measure of type 2 diabetes that does not depend on membership of an insurance scheme.
Moderating variables: mental disorders
Information on mental disorders was obtained from the Danish National Patient Register within 5 years prior to survey response and was categorized as: mental and behavioral disorders due to psychoactive substance use (ICD-10 codes F10–F19), schizophrenia and psychosis (F20–F29), affective disorders (F30–F39), and nervous disorders (F40–F49). Additionally, the Danish National Prescription Registry was utilized to identify prescriptions of antidepressants (ACT group N06A) and prescriptions of drugs used in addictive disorders (ACT group N07B) within 5 years prior to survey response. Study respondents had to redeem at least two prescriptions to be categorized as users of these two types of medication. The category of affective disorders (F30–F39) and the use of antidepressants (ATC group N06A) were then combined into a single variable representing affective disorders. Likewise, the category of mental and behavioral disorders due to psychoactive substance use (F10–F19) and drugs used in addictive disorders (ATC group N07B) were combined into a single variable reflecting mental and behavioral disorders due to psychoactive substance use.
Covariates
Covariates were obtained at the year of baseline (2000, 2005, 2010, 2013, and 2017). Information on sex (female, male), age (year of birth), marital status (married, unmarried, divorced, widow), cohabitation (living alone, living with others), and country of origin (Danish, Western, non-Western) was extracted from the Danish Civil Registration System. Highest obtained educational level was obtained from the Danish Education Register30 and was categorized into six groups (elementary school, upper secondary education, vocational education, short-cycle higher education, medium-cycle higher education, and long-cycle higher education).
Self-reported information on health behaviors was derived from the surveys. These covariates included smoking status (daily smokers, occasional smokers, former smokers, and non-smokers), physical activity (physically active vs physically inactive), weekly alcohol consumption (no intake, low/moderate consumption 1–141–21 drinks/week for women (men) and high consumption >14 (>21) drinks/week for women (men)), and the intake of salad on a weekly basis, which was used as a proxy of dietary habits (every day/several times a day, occasionally, and never/rarely). Further, self-reported height (cm) and weight (kg) were used to calculate respondents’ body mass index (BMI), which was classified as underweight (BMI<18.5 kg/m2), normal weight (BMI≥18.5–24.9 kg/m2), overweight (BMI≥25–29.9 kg/m2), obesity (BMI≥30–39.9 kg/m2), and severe obesity (BMI≥40 kg/m2).
Statistical analyses
Statistical analyses were performed using STATA 16. All analyses were performed as complete case analyses.
Cox proportional hazards regression models were used to investigate the association between loneliness and type 2 diabetes. The proportional hazards assumption was checked graphically using log-minus-log plots.
Respondents were excluded from the analyses if they (1) were diagnosed with type 2 diabetes prior to baseline (n=25 577), (2) had incomplete data on loneliness at baseline (n=19 067), or (3) were not registered in the Danish Civil Registration System (n=122). A total of 4 65 290 patients were eligible for analyses.
The age of the respondents was used as the underlying time scale, and respondents were followed until one of the following events occurred: (1) diagnosis of type 2 diabetes, (2) emigration, (3) death, or (4) end of study (31 December 2018), whichever came first.
Four main models were performed: (1) an age- and sex-adjusted model, (2) a sociodemographic-adjusted model (further adjusted for marital status, cohabitation, country of origin, and educational level), (3) a partially adjusted model (further adjusted for BMI), and (4) a fully adjusted model (further adjusted for smoking status, physical activity, weekly alcohol consumption, and dietary habits). To avoid overadjustment, the partially adjusted model (model 3) was considered the definitive model.
Several analyses were performed to investigate the potential effect modification of mental disorders on the association between loneliness and type 2 diabetes. First, the partially adjusted model (model 3) was stratified based on the presence or absence of at least one of the mental disorders included in the study. Additionally, four partially adjusted models were performed separately, each stratified based on the presence or absence of one of the four specific mental disorder groups: mental and behavioral disorders due to psychoactive substance use; schizophrenia and psychosis; affective disorders; and nervous disorders, respectively. The stratifications allowed for an investigation of the association between loneliness and type 2 diabetes within each specific mental disorder group. Subsequently, likelihood ratio tests were performed to determine if there were any significant differences in the association between loneliness and type 2 diabetes between individuals with and without a mental disorder.
Sensitivity analyses
We conducted a sensitivity analysis in a subsample (n=74 755) to examine whether the results of the partially adjusted model (model 3) remained the same when using T-ILS as a measure of loneliness.
Furthermore, we conducted a sensitivity analysis to address the issue of temporality by excluding respondents who developed type 2 diabetes within 1 year of the baseline assessment in the partially adjusted model (n=2265).
Lastly, calibration weights computed by Statistics Denmark were available in the Danish National Health Surveys from 2010, 2013, and 2017 (94.2% of the total study population). As a sensitivity analysis, we repeated the partially adjusted model in this subsample (n=4 21 563) applying calibration weighting to reduce non-response bias.23
Ethical considerations
This study was approved by the Danish Data Protection Agency (Region Zealand Journal No. REG-118–2019). According to Danish law, questionnaire-based and register-based studies do not need approval from ethical committees in Denmark.
Data and resource availability
The data that support the findings of this study are stored on a secured server at Statistics Denmark and are not available to other researchers.
Results
Study population characteristics
A total of 465 290 respondents were included in the study (table 1). In total, 76 393 (16%) of the respondents felt lonely once in a while, and 21 007 (5%) felt lonely often. Respondents who felt lonely once in a while or often were more likely to be female, younger (<30 years), have a lower educational level, and to report adverse health behaviors compared with respondents who did not feel lonely. The proportion of respondents who felt lonely once in a while or often was higher among respondents diagnosed with a mental disorder compared with respondents without a mental disorder.
Table 1.
Baseline characteristics of the study population stratified by levels of loneliness.
| Characteristic | No loneliness | Lonely once in a while | Lonely often | |||
| n | % | n | % | n | % | |
| Total | 367 890 | 79 | 76 393 | 16 | 21 007 | 5 |
| Age (years) | ||||||
| <18 | 9573 | 65 | 4045 | 28 | 1071 | 7 |
| 18–29 | 41 562 | 67 | 15 943 | 26 | 4333 | 7 |
| 30–39 | 48 394 | 79 | 10 038 | 16 | 2507 | 4 |
| 40–49 | 68 380 | 82 | 11 691 | 14 | 3183 | 4 |
| 50–59 | 72 268 | 82 | 11 995 | 14 | 3340 | 4 |
| 60–69 | 72 299 | 84 | 10 900 | 13 | 2684 | 3 |
| 70+ | 55 414 | 78 | 11 781 | 17 | 3889 | 5 |
| Sex | ||||||
| Male | 171 744 | 81 | 31 588 | 15 | 8729 | 4 |
| Female | 196 146 | 77 | 44 805 | 18 | 12 278 | 5 |
| Marital status | ||||||
| Married | 230 739 | 87 | 28 178 | 11 | 5279 | 2 |
| Never married | 88 079 | 69 | 30 762 | 24 | 8982 | 7 |
| Divorced | 30 711 | 70 | 9628 | 22 | 3444 | 8 |
| Widow | 18 361 | 62 | 7825 | 27 | 3302 | 11 |
| Cohabitation | ||||||
| Living with others | 290 133 | 85 | 42 646 | 13 | 8192 | 2 |
| Living alone | 77 757 | 63 | 33 747 | 27 | 12 815 | 10 |
| Country of origin | ||||||
| Danish | 349 031 | 80 | 69 381 | 16 | 18 315 | 4 |
| Western | 9540 | 72 | 2717 | 21 | 932 | 7 |
| Non-Western | 9319 | 61 | 4295 | 28 | 1760 | 11 |
| Educational level | ||||||
| Elementary school | 85 365 | 73 | 24 086 | 21 | 8159 | 7 |
| Upper secondary education | 25 285 | 73 | 7511 | 22 | 1901 | 6 |
| Vocational education | 131 262 | 82 | 23 417 | 15 | 5894 | 4 |
| Short-cycle higher education | 17 702 | 83 | 2895 | 14 | 648 | 3 |
| Medium-cycle higher education | 68 723 | 83 | 11 578 | 14 | 2405 | 3 |
| Long-cycle higher education | 33 163 | 85 | 4915 | 13 | 1024 | 3 |
| Unknown | 6390 | 68 | 1991 | 21 | 976 | 10 |
| Smoking status | ||||||
| Non-smokers | 173 136 | 80 | 35 270 | 16 | 8521 | 4 |
| Former smokers | 113 828 | 82 | 20 514 | 15 | 5316 | 4 |
| Occasional smokers | 14 105 | 75 | 3804 | 20 | 1001 | 5 |
| Daily smokers | 62 529 | 75 | 15 588 | 19 | 5673 | 7 |
| Unknown | 4292 | 72 | 1217 | 20 | 496 | 8 |
| Physical activity | ||||||
| Physically active | 98 052 | 81 | 18 943 | 16 | 4666 | 4 |
| Physically inactive | 252 185 | 79 | 52 378 | 16 | 14 477 | 5 |
| Unknown | 17 653 | 72 | 5072 | 21 | 1864 | 8 |
| Weekly alcohol consumption | ||||||
| No consumption | 68 069 | 73 | 18 866 | 20 | 6983 | 7 |
| Low/moderate consumption | 257 600 | 82 | 46 608 | 15 | 10 417 | 3 |
| High consumption | 30 540 | 77 | 7166 | 18 | 2235 | 6 |
| Unknown | 11 681 | 70 | 3753 | 22 | 1372 | 8 |
| Dietary habits (salad) | ||||||
| Every day/several time a day | 24 492 | 79 | 4960 | 16 | 1497 | 5 |
| Occasionally | 288 019 | 80 | 56 722 | 16 | 13 609 | 4 |
| Never/rarely | 53 193 | 73 | 14 139 | 19 | 5621 | 8 |
| Unknown | 2186 | 72 | 572 | 19 | 280 | 9 |
| Body mass index (kg/m2) | ||||||
| Underweight <18.5 | 7628 | 69 | 2483 | 23 | 879 | 8 |
| Normal weight ≥18.5–24.9 | 177 763 | 79 | 37 500 | 17 | 9335 | 4 |
| Overweight ≥25–29.9 | 127 475 | 81 | 23 517 | 15 | 6371 | 4 |
| Obese ≥30–39.9 | 45 439 | 77 | 10 100 | 17 | 3221 | 6 |
| Severe obesity ≥40 | 2967 | 67 | 951 | 22 | 481 | 11 |
| Unknown | 6618 | 72 | 1842 | 20 | 720 | 8 |
| At least one mental disorder | ||||||
| No | 331 610 | 81 | 62 901 | 15 | 14 826 | 4 |
| Yes | 36 280 | 65 | 13 492 | 24 | 6181 | 11 |
| Nervous disorders | ||||||
| No | 363 627 | 80 | 74 197 | 16 | 19 628 | 4 |
| Yes | 4263 | 54 | 2196 | 28 | 1379 | 18 |
| Affective disorders | ||||||
| No | 336 905 | 81 | 64 821 | 16 | 15 789 | 4 |
| Yes | 30 985 | 65 | 11 572 | 24 | 5218 | 11 |
| Schizophrenia and other psychosis | ||||||
| No | 367 206 | 79 | 75 868 | 16 | 20 567 | 4 |
| Yes | 684 | 42 | 525 | 32 | 440 | 27 |
| Mental and behavioral disorders due to psychoactive substance use | ||||||
| No | 362 685 | 79 | 74 384 | 16 | 19 873 | 4 |
| Yes | 5205 | 62 | 2009 | 24 | 1134 | 14 |
Loneliness and the risk of type 2 diabetes
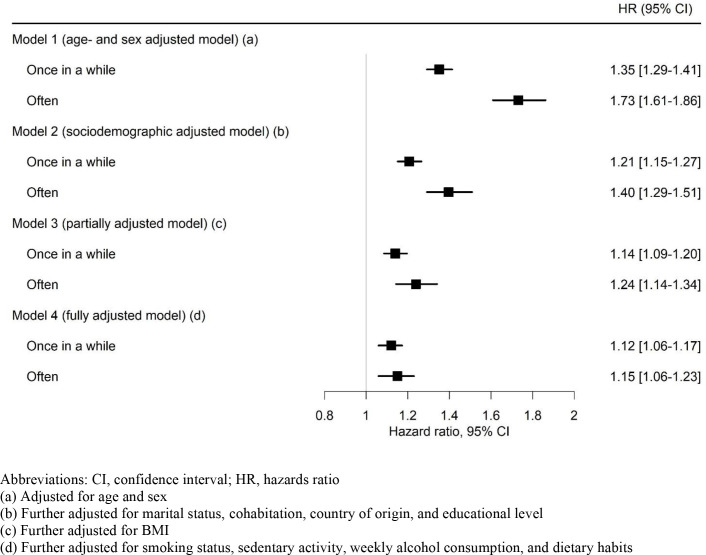
The mean follow-up time for the study was 6.3 years, during which a total of 13 771 individuals (3%) developed type 2 diabetes. Loneliness was significantly associated with an increased risk of type 2 diabetes. The strength of the association and the disparity in the risk of type 2 diabetes between individuals who felt lonely once in a while and those who felt lonely often gradually decreased as more covariates were adjusted for. Thus, in the definitive model (model 3), feeling lonely once in a while was associated with a 14% increased risk of type 2 diabetes (hazard ratio (HR) 1.14, 95% CI 1.09 to 1.20), and feeling lonely often was associated with a 24% increased risk (HR 1.24, 95% CI 1.14 to 1.34) (figure 1).
Figure 1.
Hazard ratios and 95% confidence intervals of incident type 2 diabetes by levels of loneliness.
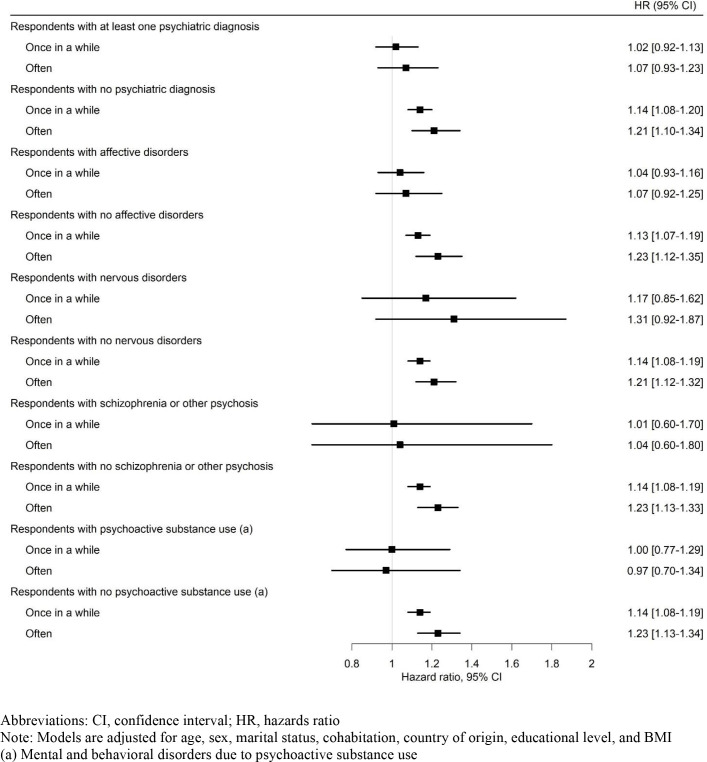
Modifying effect of mental disorders
The association between loneliness and type 2 diabetes was stronger among individuals without a mental disorder (HR 1.14, 95% CI 1.08 to 1.20 among those feeling lonely once in a while and HR 1.21, 95% CI 1.10 to 1.34 among those feeling lonely often) compared with those with at least one mental disorder (HR 1.02, 95% CI 0.92 to 1.13 and HR 1.07, 95% CI 0.93 to 1.23, respectively). A similar pattern was observed among individuals within each of the four specific mental disorder groups. However, these results are imprecise due to small numbers within each group (figure 2). The effects of mental disorders on the association between loneliness and type 2 diabetes were not statistically significant.
Figure 2.
Hazard ratios and 95% confidence intervals of incident type 2 diabetes by levels of loneliness stratified by the presence or absence of a mental disorder.
Sensitivity analyses
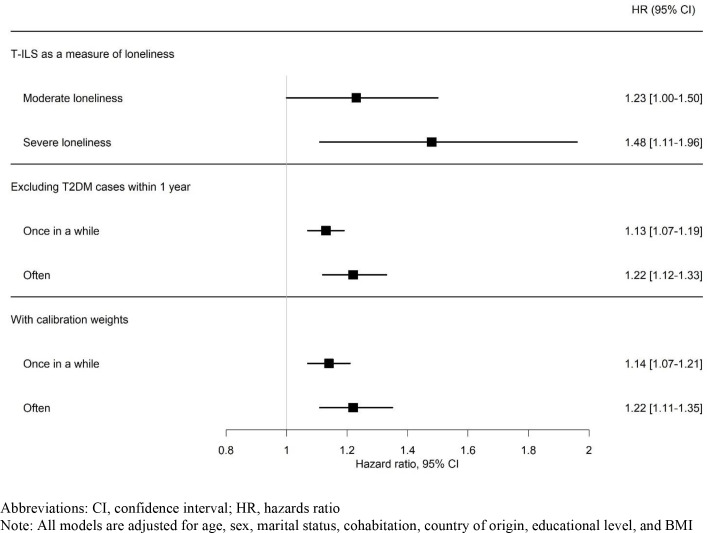
When using T-ILS as a measure of loneliness we found that moderate loneliness was associated with a 23% increased risk of type 2 diabetes (HR 1.23, 95% CI 1.00 to 1.50), whereas severe loneliness was associated with a 48% increased risk (HR 1.48, 95% CI 1.11 to 1.96) (figure 3).
Figure 3.
Hazard ratios and 95% confidence intervals of incident type 2 diabetes by levels of loneliness: sensitivity analyses. T2DM, type 2 diabetes mellitus; T-ILS, Three-Item Loneliness Scale.
The findings of the sensitivity analyses excluding individuals who developed type 2 diabetes within 1 year of survey baseline were similar to the main analyses (figure 3). Feeling lonely once in a while was associated with a 13% increased risk of type 2 diabetes (HR 1.13, 95% CI 1.07 to 1.19), and feeling lonely often was associated with a 22% increased risk (HR 1.22, 95% CI 1.12 to 1.33).
The sensitivity analyses with applied calibration weighting also yielded results similar to the main analyses (figure 3). Feeling lonely once in a while was associated with a 14% increased risk of type 2 diabetes (HR 1.14, 95% CI 1.07 to 1.21), while feeling lonely often was associated with a 22% increased risk of type 2 diabetes (HR 1.22, 95% CI 1.11 to 1.35).
Conclusions
The findings of the present study demonstrate that loneliness is associated with incident type 2 diabetes independently of a range of covariates. Specifically, feeling lonely once in a while was associated with a 14% increased risk of type 2 diabetes, while feeling lonely often was associated with a 24% increased risk of type 2 diabetes. The association was upheld, although stronger, when using T-ILS as a measure of loneliness. Furthermore, the association between loneliness and type 2 diabetes was stronger among individuals without a mental disorder compared with those with a mental disorder. However, the uncertainty of some of the estimates due to small numbers within each group and the lack of significant effects suggest that the effects of mental disorders on the association between loneliness and type 2 diabetes may not be substantial.
The main findings of this study are consistent with findings of previous cross-sectional8–10 and prospective studies,6 7 11 12 all demonstrating a higher risk of type 2 diabetes among individuals who feel lonely. A recent prospective study by Henriksen et al 11 found that those who felt most lonely had twice the risk of developing type 2 diabetes after adjusting for sex, age, and education compared with non-lonely respondents (odds ratio (OR) 2.19, 95% CI 1.16 to 4.15). Similarly, Christiansen et al 7 demonstrated a two-fold higher risk of type 2 diabetes among Danish individuals aged 35–79 years when adjusting for the same covariates (HR 1.98, 95% CI 1.47 to 2.67). A recent study by Song et al 12 also demonstrated an increased risk of type 2 diabetes in individuals aged 37–73 years living in the UK who reported feelings of loneliness (HR 1.21, 95% CI 1.13 to 1.30) independent of various covariates including socioeconomic factors, lifestyle and health behaviors, and medical history and genetics. Lastly, Hackett et al 6 demonstrated a significant association between loneliness and type 2 diabetes among individuals aged 50 years or older living in England independent of sociodemographic factors, health behaviors, and cardiometabolic comorbidities (HR 1.46, 95% CI 1.15 to 1.84).
Although these findings suggest a consistent association between loneliness and type 2 diabetes, the strength of the association varies among studies. The inconsistencies in findings across studies may be due to differences in study designs, populations, and measures of loneliness. For example, Henriksen et al 11 used a single-item direct measure, which may have underestimated the prevalence of loneliness due to the associated stigma, which can lead to feelings of shame or embarrassment and a tendency to conceal it from others.31 Conversely, Hackett et al 6 and Christensen et al 7 used the validated T-ILS reflecting different dimensions of loneliness. In our study, we used a single-item measure of feeling unwanted alone as a proxy of loneliness. However, this measurement solely considers the quantitative dimension of loneliness (lack of companionship) and not the qualitative (lack of qualitative characteristics, that is, intimacy, openness, and confidentiality). Additionally, feelings of loneliness can occur despite being with others. Furthermore, it can be argued that feeling unwanted alone reflects social isolation rather than loneliness, which refers to the absence of social contacts and relationships.32 Studies investigating both loneliness and social isolation in relation to the risk of type 2 diabetes consistently demonstrated a stronger association between loneliness and type 2 diabetes in comparison with social isolation and type 2 diabetes.6 7 12 Consequently, it is plausible that the measure of loneliness used in previous studies reflects more severe states of loneliness compared with feeling unwanted alone, which could explain the stronger associations found in those studies. This assumption is supported by the finding from our sensitivity analysis using T-ILS as a measure of loneliness, which demonstrated a stronger association between loneliness and type 2 diabetes compared with the measure of feeling unwanted alone. The present study and the study conducted by Song et al 12 and Hackett et al 6 demonstrated the weakest associations between loneliness and type 2 diabetes. Notably, these studies differed from the others by considering a broader range of covariates such as marital status, cohabitation, BMI, and various lifestyle and health behaviors. The inclusion of additional covariates may have contributed to the observed weaker association found in the present study. Finally, the inconsistencies in findings across studies may be attributed to differences in the populations included in the respective studies. The inclusion of all Danish adults aged 16 years and above in the present study likely weakens the association given the low incidence of type 2 diabetes in the youngest age group in comparison with other studies focusing on older populations.
The exact mechanisms by which loneliness increases the risk of type 2 diabetes are not fully understood, but several plausible pathways have been described in the literature, which include both biological and behavioral mechanisms. Loneliness has been associated with elevated levels of stress hormones, particularly cortisol.13 Elevated levels of cortisol are related to an increase in blood glucose levels and insulin resistance and may thus consequently result in type 2 diabetes.33 Furthermore, individuals who feel lonely may be more likely to engage in adverse health behaviors such as unhealthy dietary habits, physical inactivity, and smoking,8 all of which are well-known risk factors for type 2 diabetes.34 Additionally, unhealthy dietary habits and physical inactivity may result in overweight and obesity, which are also major risk factors for type 2 diabetes.34 While the details of these mechanisms are beyond the scope of this article, this pathway is to some extent supported by the findings of this study as the strength of the association between loneliness and type 2 diabetes decreases when adjusting for BMI and various health behaviors.
To the best of our knowledge, no previous studies have explored the potential modifying role of mental disorders in the association between loneliness and type 2 diabetes. In this study, the association between loneliness and type 2 diabetes was stronger among individuals without a mental disorder compared with those with a mental disorder. This finding may be explained by the fact that the presence of a mental disorder may obscure the effect of loneliness, as individuals with mental disorders already face an increased risk of type 2 diabetes.35 Loneliness and mental disorders may share common pathways through which they contribute to an increased risk of type 2 diabetes. For example, both loneliness and mental disorders have been associated with elevated levels of stress hormones36 37 and adverse health behaviors,8 38 which increase the risk of type 2 diabetes. Thus, the presence of a mental disorder among individuals experiencing loneliness may not necessarily be additive but may rather reflect shared pathways that lead to an increased risk of type 2 diabetes.
Strengths and limitations
The major strengths of this study are the prospective study design and the use of a comprehensive algorithm to identify individuals with type 2 diabetes by combining several health registers that include information on patients treated both within the hospital sector and general practice.25 Due to the universal and government-funded nature of the Danish healthcare system, all residents are ensured free access to healthcare services both within the hospital sector and via general practitioners.39 Thus, the use of register-based data provides a comprehensive measure of type 2 diabetes that does not depend on membership of an insurance scheme. In addition, the inclusion of patients treated within general practice is of great importance considering that approximately 80% of all type 2 diabetes patients are treated within general practice.25 Furthermore, the use of a large national survey sample, which secures a high level of generalizability and allows for the adjustment of multiple covariates, must be considered a strength of the study.
The use of register-based data also has limitations. In this study, information on mental disorders was based on both hospital contacts and medical prescriptions, but certain medications, such as antidepressants, are not only prescribed for the treatment of depression. Thus, the possibility of misclassification of affective diagnoses cannot be ruled out. Limitations related to the measure of loneliness should also be mentioned. In this study, feeling unwanted alone was used as a proxy of loneliness and was measured using a single item. However, previous studies have demonstrated that using a single item correlate significantly with the validated and commonly used UCLA Loneliness Scale40 and with the De Jong Grieveld Loneliness Scale.41 In addition, information on loneliness is self-reported and may thus be underestimated due to the negative social stigma associated with loneliness.42 This could potentially lead to an underestimation of the effect of loneliness on type 2 diabetes. Nevertheless, the measure of loneliness used in this study is indirect, meaning that the item does not include the terms “lonely” or “loneliness”, which might avoid some of the stigma associated with loneliness.42 Thus, we have no reason to believe that the measure of loneliness used in this study invalidates our results.
Furthermore, non-response is a persistent problem in most survey research. However, the sensitivity analyses with applied calibrated weights showed results similar to the main analyses, indicating that the findings of this study are robust against non-response bias. In addition, sensitivity analyses excluding respondents diagnosed with type 2 diabetes during the first year from survey response were performed to address the risk of reverse causation. The association between loneliness and type 2 diabetes remained significant, suggesting that loneliness is a predictor of type 2 diabetes.
The findings of this study demonstrate that loneliness increases the risk of type 2 diabetes independent of a range of covariates including sociodemographic factors and health behaviors. Thus, the study findings emphasize the importance of addressing loneliness as a potential modifiable risk factor in the prevention and management of type 2 diabetes. The association between loneliness and type 2 diabetes was stronger among individuals without a mental disorder compared with those with a mental disorder. Further research is warranted to understand the mechanisms underlying this association.
bmjdrc-2023-003934supp001.pdf (61.6KB, pdf)
Acknowledgments
The Danish National Health Surveys were conducted and funded by the Capital Region, Region Zealand, the Region of Southern Denmark, the Central Denmark Region, the North Denmark Region, the Ministry of Health, and the National Institute of Public Health, University of Southern Denmark.
Footnotes
Contributors: SR, LCT, SHH, ABT, and TAH designed the study. Data management and analyses were conducted by SR and LCT. All authors contributed to the interpretation of the results. SR drafted the initial version of the manuscript, and all authors reviewed, edited and approved the final version. LCT and SR are the guarantors of this work and, as such, had full access to all the study data and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding: This study was funded by Steno Diabetes Center Sjaelland. The study funder was not involved in the design of the study; the collection, analysis, and interpretation of data; writing the report; and did not impose any restrictions regarding the publication of the report.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Park C, Majeed A, Gill H, et al. The effect of loneliness on distinct health outcomes: a comprehensive review and meta-analysis. Psychiatry Res 2020;294:113514. 10.1016/j.psychres.2020.113514 [DOI] [PubMed] [Google Scholar]
- 2. Beutel ME, Klein EM, Brähler E, et al. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry 2017;17:97. 10.1186/s12888-017-1262-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Valtorta NK, Kanaan M, Gilbody S, et al. Loneliness, social isolation and risk of cardiovascular disease in the English Longitudinal Study of Ageing. Eur J Prev Cardiol 2018;25:1387–96. 10.1177/2047487318792696 [DOI] [PubMed] [Google Scholar]
- 4. Holt-Lunstad J, Smith TB, Baker M, et al. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci 2015;10:227–37. 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- 5. Rico-Uribe LA, Caballero FF, Martín-María N, et al. Association of loneliness with all-cause mortality: a meta-analysis. PLoS One 2018;13:e0190033. 10.1371/journal.pone.0190033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hackett RA, Hudson JL, Chilcot J. Loneliness and type 2 diabetes incidence: findings from the English Longitudinal Study of Ageing. Diabetologia 2020;63:2329–38. 10.1007/s00125-020-05258-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Christiansen J, Lund R, Qualter P, et al. Loneliness, social isolation, and chronic disease outcomes. Eur J Public Health 2020;30(Supplement_5). 10.1093/eurpub/ckaa166.1045 [DOI] [PubMed] [Google Scholar]
- 8. Richard A, Rohrmann S, Vandeleur CL, et al. Loneliness is adversely associated with physical and mental health and lifestyle factors: results from a Swiss National survey. PLoS One 2017;12:e0181442. 10.1371/journal.pone.0181442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Christiansen J, Larsen FB, Lasgaard M. Do stress, health behavior, and sleep mediate the association between loneliness and adverse health conditions among older people. Soc Sci Med 2016;152:80–6. 10.1016/j.socscimed.2016.01.020 [DOI] [PubMed] [Google Scholar]
- 10. Foti SA, Khambaty T, Birnbaum-Weitzman O, et al. Cardiovascular disease, and diabetes prevalence in the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. J Immigr Minor Health 2020;22:345–52. 10.1007/s10903-019-00885-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Henriksen RE, Nilsen RM, Strandberg RB. Loneliness increases the risk of type 2 diabetes: a 20 year follow-up - results from the HUNT study. Diabetologia 2023;66:82–92. 10.1007/s00125-022-05791-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Song Y, Zhu C, Shi B, et al. Social isolation, loneliness, and incident type 2 diabetes mellitus: results from two large prospective cohorts in Europe and East Asia and Mendelian randomization. EClinicalMedicine 2023;64:102236. 10.1016/j.eclinm.2023.102236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med 2010;40:218–27. 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Whisman MA. Loneliness and the metabolic syndrome in a population-based sample of middle-aged and older adults. Health Psychol 2010;29:550–4. 10.1037/a0020760 [DOI] [PubMed] [Google Scholar]
- 15. Marott SCW, Nordestgaard BG, Tybjærg-Hansen A, et al. Components of the metabolic syndrome and risk of type 2 diabetes. J Clin Endocrinol Metab 2016;101:3212–21. 10.1210/jc.2015-3777 [DOI] [PubMed] [Google Scholar]
- 16. Shankar A, McMunn A, Banks J, et al. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol 2011;30:377–85. 10.1037/a0022826 [DOI] [PubMed] [Google Scholar]
- 17. Schrempft S, Jackowska M, Hamer M, et al. Associations between social isolation, loneliness, and objective physical activity in older men and women. BMC Public Health 2019;19:74. 10.1186/s12889-019-6424-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cuesta-Lozano D, Simón-López LC, Mirón-González R, et al. Prevalence rates of loneliness and its impact on lifestyle in the healthy population of Madrid, Spain. Int J Environ Res Public Health 2020;17:5121. 10.3390/ijerph17145121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vanhalst J, Klimstra TA, Luyckx K, et al. The interplay of loneliness and depressive symptoms across adolescence: exploring the role of personality traits. J Youth Adolesc 2012;41:776–87. 10.1007/s10964-011-9726-7 [DOI] [PubMed] [Google Scholar]
- 20. Houtjes W, van Meijel B, van de Ven PM, et al. The impact of an unfavorable depression course on network size and loneliness in older people: a longitudinal study in the community. Int J Geriatr Psychiatry 2014;29:1010–7. 10.1002/gps.4091 [DOI] [PubMed] [Google Scholar]
- 21. Jørgensen ME, Kristensen JK, Reventlov Husted G, et al. The Danish Adult Diabetes Registry. Clin Epidemiol 2016;8:429–34. 10.2147/CLEP.S99518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jensen HAR, Ekholm O, Davidsen M, et al. The Danish Health and Morbidity Surveys: study design and participant characteristics. BMC Med Res Methodol 2019;19:91. 10.1186/s12874-019-0733-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Christensen AI, Lau CJ, Kristensen PL, et al. The Danish National Health Survey: study design, response rate and respondent characteristics in 2010, 2013 and 2017. Scand J Public Health 2022;50:180–8. 10.1177/1403494820966534 [DOI] [PubMed] [Google Scholar]
- 24. Hughes ME, Waite LJ, Hawkley LC, et al. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging 2004;26:655–72. 10.1177/0164027504268574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Carstensen B, Rønn PF, Jørgensen ME. Revalence, incidence and mortality of type 1 and type 2 diabetes in Denmark 1996–2016. BMJ Open Diabetes Res Care 2020;8:e001071. 10.1136/bmjdrc-2019-001071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health 2011;39(7 Suppl):30–3. 10.1177/1403494811401482 [DOI] [PubMed] [Google Scholar]
- 27. Kildemoes HW, Sørensen HT, Hallas J. The Danish National Prescription Registry. Scand J Public Health 2011;39(7 Suppl):38–41. 10.1177/1403494810394717 [DOI] [PubMed] [Google Scholar]
- 28. Andersen JS, Olivarius NDF, Krasnik A. The Danish National Health Service Register. Scand J Public Health 2011;39(7 Suppl):34–7. 10.1177/1403494810394718 [DOI] [PubMed] [Google Scholar]
- 29. Andersen N, Hjortdal JØ, Schielke KC, et al. The Danish Registry of Diabetic Retinopathy. Clin Epidemiol 2016;8:613–9. 10.2147/CLEP.S99507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jensen VM, Rasmussen AW. Danish education registers. Scand J Public Health 2011;39(7 Suppl):91–4. 10.1177/1403494810394715 [DOI] [PubMed] [Google Scholar]
- 31. Barreto M, van Breen J, Victor C, et al. Exploring the nature and variation of the stigma associated with loneliness. J Soc Pers Relat 2022;39:2658–79. 10.1177/02654075221087190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. de Jong Gierveld J, Havens B. Cross-national comparisons of social isolation and loneliness: introduction and overview. Can J Aging 2004;23:109–13. 10.1353/cja.2004.0021 [DOI] [PubMed] [Google Scholar]
- 33. Hackett RA, Kivimäki M, Kumari M, et al. Diurnal cortisol patterns, future diabetes, and impaired glucose metabolism in the Whitehall II cohort study. J Clin Endocrinol Metab 2016;101:619–25. 10.1210/jc.2015-2853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bellou V, Belbasis L, Tzoulaki I, et al. Risk factors for type 2 diabetes mellitus: an exposure-wide umbrella review of meta-analyses. PLoS One 2018;13:e0194127. 10.1371/journal.pone.0194127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lindekilde N, Scheuer SH, Diaz LJ, et al. Risk of developing type 2 diabetes in individuals with a psychiatric disorder: a nationwide register-based cohort study. Diabetes Care 2022;45:724–33. 10.2337/dc21-1864 [DOI] [PubMed] [Google Scholar]
- 36. Smith KJ, Gavey S, RIddell NE, et al. The association between loneliness, social isolation and inflammation: a systematic review and meta-analysis. Neurosci Biobehav Rev 2020;112:519–41. 10.1016/j.neubiorev.2020.02.002 [DOI] [PubMed] [Google Scholar]
- 37. Dziurkowska E, Wesolowski M. Cortisol as a biomarker of mental disorder severity. J Clin Med 2021;10:5204. 10.3390/jcm10215204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Scott D, Happell B. The high prevalence of poor physical health and unhealthy lifestyle behaviours in individuals with severe mental illness. Issues Ment Health Nurs 2011;32:589–97. 10.3109/01612840.2011.569846 [DOI] [PubMed] [Google Scholar]
- 39. Schmidt M, Schmidt SAJ, Adelborg K, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol 2019;11:563–91. 10.2147/CLEP.S179083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Xu S, Qiu D, Hahne J, et al. Psychometric properties of the short-form UCLA Loneliness Scale (ULS-8) among Chinese adolescents. Medicine (Baltimore) 2018;97:e12373. 10.1097/MD.0000000000012373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Nicolaisen M, Thorsen K. Who are lonely? Loneliness in different age groups (18-81 years old), using two measures of loneliness. Int J Aging Hum Dev 2014;78:229–57. 10.2190/AG.78.3.b [DOI] [PubMed] [Google Scholar]
- 42. Jenny de Jong Gierveld T, Dykstra PA. Loneliness and social isolation. In: The Cambridge Handbook of Personal Relationships. Cambridge: Cambridge University Press, 2006: 99. 10.1017/CBO9780511606632 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjdrc-2023-003934supp001.pdf (61.6KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available.