Abstract
Aims.
This study estimated the likelihoods of individuals transitioning to different cannabis use status following recreational cannabis legalization (RCL) in the US.
Design.
Secondary analysis of a nationally representative longitudinal cohort in the US. We used propensity score matching to balance individual characteristics between RCL and comparison states and generalized mixed regressions to estimate behavioral transitions in matched samples.
Participants.
A longitudinal cohort of 21,863 individuals (6,925 youths and 14,938 adults) participating in the Population Assessment of Tobacco and Health Waves 3 and 4.
Setting.
Four RCL states that implemented RCL between Waves 3 and 4 (California, Massachusetts, Nevada, and Maine) and comparison states in the US.
Measurements.
Transitions in cannabis use over the two waves: 1) from nonusers to users; 2) from nonusers to weekly users; 3) from users to nonusers. Individuals in RCL states were compared to matched individuals in 1) states with medical cannabis legalization (MCL), 2) states not legalizing cannabis (non-legalizing), and 3) MCL and non-legalizing states combined.
Findings.
Among youths, the association between RCL and greater odds of transition from nonusers to users was seen in comparison to non-legalizing states (OR, 95%CI: 2.18, 1.37–3.45) and combined states (1.73, 1.23–2.42). Evidence was lacking regarding the associations between RCL and transitions from nonusers to weekly users and from users to nonusers. Among adults, RCL was associated with greater odds of transitions from nonusers to users and nonusers to weekly users if RCL states were compared to non-legalizing states (1.68, 1.15–2.46; 1.82, 1.00–3.31 respectively) or combined states (1.51, 1.11–2.07; 2.09, 1.19–3.66 respectively). RCL was also associated with lower odds of transition from users to nonusers if RCL states were compared to non-legalizing states (0.54, 0.35–0.81).
Conclusions.
There was some evidence suggesting that RCL was associated with elevated odds of transition to cannabis users among both youths and adults.
Keywords: Recreational cannabis legalization, cannabis use transition, youth, adult, propensity score matching
INTRODUCTION
The prevalence of past-month cannabis use among individuals aged 12 or older in the US has increased from 7% in 2010 to 11% in 2019. (1) Meanwhile, there has been a momentum to expand legal access to cannabis. Since 2012, 18 states and the District of Columbia have removed penalties for adults’ possession of cannabis in a small amount for recreational use (recreational cannabis legalization or RCL). (2)
RCL may have impacts on adults’ use by reducing pecuniary and non-pecuniary costs of possession and consumption and forming more favorable social norms. While cannbis possession among youths under age 21 years is still prohibited, RCL may also shape favorable perceptions and attitudes among them. The opening of recreational cannabis markets in RCL states could further increase accessibility and availability of cannabis, provide products with greater variety and potency, and promote awareness and interest among both adults and youths. Because cannabis use for recreational purposes may have detrimental health effects particularly on youths, (3, 4) the potential increase in cannabis use following RCL has been a public health concern.
Most of the empirical research on the association between RCL and cannabis use in the US relied upon repeated cross-sectional data on youth population and yielded inconclusive findings. Compared to other states without RCL, Cerdá et al. (5) found that RCL was associated with an increase in cannabis use among 8th and 10th graders in the Monitoring the Future study in Washington but not in Colorado. Because Monitoring the Future study was not designed to provide state-representative estimates, it may limit the reliability and generalizability of the findings. (6) Dilley et al. (6) replicated the analysis in Washington using the state representative Washington Healthy Youth Survey and found a significant decline in cannabis use among 8th and 10th graders. Anderson et al. (7) suggested a decline in cannabis use among youths following RCL compared to states without any type of cannabis legalization. Bae and Kerr (8) reported that cannabis use among college students increased more in states with RCL than states without RCL. Kerr et al. (9) estimated that cannabis use increased only among heavy users of alcohol in a large public university following RCL in Oregon compared to six universities in other states without RCL.
Only two studies provided evidence on adult population using repeated cross-sectional data. Shi et al. (10) suggested that RCL alone was not associated with cannabis exposures but opening cannabis retail markets was associated with a substantial increase in cannabis exposures among adults if RCL states were compared to states with medical cannabis legalization or states without any type of cannabis legalization. Such increase was even higher among youths than adults. Cerda et al. (11), however, reported that RCL was associated with increases in cannabis use disorder among both youths and adults in states adopting RCL compared to states that did not adopt RCL.
A common limitation in these repeated cross-sectional studies is ecological fallacy: cross-sectional studies relied upon over-time changes in cannabis us prevalence at aggregate level (usually state level). Even though individual characteristics were controlled for in some studies, they were not able to examine behavioral changes for the same individual or identify heterogeneities in response to policies at individual level. (12, 13) Only a few studies in the US thus far estimated individual-level changes in longitudinal cohorts, all of which were restricted by sample size and sample representativeness. Comparing a cohort of 281 youths to those of the same age range prior to legalization in Washington, Bailey et al. (14) found evidence of a higher likelihood of cannabis use after RCL. Barker et al. (15) reported a higher likelihood of cannabis use only among prior cannabis users in a cohort of 338 students in a large public university in Washington compared to a similar university in Wisconsin. Comparing those who transitioned from 8th to 9th grade during RCL in Oregon to those who made the transition prior to RCL in a cohort of 444 youths, Rusby et al. (16) found an increase in cannabis use frequency among existing cannabis users. In a non-probability-based cohort of 668 parents, Epstein et al. (17) found an increase in cannabis use frequency and pro-cannabis norms in both RCL and non-RCL states, but the increase in pro-cannabis norms was faster in RCL states.
The research question of this study was to examine the relationships between RCL and the likelihoods of individuals transitioning to different cannabis use status in the US. We contributed to the still limited literature in the following ways. First, our study used data from the Population Assessment of Tobacco and Health in the US, making it the first study to estimate individual-level changes among a nationally representative longitudinal cohort. Second, PATH has a much larger sample size than previous cohort studies to power the detection of smaller effects. Third, we examined both youths and adults.
METHODS
Data and Sample
The Population Assessment of Tobacco and Health (PATH) is a probability-based, nationally representative longitudinal cohort study of non-institutionalized civilians aged 12 years and older in the US. Although PATH primarily collects information on tobacco use and related health outcomes, it started to ask cannabis use questions from Wave 2. More information about PATH is published elsewhere. (18)
Our data were obtained from Waves 3 and 4 (Figure S1). Data in the previous two waves were not used because 1) cannabis use questions were not asked in Wave 1, 2) data collection periods in Waves 1 and 2 had overlaps, 3) out of the three states implementing RCL during Wave 2, only Oregon had sufficient sample size to make statistically meaningful estimations. Four states, including California, Massachusetts, Nevada, and Maine, implemented RCL right before or at the beginning of Wave 4 data collection (Figure S1), creating a relatively clean comparison before and after RCL using Waves 3 and 4 data.
Of the 35,984 respondents who completed both PATH Waves 3 and 4 interviews, we restricted the sample to 24,061 respondents in the selected RCL and comparison states. We further excluded 2,198 respondents who had incomplete data on outcomes of interest or covariates. The final analytical sample had 21,863 respondents, including 6,925 youths who were younger than 21 years at Wave 4 (the legal age limit) and 14,938 adults who were 21 years or older at Wave 4. Tables S1-S2 compare Wave 3 characteristics between Wave 3 respondents who stayed and dropped out in Wave 4. Table S3 reports missing rates of Wave 3 characteristics among respondents who completed both Waves 3 and 4. Tables S4-S5 compare Wave 3 characteristics between respondents completing both Waves 3 and 4 with and without missing values. Table S6 reports sample sizes by state legalization status and cannabis use status.
Cannabis Use Outcomes
Cannabis use was determined by the question “have you ever used cannabis, hash, THC, grass, pot or weed in the past 30 days?” in PATH Waves 3 and 4. Among cannabis users, those who reported using cannabis weekly were classified as weekly users. Based on participants’ responses in both Waves, three binary indicators were generated to define transitions in cannabis use status, including 1) transition from nonusers at Wave 3 to users at Wave 4, 2) transition from nonusers at Wave 3 to weekly users at Wave 4, and 3) transition from users at Wave 3 to nonusers at Wave 4.
Policy Exposure
The policy exposure of interest was the implementation of RCL. Four states implemented RCL right before or at the very beginning of Wave 4 (Figure S1). They were considered treatment states in this study.
Covariates for Matching and Regressions
We included the following individual-level covariates in both matching and regressions in youth and adult samples: age, sex, race/ethnicity, urbanicity, household income, past-month cigarette use, and past-month binge drinking (having five or more drinks in a row at least once in the past month). Matching and regressions in adult sample also included marital status, educational attainment, and current employment status. All of these covariates were obtained from Wave 3 except for urbanicity which was only available in Wave 1. We also included the following state-level covariates as controls in regressions after matching: poverty rate, percentage of non-Hispanic whites, and unemployment rate. These state-level covariates were 2017 data from the US Census Bureau or Bureau of Labor Statistics.
Statistical Analysis
The three transitions from Wave 3 to Wave 4 were evaluated separately: 1) from nonusers to users (Analysis 1), 2) from nonusers to weekly users (Analysis 2), and 3) from users to nonusers (Analysis 3). Analyses 1–2 were restricted to Wave 3 nonusers and Analysis 3 was restricted to Wave 3 users. Youth and adult samples were analyzed separately in these three analyses.
Treatment states were compared to comparison states in each analysis and sample. The treatment states included four RCL states (California, Massachusetts, Nevada, and Maine). Five jurisdictions implemented RCL before Wave 3 and five states implemented medical cannabis legalization (MCL) between Wave 3 and Wave 4, so they were excluded from this study. Following previous research, (10, 19) three groups of comparison states were constructed to account for the heterogeneity of cannabis legality in the 28 states without RCL.1 The list of states is reported in Table S7. Comparison A compared RCL states to 11 states that implemented MCL before Wave 3 but had not implemented RCL when Wave 4 data collection ended. Because all the RCL states already implemented MCL before RCL, this comparison estimated the independent association between RCL and behavioral outcomes beyond the effects of MCL. Comparison B compared RCL states to 17 states that had not implemented recreational or medical cannabis legalization (non-legalizing) when Wave 4 data collection ended. This comparison estimated the association between RCL and behavioral outcomes relative to the absence of any type of cannabis legalization. Comparison C compared RCL states to 28 states (11 states in Comparison A + 17 states in Comparison B) that had not implemented RCL when Wave 4 data collection ended. This comparison estimated the association between RCL and behavioral outcomes regardless of legalization status in comparison states.
Statistically, four models were used to estimate the associations. Model 1 used multivariate logistic regressions to estimate the odds of cannabis use transitions in RCL states compared to comparison states in unmatched full samples without controlling for covariates. Model 2 extended Model 1 by including individual- and state-level covariates in multivariate logistic regressions. Models 1 and 2 had limitations as confounders may not adequately overlap between the samples in treatment and comparison states. (20) Accordingly, the validity of comparisons can be compromised. (21)
To address this concern, we adopted Propensity Score Matching (PSM) to improve the balance in covariates between the samples in RCL and comparison states. As a technique widely used in observational studies to alleviate the effects of confounding, (22, 23) PSM enables a study to mimic a randomized controlled trial by reducing any observed differences that exist between the two groups. (24) Based on PSM guidelines, (21) we first fitted logistic regressions with individual-level covariates that yielded a propensity score for each respondent. (25) We then matched individuals in RCL states to individuals in comparison states using the nearest-neighbor 1:1 matching without replacement. The nearest-neighbor matching algorithm is the most common implementation of PSM helping minimize the bias in subsequent estimations. (26) We computed standardized differences in individual-level covariates between the matched samples in RCL states and comparison states before and after PSM (Technical Note S1) and conducted χ2 tests to assess the improvement of balance. (25) A standardized difference of no more than 10% is suggested an indicator of balance. (27)
Following PSM, generalized linear mixed regressions (Binomial family) were employed to estimate the associations, accounting for the pairing between matched samples. Model 3 estimated the odds of cannabis use transitions in RCL states relative to comparison states in matched samples without controlling for covariates. Model 4 extended Model 3 in matched samples by including individual- and state-level covariates in multivariate logistic regressions.
We tested the robustness of results to PSM matching algorithms. In addition to nearest-neighbor 1:1 matching without replacement in the main analysis, we repeated Models 3 and 4 with five alternative matching algorithms, including nearest-neighbor 1:1 matching with replacement, nearest-neighbor 1:2 matching with replacement, and nearest-neighbor matching without replacement adding caliper 0.0005, 0.001 and 0.002 respectively.
Statistical analyses were conducted with STATA 16.1 (StataCorp LP, College Station, TX, USA). The study was not pre-registered and the results should be considered exploratory. The use of restricted PATH data was approved by the University of California San Diego Human Research Protection Program.
RESULTS
Propensity Score Matching
Tables S8–S9 report descriptive statistics of individual-level covariates in RCL and comparison states in youth and adult samples, respectively.
Figures 1–2 show the standardized differences in individual-level covariates between RCL and comparison states before and after PSM in youth and adult samples, respectively (detailed statistics in Table S10 for youths and Table S11 for adults). In general, PSM reduced much of the differences in covariates in matched samples. Most of the standardized differences were less than 10% after matching.
Figure 1. Standardized Differences between RCL States and Comparison States Before and After Propensity Score Matching, PATH Youth Sample.
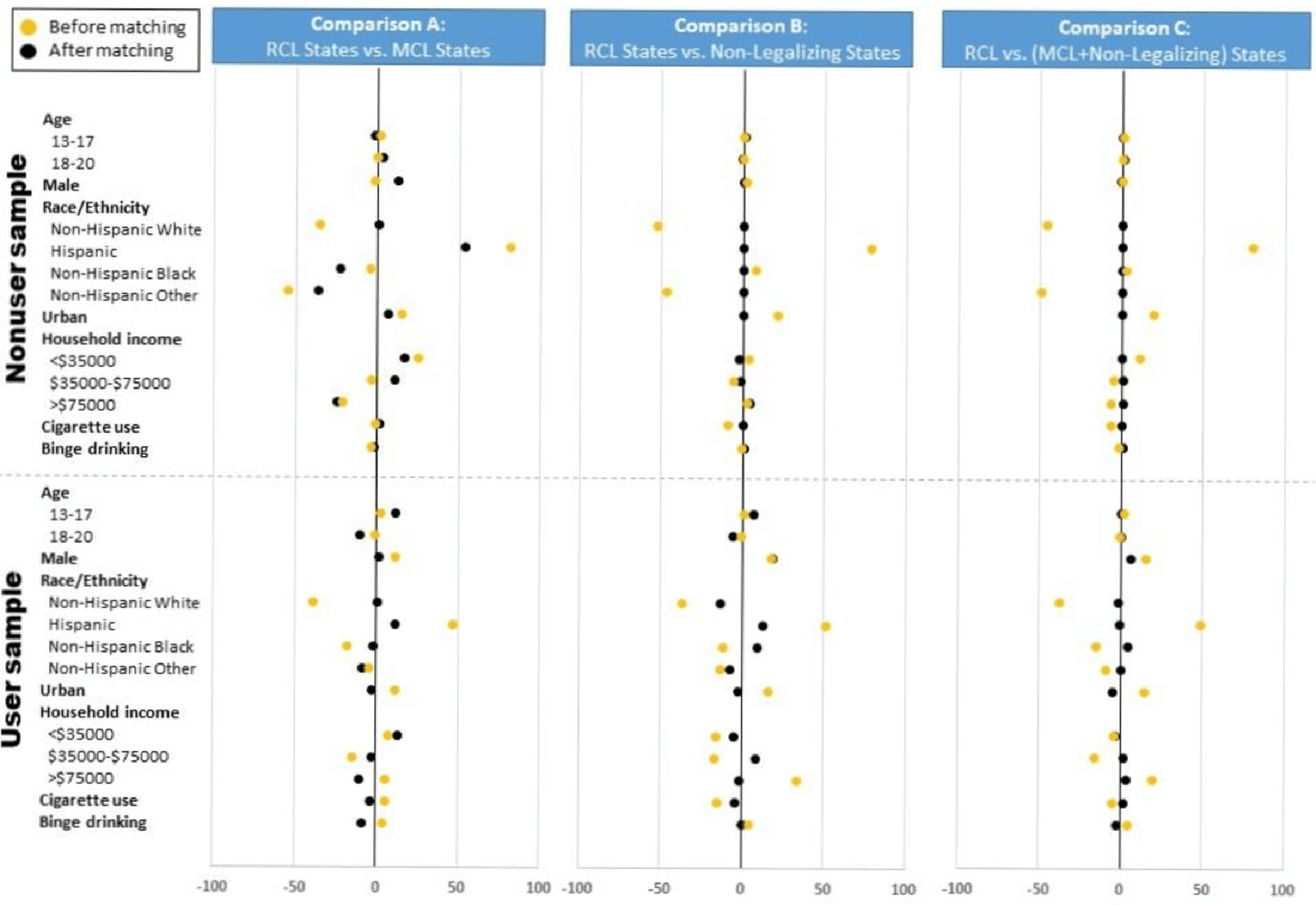
Notes:
1) The yellow dots represent standardized differences in percentage points before matching, and the black dots represent standardized differences in percentage points after matching.
2) The exact numbers in this Figure are reported in Table S10.
Figure 2. Standardized Differences between RCL States and Comparison States Before and After Propensity Score Matching, PATH Adult Sample.
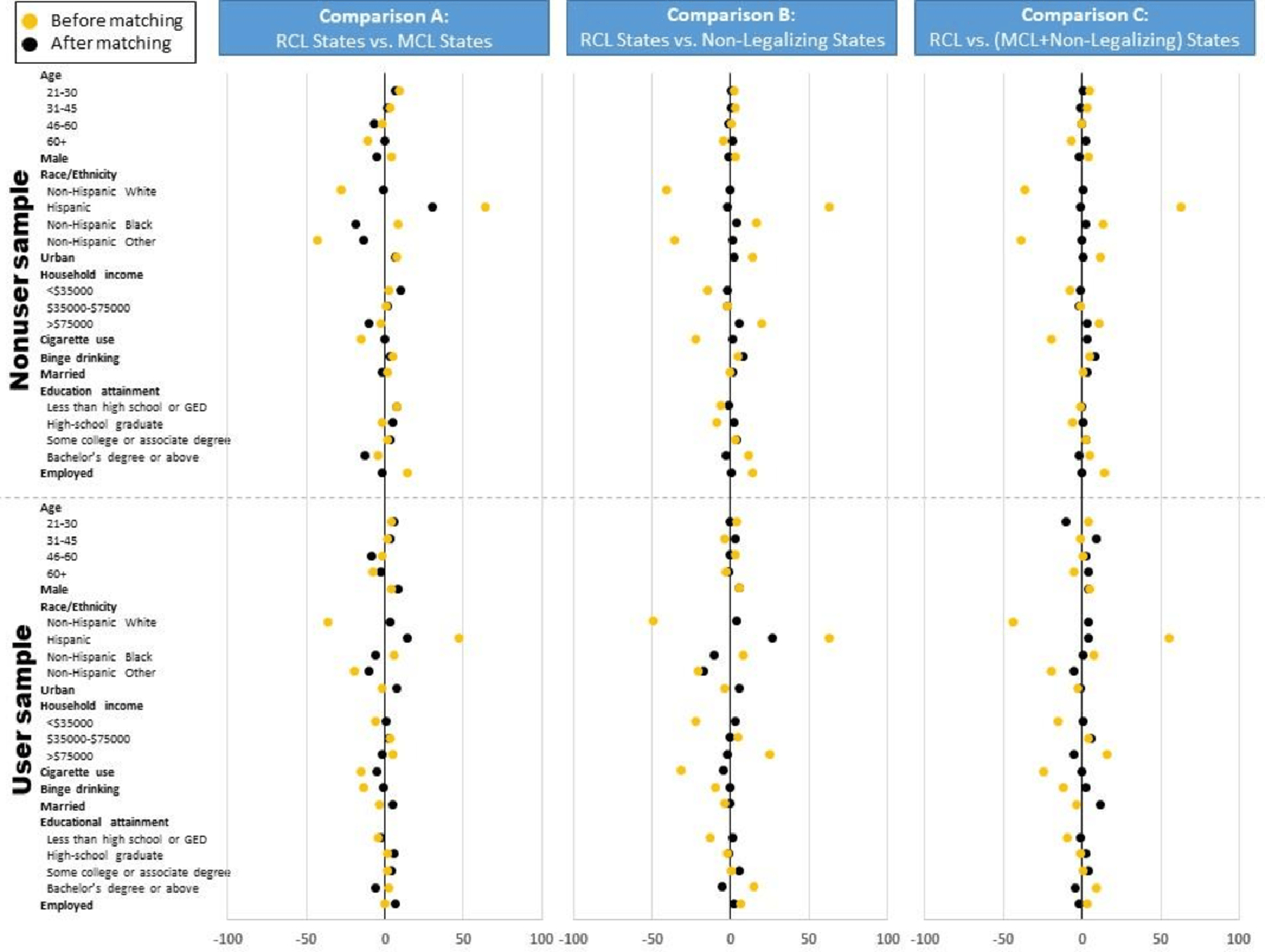
Notes:
1) The yellow dots represent standardized differences in percentage points before matching, and the black dots represent standardized differences in percentage points after matching.
2) The exact numbers in this Figure are reported in Table S11.
Association Estimation in Matched Samples
Figure 3 reports Models 3 and 4 results in matched youth sample after PSM (detailed results in Table S12). In Model 4 regressions controlling for covariates, RCL was associated with a higher odds of transition from nonusers to users when RCL states were compared to non-legalizing states (OR, 95%CI: 2.18, 1.37–3.45, p<0.001) and MCL and non-legalizing states combined (1.73, 1.23–2.42, p=0.001). We did not find evidence that RCL was associated with transition from nonusers to users when RCL states were compared to MCL states alone. We also did not find evidence that RCL was associated with transition from nonusers to weekly users or from users to nonusers in any comparisons. Model 3 without controlling for covariates yielded results similar to Model 4.
Figure 3. The Association between Recreational Cannabis Legalization and Cannabis Use Transitions, PATH Youth Sample.
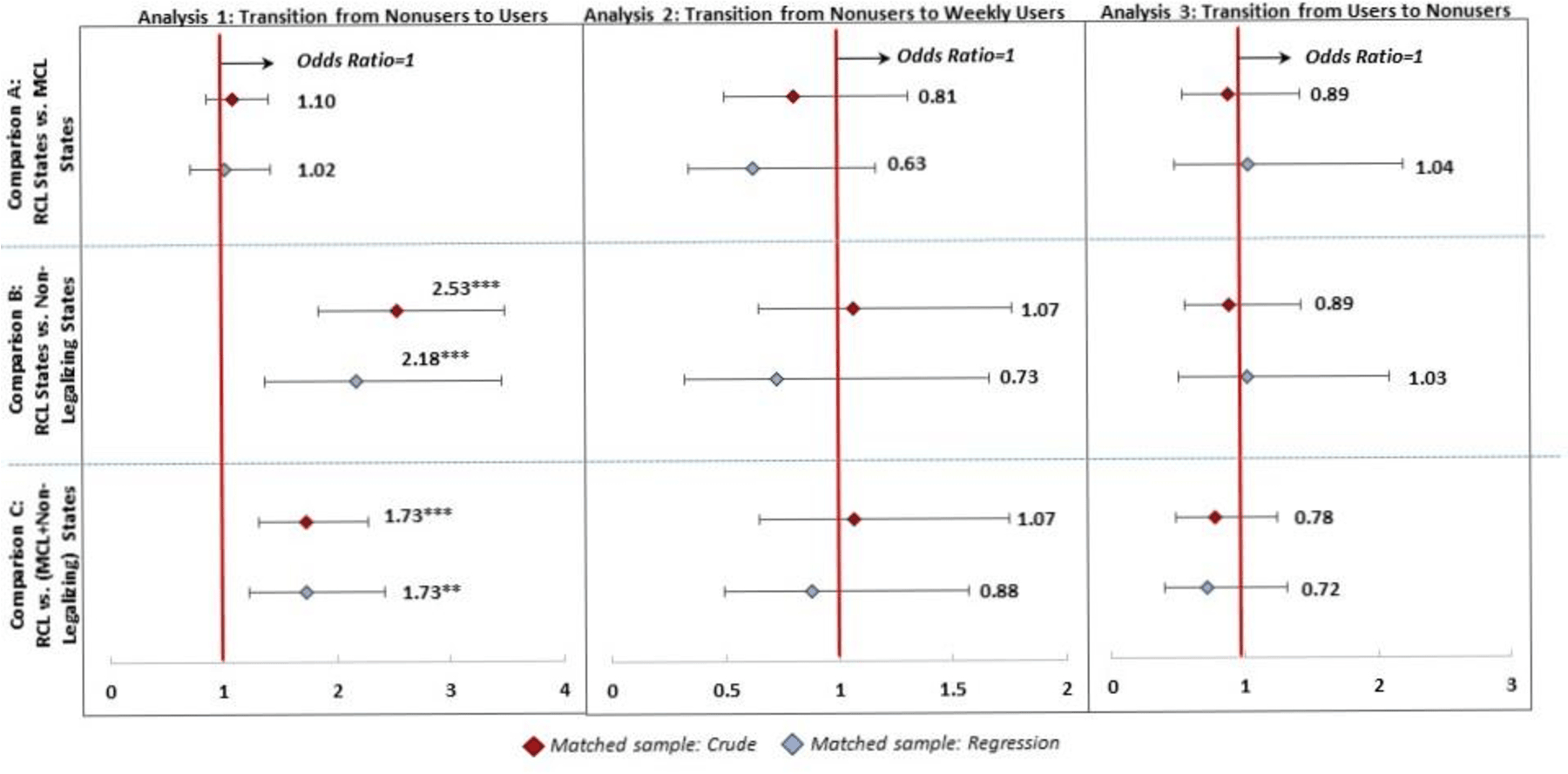
Notes:
1) **p<.01, ***p<.001.
2) Dots and lines represent odds ratios and associated 95% confidence intervals, respectively.
3) Crude results from Model 3 report estimated odds ratios in matched samples without further statistical adjustment.
4) Regression results from Model 4 report estimated odds ratios in matched samples adjusting for individual and state covariates.
5) Detailed results are reported in Table S12.
Figure 4 reports Models 3 and 4 results in matched adult sample after PSM (detailed results in Table S13). In Model 4 regressions controlling for covariates, RCL was associated with a higher odds of transition from nonusers to users when RCL states were compared to non-legalizing states (1.68, 1.15–2.46, p=0.007) and MCL and non-legalizing states combined (1.51, 1.11–2.07 p=0.010). RCL was associated with a higher odds of transition from nonusers to weekly users when RCL states were compared to non-legalizing states (1.82, 1.00–3.31, p=0.048) and MCL and non-legalizing states combined (2.09, 1.19–3.66, p=0.010). RCL was also associated with a lower odds of transition from users to nonusers when RCL states were compared to non-legalizing states (0.54, 0.35–0.81, p=0.003). We did not find evidence that RCL was associated with any type of transitions when RCL states were compared to MCL states alone. The associations found in Model 4 were consistent with results from Model 3, but Model 3 also suggested that RCL was associated with a higher odds of transitions from nonusers to users and from nonusers to weekly users when RCL states were compared to MCL states.
Figure 4. The Association between Recreational Cannabis Legalization and Cannabis Use Transitions, PATH Adult Sample.
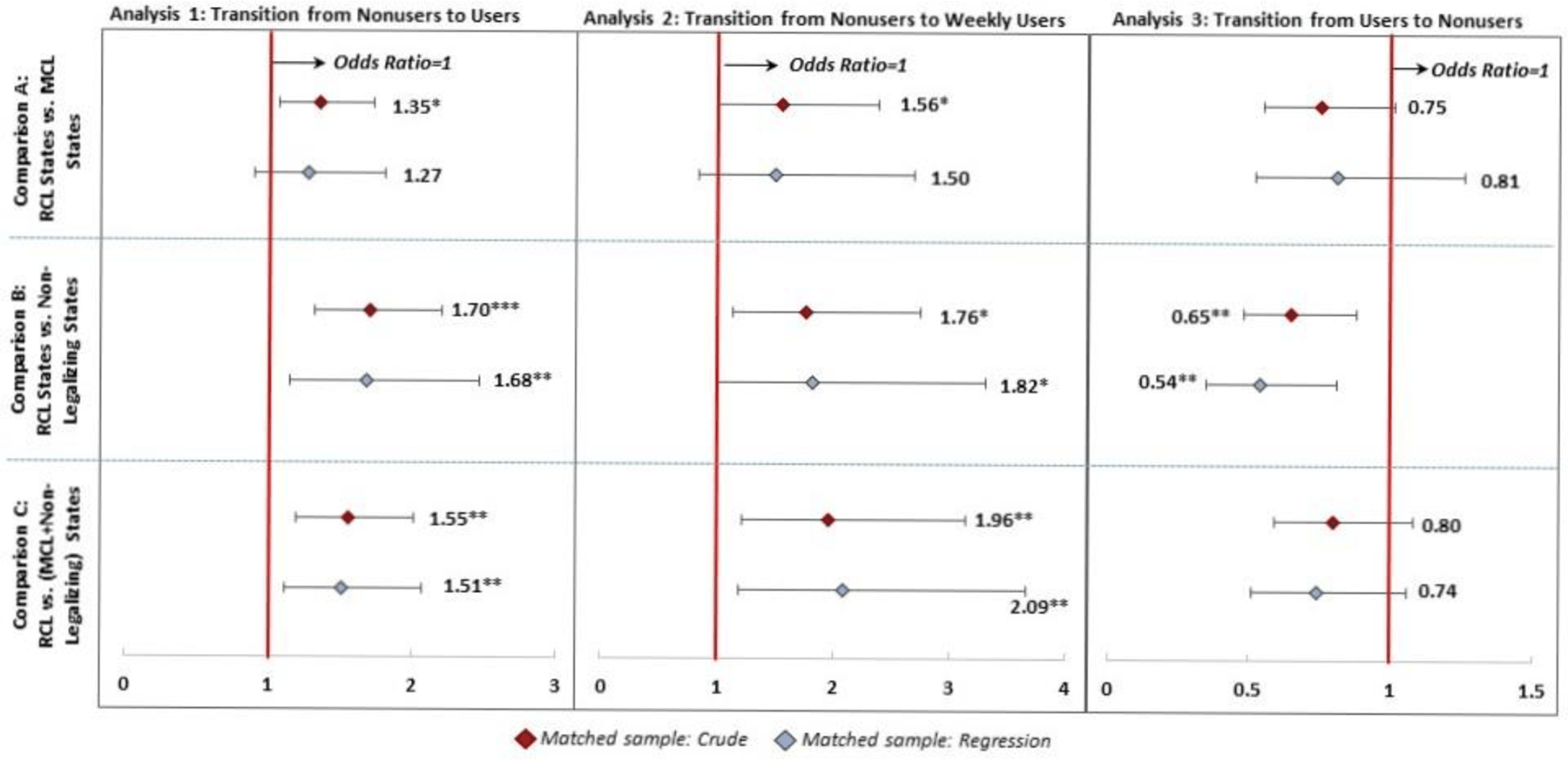
Notes:
1) *p<.05, **p<.01, ***p<.001.
2) Dots and lines represent odds ratios and associated 95% confidence intervals, respectively.
3) Crude results from Model 3 report estimated odds ratios in matched samples without further statistical adjustment.
4) Regression results from Model 4 report estimated odds ratios in matched samples adjusting for individual and state covariates.
5) Detailed results are reported in Table S13.
Tables S12–13 also report results from Models 1 and 2 before PSM. All the results were similar to Models 3 and 4 in youth sample. Models 1 and 2 results were also similar to Models 3 and 4 in adult sample except that RCL was also associated with a lower odds of transition from users to nonusers when RCL states were compared to MCL and non-legalizing states combined in Models 1 and 2.
Sensitivity Analysis
We replicated Model 4 analysis with alternative PSM matching algorithms (Table S14 for youths and Table S15 for adults). The associations found in the main analysis were generally robust to alternative matching algorithms.
DISCUSSION
This study contributes to the literature by using data on a large nationally representative longitudinal cohort in the US. The distinguishing feature of the current study alleviated the concern of ecological fallacy, which plagued most of the previous research using repeated cross-sectional data to evaluate aggregate-level changes over time. Overall, our findings provided some evidence on elevated odds of transition from cannabis nonusers to users among both youths and adults following RCL in four US states.
Our results suggested associations between RCL and cannabis use transitions if we compared RCL states to states without any type of cannabis legalization. Youths may have a higher odds of transitioning from cannabis nonusers to users if they were exposed to RCL during the transition. This finding was consistent with some repeated cross-sectional studies (5, 8, 11) and small-scale longitudinal cohort studies (14). Adult cannabis nonusers may have higher odds of transitioning to users as well as transitioning to frequent users, corroborating a repeated cross-sectional study on adult population. (11) In addition, adult cannabis users may have a lower odds of transitioning to nonusers. We encourage future research to validate our findings with alternative data sources.
We summarized our study findings as “some evidence” on the associations, because these associations were almost all manifested in comparisons to non-legalizing states and MCL and non-legalizing states combined. The associations in comparison between RCL and MCL states were not evident. This implies that RCL possibly had no independent impacts on top of MCL. If non-legalizing states pass MCL and RCL at the same time or pass RCL without MCL, cannabis use will be likely increased as indicated in our study. This scenario, however, is less likely to happen in the current legal and social contexts of the US. Meanwhile, it is worth noting that most of the previous research used MCL and non-legalizing states combined as comparison states (5, 8, 9, 11) and interpreted observed associations as evidence for the impacts of RCL. We could also adopt this interpretation but would like to leave the discretion to readers.
If past-month cannabis use is a steady status, we could roughly consider transition from nonusers to users/weekly users as cannabis initiation and transition from users to nonusers as cannabis cessation. In this case, we provided support that RCL may be associated with cannabis initiation but found less evidence on the association between RCL and cannabis cessation. This interpretation should be taken with caution, because individuals who used cannabis in the past month may include those using cannabis only occasionally, especially among youths who were in experiencing stage and have not established long-term behaviors. This interpretation may be more valid for adults but less so for youths.
This study is not without limitations. First, we reduced observed heterogeneities by PSM, but we were unable to account for unobserved confounding factors. Our findings hence should not be interpreted as causality. Second, cannabis use outcomes were self-reported and subject to reporting bias. Particularly, RCL may impact the willingness of a respondent to disclose cannabis use. We were also not able to control for the history of cannabis use prior to Wave 3. Further, cannabis use questions in PATH are very general. As vaping and edibles become increasingly popular following RCL, detailed cannabis use measures are required to evaluate the impacts on administration methods and product types.
Third, three out of the four RCL states implemented RCL one to two months after PATH Wave 4 data collection began. As a result, a very small portion of respondents in Wave 4 were not yet exposed to RCL when Wave 4 data were collected. Unfortunately, we were not able to identify this small group because exact survey dates in PATH were not publicly available. The incorrect assignment of policy exposure in this small group may attenuate the association estimation towards null. Fourth, each PATH wave was nationally representative as a whole, but it was not designed to be representative at state level. The nonrandom attrition between Wave 3 and Wave 4 may also slightly reduce the generalizability of the findings.
Fifth, the sample size in some analyses in youth sample was small despite comparable or larger than previous cohort studies. (14, 15). Insufficient statistical power may explain the lack of evidence in youth sample. Sixth, we evaluated outcomes within one year of RCL implementation, which may not be long enough to observe long-term behavioral transitions especially after the retail markets were fully open.
Finally, we grouped four RCL states into one treatment group due to sample size consideration, but we acknowledged that the provisions of RCL vary by state. Recent research highlighted the importance of accounting for cannabis law heterogeneity. (28, 29) We hope future research could explore the differential associations with law provisions. Law heterogeneity may also limit the generalizability of our findings to early adopters such as Colorado and Washington and most recent adopters such as Connecticut, New Mexico, and New York.
The results should be interpreted with caution, but we believe that they still provide useful information to policymakers and public health practitioners interested in understanding the consequences of RCL. We showed that changes in behaviors at individual level may be indeed associated with changes in cannabis legal status at state level, providing support to previous studies reporting changes in use prevalence at state level. The increase in cannabis use may happen not only among adults, but also among youths who bear health and economic consequences in adolescence and adulthood. (3, 4) Prevention strategies are particularly meaningful as the evidence on the association between RCL and transition from nonusers to users was stronger than the association between RCL and transition from users to nonusers.
CONCLUSION
Using data on a large nationally representative longitudinal cohort in the US, we found some evidence suggesting that RCL was associated with elevated odds of transition from cannabis nonusers to users among both youths and adults. Future research is warranted to assess long-term, detailed outcomes and generalizability to other jurisdictions.
Supplementary Material
WHAT THIS RESEARCH ADDS.
This study added new evidence to the relationship between recreational cannabis legalization and cannabis use by estimating the likelihoods of individuals transitioning to different cannabis use status following the legalization in the US.
It is the first study to estimate individual-level changes among a representative longitudinal cohort.
There was some evidence suggesting that recreational cannabis legalization was associated with elevated odds of transition to cannabis users among both youths and adults.
Grant Support
This research was supported by grant R01DA042290 (PI: Shi) and grant R01DA049730 (PI: Shi) from the US National Institute on Drug Abuse. This article is the sole responsibility of the authors and does not reflect the views of the National Institute on Drug Abuse.
Footnotes
DISCLOSURES
Declarations of Competing Interest: The authors report no financial relationships with commercial interests.
Nine states were further excluded from the analysis because respondents in those states had incomplete information on outcomes of interest or covariates.
REFERENCES
- 1.Substance Abuse and Mental Health Data Archive. Interactive NSDUH state estimates; 2019. [Google Scholar]
- 2.Hartman M Cannabis overview,. National Conference of State Legislature.; 2021. [Google Scholar]
- 3.Volkow ND, Baler RD, Compton WM, Weiss SR Adverse health effects of marijuana use, N Engl J Med 2014: 370: 2219–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hall W, Degenhardt L Adverse health effects of non-medical cannabis use, The Lancet 2009: 374: 1383–1391. [DOI] [PubMed] [Google Scholar]
- 5.Cerdá M, Wall M, Feng T, Keyes KM, Sarvet A, Schulenberg J et al. Association of state recreational marijuana laws with adolescent marijuana use, JAMA Pediatr 2017: 171: 142–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dilley JA, Richardson SM, Kilmer B, Pacula RL, Segawa MB, Cerdá M Prevalence of cannabis use in youths after legalization in Washington state, JAMA Pediatr 2019: 173: 192–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson DM, Hansen B, Rees DI, Sabia JJ Association of marijuana laws with teen marijuana use: new estimates from the youth risk behavior surveys, JAMA Pediatr 2019: 173: 879–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bae H, Kerr DC Marijuana use trends among college students in states with and without legalization of recreational use: initial and longer‐term changes from 2008 to 2018, Addiction 2020: 115: 1115–1124. [DOI] [PubMed] [Google Scholar]
- 9.Kerr DCR, Bae H, Phibbs S, Kern AC Changes in undergraduates’ marijuana, heavy alcohol and cigarette use following legalization of recreational marijuana use in Oregon, Addiction 2017: 112: 1992–2001. [DOI] [PubMed] [Google Scholar]
- 10.Shi Y, Liang D The association between recreational cannabis commercialization and cannabis exposures reported to the US National Poison Data System, Addiction 2020: 115: 1890–1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cerdá M, Mauro C, Hamilton A, Levy NS, Santaella-Tenorio J, Hasin D et al. Association between recreational marijuana legalization in the United States and changes in marijuana use and cannabis use disorder from 2008 to 2016, JAMA Psychiatry 2020: 77: 165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caputi TL, Sabet KA Population-Level Analyses Cannot Tell Us Anything About Individual-Level Marijuana-Opioid Substitution, Am J Public Health 2018: 108: e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harris AHS, Humphreys K, Finney JW State-Level Relationships Cannot Tell Us Anything About Individuals, American Journal of Public Health 2015: 105: E8–E8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bailey JA, Epstein M, Roscoe JN, Oesterle S, Kosterman R, Hill KG Marijuana legalization and youth marijuana, alcohol, and cigarette use and norms, Am J Prev Med 2020: 59: 309–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barker AK, Moreno MA Effects of recreational marijuana legalization on college students: a longitudinal study of attitudes, intentions, and use behaviors, J Adolesc Health 2021: 68: 110–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rusby JC, Westling E, Crowley R, Light JM Legalization of recreational marijuana and community sales policy in Oregon: Impact on adolescent willingness and intent to use, parent use, and adolescent use, Psychol Addict Behav 2018: 32: 84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Epstein M, Bailey JA, Kosterman R, Furlong M, Hill KG Evaluating the effect of retail marijuana legalization on parent marijuana use frequency and norms in U.S. States with retail marijuana legalization, Addict Behav 2020: 111: 106564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hyland A, Ambrose BK, Conway KP, Borek N, Lambert E, Carusi C et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study, Tob Control 2017: 26: 371–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shi Y, Liang D, Bao Y, An R, Wallace MS, Grant I Recreational marijuana legalization and prescription opioids received by Medicaid enrollees, Drug Alcohol Depend 2019: 194: 13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liang D, Wallace MS, Shi Y Medical and non‐medical cannabis use and risk of prescription opioid use disorder: Findings from propensity score matching, Drug Alcohol Rev 2019: 38: 597–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yao XI, Wang X, Speicher PJ, Hwang ES, Cheng P, Harpole DH et al. Reporting and guidelines in propensity score analysis: a systematic review of cancer and cancer surgical studies, J Natl Cancer Inst 2017: 109: djw323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Austin PC Double propensity-score adjustment: a solution to design bias or bias due to incomplete matching, Stat Method Med Res 2017: 26: 201–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Austin PC An introduction to propensity score methods for reducing the effects of confounding in observational studies, Multivar Behav Res 2011: 46: 399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Austin PC, Grootendorst P, Anderson GM A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: a Monte Carlo study, Stat Med 2007: 26: 734–753. [DOI] [PubMed] [Google Scholar]
- 25.Aldridge A, Dowd W, Bray J The relative impact of brief treatment versus brief intervention in primary health‐care screening programs for substance use disorders, Addiction 2017: 112: 54–64. [DOI] [PubMed] [Google Scholar]
- 26.Austin PC Statistical criteria for selecting the optimal number of untreated subjects matched to each treated subject when using many-to-one matching on the propensity score, Am J Epidemiol 2010: 172: 1092–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Austin PC Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research, Commun Stat-Simul C 2009: 38: 1228–1234. [Google Scholar]
- 28.Cerda M Commentary on Bae & Kerr (2020): Recreational marijuana legalization-we need to think about heterogeneity of policy effects, Addiction 2020: 115: 1125–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Johnson JK, Doonan SM Cannabis Policy Heterogeneity and Effects on Research-Complexity Expected, JAMA Netw Open 2021: 4: e212545. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


