Abstract
We investigate the impacts of a perinatal psychosocial intervention on trajectories of maternal mental health and child skills, from birth to age 3. We find improved maternal mental health and functioning (0.17 to 0.29 SD), modest but imprecisely estimated improvements in parenting (0.07 to 0.11 SD), and transitory improvements in child socioemotional development (0.06 to 0.39 SD). The intervention had negligible influence on physical health and cognition. Estimates of a skill production function reveal the intervention attenuated the negative association between maternal depression and child outcomes, and narrowed outcome gaps between mothers who were and were not depressed in pregnancy.
Keywords: Mental health, stress, socioemotional, RCT, child development, technology of skill formation, gender
1. Introduction
Social and emotional skills are an integral component of human capital. Children living in disadvantaged families, with mothers more likely to be suffering from poor mental health or depression, tend to show greater socioemotional difficulties (Rahman et al., 2013; Hollins, 2007; Bennett et al., 2016; Halfon et al., 2014; Attanasio et al., 2022a). Socioemotional difficulties become apparent early in life, and are prone to get ingrained and intensify over time, in a cascading cycle of disadvantage (Feil et al., 1995; Sprague and Walker, 2000).1 For instance, there is some evidence that socioemotional problems at ages 1–3 predict socioemotional difficulties in elementary school (Briggs-Gowan and Carter, 2008), which in turn reduce school performance (Fletcher, 2010; Ding et al., 2009; Busch et al., 2014; Bhalotra et al., 2021) and predict mental health issues in early adulthood (Class et al., 2019; National Scientific Council on the Developing Child, 2012). Despite these patterns, causal evidence of the consequences of maternal depression, or its treatment, for child socioemotional skills is relatively scarce.
In this paper, we analyze the impact of a perinatal psychosocial intervention targeted at depressed mothers on the joint evolution of maternal mental health and functioning, parental investment, and child skills from birth through to three years of age. The skills that we analyse encompass not only socioemotional, but also cognitive skills and physical health. This inclusion is important as these skills tend to evolve jointly. Our focus is on the mother since she is the primary caregiver in our setting and, in general, the child interacts with her more than with anyone else. As a result, her mental health and functioning have a potentially strong influence on the child. Depression and stress often manifest in low energy, impaired functionality, insomnia, poor concentration, pessimism, and a lack of interest in one’s environment (de Quidt and Haushofer, 2018). It is thus plausible that depression modifies the mother’s parenting behaviors and investment in the child (Herba et al., 2016; Baranov et al., 2020; Angelucci and Bennett, 2021). A rich literature in developmental psychology posits that improving maternal depression can lead to more responsive mother-child interactions and support secure infant attachment (Erickson et al., 2019; Tsivos et al., 2015).
The intervention we study, the Thinking Healthy Programme - Peer Delivered (THPP), was targeted at perinatally depressed women in rural Pakistan. So as to improve scalability, it was delivered by trained peer-volunteers through a combination of home visits and group sessions. In total, between the third trimester of pregnancy and the child turning 3 years of age, a mother in the program received 32 sessions. The intervention provided cognitive behavioral therapy with a focus on behavioral activation, self-care, and the child’s health and development. Thus the content of the program was such that it could influence child outcomes directly, or through modifying the mother’s mental health and her parenting behaviors.
Rich longitudinal data on mother-child pairs were collected in multiple waves throughout the intervention period. Socioemotional skills are measured using the Ages and Stages Questionnaire-Social-Emotional (ASQ-SE) which contains validated psychometric indices of competencies in self-regulation, adaptive functioning, emotional balance, communication, and prosociality. Cognitive skills are tested using the Bayley Scales of Infant Development (Bayley-III) which includes cognitive, language, and motor skills. Maternal mental health and functioning are assessed using established scales for measurement of depression (a clinical assessment and symptom severity), stress, and functional disability. Parental investment in children is measured using the HOME score, assessing the quality of cognitive stimulation and emotional support in the household.
In order to link the observed variables in the dataset to the underlying developmental trajectories of children, we use a latent variable approach, common in psychometrics and economics (Spearman, 1904; Jöreskog and Goldberger, 1975; Carneiro et al., 2003). We generate factor scores and use these to estimate treatment effects on six indicators: cognition, physical development, and socioemotional skills of the child; parental investment; maternal mental health, and maternal functioning. The reduced form treatment effects tell us how the intervention modified inputs to child development (note that child skills at a younger age are inputs to child skills at an older age). So as to synthesize these reduced-form results, and describe how the intervention modified the returns to the inputs, we estimatethe production functions for child skills in the first three years of life, using as a point of departure, the formulation in Cunha and Heckman (2008); Attanasio et al. (2020c).
We make two main contributions. First, we identify the impact of the intervention on trajectories of maternal mental health, parenting, and child development. In contrast to much of the literature, we use longitudinal data on children from birth to age 3, and we allow intervention impacts to vary with age, identified at 6, 12, and 36 months after birth.2 We find that the intervention improves maternal mental health (ranging from 0.17 to 0.27 standard deviations, SD) and daily functioning (0.18 – 0.29 SD) immediately (at 6 months) and persistently up until the end of the study window, 36 months after birth. The intervention results in weakly identified increases in parental investment at 12 and 36 months (0.07 – 0.11 SD), and a short-term positive effect on the child’s socioemotional skills at 6 and 12 months (0.19 – 0.39 SD), without any discernible impacts on the other domains of child development (physical health impacts ranged from −0.17 to 0.02 SD and cognitive development impacts ranged from −0.08 to 0.06 SD). All of these results are stronger for mothers of boys.
Our second contribution is to estimate a model of child skill formation in which, in a departure from related studies (Cunha and Heckman, 2008; Cunha et al., 2010; Attanasio et al., 2020a), we include dynamic latent factors measuring maternal mental health (including depression and stress) and functioning. We conceptualize maternal mental health as a capital input in the production function, a stock that can depreciate over time or that can be invested in, for instance with therapy.
Similar to other studies estimating the child skills production function, we do not have multiple instruments and we cannot identify causal effects of (endogenous) inputs. However, we allow the model parameters to vary by treatment arm. The model allows the intervention to influence both the levels and the productivity of the inputs, similar in spirit to Kitagawa (1955); Oaxaca (1973); Blinder (1973).
Our findings suggest that maternal mental health is an important input in the technology of skill formation, especially for moderately or severely depressed mothers, and that the intervention changes the shape of the production function, especially in the first year of life. In the control group, all child skills are increasing in maternal mental health, but at a decreasing rate. We see a larger improvement in children’s skills when moving from severe to moderate depression than we do when moving from moderate to mild depression. The intervention shifts the production function up (an increase in TFP), and also attenuates the slope of the production function with respect to maternal mental health, leading to improvements in skills particularly for children whose mothers did not recover from depression.3 The intervention modifies the production function parameters in a manner that brings outcomes for treated mothers closer to outcomes for mothers who were not depressed at baseline.
These findings help reconcile the pattern of results identified in the reduced form models of intervention effects, namely, the absence of durable effects of the intervention on child skills alongside long-lasting improvements in maternal mental health. The intervention helps women recover from depression and stress, and it also improves children’s socioemotional skills in the short run. We might have surmised from this evidence that the improvement in maternal mental health at 6 and 12 months was the cause of the improvement in socioemotional skills at 12 months. However the production function estimates suggest this is not the case, as the intervention improves child socioemotional skills particularly in the sample of mothers who do not recover from depression. This is consistent with the fact that the intervention did not just provide therapy for the mother’s depression, it also provided information and support for child development. Our estimates indicate that the latter shielded children from the negative consequences of poor maternal mental health. As time progresses, additional increases in the stock of maternal mental health shift the treated group into a flatter part of the production function, where variation in the underlying measure of mental health is less predictive of child skills. Thus it makes sense that, although on average maternal mental health in the treated group remained persistently better than in the control group, other aspects of the intervention enabled the control group children to catch up with the treated children, resulting in convergence by 36 months in their (socioemotional) skills. The production function estimates also contribute to still scarce evidence on self- and cross-productivity of skills across domains at very early ages.
Understanding how maternal depression at birth may influence the formation of skills in the early years is important given the high prevalence of maternal depression: it is estimated that between 10 and 30 percent of children worldwide are exposed to maternal depression at birth, and that this share is higher in developing countries (O’hara and Swain, 1996; Parsons et al., 2012). Maternal depression is often undiagnosed and untreated, and between a third and a half of all women who are depressed during pregnancy remain depressed a year later, which implies a significant duration of exposure for many children.
Our finding that maternal mental health (in the control group of women diagnosed as clinically depressed at baseline, and not treated) is linked to the child’s socioemotional development has important consequences. A number of studies have documented that socioemotional skills in childhood are predictive of adult outcomes including mental health, educational attainment, and earnings (Currie and Stabile, 2006; Bennett et al., 2016; Halfon et al., 2014). Another strand of the literature demonstrates that socioemotional skills have an even longer-lasting impact, influencing the next generation.
In particular, a number of studies show a positive intergenerational correlation in socioemotional skills (Loehlin, 2005; Groves, 2005; Anger, 2012; Dohmen et al., 2012; Grönqvist et al., 2017; Attanasio et al., 2022a). Most of the cited studies measure socioemotional outcomes in adolescence or adulthood. One study that, like us, measures socioemotional outcomes in childhood is Attanasio et al. (2022a). However, they associate the child’s outcome with the mother’s socioemotional skills when she was a child, whereas we are primarily interested in the mother’s socioemotional skills when she is parenting the newborn child. A second difference in our study from the cited literature is that it is set in a developing country, and we know much less about socioemotional developmental paths in these settings. Third, none of the cited studies uses experimental variation in the mother’s socioemotional skills.
The paper is laid out as follows. Section 2 provides the details of the intervention, discusses baseline balance and attrition over time, describes the data set and the outcomes, and discusses the methodology used to reduce the dimensionality of the outcome space and estimate the treatment effects; Section 4 presents the empirical results; Section 5 discusses the mechanisms through the lens of a simple structural model; and Section 6 concludes.
2. Study Design and Data
2.1. The Intervention
We use longitudinal data on a pregnancy cohort, established in the context of a clustered Randomized Controlled Trial (RCT) in rural Punjab, Pakistan, a low-resource context characterized by a high prevalence of maternal depression and limited access to clinical mental health care. The trial recruited women who were depressed during pregnancy and provided them with a 3-year-long, peer-delivered psychosocial intervention (Thinking Healthy Programme Peer-Delivered Plus, THPP+) consisting of cognitive behavioral therapy with a focus on behavioral activation, self-care, and attention to the infant’s health and development.
Depression Screening.
Between October 2014 and February 2016, all pregnant women who were eligible for the study—married, resident in Kallar Syedan, a subdistrict of Rawalpindi in Pakistan, and not in need of immediate medical attention, were approached and screened for depression using the Patient Health Questionnaire (PHQ-9). The PHQ-9 is a standard instrument for screening and monitoring the severity of depression; it includes questions about the frequency of depressive symptoms in the last two weeks, such as lack of interest or ability to concentrate, feelings of sadness or hopelessness, sleeping or eating problems, restlessness, suicidal thoughts. Pregnant women who scored 10 or more on the PHQ-9 were invited to participate in the trial.
Among 1731 women who were screened for depression, 572 (33%) were identified as depressed according to the PHQ-9 criteria. 287 of these mothers were in the clusters randomized to the intervention, 283 in the control clusters, and two mothers refused to participate before the baseline assessment. Of the 1159 pregnant women who were screened as not depressed, 584 were randomly selected to constitute the non-depressed arm of the study. They represent a natural reference group to understand the evolution of maternal and child outcomes, and to benchmark the potential effectiveness of the intervention.
Randomization.
The trial was randomized across 40 village clusters. These clusters were geographically separate to minimize the risk of spillover. Twenty clusters were randomized into receiving the intervention and twenty to the control arm. Each village cluster contributed approximately 14 perinatally depressed women. Research teams responsible for identifying, obtaining consent, allocating, and interviewing study participants were blind to the participants’ original depression status and their allocation across the study arms.
THPP+ Intervention.
Thinking Healthy Programme Peer-Delivered Plus (THPP+) is a low-intensity scaleable psychosocial intervention delivered by volunteer peer women from the same community as the mother. Peers received prior classroom training in accordance with the intervention content, which builds on a previous intervention that proved very successful in a similar context (Rahman et al., 2008). They were provided supervision throughout the trial period. The intervention strategy includes behavioral activation to overcome unhealthy thinking with a focus on self-care and infant development.
The timeline of the THPP+ intervention and all follow-up surveys is summarized in Figure 1. In the intervention group, depressed women received a combination of individual and group sessions. Starting from the third trimester of pregnancy until 6 months postpartum, participants attended ten individual and four group-based sessions, with a primary focus on modifying maladaptive thoughts and behaviors frequently observed among individuals experiencing depression. From 7 to 36 months postnatal, another 18 group sessions were delivered: the first six sessions were delivered monthly, the rest every two months. The content of these lower-intensity booster sessions was a continuation of the behavioral activation strategy with a special focus on contributing to the mother-child interaction and child development by providing examples of age-appropriate activities as well as information about childcare. Since a large part of the intervention was delivered in group sessions, the social component of meeting with other mothers, alongside the behavioural activation content discussed during the sessions, might have contributed to any intervention effects.
Figure 1:
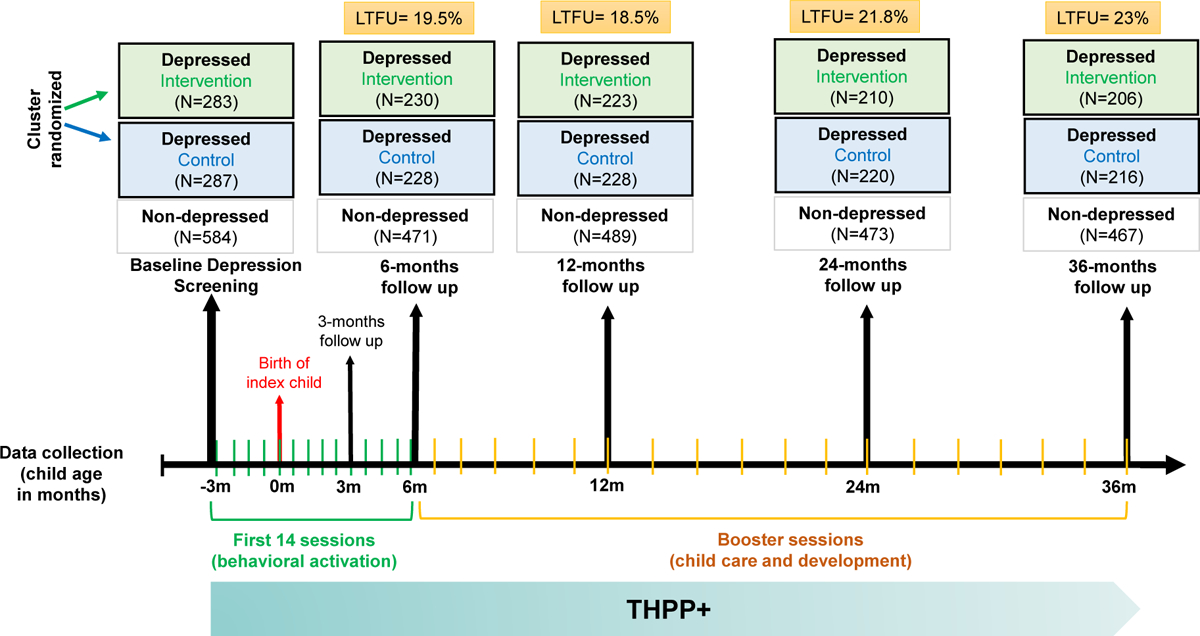
Timeline of THPP+ Intervention and Follow-ups
Perinatally depressed women in the treatment arm received the THPP+ intervention throughout the trial, while women in the control arm received Enhanced Usual Care (EUC). EUC is the routine health care provided in the region. It is enhanced in the sense that the participants were informed of their depression status and offered guidance about how to seek help. Women who were not diagnosed as perinatally depressed (non-depressed group) did not receive any treatment.4
Sample and longitudinal follow up.
Our study sample consists of the experimental group of depressed mothers who were randomized into treatment and control arms, and the group of mothers who were not depressed at baseline. Data collection on the mother-child dyads was done six times: at the third trimester of pregnancy and 3, 6, 12, 24, and 36 months postpartum. Figure 1 provides the compositions of the follow-up samples and the respective loss-to-follow-up rates (LTFU). A longitudinal comparison requires a similar measurement system over time, but we have no measure of cognition at 3, 6, and 24 months and we have a different measure of parental investment at 24 months (see Table A1). For consistency, we only analyse data from the waves at 6, 12, and 36 months.5
2.2. Measurement and Outcomes
The data contain multiple validated and widely used scales of maternal mental health and functioning, and of the cognition, socioemotional, and physical health of children. A full list of measures is provided in Table A1 in the Appendix.
To measure maternal mental health across all of the waves, we use the Patient Health Questionnaire (PHQ-9) and the Structured Clinical Interview for DSM (SCID), a 13-item semi-structured interview for making the major DSM-5 diagnoses. We also include the Cohen Perceived Stress Scale (PSS), a 10-item instrument among the most widely used in the psychological literature to measure self-reported stress. To measure her functioning, we use the WHO Disability Assessment Schedule (WHO-DAS), a 17-item assessment instrument developed by the World Health Organization (WHO) to evaluate across cultures and domains a person’s ability to perform various activities of daily living.
To assess the child’s cognitive development at 12 and 36 months of age, we use five scales from the Bayley Scales of Infant Development (Bayley-III). These scales measure various aspects of infant and toddler development in the following domains: Cognitive, Language (Receptive and Expressive), and Motor (Gross and Fine).
To measure the child’s socioemotional skills we use the social-emotional sub-scale of the Ages and Stages Questionnaire: (ASQ-SE), a validated screening tool for assessing social-emotional development in children aged 1 month to 6 years (Lamsal et al., 2018).6 The ASQ-SE uses parent-reported questions to identify potential difficulties or delays in the areas of self-regulation, compliance, communication, adaptive functioning, autonomy, interaction with people, and affect (the child’s ability or willingness to demonstrate their own feelings and empathy for others). At age 36 months we also include the Strengths and Difficulties Questionnaire (SDQ), a brief behavioral screening questionnaire used to assess children’s mental health. It has sub-scales to detect emotional symptoms, conduct problems, hyperactivity and inattention, peer relationship problems, and prosocial behaviour.
The child’s physical health was assessed by measuring their weight, height, and head circumference from 3 to 36 months. These measurements were converted to age-adjusted Z-scores, serving as proxies for the child’s anthropometrics and indicating their physical growth and development.
To measure parental investment at 12 and 36 months we used the HOME inventory, a well-established observational tool that evaluates the quality of cognitive stimulation and emotional support offered by parents to their child. It is a widely used measure to examine the level of parental investment in a child’s development.
Given the richness of the data for both mothers and children, we aggregate outcomes into indices to overcome measurement error problems, improve statistical power, reduce the dimensionality of the data, and mitigate the issue of multiple hypothesis testing. We present the main results using latent factor scores, described below, although patterns are similar using Inverse Covariance Weighted (ICW) indices.7
2.3. Balance and Attrition
Balance:
The experimental sample was slightly imbalanced at baseline, as shown by the summary statistics in Table 1. For instance, pregnant women in the treatment arm were on average 1 cm taller and lived in households with 0.3 more people per room than women in the control clusters. Treated women also suffered from slightly—albeit not significantly—worse mental health, scoring 0.4 higher on the PHQ-9 (depression), 0.6 on the WHODAS (functioning), and 0.9 on the PSS (stress). A joint F-test rejects balance of baseline characteristics (p-value=0.01).8 Splitting by gender of the index child shows that the sample of mothers of boys is more balanced than that of girls: treated mothers of girls scored 1.6 higher on the PSS, had 0.5 higher number of people per room, lower socio-economic status, and less educated husbands (Table A8). However, a joint test of balance for covariates within each gender group does not indicate any statistically significant imbalance, possibly due to lower statistical power (p-values of 0.41 for mothers of boys and 0.12 for mothers of girls).
Table 1:
Baseline Balance
| Baseline Sample (N=1154) | 6-months (N=929) |
12-months (N=940) |
24-months (N=903) |
36-months (N=889) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | Treatment | Nondep. | Diff. | p-val | Diff. | Diff. | p-val | Diff. | p-val | Diff. | p-val | Diff. | ||||
| Mean | SD | Mean | Mean | (ND-D) | (T-C) | p-val | (T-C) | (T-C) | (T-C) | (T-C) | p-val | |||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | (13) | (14) | (15) | (16) | |
| Mother’s Age | 27.289 | 4.973 | 26.802 | 26.373 | −0.674 | 0.023 | −0.487 | 0.260 | −0.595 | 0.215 | −0.361 | 0.434 | −0.310 | 0.510 | −0.314 | 0.478 |
| Mother’s height (cm) | 156.330 | 6.088 | 157.429 | 157.105 | 0.230 | 0.545 | 1.100 | 0.074 | 0.996 | 0.145 | 1.043 | 0.109 | 1.352 | 0.031 | 1.023 | 0.131 |
| Mother’s weight (kg) | 61.241 | 12.883 | 60.172 | 59.887 | −0.823 | 0.186 | −1.070 | 0.359 | −1.205 | 0.325 | −0.861 | 0.476 | −1.065 | 0.432 | −1.286 | 0.385 |
| Mother’s waist circ. (in) | 37.555 | 4.088 | 36.852 | 37.134 | −0.071 | 0.746 | −0.704 | 0.115 | −0.793 | 0.068 | −0.628 | 0.421 | −0.843 | 0.075 | −0.688 | 0.176 |
| Mother’s blood pressure | 72.326 | 12.790 | 70.915 | 71.667 | 0.043 | 0.950 | −1.411 | 0.173 | −0.352 | 0.723 | −1.169 | 0.263 | −0.339 | 0.748 | −1.049 | 0.308 |
| PHQ total | 14.484 | 3.580 | 14.894 | 2.796 | −11.891 | 0.000 | 0.410 | 0.248 | 0.400 | 0.305 | 0.484 | 0.227 | 0.364 | 0.362 | 0.380 | 0.347 |
| WHODAS total | 16.111 | 9.119 | 16.714 | 5.613 | −10.798 | 0.000 | 0.602 | 0.475 | 0.600 | 0.513 | 0.814 | 0.376 | 0.999 | 0.291 | 0.809 | 0.423 |
| PSS total | 22.899 | 7.523 | 23.841 | 12.212 | −11.154 | 0.000 | 0.942 | 0.100 | 1.311 | 0.036 | 1.113 | 0.072 | 1.216 | 0.062 | 1.020 | 0.151 |
| Current Major Dep. Episode | 0.732 | 0.444 | 0.777 | 0.021 | −0.734 | 0.000 | 0.046 | 0.373 | 0.055 | 0.359 | 0.039 | 0.509 | 0.044 | 0.461 | 0.045 | 0.443 |
| Joint/extended family | 0.634 | 0.483 | 0.580 | 0.707 | 0.100 | 0.000 | −0.055 | 0.175 | −0.058 | 0.228 | −0.049 | 0.321 | −0.060 | 0.206 | −0.075 | 0.096 |
| Grandmother present | 0.666 | 0.473 | 0.629 | 0.717 | 0.070 | 0.005 | −0.037 | 0.331 | −0.028 | 0.504 | −0.029 | 0.473 | −0.043 | 0.329 | −0.034 | 0.434 |
| Total adults in the hh | 5.700 | 2.993 | 5.332 | 5.985 | 0.467 | 0.011 | −0.368 | 0.201 | −0.320 | 0.334 | −0.325 | 0.316 | −0.212 | 0.527 | −0.281 | 0.402 |
| People per room | 2.473 | 1.870 | 2.792 | 2.215 | −0.416 | 0.001 | 0.319 | 0.087 | 0.325 | 0.078 | 0.348 | 0.056 | 0.322 | 0.066 | 0.316 | 0.097 |
| Number of girls | 0.854 | 1.064 | 0.958 | 0.663 | −0.243 | 0.000 | 0.104 | 0.328 | 0.071 | 0.120 | 0.090 | 0.433 | 0.124 | 0.308 | 0.051 | 0.655 |
| Number of boys | 0.787 | 0.961 | 0.855 | 0.560 | −0.261 | 0.000 | 0.068 | 0.443 | 0.002 | 0.987 | 0.023 | 0.817 | 0.037 | 0.705 | 0.039 | 0.700 |
| First child | 0.251 | 0.434 | 0.230 | 0.363 | 0.123 | 0.000 | −0.021 | 0.506 | −0.002 | 0.951 | 0.005 | 0.869 | −0.012 | 0.709 | −0.023 | 0.468 |
| SES asset index | −0.320 | 1.688 | −0.560 | 0.422 | 0.861 | 0.000 | −0.240 | 0.152 | −0.133 | 0.201 | −0.130 | 0.489 | −0.161 | 0.398 | −0.169 | 0.359 |
| Mother’s education | 6.801 | 4.546 | 6.827 | 8.567 | 1.753 | 0.000 | 0.025 | 0.957 | 0.376 | 0.428 | 0.311 | 0.537 | 0.087 | 0.863 | 0.096 | 0.849 |
| Father’s education | 8.331 | 3.288 | 7.848 | 9.151 | 1.059 | 0.000 | −0.483 | 0.134 | −0.560 | 0.117 | −0.609 | 0.102 | −0.844 | 0.026 | −0.750 | 0.037 |
| Life Events Checklist | 4.098 | 2.335 | 4.696 | 2.896 | −1.499 | 0.000 | 0.599 | 0.003 | 0.673 | 0.001 | 0.599 | 0.003 | 0.648 | 0.001 | 0.590 | 0.003 |
| Observations | 287 | 283 | 584 | |||||||||||||
| Joint test (p-value) | 0.011 | 0.028 | 0.053 | 0.018 | 0.141 | |||||||||||
Note: Table tests for balance of baseline characteristics. Columns 1, 3, and 4 show the mean in the control, treatment, and nondepressed group in the baseline sample, respectively. Column 5 shows the difference in means between non-depressed and depressed groups. Columns 7, 9, 11, 13, and 15 show the mean differences between treatment and control groups in the baseline sample and 6 months, 12 months, 24 months, and 36 months follow-up samples, respectively. p-values at the bottom of the table come from the F-test of overall significance from a regression of the treatment dummy on all the baseline controls.
Overall, this slight imbalance seems to be driven by small differences in participants’ baseline characteristics, not by systematic differences between treatment and control village-clusters. We confirm balance across village-clusters by using the mothers who were not depressed at baseline and lived in the same villages as treated and control mothers (Table A9). A joint test of balance using the baseline characteristics of mothers who were not depressed in pregnancy (baseline) shows balance across treatment and control clusters (p-value 0.456). Similarly, a joint test of balance using the whole sample (non-depressed and depressed mothers pooled) is not rejected. (p-value=0.317).
Attrition:
Lost to follow-up (LTFU) rates range between 18.5%−23% in the study period, and it is balanced across study arms. These attrition rates compare favorably with attrition rates in pregnancy cohort data. The main reason for being lost to follow-up was the death of the index child (constituting around 40% of the attritors),9 which was also balanced across study arms. We find some small imbalance in attritor characteristics (Tables A2–A5), but these differences are not statistically significant.10 Attritors generally had more crowded households and higher baseline PHQ-9 total scores. Attritors at 6 months additionally differ by having higher blood pressure and lower socio-economic status, and were more likely to be pregnant for the first time. Mothers who were lost to 36-month follow-up had higher weight and were more likely to co-reside with their mother or mother-in-law.
In the analysis to follow, we address baseline balance concerns by including covariates in the model, demeaned and interacted with the treatment indicator (Goldsmith-Pinkham et al., 2022). Although attrition is not differential by treatment status, we show that our estimates are robust to using inverse probability weights to adjust for attrition.
3. Analytical Framework
To study the impact of THPP+ on the developmental trajectory of maternal mental health and child skills, we use latent factor scores, following a long history in psychometrics (Spearman, 1904; Jöreskog and Goldberger, 1975) and a more recent one in economics (Cunha and Heckman, 2008; Cunha et al., 2010; Attanasio et al., 2020a,c). Latent factor analysis is a model-based approach that facilitates the study of maternal and child developmental trajectories by reducing measurement error and the dimensionality of the outcomes.
We construct the factor scores by assuming a separate measurement system for each domain and then employ Exploratory Factor Analysis (EFA) to select a concise set of measures. This approach helps us identify key factors that best represent the underlying constructs within each domain, while maintaining simplicity and efficiency in the measurement process. Following Agostinelli and Wiswall (2016), the scaling of each factor is standardized by normalizing the measure with the highest factor loading to one, while maintaining the same measure at all time points. The location is fixed by normalizing the means of the latent factors to zero for the control group at the initial time point (6 months). This approach ensures consistent and comparable scaling across the factors over the different time points in the analysis, allowing us to capture the growth of the latent factors over time.11
To close the model, we connect factor scores over time and capture the dynamic evolution of the child’s latent human capital. We follow Cunha and Heckman (2008); Attanasio et al. (2020a) and specify the production function for child development as:
| (1) |
where and are vectors for child skills in treatment arm —where indicates the control group, indicates the treatment group, and the baseline non-depressed—at time and respectively. stands for parental investment, which occurs between the realizations of and 12. is maternal mental health and functioning at time which we conceptualize as a capital input, contains baseline covariates measured before the treatment assignment, and is the vector of random shocks to child development. We allow the distribution of the latent factors and the parameters of the production function to vary by the child’s age (we estimate one production function at age 12 months and another one at age 36) and by intervention arm .
Allowing the factors and the parameters to vary by intervention arm, this model can be seen as a generalization of a Kitagawa-Oaxaca-Blinder decomposition (Kitagawa, 1955; Oaxaca, 1973; Blinder, 1973). The intervention can act through two main mechanisms: a change in the level of inputs, parental investments and maternal health; and a change in the returns to inputs, i.e. the efficiency with which the inputs translate into child outcomes. This change in efficiency can happen through a combination of changes in TFP, i.e. a different intercept and a shift of the whole production function upwards or downwards, and changes in input-specific-returns, i.e. a different slope of the production function and shift in the derivative between child development and a particular input or .13
We present illustrative examples of the pathways through which the intervention may impact the outcomes. First, it may increase the level of inputs, including maternal mental health and parental investments. For instance, the intervention could alleviate maternal depression by facilitating mothers’ engagement in activities that provide them with a sense of achievement and enjoyment through behavioral activation. Alternatively or in addition, it might encourage mothers to dedicate more quality time to their children and invest in enriching resources like new toys and educational materials, thereby enhancing the home environment (parental investment).14
The intervention may also alter the production function, influencing the way that inputs translate into outputs. For example, the intervention may increase the productivity of each unit of maternal time spent with the child by improving maternal focus and empathy, or by inducing a more age-appropriate use of time and physical resources. Conversely, it could potentially diminish the productivity of maternal mental health if there are decreasing returns. In particular, cases of maternal depression shifting from moderate to mild may exert a weaker influence on child development than cases where the shift is from severe to moderate depression.
The analysis is conducted in two steps: Firstly, we employ maximum likelihood to estimate the factor model and extract the predicted factor scores, as described in detail in Appendix Section D.1. The factor scores are then used to assess the causal impact of the intervention on maternal mental health and child outcomes at each time point. The results of this reduced-form analysis are discussed in Section 4.
In the second step, we estimate the parameters of equation (1), aggregating the reduced-form results of the first step in two systems of equations—one at age 12 and the other at age 36 months. Since we lack instrumental variables that might induce quasi-exogenous variation in the inputs of the production function, this analysis is descriptive. Yet, this synthesis helps us explore the reasons why intervention effects on maternal mental health did not spillover to child development. The results of the production function estimates are presented in section 5.
4. Treatment effects
We evaluate the impact of the perinatal psychosocial intervention on maternal mental health, daily functioning, and child skills during the first three years of life leveraging the cluster-randomized nature of the intervention and using ordinary least squares. We estimate intention-to-treat (ITT) effects on the latent factor scores for the domains of maternal mental health, maternal functioning, child cognition, physical, and socioemotional skills, and parental investment (Table 2 and Figure 2). Table 2 reports the estimated ITT on the latent factors normalized to mean zero and standard deviation 1 for the control group at the initial time point (6 months) only, to understand the evolution of the latent factors over time, while Figure 2 and Appendix Table A22 report ITT on latent factors that are normalized to mean 0 and standard deviation 1 at each time point, to allow for comparison of effect sizes in standard deviation units. For completeness, we also report ITT effects on each individual measure in Appendix Tables A18–A21.
Table 2:
Trajectory of Summary Indices
| Measurement | Control | Treatment | Nondep. | Adjusted Beta | s.e. | p-val | N | |
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | Mean | |||||
| Maternal Factor Scores | ||||||||
| Mental Health (6 months) | 0 | 1 | 0.160 | 0.648 | 0.205 | 0.052 | 0.000 | 929 |
| Mental Health (12 months) | −0.002 | 0.703 | 0.067 | 0.455 | 0.119 | 0.038 | 0.002 | 940 |
| Mental Health (36 months) | −0.023 | 0.760 | 0.078 | 0.399 | 0.204 | 0.059 | 0.001 | 889 |
| Functioning (6 months) | 0 | 1 | 0.108 | 0.547 | 0.182 | 0.075 | 0.015 | 929 |
| Functioning (12 months) | 0.013 | 0.781 | 0.138 | 0.382 | 0.152 | 0.054 | 0.005 | 940 |
| Functioning (36 months) | 0.043 | 0.856 | 0.139 | 0.365 | 0.246 | 0.069 | 0.000 | 889 |
| Child Factor Scores | ||||||||
| Physical Health (6 months) | 0 | 1 | −0.016 | −0.034 | −0.021 | 0.079 | 0.792 | 929 |
| Physical Health (12 months) | −0.039 | 0.799 | −0.003 | −0.011 | 0.015 | 0.056 | 0.784 | 940 |
| Physical Health (36 months) | −0.026 | 0.806 | −0.136 | 0.007 | −0.134 | 0.071 | 0.060 | 889 |
| SE Skills (6 months) | 0 | 1 | 0.167 | 0.100 | 0.187 | 0.056 | 0.001 | 940 |
| SE Skills (12 months) | −0.183 | 0.842 | 0.168 | 0.082 | 0.328 | 0.059 | 0.000 | 940 |
| SE Skills (36 months) | 0.864 | 0.907 | 0.917 | 0.966 | 0.057 | 0.068 | 0.400 | 889 |
| Cognition (12 months) | 0 | 1 | −0.059 | 0.069 | −0.080 | 0.083 | 0.334 | 940 |
| Cognition (36 months) | 0.041 | 0.426 | 0.061 | 0.033 | 0.028 | 0.031 | 0.386 | 889 |
| Investment Factor Scores | ||||||||
| Investment (12 months) | 0 | 1 | 0.062 | 0.448 | 0.075 | 0.086 | 0.382 | 940 |
| Investment (36 months) | −0.002 | 0.643 | 0.041 | 0.230 | 0.072 | 0.049 | 0.143 | 889 |
SE skills = socioemotional skills. The first two columns report the mean and standard deviation of the outcome variables in the control group. The following columns report the means for the treatment group and the group of mothers who were non-depressed at baseline (Nondep.). Adjusted Beta coefficients are obtained from the regressions of items on the treatment indicator and its interactions with the (demeaned) baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset-based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. All estimations control for child gender and age (in days). Standard errors clustered at the village-cluster level are reported in the s.e. column. Reported p-values and standard errors refer to the adjusted beta coefficient. N reports the number of observations of each analysis. Factor scores are coded so that a higher score always indicates a better outcome.
Figure 2:
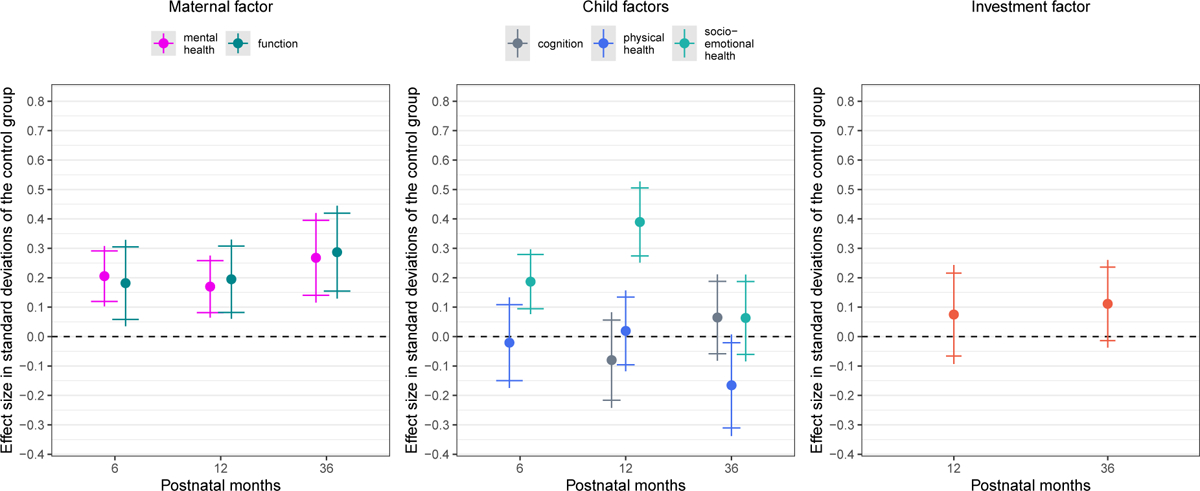
Coefficient Plots of Factors
Notes: Plot of the adjusted beta coefficients reported in Table A22 and their 90% and 95% confidence intervals. Latent factors are normalized to mean 0 and standard deviation 1 in the control group at each time point, to allow comparability of effect sizes in standard deviations. Coefficients are obtained from the regressions of items on the treatment indicator and its interactions with the (demeaned) baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset-based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. All estimations control for child gender and age (in days). Standard errors clustered at the village-cluster level. Factor scores are coded so that a higher score always indicates a better outcome and standardized to have mean 0 and SD 1 in the control group at each time point.
As our baseline and follow-up samples were not completely balanced along baseline characteristics, the regressions control not only for child age in days, interviewer fixed effects, and union council fixed effects (stratification unit), but also for the full set of baseline characteristics (demeaned) and their interactions with the treatment indicator (adjusted ).15 Note that we can only identify the overall causal effect of the THPP+ intervention and not the causal effect of recovering from depression or of any individual component of the intervention, such as behavioral activation or group-based aspects of the treatment. Including interactions with treatment allows us to control for possible heterogeneity in the impacts of baseline characteristics on outcomes. Reported standard errors are clustered at the village cluster level (i.e., the randomization unit). We also compute p-values using randomization inference based on Young (2019) with the randomization permuted at the cluster level. We observe minimal changes in the p-values due to the randomization inference, as shown in Appendix Tables A27–A28.
We additionally present results of the intervention on the distribution of outcomes. Figure A6 presents the estimated densities of the latent factors for the control and treatment clusters. To compare the CDFs of the two groups, we perform a Kolmogorov-Smirnov test with bootstrap.16 Quantile treatment effects are reported in Appendix Figure A7.
4.1. Maternal mental health and functioning
The intervention is effective in improving the mother’s condition at 6, 12, and 36 months post-partum. The upper panel of Table 2 and the first panel of Figure 2 present the adjusted beta coefficient plots of latent factor scores. Improvements range between 0.17 and 0.27 standard deviations in maternal mental health, and between 0.18 and 0.29 SD in maternal functioning, with the largest effect sizes observed at 36 months.
Plots of the outcome distributions show a rightward shift in the latent factor score for maternal mental health throughout the trial period. These effects are bigger in the lower half of the distribution, although this difference in quantile treatment effects is not always statistically significant.
Treatment effects on individual maternal outcomes are reported in Appendix Table A18. Treated women experienced a significant reduction in depression scores (PHQ-9) at 6 and 36 months postpartum relative to women in the control clusters (p-values 0.014 and 0.001, respectively). Splitting the PHQ score into different categories, the greatest reduction is concentrated in the moderate-severity category (15 ≤ PHQ-score ≤ 19), with an increase in the women in the minimal category (PHQ-score ≤ 4). Treated women were less likely to have a major depression episode at 6, 12, and 36 months, with a reduction of likelihood ranging between 7 and 12 percentage points (p-values 0.011, 0.011, and 0.001, respectively). Their stress score is significantly lower, and their daily functioning significantly better than in the control group. Overall, we observe positive and significant treatment effects across multiple indicators of maternal depression, stress, and functioning in the three waves analyzed.
4.2. Parental investment and behaviour
The adjusted beta coefficients related to the parental investment factor score are all positive (0.08–0.11 SD), but not statistically different from zero. These treatment effects, even if they were to be more precisely estimated, would suggest only modest improvements when compared to other global studies focusing on at-risk parents (Rayce et al., 2017; Jeong et al., 2021).
Analyzing the different measures of parental investment in Appendix Table A21, we find the intervention improved most subscales of the HOME inventory indicating maternal responsivity, avoidance of restrictions and punishment, organization of the child’s environment, and provision of appropriate learning materials at 12 months postpartum. At 36 months, the intervention had positive effects on the total HOME score, acceptance, and learning materials, albeit imprecisely estimated, but only small positive and sometimes negative effects on other subscales.
4.3. Child outcomes
The estimated treatment effects on child outcomes are generally noisier than on mothers. The intervention seems to have no clear effect on cognition—with estimated ITT coefficients smaller than 10% of a standard deviation and hovering around zero, or on physical health, which displays both slightly positive and mildly negative adjusted beta coefficients. Notably, the intervention has a sizeable, albeit transitory effect on socioemotional skills: the estimated ITT at 6 and 12 months are 0.19 and 0.39 SD respectively, indicating considerable improvements. However, these treatment-control differences fade out by the 36-month mark, when the estimated ITT effect is only 0.06 and it is neither economically meaningful nor statistically different from zero.
The transitory effect might have persistent consequences, even if it does not itself persist. For instance, socio-emotional skills in infancy might fuel self-regulation, interaction, and curiosity (and possibly other domains that are hard to measure, especially at an early age) which in turn might improve school achievement and later life outcomes. In line with this, in the next section, we report small but positive estimates of cross-skill productivity between socioemotional ability and cognition up until age 3.
Looking at the individual indices in Appendix Tables A19–A20, we observe significant improvements only in certain socioemotional and cognitive domains. The total ASQ-SE score is generally lower (indicating better socioemotional skills) in the treatment group. Looking at the sub-components of ASQ-SE shows that, at 12 months, the improved ASQ-SE in the treatment group is driven by significant improvements in self-regulation (measuring the child’s ability to regulate her emotions and adjust to new environments). These effects are mainly driven by male children. At 36 months, the intervention impacts are once again on self-regulation and now, also, on autonomy.
In terms of cognitive outcomes, the estimated treatment effect on the Bayley receptive domain score (one of the two components of Bayley-III) is significantly positive at 36 months, with a score increase of 0.39 (p-value 0.06) in the treatment group, which brings the mean scores of the treatment group close to the scores of the non-depressed group. However, treatment effects on the aggregate cognition index and factor score are small (0.09 and 0.07 SD, respectively) and imprecisely estimated.
Looking at the distribution of outcomes, there is a shift to the right in the distribution of children’s socioemotional skills in the treatment group in the first 12 months of the trial. However, at 36 months, the two densities overlap again suggesting a short-term effect. Quantile treatment effect analysis yields larger effects in the lower half of the distribution in the first two years, which become insignificant at 36 months postpartum (Appendix Figure A7).
The distribution of the child cognition factor shows a scale shift at 12 months and a small location shift at 36 months postpartum. For children’s physical health, the densities for the control and treatment groups overlap and the Kolmogorov-Smirnov test cannot reject that they are equal. Quantile treatment effects are also not generally different from zero in any part of these distributions.
4.4. Heterogeneity
Exploring treatment effect heterogeneity on maternal outcomes by gender of the index child reveals that the estimated benefits are larger for the mothers of boys (Figures 3–4 and appendix tables A29–A31). As discussed earlier, intervention effects on investment and child skills also show a tendency to be stronger for boys. There is well-documented son preference in South Asia, and some evidence that women who have sons are treated better by the family than women who have daughters (Sathar et al., 2015; Milazzo, 2018; Bhalotra et al., 2020). It seems plausible that women who are in a generally more supportive environment are more responsive to treatment, and this would explain our finding. However, we can imagine the reverse, i.e., that treatment effects are larger where the environment is harsher. Indeed, in Baranov et al. (2020) we found that a similar intervention (THP) run on a different sample of new mothers in rural Pakistan was more effective for mothers of girls in a 7-year follow-up. The length of the follow-up aside, the intervention analyzed in this study (THPP+) differs in duration and in intervention modality (see Section 1 for details), making it hard to compare the findings. THPP+ was peer-delivered, while THP was delivered by trained community health workers. One possible explanation is that peers (other mothers in the community) might implicitly reinforce gender norms, whereas community health workers might act to empower mothers of girls. We have no hard evidence of this potential channel, but it is a relevant consideration to highlight when considering task-shifting to peers in an attempt to scale up interventions.
Figure 3:
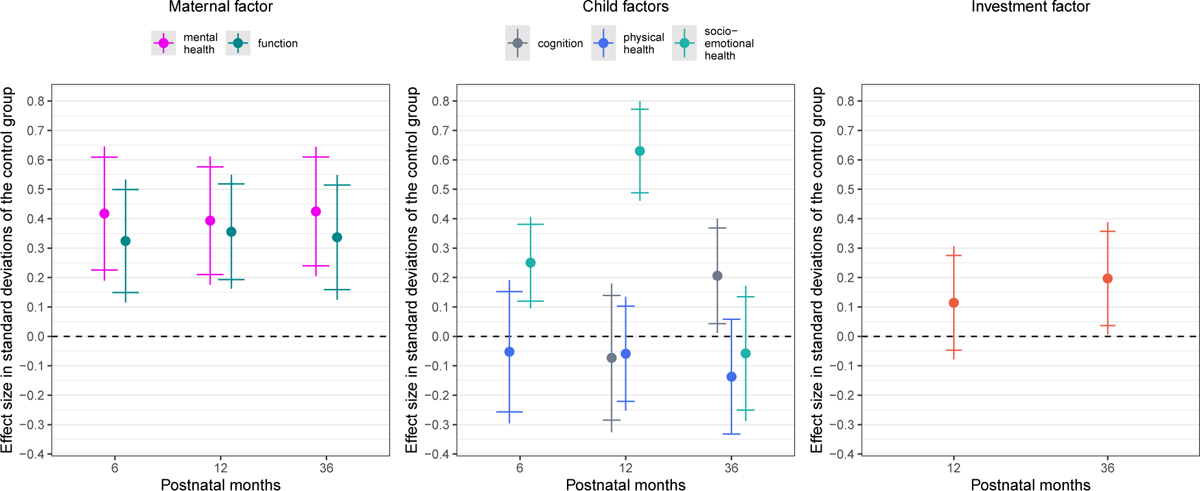
Coefficient Plots of Factors (Boys)
Notes: Plot of the 90% and 95% confidence intervals and the adjusted beta coefficients obtained from the regressions, using only the sample of families where the index child is a boy, of items on the treatment indicator and its interactions with the (demeaned) baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset-based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. All estimations control for age (in days). Standard errors clustered at the village-cluster level. Factor scores are coded so that a higher score always indicates a better outcome and standardized to have mean 0 and SD 1 in the control group at each time point.
Figure 4:
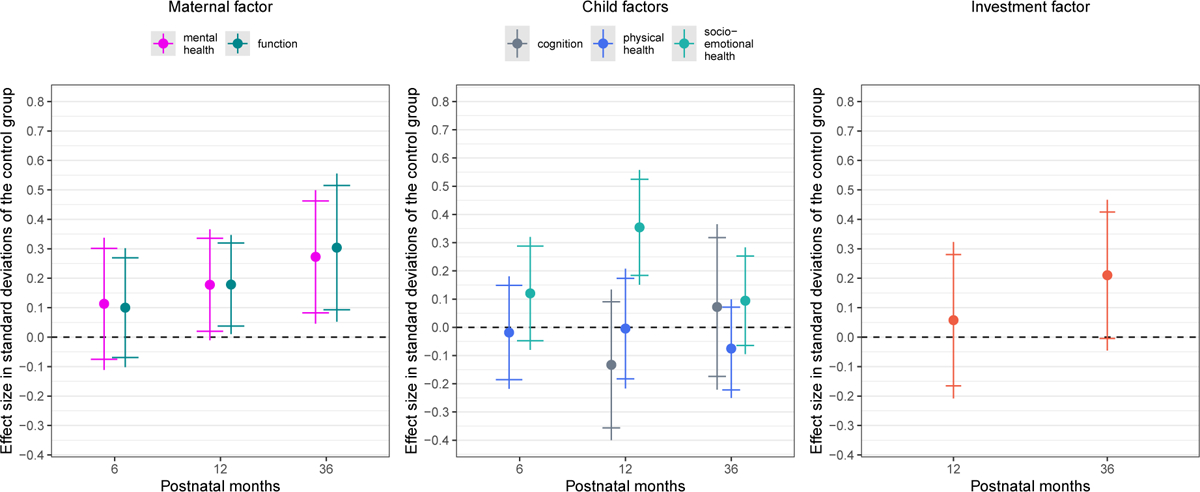
Coefficient Plots of Factors (Girls)
Notes: Plot of the 90% and 95% confidence intervals and the adjusted beta coefficients obtained from the regressions, using only the sample of families where the index child is a girl, of items on the treatment indicator and its interactions with the (demeaned) baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset-based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. All estimations control for age (in days). Standard errors clustered at the village-cluster level. Factor scores are coded so that a higher score always indicates a better outcome and standardized to have mean 0 and SD 1 in the control group at each time point.
We investigated heterogeneity by birth-order of the index child, an asset-based index of socioeconomic status of the family, education of the mother, and baseline depression severity (PHQ-9 total score). We find no systematic patterns here.
4.5. Discussion
The group-based, peer-delivered psychosocial intervention was effective at achieving one of its targets, which was improving maternal mental health and daily functioning. These improvements in well-being are complemented by smaller and imprecisely estimated increases in parenting behavior of 8 to 11% of a standard deviation, and by a sizeable but transitory change in children’s socioemotional development. This improvement in child skills at 12 months appears to be a direct effect of the intervention, which included training and support for child development.
Our results do not appear to be driven by attrition. Attrition-adjusted estimates using inverse probability weighting (IPW) and Lee Bounds (Lee, 2009) are shown in Appendix Table A6, with gender-specific results in Appendix Table A7. Our results are robust to the IPW correction, which only marginally changes the estimated coefficients and their precision. The attrition-corrected Lee bounds are wide, but in the sample of mothers of boys (in which baseline characteristics are more balanced) show positive and significant effects on maternal mental health and on child socioemotional skills both at 6 and 12 months.
To provide a benchmark for the effectiveness of the intervention and to put the magnitude of the treatment effects in perspective, we compare the adjusted beta coefficients with the mean level of the summary indices for the mothers who were not depressed at baseline. Since the mean summary index for the control group is standardized to be zero, the average outcome for the nondepressed mothers represents the association between prenatal depression and outcomes. We call this descriptive statistic the “depression gap” and display this in Appendix Table A33, Columns 5–7.
The intervention acted to narrow depression gaps, tending to bring the medium-term outcomes of perinatally depressed women closer to the outcomes of women who were in the same pregnancy cohort but not depressed at baseline. This is the case for child socioemotional skills and parental investment.17 The depression gap in child health and cognitive skills is often small and imprecisely estimated. As such, there was limited leeway for the intervention to improve these domains.
The results in this paper build upon our findings in Maselko et al. (2020). We extend that analysis in the following ways. We investigate dynamics, exploring multiple indicators and their evolution throughout the study period. As child development is not a linear process, a more granular approach is of substantive importance. At each age, we estimate treatment effects by gender of the child and on the distribution of outcomes rather than only at the mean. We provide treatment effects on a broader set of outcomes (including, for instance, the ASQ-SE for socioemotional development). We use aggregate summary indices and factor scores to provide summary measures of maternal well-being and child development and to improve statistical power. We also adopt a less restrictive statistical specification.18 A final and key differentiation is that we now impose some structure on the dynamic evolution of children’s skills, accounting for the trajectory of maternal mental health, functioning, and parenting, and estimate the production function for skills at age 12 and 36 months. We discuss this next.
5. The Technology of Skill Formation
The results above indicate that the intervention improved maternal mental health, but these enhancements did not consistently transfer into lasting improvements in child skills. This discrepancy is at odds with some of the descriptive literature comparing the socioemotional outcomes of children of depressed and non-depressed mothers (Herba et al., 2016; Leung and Kaplan, 2009; Gaynes et al., 2005), but consistent with other literature that finds that moderate levels of maternal depression are not systematically associated with impaired child development (Laplante et al., 2008; DiPietro et al., 2006). To reconcile the suite of reduced form findings and understand the mechanisms by which the intervention might have influenced the outcomes, we impose the simplifying structure discussed in Section 3 on the dynamic evolution of the child’s latent human capital.
We contribute to the literature on mental health and child development in two related ways. First, we include in the model two dynamic latent factors measuring maternal mental health and functioning . Their measurement is consistent over time and uses state-of-the-art measurements for the screening and assessment of three relevant dimensions of maternal mental health—depression, stress, and daily functioning. We estimate their contribution to the production function of the child’s cognitive, socioemotional, and physical health. Earlier related studies at best include a time-invariant measure of maternal characteristics such as cognitive skills, physical health, or noncognitive skills (Cunha and Heckman, 2008; Cunha et al., 2010; Attanasio et al., 2022b). To distinguish maternal mental health from parental investments, we conceptualize it as capital in the production function, similar in principle to the conceptualization of physical health as capital (Grossman, 1972).
Second, this study is the first to estimate how a psychosocial intervention targeting the mother might influence the production function of children’s skills, allowing some parameters of the production function to vary with the intervention. Similar to a Kitagawa-Oaxaca-Blinder decomposition (Kitagawa, 1955; Oaxaca, 1973; Blinder, 1973), we allow the intervention to act through two potential mechanisms: a change in the level of parental inputs; and a change in the productivity of these inputs, i.e. the slope of the production function.
These two channels are embedded into our specification of the dynamic model of skill formation. For ease of interpretation and estimation, we assume that the production functions for child socioemotional skills, physical health, cognition, parental investment, and maternal mental health described in equation (1) are log-linear (Cobb Douglas).19
| (2) |
| (3) |
| (4) |
where , and stand for physical health, socioemotional skills, and cognition of the child, respectively. Eq. (2) reflects that children’s health and cognition in period are functions of the previous period stock of skills and health , investments made by parents up to that point , parental education, as well as maternal mental health and functioning denotes the same baseline covariates used in the treatment effect estimation in Section 4, notably the mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of children (split by gender), whether the index child is the first child, asset-based SES index and child gender.20 stands for total factor productivity (TFP) and represents unobserved shocks to child development. Eq.(3) and (4) model the evolution of the main inputs: the stock of maternal mental health and the flow of parental investment. The same control variables are included as in Eq.(2).
We estimate the production and investment functions in equations (2)–(4) in two stages: at 12 months and at 36 months. To do so, we use the factor scores resulting from the measurement system discussed above and in Appendix Section D.1. We exclude lagged cognition in the estimations for 12 months, as we did not measure cognition at 6 months.
While all of the distributions of latent factors are allowed to be different across treatment, control, and baseline non-depressed mothers—capturing potential changes in the level of inputs—we only allow the coefficients of and to vary with treatment status —capturing potential changes in slope and therefore productivity. We do this by including an indicator for the treatment group (treat) and an indicator for the group of mothers who were non-depressed at baseline (nondep) and interacting them with parental investment and maternal mental health (the two main inputs of interest). This simplifying assumption focuses the estimation on the two main channels that were targeted by the intervention: maternal mental health and investments. It allows us to study how the productivity of maternal mental health and investments changes as a function of the intervention.
Theoretically, we may observe the productivity of mental health increase or decrease as a result of the intervention. On the one hand, if the true relationship between the input (lagged maternal mental health) and the output (child skill development) is subject to diminishing returns, then an improvement in maternal mental health due to the intervention could move the treatment group further up and to the right along the curve, where the slope is flatter (see this notional curve in Figure 5a). The estimated relationship between the input and output in the control group would then exhibit a lower constant and a steeper slope than the treatment group. This would manifest as a positive parameter on the interaction between TFP and treatment (TFP × treat) and a negative interaction between maternal mental health and treatment (motherMH × treat). Plotting the observed non-parametric relationship between maternal mental health at 6 months, , and child skills at 12 months, , using the control group data does in fact indicate a nonlinear, concave relationship (Figure 5b), similar to Figure 5a and in line with the descriptive findings of Laplante et al. (2008); DiPietro et al. (2006).21
Figure 5:
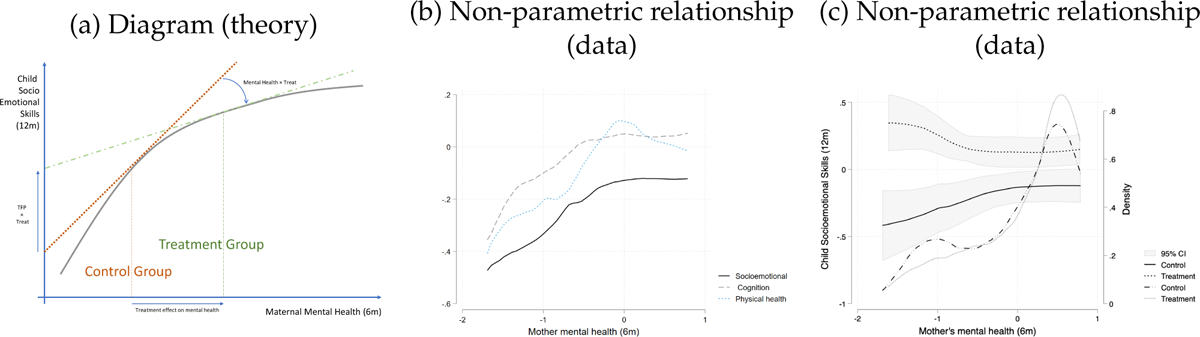
Relationship between maternal mental health (6m) and child skills (12m)
Notes: (a) Theoretical representation of a concave relationship between maternal mental health (input) and children skills (output), and the consequence of log-linearization at different average levels of the input. (b) Kernel-weighted local polynomial smoothing of the relationship in the control group between maternal mental health at 6 months and: child socioemotional skill factor (solid dark line), child cognition factor (dashed grey line), and child physical health factor (dotted blue line) at 12 months. (c) Left-y-axis: Kernel-weighted local polynomial smoothing and 95% confidence interval of the relationship between maternal mental health at 6 months and child socioemotional skill factor at 12 months in the control group (solid dark line) and the treatment group (dotted blue line). Right-y-axis: kernel density estimation of the distribution of maternal mental health at 6 months in the control group (dash-dotted dark line) and the treatment group (dotted gray line).
Alternatively, the intervention could change the shape and the location of the production function: for example, intervention components not specifically targeting maternal mental health (e.g. improving mother-child bonding, seeking social support) may change the relative productivity of mental health, parental investments, or both. These non-mental health components of the intervention might reinforce and complement the intervention-lead effects on maternal mental health, for example allowing mothers who have recovered from depression to engage in more fruitful parental interaction with the children. This would lead to a positive coefficient on the interaction between maternal mental health and treatment (motherMH × treat). But the non-mental health component of the intervention could also act as a substitute, shielding children from maternal depression and improving particularly the outcomes of children whose mothers did not recover from depression even after therapy. This would lead to a negative coefficient for motherMH × treat. Plotting the observed non-parametric relationship between maternal mental health at 6 months, , and child socioemotional skills at 12 months, separately for treated and control group indicates a potential substitution effect, with greater intervention effects for children whose mothers did not recover from depression (Figure 5c).
We now turn to the discussion of the empirical estimates of equations 2–4. It is important to remember that we have one instrument (the intervention) and multiple endogenous inputs, for which it is difficult to find a plausible source of exogenous variation. The results of this analysis should therefore be considered as descriptive, similar to the existing literature estimating child skill production functions (see, for instance, the summary of the literature in Table 1 of Attanasio et al., 2022b).
5.1. Estimates of the Technology
Tables 3–4 report estimates for the outcomes at 12 months and 36 months respectively. The estimates reveal that children’s skills and maternal mental health are persistent over time, indicating ‘self-productivity’ in skills. Socioemotional skills, physical health, and maternal mental health exhibit persistence through from 6 to 36 months, while cognitive skills are only clearly persistent from 6 to 12 months. For cognitive and socioemotional skills, self-productivity is larger earlier in childhood. Consistent with estimates of skill formation in other settings (Attanasio et al., 2022b; Bufferd et al., 2012), skills are less predictive across domains—the ‘cross-productivity’ of skills is at least a degree of magnitude smaller than self-productivity, often non-statistically different from zero, except for the predictive power of physical health on cognitive skill development at both 12 and 36 months. Evidence on self- and cross-productivity of skills across domains at very early ages, 0–3, is relatively scarce, therefore providing an important contribution to the literature.
Table 3:
Estimates of the Production Function and Input Equations I
| Socioemotional skills (12m) (1) |
Physical health (12m) (2) |
Cognition (12m) (3) |
Parental investment (12m) (4) |
Maternal mental health (12m) (5) |
|
|---|---|---|---|---|---|
| SE skills (6m) | 0.450*** (0.042) |
0.004 (0.014) |
0.065* (0.035) |
0.034 (0.024) |
0.031 (0.024) |
| physical health (6m) | 0.070 (0.044) |
0.928*** (0.014) |
0.109*** (0.042) |
0.077*** (0.024) |
0.006 (0.022) |
| mother mental health (6m) | 0.117* (0.062) |
0.083*** (0.029) |
0.131* (0.076) |
−0.104 (0.069) |
0.384*** (0.067) |
| mother functioning (6m) | −0.033 (0.053) |
−0.044** (0.020) |
−0.025 (0.045) |
0.081** (0.040) |
0.093** (0.042) |
| investment (12m) | 0.086 (0.082) |
0.030 (0.022) |
−0.016 (0.060) |
0.162** (0.053) |
|
| Interactions | |||||
| mother MH (6m) × treat | −0.199*** (0.076) |
−0.061 (0.038) |
−0.199** (0.096) |
0.101 (0.085) |
−0.022 (0.073) |
| mother MH (6m) × nondep. | −0.052 (0.094) |
−0.133*** (0.034) |
−0.066 (0.094) |
0.106 (0.080) |
−0.155* (0.084) |
| investment (12m) × treat | −0.022 (0.108) |
−0.030 (0.035) |
0.346*** (0.090) |
−0.007 (0.067) |
|
| investment (12m) × nondep. | −0.033 (0.082) |
−0.026 (0.030) |
0.206*** (0.073) |
−0.072 (0.063) |
|
| Total factor productivity (TFP) | |||||
| TFP | −0.567 (0.887) |
−0.465 (0.346) |
4.208*** (0.919) |
0.101 (0.799) |
−0.453 (0.664) |
| TFP × treat | 0.257*** (0.061) |
0.033* (0.020) |
−0.023 (0.058) |
0.065 (0.060) |
0.043 (0.049) |
| TFP × nondep. | 0.243** (0.100) |
0.118*** (0.038) |
−0.069 (0.089) |
0.022 (0.094) |
−0.001 (0.084) |
| Baseline controls | |||||
| SES assets | −0.016 (0.020) |
0.004 (0.007) |
0.009 (0.024) |
0.087*** (0.016) |
−0.019 (0.015) |
| mother’s education (years) | −0.003 (0.006) |
0.005 (0.003) |
−0.004 (0.007) |
0.019*** (0.004) |
0.011** (0.005) |
| husband’s education (years) | 0.001 (0.007) |
−0.006** (0.003) |
−0.002 (0.006) |
0.016** (0.007) |
0.001 (0.006) |
| Observations | 932 | 932 | 927 | 932 | 932 |
| R2 | 0.430 | 0.881 | 0.258 | 0.384 | 0.429 |
| Adjusted R2 | 0.387 | 0.873 | 0.202 | 0.340 | 0.387 |
SE= socioemotional skills, MH=mental health. Dependent variables are child outcomes and parental investment and maternal mental health factors at 12 months postpartum. Independent variables include an indicator of treatment status (control, treatment, nondepressed), child and maternal factors at 6 months (except for cognition as we did not measure cognition at 6 months), parental investment factor at 12 months. Maternal mental health and parental investment are interacted with the treatment status. All estimations control for baseline characteristics including, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect, days from baseline and child age in days. Robust and clustered standard errors at the cluster level are reported in paranthesis.
Note:
p<0.1;
p<0.05;
p<0.01
Table 4:
Estimates of the Production Function and Input Equations II
| Socioemotional skills (36m) (1) |
Physical health (36m) (2) |
Cognition (36m) (3) |
Parental investment (36m) (4) |
Maternal mental health (36m) (5) |
|
|---|---|---|---|---|---|
| SE skills (12m) | 0.183*** (0.037) |
0.033* (0.020) |
0.012 (0.023) |
−0.075** (0.031) |
0.024 (0.032) |
| physical health (12m) | 0.026 (0.042) |
1.048*** (0.026) |
0.046** (0.023) |
0.067** (0.029) |
−0.023 (0.038) |
| cognition (12m) | 0.012 (0.038) |
−0.017 (0.022) |
0.059*** (0.022) |
0.029 (0.033) |
−0.057** (0.027) |
| mother mental health (12m) | 0.083 (0.097) |
0.045 (0.050) |
−0.074 (0.059) |
0.202*** (0.075) |
0.287*** (0.067) |
| mother functioning (12m) | −0.063 (0.049) |
−0.049* (0.028) |
0.065** (0.033) |
−0.010 (0.049) |
0.094* (0.054) |
| investment (36m) | 0.158** (0.071) |
0.001 (0.039) |
0.092** (0.039) |
0.150* (0.077) |
|
| Interactions | |||||
| mother MH (12m) × treat | 0.057 (0.118) |
−0.055 (0.056) |
0.060 (0.066) |
−0.152* (0.084) |
−0.028 (0.096) |
| mother MH (12m) × nondep. | −0.001 (0.112) |
0.003 (0.046) |
−0.005 (0.068) |
−0.074 (0.086) |
−0.100 (0.093) |
| investment (36m) × treat | −0.214* (0.112) |
0.034 (0.053) |
−0.086 (0.059) |
−0.117 (0.080) |
|
| investment (36m) × nondep. | 0.017 (0.101) |
−0.048 (0.045) |
−0.008 (0.051) |
−0.158** (0.071) |
|
| Total factor productivity (TFP) | |||||
| TFP | 0.564 (2.503) |
−1.546** (0.702) |
1.960** (0.949) |
1.918 (1.380) |
1.344 (1.332) |
| TFP × treat | −0.031 (0.079) |
−0.160*** (0.043) |
0.022 (0.036) |
0.133** (0.059) |
0.113 (0.071) |
| TFP × nondep. | −0.164 (0.123) |
0.039 (0.060) |
−0.046 (0.072) |
0.120 (0.093) |
−0.035 (0.104) |
| Baseline controls | |||||
| SES assets | −0.014 (0.015) |
−0.004 (0.012) |
−0.001 (0.011) |
0.053*** (0.019) |
−0.004 (0.018) |
| mother’s education (years) | −0.006 (0.006) |
0.006 (0.004) |
0.013*** (0.004) |
0.016*** (0.005) |
0.010* (0.005) |
| husband’s education (years) | 0.009 (0.007) |
−0.003 (0.004) |
0.008 (0.006) |
0.031*** (0.008) |
0.012* (0.012) |
| Observations | 881 | 881 | 881 | 881 | 881 |
| R2 | 0.404 | 0.839 | 0.302 | 0.311 | 0.331 |
| Adjusted R2 | 0.363 | 0.827 | 0.253 | 0.266 | 0.285 |
SE= socioemotional skills, MH=mental health. Dependent variables are child outcomes and parental investment and maternal mental health factors at 36 months postpartum. Independent variables include an indicator of treatment status (control, treatment, nondepressed), child and maternal factors at 12 months, parental investment factor at 36 months. Maternal mental health and parental investment are interacted with the treatment status. All estimations control for baseline characteristics including mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect, days from baseline and child age in days. Robust and clustered standard errors at the cluster level are reported in paranthesis.
Note:
p<0.1;
p<0.05;
p<0.01
We now discuss the role of maternal mental health and parental investment across the three groups of women (control, treatment, and baseline non-depressed), initially for outcomes at 12 months of age, Table 3, and then for outcomes at 36 months, Table 4. First consider column 1 of Table 3 for child socioemotional (SE) skills, as this is where we find intervention effects at 12 months (see Figure 2). In the control group of women who were depressed in pregnancy but received no intervention (top panel), maternal mental health at 6 months is a significant predictor of socioemotional skills at 12 months, consistent with Figure 5b.22 Parental investment at 12 months is positive but imprecisely determined.
The intervention modifies the shape of the production function in two significant dimensions (second panel, interactions). We see a positive coefficient on the interaction of TFP with treat and a negative coefficient on the interaction of maternal mental health with treat. A higher TFP in the treatment group indicated that the intercept and the whole production function have shifted up: the outcome is higher for each level of input. The negative interaction with maternal mental health tells us that the slope of the curve describing how the outcome varies with maternal MH is flatter in the treated group than in the control group. This is consistent with decreasing returns to improvements in mental health (Figure 5b) as well as a larger effect of the intervention on the socioemotional skills of children whose mothers did not recover from depression (Figure 5c).
Both the positive TFP shift and the shallowing of the slope of the relationship with maternal MH that we see in the treated group are also evident in the group of mothers who were non-depressed at baseline. Thus, in line with expectations, the intervention moved the outcomes of children and mothers with prenatal depression closer to the outcomes of children and mothers who were not depressed during pregnancy. Put differently, the intervention bridges the “depression gap” in the production function, morphing the technology of skill formation for depressed mothers to look more like that for women who did not suffer depression during pregnancy.
We now summarize the main results for other outcomes at 12 months of age, in columns 2–5 of Table 3. In the control group, maternal mental health at 6 months is predictive not only of socioemotional skills but also of cognitive skills and physical health: it is significantly associated with child development across domains. Maternal functioning at 6 months has no direct relationship with child development above and beyond other inputs, such as maternal mental health and parental investments, but it raises parental investment. Parental investments at this early age are not predictive of any domain of child development, but they are related to maternal mental health. It is also no-table that parental education and assets have a significant positive impact on parental investments but, conditional on investment, have no direct impact on child outcomes.
Intervention effects are reported in the second and third panels of Table 3. The intervention raises TFP in the production of physical (but not cognitive) development. It attenuates the relationship between maternal MH and cognition, and it strengthens the return to investments when the outcome is cognition. Once again, the direction of effects in the intervention arm is the same as the direction of effects among the group of mothers not depressed in pregnancy.
Now consider estimates for the production function for child skills at 36 months (Table 4). The estimates for the control group show that maternal mental health at 12 months has only small and statistically insignificant associations with child skills at 36 months, but is predictive of higher parental investments. In turn, parental investment at 36 months predicts higher socioemotional and cognitive skills at 36 months, conditional on maternal MH. Intervention effects at 36 months are also most evident for the investment outcome. The pattern is similar to that observed for skills outcomes at 12 months: TFP is higher, and there is an attenuation of the relationship between maternal MH and parental investment. The only significant intervention effect in the production functions for child skills indicates lower TFP in the production of the physical health of the child, for which we have no clear explanation.
Mirroring our reduced form analysis of treatment effects and following recent trends in the literature focusing on socioemotional skills and mental health (Moroni et al., 2019), we split the sample by gender and estimate the technology of skill formation separately for boys and girls. Appendix Tables A36–A37 suggest that the overall pattern of production function results is similar across child genders. If anything, maternal mental health seems to be more predictive of parenting for mothers of girls, although statistical power is limited for this comparison.
5.2. Discussion
Taking stock, the intervention changes both the level of the inputs and their associations with the outcomes (returns). First, it improves maternal mental health (at 6, 12, and 36 months). This is an input to the production function, being directly associated with an improvement in child skills at 12 months while, at 36 months, it is associated with improved child skills through increasing parental investment. Second, the intervention changes the shape of the production function, changing both its intercept (TFP) and its slope (the productivity of specific inputs—maternal health at 12 months, and parental investment at 36 months).
These results are well summarized by Figure 5c, plotting the distribution of maternal mental health at 6m in the treatment and control group, and their non-parametric relationship with child socioemotional skills at 12m. The intervention improves the whole distribution of maternal mental health, bringing more mothers into a flatter part of the production function, as modeled in Figure 5a. It seems plausible that, in the sample of women who have largely recovered from depression, marginal improvements in mental health have smaller impacts. Consistent with this, the productivity of maternal mental health is weaker in both the intervention group and the non-depressed group relative to the control group.
At the same time, our results are not consistent with a simple shift along a single production technology curve: treatment induced an upward shift of the whole curve, with an overall improvement in productivity (a positive TFP × treat coefficient). The upward shift is largely driven by mothers at the low end of the mental health distribution (who did not respond to the intervention), and this induces a greater flattening of the curve (a negative motherMH × treat coefficient). The evidence here indicates that the intervention had a direct impact on the improvement in socioemotional skills of children at 12 months.
6. Conclusion
We estimate the impacts of a peer-led psychosocial intervention delivered to women diagnosed as depressed in pregnancy, starting in the third trimester of pregnancy and continuing till the child was 36 months of age. Our findings reveal that the intervention resulted in significant and lasting improvements in maternal mental health and functioning. There was also a moderate increase in parental investment, although the estimate is not precisely estimated. However, despite these positive changes, we did not observe any noticeable improvements in overall indicators of child development in the long term.
To understand the associations of the multiple endogenous variables and the dynamics more clearly, we estimated a production function for child skills. Among women diagnosed as depressed in pregnancy but untreated (the control group), mental health is strongly related to child outcomes in early childhood and to investments in children in later childhood. These relations are economically significant: for example, they tend to be larger in magnitude than the associations between socio-economic status and child skill development.
This suggests that an intervention targeting maternal mental health and parenting behaviors might improve children’s future skills. However, this does not seem to be the case. The potential reason for this is that the intervention mutes the relationship between maternal mental health and children’s outcomes. Just as in the sample of non-depressed mothers, the rate of return of mental health in the production function is close to zero for the treatment group. Therefore, any potential impact of the increase in mental health induced by the intervention is offset by a reduction in its efficiency in producing children’s skills.
Overall, both the reduced form and the production function estimates suggest that the intervention is effective and tends to move outcomes for perinatally depressed mothers towards outcomes for those who were not depressed during pregnancy.
Acknowledgments:
Atif Rahman and Siham Sikander designed the intervention. We are grateful to Siham Sikander and his colleagues at the Human Development Research Foundation in Pakistan for implementing the trial and the follow-up, and at the Bachpan Study Team for interdisciplinary guidance and support. For their comments and suggestions, we thank Anna Aizer, Tania Barham, Janet Currie, Davide Dragone, Alex Frankel, Allison Frost, Cheti Nicoletti, Jonathan de Quidt, Maya Rossin-Slater, Kosali Simon, Denni Tommasi, Joe Vecci, Matt Wiswall, and participants at the 13th Workshop on the Economics of Health and Wellbeing, Princeton Workshop on Child Mental Health, the University of Milan Bicocca Seminar, and the Warwick-CAGE conference on mental health. Sonia Bhalotra acknowledges partial funding for her time from ESRC award ES/S003681/1 to the Centre for Microsocial Change, and from Warwick-CAGE. The data collection was partially funded by NICHD award R01HD075875 and NIMH U19MH95687. The study procedures were approved by ethics committees in the US (Duke University, UNC) and Pakistan (Human Development Research Foundation’s Ethics Committee). This paper uses confidential data from the Bahcpan Cohort Study https://www.bachpanstudy.com/. The data can be obtained upon request to the last author. At the end of the grant period, the anonymized data will be published in an open-access NIH repository. The code to replicate the results found in the paper is publicly available on github here https://github.com/pietrobiroli/tech_depression_BACHPAN.
Appendix to “Trajectories of Early Childhood Skill Development and Maternal Mental Health”
A. Measures of Child Development, Parental Background and Investment
The following table provides the full list of measurements for child development, parental skills investment and baseline household characteristics that we were initially interested in.
Table A1:
Possible Measures for Child Development, Parental Background and Investment
| Latent Factor | Measurements | Baseline | 3 months | 6 months | 12 months | 24 months | 36 months |
|---|---|---|---|---|---|---|---|
| Child’s Physical Health and | Ages and Stages Questionnaire (ASQ-SE) : all items | NA | NA | ✓ | ✓ | ✓ | ✓ |
| Strengths and Difficulties Questionnaire (SDQ) : all items | NA | NA | NA | NA | NA | ✓ | |
| Child’s Physical Health and | Child’s weight for age Z-score | NA | ✓ | ✓ | ✓ | ✓ | ✓ |
| Child’s height for age Z-score | NA | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Child’s Head Circumference for age Z-score | NA | ✓ | ✓ | ✓ | ✓ | NA | |
| Child’s Cognition and | Bayley Scales of Infant Development: Fine Motor | NA | NA | NA | ✓ | NA | ✓ |
| Bayley Scales of Infant Development: Gross Motor | NA | NA | NA | ✓ | NA | NA | |
| Bayley Scales of Infant Development: Cognitive | NA | NA | NA | ✓ | NA | NA | |
| Bayley Scales of Infant Development: Expressive | NA | NA | NA | ✓ | NA | NA | |
| Bayley Scales of Infant Development: Receptive | NA | NA | NA | ✓ | NA | ✓ | |
| Parents’ Education at Baseline | Number of years the mother spent in education | ✓ | NA | NA | NA | NA | NA |
| Number of years the father spent in education | ✓ | NA | NA | NA | NA | NA | |
| Mothers’ Mental Health | Patient Health Questionnaire (PHQ - 9): all items | ✓ | ✓ | ✓ | NA | ✓ | ✓ |
| Structured Clinical Interview for the DSM (SCID) : all items | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Cohen Perceived Stress Scale (PSS): all items | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Mothers’ Functioning | WHO Disability Assessment Schedule (WHO-DAS): all items | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Parental Investment and | HOME:Learning Material Subscale | NA | ✓ | NA | ✓ | NA | ✓ |
| HOME:Responsivity Subscale | NA | ✓ | NA | ✓ | NA | ✓ | |
| HOME:Acceptance Subscale | NA | ✓ | NA | ✓ | NA | ✓ | |
| HOME:Organization Subscale | NA | ✓ | NA | ✓ | NA | ✓ | |
| HOME:Involvement Subscale | NA | ✓ | NA | ✓ | NA | ✓ | |
| HOME:Variety Subscale | NA | ✓ | NA | ✓ | NA | ✓ | |
| Observation of Mother-Child Interaction | NA | NA | NA | NA | ✓ | ✓ |
B. Balance and Attrition
Table A2:
Characteristics of Attritors at 6 months
| Attritor characteristics | Attritor characteristics by treatment arm | |||||||
|---|---|---|---|---|---|---|---|---|
| Sample mean (1) |
Attritor mean (2) |
Diff. (2)-(1) (3) |
p-val (4) |
Attritor T mean (5) |
Attritor C mean (6) |
Diff. T-C (7) |
p-val (8) |
|
| Mother’s age | 26.617 | 27.076 | 0.459 | 0.208 | 26.906 | 26.966 | −0.060 | 0.949 |
| Mother’s height (cm) | 157.012 | 156.909 | −0.103 | 0.832 | 157.323 | 155.834 | 1.489 | 0.214 |
| Mother’s weight (kg) | 60.378 | 59.945 | −0.434 | 0.513 | 58.711 | 59.417 | −0.706 | 0.737 |
| Mother’s waist circ. (in) | 37.217 | 36.976 | −0.240 | 0.393 | 36.225 | 36.651 | −0.426 | 0.593 |
| Mother’s blood pressure | 71.242 | 73.312 | 2.071 | 0.041 | 69.604 | 75.220 | −5.617 | 0.036 |
| PHQ total | 8.671 | 8.667 | −0.004 | 0.995 | 15.094 | 14.627 | 0.467 | 0.483 |
| WHODAS total | 10.861 | 11.298 | 0.437 | 0.613 | 17.302 | 16.627 | 0.675 | 0.709 |
| PSS total | 17.670 | 17.938 | 0.268 | 0.705 | 23.075 | 23.644 | −0.569 | 0.707 |
| Joint/extended family | 0.665 | 0.627 | −0.039 | 0.340 | 0.491 | 0.542 | −0.052 | 0.566 |
| Grandmother present | 0.700 | 0.613 | −0.086 | 0.058 | 0.472 | 0.559 | −0.088 | 0.447 |
| Total adults in the hh | 5.742 | 5.804 | 0.063 | 0.769 | 4.792 | 5.407 | −0.614 | 0.337 |
| People per room | 2.348 | 2.721 | 0.373 | 0.012 | 3.077 | 2.749 | 0.328 | 0.481 |
| Number of girls | 0.776 | 0.809 | 0.033 | 0.699 | 1.075 | 0.831 | 0.245 | 0.227 |
| Number of boys | 0.688 | 0.693 | 0.005 | 0.923 | 1.057 | 0.712 | 0.345 | 0.033 |
| First child | 0.292 | 0.347 | 0.055 | 0.074 | 0.226 | 0.322 | −0.096 | 0.196 |
| SES asset index | 0.041 | −0.186 | −0.227 | 0.097 | −1.155 | −0.440 | −0.715 | 0.011 |
| Mother’s education | 7.792 | 7.324 | −0.468 | 0.145 | 5.547 | 7.017 | −1.470 | 0.105 |
| Father’s education | 8.643 | 8.564 | −0.078 | 0.740 | 7.679 | 7.881 | −0.202 | 0.758 |
| Life Events Checklist | 3.632 | 3.653 | 0.021 | 0.899 | 4.377 | 4.102 | 0.276 | 0.623 |
| Observations | 929 | 225 | 1154 | 53 | 59 | 112 | ||
| Joint test (p-value) | 0.138 | |||||||
Note: Table shows baseline characteristics and their differences for women who were lost to 6 months follow-up. Columns 1–4 compare the 6 months follow-up sample to attritors at 6 months. Columns 5–8 compares the baseline characteristics of attritors at 6 months by treatment arm. p-value at the bottom of the table comes from the F-test that jointly tests all coefficients with the null hypothesis of attritors in the treatment and control groups being balanced.
Table A3:
Characteristics of Attritors at 12 months
| Attritor characteristics | Attritor characteristics by treatment arm | |||||||
|---|---|---|---|---|---|---|---|---|
| Sample mean (1) |
Attritor mean (2) |
Diff. (2)-(1) (3) |
p-val (4) |
Attritor T mean (5) |
Attritor C mean (6) |
Diff. T-C (7) |
p-val (8) |
|
| Mother’s age | 26.719 | 26.650 | −0.070 | 0.850 | 26.267 | 27.220 | −0.954 | 0.298 |
| Mother’s height (cm) | 157.035 | 156.804 | −0.231 | 0.618 | 156.948 | 155.608 | 1.340 | 0.214 |
| Mother’s weight (kg) | 60.442 | 59.642 | −0.800 | 0.238 | 57.970 | 59.758 | −1.788 | 0.422 |
| Mother’s waist circ. (in) | 37.224 | 36.931 | −0.293 | 0.315 | 36.083 | 37.051 | −0.968 | 0.285 |
| Mother’s blood pressure | 71.449 | 72.512 | 1.063 | 0.324 | 70.817 | 73.153 | −2.336 | 0.386 |
| PHQ total | 8.478 | 9.514 | 1.036 | 0.034 | 14.983 | 14.864 | 0.119 | 0.857 |
| WHODAS total | 10.714 | 11.967 | 1.253 | 0.214 | 16.750 | 16.966 | −0.216 | 0.905 |
| PSS total | 17.589 | 18.304 | 0.714 | 0.305 | 23.367 | 23.068 | 0.299 | 0.831 |
| Joint/extended family | 0.653 | 0.678 | 0.024 | 0.445 | 0.550 | 0.627 | −0.077 | 0.317 |
| Grandmother present | 0.694 | 0.636 | −0.058 | 0.166 | 0.517 | 0.576 | −0.060 | 0.560 |
| Total adults in the hh | 5.747 | 5.785 | 0.038 | 0.866 | 5.167 | 5.695 | −0.528 | 0.376 |
| People per room | 2.360 | 2.686 | 0.326 | 0.046 | 3.025 | 2.824 | 0.201 | 0.672 |
| Number of girls | 0.762 | 0.874 | 0.112 | 0.178 | 1.100 | 0.949 | 0.151 | 0.424 |
| Number of boys | 0.699 | 0.645 | −0.054 | 0.414 | 0.933 | 0.695 | 0.238 | 0.178 |
| First child | 0.293 | 0.346 | 0.053 | 0.188 | 0.217 | 0.339 | −0.122 | 0.154 |
| SES asset index | 0.025 | −0.131 | −0.156 | 0.240 | −0.917 | −0.267 | −0.650 | 0.024 |
| Mother’s education | 7.737 | 7.542 | −0.195 | 0.578 | 6.183 | 7.237 | −1.054 | 0.209 |
| Father’s education | 8.643 | 8.561 | −0.082 | 0.734 | 7.967 | 7.966 | 0.001 | 0.999 |
| Life Events Checklist | 3.629 | 3.668 | 0.040 | 0.833 | 4.567 | 3.966 | 0.601 | 0.275 |
| Observations | 940 | 214 | 1154 | 60 | 59 | 119 | ||
| Joint test (p-value) | 0.498 | |||||||
Note: Table shows baseline characteristics and their differences for women who were lost to 12 months follow-up. Columns 1–4 compare the 12 months follow-up sample to attritors at 12 months. Columns 5–8 compares the baseline characteristics of attritors at 12 months by treatment arm. p-value at the bottom of the table comes from the F-test that jointly tests all coefficients with the null hypothesis of attritors in the treatment and control groups being balanced.
Table A4:
Characteristics of Attritors at 24 months
| Attritor characteristics | Attritor characteristics by treatment arm | |||||||
|---|---|---|---|---|---|---|---|---|
| Sample mean (1) |
Attritor mean (2) |
Diff. (2)-(1) (3) |
p-val (4) |
Attritor T mean (5) |
Attritor C mean (6) |
Diff. T-C (7) |
p-val (8) |
|
| Mother’s age | 26.638 | 26.952 | 0.314 | 0.411 | 26.562 | 27.597 | −1.035 | 0.308 |
| Mother’s height (cm) | 157.120 | 156.530 | −0.591 | 0.196 | 156.705 | 156.331 | 0.374 | 0.744 |
| Mother’s weight (cm) | 60.489 | 59.592 | −0.897 | 0.246 | 58.074 | 58.863 | −0.789 | 0.684 |
| Mother’s waist circ. (in) | 37.262 | 36.838 | −0.424 | 0.180 | 36.332 | 36.504 | −0.173 | 0.828 |
| Mother’s blood pressure | 71.411 | 72.488 | 1.077 | 0.360 | 69.699 | 74.433 | −4.734 | 0.085 |
| PHQ total | 8.373 | 9.737 | 1.364 | 0.007 | 15.425 | 14.940 | 0.484 | 0.439 |
| WHODAS total | 10.647 | 12.024 | 1.377 | 0.082 | 16.219 | 16.851 | −0.632 | 0.704 |
| PSS total | 17.435 | 18.753 | 1.318 | 0.058 | 23.534 | 23.448 | 0.086 | 0.947 |
| Joint/extended family | 0.661 | 0.645 | −0.016 | 0.603 | 0.548 | 0.582 | −0.034 | 0.676 |
| Grandmother present | 0.695 | 0.637 | −0.058 | 0.111 | 0.562 | 0.567 | −0.006 | 0.954 |
| Total adults in the hh | 5.728 | 5.849 | 0.121 | 0.565 | 5.014 | 5.851 | −0.837 | 0.139 |
| People per room | 2.311 | 2.815 | 0.504 | 0.002 | 3.054 | 2.811 | 0.242 | 0.603 |
| Number of girls | 0.753 | 0.888 | 0.135 | 0.057 | 1.014 | 0.985 | 0.029 | 0.884 |
| Number of boys | 0.687 | 0.697 | 0.011 | 0.866 | 0.945 | 0.791 | 0.154 | 0.335 |
| First child | 0.297 | 0.323 | 0.026 | 0.483 | 0.233 | 0.284 | −0.051 | 0.555 |
| SES asset index | 0.033 | −0.135 | −0.168 | 0.187 | −0.788 | −0.321 | −0.466 | 0.086 |
| Mother’s education | 7.746 | 7.538 | −0.209 | 0.507 | 6.863 | 7.045 | −0.182 | 0.833 |
| Father’s education | 8.731 | 8.255 | −0.476 | 0.056 | 7.890 | 7.194 | 0.696 | 0.290 |
| Life Events Checklist | 3.579 | 3.841 | 0.261 | 0.132 | 4.548 | 4.090 | 0.458 | 0.364 |
| Observations | 903 | 251 | 1154 | 73 | 67 | 140 | ||
| Joint test (p-value) | 0.046 | |||||||
Note: Table shows baseline characteristics and their differences for women who were lost to 24 months follow-up. Columns 1–4 compare the 24 months follow-up sample (including nondepressed arm) to attritors at 24 months. Columns 5–8 compares the baseline characteristics of attritors at 24 months by treatment arm. p-value at the bottom of the table comes from the F-test that jointly tests all coefficients with the null hypothesis of attritors in the treatment and control groups being balanced.
Table A5:
Characteristics of Attritors at 36 months
| Attritor characteristics | Attritor characteristics by treatment arm | |||||||
|---|---|---|---|---|---|---|---|---|
| Sample mean (1) |
Attritor mean (2) |
Diff. (2)-(1) (3) |
p-val (4) |
Attritor T mean (5) |
Attritor C mean (6) |
Diff. T-C (7) |
p-val (8) |
|
| Mother’s age | 26.669 | 26.830 | 0.161 | 0.640 | 26.468 | 27.437 | −0.969 | 0.317 |
| Mother’s height (cm) | 157.047 | 156.806 | −0.242 | 0.658 | 157.260 | 155.903 | 1.357 | 0.229 |
| Mother’s weight (kg) | 60.582 | 59.325 | −1.257 | 0.064 | 58.739 | 58.955 | −0.216 | 0.911 |
| Mother’s waist circ. (in) | 37.262 | 36.862 | −0.400 | 0.155 | 36.304 | 36.980 | −0.676 | 0.350 |
| Mother’s blood pressure | 71.504 | 72.121 | 0.617 | 0.573 | 70.532 | 72.986 | −2.453 | 0.344 |
| PHQ total | 8.379 | 9.645 | 1.266 | 0.007 | 15.130 | 14.662 | 0.468 | 0.446 |
| WHODAS total | 10.714 | 11.725 | 1.010 | 0.160 | 16.299 | 16.268 | 0.031 | 0.982 |
| PSS total | 17.553 | 18.287 | 0.733 | 0.310 | 23.325 | 22.549 | 0.775 | 0.548 |
| Joint/extended family | 0.666 | 0.630 | −0.036 | 0.278 | 0.571 | 0.563 | 0.008 | 0.919 |
| Grandmother present | 0.697 | 0.634 | −0.063 | 0.094 | 0.558 | 0.592 | −0.033 | 0.691 |
| Total adults in the hh | 5.763 | 5.725 | −0.038 | 0.865 | 5.078 | 5.676 | −0.598 | 0.304 |
| People per room | 2.353 | 2.647 | 0.294 | 0.041 | 3.013 | 2.715 | 0.298 | 0.443 |
| Number of girls | 0.759 | 0.860 | 0.101 | 0.133 | 1.104 | 0.859 | 0.245 | 0.181 |
| Number of boys | 0.701 | 0.649 | −0.052 | 0.428 | 0.883 | 0.732 | 0.151 | 0.331 |
| First child | 0.290 | 0.343 | 0.053 | 0.115 | 0.273 | 0.296 | −0.023 | 0.784 |
| SES asset index | 0.038 | −0.144 | −0.182 | 0.164 | −0.862 | −0.449 | −0.413 | 0.159 |
| Mother’s education | 7.738 | 7.577 | −0.161 | 0.536 | 6.714 | 6.887 | −0.173 | 0.808 |
| Father’s education | 8.682 | 8.445 | −0.236 | 0.266 | 7.948 | 7.634 | 0.314 | 0.600 |
| Life Events Checklist | 3.620 | 3.691 | 0.071 | 0.659 | 4.558 | 3.915 | 0.643 | 0.163 |
| Observations | 889 | 265 | 1154 | 77 | 71 | 148 | ||
| Joint test (p-value) | 0.652 | |||||||
Note: Table shows baseline characteristics and their differences for women who were lost to 36 months follow-up. Columns 1–4 compare the 36 months follow-up sample (including nondepressed arm) to attritors at 36 months. Columns 5–8 compares the baseline characteristics of attritors at 36 months by treatment arm. p-value at the bottom of the table comes from the F-test that jointly tests all coefficients with the null hypothesis of attritors in the treatment and control groups being balanced.
Table A6:
Attrition Corrected Treatment Effects on Factor Scores
| Adjusted Beta | Attrition bounds | ||
|---|---|---|---|
| Unweighted (1) |
IPW (2) |
95% CI (3) |
|
| Maternal Factor Scores | |||
| Mental Health (6m) | 0.205*** (0.052) |
0.205*** (0.052) |
[−0.021 0.394] |
| Mental Health (12m) | 0.170*** (0.054) |
0.169*** (0.054) |
[−0.105 0.385] |
| Mental Health (24m) | −0.002 (0.057) |
0.001 (0.058) |
[−0.294 0.231] |
| Mental Health (36m) | 0.268*** (0.078) |
0.265*** (0.077) |
[−0.159 0.372] |
| Functioning (6m) | 0.182** (0.075) |
0.182** (0.075) |
[−0.052 0.364] |
| Functioning (12m) | 0.195*** (0.069) |
0.196*** (0.069) |
[−0.027 0.406] |
| Functioning (24m) | −0.036 (0.072) |
−0.034 (0.074) |
[−0.341 0.204] |
| Functioning (36m) | 0.287***
(0.081) |
0.280*** (0.079) |
[−0.200 0.349] |
| Child Factor Scores | |||
| Physical Health (6m) | −0.021 (0.079) |
−0.021 (0.079) |
[−0.217 0.204] |
| Physical Health (12m) | 0.019 (0.070) |
0.021 (0.069) |
[−0.187 0.287] |
| Physical Health (24m) | −0.100 (0.083) |
−0.091 (0.083) |
[−0.404 0.171] |
| Physical Health (36m) | −0.166* (0.088) |
−0.160* (0.089) |
[−0.434 0.154] |
| Socioemotional Skills (6m) | 0.187*** (0.056) |
0.187*** (0.056) |
[−0.006 0.375] |
| Socioemotional Skills (12m) | 0.389*** (0.070) |
0.389*** (0.070) |
[0.149 0.601] |
| Socioemotional Skills (24m) | −0.065 (0.067) |
−0.060 (0.071) |
[−0.347 0.162] |
| Socioemotional Skills (36m) | 0.063 (0.075) |
0.073 (0.076) |
[−0.308 0.291] |
| Cognition (12m) | −0.080 (0.083) |
−0.080 (0.084) |
[−0.357 0.227] |
| Cognition (36m) | 0.065 (0.075) |
0.065 (0.073) |
[−0.234 0.364] |
| Investment Factor Scores | |||
| Parental Investment (12m) | 0.075 (0.086) |
0.075 (0.087) |
[−0.204 0.309] |
| Parental Investment (36m) | 0.111 (0.076) |
0.111 (0.078) |
[−0.274 0.321] |
Column 1 reproduces the adjusted treatment effect coefficient on factor scores without attrition correction. Column 2 reports attrition-corrected treatment effect estimates using Inverse Probability of Attrition Weighting (IPAW), where the weights are the inverse of the predicted probability to participate in the respective follow-up based on the baseline covariates. Column 3 shows 95 percent confidence intervals for the treatment effect using attrition bounds that are tightened by child gender and the indicator of whether the baseline PHQ-9 score is above the median (Lee, 2009).
Note:
p<0.1;
p<0.05;
p<0.01
Table A7:
Attrition Corrected Treatment Effects on Factor Scores by Child Gender
| Boys | Girls | |||
|---|---|---|---|---|
| Adjusted Beta (1) |
Attrition bounds 95% CI (2) |
Adjusted Beta (3) |
Attrition bounds 95% CI (4) |
|
| Maternal Factor Scores | ||||
| Mental Health (6m) | 0.417*** (0.117) |
[0.080 0.634] | 0.113 (0.114) |
[−0.278 0.312] |
| Mental Health (12m) | 0.393*** (0.111) |
[0.034 0.597] | 0.178* (0.096) |
[−0.344 0.315] |
| Mental Health (24m) | 0.046 (0.113) |
[−0.396 0.311] | 0.016 (0.129) |
[−0.704 0.112] |
| Mental Health (36m) | 0.425*** (0.116) |
[−0.093 0.576] | 0.273** (0.124) |
[−0.388 0.320] |
| Functioning (6m) | 0.324*** (0.106) |
[−0.017 0.510] | 0.182** (0.075) |
[−0.257 0.333] |
| Functioning (12m) | 0.356*** (0.099) |
[0.077 0.622] | 0.195*** (0.069) |
[−0.233 0.399] |
| Functioning (24m) | −0.066 (0.098) |
[−0.580 0.130] | −0.026 (0.139) |
[−0.465 0.324] |
| Functioning (36m) | 0.337*** (0.108) |
[−0.206 0.489] | 0.287*** (0.081) |
[−0.380 0.357] |
| Child Factor Scores | ||||
| Physical Health (6m) | −0.052 (0.124) |
[−0.200 0.441] | −0.018 (0.102) |
[−0.407 0.131] |
| Physical Health (12m) | −0.059 (0.099) | [−0.239 0.337] | −0.004 (0.108) |
[−0.298 0.296] |
| Physical Health (24m) | −0.116 (0.117) |
[−0.451 0.253] | −0.036 (0.124) |
[−0.505 0.299] |
| Physical Health (36m) | −0.137 (0.119) |
[−0.440 0.288] | −0.075 (0.089) |
[−0.592 0.182] |
| Socioemotional Skills (6m) | 0.250*** (0.079) |
[0.037 0.618] | 0.120 (0.102) |
[−0.251 0.269] |
| Socioemotional Skills (12m) | 0.630*** (0.086) |
[0.289 0.873] | 0.354*** (0.104) |
[−0.103 0.530] |
| Socioemotional Skills (24m) | −0.163 (0.116) |
[−0.509 0.205] | −0.257 (0.219) |
[−0.422 0.335] |
| Socioemotional Skills (36m) | −0.058 (0.117) |
[−0.403 0.346] | 0.094 (0.096) |
[−0.404 0.395] |
| Cognition (12m) | −0.073 (0.129) |
[−0.315 0.308] | −0.133 (0.136) |
[−0.520 0.320] |
| Cognition (36m) | 0.206** (0.099) |
[−0.220 0.514] | 0.072 (0.149) |
[−0.419 0.402] |
| Investment Factor Scores | ||||
| Parental Investment (12m) | 0.114 (0.098) |
[−0.130 0.479] | 0.058 (0.135) |
[−0.411 0.261] |
| Parental Investment (36m) | 0.197** (0.097) |
[−0.243 0.517] | 0.210 (0.131) |
[−0.486 0.290] |
Column 1 and 3 reproduce the adjusted treatment effect coefficient on factor scores separately by child gender without attrition correction. Column 2 and 4 report 95 percent confidence intervals for the treatment effect by child gender using attrition bounds tightened by the indicator of whether the baseline PHQ-9 score is above the median (Lee, 2009).
Note:
p<0.1;
p<0.05;
p<0.01
Table A8:
Baseline Balance By Gender
| Baseline Sample: Boys (N=511) | Baseline Sample: Girls (N=503) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | T | ND | Diff | p-val | Control | T | ND | Diff | p-val | |||
| Mean | SD | Mean | Mean | T-C | Mean | SD | Mean | Mean | T-C | |||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | |
| Mother’s age | 27.339 | 5.240 | 27.118 | 26.126 | −0.221 | 0.762 | 27.279 | 4.495 | 26.460 | 26.424 | −0.819 | 0.100 |
| Mother’s height (cm) | 156.407 | 6.714 | 157.678 | 157.018 | 1.271 | 0.138 | 156.633 | 5.662 | 157.527 | 157.070 | 0.894 | 0.281 |
| Mother’s weight (kg) | 61.214 | 13.604 | 61.152 | 59.524 | −0.062 | 0.973 | 62.139 | 12.189 | 59.698 | 59.972 | −2.441 | 0.139 |
| Mother’s waist circ. (in) | 37.601 | 3.975 | 36.949 | 37.067 | −0.652 | 0.321 | 37.821 | 4.039 | 36.837 | 37.151 | −0.992 | 0.044 |
| Mother’s blood pressure | 72.115 | 9.857 | 70.780 | 71.200 | −1.335 | 0.333 | 71.760 | 14.023 | 71.306 | 71.759 | −0.453 | 0.732 |
| PHQ total | 14.539 | 3.885 | 14.437 | 2.783 | −0.102 | 0.846 | 14.333 | 3.346 | 15.121 | 2.796 | 0.788 | 0.133 |
| WHODAS total | 15.538 | 9.023 | 16.487 | 5.379 | 0.905 | 0.443 | 16.450 | 8.845 | 16.750 | 5.528 | 0.300 | 0.786 |
| PSS total | 23.043 | 8.276 | 23.765 | 12.282 | 0.721 | 0.428 | 22.659 | 7.221 | 24.218 | 12.076 | 1.559 | 0.078 |
| Current Major Dep. Episode | 0.713 | 0.454 | 0.748 | 0.018 | 0.035 | 0.566 | 0.721 | 0.450 | 0.782 | 0.024 | 0.061 | 0.431 |
| Joint/extended family | 0.661 | 0.475 | 0.563 | 0.700 | −0.098 | 0.046 | 0.628 | 0.485 | 0.637 | 0.704 | 0.009 | 0.883 |
| Grandmother present | 0.643 | 0.481 | 0.639 | 0.682 | −0.005 | 0.948 | 0.705 | 0.458 | 0.677 | 0.752 | −0.028 | 0.613 |
| Total adults in the hh | 5.635 | 3.044 | 5.454 | 5.722 | −0.181 | 0.692 | 5.721 | 2.823 | 5.379 | 6.260 | −0.342 | 0.391 |
| People per room | 2.365 | 1.218 | 2.565 | 2.211 | 0.199 | 0.342 | 2.409 | 1.359 | 2.934 | 2.241 | 0.525 | 0.045 |
| Number of girls | 0.904 | 1.116 | 0.874 | 0.697 | −0.030 | 0.839 | 0.783 | 1.007 | 0.984 | 0.600 | 0.201 | 0.186 |
| Number of boys | 0.817 | 0.894 | 0.790 | 0.574 | −0.027 | 0.822 | 0.791 | 0.982 | 0.855 | 0.600 | 0.064 | 0.621 |
| First child | 0.209 | 0.408 | 0.261 | 0.354 | 0.052 | 0.311 | 0.264 | 0.442 | 0.210 | 0.352 | −0.054 | 0.252 |
| SES asset index | −0.323 | 1.598 | −0.136 | 0.216 | 0.187 | 0.359 | −0.268 | 1.756 | −0.802 | 0.611 | −0.535 | 0.049 |
| Mother’s education | 6.652 | 4.621 | 7.529 | 8.177 | 0.877 | 0.187 | 6.829 | 4.316 | 6.403 | 8.948 | −0.426 | 0.499 |
| Father’s education | 8.313 | 3.147 | 7.958 | 8.906 | −0.355 | 0.395 | 8.550 | 3.264 | 7.734 | 9.328 | −0.817 | 0.093 |
| Life Events Checklist | 4.061 | 2.137 | 4.588 | 2.989 | 0.527 | 0.067 | 4.163 | 2.361 | 4.976 | 2.712 | 0.813 | 0.001 |
| Observations | 115 | 119 | 277 | 129 | 124 | 250 | ||||||
| Joint test (p-value) | 0.412 | 0.123 | ||||||||||
T = treatment, ND = non-depressed. Table tests for balance for the baseline characteristics by child gender. Columns 1,3 and 4 show the mean of the mothers of boys in the control, treatment and nondepressed group in the baseline sample, respectively. Columns 7,9 and 10 show the mean of the mothers of girls in the control, treatment and nondepressed group in the baseline sample, respectively. Columns 5 and 11 show the difference in means between nondepressed and depressed group, for mothers of boys and girls, respectively. p-values at the bottom of the table comes from the F-test of overall significance from a regression of the treatment dummy on all the baseline controls.
Table A9:
Balance in the Non-depressed Sample
| Control ND | Treat ND | Diff. | s.e. | p-val | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | (TND-CND) | |||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Mother’s Age | 26.170 | 4.185 | 26.573 | 0.403 | 0.390 | 0.301 |
| Mother’s height (cm) | 157.422 | 6.426 | 156.794 | −0.628 | 0.516 | 0.224 |
| Mother’s weight (kg) | 60.127 | 10.796 | 59.652 | −0.475 | 1.103 | 0.667 |
| Mother’s waist circ. (in) | 37.092 | 4.223 | 37.176 | 0.084 | 0.420 | 0.841 |
| Mother’s blood pressure | 71.576 | 9.687 | 71.757 | 0.180 | 0.804 | 0.822 |
| PHQ Total | 2.792 | 2.438 | 2.800 | 0.008 | 0.293 | 0.979 |
| WHODAS Total | 5.381 | 6.235 | 5.841 | 0.460 | 0.596 | 0.440 |
| PSS Total | 12.467 | 6.619 | 11.963 | −0.504 | 0.722 | 0.485 |
| Current Major Dep. Episode | 0.014 | 0.117 | 0.027 | 0.013 | 0.012 | 0.258 |
| Joint/extended family | 0.716 | 0.452 | 0.698 | −0.018 | 0.044 | 0.686 |
| Grandmother present | 0.727 | 0.446 | 0.708 | −0.018 | 0.035 | 0.600 |
| Total adults in the hh | 6.042 | 3.216 | 5.929 | −0.113 | 0.256 | 0.659 |
| People per room | 2.260 | 1.825 | 2.171 | −0.089 | 0.158 | 0.572 |
| Number of girls | 0.661 | 0.914 | 0.664 | 0.004 | 0.081 | 0.965 |
| Number of boys | 0.599 | 0.836 | 0.522 | −0.077 | 0.069 | 0.270 |
| First child | 0.374 | 0.485 | 0.353 | −0.021 | 0.037 | 0.566 |
| SES asset index | 0.365 | 1.429 | 0.477 | 0.112 | 0.156 | 0.474 |
| Mother’s education | 8.176 | 4.310 | 8.949 | 0.773 | 0.476 | 0.104 |
| Father’s education | 9.142 | 3.223 | 9.159 | 0.017 | 0.332 | 0.958 |
| Life Events Checklist | 2.799 | 2.197 | 2.990 | 0.191 | 0.267 | 0.476 |
| Observations | 289 | 295 | 584 | |||
| Joint test (p-value) | 0.456 | |||||
Note: Table tests for baseline balance in the sample of mothers who were not depressed at baseline. Columns 1 and 3 show the mean of the non-depressed mothers in the control and treatment clusters in the baseline sample, respectively. Column 4 shows the difference in means of the non-depressed mothers between treatment and control clusters. p-value at the bottom of the table comes from the F-test that jointly tests all coefficients with the null hypothesis of non-depressed women in the treatment and control clusters being balanced.
C. 24 Month Wave
The measurement system at 24 month was different than the adjoining waves: there is no measure of cognitive ability and parental investment was measured using the Observation of Mother-Child Interaction (OMCI), a tool used to capture parental sensitivity and responsiveness, instead of the HOME. As a longitudinal comparison of latent variables requires normalization of the factors on the same measure over time, we decided to exclude the 24 month wave from the main analysis. For completeness, we report estimates of the treatment effects at 24 months throughout the Appendix Tables. In this section we briefly discuss some of the anomalies that were found at the 24 month wave, where we find null, slightly negative, effects across most outcomes.
As noted in Appendix B, there is evidence of differential attrition in the 24-month follow-up. At the 24-month follow-up, attritors had higher WHODAS and PSS scores, a higher number of girls, and less educated husbands. Although this is unlikely to explain a null treatment effect, to investigate we estimated treatment effects using the fixed sample of 771 mothers who were present at all follow-up points (A23–A26). The treatment effects in this sample are similar to the treatment effects in the full sample, suggesting that the dip in treatment effects at 24 months is not an artifact of differential attrition.
We also investigate whether the dip in the treatment effect at 24 months can be explained by differential fertility, differential shocks to treatment or control clusters, or measurement error, and find that it cannot. The median birth spacing in our sample is 24 months, and the treatment has a marginal effect in reducing fertility (adjusted beta coefficient of −0.08, p-value< 0.10) but flexibly controlling for post-treatment fertility choices does not change the treatment effect on maternal mental health. It does not seem that different shocks in the treated vs control clusters occur at 24 months as we do not find any differences at this point in the mothers who were not depressed at baseline (who are not treated but live in the same villages as mothers in the intervention). Measurement error is an unlikely explanation because, looking at the estimated factor scores, the variance of the error term and the signal-to-noise ratios in the measurement system are similar across waves. We do find that the gap between the depressed controls and baseline non-depressed disappears for some outcomes at 24 months, suggesting the control group differentially experienced a positive shock in that wave.
D. Measurement System and Latent Factor Distributions
D.1. Latent Factor Scores
Following a long history in psychometrics (Spearman, 1904) and a more recent one in economics (Cunha and Heckman, 2008; Cunha et al., 2010; Attanasio et al., 2020a,c), we construct latent factor scores leveraging the correlation structure of the outcomes. Latent factor analysis is a model-based approach that reduces the measurement error and the dimensionality of the outcomes under the assumption that a latent variable exists and explains all of the correlations between related outcomes.
Specifically, assuming dedicated measurements for each latent factor , we denote the -th measure of the child’s skill of type at time with -th measure of parental skills at with and -th measure of parental investment at t with , where indicates the control group and indicates the treatment group. We assume a semi-log relationship linking the observed measures to the unobserved latent trait as follows:
| (A1) |
| (A2) |
| (A3) |
where are the latent factors for child skills, parental outcomes, and parental investment, represent the intercepts, are factor loadings, and are the error terms capturing measurement error, assumed to be normally distributed, with mean zero, independent of the latent factors and of each other.23 We further assume a dedicated measurement system which means each measure is associated only with one factor. These assumptions make sure that any correlation between observed variables in the data set results from the correlation of the latent variables. Finally, we assume that the same measurement system governs both groups (control, treatment, and nondepressed) and is consistent throughout the study period.
For identification purposes, the scale and the location of the latent log-factors are set by normalizing the measure that has the highest factor loading of each latent factor to one, i.e. . For longitudinal comparison purposes, we normalize each factor on the same measure at all time points.24 Regarding the location, since we are interested in the mean comparison between groups and over time, we fix the means of the latent factors in logs to 0 for the control group only at the initial time point (6 months) following Agostinelli and Wiswall (2016). This allows us to capture the growth of the latent factors over time.
Using exploratory factor analysis (EFA), we reduce the number of items contributing to each latent factor by discarding the ones that do not strongly correlate with the underlying latent trait of interest. The details of the EFA are reported in Section D.2 in the appendix. Next, we jointly estimate the measurement system using a maximum likelihood estimator, and predict factor scores for each individual in the sample.
The results of the estimation of the measurement system are reported in Tables A11–A17. To provide summary statistics for the importance of each measure in the system, we report the signal-to-noise ratio.26 The results indicate that the information contained in each measure of the same factor varies a lot, and that most measures are quite far from a 100% signal-to-noise ratio. This provides a justification for the latent variable approach to modelling child skill formation. Without such an approach, one would fail to capture the variety of aspects of child development in the early years of life.
Latent factor scores are more appropriate as aggregate indices if there are multiple domains, as they result from a multi-dimensional allocation of observed variables influenced by different factors. Indeed, latent factor analysis has been widely used to deal with measurement error problem in modelling child development (See, for example Cunha and Heckman, 2008; Cunha et al., 2010; Attanasio et al., 2020a,c).
D.2. Exploratory Factor Analysis
This section provides the details of exploratory factor analysis (EFA) performed to specify the measurement system described in Tables A11–A17. EFA consists of two parts: determination of the number of latent factors to be extracted from the set of measures in the data set and specifying the measurement system by allocating each measure to a factor and estimating factor loadings.
D.2.1. Determining the number of latent factors
To select the appropriate number of latent factors for child development, parental investment, and maternal mental health, the following methods are compared: Kaiser’s eigenvalue rule, Cattel’s scree plot, and Velicer’s minimum average partial correlation rule. The resulting number of factors is reported in Table A10. The results support our assumptions of two-three dimensions for child development, two dimensions for maternal skills, and one dimension for parental investment.
Table A10:
Results of different methods to determine the number of factors
| Number of Factors according to the following methods: | |||
|---|---|---|---|
| Kaiser’s Eigenvalue Rule | Cattell’s Scree Plot | Velicer’s MAP Rule | |
| Child’s Skills at 6 Months | 2 | 2 | 1 |
| Child’s Skills at 12 Months | 3 | 2 | 1 |
| Child’s Skills at 24 Months | 2 | 2 | 3 |
| Child’s Skills at 36 Months | 3 | 2 | 4 |
| Maternal Skills at 6 Months | 3 | 2 | 1 |
| Maternal Skills at 12 Months | 2 | 2 | 1 |
| Maternal Skills at 24 Months | 4 | 2 | 5 |
| Maternal Skills at 36 Months | 3 | 2 | 1 |
| Parental Investment at 6 Months | 1 | 2 | 1 |
| Parental Investment at 12 Months | 1 | 2 | 1 |
| Parental Investment at 24 Months | 3 | 2 | 2 |
| Parental Investment at 36 Months | 1 | 2 | 1 |
D.2.2. Specifying the Measurement System
Once we have evidence about how many latent factors should be extracted, we need to allocate each measure to a factor in accordance with the dedicated measurement system. To do this, we implement the quartimin rotation method and identify the measures that primarily load on one factor. The reason why we choose this method among others is that since our factors are likely to be correlated, an oblique rotation is more suitable. At this stage, we also discard measures that load on more than one factor or are not strongly related to one factor as such measures would conflict with our assumption of a dedicated measurement system.
Table A11:
Maternal Mental Health Measures I: Loadings and Signal-to-noise Ratio
| Measurement | Loading | % Signal | ||
|---|---|---|---|---|
| Control | Treated | Nondep. | ||
| 6 months | ||||
| scid13: Current major depressive episode(−) | 1.000 | 61.4% | 90.5% | 63.4% |
| scid1: Depressed Mode (−) | 1.059 | 57.5% | 56.2% | 49.5% |
| scid2: Loss of interest (−) | 1.035 | 57.3% | 56.1% | 59.3% |
| scid3: Weight/appetite loss or gain (−) | 0.832 | 37.9% | 34.3% | 37.3% |
| scid4: Sleep disturbance (−) | 0.858 | 38.6% | 38.9% | 37.9% |
| scid5: Psychomotor agitation or retardation(−) | 1.055 | 61.2% | 58.2% | 55.2% |
| scid6: Fatigue or loss of energy (−) | 1.025 | 50.0% | 45.5% | 33.4% |
| scid7: Feeling of worthlessness or inapropriate guilt (−) | 0.696 | 30.0% | 27.8% | 36.3% |
| scid8: Diminished ability to concentrate or indecisiveness (−) | 0.886 | 44.6% | 43.5% | 40.5% |
| scid9: Recurrent thoughts of death or suicidal ideation (−) | 0.304 | 5.3% | 7.4% | 12.8% |
| scid10: Symptoms cause significant distress or impairment (−) | 1.034 | 55.2% | 55.9% | 47.8% |
| pss3: How often have you felt nervous or stressed? (−) | 1.047 | 53.2% | 43.3% | 36.3% |
| phq1: Feeling tired or having little energy. (−) | 0.935 | 42.5% | 39.5% | 29.2% |
| phq2: Poor appetite or overeating. (−) | 0.766 | 32.0% | 31.2% | 25.7% |
| phq3: Trouble falling or staying asleep (−) | 0.705 | 26.3% | 28.3% | 26.7% |
| phq4: Moving/speaking so slowly (−) | 0.871 | 44.0% | 38.2% | 43.3% |
| phq5: Trouble concentrating on things(−) | 0.831 | 35.2% | 36.8% | 32.7% |
| phq6: Little interest or pleasure in doing things (−) | 0.986 | 48.5% | 50.3% | 45.9% |
| phq7: Feeling down, depressed, hopeless (−) | 1.077 | 59.1% | 54.8% | 47.6% |
| phq8: Feeling bad about yourself (−) | 0.808 | 38.2% | 40.9% | 39.7% |
| 12 months | ||||
| scid13: Current major depressive episode(−) | 1.000 | 65.0% | 57.5% | 62.1% |
| scid1: Depressed Mode (−) | 1.059 | 59.3% | 53.7% | 42.9% |
| scid2: Loss of interest (−) | 1.035 | 60.2% | 54.7% | 47.6% |
| scid3: Weight/appetite loss or gain (−) | 0.832 | 35.3% | 28.3% | 29.0% |
| scid4: Sleep disturbance (−) | 0.858 | 38.9% | 32.1% | 32.0% |
| scid5: Psychomotor agitation or retardation(−) | 1.055 | 56.5% | 51.9% | 46.3% |
| scid6: Fatigue or loss of energy (−) | 1.025 | 50.5% | 42.8% | 31.4% |
| scid7: Feeling of worthlessness or inapropriate guilt (−) | 0.696 | 32.0% | 30.0% | 34.4% |
| scid8: Diminished ability to concentrate or indecisiveness (−) | 0.886 | 49.0% | 41.4% | 45.0% |
| scid10: Symptoms cause significant distress or impairment (−) | 1.034 | 57.2% | 49.6% | 50.2% |
| pss1: In the last month, how often have you been upset? (−) | 0.971 | 49.6% | 47.3% | 33.6% |
| pss2: How often have you felt you were unable to control things? (−) | 0.968 | 53.8% | 47.2% | 34.8% |
| pss3: How often have you felt nervous or stressed? (−) | 1.047 | 59.1% | 56.5% | 42.4% |
| pss4: How often have you felt confident? | 0.890 | 39.4% | 61.4% | 21.6% |
| pss5: How often have you felt that things were going your way? | 0.903 | 37.2% | 39.9% | 26.5% |
| pss8: How often have you felt that you were on top of things? | 0.874 | 39.4% | 35.1% | 24.0% |
| pss10: How often have you felt difficulties piling up?(−) | 0.926 | 44.7% | 40.7% | 31.2% |
Note: This table reports the factor loadings of the measures allowed to load on the maternal mental health factor along with the fraction of variance in each measure that is explained by the variance of the underlying latent factor for the control, treatment and nondepressed group separately. All measures that were negatively worded in the follow-up surveys are reverse coded so that higher score means higher level of underlying skill.
Table A12:
Maternal Mental Health Measures II: Loadings and Signal-to-noise Ratio
| Measurement | Loading | % Signal | ||
|---|---|---|---|---|
| Control | Treated | Nondep. | ||
| 24 months | ||||
| scid13: Current major depressive episode(−) | 1.000 | 25.2% | 25.2% | 15.9% |
| scid1: Depressed Mode (−) | 1.059 | 46.5% | 44.9% | 32.0% |
| scid2: Loss of interest (−) | 1.035 | 21.9% | 34.0% | 18.5% |
| scid3: Weight/appetite loss or gain (−) | 0.832 | 51.7% | 63.8% | 37.9% |
| scid4: Sleep disturbance (−) | 0.858 | 80.5% | 65.6% | 34.3% |
| scid5: Psychomotor agitation or retardation(−) | 1.055 | 41.3% | 58.2% | 26.2% |
| scid6: Fatigue or loss of energy (−) | 1.025 | 62.5% | 65.0% | 61.1% |
| scid7: Feeling of worthlessness or inapropriate guilt (−) | 0.696 | 66.6% | 54.2% | 29.3% |
| scid8: Diminished ability to concentrate or indecisiveness (−) | 0.886 | 49.3% | 46.4% | 33.3% |
| scid10: Symptoms cause significant distress or impairment (−) | 1.034 | 32.5% | 25.5% | 27.9% |
| phq2: Poor appetite or overeating. (−) | 0.766 | 58.4% | 82.8% | 43.3% |
| phq3: Trouble falling or staying asleep (−) | 0.705 | 77.3% | 78.8% | 44.4% |
| phq4: Moving/speaking so slowly (−) | 0.871 | 59.7% | 58.1% | 32.4% |
| phq6: Little interest or pleasure in doing things (−) | 0.986 | 60.6% | 26.2% | 45.9% |
| phq7: Feeling down, depressed, hopeless (−) | 1.077 | 55.8% | 46.1% | 39.7% |
| phq8: Feeling bad about yourself (−) | 0.808 | 60.8% | 40.9% | 26.2% |
| 36 months | ||||
| scid13: Current major depressive episode (−) | 1.000 | 66.6% | 56.0% | 58.8% |
| scid1: Depressed Mode (−) | 1.059 | 62.8% | 54.0% | 56.9% |
| scid5: Psychomotor agitation or retardation(−) | 1.055 | 69.4% | 57.3% | 64.5% |
| scid6: Fatigue or loss of energy (−) | 1.025 | 59.1% | 50.9% | 49.9% |
| scid10: Symptoms cause significant distress or impairment (−) | 1.034 | 68.8% | 54.4% | 59.0% |
| pss1: In the last month, how often have you been upset? (−) | 0.971 | 62.9% | 52.3% | 53.5% |
| pss2: How often have you felt you were unable to control things? (−) | 0.968 | 62.8% | 54.5% | 52.4% |
| pss3: How often have you felt nervous or stressed? (−) | 1.047 | 71.7% | 59.8% | 56.8% |
| pss4: How often have you felt confident? | 0.890 | 51.9% | 45.6% | 39.6% |
| pss5: How often have you felt that things were going your way? | 0.903 | 52.2% | 46.9% | 35.6% |
| pss6: How often have you felt that you cannot cope with things?(−) | 0.939 | 51.3% | 41.8% | 35.9% |
| pss8: How often have you felt that you were on top of things? | 0.874 | 39.4% | 48.3% | 38.9% |
| pss10: How often have you felt difficulties piling up? (−) | 0.926 | 53.0% | 50.4% | 38.8% |
| phq1: Feeling tired or having little energy. (−) | 0.935 | 47.5% | 39.1% | 38.7% |
| phq3: Trouble falling or staying asleep (−) | 0.705 | 33.1% | 25.2% | 30.1% |
| phq4: Moving/speaking so slowly (−) | 0.871 | 51.2% | 38.2% | 50.1% |
| phq5: Trouble concentrating on things (−) | 0.831 | 42.1% | 32.1% | 32.9% |
| phq6: Little interest or pleasure in doing things (−) | 0.986 | 61.7% | 51.3% | 59.7% |
| phq7: Feeling down, depressed, hopeless (−) | 1.077 | 77.2% | 60.8% | 58.5% |
| phq8: Feeling bad about yourself (−) | 0.808 | 47.6% | 40.9% | 46.5% |
| gad1: Feeling nervous, anxious or on edge. (−) | 0.988 | 65.2% | 54.6% | 56.0% |
| gad2: Not being able to stop or control worrying. (−) | 0.965 | 68.7% | 54.5% | 57.9% |
| gad3: Worrying too much about different things. (−) | 0.906 | 59.8% | 59.9% | 51.5% |
| gad4: Trouble relaxing (−) | 0.919 | 38.2% | 60.9% | 57.9% |
| gad5: Being so restless it’s hard to sit still. (−) | 0.916 | 59.8% | 58.7% | 57.9% |
| gad6: Becoming easily annoyed or irritable. (−) | 0.967 | 56.7% | 54.4% | 51.4% |
| gad7: Feeling afraid as if something awful might happen. (−) | 0.972 | 60.8% | 45.2% | 55.1% |
Note: This table reports the factor loadings of the measures allowed to load on the maternal mental health factor along with the fraction of variance in each measure that is explained by the variance of the underlying latent factor for the control, treatment and nondepressed group separately. All measures that were negatively worded in the follow-up surveys are reverse coded so that higher score means higher level of underlying skill.
Table A13:
Maternal Functioning Measures: Loadings and Signal-to-noise Ratio
| Measurement | Loading | % Signal | ||
|---|---|---|---|---|
| Control | Treated | Nondep. | ||
| 6 months | ||||
| whodas12: Difficulty affecting day-to-day work.(−) | 1.000 | 69.5% | 61.1% | 62.4% |
| whodas2: Difficulty standing for long periods (−) | 0.949 | 55.1% | 55.7% | 36.8% |
| whodas3: Difficulty taking care of household responsibilities (−) | 1.032 | 68.7% | 64.2% | 50.9% |
| whodas4: Difficulty learning a new task (−) | 0.820 | 55.1% | 46.5% | 35.5% |
| whodas5: Difficulty joining in community activities (−) | 0.894 | 54.5% | 45.4% | 46.7% |
| whodas6: Difficulty concentrating (−) | 0.881 | 58.2% | 53.4% | 41.5% |
| whodas7: Difficulty walking a long distance (−) | 0.917 | 52.5% | 49.9% | 27.0% |
| whodas8: Difficulty washing your whole body (−) | 0.612 | 31.0% | 26.4% | 31.2% |
| whodas9: Difficulty getting dressed (−) | 0.588 | 27.9% | 20.5% | 39.1% |
| whodas10: Difficulty dealing with people you do not know (−) | 0.797 | 39.1% | 44.9% | 31.7% |
| whodas11: Dealing with maintaining a friendship (−) | 0.741 | 37.7% | 37.7% | 32.1% |
| whodas13: How much have you been affected by your health problems? (−) | 0.986 | 63.7% | 58.3% | 45.6% |
| 12 months | ||||
| whodas12: Difficulty affecting day-to-day work.(−) | 1.000 | 67.4% | 63.3% | 66.6% |
| whodas2: Difficulty standing for long periods (−) | 0.949 | 56.6% | 49.9% | 43.8% |
| whodas3: Difficulty taking care of household responsibilities (−) | 1.032 | 70.1% | 64.5% | 61.6% |
| whodas4: Difficulty learning a new task (−) | 0.820 | 50.3% | 43.5% | 42.0% |
| whodas5: Difficulty joining in community activities (−) | 0.894 | 52.7% | 48.4% | 46.2% |
| whodas6: Difficulty concentrating (−) | 0.881 | 55.3% | 52.7% | 55.1% |
| whodas7: Difficulty walking a long distance (−) | 0.917 | 55.8% | 43.5% | 41.8% |
| whodas8: Difficulty washing your whole body (−) | 0.612 | 29.5% | 33.6% | 41.6% |
| whodas9: Difficulty getting dressed (−) | 0.588 | 27.5% | 30.9% | 32.4% |
| whodas10: Difficulty dealing with people you do not know (−) | 0.797 | 41.8% | 36.9% | 34.9% |
| whodas13: How much have you been affected by your health problems? (−) | 0.986 | 62.6% | 52.9% | 55.5% |
| 24 months | ||||
| whodas12: Difficulty affecting day-to-day work.(−) | 1.000 | 67.4% | 68.4% | 71.6% |
| whodas2: Difficulty standing for long periods (−) | 0.949 | 59.5% | 57.0% | 57.2% |
| whodas3: Difficulty taking care of household responsibilities (−) | 1.032 | 69.8% | 70.2% | 74.2% |
| whodas4: Difficulty learning a new task (−) | 0.820 | 47.7% | 34.3% | 62.6% |
| whodas5: Difficulty joining in community activities (−) | 0.894 | 55.8% | 54.9% | 57.4% |
| whodas6: Difficulty concentrating (−) | 0.881 | 53.0% | 44.2% | 61.8% |
| whodas7: Difficulty walking a long distance (−) | 0.917 | 55.5% | 51.4% | 48.6% |
| whodas8: Difficulty washing your whole body (−) | 0.612 | 27.2% | 21.9% | 32.2% |
| whodas9: Difficulty getting dressed (−) | 0.588 | 25.1% | 14.4% | 13.6% |
| whodas10: Difficulty dealing with people you do not know (−) | 0.797 | 48.9% | 43.0% | 47.5% |
| whodas11: Dealing with maintaining a friendship (−) | 0.741 | 36.1% | 32.8% | 37.3% |
| whodas13: How much have you been affected by your health problems? (−) | 0.986 | 66.8% | 59.5% | 62.1% |
| 36 months | ||||
| whodas12: Difficulty affecting day-to-day work.(−) | 1.000 | 82.2% | 75.7% | 77.7% |
| whodas2: Difficulty standing for long periods (−) | 0.949 | 66.0% | 54.1% | 50.7% |
| whodas3: Difficulty taking care of household responsibilities (−) | 1.032 | 78.7% | 70.5% | 69.9% |
| whodas4: Difficulty learning a new task (−) | 0.820 | 58.2% | 51.9% | 54.0% |
| whodas5: Difficulty joining in community activities (−) | 0.894 | 66.4% | 61.2% | 65.6% |
| whodas6: Difficulty concentrating (−) | 0.881 | 71.8% | 65.5% | 64.6% |
| whodas7: Difficulty walking a long distance (−) | 0.917 | 64.1% | 56.7% | 52.1% |
| whodas8: Difficulty washing your whole body (−) | 0.612 | 32.1% | 31.1% | 33.5% |
| whodas9: Difficulty getting dressed (−) | 0.588 | 30.3% | 29.9% | 43.6% |
| whodas10: Difficulty dealing with people you do not know (−) | 0.797 | 53.2% | 44.5% | 48.2% |
| whodas11: Dealing with maintaining a friendship (−) | 0.741 | 46.2% | 44.5% | 38.1% |
| whodas13: How much have you been affected by your health problems? (−) | 0.986 | 76.5% | 69.8% | 70.5% |
Note: This table reports the factor loadings of the measures allowed to load on the maternal functioning factor along with the fraction of variance in each measure that is explained by the variance of the underlying latent factor for the control, treatment and nondepressed group separately. All measures that were negatively worded in the follow-up surveys are reverse coded so that higher score means higher level of underlying skill.
Table A14:
Socioemotional Measures of Child: Loadings and Signal-to-noise Ratio
| Measurement | Loading | % Signal | ||
|---|---|---|---|---|
| Control | Treated | Nondep. | ||
| 6 months | ||||
| asq1:Baby calms down within a half hour. | 1.000 | 31.2% | 22.0% | 16.5% |
| asq6:Baby lets you know when she is hungry/sick. | 0.391 | 4.8% | 2.0% | 2.0% |
| asq8:Baby is able to calm herself down.(−) | 0.949 | 27.5% | 17.2% | 13.8% |
| asq9:Baby cries for a long period of time. (−) | 1.130 | 34.8% | 31.4% | 26.7% |
| asq10:Baby’s body is relaxed. | 0.878 | 21.8% | 5.2% | 17.5% |
| asq11:Baby has trouble sucking.(−) | 0.508 | 7.5% | 2.5% | 3.4% |
| asq14:Baby has an eating problem. (−) | 0.575 | 11.6% | 7.6% | 5.1% |
| asq16:Baby has trouble falling asleep. (−) | 0.700 | 17.1% | 5.5% | 8.80% |
| asq17:Baby sleeps at least 10 hours a day. | 0.720 | 18.7% | 6.5% | 11.9% |
| asq18:Baby gets constipated or have diarrhea. (−) | 0.654 | 14.2% | 4.8% | 5.5% |
| asq19:Someone expressed concerns about baby’s behaviour. (−) | 0.601 | 12.7% | 3.6% | 4.0% |
| 12 months | ||||
| asq1:Baby calms down within a half hour. | 1.000 | 37.2% | 34.5% | 22.3% |
| asq3:Baby likes to be picked up. | 0.396 | 5.7% | 9.0% | 1.1% |
| asq4:Baby stiffens when picked up. (−) | 0.482 | 8.3% | 5.8% | 4.3% |
| asq8:Baby is able to calm herself down. | 0.949 | 32.6% | 23.9% | 15.4% |
| asq9:Baby cries for a long time.(−) | 1.130 | 46.0% | 51.1% | 38.1% |
| asq10:Baby’s body is relaxed. | 0.878 | 24.7% | 30.6% | 22.9% |
| asq14:Baby has an eating problem. (−) | 0.575 | 10.8% | 8.6% | 8.3% |
| asq16:Baby has a problem falling asleep. (−) | 0.700 | 16.3% | 30.1% | 13.1% |
| asq17:Baby sleeps at least 10 hours a day. | 0.720 | 16.5% | 14.5% | 12.5% |
| asq18:Baby gets constipated or have diarrhea.(−) | 0.654 | 13.2% | 10.5% | 7.9% |
| asq19:Someone expressed concerns about baby’s behaviour. (−) | 0.601 | 12.4% | 11.4% | 4.6% |
| asq20:Concerns about baby’s eating/sleeping behaviour. (−) | 0.495 | 8.5% | 6.6% | 4.1% |
| 24 months | ||||
| asq8:Child calms down within 15 minutes. | 1.000 | 44.0% | 46.4% | 78.5% |
| asq3:Child laughs or smile when you play with her. | 1.539 | 98.6% | 76.2% | 95.2% |
| asq4:Child’s body is relaxed. | 0.878 | 65.8% | 66.1% | 79.6% |
| asq6:Child greets familiar adults. | 1.581 | 70.2% | 87.0% | 92.7% |
| asq10:Child is interested in surroundings. | 1.131 | 56.9% | 87.4% | 89.4% |
| asq12:You and your child enjoy mealtimes together. | 1.359 | 69.3% | 96.2% | 78.4% |
| asq19:Child lets you know how she feels. | 0.964 | 35.5% | 35.6% | 52.1% |
| asq20:Child checks to make sure you are near. | 1.024 | 32.7% | 40.0% | 50.0% |
| asq22:Child likes to hear stories/songs. | 0.891 | 32.7% | 46.0% | 49.4% |
| 36 months | ||||
| asq5:Child calms down within 15 minutes. | 1.000 | 28.1% | 37.2% | 12.1% |
| asq3:Child plays/talks with adults she knows well. | 0.810 | 20.1% | 25.4% | 17.2% |
| asq7:Child can settle herself down. | 1.565 | 65.2% | 63.0% | 35.0% |
| asq8:Child easily moves from one activity to next. | 1.036 | 28.7% | 36.3% | 9.3% |
| asq9:Child seems happy. | 1.710 | 72.0% | 58.0% | 49.2% |
| asq10:Child is interested in surroundings. | 1.131 | 33.3% | 29.6% | 13.5% |
| asq11:Child does what you ask her to do. | 1.351 | 39.1% | 35.4% | 22.0% |
| asq13:Child can stay with an activity for 5 min. | 0.993 | 25.3% | 36.6% | 21.4% |
| asq14:You and your child enjoy mealtimes together. | 1.359 | 43.9% | 35.2% | 24.7% |
| sdq14:Generally liked by other children | 0.561 | 7.5% | 7.5% | 4.8% |
| sdq25:Good attention span. | 0.666 | 10.4% | 9.1% | 4.0% |
Note: This table reports the factor loadings of the measures allowed to load on the socioemotional factor of the child along with the fraction of variance in each measure that is explained by the variance of the underlying latent factor for the control, treatment and nondepressed group separately. All measures that were negatively worded in the follow-up surveys are reverse coded so that higher score means higher level of underlying skill.
Table A15:
Physical Health Measures of Child: Loadings and Signal-to-noise Ratio
| Measurement | Loading | % Signal | ||
|---|---|---|---|---|
| Control | Treated | Nondep. | ||
| 6 months | ||||
| Weight for age z-score | 1.000 | 75.0% | 62.8% | 60.9% |
| Height for age z-score | 0.819 | 43.9% | 43.4% | 42.8% |
| Head circumference for age z-score | 0.709 | 34.6% | 31.9% | 32.4% |
| 12 months | ||||
| Weight for age z-score | 1.000 | 68.9% | 58.9% | 60.8% |
| Height for age z-score | 0.819 | 53.6% | 46.8% | 25.7% |
| Head circumference for age z-score | 0.709 | 27.0% | 24.1% | 29.8% |
| 24 months | ||||
| Weight for age z-score | 1.000 | 66.5% | 75.1% | 67.7% |
| Height for age z-score | 0.818 | 44.1% | 47.5% | 45.3% |
| Head circumference for age z-score | 0.709 | 31.0% | 26.4% | 28.3% |
| 36 months | ||||
| Weight for age z-score | 1.000 | 78.0% | 87.9% | 82.8% |
| Height for age z-score | 0.819 | 53.6% | 45.9% | 45.8% |
Note: This table reports the factor loadings of the measures allowed to load on the physical health factor of the child along with the fraction of variance in each measure that is explained by the variance of the underlying latent factor for the control, treatment and nondepressed group separately. Z-scores are calculated based on the WHO Child Growth Standards.
Table A16:
Cognitive Measures of Child: Loadings and Signal-to-noise Ratio
| Measurement | Loading | % Signal | ||
|---|---|---|---|---|
| Control | Treated | Nondep. | ||
| 12 months | ||||
| Bayley: Fine motor scaled score | 1.000 | 57.5% | 67.3% | 55.4% |
| Bayley: Receptive scaled score | 0.679 | 28.2% | 35.0% | 22.0% |
| Bayley: Cognitive scaled score | 0.949 | 48.2% | 69.7% | 60.1% |
| Bayley: Expressive scaled score | 0.648 | 23.7% | 38.0% | 27.8% |
| Bayley: Gross motor scaled score | 0.639 | 23.6% | 31.0% | 20.0% |
| 36 months | ||||
| Bayley: Fine motor scaled score | 1.000 | 44.3% | 49.4% | 49.8% |
| Bayley: Receptive scaled score | 0.679 | 20.2% | 19.0% | 18.5% |
Note: This table reports the factor loadings of the measures allowed to load on the cognition factor of the child along with the fraction of variance in each measure that is explained by the variance of the underlying latent factor for the control, treatment and nondepressed group separately. Bayley scaled scores are calculated from the raw scores such that they have mean=10 and SD=3.
Table A17:
Parental Investment Measures: Loadings and Signal-to-noise Ratio
| Measurement | Loading | % Signal | ||
|---|---|---|---|---|
| Control | Treated | Nondep. | ||
| 6 months | ||||
| Maternal Postnatal Attachment Score | 1.000 | 41.4% | 37.5% | 45.9% |
| Maternal Self-Efficacy Score | 0.869 | 35.5% | 29.2% | 38.2% |
| 12 months | ||||
| HOME: Learning Material | 1.000 | 63.0% | 59.1% | 55.4% |
| HOME: Responsivity | 0.284 | 5.1% | 6.4% | 5.1% |
| HOME: Organization | 0.602 | 23.6% | 25.8% | 20.4% |
| HOME: Involvement | 0.872 | 46.7% | 49.2% | 44.5% |
| HOME: Variety | 0.535 | 17.4% | 11.9% | 14.4% |
| 24 months | ||||
| Omci2: Mom shows negative affect for child (−) | 1.000 | 85.3% | 69.2% | 61.9% |
| Omci1: Mom shows positive affect for child. | 0.291 | 9.7% | 3.5% | 7.9% |
| Omci3: Mom loses attention towards the child. (−) | 0.436 | 13.5% | 9.1% | 10.1% |
| Omci5: Mom shows negative touch. (−) | 0.836 | 47.1% | 25.4% | 34.6% |
| Omci7: Mom expresses negative verbal statement.(−) | 0.708 | 32.4% | 26.1% | 38.7% |
| Omci8: Mom shows intrusiveness. (−) | 0.534 | 13.5% | 28.8% | 13.4% |
| 36 months | ||||
| HOME: Learning Material | 1.000 | 57.7% | 55.5% | 58.6% |
| HOME: Acceptance | 0.158 | 1.5% | 1.9% | 1.5% |
| HOME: Organization | 0.602 | 21.3% | 20.8% | 20.9% |
| HOME: Involvement | 0.872 | 48.3% | 49.3% | 41.2% |
| HOME: Variety | 0.535 | 17.1% | 18.9% | 14.4% |
Note: This table reports the factor loadings of the measures allowed to load on the parental investment factor along with the fraction of variance in each measure that is explained by the variance of the underlying latent factor for the control, treatment and nondepressed group separately. Maternal postnatal attachment score is a sum score from a 19 item questionnaire assessing mother-infant attachment. Maternal self-efficacy score is a sum score from a 10 item questionnaire measuring mother’s ability to care for her child. Items reported under 12 and 36 months are used to estimate the longitudinal investment factor model. Items at 6 and 24 months are used to estimate investment factors at these follow-up points for descriptive purposes.
D.3. Estimated Latent Factor Correlations
The following figures provide the correlations between the estimated latent factors at 6, 12 and 36 months in control and the treatment groups separately.
Figure A1:
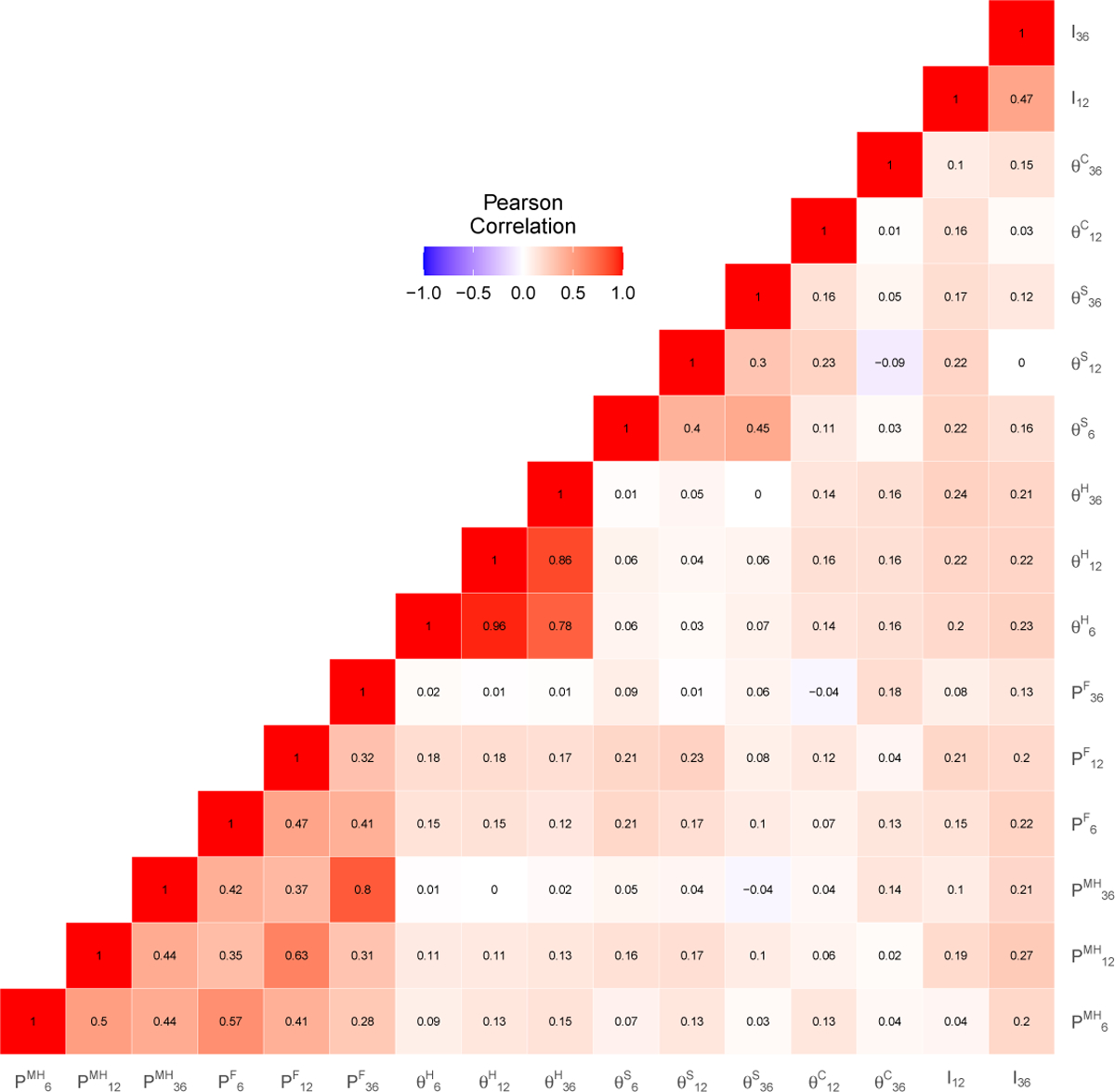
Estimated Latent Factor Correlations: Control Group
Figure A2:
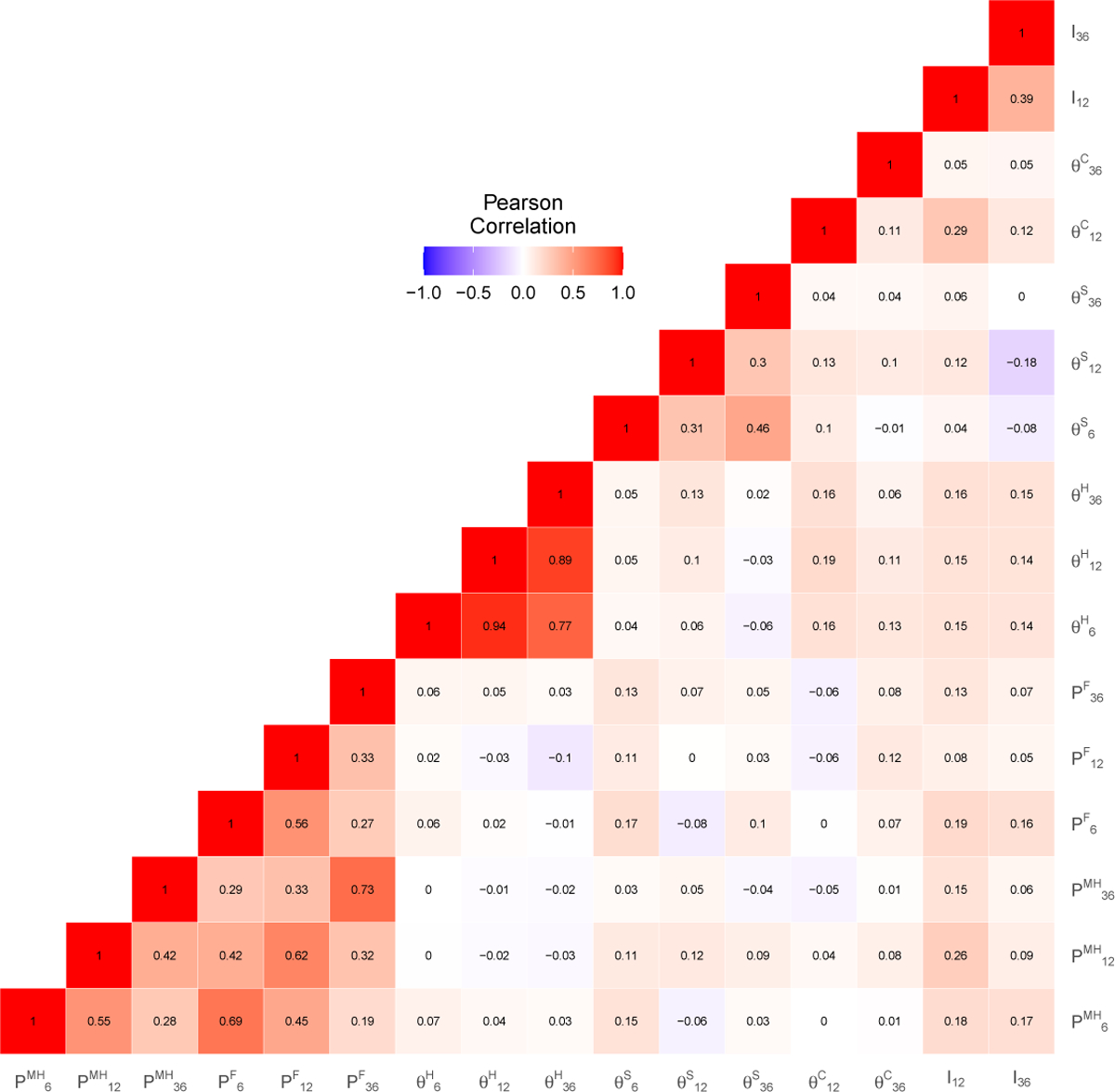
Estimated Latent Factor Correlations: Treatment Group
Figure A3:
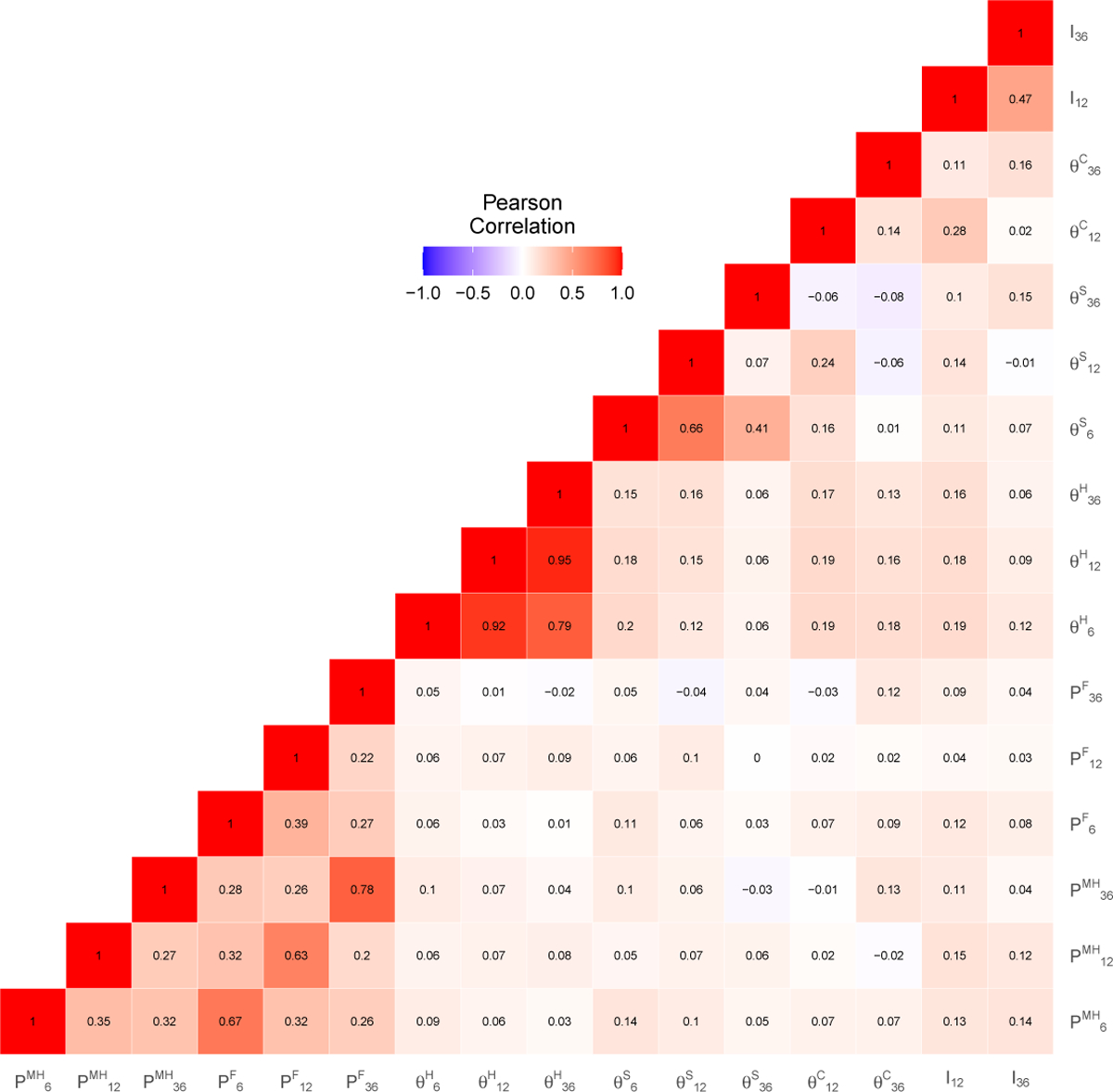
Estimated Latent Factor Correlations: Non-depressed Group
E. Reduced Form Outputs
Table A18:
Trajectory of Maternal Measures
| Measurement | Control | Treatment | Nondep. | Diff. (T-C) | Adjusted Beta | s.e. | p-val | N | |
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | Mean | ||||||
| 6 Months | |||||||||
| PHQ Total | 6.842 | 6.263 | 6.074 | 3.159 | −0.768 | −1.116 | 0.452 | 0.014 | 929 |
| PHQ Categorized | 929 | ||||||||
| Minimal (0–4) | 0.447 | 0.498 | 0.491 | 0.732 | 0.044 | 0.060 | 0.037 | 0.106 | 929 |
| Mild (5–9) | 0.241 | 0.429 | 0.265 | 0.180 | 0.024 | 0.035 | 0.034 | 0.301 | 929 |
| Moderate (10–14) | 0.149 | 0.357 | 0.122 | 0.049 | −0.027 | −0.042 | 0.035 | 0.228 | 929 |
| Moderately Severe (15–19) | 0.127 | 0.334 | 0.087 | 0.032 | −0.054 | −0.050 | 0.024 | 0.041 | 929 |
| Severe (20+) | 0.035 | 0.184 | 0.035 | 0.006 | 0.000 | −0.003 | 0.011 | 0.752 | 929 |
| PSS Total | 17.219 | 9.369 | 15.887 | 11.270 | −1.332 | −1.520 | 0.648 | 0.019 | 929 |
| Current Major Dep. Episode | 0.225 | 0.418 | 0.179 | 0.060 | −0.046 | −0.071 | 0.028 | 0.011 | 926 |
| Remission | 0.447 | 0.498 | 0.491 | 0.044 | 0.060 | 0.037 | 0.106 | 458 | |
| Recovery | 0.452 | 0.499 | 0.583 | 0.131 | 0.128 | 0.036 | 0.000 | 458 | |
| Mental Health Index | 0 | 1 | 0.142 | 0.516 | 0.142 | 0.205 | 0.056 | 0.000 | 929 |
| Mental Health Factor | 0 | 1 | 0.160 | 0.648 | 0.160 | 0.205 | 0.052 | 0.000 | 929 |
| WHODAS Total | 7.623 | 9.420 | 6.683 | 2.943 | −0.940 | −1.652 | 0.807 | 0.041 | 926 |
| Functioning Index | 0 | 1 | 0.136 | 0.459 | 0.136 | 0.184 | 0.079 | 0.019 | 929 |
| Functioning Factor | 0 | 1 | 0.108 | 0.547 | 0.108 | 0.182 | 0.075 | 0.015 | 929 |
| Mother Index | 0 | 1 | 0.168 | 0.531 | 0.168 | 0.211 | 0.061 | 0.001 | 929 |
| 12 Months | |||||||||
| PSS Total | 17.724 | 9.534 | 17.309 | 12.031 | −0.414 | −1.169 | 0.743 | 0.116 | 940 |
| Current Major Dep. Episode | 0.303 | 0.460 | 0.256 | 0.101 | −0.047 | −0.091 | 0.036 | 0.011 | 938 |
| Mental Health Index | 0 | 1 | 0.103 | 0.478 | 0.103 | 0.135 | 0.067 | 0.044 | 940 |
| Mental Health Factor | 0 | 1 | 0.098 | 0.650 | 0.098 | 0.170 | 0.054 | 0.002 | 940 |
| WHODAS Total | 7.175 | 9.008 | 5.843 | 3.333 | −1.332 | −1.878 | 0.731 | 0.010 | 940 |
| Functioning Index | 0 | 1 | 0.192 | 0.378 | 0.192 | 0.248 | 0.059 | 0.000 | 940 |
| Functioning Factor | 0 | 1 | 0.159 | 0.471 | 0.159 | 0.195 | 0.069 | 0.005 | 940 |
| Mother Index | 0 | 1 | 0.165 | 0.457 | 0.164 | 0.214 | 0.071 | 0.002 | 940 |
| 24 Months | |||||||||
| PHQ Total | 6.782 | 6.152 | 6.829 | 3.951 | 0.047 | 0.052 | 0.478 | 0.913 | 903 |
| PHQ Categorized | 903 | ||||||||
| Minimal (0–4) | 0.445 | 0.498 | 0.424 | 0.666 | −0.022 | −0.025 | 0.034 | 0.458 | 903 |
| Mild (5–9) | 0.291 | 0.455 | 0.333 | 0.218 | 0.042 | 0.028 | 0.034 | 0.414 | 903 |
| Moderate (10–14) | 0.141 | 0.349 | 0.129 | 0.072 | −0.012 | −0.001 | 0.029 | 0.966 | 903 |
| Moderately Severe (15–19) | 0.064 | 0.245 | 0.057 | 0.027 | −0.006 | 0.005 | 0.020 | 0.792 | 903 |
| Severe (20+) | 0.059 | 0.236 | 0.057 | 0.017 | −0.002 | −0.007 | 0.017 | 0.692 | 903 |
| PSS Total | 14.027 | 8.257 | 15.724 | 10.645 | 1.697 | 1.129 | 0.633 | 0.075 | 903 |
| Current Major Dep. Episode | 0.251 | 0.435 | 0.254 | 0.106 | 0.002 | 0.012 | 0.033 | 0.713 | 900 |
| Mental Health Index | 0 | 1 | −0.139 | 0.328 | −0.139 | −0.033 | 0.051 | 0.515 | 903 |
| Mental Health Factor | 0 | 1 | 0.028 | 0.532 | 0.028 | −0.002 | 0.057 | 0.970 | 903 |
| WHODAS Total | 7.532 | 8.476 | 7.757 | 4.230 | 0.225 | 0.503 | 0.648 | 0.437 | 903 |
| Functioning Index | 0 | 1 | −0.087 | 0.303 | −0.087 | −0.095 | 0.077 | 0.219 | 903 |
| Functioning Factor | 0 | 1 | −0.013 | 0.406 | −0.013 | −0.036 | 0.072 | 0.616 | 903 |
| Mother Index | 0 | 1 | −0.170 | 0.302 | −0.170 | −0.071 | 0.061 | 0.240 | 903 |
| 36 Months | |||||||||
| PHQ Total | 6.481 | 6.254 | 5.845 | 3.441 | −0.637 | −1.737 | 0.505 | 0.001 | 889 |
| PHQ Categorized | 889 | ||||||||
| Minimal (0–4) | 0.509 | 0.501 | 0.534 | 0.730 | 0.025 | 0.071 | 0.039 | 0.067 | 889 |
| Mild (5–9) | 0.241 | 0.429 | 0.218 | 0.139 | −0.024 | −0.022 | 0.030 | 0.458 | 889 |
| Moderate (10–14) | 0.097 | 0.297 | 0.150 | 0.090 | 0.053 | 0.061 | 0.021 | 0.004 | 889 |
| Moderately Severe (15–19) | 0.106 | 0.309 | 0.068 | 0.034 | −0.039 | −0.056 | 0.021 | 0.009 | 889 |
| Severe (20+) | 0.046 | 0.211 | 0.029 | 0.006 | −0.017 | −0.055 | 0.019 | 0.004 | 889 |
| PSS Total | 14.931 | 9.731 | 13.971 | 9.857 | −0.960 | −2.855 | 0.885 | 0.001 | 889 |
| GAD Total | 5.542 | 6.437 | 4.644 | 3.028 | −0.899 | −2.571 | 0.632 | 0.000 | 623 |
| GAD Total > 10 | 0.165 | 0.372 | 0.113 | 0.070 | −0.052 | −0.089 | 0.038 | 0.019 | 623 |
| Current Major Dep. Episode | 0.213 | 0.410 | 0.160 | −0.102 | 0.043 | −0.119 | 0.035 | 0.001 | 889 |
| Mental Health Index | 0 | 1 | 0.168 | 0.425 | 0.168 | 0.325 | 0.090 | 0.000 | 889 |
| Mental Health Factor | 0 | 1 | 0.133 | 0.556 | 0.133 | 0.268 | 0.078 | 0.001 | 889 |
| WHODAS Total | 6.778 | 9.444 | 5.874 | 3.338 | −0.904 | −2.790 | 0.867 | 0.001 | 889 |
| Functioning Index | 0 | 1 | 0.066 | 0.317 | 0.066 | 0.220 | 0.074 | 0.003 | 889 |
| Functioning Factor | 0 | 1 | 0.112 | 0.376 | 0.112 | 0.287 | 0.081 | 0.000 | 889 |
| Mother Index | 0 | 1 | 0.128 | 0.372 | 0.128 | 0.291 | 0.092 | 0.001 | 889 |
Note: Adjusted coefficients are obtained from the regressions of items on the treatment indicator and its interactions with the (demeaned) baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (splitted by gender), whether the index child is the first child, parental education (in years), asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. Robust and clustered standard errors at the cluster level are reported in the SE column. Reported p-values and standard errors refer to the adjusted beta coefficient. Anderson indices and factor scores are coded so that higher score always indicates better outcome. Mental Health Index : all PHQ items + all PSS items + all SCID items + all GAD items whenever available. Functioning Index : all WHODAS items. Mother Index : all PHQ items + all PSS items + all SCID items + all GAD items + all WHODAS items whenever available. Remission: Proportion of depressed at baseline having PHQ Total<5 at 3 or 6 months. Recovery: Proportion of depressed at baseline having PHQ Total<5 at 3 and 6 months.
Table A19:
Trajectory of Child Measures I
| Measurement | Control | Treatment | Nondep. | Diff.(T-C) | Adjusted Beta | s.e. | p-val | N | |
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | Mean | ||||||
| 6 Months | |||||||||
| Weight for age z-score | −0.857 | 1.140 | −0.903 | −0.892 | −0.046 | −0.140 | 0.123 | 0.254 | 923 |
| Height for age z-score | 0.086 | 1.688 | 0.278 | 0.053 | 0.192 | 0.063 | 0.177 | 0.720 | 920 |
| Head Circ. for age z-score | −0.809 | 1.044 | −0.882 | −0.813 | −0.073 | −0.133 | 0.099 | 0.178 | 923 |
| Child Health Index | 0 | 1 | 0.001 | −0.020 | 0.001 | −0.055 | 0.067 | 0.419 | 929 |
| Child Health Factor | 0 | 1 | −0.016 | −0.034 | −0.016 | −0.021 | 0.079 | 0.792 | 929 |
| ASQ-SE Total | 9.512 | 13.247 | 9.677 | 9.302 | 0.165 | 0.045 | 1.217 | 0.971 | 852 |
| ASQ-SE Self-regulation | 3.902 | 6.906 | 3.848 | 4.000 | −0.055 | −0.507 | 0.600 | 0.398 | 852 |
| ASQ-SE Communication | 0.366 | 1.711 | 0.461 | 0.547 | 0.095 | 0.061 | 0.196 | 0.757 | 852 |
| ASQ-SE Adaptive Func. | 3.805 | 6.275 | 4.078 | 3.651 | 0.273 | −0.579 | 0.521 | 0.266 | 852 |
| ASQ-SE Affect | 0.415 | 1.839 | 0.691 | 0.442 | 0.277 | 0.407 | 0.169 | 0.016 | 852 |
| ASQ-SE Interaction | 0.829 | 2.581 | 0.599 | 0.477 | −0.230 | −0.636 | 0.237 | 0.007 | 852 |
| Child SE Index | 0 | 1 | −0.034 | 0.041 | −0.034 | −0.049 | 0.073 | 0.495 | 852 |
| Child SE Factor | 0 | 1 | 0.167 | 0.100 | 0.167 | 0.187 | 0.056 | 0.001 | 852 |
| Child Index | 0 | 1 | −0.028 | 0.033 | −0.028 | −0.067 | 0.073 | 0.357 | 929 |
| 12 Months | |||||||||
| Weight for age z-score | −0.795 | 1.128 | −0.751 | −0.769 | 0.044 | 0.208 | 0.122 | 0.088 | 934 |
| Height for age z-score | −0.782 | 1.312 | −0.713 | −0.784 | 0.069 | 0.119 | 0.108 | 0.273 | 934 |
| Head Circ. for age z-score | −0.849 | 1.000 | −0.951 | −0.911 | −0.102 | −0.110 | 0.095 | 0.247 | 938 |
| Child Health Index | 0 | 1 | 0.012 | −0.016 | 0.012 | −0.031 | 0.063 | 0.623 | 940 |
| Child Health Factor | 0 | 1 | 0.044 | 0.035 | 0.044 | 0.019 | 0.070 | 0.784 | 940 |
| ASQ-SE Total | 11.689 | 13.958 | 9.731 | 10.112 | −1.958 | −1.795 | 1.002 | 0.073 | 940 |
| ASQ-SE Self-regulation | 5.022 | 8.799 | 3.655 | 4.427 | −1.367 | −1.633 | 0.604 | 0.007 | 940 |
| ASQ-SE Communication | 0.504 | 2.117 | 0.717 | 0.450 | 0.213 | 0.474 | 0.205 | 0.021 | 940 |
| ASQ-SE Adaptive Func. | 5.219 | 6.240 | 4.596 | 4.233 | −0.623 | −0.450 | 0.415 | 0.278 | 940 |
| ASQ-SE Affect | 0.307 | 1.452 | 0.224 | 0.368 | −0.083 | 0.026 | 0.120 | 0.827 | 940 |
| ASQ-SE Interaction | 0.439 | 1.825 | 0.359 | 0.317 | −0.080 | −0.143 | 0.117 | 0.219 | 940 |
| Child SE Index | 0 | 1 | 0.106 | 0.050 | 0.106 | 0.105 | 0.057 | 0.064 | 940 |
| Child SE Factor | 0 | 1 | 0.417 | 0.315 | 0.417 | 0.389 | 0.070 | 0.000 | 940 |
| Bayley Cognitive (scaled) | 9.196 | 2.249 | 9.276 | 9.430 | 0.081 | 0.022 | 0.182 | 0.904 | 923 |
| Bayley Receptive (scaled) | 7.942 | 1.373 | 7.949 | 7.969 | 0.007 | −0.141 | 0.111 | 0.205 | 923 |
| Bayley Expressive (scaled) | 9.076 | 1.634 | 8.954 | 9.212 | −0.122 | −0.145 | 0.154 | 0.346 | 923 |
| Bayley Fine motor (scaled) | 9.036 | 1.724 | 8.908 | 9.012 | −0.128 | −0.265 | 0.170 | 0.118 | 923 |
| Bayley Gross motor (scaled) | 8.209 | 2.217 | 8.120 | 8.096 | −0.089 | 0.065 | 0.221 | 0.768 | 923 |
| Child Cog Index | 0 | 1 | −0.038 | 0.038 | −0.038 | −0.050 | 0.070 | 0.471 | 940 |
| Child Cog Factor | 0 | 1 | −0.059 | 0.069 | −0.059 | −0.080 | 0.083 | 0.334 | 940 |
| Child Index | 0 | 1 | 0.096 | 0.051 | 0.096 | 0.069 | 0.050 | 0.169 | 940 |
Note: SE=socioemotional skills. Adjusted coefficients are obtained from the regressions of items on the treatment indicator and its interactions with (demeaned) baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. All estimations control for child gender and age (in days). Robust and clustered standard errors at the cluster level are reported in the SE column. Reported p-values and standard errors refer to the adjusted beta coefficient. Anderson indices and factor scores are coded so that higher score always indicates better outcome. Health Index : weight for age + height for age + head circumference for age z-scores. SE index : all ASQ-SE items. Cog Index : all Bayley-III subscales. Child Index : all anthropometrics + all ASQ-SE items + all Bayley-III items whenever available.
Table A20:
Trajectory of Child Measures II
| Measurement | Control | Treatment | Nondep. | Diff.(T-C) | Adjusted Beta | s.e. | p-val | N | |
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | Mean | ||||||
| 24 Months | |||||||||
| Weight for age z-score | −0.911 | 1.045 | −1.003 | −0.847 | −0.092 | −0.058 | 0.077 | 0.453 | 895 |
| Height for age z-score | −1.149 | 1.183 | −1.133 | −1.045 | 0.017 | −0.007 | 0.099 | 0.941 | 900 |
| Head Circ. for age z-score | −0.852 | 0.875 | −0.975 | −0.964 | −0.123 | −0.166 | 0.083 | 0.044 | 901 |
| Child Health Index | 0 | 1 | −0.097 | 0.004 | −0.097 | −0.082 | 0.077 | 0.290 | 903 |
| Child Health Factor | 0 | 1 | −0.130 | 0.053 | −0.130 | −0.100 | 0.083 | 0.227 | 903 |
| ASQ-SE Total | 12.237 | 23.633 | 13.900 | 15.764 | 1.662 | 1.232 | 1.346 | 0.360 | 899 |
| ASQ-SE Self-regulation | 2.591 | 5.623 | 2.738 | 2.717 | 0.147 | 0.144 | 0.334 | 0.667 | 903 |
| ASQ-SE Compliance | 0.182 | 1.339 | 0.286 | 0.486 | 0.104 | 0.112 | 0.104 | 0.284 | 903 |
| ASQ-SE Communication | 0.841 | 4.065 | 0.833 | 1.438 | −0.008 | 0.028 | 0.245 | 0.910 | 903 |
| ASQ-SE Adaptive Func. | 1.250 | 3.046 | 1.286 | 1.522 | 0.036 | −0.166 | 0.201 | 0.408 | 903 |
| ASQ-SE Autonomy | 0.250 | 1.528 | 0.381 | 0.581 | 0.131 | 0.122 | 0.097 | 0.211 | 903 |
| ASQ-SE Affect | 0.932 | 3.533 | 0.952 | 1.353 | 0.021 | −0.026 | 0.283 | 0.925 | 903 |
| ASQ-SE Interaction | 5.982 | 9.841 | 7.225 | 7.516 | 1.243 | 1.150 | 0.615 | 0.061 | 899 |
| Child SE Index | 0 | 1 | −0.043 | −0.162 | −0.043 | 0.054 | 0.071 | 0.453 | 903 |
| Child SE Factor | 0 | 1 | −0.050 | −0.217 | −0.050 | −0.065 | 0.067 | 0.334 | 903 |
| Child Index | 0 | 1 | −0.071 | −0.128 | −0.071 | 0.030 | 0.074 | 0.681 | 903 |
| 36 Months | |||||||||
| Weight for age z-score | −0.951 | 1.030 | −1.056 | −0.939 | −0.105 | −0.160 | 0.098 | 0.101 | 881 |
| Height for age z-score | −0.846 | 1.012 | −0.925 | −0.778 | −0.079 | −0.176 | 0.123 | 0.152 | 885 |
| Child Health Index | 0 | 1 | −0.099 | 0.045 | −0.099 | −0.120 | 0.090 | 0.182 | 889 |
| Child Health Factor | 0 | 1 | −0.137 | 0.041 | −0.137 | −0.166 | 0.088 | 0.060 | 889 |
| ASQ-SE Total | 41.181 | 19.526 | 41.189 | 38.576 | 0.009 | −1.450 | 1.637 | 0.376 | 889 |
| ASQ-SE Self-regulation | 19.630 | 10.120 | 18.689 | 17.944 | −0.940 | −1.321 | 0.732 | 0.071 | 889 |
| ASQ-SE Compliance | 0.602 | 2.071 | 0.728 | 0.685 | 0.126 | 0.136 | 0.196 | 0.486 | 889 |
| ASQ-SE Communication | 0.741 | 2.294 | 0.947 | 0.642 | 0.206 | −0.117 | 0.260 | 0.653 | 889 |
| ASQ-SE Adaptive Func. | 2.940 | 4.874 | 3.617 | 3.062 | 0.677 | 0.312 | 0.623 | 0.616 | 889 |
| ASQ-SE Autonomy | 10.069 | 2.872 | 9.515 | 9.839 | −0.555 | −0.382 | 0.207 | 0.065 | 889 |
| ASQ-SE Affect | 0.810 | 3.150 | 0.801 | 0.450 | −0.009 | −0.223 | 0.380 | 0.557 | 889 |
| ASQ-SE Interaction | 6.389 | 5.491 | 6.893 | 5.953 | 0.504 | 0.143 | 0.275 | 0.603 | 889 |
| SDQ Total | 14.718 | 6.127 | 14.733 | 13.687 | 0.015 | 0.262 | 0.331 | 0.428 | 889 |
| Boi Total | 18.617 | 11.174 | 18.124 | 20.021 | −0.493 | 0.291 | 0.357 | 0.415 | 889 |
| Child SE Index | 0 | 1 | −0.022 | 0.240 | −0.022 | 0.012 | 0.076 | 0.875 | 889 |
| Child SE Factor | 0 | 1 | 0.058 | 0.108 | 0.058 | 0.063 | 0.075 | 0.400 | 889 |
| Bayley Receptive (scaled) | 9.977 | 2.600 | 10.417 | 10.413 | 0.440 | 0.390 | 0.206 | 0.058 | 886 |
| Bayley Fine motor (scaled) | 11.377 | 4.117 | 11.422 | 11.308 | 0.045 | 0.041 | 0.286 | 0.885 | 886 |
| Child Cog Index | 0 | 1 | 0.092 | 0.074 | 0.092 | 0.090 | 0.074 | 0.225 | 889 |
| Child Cog Factor | 0 | 1 | 0.047 | −0.020 | 0.047 | 0.065 | 0.075 | 0.386 | 889 |
| Child Index | 0 | 1 | −0.034 | 0.242 | −0.034 | −0.005 | 0.079 | 0.953 | 889 |
Note: SE=socioemotional skills. Adjusted coefficients are obtained from the regressions of items on the treatment indicator and its interactions with (demeaned) baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. All estimations control for child gender and age (in days). Robust and clustered standard errors at the cluster level are reported in the SE column. Reported p-values and standard errors refer to the adjusted beta coefficient. Anderson indices and factor scores are coded so that higher score always indicates better outcome. Health Index : weight for age + height for age + head circumference for age z-scores. SE index : all ASQ-SE items + all SDQ items + all Boi items. Cog Index : all Bayley-III subscales. Child Index : all anthropometrics + all ASQ-SE items + all SDQ items + all Bayley-III items whenever available.
Table A21:
Trajectory of Parental Investment
| Measurement | Control | Treatment | Nondep. | Diff. (T-C) | Adjusted Beta | s.e. | p-val | N | |
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | Mean | ||||||
| 6 Months | |||||||||
| MPAS Total | 86.354 | 6.146 | 86.166 | 87.397 | −0.188 | 0.302 | 0.624 | 0.629 | 929 |
| MSES Total | 36.886 | 3.710 | 37.265 | 37.726 | 0.379 | 0.229 | 0.264 | 0.387 | 929 |
| Investment Index | 0 | 1 | 0.083 | 0.180 | 0.083 | 0.095 | 0.065 | 0.145 | 929 |
| Investment Factor | 0 | 1 | 0.060 | 0.417 | 0.060 | 0.076 | 0.057 | 0.187 | 929 |
| 12 Months | |||||||||
| HOME Total | 30.680 | 5.683 | 31.099 | 32.419 | 0.419 | 0.639 | 0.499 | 0.200 | 940 |
| HOME Responsivity | 9.732 | 1.434 | 9.865 | 9.787 | 0.133 | 0.226 | 0.114 | 0.047 | 940 |
| HOME Acceptance | 6.088 | 1.389 | 6.224 | 6.192 | 0.136 | 0.152 | 0.126 | 0.226 | 940 |
| HOME Organization | 3.434 | 1.417 | 3.556 | 3.775 | 0.122 | 0.153 | 0.142 | 0.281 | 940 |
| HOME Learning Mat. | 4.728 | 2.643 | 4.798 | 5.487 | 0.070 | 0.176 | 0.256 | 0.493 | 940 |
| HOME Involvement | 3.886 | 1.453 | 3.892 | 4.264 | 0.006 | 0.001 | 0.128 | 0.995 | 940 |
| HOME Variety | 2.811 | 0.582 | 2.762 | 2.914 | −0.049 | −0.069 | 0.066 | 0.298 | 940 |
| Investment Index | 0 | 1 | 0.131 | 0.262 | 0.131 | 0.142 | 0.075 | 0.059 | 940 |
| Investment Factor | 0 | 1 | 0.062 | 0.448 | 0.062 | 0.075 | 0.086 | 0.382 | 940 |
| 24 Months | |||||||||
| OMCI Total | 37.374 | 4.641 | 37.074 | 38.161 | −0.267 | −0.146 | 0.409 | 0.721 | 885 |
| Investment Index | 0 | 1 | −0.076 | 0.166 | −0.076 | −0.045 | 0.084 | 0.592 | 889 |
| Investment Factor | 0 | 1 | 0.012 | 0.035 | 0.012 | −0.031 | 0.083 | 0.710 | 889 |
| 36 Months | |||||||||
| HOME Total | 37.347 | 4.494 | 37.607 | 38.582 | 0.260 | 0.279 | 0.366 | 0.446 | 889 |
| HOME Responsivity | 10.472 | 0.899 | 10.437 | 10.497 | −0.035 | −0.040 | 0.065 | 0.535 | 889 |
| HOME Acceptance | 6.759 | 1.204 | 6.898 | 6.919 | 0.139 | 0.173 | 0.095 | 0.068 | 889 |
| HOME Organization | 5.028 | 0.935 | 5.049 | 5.148 | 0.021 | −0.002 | 0.075 | 0.982 | 889 |
| HOME Learning Mat. | 6.435 | 2.451 | 6.505 | 7.004 | 0.070 | 0.134 | 0.222 | 0.546 | 889 |
| HOME Involvement | 5.065 | 1.303 | 5.121 | 5.313 | 0.057 | 0.039 | 0.090 | 0.665 | 889 |
| HOME Variety | 3.588 | 0.847 | 3.597 | 3.702 | 0.009 | −0.025 | 0.052 | 0.625 | 889 |
| OMCI Total | 40.958 | 3.992 | 41.362 | 41.353 | 0.403 | 0.261 | 0.390 | 0.503 | 886 |
| Investment Index | 0 | 1 | 0.060 | 0.179 | 0.060 | 0.079 | 0.071 | 0.264 | 889 |
| Investment Factor | 0 | 1 | 0.067 | 0.361 | 0.067 | 0.111 | 0.076 | 0.143 | 889 |
Note: MPAS : Maternal Postnatal Attachment Scale, MSES : Maternal Self-Efficacy Scale, OMCI: Observation for Mother Child Interaction. Adjusted coefficients are obtained from the regressions of items on the treatment indicator and its interactions with the (demeaned) baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. All estimations control for child gender and age (in days). Robust and clustered standard errors at the cluster level are reported in the SE column. Reported p-values and standard errors refer to the adjusted beta coefficient. Anderson indices and factor scores are coded so that higher score always indicates better outcome. Investment Index : all MPAS items +all MSES items at 6 months, all HOME items at 12 and 36 months, all OMCI items at 24 months.
Table A22:
Trajectory of Standardized Summary Indices
| Measurement | Control | Treatment | Nondep. | Adjusted Beta | s.e. | p-val | N | |
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | Mean | |||||
| Maternal Factor Scores | ||||||||
| Mental Health (6 months) | 0 | 1 | 0.160 | 0.648 | 0.205 | 0.052 | 0.000 | 929 |
| Mental Health (12 months) | 0 | 1 | 0.098 | 0.650 | 0.170 | 0.054 | 0.002 | 940 |
| Mental Health (36 months) | 0 | 1 | 0.133 | 0.556 | 0.268 | 0.078 | 0.001 | 889 |
| Functioning (6 months) | 0 | 1 | 0.108 | 0.547 | 0.182 | 0.075 | 0.015 | 929 |
| Functioning (12 months) | 0 | 1 | 0.159 | 0.471 | 0.195 | 0.069 | 0.005 | 940 |
| Functioning (36 months) | 0 | 1 | 0.112 | 0.376 | 0.287 | 0.081 | 0.000 | 889 |
| Child Factor Scores | ||||||||
| Physical Health (6 months) | 0 | 1 | −0.016 | −0.034 | −0.021 | 0.079 | 0.792 | 929 |
| Physical Health (12 months) | 0 | 1 | 0.044 | 0.035 | 0.019 | 0.070 | 0.784 | 940 |
| Physical Health (36 months) | 0 | 1 | −0.137 | 0.041 | −0.166 | 0.088 | 0.060 | 889 |
| SE Skills (6 months) | 0 | 1 | 0.167 | 0.100 | 0.187 | 0.056 | 0.001 | 940 |
| SE Skills (12 months) | 0 | 1 | 0.417 | 0.315 | 0.389 | 0.070 | 0.000 | 940 |
| SE Skills (36 months) | 0 | 1 | 0.058 | 0.108 | 0.063 | 0.075 | 0.400 | 889 |
| Cognition (12 months) | 0 | 1 | −0.059 | 0.069 | −0.080 | 0.083 | 0.334 | 940 |
| Cognition (36 months) | 0 | 1 | 0.047 | −0.020 | 0.065 | 0.075 | 0.386 | 889 |
| Investment Factor Scores | ||||||||
| Investment (12 months) | 0 | 1 | 0.062 | 0.448 | 0.075 | 0.086 | 0.382 | 940 |
| Investment (36 months) | 0 | 1 | 0.067 | 0.361 | 0.111 | 0.076 | 0.143 | 889 |
SE skills = socioemotional skills. Factor scores are standardized at each time point to have mean 0 and SD 1 in the control group. The first two columns report the mean and standard deviation of the outcome variables in the control group. The following columns report the means for the treatment group and the group of mothers who were non-depressed at baseline (Nondep.). Adjusted Beta coefficients are obtained from the regressions of items on the treatment indicator and its interactions with the (demeaned) baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset-based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. All estimations control for child gender and age (in days). Standard errors clustered at the village-cluster level are reported in the s.e. column. Reported p-values and standard errors refer to the adjusted beta coefficient. N reports the number of observations of each analysis. Factor scores are coded so that a higher score always indicates a better outcome.
F. Treatment Effects on the Fixed Subset
The following tables present the estimated treatment effects for the fixed subset of mothers who were present at 6, 12, 24, and 36 months follow-up waves. (N=771).
Table A23:
Trajectory of Maternal Measures for the Fixed Subset (N=771)
| Measurement | Control | Treatment | Nondep. | Diff.(T-C) | Adjusted Beta | s.e. | p-val | |
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | Mean | |||||
| 6 Months | ||||||||
| PHQ Total | 6.590 | 6.141 | 5.995 | 3.261 | −0.596 | −0.897 | 0.404 | 0.026 |
| PHQ Categorized | ||||||||
| Minimal (0–4) | 0.463 | 0.500 | 0.516 | 0.722 | 0.054 | 0.072 | 0.031 | 0.020 |
| Mild (5–9) | 0.234 | 0.425 | 0.255 | 0.188 | 0.021 | 0.017 | 0.034 | 0.610 |
| Moderate (10–14) | 0.144 | 0.352 | 0.109 | 0.045 | −0.035 | −0.039 | 0.029 | 0.177 |
| Moderately Severe (15–19) | 0.133 | 0.340 | 0.082 | 0.038 | −0.051 | −0.048 | 0.022 | 0.030 |
| Severe (20+) | 0.027 | 0.161 | 0.038 | 0.008 | 0.011 | −0.003 | 0.012 | 0.825 |
| PSS Total | 16.761 | 9.334 | 15.701 | 11.318 | −1.060 | −1.647 | 0.537 | 0.002 |
| Current Major Dep. Episode | 0.209 | 0.407 | 0.168 | 0.065 | −0.040 | −0.071 | 0.025 | 0.005 |
| Remission | 0.463 | 0.500 | 0.516 | 0.054 | 0.072 | 0.031 | 0.020 | |
| Recovery | 0.457 | 0.500 | 0.592 | 0.135 | 0.147 | 0.032 | 0.000 | |
| Mental Health Index | 0 | 1 | 0.098 | 0.420 | 0.098 | 0.156 | 0.078 | 0.045 |
| Mental Health Factor | 0 | 1 | 0.142 | 0.580 | 0.142 | 0.196 | 0.059 | 0.001 |
| WHODAS Total | 7.574 | 9.551 | 6.337 | 2.940 | −1.238 | −1.820 | 0.711 | 0.010 |
| Functioning Index | 0 | 1 | 0.182 | 0.433 | 0.182 | 0.225 | 0.080 | 0.005 |
| Functioning Factor | 0 | 1 | 0.127 | 0.514 | 0.127 | 0.190 | 0.073 | 0.010 |
| Mother Index | 0 | 1 | 0.159 | 0.449 | 0.159 | 0.210 | 0.079 | 0.008 |
| 12 Months | ||||||||
| PSS Total | 16.851 | 9.384 | 16.897 | 11.935 | 0.046 | −0.282 | 0.647 | 0.663 |
| Current Major Dep. Episode | 0.266 | 0.443 | 0.266 | 0.093 | 0.000 | −0.008 | 0.026 | 0.746 |
| Mental Health Index | 0 | 1 | 0.053 | 0.392 | 0.053 | 0.045 | 0.058 | 0.444 |
| Mental Health Factor | 0 | 1 | 0.033 | 0.572 | 0.033 | 0.026 | 0.053 | 0.624 |
| WHODAS Total | 6.590 | 8.605 | 5.630 | 3.135 | −0.960 | −1.713 | 0.562 | 0.002 |
| Functioning Index | 0 | 1 | 0.194 | 0.379 | 0.194 | 0.280 | 0.064 | 0.000 |
| Functioning Factor | 0 | 1 | 0.116 | 0.428 | 0.116 | 0.186 | 0.057 | 0.001 |
| Mother Index | 0 | 1 | 0.174 | 0.397 | 0.174 | 0.208 | 0.064 | 0.001 |
| 24 Months | ||||||||
| PHQ Total | 6.697 | 5.823 | 6.848 | 3.810 | 0.151 | −0.117 | 0.418 | 0.779 |
| PHQ Categorized | ||||||||
| Minimal (0–4) | 0.431 | 0.497 | 0.435 | 0.682 | 0.004 | 0.028 | 0.033 | 0.396 |
| Mild (5–9) | 0.303 | 0.461 | 0.315 | 0.203 | 0.012 | −0.020 | 0.034 | 0.548 |
| Moderate (10–14) | 0.154 | 0.362 | 0.136 | 0.078 | −0.018 | −0.007 | 0.028 | 0.813 |
| Moderately Severe (15–19) | 0.064 | 0.245 | 0.054 | 0.025 | −0.009 | −0.005 | 0.022 | 0.836 |
| Severe (20+) | 0.048 | 0.214 | 0.060 | 0.013 | −0.012 | 0.004 | 0.011 | 0.735 |
| PSS Total | 13.489 | 7.946 | 15.870 | 10.426 | 2.380 | 1.712 | 0.658 | 0.009 |
| Current Major Dep. Episode | 0.246 | 0.432 | 0.246 | 0.101 | 0.000 | 0.004 | 0.033 | 0.396 |
| Mental Health Index | 0 | 1 | −0.178 | 0.334 | −0.178 | −0.081 | 0.062 | 0.195 |
| Mental Health Factor | 0 | 1 | 0.005 | 0.515 | 0.005 | −0.009 | 0.062 | 0.889 |
| WHODAS Total | 7.339 | 8.350 | 7.913 | 3.892 | 0.514 | 0.561 | 0.581 | 0.335 |
| Functioning Index | 0 | 1 | −0.039 | 0.390 | −0.039 | −0.059 | 0.073 | 0.422 |
| Functioning Factor | 0 | 1 | −0.050 | 0.449 | −0.050 | −0.057 | 0.067 | 0.395 |
| Mother Index | 0 | 1 | −0.169 | 0.360 | −0.169 | −0.096 | 0.067 | 0.152 |
| 36 Months | ||||||||
| PHQ Total | 5.995 | 5.889 | 5.918 | 3.461 | −0.076 | −0.970 | 0.411 | 0.018 |
| PHQ Categorized | ||||||||
| Minimal (0–4) | 0.537 | 0.500 | 0.527 | 0.734 | −0.010 | 0.036 | 0.034 | 0.290 |
| Mild (5–9) | 0.239 | 0.428 | 0.217 | 0.128 | −0.022 | −0.014 | 0.031 | 0.643 |
| Moderate (10–14) | 0.090 | 0.288 | 0.152 | 0.095 | 0.062 | 0.051 | 0.018 | 0.005 |
| Moderately Severe (15–19) | 0.101 | 0.302 | 0.071 | 0.035 | −0.030 | −0.062 | 0.016 | 0.000 |
| Severe (20+) | 0.032 | 0.176 | 0.033 | 0.008 | 0.001 | −0.011 | 0.014 | 0.459 |
| PSS Total | 14.399 | 9.681 | 13.832 | 9.817 | −0.567 | −1.967 | 0.770 | 0.011 |
| GAD Total | 5.188 | 6.162 | 4.607 | 3.068 | −0.581 | −1.917 | 0.503 | 0.000 |
| GAD Total > 10 | 0.176 | 0.381 | 0.130 | 0.085 | −0.045 | −0.072 | 0.033 | 0.027 |
| Current Major Dep. Episode | 0.191 | 0.395 | 0.158 | 0.093 | −0.034 | −0.096 | 0.029 | 0.001 |
| Mental Health Index | 0 | 1 | 0.163 | 0.401 | 0.163 | 0.306 | 0.096 | 0.001 |
| Mental Health Factor | 0 | 1 | 0.051 | 0.451 | 0.051 | 0.190 | 0.071 | 0.008 |
| WHODAS Total | 5.915 | 8.576 | 5.815 | 3.391 | −0.100 | −1.551 | 0.626 | 0.013 |
| Functioning Index | 0 | 1 | 0.009 | 0.281 | 0.009 | 0.161 | 0.076 | 0.033 |
| Functioning Factor | 0 | 1 | 0.017 | 0.310 | 0.017 | 0.186 | 0.073 | 0.011 |
| Mother Index | 0 | 1 | 0.159 | 0.384 | 0.159 | 0.325 | 0.096 | 0.001 |
Note: Table shows treatment effects on the reported items and Anderson indices for the subset of mothers who were present at all four waves (N=771). Adjusted coefficients are obtained from the regressions of items on the treatment indicator and its interactions with (demeaned) baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. Robust and clustered standard errors at the cluster level are reported in the SE column. Reported p-values and standard errors refer to the adjusted beta coefficient. Anderson indices and factor scores are coded so that higher score always indicates better outcome. Mental Health Index : all PHQ items + all PSS items + all SCID items + all GAD items whenever available. Functioning Index : all WHODAS items. Mother Index : all PHQ items + all PSS items + all SCID items + all GAD items + all WHODAS items whenever available. Remission: Proportion of depressed at baseline having PHQ Total<5 at 3 or 6 months. Recovery: Proportion of depressed at baseline having PHQ Total<5 at 3 and 6 months.
Table A24:
Trajectory of Child Measures for the Fixed Subset I (N=771)
| Measurement | Control | Treatment | Nondep. | Diff. (T-C) | Adjusted Beta | s.e | p-val | |
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | Mean | |||||
| 6 Months | ||||||||
| Weight for age z-score | −0.806 | 1.099 | −0.885 | −0.882 | −0.080 | −0.132 | 0.086 | 0.125 |
| Height for age z-score | 0.098 | 1.625 | 0.323 | 0.080 | 0.224 | 0.020 | 0.124 | 0.873 |
| Head Circ. for age z-score | −0.801 | 1.035 | −0.840 | −0.826 | −0.039 | −0.139 | 0.087 | 0.110 |
| Child Health Index | 0 | 1 | 0.027 | −0.040 | 0.027 | −0.090 | 0.075 | 0.229 |
| Child Health Factor | 0 | 1 | −0.012 | −0.068 | −0.012 | −0.090 | 0.076 | 0.234 |
| ASQ-SE Total | 9.940 | 13.777 | 9.600 | 9.288 | −0.340 | 0.533 | 1.270 | 0.674 |
| ASQ-SE Self-regulation | 4.077 | 7.085 | 3.857 | 4.000 | −0.220 | −0.092 | 0.647 | 0.888 |
| ASQ-SE Communication | 0.268 | 1.369 | 0.457 | 0.548 | 0.189 | 0.366 | 0.155 | 0.018 |
| ASQ-SE Adaptive Func. | 4.137 | 6.589 | 3.857 | 3.658 | −0.280 | −0.265 | 0.525 | 0.614 |
| ASQ-SE Affect | 0.387 | 1.730 | 0.714 | 0.411 | 0.327 | 0.542 | 0.164 | 0.001 |
| ASQ-SE Interaction | 0.893 | 2.698 | 0.543 | 0.397 | −0.350 | −0.538 | 0.251 | 0.032 |
| Child SE Index | 0 | 1 | 0.073 | 0.160 | 0.073 | 0.021 | 0.068 | 0.759 |
| Child SE Factor | 0 | 1 | 0.174 | 0.037 | 0.174 | 0.208 | 0.069 | 0.003 |
| Child Index | 0 | 1 | 0.080 | 0.152 | 0.080 | −0.001 | 0.066 | 0.987 |
| 12 Months | ||||||||
| Weight for age z-score | −0.797 | 1.154 | −0.736 | −0.778 | 0.061 | 0.079 | 0.096 | 0.409 |
| Height for age z-score | −0.817 | 1.308 | −0.726 | −0.765 | 0.092 | 0.051 | 0.084 | 0.544 |
| Head Circ. for age z-score | −0.819 | 1.000 | −0.951 | −0.936 | −0.132 | −0.224 | 0.085 | 0.009 |
| Child Health Index | 0 | 1 | −0.015 | −0.035 | −0.015 | −0.058 | 0.082 | 0.478 |
| Child Health Factor | 0 | 1 | 0.033 | −0.013 | 0.033 | 0.007 | 0.074 | 0.929 |
| ASQ Total | 11.489 | 14.373 | 9.538 | 9.737 | −1.951 | −1.949 | 0.949 | 0.040 |
| ASQ-SE Self-regulation | 5.226 | 8.967 | 3.451 | 4.060 | −1.815 | −2.126 | 0.579 | 0.000 |
| ASQ-SE Communication | 0.452 | 2.051 | 0.734 | 0.489 | 0.282 | 0.185 | 0.116 | 0.111 |
| ASQ-SE Adaptive Func. | 4.920 | 6.364 | 4.538 | 4.286 | −0.382 | 0.107 | 0.432 | 0.804 |
| ASQ-SE Affect | 0.293 | 1.385 | 0.190 | 0.326 | −0.102 | −0.160 | 0.119 | 0.177 |
| ASQ-SE Interaction | 0.372 | 1.674 | 0.408 | 0.276 | 0.035 | 0.079 | 0.121 | 0.515 |
| Child SE Index | 0 | 1 | 0.115 | 0.099 | 0.115 | 0.137 | 0.059 | 0.020 |
| Child SE Factor | 0 | 1 | 0.424 | 0.374 | 0.424 | 0.417 | 0.078 | 0.000 |
| Bayley Cognitive (scaled) | 9.414 | 2.150 | 9.339 | 9.466 | −0.075 | −0.058 | 0.215 | 0.786 |
| Bayley Receptive (scaled) | 8.032 | 1.347 | 7.983 | 7.959 | −0.049 | −0.109 | 0.095 | 0.252 |
| Bayley Expressive (scaled) | 9.215 | 1.513 | 9.006 | 9.244 | −0.209 | −0.242 | 0.131 | 0.065 |
| Bayley Fine motor (scaled) | 9.199 | 1.597 | 8.878 | 9.079 | −0.321 | −0.390 | 0.140 | 0.005 |
| Bayley Gross motor (scaled) | 8.333 | 2.107 | 8.206 | 8.206 | −0.128 | −0.159 | 0.203 | 0.433 |
| Child Cog Index | 0 | 1 | −0.121 | −0.038 | −0.121 | −0.165 | 0.095 | 0.082 |
| Child Cog Factor | 0 | 1 | −0.161 | −0.015 | −0.161 | −0.205 | 0.104 | 0.048 |
| Child Index | 0 | 1 | 0.082 | 0.079 | 0.082 | 0.074 | 0.057 | 0.196 |
Note: SE=socioemotional skills. Table shows treatment effects on the reported items and Anderson indices for the subset of mothers who were present at all four waves (N=771). Adjusted coefficients are obtained from the regressions of items on the treatment indicator and its interactions with (demeaned) baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. All estimations control for child gender and age (in days). Robust and clustered standard errors at the cluster level are reported in the SE column. Reported p-values and standard errors refer to the adjusted beta coefficient. Anderson indices and factor scores are coded so that higher score always indicates better outcome. Mental Health Index : all PHQ items + all PSS items + all SCID items + all GAD items whenever available. Physical Health Index : all WHODAS items. Mother Index : all PHQ items + all PSS items + all SCID items + all GAD items + all WHODAS items whenever available.
Table A25:
Trajectory of Child Measures for the Fixed Subset II (N=771)
| Measurement | Control | Treatment | Nondep. | Diff. (T-C) | Adjusted Beta | s.e. | p-val | |
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | Mean | |||||
| 24 Months | ||||||||
| Weight for age z-score | −0.861 | 1.010 | −1.007 | −0.844 | −0.146 | −0.146 | 0.073 | 0.045 |
| Height for age z-score | −1.097 | 1.223 | −1.146 | −0.994 | −0.050 | −0.066 | 0.095 | 0.485 |
| Head Circ. for age z-score | −0.782 | 0.874 | −0.938 | −0.956 | −0.156 | −0.230 | 0.085 | 0.007 |
| Child Health Index | 0 | 1 | −0.149 | −0.039 | −0.149 | −0.183 | 0.080 | 0.023 |
| Child Health Factor | 0 | 1 | −0.179 | −0.017 | −0.179 | −0.198 | 0.085 | 0.020 |
| ASQ-SE Total | 10.856 | 20.434 | 12.596 | 12.103 | 1.740 | 1.807 | 1.184 | 0.127 |
| ASQ-SE Self-regulation | 2.473 | 5.509 | 2.554 | 2.318 | 0.081 | 0.220 | 0.367 | 0.549 |
| ASQ-SE Compliance | 0.106 | 1.029 | 0.217 | 0.301 | 0.111 | 0.176 | 0.069 | 0.011 |
| ASQ-SE Communication | 0.665 | 3.539 | 0.571 | 0.777 | −0.094 | 0.047 | 0.187 | 0.801 |
| ASQ-SE Adaptive Func. | 1.170 | 2.918 | 1.277 | 1.103 | 0.107 | −0.045 | 0.250 | 0.856 |
| ASQ-SE Autonomy | 0.213 | 1.447 | 0.326 | 0.426 | 0.113 | 0.147 | 0.077 | 0.058 |
| ASQ-SE Affect | 0.771 | 3.114 | 0.761 | 0.802 | −0.010 | 0.008 | 0.248 | 0.973 |
| ASQ-SE Interaction | 5.321 | 8.561 | 6.694 | 6.247 | 1.373 | 1.347 | 0.526 | 0.011 |
| Child SE Index | 0 | 1 | 0.125 | 0.117 | 0.125 | 0.157 | 0.069 | 0.023 |
| Child SE Factor | 0 | 1 | −0.047 | −0.111 | −0.047 | −0.122 | 0.057 | 0.032 |
| Child Index | 0 | 1 | 0.085 | 0.111 | 0.085 | 0.109 | 0.072 | 0.133 |
| 36 Months | ||||||||
| Weight for age z-score | −0.916 | 1.016 | −1.058 | −0.967 | −0.141 | −0.167 | 0.100 | 0.095 |
| Height for age z-score | −0.859 | 1.020 | −0.919 | −0.788 | −0.061 | −0.091 | 0.103 | 0.375 |
| Child Health Index | 0 | 1 | −0.121 | −0.006 | −0.121 | −0.157 | 0.099 | 0.113 |
| Child Health Factor | 0 | 1 | −0.158 | −0.019 | −0.158 | −0.196 | 0.100 | 0.049 |
| ASQ-SE Total | 40.718 | 17.570 | 40.625 | 38.784 | −0.093 | −0.490 | 1.438 | 0.733 |
| ASQ-SE Self-regulation | 19.255 | 9.728 | 18.397 | 18.083 | −0.859 | −0.988 | 0.616 | 0.108 |
| ASQ-SE Compliance | 0.612 | 2.074 | 0.788 | 0.639 | 0.176 | 0.272 | 0.177 | 0.123 |
| ASQ-SE Communication | 0.691 | 2.206 | 0.761 | 0.614 | 0.069 | −0.009 | 0.265 | 0.974 |
| ASQ-SE Adaptive Func. | 2.952 | 4.646 | 3.451 | 2.982 | 0.499 | 0.204 | 0.506 | 0.688 |
| ASQ-SE Autonomy | 10.160 | 2.780 | 9.511 | 9.850 | −0.649 | −0.616 | 0.157 | 0.000 |
| ASQ-SE Affect | 0.612 | 2.375 | 0.842 | 0.414 | 0.231 | 0.415 | 0.249 | 0.095 |
| ASQ-SE Interaction | 6.436 | 5.429 | 6.875 | 6.203 | 0.439 | 0.232 | 0.383 | 0.545 |
| SDQ Total | 14.649 | 6.279 | 14.467 | 13.424 | −0.182 | 0.054 | 0.307 | 0.859 |
| Boi Total | 24.883 | 3.754 | 24.875 | 25.000 | −0.008 | −0.065 | 0.341 | 0.848 |
| Child SE Index | 0 | 1 | 0.102 | 0.254 | 0.102 | 0.087 | 0.089 | 0.324 |
| Child SE Factor | 0 | 1 | 0.038 | 0.133 | 0.038 | −0.012 | 0.073 | 0.869 |
| Bayley Receptive (scaled) | 10.016 | 2.593 | 10.412 | 10.303 | 0.396 | 0.332 | 0.229 | 0.148 |
| Bayley Fine motor (scaled) | 11.610 | 4.109 | 11.500 | 11.246 | −0.110 | −0.021 | 0.290 | 0.943 |
| Child Cog Index | 0 | 1 | 0.055 | −0.005 | 0.055 | 0.055 | 0.080 | 0.496 |
| Child Cog Factor | 0 | 1 | 0.016 | −0.085 | 0.016 | 0.039 | 0.079 | 0.624 |
| Child Index | 0 | 1 | 0.079 | 0.240 | 0.079 | 0.061 | 0.088 | 0.493 |
Note: SE=socioemotional skills. Table shows treatment effects on the reported items and Anderson indices for the subset of mothers who were present at all four waves (N=771). Adjusted coefficients are obtained from the regressions of items on the treatment indicator and its interactions with (demeaned) baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. All estimations control for child gender and age (in days). Robust and clustered standard errors at the cluster level are reported in the SE column. Reported p-values and standard errors refer to the adjusted beta coefficient. Anderson indices and factor scores are coded so that higher score always indicates better outcome. Mental Health Index : all PHQ items + all PSS items + all SCID items + all GAD items whenever available. Physical Health Index : all WHODAS items. Mother Index : all PHQ items + all PSS items + all SCID items + all GAD items + all WHODAS items whenever available.
Table A26:
Trajectory of Parental Investment for the Fixed Subset (N=771)
| Measurement | Control | Treatment | Nondep. | Diff. (T-C) | Adjusted Beta | s.e. | p-val | |
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | Mean | |||||
| 6 Months | ||||||||
| MPAS Total | 86.296 | 6.345 | 86.221 | 87.543 | −0.075 | 0.007 | 0.362 | 0.984 |
| MSES Total | 36.963 | 3.650 | 37.201 | 37.840 | 0.238 | 0.083 | 0.228 | 0.718 |
| Investment Index | 0 | 1 | 0.135 | 0.226 | 0.135 | 0.111 | 0.056 | 0.047 |
| Investment Factor | 0 | 1 | 0.039 | 0.417 | 0.039 | 0.034 | 0.049 | 0.485 |
| 12 Months | ||||||||
| HOME Total | 30.803 | 5.761 | 31.212 | 32.534 | 0.409 | 0.748 | 0.451 | 0.098 |
| HOME Responsivity | 9.644 | 1.504 | 9.853 | 9.810 | 0.210 | 0.244 | 0.128 | 0.056 |
| HOME Acceptance | 6.112 | 1.427 | 6.277 | 6.216 | 0.165 | 0.270 | 0.105 | 0.010 |
| HOME Organization | 3.505 | 1.358 | 3.489 | 3.772 | −0.016 | 0.000 | 0.105 | 0.998 |
| HOME Learning Mat. | 4.793 | 2.555 | 4.913 | 5.589 | 0.120 | 0.269 | 0.192 | 0.161 |
| HOME Involvement | 3.894 | 1.477 | 3.929 | 4.238 | 0.036 | 0.056 | 0.114 | 0.625 |
| HOME Variety | 2.856 | 0.523 | 2.750 | 2.910 | −0.106 | −0.091 | 0.068 | 0.179 |
| Investment Index | 0 | 1 | 0.153 | 0.281 | 0.153 | 0.158 | 0.099 | 0.112 |
| Investment Factor | 0 | 1 | 0.039 | 0.419 | 0.039 | 0.091 | 0.082 | 0.271 |
| 24 Months | ||||||||
| OMCI Total | 37.396 | 4.699 | 36.921 | 38.213 | −0.475 | −0.360 | 0.428 | 0.401 |
| Investment Index | 0 | 1 | −0.095 | 0.189 | −0.095 | −0.078 | 0.086 | 0.360 |
| Investment Factor | 0 | 1 | 0.006 | 0.100 | 0.006 | −0.028 | 0.082 | 0.736 |
| 36 Months | ||||||||
| HOME Total | 37.601 | 4.261 | 37.647 | 38.496 | 0.046 | 0.406 | 0.371 | 0.274 |
| HOME Responsivity | 10.473 | 0.933 | 10.418 | 10.486 | −0.055 | −0.055 | 0.089 | 0.536 |
| HOME Acceptance | 5.016 | 0.956 | 5.043 | 5.143 | 0.028 | 0.186 | 0.099 | 0.060 |
| HOME Organization | 5.016 | 0.956 | 5.043 | 5.143 | 0.028 | 0.082 | 0.063 | 0.197 |
| HOME Learning Mat. | 6.553 | 2.315 | 6.473 | 6.952 | −0.080 | 0.108 | 0.213 | 0.612 |
| HOME Involvement | 5.096 | 1.280 | 5.158 | 5.288 | 0.062 | 0.115 | 0.094 | 0.222 |
| HOME Variety | 3.638 | 0.851 | 3.625 | 3.719 | −0.013 | −0.029 | 0.049 | 0.548 |
| OMCI Total | 41.027 | 4.034 | 41.344 | 41.539 | 0.318 | 0.234 | 0.356 | 0.510 |
| Investment Index | 0 | 1 | 0.191 | 0.313 | 0.191 | 0.236 | 0.071 | 0.001 |
| Investment Factor | 0 | 1 | 0.0126 | 0.296 | 0.026 | 0.111 | 0.075 | 0.137 |
Note: MPAS : Maternal Postnatal Attachment Scale, MSES : Maternal Self-Efficacy Scale, OMCI: Observation for Mother Child Interaction. Adjusted coefficients are obtained from the regressions of items on the treatment indicator and its interactions with (demeaned) baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. All estimations control for child gender and age (in days). Robust and clustered standard errors at the cluster level are reported in the SE column. Reported p-values and standard errors refer to the adjusted beta coefficient. Anderson indices and factor scores are coded so that higher score always indicates better outcome. Investment Index : all MPAS items +all MSES items at 6 months, all HOME items at 12 and 36 months, all OMCI items at 24 months.
G. Randomization Inference
Table A27:
Randomization Inference on Aggregate Maternal Outcomes
| Adjusted Beta | s.e. | p-val | RI p-val | |
|---|---|---|---|---|
| Mental Health Factor (6m) | 0.205 | 0.052 | 0.000 | 0.003 |
| Functioning Factor (6m) | 0.182 | 0.075 | 0.015 | 0.038 |
| Mental Health Factor (12m) | 0.170 | 0.054 | 0.002 | 0.007 |
| Functioning Factor (12m) | 0.195 | 0.069 | 0.005 | 0.022 |
| Mental Health Factor (24m) | −0.002 | 0.057 | 0.970 | 0.967 |
| Functioning Factor (24m) | −0.036 | 0.072 | 0.616 | 0.665 |
| Mental Health Factor (36m) | 0.268 | 0.078 | 0.001 | 0.006 |
| Functioning Factor (36m) | 0.287 | 0.081 | 0.000 | 0.006 |
Note: p-values reported in the last column are computed using randomization inference based on Young (2019) with the randomization permuted at the cluster level.
Table A28:
Randomization Inference on Aggregate Child and Investment Outcomes
| Adjusted Beta | s.e. | p-val | RI p-val | |
|---|---|---|---|---|
| Child Health Factor (6m) | −0.021 | 0.079 | 0.792 | 0.811 |
| Child SE Factor (6m) | 0.187 | 0.056 | 0.001 | 0.007 |
| Investment Factor (6m) | 0.076 | 0.057 | 0.187 | 0.264 |
| Child Health Factor (12m) | 0.019 | 0.070 | 0.784 | 0.795 |
| Child SE Factor (12m) | 0.389 | 0.070 | 0.000 | 0.001 |
| Child Cog Factor (12m) | −0.080 | 0.083 | 0.334 | 0.411 |
| Investment Factor (12m) | 0.075 | 0.086 | 0.382 | 0.443 |
| Child Health Factor (24m) | −0.100 | 0.083 | 0.227 | 0.287 |
| Child SE Factor (24m) | −0.065 | 0.067 | 0.334 | 0.438 |
| Investment Factor (24m) | −0.031 | 0.083 | 0.710 | 0.744 |
| Child Health Factor (36m) | −0.166 | 0.088 | 0.060 | 0.104 |
| Child SE Factor (36m) | 0.063 | 0.075 | 0.400 | 0.464 |
| Child Cog Factor (36m) | 0.065 | 0.075 | 0.386 | 0.422 |
| Investment Factor (36m) | 0.111 | 0.076 | 0.143 | 0.222 |
Note: p-values reported in the last column are computed using randomization inference based on Young (2019) with the randomization permuted at the cluster level.
H. Heterogeneity in Treatment Effects
Figure A4:
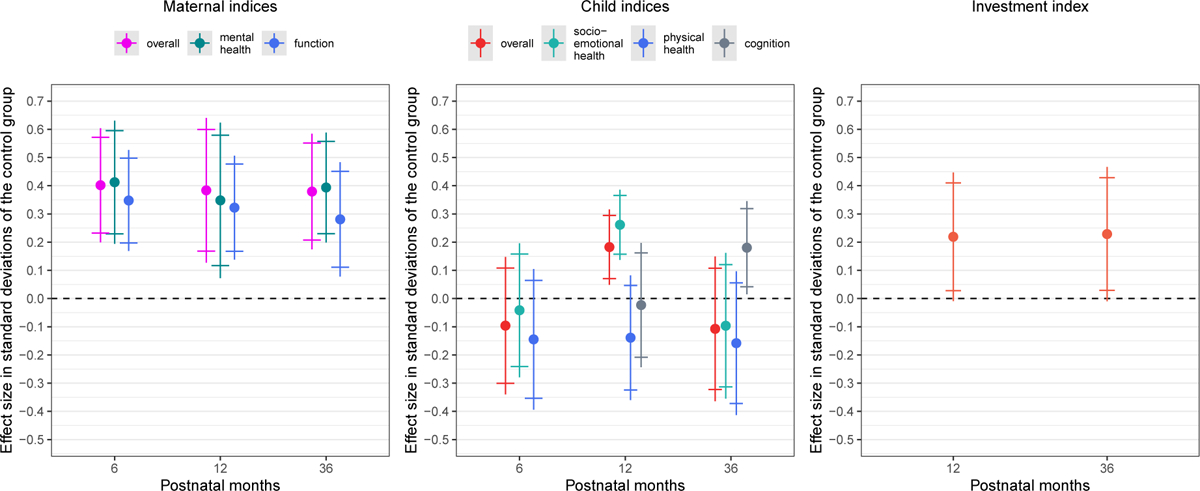
Coefficient Plots of Indices (Boys)
Figure A5:
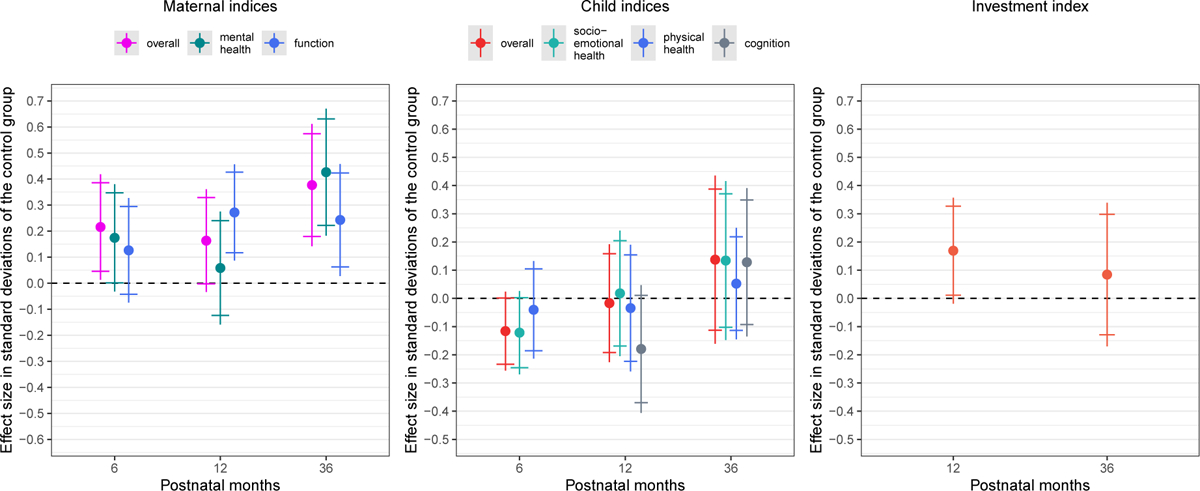
Coefficient Plots of Indices (Girls)
Figure A6:
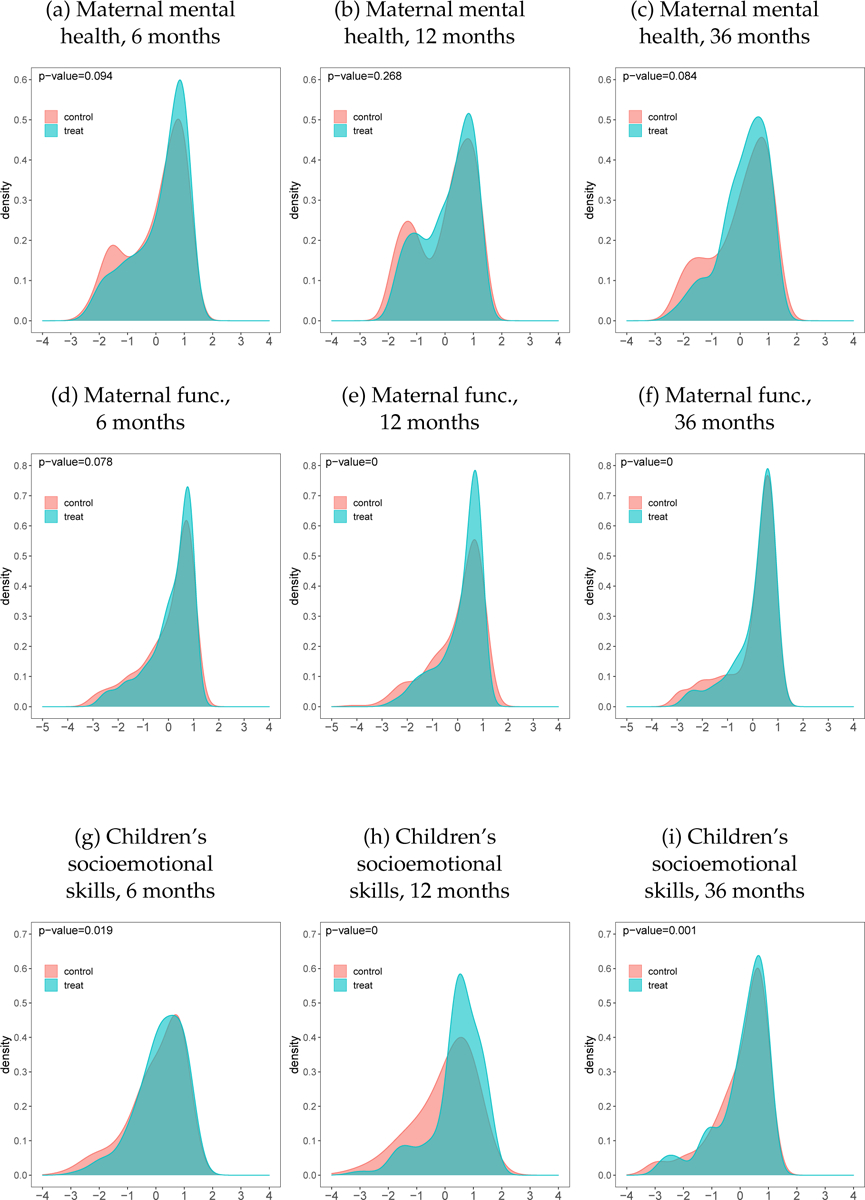
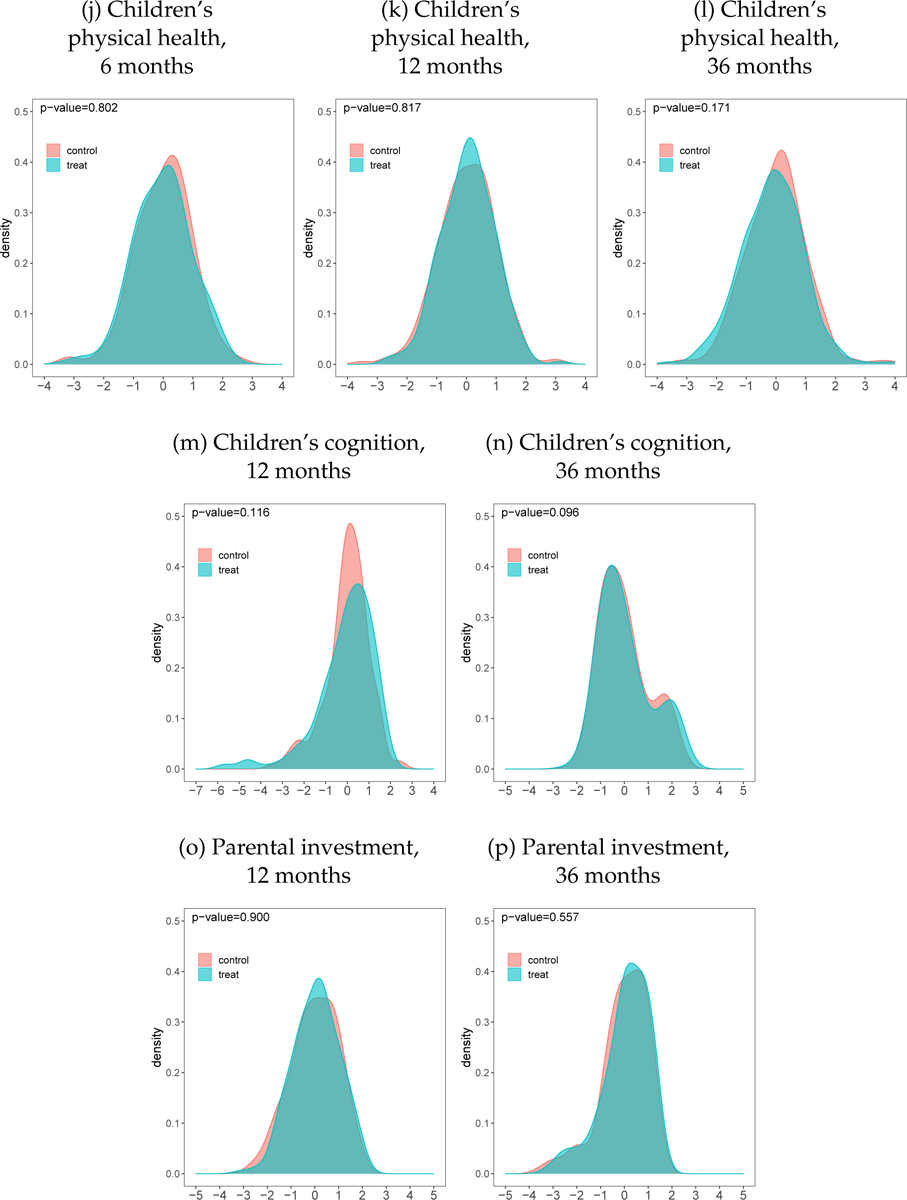
Kernel Densities of Latent Factors
Figure A7:
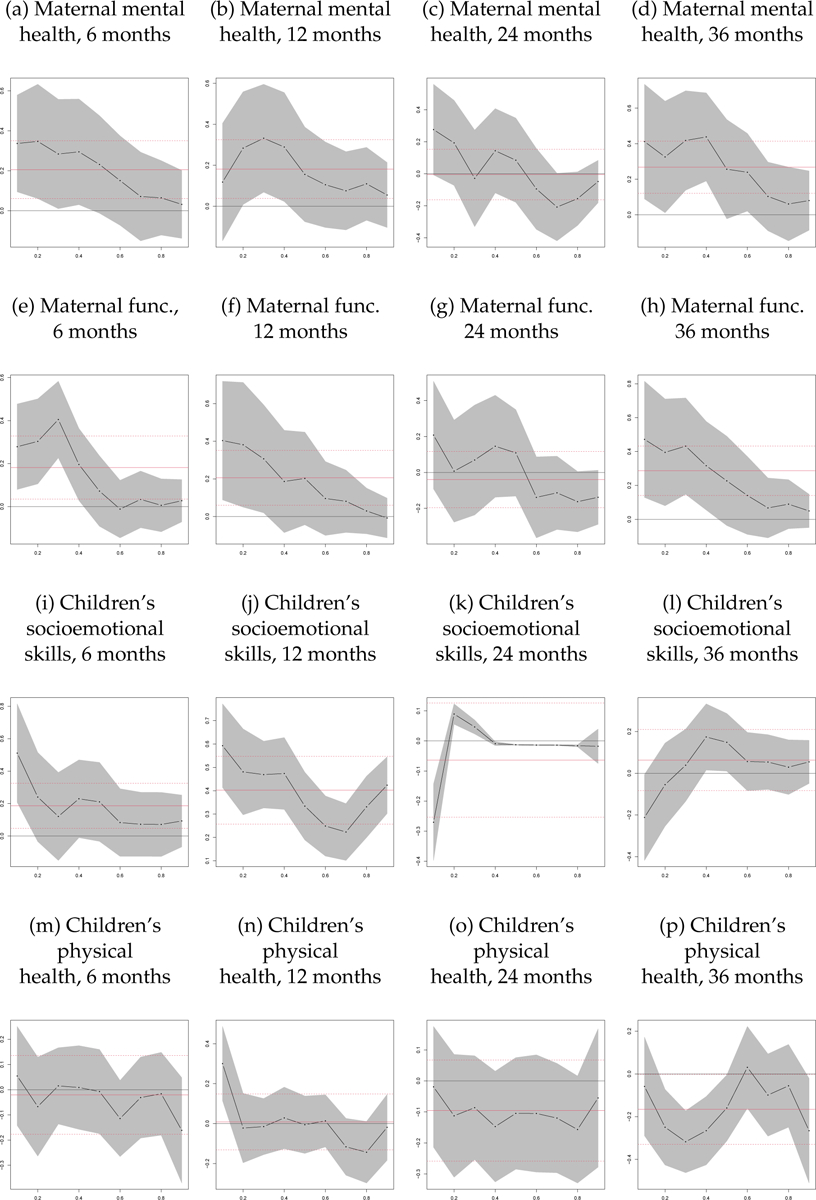
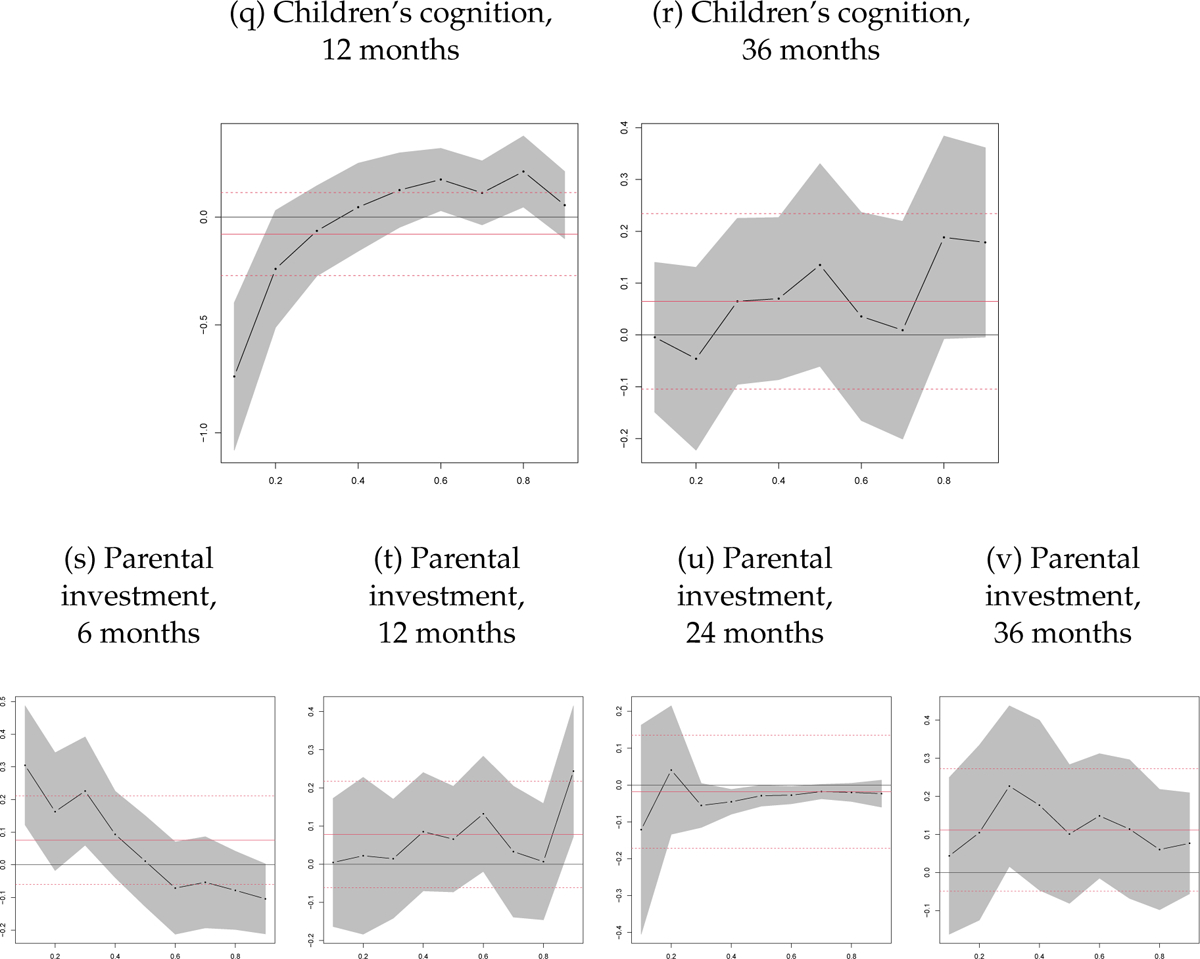
Quantile Treatment Effects on Latent Factors
Note: Quantile treatment effects of THPP+ intervention on latent factors. 95% confidence intervals are calculated by bootstrapping using 1000 replications and clustering at the level of randomization.
Table A29:
Heterogeneity in treatment effects for maternal mental health
| Coefficient on | |||
|---|---|---|---|
| treatment (1) |
baseline characteristic (2) |
treat × baseline characteristic (3) |
|
| Baseline characteristic: index child is female | |||
| mental health (6m) | 0.422*** (0.095) |
0.065 (0.114) |
−0.413*** (0.154) |
| mental health (12m) | 0.338*** (0.099) |
0.108 (0.109) |
−0.254 (0.160) |
| mental health (24m) | −0.056 (0.118) |
−0.095 (0.184) |
0.096 (0.205) |
| mental health (36m) | 0.364** (0.145) |
0.100 (0.111) |
−0.222 (0.173) |
| Baseline characteristic: first child | |||
| mental health (6m) | 0.172** (0.086) |
0.051 (0.165) |
0.148 (0.186) |
| mental health (12m) | 0.175** (0.088) |
−0.075 (0.169) |
0.132 (0.212) |
| mental health (24m) | −0.081 (0.092) |
−0.230 (0.171) |
0.293 (0.219) |
| mental health (36m) | 0.261** (0.113) |
0.013 (0.205) |
−0.045 (0.226) |
| Baseline characteristic: SES index | |||
| mental health (6m) | 0.222*** (0.067) |
−0.020 (0.054) |
0.043 (0.065) |
| mental health (12m) | 0.170*** (0.066) |
0.024 (0.045) |
−0.089* (0.047) |
| mental health (24m) | 0.021 (0.073) |
−0.031 (0.046) |
0.066 (0.053) |
| mental health (36m) | 0.212** (0.100) |
0.017 (0.055) |
−0.105* (0.054) |
| Baseline characteristic: mother’s education | |||
| mental health (6m) | −0.089 (0.156) |
0.001 (0.012) |
0.042** (0.019) |
| mental health (12m) | 0.206 (0.150) |
0.045*** (0.014) |
0.000 (0.018) |
| mental health (24m) | −0.243* (0.143) |
0.013 (0.013) |
0.034* (0.018) |
| mental health (36m) | 0.487** (0.218) |
0.041** (0.018) |
−0.034 (0.025) |
| Baseline characteristic: PHQ Total | |||
| mental health (6m) | 0.377 (0.328) |
0.049* (0.026) |
−0.014 (0.027) |
| mental health (12m) | 0.579* (0.297) |
0.082*** (0.019) |
−0.030 (0.023) |
| mental health (24m) | −0.115 (0.340) |
0.052* (0.027) |
0.009 (0.026) |
| mental health (36m) | 0.101 (0.333) |
0.027 (0.021) |
0.012 (0.026) |
treatment=1 if the observation is in treatment clusters, =0 otherwise. Dependent variables (listed on the first column) are latent factor scores of maternal mental health, coded in a way that higher score means better outcome and standardized to be mean 0 and SD 1 in the control group. Coefficients are obtained from the regressions of factor scores on the treatment indicator, its interactions with the respective dimension and the baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education (in years), asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. Robust and clustered standard errors at the cluster level are reported in the SE column.
Note:
p<0.1;
p<0.05;
p<0.01
Table A30:
Heterogeneity in treatment effects for selected child outcomes
| Coefficient on | |||
|---|---|---|---|
| treatment (1) |
baseline characteristic (2) |
treat × baseline characteristic (3) |
|
| Baseline characteristic: index child is female | |||
| socioemotional skills (6m) | 0.294** (0.132) |
0.247* (0.128) |
−0.230 (0.175) |
| socioemotional skills (12m) | 0.640*** (0.136) |
0.189 (0.132) |
−0.430** (0.171) |
| socioemotional skills (24m) | 0.003 (0.148) |
0.117 (0.146) |
−0.140 (0.235) |
| socioemotional skills (36m) | 0.027 (0.130) |
−0.014 (0.113) |
0.034 (0.171) |
| cognition (12m) | −0.033 (0.118) |
−0.135 (0.150) |
−0.021 (0.209) |
| cognition (36m) | 0.070 (0.131) |
−0.017 (0.091) |
−0.008 (0.188) |
| Baseline characteristic: first child | |||
| socioemotional skills (6m) | 0.067 (0.081) |
−0.239 (0.178) |
0.458** (0.183) |
| socioemotional skills (12m) | 0.467*** (0.106) |
0.099 (0.132) |
−0.212 (0.185) |
| socioemotional skills (24m) | −0.092 (0.108) |
0.126 (0.196) |
0.092 (0.162) |
| socioemotional skills (36m) | −0.003 (0.088) |
−0.015 (0.171) |
0.206 (0.183) |
| cognition (12m) | −0.128 (0.107) |
−0.143 (0.183) |
0.357 (0.227) |
| cognition (36m) | 0.073 (0.106) |
−0.174 (0.182) |
−0.031 (0.247) |
| Baseline characteristic: SES index | |||
| socioemotional skills (6m) | 0.161** (0.078) |
0.067 (0.044) |
−0.040 (0.043) |
| socioemotional skills (12m) | 0.413*** (0.083) |
−0.040 (0.049) |
−0.011 (0.051) |
| socioemotional skills (24m) | −0.034 (0.081) |
0.046 (0.055) |
0.080 (0.106) |
| socioemotional skills (36m) | 0.029 (0.080) |
0.004 (0.043) |
−0.043 (0.044) |
| cognition (12m) | 0.009 (0.088) |
−0.034 (0.067) |
0.130* (0.079) |
| cognition (36m) | 0.069 (0.089) |
−0.034 (0.041) |
0.008 (0.054) |
| Baseline characteristic: mother’s education | |||
| socioemotional skills (6m) | 0.042 (0.120) |
−0.026* (0.016) |
0.019 (0.020) |
| socioemotional skills (12m) | 0.463** (0.190) |
−0.004 (0.020) |
−0.007 (0.022) |
| socioemotional skills (24m) | −0.503** (0.210) |
−0.045*** (0.017) |
0.063** (0.027) |
| socioemotional skills (36m) | 0.195 (0.174) |
−0.002 (0.014) |
−0.022 (0.020) |
| cognition (12m) | −0.491 ** (0.210) |
−0.016 (0.023) |
0.063*** (0.024) |
| cognition (36m) | 0.224 (0.162) |
0.043*** (0.015) |
−0.023 (0.022) |
| Baseline characteristic: PHQ Total | |||
| socioemotional skills (6m) | 0.140 (0.327) |
0.021 (0.019) |
0.003 (0.026) |
| socioemotional skills (12m) | 0.766** (0.326) |
0.037 (0.025) |
−0.028 (0.024) |
| socioemotional skills (24m) | −0.564 (0.456) |
−0.007 (0.024) |
0.040 (0.034) |
| socioemotional skills (36m) | 0.649** (0.300) |
0.025 (0.020) |
−0.049* (0.025) |
| cognition (12m) | −0.182 (0.365) |
−0.004 (0.020) |
0.011 (0.028) |
| cognition (36m) | 0.301 (0.376) |
0.012 (0.018) |
−0.019 (0.028) |
treatment=1 if the observation is in treatment clusters, =0 otherwise. Dependent variables (listed on the first column) are latent factor scores of child socio-emotional health and cognition, coded in a way that higher score means better outcome and standardized to be mean 0 and SD 1 in the control group. Coefficients are obtained from the regressions of factor scores on the treatment indicator, its interactions with the respective dimension and the baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education (in years), asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. Robust and clustered standard errors at the cluster level are reported in the SE column.
Note:
p<0.1;
p<0.05;
p<0.01
Table A31:
Heterogeneity in treatment effects for parental investment
| Coefficient on | |||
|---|---|---|---|
| treatment (1) |
baseline characteristic (2) |
treat × baseline characteristic (3) |
|
| Baseline characteristic: index child is female | |||
| parental investment (12m) | 0.131 (0.115) |
−0.003 (0.119) |
−0.097 (0.173) |
| parental investment (36m) | 0.121 (0.114) |
0.024 (0.093) |
−0.012 (0.153) |
| Baseline characteristic: first child | |||
| parental investment (12 m) | 0.020 (0.118) |
−0.060 (0.150) |
0.255 (0.210) |
| parental investment (36m) | 0.127 (0.102) |
−0.081 (0.151) |
−0.054 (0.186) |
| Baseline characteristic: SES index | |||
| parental investment (12m) | 0.077 (0.099) |
0.116*** (0.040) |
−0.009 (0.050) |
| parental investment (36m) | 0.085 (0.082) |
0.092* (0.048) |
−0.081 (0.067) |
| Baseline characteristic: mother’s education | |||
| parental investment (12 m) | 0.007 (0.186) |
0.046*** (0.013) |
0.010 (0.020) |
| parental investment (36 m) | 0.338* (0.187) |
0.056*** (0.013) |
−0.033 (0.024) |
| Baseline characteristic: PHQ Total | |||
| parental investment (12m) | 0.063 (0.379) |
0.007 (0.02) |
0.001 (0.027) |
| parental investment (36m) | 0.452 (0.365) |
0.019 (0.018) |
−0.027 (0.028) |
treatment=1 if the observation is in treatment clusters, =0 otherwise. Dependent variables (listed on the first column) are latent factor scores of parental investment, coded in a way that higher score means better outcome and standardized to be mean 0 and SD 1 in the control group. Coefficients are obtained from the regressions of factor scores on the treatment indicator, its interactions with the respective dimension and the baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education (in years), asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. Robust and clustered standard errors at the cluster level are reported in the SE column.
Note:
p<0.1;
p<0.05;
p<0.01
I. Depression Gap
Table A32:
Difference in ICW Indices between Non-depressed and Control Groups
| treated depressed-control depressed | nondepressed-control depressed | ||||||
|---|---|---|---|---|---|---|---|
| Diff. (T-C) (1) |
Adjusted Beta (2) |
s.e. (3) |
p-val (4) |
Diff. (ND-C) (5) |
s.e. (6) |
p-val (7) |
|
| Maternal Indices | |||||||
| Mental Health (6m) | 0.142 | 0.163 | 0.084 | 0.053 | 0.516 | 0.062 | 0.000 |
| Mental Health (12m) | 0.103 | 0.142 | 0.085 | 0.096 | 0.478 | 0.069 | 0.000 |
| Mental Health (24m) | −0.139 | −0.048 | 0.079 | 0.541 | 0.328 | 0.086 | 0.000 |
| Mental Health (36m) | 0.168 | 0.292 | 0.098 | 0.003 | 0.425 | 0.071 | 0.000 |
| Functioning (6m) | 0.136 | 0.175 | 0.088 | 0.047 | 0.459 | 0.092 | 0.000 |
| Functioning (12m) | 0.192 | 0.241 | 0.077 | 0.002 | 0.378 | 0.067 | 0.000 |
| Functioning (24m) | −0.087 | −0.095 | 0.097 | 0.332 | 0.303 | 0.085 | 0.000 |
| Functioning (36m) | 0.066 | 0.211 | 0.079 | 0.008 | 0.317 | 0.073 | 0.000 |
| Child Indices | |||||||
| Physical Health (6m) | 0.001 | −0.021 | 0.096 | 0.826 | −0.020 | 0.080 | 0.806 |
| Physical Health (12m) | 0.012 | 0.002 | 0.080 | 0.981 | −0.016 | 0.081 | 0.845 |
| Physical Health (24m) | −0.097 | −0.035 | 0.095 | 0.710 | 0.004 | 0.092 | 0.965 |
| Physical Health (36m) | −0.099 | −0.099 | 0.099 | 0.315 | 0.045 | 0.081 | 0.579 |
| Socioemotional Skills (6m) | −0.034 | −0.046 | 0.085 | 0.589 | 0.041 | 0.080 | 0.610 |
| Socioemotional Skills (12m) | 0.106 | 0.100 | 0.081 | 0.215 | 0.050 | 0.069 | 0.469 |
| Socioemotional Skills (24m) | −0.043 | 0.046 | 0.089 | 0.604 | −0.162 | 0.073 | 0.027 |
| Socioemotional Skills (36m) | 0.022 | −0.024 | 0.118 | 0.842 | 0.240 | 0.091 | 0.008 |
| Cognition (12m) | −0.038 | −0.040 | 0.105 | 0.704 | 0.038 | 0.077 | 0.623 |
| Cognition (36m) | 0.092 | 0.104 | 0.088 | 0.235 | 0.074 | 0.079 | 0.348 |
| Investment Indices | |||||||
| Parental Investment (6m) | 0.083 | 0.085 | 0.071 | 0.228 | 0.180 | 0.098 | 0.065 |
| Parental Investment (12m) | 0.131 | 0.160 | 0.086 | 0.064 | 0.262 | 0.087 | 0.003 |
| Parental Investment (24m) | −0.076 | −0.045 | 0.093 | 0.626 | 0.166 | 0.067 | 0.013 |
| Parental Investment (36m) | 0.060 | 0.082 | 0.080 | 0.301 | 0.179 | 0.065 | 0.006 |
Column 2 reports the adjusted treatment coefficient from the regression of ICW indices on treatment indicator and its interaction with the (demeaned) baseline covariates using the experimental sample. Column 5 reports the raw differences of outcomes between nondepressed group and the control group. Baseline covariates include baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. Robust and clustered standard errors at the cluster level are reported in the SE columns. ICW indices are coded so that higher score indicates better outcome and standardized to have mean 0 and SD 1 in the control group.
Table A33:
Difference in Factor Scores between Non-depressed and Control Groups
| treated depressed-control depressed | nondepressed-control depressed | ||||||
|---|---|---|---|---|---|---|---|
| Diff. (T-C) (1) |
Adjusted Beta (2) |
s.e. (3) |
p-val (4) |
Diff. (ND-C) (5) |
s.e. (6) |
p-val (7) |
|
| Maternal Factors | |||||||
| Mental Health (6m) | 0.160 | 0.205 | 0.052 | 0.000 | 0.648 | 0.079 | 0.000 |
| Mental Health (12m) | 0.098 | 0.170 | 0.054 | 0.002 | 0.650 | 0.069 | 0.000 |
| Mental Health (36m) | 0.133 | 0.268 | 0.078 | 0.001 | 0.556 | 0.063 | 0.000 |
| Functioning (6m) | 0.108 | 0.182 | 0.075 | 0.015 | 0.547 | 0.083 | 0.000 |
| Functioning (12m) | 0.159 | 0.195 | 0.069 | 0.005 | 0.471 | 0.070 | 0.000 |
| Functioning (36m) | 0.112 | 0.287 | 0.081 | 0.000 | 0.376 | 0.069 | 0.000 |
| Child Factors | |||||||
| Physical Health (6m) | −0.016 | 0.021 | 0.079 | 0.792 | −0.034 | 0.077 | 0.662 |
| Physical Health (12m) | 0.044 | 0.019 | 0.070 | 0.784 | 0.035 | 0.076 | 0.650 |
| Physical Health (36m) | −0.137 | −0.166 | 0.088 | 0.060 | 0.041 | 0.080 | 0.803 |
| Socioemotional Skills (6m) | 0.167 | 0.187 | 0.056 | 0.001 | 0.100 | 0.087 | 0.250 |
| Socioemotional Skills (12m) | 0.417 | 0.389 | 0.070 | 0.000 | 0.315 | 0.069 | 0.000 |
| Socioemotional Skills (36m) | 0.058 | 0.063 | 0.075 | 0.400 | 0.108 | 0.073 | 0.138 |
| Cognition (12m) | −0.059 | −0.080 | 0.083 | 0.334 | 0.069 | 0.078 | 0.373 |
| Cognition (36m) | 0.047 | 0.065 | 0.075 | 0.386 | −0.020 | 0.080 | 0.803 |
| Investment Factors | |||||||
| Parental Investment (12m) | 0.062 | 0.075 | 0.086 | 0.382 | 0.448 | 0.104 | 0.000 |
| Parental Investment (36m) | 0.067 | 0.111 | 0.076 | 0.143 | 0.361 | 0.091 | 0.000 |
Column 2 reports the adjusted treatment coefficient from the regression of factors on treatment indicator and its interaction with the (demeaned) baseline covariates using the experimental sample. Column 5 reports the raw differences of outcomes between nondepressed group and the control group. Baseline covariates include baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. Robust and clustered standard errors at the cluster level are reported in the SE columns. Latent factor scores are coded so that higher score indicates better outcome and standardized to have mean 0 and SD 1 in the control group.
J. Technology of Skill Formation
Table A34:
Estimates of the Production Function Controlling for Baseline Mental Health (12 months)
| Socioemotional skills (12m) (1) |
Physical health (12m) (2) |
Cognition (12m) (3) |
Parental investment (12m) (4) |
|
|---|---|---|---|---|
| SE skills (6m) | 0.542*** (0.049) |
0.003 (0.013) |
0.057* (0.034) |
0.040 (0.029) |
| physical health (6m) | 0.042 (0.037) |
0.928*** (0.014) |
0.111*** (0.042) |
0.077*** (0.024) |
| mother mental health (6m) | 0.119* (0.063) |
0.083*** (0.030) |
0.130* (0.076) |
−0.114* (0.069) |
| mother functioning (6m) | −0.040 (0.053) |
−0.044** (0.020) |
−0.024 (0.045) |
0.080** (0.040) |
| investment (12m) | 0.050 (0.083) |
0.030 (0.022) |
−0.014 (0.060) |
|
| Interactions | ||||
| mother MH (6m) × treat | −0.216*** (0.078) |
−0.061 (0.038) |
−0.198** (0.096) |
0.100 (0.085) |
| mother MH (6m) × nondep. | −0.060 (0.097) |
−0.133***
(0.034) |
−0.065 (0.094) |
0.106 (0.080) |
| investment (12m) × treat | 0.104 (0.106) |
−0.030 (0.035) |
0.343*** (0.090) |
|
| investment (12m) × nondep. | −0.011 (0.084) |
−0.026 (0.030) |
0.205*** (0.073) |
|
| Total factor productivity (TFP) | ||||
| TFP | −0.639 (0.912) |
−0.466 (0.346) |
4.199*** (0.918) |
0.105 (0.798) |
| TFP × treat | 0.480*** (0.060) |
0.034* (0.020) |
−0.025 (0.058) |
0.062 (0.060) |
| TFP × nondep. | 0.267*** (0.098) |
0.118*** (0.038) |
−0.072 (0.088) |
0.023 (0.094) |
| Baseline controls | ||||
| SES assets | −0.017 (0.019) |
0.004 (0.007) |
0.009 (0.024) |
0.087*** (0.016) |
| mother’s education (years) | −0.001 (0.064) |
0.005 (0.003) |
−0.004 (0.007) |
0.018*** (0.004) |
| husband’s education (years) | 0.001 (0.007) |
−0.006**
(0.003) |
−0.001 (0.006) |
0.017** (0.008) |
| Observations | 932 | 932 | 927 | 932 |
| R2 | 0.505 | 0.882 | 0.257 | 0.385 |
| Adjusted R2 | 0.467 | 0.873 | 0.201 | 0.341 |
SE= socioemotional skills, MH=mental health. Dependent variables are child outcomes and parental investment factors at 12 months postpartum. Independent variables include an indicator of treatment status (control, treatment, nondepressed), child and maternal factors at 6 months, parental investment factor at 12 months. Maternal mental health and parental investment are interacted with the treatment status. All estimations control for baseline characteristics including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect, days from baseline and child age in days. Robust and clustered standard errors at the cluster level are reported in paranthesis.
Note:
p<0.1
p<0.05;
p<0.01
Table A35:
Estimates of the Production Function Controlling for Baseline Mental Health (36 months)
| Socioemotional skills (36m) (1) |
Physical health (36m) (2) |
Cognition (36m) (3) |
Parental investment (36m) (4) |
|
|---|---|---|---|---|
| SE skills (12m) | 0.241*** (0.036) |
0.035* (0.019) |
0.012 (0.023) |
−0.083** (0.032) |
| physical health (12m) | 0.027 (0.041) |
1.049*** (0.026) |
0.046** (0.023) |
0.066** (0.029) |
| cognition (12m) | 0.001 (0.038) |
−0.018 (0.022) |
0.059*** (0.022) |
0.031 (0.033) |
| mother mental health (12m) | 0.078 (0.096) |
0.045 (0.050) |
−0.074 (0.059) |
0.202*** (0.076) |
| mother functioning (12m) | −0.070 (0.048) |
−0.049* (0.027) |
0.065* (0.033) |
−0.009 (0.049) |
| investment (36m) | 0.164** (0.069) |
0.001 (0.039) |
0.092** (0.039) |
|
| Interactions | ||||
| mother MH (12m) × treat | 0.049 (0.114) |
−0.057 (0.056) |
0.059 (0.066) |
−0.150* (0.085) |
| mother MH (12m) × nondep. | 0.003 (0.112) |
−0.004 (0.047) |
−0.005 (0.068) |
−0.074 (0.087) |
| investment (36m) × treat | −0.188* (0.109) |
0.036 (0.054) |
−0.085 (0.060) |
|
| investment (36m) × nondep. | 0.013 (0.100) |
−0.048 (0.045) |
−0.008 (0.051) |
|
| Total factor productivity (TFP) | ||||
| TFP | 0.570 (2.474) |
−1.537** (0.698) |
1.966** (0.949) |
1.895 (1.376) |
| TFP × treat | −0.115 (0.084) |
−0.170*** (0.045) |
0.019 (0.039) |
0.131** (0.059) |
| TFP × nondep. | −0.178 (0.122) |
0.038 (0.060) |
−0.046 (0.072) |
0.122 (0.092) |
| Baseline controls | ||||
| SES assets | −0.016 (0.016) |
−0.004 (0.012) |
−0.002 (0.011) |
0.055*** (0.019) |
| mother’s education (years) | −0.006 (0.006) |
0.006 (0.004) |
0.014*** (0.004) |
0.016*** (0.006) |
| husband’s education (years) | 0.009 (0.007) |
−0.003 (0.004) |
0.008 (0.006) |
0.031*** (0.008) |
| Observations | 881 | 881 | 881 | 881 |
| R2 | 0.422 | 0.839 | 0.302 | 0.313 |
| Adjusted R2 | 0.382 | 0.828 | 0.253 | 0.268 |
SE= socioemotional skills, MH=mental health. Dependent variables are child outcomes and parental investment factors at 36 months postpartum. Independent variables include an indicator of treatment status (control, treatment, nondepressed), child and maternal factors at 12 months, parental investment factor at 36 months. Maternal mental health and parental investment are interacted with the treatment status. All estimations control for baseline characteristics including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset based SES index, life events cheklist score, interviewer fixed effect, union council fixed effect, days from baseline and child age in days. Robust and clustered standard errors at the cluster level are reported in paranthesis.
Note:
p<0.1;
p<0.05;
p<0.01
Table A36:
Estimates of the Production Function and Investment Equation by Gender (12 months)
| Boys | Girls | |||||||
|---|---|---|---|---|---|---|---|---|
| Socioemotional skills (12m) (1) |
Physical health (12m) (2) |
Cognition (12m) (3) |
Parental investment (12m) (4) |
Socioemotional skills (12m) (1) |
Physical health (12m) (2) |
Cognition (12m) (3) |
Parental investment (12m) (4) |
|
| SE skills (6m) | 0.536*** (0.067) |
−0.022 (0.020) |
0.051 (0.053) |
0.035 (0.048) |
0.560*** (0.047) |
0.032 (0.020) |
0.070 (0.050) |
0.040 (0.040) |
| physical health (6m) | 0.058 (0.057) |
0.917*** (0.019) |
0.134** (0.063) |
0.100*** (0.029) |
0.046 (0.041) |
0.935*** (0.022) |
0.103* (0.054) |
0.043 (0.044) |
| mother mental health (6m) | 0.060 (0.129) |
0.066 (0.046) |
0.170 (0.133) |
−0.034 (0.100) |
0.112 (0.111) |
0.093** (0.039) |
0.063 (0.083) |
−0.219** (0.096) |
| mother functioning (6m) | −0.023 (0.119) |
−0.013 (0.032) |
−0.038 (0.068) |
0.102* (0.050) |
−0.057 (0.062) |
−0.048** (0.023) |
0.003 (0.060) |
0.051 (0.066) |
| investment (12m) | 0.085 (0.119) |
0.017 (0.045) |
−0.189* (0.102) |
−0.011 (0.122) |
0.046* (0.028) |
0.036 (0.085) |
||
| Interactions | ||||||||
| mother MH (6m) × treat | −0.125 (0.148) |
−0.025 (0.055) |
−0.068 (0.179) |
−0.020 (0.122) |
−0.241** (0.119) |
−0.077 (0.052) |
−0.264** (0.126) |
0.227* (0.134) |
| mother MH (6m) × nondep. | 0.005 (0.166) |
−0.155*** (0.055) |
−0.098 (0.140) |
−0.035 (0.124) |
−0.109 (0.116) |
−0.118** (0.052) |
−0.050 (0.088) |
0.299*** (0.106) |
| investment (12m) × treat | 0.056 (0.165) |
−0.020 (0.058) |
0.260* (0.144) |
0.114 (0.148) |
−0.045 (0.046) |
0.451*** (0.155) |
||
| investment (12m) × nondep. | −0.016 (0.117) |
−0.007 (0.060) |
0.289** (0.114) |
0.042 (0.118) |
−0.047 (0.041) |
0.233** (0.116) |
||
| Total factor productivity (TFP) | ||||||||
| TFP | −0.114 (1.403) |
−0.607 (0.536) |
4.065*** (1.265) |
0.303 (0.855) |
−1.102 (1.123) |
−0.628 (0.486) |
3.495** (1.459) |
−0.016 (1.285) |
| TFP × treat | 0.571*** (0.105) |
0.031 (0.027) |
−0.030 (0.084) |
0.080 (0.070) |
0.411*** (0.083) |
0.038 (0.026) |
−0.030 (0.092) |
0.059 (0.092) |
| TFP × nondep. | 0.286* (0.162) |
0.136** (0.054) |
−0.252* (0.150) |
−0.027 (0.122) |
0.169 (0.123) |
0.134** (0.056) |
−0.047 (0.123) |
0.084 (0.143) |
| Baseline controls | ||||||||
| SES assets | −0.059* (0.031) |
0.017 (0.013) |
−0.014 (0.032) |
0.074*** (0.021) |
0.017 (0.020) |
−0.009 (0.011) |
0.046 (0.033) |
0.106*** (0.024) |
| mother’s education (years) | 0.009 (0.010) |
0.005 (0.005) |
−0.005 (0.011) |
0.019*** (0.006) |
−0.002 (0.007) |
0.004 (0.003) |
−0.003 (0.009) |
0.016* (0.008) |
| husband’s education (years) | −0.006 (0.012) |
−0.012** (0.005) |
−0.001 (0.010) |
0.015* (0.009) |
0.006 (0.009) |
−0.001 (0.004) |
−0.001 (0.009) |
0.015 (0.011) |
| Observations | 466 | 466 | 464 | 466 | 466 | 466 | 463 | 466 |
| R2 | 0.507 | 0.898 | 0.278 | 0.482 | 0.589 | 0.882 | 0.343 | 0.358 |
| Adjusted R2 | 0.431 | 0.882 | 0.166 | 0.407 | 0.527 | 0.864 | 0.243 | 0.266 |
SE= socioemotional skills, MH=mental health. Table shows estimates of the production function at 12 months by the gender of the index child. Dependent variables are child outcomes and parental investment factors at 12 months postpartum. Independent variables include an indicator of treatment status (control, treatment, nondepressed), child and maternal factors at 6 months, parental investment factor at 12 months. Maternal mental health and parental investment are interacted with the treatment status. All estimations control for baseline characteristics including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (splitted by gender), whether the index child is the first child, parental education levels, asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect, days from baseline and child age in days. Robust and clustered standard errors at the cluster level are reported in paranthesis.
Note:
p<0.1;
p<0.05;
p<0.01
Table A37:
Estimates of the Production Function and Investment Equation by Gender (36 months)
| Boys | Girls | |||||||
|---|---|---|---|---|---|---|---|---|
| Socioemotional skills (36m) (1) |
Physical health (36m) (2) |
Cognition (36m) (3) |
Parental investment (36m) (4) |
Socioemotional skills (36m) (1) |
Physical health (36m) (2) |
Cognition (36m) (3) |
Parental investment (36m) (4) |
|
| SE skills (12m) | 0.250*** (0.060) |
0.046* (0.028) |
−0.011 (0.027) |
−0.045 (0.042) |
0.272*** (0.053) |
0.027 (0.026) |
0.036 (0.033) |
0.129*** (0.038) |
| physical health (12m) | 0.037 (0.061) |
1.017*** (0.034) |
0.043 (0.038) |
0.101*** (0.035) |
−0.008 (0.046) |
1.076*** (0.029) |
0.041 (0.033) |
0.022 (0.048) |
| cognition (12m) | −0.011 (0.074) |
−0.009 (0.034) |
0.109*** (0.031) |
0.055 (0.038) |
−0.006 (0.042) |
−0.028 (0.033) |
0.018 (0.032) |
0.015 (0.049) |
| mother mental health (12m) | 0.313** (0.135) |
−0.004 (0.093) |
−0.050 (0.074) |
0.391*** (0.125) |
−0.062 (0.113) |
0.080 (0.061) |
−0.124* (0.077) |
0.054 (0.082) |
| mother functioning (12m) | −0.095 (0.083) |
−0.069 * (0.040) |
0.082* (0.049) |
−0.020 (0.072) |
−0.025 (0.060) |
−0.035 (0.045) |
0.054 (0.039) |
−0.015 (0.066) |
| investment (36m) | 0.024 (0.107) |
−0.044 (0.076) |
0.135** (0.062) |
0.283** (0.115) |
0.069 (0.051) |
0.068 (0.067) |
||
| Interactions | ||||||||
| mother MH (12m) × treat | −0.072 (0.197) |
0.076 (0.102) |
0.101 (0.097) |
−0.375*** (0.137) |
0.161 (0.156) |
−0.161** (0.072) |
0.084 (0.075) |
0.010 (0.128) |
| mother MH (12m) × nondep. | −0.248 (0.153) |
0.076 (0.078) |
−0.009 (0.087) |
−0.380*** (0.128) |
0.113 (0.138) |
−0.060 (0.063) |
0.032 (0.097) |
0.206* (0.110) |
| investment (36m) × treat | −0.032 (0.160) |
0.086 (0.096) |
−0.073 (0.075) |
−0.302* (0.172) |
0.003 (0.063) |
−0.114 (0.096) |
||
| investment (36m) × nondep. | 0.088 (0.149) |
−0.021 (0.084) |
−0.070 (0.076) |
−0.075 (0.134) |
−0.113* (0.058) |
0.041 (0.089) |
||
| Total factor productivity (TFP) | ||||||||
| TFP | −1.226 (3.612) |
−2.654** (1.288) |
−0.702 (1.540) |
1.761 (1.727) |
3.063 (2.538) |
−1.168 (1.203) |
4.897*** (1.150) |
1.299 (2.177) |
| TFP × treat | −0.194 (0.129) |
−0.182*** (0.062) |
0.024 (0.064) |
0.119 (0.083) |
−0.078 (0.112) |
−0.154*** (0.056) |
0.031 (0.053) |
0.165** (0.070) |
| TFP × nondep. | −0.310* (0.167) |
−0.011 (0.075) |
−0.009 (0.092) |
0.161 (0.145) |
−0.102 (0.131) |
0.114 (0.088) |
−0.084 (0.122) |
0.063 (0.129) |
| Baseline controls | ||||||||
| SES assets | −0.034 (0.028) |
−0.012 (0.016) |
−0.003 (0.017) |
0.031 (0.027) |
0.008 (0.022) |
−0.002 (0.017) |
0.009 (0.014) |
0..074***
(0.026) |
| mother’s education (years) | −0.008 (0.009) |
0.008 (0.005) |
0.014** (0.006) |
0.022*** (0.007) |
−0.005 (0.010) |
0.005 (0.006) |
0.011** (0.005) |
0.011 (0.008) |
| husband’s education (years) | 0.017 (0.014) |
−0.006 (0.006) |
0.004 (0.007) |
0.047*** (0.011) |
0.008 (0.010) |
0.004 (0.006) |
0.013 (0.009) |
0.020* (0.011) |
| Observations | 442 | 442 | 442 | 442 | 439 | 439 | 439 | 439 |
| R2 | 0.421 | 0.851 | 0.374 | 0.360 | 0.505 | 0.850 | 0.332 | 0.346 |
| Adjusted R2 | 0.339 | 0.830 | 0.284 | 0.275 | 0.433 | 0.828 | 0.234 | 0.256 |
SE= socioemotional skills, MH=mental health. Table shows estimates of the production function at 36 months by the gender of the index child. Dependent variables are child outcomes and parental investment factors at 36 months postpartum. Independent variables include an indicator of treatment status (control, treatment, nondepressed), child and maternal factors at 12 months, parental investment factor at 36 months. Maternal mental health and parental investment are interacted with the treatment status. All estimations control for baseline characteristics including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (splitted by gender), whether the index child is the first child, parental education levels, asset based SES index, life events checklist score, interviewer fixed effect, union council fixed effect, days from baseline and child age in days. Robust and clustered standard errors at the cluster level are reported in paranthesis.
Note:
p<0.1;
p<0.05;
p<0.01
Footnotes
These skills are malleable in childhood, but there is limited causal evidence of how malleable they are in the early years of life (Heckman et al., 2006; Roberts et al., 2007; Almlund et al., 2011; Lundberg, 2017; Nangle et al., 2020; Abrahams et al., 2019).
We analysed a similar but distinct intervention in Baranov et al. (2020). The intervention analyzed in Baranov et al. (2020) was delivered by salaried community health workers rather than by peer volunteers; it ran for 10 months, whereas the intervention we analyze here ran for 36 months; and the two interventions were run in different locations in Pakistan. Also, there was no follow-up between 12 months and 8 years in the previous study, and no measurement of child socioemotional or cognitive skills prior to 8 years. A key feature of this study is that we have frequent follow-up between birth and 36 months. Baranov et al. (2020) report intervention effects on skills at age 8, but do not estimate the production function for skills.
This is the case for the production of skills at 12 months of age. At 36 months, we see both an increase in TFP and diminishing returns to parental investment which, in turn, is shaped by maternal mental health. Details are in Section 5.
More information about the trial is in Sikander et al. (2015, 2019 a,b); Turner et al. (2016).
Further discussion of the 24-month wave is presented in Appendix Section C.
Longitudinal analyses using the ASQ-SE as a screening tool have been performed in several countries, when involving the general population (Marks et al., 2019), at risk groups (Keenan et al., 2019; Cho et al., 2021), and as an evaluation of a randomized controlled trial (Salisbury et al., 2022; Nores et al., 2019).
In Appendix Tables A18–A21 and Appendix Figures A4–A5, we show reduced form results with ICW indices constructed by weighting the mean vector of outcomes by the row-sum of the inverse of their covariance matrix, following Kling et al. (2007) and Anderson (2008). ICW indices are useful to minimize the noise resulting from random errors that are uncorrelated across indicators and provide an efficient estimation of the treatment effect by allowing single hypothesis testing, which increases statistical power. They also offer flexibility to aggregate information from the observed measures that are not highly correlated or from different domains. The ICW index puts more weight on measures that are less correlated and thus capture new information. That’s why, apart from estimating an index for each domain of child and maternal outcomes, we also construct an overall ICW index (e.g., child index) to capture a comprehensive effect of treatment on mothers and their children. Each index for each domain at each time point is normalized to have a mean of 0 and a standard deviation of 1 in the control group.
We regress a treatment dummy on all the baseline controls and report the p-value of the F-test of overall significance.
The high level of mortality in our sample is sadly in line with the region: Pakistan in 2020 had an infant mortality rate of 65.2 per 1000 deaths. Our mortality rate is higher, at 89/1000 by age 3, likely because our sample is rural and more disadvantaged, and it also includes stillbirths whereas under-five mortality is reported with reference to live births.
An exception is the 24-month follow-up, when a joint test for balance is rejected (p-value=0.046, see Table A4). We do not use the 24 month wave in the analysis. See Appendix Section C for additional information.
Additional details on the construction of latent factor scores are provided in Appendix Section D.1.
We use instead of as an input in the production function to capture investments that accumulated up until t+1. As parental investment is a flow variable and our indicators for investment mostly measure material investment (e.g., whether the index child has certain toys), is more relevant in the production of
Put differently, the specification is flexible enough to capture several ways in which the intervention can boost children’s skills. It could improve the inputs (including maternal mental health or parental investment), leaving the production function parameters constant. It could shift the production function upwards (increasing total factor productivity, TFP). It could differentially boost the skills of the children whose mothers did not recover from depression, reducing the slope of the production function (i.e. the marginal productivity) with respect to maternal mental health.
This channel is found in two related studies, Baranov et al. (2020); Angelucci and Bennett (2021), and appears even more likely in this intervention, which directly encouraged mothers to engage with and stimulate the child.
Adjusted beta coefficients are obtained from the regressions on the treatment indicator and its interactions with the (demeaned) baseline covariates including baseline PHQ Total, baseline WHODAS Total, baseline PSS Total, mother’s baseline age, weight, height, waist circumference and blood pressure, family structure, grandmother being resident, total adults in the household, people per room, number of living children (split by gender), whether the index child is the first child, parental education levels, asset-based SES index, life events checklist score, interviewer fixed effect, union council fixed effect and days from baseline. All estimations control for child gender and age (in days). Considering the baseline imbalance in some key characteristics, we always focus our discussion on the adjusted treatment effect coefficients and the respective p-values in the text below.
The null hypothesis is that two CDFs are the same. Bootstrapped p-values are reported at the upper left corner of each plot.
For these outcomes, the depression gap is positive, favoring the healthy comparison group. It is statistically significant only for socioemotional skills at 12 months, and for parental investment at 12 and 36 months. The treatment effects on socioemotional skills are similar in magnitude to the depression gap, but for parental investment the effects are only about a quarter of the depression gap.
In Maselko et al. (2020) we controlled for only those variables that were statistically significantly imbalanced by treatment-arm at baseline, or predicted missingness at 36 months at the p<0.10 level, following common practice in the public health literature. In this paper, we include a broader set of covariates and their interaction with the treatment indicator. Our controls include baseline PHQ-9 (depression), PSS (stress), and WHODAS (functionality) scores, which are significantly imbalanced at baseline when considered jointly, but not individually. The inclusion of baseline mental health measures drives the differences in point estimates between the findings in Maselko et al. (2020) and this paper. Another difference is that in Maselko et al. (2020) we report the impacts of the THPP+ intervention only on a pre-registered set of maternal and child outcomes at 36 months postpartum. For instance, Maselko et al. (2020) focus on clinical measures of depression (PHQ-9 score, depression remission, and major depressive episode)—while we construct a broader measure of maternal mental health. Focusing on a narrow set of pre-specified outcomes increases transparency and replicability, but might hinder our ability to learn systematically from the data (Coffman and Niederle, 2015).
Freyberger (2020) shows that an erroneous normalization or misspecification of the latent factor structure might lead to biased estimates, especially in the case of non-linear production functions such as CES.
As a robustness check, we also include in the controls the baseline level of mental health during pregnancy, , to capture the idea that pregnancy might be a critical developmental window in terms of exposure to depression, and to test for potential departures from the simple Markov dynamics as suggested by Attanasio et al. (2020b). Results in Appendix Tables A34–A35 show that the estimates do not change sizeably once baseline depression is added as a control.
To mitigate the imposition of functional form assumptions and focus solely on localized averages, in Figure 5b we employ a Kernel-weighted local polynomial smoothing estimator. Results for 36 months display a similar pattern, but with a lower degree of concavity. In the estimation of the production function, we impose a linear-in-log relationship which might be an approximation of the true underlying production function.
Note that the coefficient on maternal mental health reflects its direct association with child skills, conditional upon maternal functioning, maternal investment in children, and lagged child skills, all of which are potentially a function of maternal mental health.
We allow the cross-time correlation of the residuals to be non-zero for the measures that are asked at multiple time points.
For child physical health, we normalize to one the weight-for-age z score; child cognition is normalized on Bayley-III fine motor scale score; socioemotional skills are normalized on the ASQ-SE item ‘when upset, whether the baby can calm down within a half hour’;
maternal mental health is normalized on the SCID item ‘current major depressive episode’; maternal functioning is normalized on the WHODAS item ‘difficulty affecting day-to-day work’; parental investment is normalized on the HOME subscale of learning materials.
The signal-to-noise ratio, also known as communality, gives the amount of variance of each measure that can be explained by the underlying latent factor.
Contributor Information
Dilek Sevim, University of Basel..
Victoria Baranov, University of Melbourne.
Sonia Bhalotra, University of Warwick.
Joanna Maselko, University of North Carolina.
Pietro Biroli, University of Bologna.
Bibliography
- Abrahams L, Pancorbo G, Primi R, Santos D, Kyllonen P, John OP, and De Fruyt F (2019). Social-emotional skill assessment in children and adolescents: Advances and challenges in personality, clinical, and educational contexts. Psychological Assessment, 31(4):460. [DOI] [PubMed] [Google Scholar]
- Agostinelli F and Wiswall M (2016). Identification of dynamic latent factor models: The implications of re-normalization in a model of child development. Technical report, National Bureau of Economic Research. [Google Scholar]
- Almlund M, Duckworth AL, Heckman JJ, and Kautz T (2011). Personality Psychology and Economics. In Hanushek E, editor, Handbook of the Economics of Education, volume 4, pages 1–181. North Holland, Amsterdam, The Netherlands. [Google Scholar]
- Anderson ML (2008). Multiple inference and gender differences in the effects of early intervention: A reevaluation of the abecedarian, perry preschool, and early training projects. Journal of the American statistical Association, 103(484):1481–1495. [Google Scholar]
- Angelucci M and Bennett D (2021). The Economic Impact of Depression Treatment in India. IZA DP No. 14393. [Google Scholar]
- Anger S (2012). From parents to children: The intergenerational transmission of advantage, chapter intergenerational transmission of cognitive and noncognitive skills. Russell Sage Foundation, 3(14):5. [Google Scholar]
- Attanasio O, Cattan S, Fitzsimons E, Meghir C, and Rubio-Codina M (2020a). Estimating the production function for human capital: results from a randomized controlled trial in colombia. American Economic Review, 110(1):48–85. [Google Scholar]
- Attanasio O, de Paula Á, and Toppeta A (2020b). The persistence of socio-emotional skills: Life cycle and intergenerational evidence.
- Attanasio O, de Paula Á, and Toppeta A (2022a). Intergenerational mobility in socio-emotional skills. Working Paper. [Google Scholar]
- Attanasio O, Meghir C, and Nix E (2020c). Human capital development and parental investment in india. The Review of Economic Studies, 87(6):2511–2541. [Google Scholar]
- Attanasio OP, Cattan S, and Meghir C (2022b). Early Childhood Development, Human Capital, and Poverty. Annual Review of Economics, 14(1). [Google Scholar]
- Baranov V, Bhalotra S, Biroli P, and Maselko J (2020). Maternal Depression, Women’s Empowerment, and Parental Investment: Evidence from a Randomized Controlled Trial. American Economic Review, 110(3):824–859. [Google Scholar]
- Bennett IM, Schott W, Krutikova S, and Behrman JR (2016). Maternal mental health and child growth and development in four low-income and middle-income countries. Journal of Epidemiological Community Health, 70(2):168–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhalotra S, Chakravarty A, and Gulesci S (2020). The price of gold: Dowry and death in india. Journal of Development Economics, 143:102413. [Google Scholar]
- Bhalotra S, Daysal M, Trandafir M, and Lydiksen NV (2021). Antidepressant use and school test scores: Evidence from Danish administrative data. Mimeo. [Google Scholar]
- Blinder AS (1973). Wage discrimination: reduced form and structural estimates. Journal of Human Resources, pages 436–455. [Google Scholar]
- Briggs-Gowan MJ and Carter AS (2008). Social-emotional screening status in early childhood predicts elementary school outcomes. Pediatrics, 121(5):957–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bufferd SJ, Dougherty LR, Carlson GA, Rose S, and Klein DN (2012). Psychiatric disorders in preschoolers: continuity from ages 3 to 6. American Journal of Psychiatry, 169(11):1157–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busch SH, Golberstein E, and Meara E (2014). The FDA and ABCs: Unintended Consequences of Antidepressant Warnings on Human Capital. Journal of Human Resources, 49(3):540–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carneiro P, Hansen KT, and Heckman JJ (2003). Estimating distributions of treatment effects with an application to the returns to schooling and measurement of the effects of uncertainty on college choice. International Economic Review, 44(2):361–422. [Google Scholar]
- Cho J, Chien L-C, and Holditch-Davis D (2021). Associations between hormonal biomarkers and preterm infant health and development during the first 2 years after birth. Biological Research For Nursing, 23(2):188–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Class QA, Van Hulle CA, Rathouz PJ, Applegate B, Zald DH, and Lahey BB (2019). Socioemotional dispositions of children and adolescents predict general and specific second-order factors of psychopathology in early adulthood: A 12-year prospective study. Journal of abnormal psychology, 128(6):574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffman LC and Niederle M (2015). Pre-analysis plans have limited upside, especially where replications are feasible. Journal of Economic Perspectives, 29(3):81–98. [Google Scholar]
- Cunha F and Heckman JJ (2008). Formulating, identifying and estimating the technology of cognitive and noncognitive skill formation. Journal of human resources, 43(4):738–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunha F, Heckman JJ, and Schennach SM (2010). Estimating the technology of cognitive and noncognitive skill formation. Econometrica, 78(3):883–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie J and Stabile M (2006). Child mental health and human capital accumulation: The case of ADHD. Journal of Health Economics, 25(6):1094–1118. [DOI] [PubMed] [Google Scholar]
- de Quidt J and Haushofer J (2018). Depression through the Lens of Economics: A Research Agenda. NBER Volume: The Economics of Poverty Traps, pages 1–35. [Google Scholar]
- Ding W, Lehrer SF, Rosenquist JN, and Audrain-McGovern J (2009). The impact of poor health on academic performance: New evidence using genetic markers. Journal of Health Economics, 28(3):578–597. [DOI] [PubMed] [Google Scholar]
- DiPietro JA, Novak MF, Costigan KA, Atella LD, and Reusing SP (2006). Maternal psychological distress during pregnancy in relation to child development at age two. Child development, 77(3):573–587. [DOI] [PubMed] [Google Scholar]
- Dohmen T, Falk A, Huffman D, and Sunde U (2012). The intergenerational transmission of risk and trust attitudes. The Review of Economic Studies, 79(2):645–677. [Google Scholar]
- Erickson N, Julian M, and Muzik M (2019). Perinatal depression, ptsd, and trauma: Impact on mother–infant attachment and interventions to mitigate the transmission of risk. International Review of Psychiatry, 31(3):245–263. [DOI] [PubMed] [Google Scholar]
- Feil EG, Walker HM, and Severson HH (1995). The Early Screening Project for young children with behavior problems. Journal of Emotional and Behavioral Disorders, 3:194–202. [Google Scholar]
- Fletcher JM (2010). Adolescent depression and educational attainment: results using sibling fixed effects. Health Economics, 19(7):855–871. [DOI] [PubMed] [Google Scholar]
- Freyberger J (2020). Normalizations and misspecification in skill formation models. Working Paper. [Google Scholar]
- Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, Brody S, and Miller WC (2005). Perinatal depression: Prevalence, screening accuracy, and screening outcomes: Summary. In AHRQ evidence report summaries. Agency for Healthcare Research and Quality (US). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsmith-Pinkham P, Hull P, and Kolesár M (2022). Contamination bias in linear regressions.
- Grönqvist E, Öckert B, and Vlachos J (2017). The intergenerational transmission of cognitive and noncognitive abilities. Journal of Human Resources, 52(4):887–918. [Google Scholar]
- Grossman M (1972). On the concept of health capital and the demand for health. Journal of Political Economy, 80(2):223–255. [Google Scholar]
- Groves MO (2005). Personality and the intergenerational transmission of economic status. Unequal chances: Family background and economic success, pages 208–231. [Google Scholar]
- Halfon N, Larson K, Lu M, Tullis E, and Russ S (2014). Lifecourse health development: past, present and future. Maternal and child health journal, 18(2):344–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman JJ, Stixrud J, and Urzua S (2006). The effects of cognitive and noncognitive abilities on labor market outcomes and social behavior. Journal of Labor Economics, 24(3):411–482. [Google Scholar]
- Herba CM, Glover V, Ramchandani PG, and Rondon MB (2016). Maternal depression and mental health in early childhood: an examination of underlying mechanisms in low-income and middle-income countries. The Lancet Psychiatry, 3(10):983–992. [DOI] [PubMed] [Google Scholar]
- Hollins K (2007). Consequences of antenatal mental health problems for child health and development. Current Opinion in Obstetrics and Gynecology, 19(6):568–572. [DOI] [PubMed] [Google Scholar]
- Jeong J, Franchett EE, Oliveira C. V. R. d., Rehmani K, and Yousafzai AK (2021). Parenting interventions to promote early child development in the first three years of life: A global systematic review and meta-analysis. PLOS Medicine, 18(5):e1003602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jöreskog KG and Goldberger AS (1975). Estimation of a model with multiple indicators and multiple causes of a single latent variable. Journal of the American statistical Association, 70(351a):631–639. [Google Scholar]
- Keenan HT, Presson AP, Clark AE, Cox CS, and Ewing-Cobbs L (2019). Longitudinal developmental outcomes after traumatic brain injury in young children: Are infants more vulnerable than toddlers? Journal of Neurotrauma, 36(2):282–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitagawa EM (1955). Components of a Difference Between Two Rates. Journal of the American Statistical Association, 50(272):1168. [Google Scholar]
- Kling JR, Liebman JB, and Katz LF (2007). Experimental analysis of neighborhood effects. Econometrica, 75(1):83–119. [Google Scholar]
- Lamsal R, Dutton DJ, and Zwicker JD (2018). Using the ages and stages questionnaire in the general population as a measure for identifying children not at risk of a neurodevelopmental disorder. BMC Pediatrics, 18(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laplante DP, Brunet A, Schmitz N, Ciampi A, and King S (2008). Project ice storm: Prenatal maternal stress affects cognitive and linguistic functioning in 51/2-year-old children. Journal of the American Academy of Child & Adolescent Psychiatry, 47(9):1063–1072. [DOI] [PubMed] [Google Scholar]
- Lee DS (2009). Training, wages, and sample selection: Estimating sharp bounds on treatment effects. The Review of Economic Studies, 76(3):1071–1102. [Google Scholar]
- Leung BM and Kaplan BJ (2009). Perinatal depression: prevalence, risks, and the nutrition link—a review of the literature. Journal of the American Dietetic Association, 109(9):1566–1575. [DOI] [PubMed] [Google Scholar]
- Loehlin JC (2005). Resemblance in personality and attitudes between parents and their children. Unequal chances: Family background and economic success, pages 192–207. [Google Scholar]
- Lundberg S (2017). Noncognitive skills as human capital. In Education, Skills, and Technical Change: Implications for Future US GDP Growth, pages 219–243. University of Chicago Press. [Google Scholar]
- Marks KP, Madsen Sjö N, and Wilson P (2019). Comparative use of the ages and stages questionnaires in the usa and scandinavia: a systematic review. Developmental Medicine & Child Neurology, 61(4):419–430. [DOI] [PubMed] [Google Scholar]
- Maselko J, Sikander S, Turner EL, Bates LM, Ahmad I, Atif N, Baranov V, Bhalotra S, Bibi A, Bibi T, Bilal S, Biroli P, Chung E, Gallis JA, Hagaman A, Jamil A, LeMasters K, O’Donnell K, Scherer E, Sharif M, Waqas A, Zaidi A, Zulfiqar S, and Rahman A (2020). Effectiveness of a peer-delivered, psychosocial intervention on maternal depression and child development at 3 years postnatal: a cluster randomised trial in Pakistan. The Lancet Psychiatry, 7(9):775–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milazzo A (2018). Why are adult women missing? son preference and maternal survival in india. Journal of Development Economics, 134:467–484. [Google Scholar]
- Moroni G, Nicoletti C, and Tominey E (2019). Child Socio-Emotional Skills: The Role of Parental Inputs.
- Nangle D, Erdley C, and Schwartz-Mette R (2020). Social Skills Across the Life Span, volume 1. Academic Press. [Google Scholar]
- National Scientific Council on the Developing Child (2012). Establishing a level foundation for life: Mental health begins in early childhood. Harvard University, Center on the Developing Child. [Google Scholar]
- Nores M, Bernal R, and Barnett WS (2019). Center-based care for infants and toddlers: The aeiotu randomized trial. Economics of Education Review, 72:30–43. [Google Scholar]
- Oaxaca R (1973). Male-female wage differentials in urban labor markets. International Economic Review, pages 693–709. [Google Scholar]
- O’hara MW and Swain AM (1996). Rates and risk of postpartum depression—a meta-analysis. International review of psychiatry, 8(1):37–54. [Google Scholar]
- Parsons CE, Young KS, Rochat TJ, Kringelbach ML, and Stein A (2012). Postnatal depression and its effects on child development: a review of evidence from low-and middle-income countries. British medical bulletin, 101(1):57–79. [DOI] [PubMed] [Google Scholar]
- Rahman A, Fisher J, Bower P, Luchters S, Tran T, Yasamy MT, Saxena S, and Waheed W (2013). Interventions for common perinatal mental disorders in women in low-and middle-income countries: a systematic review and meta-analysis. Bulletin of the World Health Organization, 91:593–601I. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A, Malik A, Sikander S, Roberts C, and Creed F (2008). Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural pakistan: a cluster-randomised controlled trial. Lancet, 372(9642):902–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rayce SB, Rasmussen IS, Klest SK, Patras J, and Pontoppidan M (2017). Effects of parenting interventions for at-risk parents with infants: a systematic review and meta-analyses. BMJ Open, 7(12):e015707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, Kuncel NR, Shiner R, Caspi A, and Goldberg LR (2007). The power of personality: The comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspectives on Psychological science, 2(4):313–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salisbury MR, Roos LE, Horn SR, Peake SJ, and Fisher PA (2022). The effectiveness of keep for families of children with developmental delays: Integrating find video coaching into parent management training—oregon model: A randomized trial. Prevention Science, 23(6):1029–1040. [DOI] [PubMed] [Google Scholar]
- Sathar Z, Rashida G, Hussain S, and Hassan A (2015). Evidence of son preference and resulting demographic and health outcomes in pakistan. Islamabad Population Council. [Google Scholar]
- Sikander S, Ahmad I, Atif N, Zaidi A, Vanobberghen F, Weiss HA, Nisar A, Tabana H, Ain QU, Bibi A, et al. (2019a). Delivering the thinking healthy programme for perinatal depression through volunteer peers: a cluster randomised controlled trial in pakistan. The Lancet Psychiatry, 6(2):128–139. [DOI] [PubMed] [Google Scholar]
- Sikander S, Ahmad I, Bates LM, Gallis J, Hagaman A, O’Donnell K, Turner EL, Zaidi A, Rahman A, and Maselko J (2019b). Cohort profile: Perinatal depression and child socioemotional development; the bachpan cohort study from rural pakistan. BMJ open, 9(5):e025644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikander S, Lazarus A, Bangash O, Fuhr DC, Weobong B, Krishna RN, Ahmad I, Weiss HA, Price L, Rahman A, et al. (2015). The effectiveness and cost-effectiveness of the peer-delivered thinking healthy programme for perinatal depression in pakistan and india: the share study protocol for randomised controlled trials. Trials, 16(1):534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spearman C (1904). ‘general intelligence,’ objectively determined and measured. The American Journal of Psychology, 15:201–293. [Google Scholar]
- Sprague J and Walker H (2000). Early Identification and Intervention for Youth with Antisocial and Violent Behavior. Exceptional Children, 66(3):367–379. [Google Scholar]
- Tsivos Z-L, Calam R, Sanders MR, and Wittkowski A (2015). Interventions for postnatal depression assessing the mother–infant relationship and child developmental outcomes: a systematic review. International Journal of Women’s Health, pages 429–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner EL, Sikander S, Bangash O, Zaidi A, Bates L, Gallis J, Ganga N, O’Donnell K, Rahman A, and Maselko J (2016). The effectiveness of the peer delivered thinking healthy plus (thpp+) programme for maternal depression and child socio-emotional development in pakistan: study protocol for a three-year cluster randomized controlled trial. Trials, 17(1):442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young A (2019). Channeling fisher: Randomization tests and the statistical insignificance of seemingly significant experimental results. The Quarterly Journal of Economics, 134(2):557–598. [Google Scholar]


