Abstract
Background
This study aims to systematically assess the risk factors, the overall strength of association, and evidence quality related to sepsis-associated encephalopathy.
Methods
A systematic search was conducted in the Cochrane Library, PubMed, Web of Science, and Embase for cohort or case-control studies published up to August 2023 on risk factors associated with sepsis-related encephalopathy. The selected studies were screened, data were extracted, and the quality was evaluated using the Newcastle–Ottawa Scale. Meta-analysis was performed using RevMan 5.3 software. The certainty of the evidence was assessed using the GRADE criteria.
Results
A total of 13 studies involving 1,906 participants were included in the analysis. Among these studies, 12 were of high quality, and one was of moderate quality. Our meta-analysis identified six risk factors significantly associated with Serious Adverse Events (SAE). These included APACHE II, SOFA, age, tau protein, and IL-6, which were found to be risk factors with significant effects (standard mean difference SMD: 1.24–2.30), and albumin, which was a risk factor with moderate effects (SMD: −0.55). However, the certainty of evidence for the risk factors identified in this meta-analysis ranged from low to medium.
Conclusion
This systematic review and meta-analysis identified several risk factors with moderate to significant effects. APACHE II, SOFA, age, tau protein, IL-6, and albumin were associated with sepsis-related encephalopathy and were supported by medium- to high-quality evidence. These findings provide healthcare professionals with an evidence-based foundation for managing and treating hospitalized adult patients with sepsis-related encephalopathy.
Keywords: sepsis, encephalopathy, delirium, risk factors, meta-analysis
Introduction
Sepsis is a life-threatening disease caused by a dysregulation of the body’s response to infection (1). To distinguish sepsis-induced brain dysfunction from intracranial infection, sepsis-associated encephalopathy (SAE) was introduced and defined as diffuse brain dysfunction caused by a systemic immune-inflammatory response to a disease without clinical or laboratory evidence of direct brain infection (2). Sepsis-associated encephalopathy (SAE) and sepsis-associated delirium (SAD) are closely related neurological manifestations of sepsis. SAD, a subtype of SAE, explicitly denotes the acute and fluctuating cognitive impairments that occur in the context of sepsis. While all patients with SAD have SAE, not all SAE patients exhibit the characteristic confusion and reduced awareness seen in delirium. SAE usually presents as an acute deterioration in mental status, manifested by cognitive confusion, impaired consciousness, disorientation, agitation, rigidity, and coma (3). The pathophysiologic basis of SAE is very complex and involves multiple mechanisms that lead to brain dysfunction and injury (4). One of its main mechanisms is the release of pro-inflammatory cytokines, which leads to the breakdown of the blood-brain barrier (BBB), causing the influx of immune cells and inflammatory mediators into the brain (5).
SAE is considered the most common cause of encephalopathy in the intensive care unit (ICU) (6). Sepsis has a variety of complications, among which sepsis-associated encephalopathy (SAE) is one of the critical clinical manifestations, and severe SAE can occur in about 30 to 70% of patients with sepsis (7). In a landmark study of 50 non-sedated ICU sepsis patients, SAE was observed in 54% of patients (8). The incidence reported in a specific French multicenter cohort of ICUs was 53 percent (9). SAE prevalence is up to 68% in US MIMIC-IV and eICU databases (10). The diagnostic criteria for sepsis have evolved from Sepsis 1.0 to Sepsis 3.0 (11–13). There are no standardized criteria for the diagnosis of SAE, and the following diagnostic criteria are currently in use: (1) cognitive and neuropsychiatric disorders documented by healthcare professionals (doctors and nurses); (2) manifestations of Delirium (diagnosed by assessment methods such as CAM-ICU); and (3) Glasgow Coma Score (GCS) <15 (6, 14–16). Numerous studies have shown that SAEs are associated with increased short-term mortality, prolonged hospitalization, or over-expenditure of healthcare resources and have the potential to cause permanent neurological sequelae (17–19).
This systematic review aimed to identify key risk factors for sepsis-associated encephalopathy. Historically, there have been several problems with research reviews on SAE, such as confusing diagnoses of SAE, different study sample sizes, and different clinical populations. Identifying risk factors for SAE will help develop and implement prevention strategies for patients with sepsis.
Methods
Study protocol
It is a systematic review and meta-analysis assessing risk factors for sepsis-associated encephalopathy. Before the study started, a proposal was developed and registered in PROSPERO (CRD42023483721) (see Supplementary Table S1 for PROSPERO protocol). This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines (20).
Search strategy
We based search terms on Medical Subject Headings (MeSH) and other standard (controlled vocabulary) terms. A concept-based approach was used, including terms related to “Sepsis,” “Encephalopathy,” “Delirium,” “Risk Factors,” and others. Supplementary Table S2 details the entire search strategy. Two reviewers (ZZ and LJ) independently searched the Web of Science, Cochrane Library, Embase, and PubMed databases from inception to August 10, 2023. Our research team then searched the references of relevant studies to identify possible additional eligible studies. We used Endnote documentation software as a literature screening tool. Our research team repeated this process until we found no new relevant papers. Any discrepancies or differences were resolved through discussion or consultation with a third reviewer to reach a consensus.
Inclusion and exclusion criteria
Inclusion criteria
Study subjects
We included studies involving human subjects aged 18 and above.
Case number requirements
Each study must include at least five cases of sepsis-associated encephalopathy (SAE), ensuring a representative dataset and statistical robustness.
Diagnostic tools
Included studies must utilize industry-recognized diagnostic or assessment tools for SAE to ensure consistency and accuracy in case diagnosis and evaluation (6, 14–16).
Type of study
Only studies assessing risk factors for the onset of SAE were included. Specifically, we focused on cohort, case-control, and cross-sectional studies as these designs are suitable for identifying associations between risk factors and disease occurrence.
Publication requirements
Studies must be peer-reviewed, published in scientific journals, and provide full-text articles for comprehensive quality assessment and data extraction.
Exclusion criteria
Specific patient groups
We excluded studies involving intracranial infections as their pathology and treatment could significantly differ from those of standard SAE patients, potentially skewing the results.
Study design limitations
We excluded case reports and case series involving four or fewer patients due to their insufficient data volume to support broad scientific conclusions. Similarly, literature reviews were excluded as they often rely on secondary data, which may not provide original data or detailed methods.
Language limitations
Only studies published in English were included to ensure accurate understanding and analysis of the data by our research team.
Study selection and data extraction
Data extraction was independently and systematically conducted by two reviewers (ZZ and LG) using a pre-specified data extraction form; any disputes were resolved through consensus or adjudicated by a third reviewer (HZ) until the disagreement was resolved. Data collection included study characteristics: first author, publication year, study design, total number of patients, age, gender, incidence of SAE, sepsis diagnostic criteria, and SAE diagnostic criteria. The baseline characteristics of the included studies are illustrated in Table 1.
Table 1.
Characteristics of the 13 studies.
| Study | County | Study design | Age (year) | Male/female | Total patients | Cases number | Controls number | SAE incidence (%) | Sepsis diagnostic criteria | SAE assessment tools/diagnostic criteria |
|---|---|---|---|---|---|---|---|---|---|---|
| Li et al. (2011) | China | Case-control | 51.1 ± 27.1 | 164/120 | 284 | 107 | 177 | 37.68% | Sepsis2.0 | Data recorded by medical staff |
| Zhang et al. (2012) | China | Case-control | 51.5 ± 14.8 | 157/75 | 232 | 41 | 191 | 17.67% | Sepsis2.0 | Data recorded by medical staff |
| Zhao et al. (2019) | China | Cohort | 61.7 ± 13.0 | 64/45 | 109 | 27 | 82 | 24.77% | Sepsis1.0 | Data recorded by medical staff |
| Chen et al. (2023) | China | Cohort | 64.3 ± 15.5 | 61/29 | 90 | 57 | 33 | 63.33% | Sepsis3.0 | GCS <15 |
| Lu et al. (2016) | China | Cohort | 58.7 ± 8.4 | 57/29 | 86 | 34 | 52 | 39.53% | Sepsis2.0 | Data recorded by medical staff |
| Kristo et al. (2018) | Finland | Case-control | 64.2 ± 16.9 | 14/8 | 22 | 10 | 12 | 45.45% | Sepsis1.0 | CAM-ICU |
| Chen et al. (2020) | China | Case-control | 58.6 ± 20.1 | 213/78 | 291 | 127 | 164 | 43.64% | Sepsis3.0 | GCS <15 OR CAM-ICU |
| Jin et al. (2022) | China | Cohort | 75.3 ± 10.4 | 155/67 | 222 | 132 | 90 | 59.46% | Sepsis3.0 | GCS <15 OR CAM-ICU |
| Yeunwoo et al. (2020) | Korea | Case-control | 67.3 ± 15.0 | 95/80 | 175 | 107 | 68 | 61.14% | Sepsis1.0 | CAM-ICU |
| Feng et al. (2021) | China | Cohort | 53.0 ± 11.0 | 20/31 | 51 | 20 | 31 | 39.22% | Sepsis3.0 | CAM-ICU |
| Duc et al. (2014) | Belgium | Case-control | 65.0 ± 14.0 | 83/45 | 128 | 107 | 21 | 83.59% | Sepsis2.0 | GCS <15 OR CAM-ICU |
| Feng et al. (2017) | China | Cohort | 56.7 ± 15.0 | 107/68 | 175 | 74 | 101 | 42.29% | Sepsis1.0 | CAM-ICU |
| Li et al.(2022) | China | Case-control | 37.5 ± 4.5 | 18/23 | 41 | 21 | 20 | 51.22% | Diagnostic criteria for burn infection | Data recorded by medical staff |
When only 1 study provided data on the association between a potential risk factor and SAE, we reported the estimate extracted from the original article in the table (i.e., no meta-analysis was performed). When two or more studies provided data on the association between a potential risk factor and SAE, we calculated a meta-analyzed estimate of that possible association. When encountering studies that provided unadjusted and adjusted estimates, we preferred to use adjusted effect estimates because they represent effect estimates closer to the actual value (i.e., less biased). If forecasts from different overlapping cohorts were available, we used data from the report with the largest sample size to avoid duplicating data in the meta-analysis.
Definitions and outcomes
The diagnostic criteria for sepsis are constantly being updated. There are also no uniform diagnostic criteria for sepsis-associated encephalopathy. In each study we included, the diagnosis of both conditions varied. If it does not violate general principles, we respect the diagnostic criteria for sepsis and sepsis-associated encephalopathy used by researchers in each study and directly extract patient information from the data published in each study. The primary outcome of this study was the risk factors of sepsis-associated encephalopathy.
Pre-specified subgroup analysis and heterogeneity analysis
We will group the studies included based on the type of study design (case-control studies or cohort studies). Additionally, due to the lack of uniform diagnostic criteria for sepsis-associated encephalopathy, we will also group the studies based on whether the diagnosis in the included studies was made using objective scoring (GCS <15 or CAM-ICU) or based on the subjective evaluation of medical personnel. If heterogeneity analysis is required, we will determine the source of heterogeneity by employing a study-by-study exclusion approach for the included studies.
Quality evaluation and certainty assessment
Two independent authors assessed the included studies’ methodological strength and risk of bias using the Newcastle–Ottawa Scale (NOS) (22). We used this assessment tool to evaluate the design quality of nonrandomized case-control and cohort studies. Scores were assigned based on selection criteria, comparability, and outcome (cohort studies) or exposure (case-control studies). The maximum score of 9 reflects the highest quality.
We used the Grades of Recommendations, Assessment, Development, and Evaluation (GRADE) evidence rating system to assess the credibility of the available evidence for the relevant factors associated with this meta-analysis (23, 24). We initially regarded observational studies as being of poor quality. Depending on the GRADE criteria, the level of credibility may be reduced (with five domains, including the risk of bias, inconsistency, circumstantial evidence, uncertainty, or publication bias) or increased (with three fields, including larger effect sizes, dose-response relationships, or confounders). We ultimately categorized the credibility of the evidence as high, moderate, low, or very low.
Statistical analyses
We used Review Manager (version 5.3; Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) (25) to perform meta-analysis. Continuous variables were pooled using standard mean difference (SMD), and We calculated a 95% confidence interval (CI). In contrast, binary variables were pooled using odds ratio (OR), and a 95% confidence interval (CI) was calculated. A fixed effects model was used when statistical heterogeneity was low (I2 ≤ 50%). When statistical heterogeneity was high (I2 > 50%), meta-analysis was performed using a random-effects model, and sensitivity and subgroup analyses were performed to investigate potential sources of heterogeneity (26). p < 0.05 was considered statistically significant.
Results
Study process
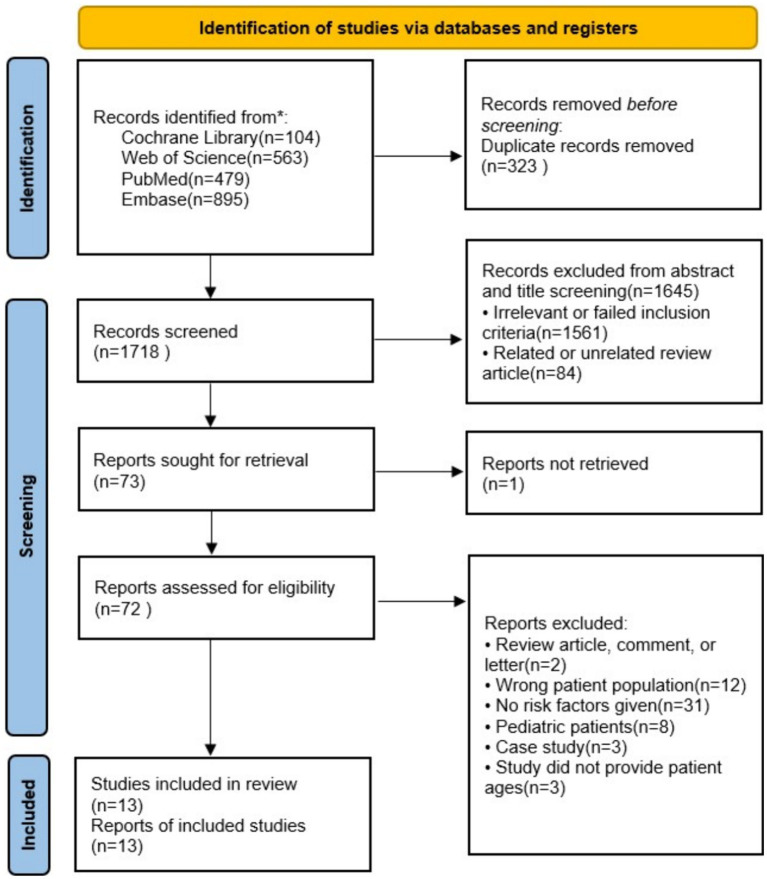
A flow diagram for study selection is shown in Figure 1. Through database searching from inception to August 10, 2023, the date of our final search, we identified 2,041 original literature records. After the removal of duplicates, 1,718 records remained. Of these, 1,645 were excluded after screening titles and abstracts as they met our exclusion criteria. Excluding one article that could not be retrieved, we assessed the full texts of the remaining 72 articles. Ultimately, a total of 13 studies met the eligibility criteria for a full-text review (27–39).
Figure 1.
Flow diagram of the literature and selection in the meta-analysis.
Study characteristics
Of the 13 studies included, there were six cohort studies and seven case-control studies. All these studies were published in English. The total sample size of these studies was 1906, with a cumulative case group of 864 and a control group of 1,042. The prevalence of SAE ranged from 17.67 to 83.59%. The studies were published between 2011 and 2023. The included studies were conducted in multiple countries, including China (n = 10), South Korea (n = 1), Finland (n = 1), and Belgium (n = 1). Thirteen studies were conducted in single-center settings. One study exclusively utilized the Glasgow Coma Scale (GCS) criteria for assessing SAE. Four studies solely employed the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) criteria for evaluating SAE. Three studies incorporated both GCS and CAM-ICU criteria for the assessment of SAE. Additionally, five studies assessed SAE through clinical records maintained by healthcare professionals (more details are seen in Table 1).
Quality evaluation of included studies
According to the NOS scores, 12 were high-quality studies, and one was of moderate quality (Supplementary Table S3). When performing multivariate analyses, explanations of the factors that accounted for most of the lost points were made more evident.
GRADE assessment of the certainty of the evidence
In our study, observational cohort studies were initially considered low quality. However, there was no high-quality evidence for any of the risk factors regarding deterministic assessment. Only APACHE II, SOFA, age, dependent activities, high care needs, low level of consciousness, and ALT showed moderate-quality evidence (Table 2). For all other risk factors, the certainty of evidence was categorized as low. The reduced quality of evidence for some risk factors was attributed to variations in study results and imprecision.
Table 2.
Potential risk factors for SAE and its effect estimates.
| Potential risk factor for SAE | Number of studies | Total sample | Effect estimates (95% CI), random-effects meta-analysis | Heterogeneity test | p-value | Effect size model | Certainty in the evidence using the GRADE approach | |
|---|---|---|---|---|---|---|---|---|
| I2 | Chi2 | |||||||
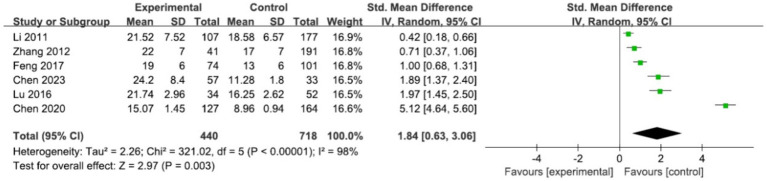
| APACHE II | 6 | 1,158 | SMD 1.84 (0.63, 3.06) | 98% | 321.02 | 0.003 | Random | Medium |
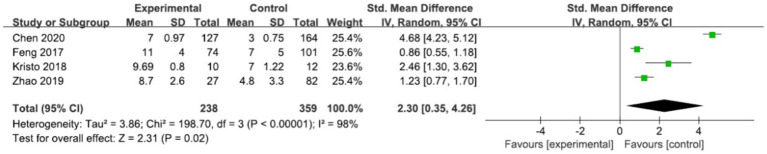
| SOFA | 4 | 597 | SMD 2.30 (0.35, 4.26) | 98% | 198.7 | 0.02 | Random | Medium |
| GCS | 1 | 232 | SMD −0.94 (−1.28, −0.59) | NA | NA | NA | NA | Low |
| Age | 3 | 688 | SMD 1.24 (0.71, 1.78) | 90% | 20.28 | <0.00001 | Random | Medium |
| Hypertension | 1 | 291 | OR 1.82 (1.07, 3.10) | NA | NA | NA | NA | Low |
| COPD | 1 | 222 | OR 2.70 (1.34, 5.60) | NA | NA | NA | NA | Low |
| Dependent activity | 1 | 175 | OR 5.83 (2.85, 11.93) | NA | NA | NA | NA | Medium |
| High nursing needs | 1 | 175 | OR 3.75 (1.96, 7.17) | NA | NA | NA | NA | Medium |
| Low level of consciousness | 1 | 175 | OR 4.23 (1.90, 9.44) | NA | NA | NA | NA | Medium |
| Tachypnoea | 1 | 175 | OR 2.80 (1.49, 5.28) | NA | NA | NA | NA | Low |
| Gastrointestinal infections | 1 | 291 | OR 2.03 (1.14, 3.63) | NA | NA | NA | NA | Low |
| Detection rate of enterococcus | 1 | 291 | OR 2.30 (1.10, 4.80) | NA | NA | NA | NA | Low |
| Heart rate | 1 | 232 | SMD 0.52 (0.18, 0.86) | NA | NA | NA | NA | Low |
| PaO2 | 1 | 284 | SMD −0.36 (−0.61, −0.12) | NA | NA | NA | NA | Low |
| ALT | 1 | 284 | SMD 0.37 (0.13, 0.61) | NA | NA | NA | NA | Medium |
| Blood lactate | 1 | 232 | SMD 0.43 (0.09, 0.77) | NA | NA | NA | NA | Low |
| Serum sodium | 2 | 454 | SMD −0.15 (−1.29, 0.99) | 95% | 21.47 | 0.8 | Random | Low |
| Platelets | 1 | 232 | SMD −0.35 (−0.69, −0.01) | NA | NA | NA | NA | Low |
| Serum albumin | 2 | 322 | SMD −0.55 (−0.82, −0.28) | 0% | 0.78 | <0.0001 | Fixed | Low |
| PH | 1 | 232 | SMD −0.39 (−0.73, −0.05) | NA | NA | NA | NA | Low |
| Tau protein | 2 | 150 | SMD 1.52 (0.58, 2.47) | 78% | 4.48 | 0.002 | Random | Low |
| MFI of CD86 in NKT | 1 | 90 | SMD-2.19 (−2.73,-1.65) | NA | NA | NA | NA | Low |
| CD4+ | 1 | 86 | SMD −1.69 (−2.20, −1.19) | NA | NA | NA | NA | Low |
| IL-6 | 2 | 63 | SMD 1.84 (0.24, 3.44) | 85% | 6.58 | 0.02 | Random | Low |
| S100 β | 1 | 22 | SMD 1.65 (0.66, 2.65) | NA | NA | NA | NA | Low |
| THRR index <1.09 | 1 | 51 | OR 5.78 (1.22, 27.26) | NA | NA | NA | NA | Low |
| Mean value for rSO2 <55% | 1 | 51 | OR 3.86 (1.02–14.55) | NA | NA | NA | NA | Low |
| Cortisol | 2 | 169 | SMD 3.67 (−3.01, 10.36) | 98% | 55.26 | 0.28 | Random | Low |
| ACTH | 1 | 41 | SMD 2.73 (1.86, 3.60) | NA | NA | NA | NA | Low |
CI, confidence interval; NA, not applicable; OR, odds ratio; RR, risk ratio; SMD, standard mean difference; PaO2, partial pressure of oxygen in arterial blood; ALT, alanine aminotransferase; APACHEII, Acute Physiology and Chronic Health Evaluation II; PH, potential of hydrogen; SOFA, Sequential Organ Failure Assessment; MFI of CD86 in NKT, Mean Fluorescence Intensity of CD86 in Natural Killer T cells; CD4+, cluster of differentiation 4; IL-6, interleukin-6; S100 β, S100 calcium-binding protein beta; COPD, chronic obstructive pulmonary disease; THRR, transient hyperemic response ratio; rSO2, regional cerebral oxygen saturation; ACTH, adrenocorticotropic hormone.
Meta-analysis of risk factors for SAE
APACHE II
We conducted a meta-analysis of data from 6 studies (27, 28, 30, 31, 33, 38) examining the relationship between APACHE II and SAE, with 440 cases in the SAE group and 718 cases in the non-SAE group. The results showed a statistically positive effect between the two {[SMD = 1.84, 95% CI (0.63, 3.06)], p = 0.003} (Table 2 and Figure 2). However, there was a high degree of heterogeneity between studies (I2 = 98%, p < 0.00001), and the source of the heterogeneity could not be determined despite a study-by-study exclusion maneuver. Subgroup analyses were performed based on differences in study design and diagnostic criteria for encephalopathy between studies (Supplementary Figures S1, S2).
Figure 2.
Forest plot of the studies in APACHEII.
SOFA
The effect of SOFA on SAE was examined in four studies (29, 32, 33, 38). There were 238 cases in the SAE group and 359 cases in the non-SAE group. The results demonstrated a statistically significant positive association between the two variables, as evidenced by a standard mean difference (SMD) of 2.3 with a 95% confidence interval (CI) ranging from 0.35 to 4.26 (p = 0.02) (Table 2 and Figure 3). Notably, the studies had substantial heterogeneity (I2 = 98%, p < 0.00001). Despite conducting a thorough exclusion analysis for each study, the root cause of this heterogeneity remained elusive. Consequently, subgroup analyses were undertaken to explore the potential effects of variations in study designs across the studies (Supplementary Figure S3).
Figure 3.
Forest plot of the studies in SOFA.
Age
In three studies, the impact of age on sepsis-associated encephalopathy (SAE) was examined, and a meta-analysis was conducted (33, 34, 38). The SAE group comprised 368 cases, while the non-SAE group included 322 cases. The results showed a statistically positive effect between the two {[SMD = 1.24, 95% CI (0.71, 1.78)], p < 0.00001} (Table 2 and Figure 4). However, there was a high degree of between-study heterogeneity (I2 = 90%, p < 0.0001), and despite a study-by-study exclusion maneuver, the source of the heterogeneity could not be determined. Subgroup analyses were then performed based on differences in study design between studies (Supplementary Figure S4).
Figure 4.
Forest plot of the studies in age.
Albumin and serum sodium
We conducted a meta-analysis of data from 2 studies (28, 30) examining the relationship between albumin and SAE, with 98 cases in the SAE group and 224 cases in the non-SAE group. The results showed a statistically negative effect between the two {[SMD = −0.55, 95% CI (−0.82, −0.28)], p < 0.0001} and low heterogeneity in the meta-analysis. In our meta-analysis (28, 34), sodium was not found to be a significant risk factor in the occurrence of SAE (p = 0.8) (Table 2 and Supplementary Figures S5, S6).
Tau protein, IL-6 and cortisol
The effect of tau protein on SAE was examined in 2 studies (29, 39). The results showed a statistically positive effect between the two {[SMD = 1.52, 95% CI (0.58, 2.47)], p = 0.002}, with high heterogeneity in the meta-analysis (I2 = 78%, p = 0.03). The effect of IL-6 on SAE was examined in 2 studies (32, 39). The results showed a statistically positive effect between the two {[SMD = 1.84, 95% CI (0.24, 3.44)], p = 0.02}, with high heterogeneity in the meta-analysis (I2 = 85%, p = 0.01). In our meta-analysis (37, 39), cortisol was not found to be a significant risk factor in SAE (p = 0.28) (Table 2 and Supplementary Figures S7–S9).
Other risk factors
In our study, multiple regression analysis identified 21 potential risk factors for developing encephalopathy in patients with sepsis. These factors include GCS, hypertension, COPD, dependent activity, high nursing needs, low level of consciousness, tachypnoea, gastrointestinal infections, detection rate of enterococcus, heart rate, PaO2, ALT, blood lactate, platelets, pH, MFI of CD86 in NKT cells, CD4+, S100 β, THRR index <1.09, mean value for rSO2 <55%, and ACTH. However, as these risk factors were only reported in a single study and insufficient data from multiple studies for a meta-analysis, they were omitted in our meta-analysis (more details seen in Table 2).
Discussion
Six risk factors significantly associated with SAE were identified in this meta-analysis of 13 studies involving 1,906 patients hospitalized with sepsis. Among these, APACHE II, SOFA, age, tau protein, and IL-6 were found to be risk factors with significant effects (SMD: 1.24–2.30), and albumin was a risk factor with moderate effects (SMD: −0.55). However, for the risk factors identified in this meta-analysis, the certainty of evidence was low to moderate.
According to our results, the incidence of APACHE II and SOFA in SAE was statistically a risk factor for more significant effects, but considerable heterogeneity was seen between studies. We could not determine the heterogeneity source even after sensitivity analyses.
We performed subgroup analyses based on some subgroups that may affect heterogeneity, such as differences in study design and diagnostic criteria for encephalopathy. Despite these subgroups, there was still more significant heterogeneity in the within-group analyses of APACHE II and SOFA, suggesting that the significant inconsistency in the study results was not caused by differences in study design and diagnostic criteria for encephalopathy and that further exploration of the sources of heterogeneity is needed. Both APACHE II and SOFA scores are important indicators of the severity of a patient’s condition and have been widely used to evaluate critically ill patients (8, 40). Encephalopathy is seen as an indicator of a poor prognosis for patients suffering from sepsis; the severity of encephalopathy is closely related to the severity of the systemic disease and requires prompt and aggressive treatment. According to our study, both APACHE II and SOFA scores were risk factors for a more significant effect of SAE, with advantages in assessing the severity and prognosis of encephalopathy, consistent with previous reports (41). Compared to non-SAE patients, SAE patients are more severely ill, as evidenced by higher costs, prolonged hospitalization, and higher duration of mechanical ventilation (17–19). Also, patients with SAE had a higher hospital mortality rate, suggesting that once SAE occurs in septic patients, the mortality rate is significantly higher. In the studies included in our meta-analysis, the incidence of SAE in septic patients may be as high as 83.59% (37). The high incidence of SAE may explain why sepsis is still fatal today. It is important to note that GCS scores <15 were used to diagnose patients with SAE; however, GCS scores are a component of SOFA and APACHE II scores. Patients with higher SOFA and APACHE II scores were likelier to have SAE, which may have biased the conclusions (34).
In our study, age incidence in SAE was also statistically a risk factor for more significant effects, but considerable heterogeneity was seen between studies. Sensitivity analyses could not identify the source of the heterogeneity. Because only three studies were included, we did not perform subgroup analyses, and the small sample size made the results we obtained less reliable. There was a significant publication bias and other circumstances. Elderly patients are at higher risk of developing sepsis, and critically ill patients with underlying disease usually have a more rapid progression and a poorer prognosis. Especially if the underlying illness is hypertension COPD, these patients may be more likely to develop central nervous system complications (9, 42–44). In addition, hospitalization of elderly patients is often associated with an increase in the need for nursing care due to dependence on daily activities and poor self-care ability, which further aggravates their condition (45, 46). This finding is consistent with some of the SAE-associated risk factors identified in our META analysis, including Age, COPD, and others.
Laboratory parameters such as tau protein, IL-6, and albumin in our study, although risk factors for predicting a medium to significant effect for the occurrence of SAEs, were included in a limited number of studies with small sample sizes and were only supported by low-quality evidence. In our meta-analysis, we applied the GRADE system to ensure the scientific validity of our findings. Despite many studies initially rated as low quality, careful reassessment allowed for upgrades based on study design and execution. We recognize heterogeneity due to geographical and ethnic variations, which introduces some uncertainty in interpretation. Also, potential biases and unmeasured confounders in primary studies could affect the generalizability of our results. Our findings, while insightful, should be applied cautiously in clinical practice, integrating high-quality evidence, clinical experience, and patient values. They provide a basis for guidelines but require adaptation to local contexts. Future research should aim to enhance study design quality, increase sample sizes, and broaden demographic coverage to improve evidence quality and extend its applicability.
Further inflammation is needed in the future through more extensive studies supported by higher levels of evidence. However, IL-6 and albumin are conveniently available and cost-effective biomarkers during hospitalization because they can be calculated from standard peripheral blood tests without additional effort or expense. Monitoring changes in IL-6 and albumin levels can be a useful clinical tool for assessing the risk of SAE and developing appropriate medical interventions. This meta-analysis needed to have identified specific thresholds for predicting SAE due to the limited sample size and potential heterogeneity of baseline values in different studies. Future prospective studies are required to establish validated entries for predicting SAE. We confidently use IL-6 and Albumin as clinical tools for predicting SAE risk.
Advantages and limitations
The main strength of this study is that it is the first meta-analysis of risk factors for SAE, where multiple factors affecting SAE were analyzed separately. However, like all studies, this study has some limitations. First, the diagnostic criteria for sepsis and sepsis-associated encephalopathy differed between studies. The diagnostic criteria for sepsis 1.0 have high sensitivity but low specificity, which may lead to overdiagnosis while missing some immunosuppressed patients. Sepsis 2.0 is a transitional criterion. However, the latest definition of sepsis 3.0 remains controversial. When a patient’s SOFA score changes by ≥2 points, the patient’s condition is exacerbated, caused by an infection that may adversely affect the early recognition and treatment of sepsis and lead to a delayed diagnosis of the disease. In addition, non-infectious conditions in critically ill patients may also lead to organ damage that can achieve a SOFA score of ≥2, leading to overdiagnosis. The diagnostic criteria for burn infection are expressly limited to burn patients (21). All four diagnostic criteria for sepsis are deficient. Among the currently used diagnostic criteria for SAE, GCS <15 and CAM-ICU are relatively objective diagnostic methods. At the same time, data recorded by medical staff is somewhat subjective; all three diagnostic procedures are based on consistent clinical symptoms of SAE. Second, only English-language databases were searched, possibly excluding relevant studies published in other languages. Third, only a few studies were included for certain factors such as tau protein, IL-6, and albumin, resulting in small sample sizes for these studies. Fourth, the exclusion of minors under the age of 18 limits the generalizability of the results. In addition, most of the studies were conducted in Asia and Europe, limiting the applicability of generalizing the results to other parts of the world.
Therefore, future research needs to address these limitations and provide a more comprehensive investigation of the risk factors associated with SAE. Efforts should include studies from different geographic regions and populations, consider a broader range of languages, and use standardized assessment methods. By overcoming these limitations, we can further advance our understanding of SAE and provide more substantial evidence for clinical practice.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
ZZ: Writing – original draft. LG: Writing – review & editing. LJ: Writing – review & editing. HD: Writing – review & editing. LS: Writing – review & editing. HZ: Writing – review & editing.
Funding Statement
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1379019/full#supplementary-material
Glossary
| SAE | Sepsis-related encephalopathy |
| BBB | Blood-brain barrier |
| ICU | Intensive care unit |
| GCS | Glasgow Coma Score |
| CAM-ICU | Confusion Assessment Method for the Intensive Care Unit |
| MeSH | Medical Subject Headings |
| NOS | Newcastle–Ottawa Scale |
| GRADE | Grading of Recommendations Assessment |
| SMD | Standard mean difference |
| CI | Confidence interval |
| OR | Odds ratio |
| NA | Not applicable |
| RR | Risk ratio |
| PaO2 | Partial pressure of oxygen in arterial blood |
| ALT | Alanine aminotransferase |
| APACHEII | Acute Physiology and Chronic Health Evaluation II |
| PH | Potential of hydrogen |
| SOFA | Sequential Organ Failure Assessment |
| MFI of CD86 in NKT | Mean Fluorescence Intensity of CD86 in Natural Killer T cells |
| CD4+ | Cluster of differentiation 4 |
| IL-6 | Interleukin-6 |
| S100 β | S100 calcium-binding protein beta |
| COPD | Chronic obstructive pulmonary disease |
| THRR | Transient hyperemic response ratio |
| rSO2 | Regional cerebral oxygen saturation |
| ACTH | Adrenocorticotropic hormone |
References
- 1.Slooter AJC, Otte WM, Devlin JW, Arora RC, Bleck TP, Claassen J, et al. Updated nomenclature of delirium and acute encephalopathy: statement of ten societies. Intensive Care Med. (2020) 46:1020–2. doi: 10.1007/s00134-019-05907-4, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson JX, Young GB. Progress in clinical neurosciences: sepsis-associated encephalopathy: evolving concepts. Can J Neurol Sci. (2003) 30:98–105. doi: 10.1017/S031716710005335X, PMID: [DOI] [PubMed] [Google Scholar]
- 3.Iacobone E, Bailly-Salin J, Polito A, Friedman D, Stevens RD, Sharshar T. Sepsis-associated encephalopathy and its differential diagnosis. Crit Care Med. (2009) 37:S331–6. doi: 10.1097/CCM.0b013e3181b6ed58 [DOI] [PubMed] [Google Scholar]
- 4.Heming N, Mazeraud A, Verdonk F, Bozza FA, Chrétien F, Sharshar T. Neuroanatomy of sepsis-associated encephalopathy. Crit Care. (2017) 21:65. doi: 10.1186/s13054-017-1643-z, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharshar T, Annane D, de la Grandmaison GL, Brouland JP, Hopkinson NS, Françoise G. The neuropathology of septic shock. Brain Pathol. (2004) 14:21–33. doi: 10.1111/j.1750-3639.2004.tb00494.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bleck TP, Smith MC, Pierre-Louis SJ, Jares JJ, Murray J, Hansen CA. Neurologic complications of critical medical illnesses. Crit Care Med. (1993) 21:98–103. doi: 10.1097/00003246-199301000-00019 [DOI] [PubMed] [Google Scholar]
- 7.Czempik PF, Pluta MP, Krzych ŁJ. Sepsis-associated brain dysfunction: a review of current literature. Int J Environ Res Public Health. (2020) 17:5852. doi: 10.3390/ijerph17165852, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eidelman LA, Putterman D, Putterman C, Sprung CL. The spectrum of septic encephalopathy. Definitions, etiologies, and mortalities. JAMA. (1996) 275:470–3. doi: 10.1001/jama.1996.03530300054040 [DOI] [PubMed] [Google Scholar]
- 9.Sonneville R, de Montmollin E, Poujade J, Garrouste-Orgeas M, Souweine B, Darmon M, et al. Potentially modifiable factors contributing to sepsis-associated encephalopathy. Intensive Care Med. (2017) 43:1075–84. doi: 10.1007/s00134-017-4807-z, PMID: [DOI] [PubMed] [Google Scholar]
- 10.Lu X, Qin M, Walline JH, Gao Y, Yu S, Ge Z, et al. Clinical phenotypes of SEPSIS-associated encephalopathy: a retrospective cohort study. Shock. (2023) 59:583–90. doi: 10.1097/SHK.0000000000002092, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. (2013) 41:580–637. doi: 10.1097/CCM.0b013e31827e83af [DOI] [PubMed] [Google Scholar]
- 12.Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med. (2008) 34:17–60. doi: 10.1007/s00134-007-0934-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. (2017) 43:304–77. doi: 10.1007/s00134-017-4683-6, PMID: [DOI] [PubMed] [Google Scholar]
- 14.Young GB, Bolton CF, Austin TW, Archibald YM, Gonder J, Wells GA. The encephalopathy associated with septic illness. Clin Invest Med. (1990) 13:297–304. PMID: [PubMed] [Google Scholar]
- 15.Eggers V, Schilling A, Kox WJ, Spies C. Septic encephalopathy. Diagnosis und therapy. Anaesthesist. (2003) 52:294–303. doi: 10.1007/s00101-003-0496-9, PMID: [DOI] [PubMed] [Google Scholar]
- 16.Chelazzi C, Consales G, De Gaudio A. Sepsis associated encephalopathy. Curr Anaesth Crit Care. (2008) 19:15–21. doi: 10.1016/j.cacc.2007.07.009 [DOI] [Google Scholar]
- 17.Ren C, Yao RQ, Zhang H, Feng YW, Yao YM. Sepsis-associated encephalopathy: a vicious cycle of immunosuppression. J Neuroinflammation. (2020) 17:14. doi: 10.1186/s12974-020-1701-3, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kikuchi DS, Campos ACP, Qu H, Forrester SJ, Pagano RL, Lassègue B, et al. Poldip2 mediates blood-brain barrier disruption in a model of sepsis-associated encephalopathy. J Neuroinflammation. (2019) 16:241. doi: 10.1186/s12974-019-1575-4, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sonneville R, Benghanem S, Jeantin L, de Montmollin E, Doman M, Gaudemer A, et al. The spectrum of sepsis-associated encephalopathy: a clinical perspective. Crit Care. (2023) 27:386. doi: 10.1186/s13054-023-04655-8, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peng YZ, Yuan ZQ, Li XL, Luo GX, Wu J. Guidelines for the diagnosis and treatment of burn infection (2012 edition). Chin J Burns. (2012) 28:401–3. doi: 10.3760/cma.j.issn.1009-2587 [DOI] [Google Scholar]
- 22.Wells GA, Wells G, Shea B, Shea B, O’Connell D, Peterson J, et al. (Eds). The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. (2014). Available at: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 23.Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. (2011) 64:401–6. doi: 10.1016/j.jclinepi.2010.07.015 [DOI] [PubMed] [Google Scholar]
- 24.Foroutan F, Guyatt G, Zuk V, Vandvik PO, Alba AC, Mustafa R, et al. GRADE guidelines 28: use of GRADE for the assessment of evidence about prognostic factors: rating certainty in identification of groups of patients with different absolute risks. J Clin Epidemiol. (2020) 121:62–70. doi: 10.1016/j.jclinepi.2019.12.023, PMID: [DOI] [PubMed] [Google Scholar]
- 25.DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. (2015) 45:139–45. doi: 10.1016/j.cct.2015.09.002, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li J, Li A, Weng Y, Zhang S, Duan M. Risk factors for sepsis-associated encephalopathy. Neural Regen Res. (2011) 6:309–12. doi: 10.3969/j.issn.1673-5374 [DOI] [Google Scholar]
- 28.Zhang LN, Wang XT, Ai YH, Guo QL, Huang L, Liu ZY, et al. Epidemiological features and risk factors of sepsis-associated encephalopathy in intensive care unit patients: 2008–2011. Chin Med J. (2012) 125:828–31. doi: 10.3760/cma.j.issn.0366-6999.2012.05.018 PMID: [DOI] [PubMed] [Google Scholar]
- 29.Zhao T, Xia Y, Wang D, Pang L. Association between elevated serum tau protein level and sepsis-associated encephalopathy in patients with severe sepsis. Can J Infect Dis Med Microbiol. (2019) 2019:1–6. doi: 10.1155/2019/1876174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen SL, Liu XY, Huang JH, Xian LH, Li XS, Wang KR, et al. The expression of CD86 in CD3+ CD56+ NKT cells is associated with the occurrence and prognosis of sepsis-associated encephalopathy in sepsis patients: a prospective observational cohort study. Immunol Res. (2023) 71:929–40. doi: 10.1007/s12026-023-09405-0, PMID: [DOI] [PubMed] [Google Scholar]
- 31.Lu CX, Qiu T, Tong HS, Liu ZF, Su L, Cheng B. Peripheral T-lymphocyte and natural killer cell population imbalance is associated with septic encephalopathy in patients with severe sepsis. Exp Ther Med. (2016) 11:1077–84. doi: 10.3892/etm.2016.3000, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Erikson K, Ala-Kokko TI, Koskenkari J, Liisanantti JH, Kamakura R, Herzig KH, et al. Elevated serum S-100β in patients with septic shock is associated with delirium. Acta Anaesthesiol Scand. (2019) 63:69–73. doi: 10.1111/aas.13228, PMID: [DOI] [PubMed] [Google Scholar]
- 33.Chen J, Shi X, Diao M, Jin G, Zhu Y, Hu W, et al. A retrospective study of sepsis-associated encephalopathy: epidemiology, clinical features and adverse outcomes. BMC Emerg Med. (2020) 20:77. doi: 10.1186/s12873-020-00374-3, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jin G, Wang S, Chen J, Hu W, Zhu Y, Xi S. Identification of sepsis-associated encephalopathy risk factors in elderly patients: a retrospective observational cohort study. Turk J Med Sci. (2022) 52:1513–22. doi: 10.55730/1300-0144.5491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim Y, Jin Y, Jin T, Lee SM. Risk factors and outcomes of sepsis-associated delirium in intensive care unit patients: a secondary data analysis. Intensive Crit Care Nurs. (2020) 59:102844. doi: 10.1016/j.iccn.2020.102844, PMID: [DOI] [PubMed] [Google Scholar]
- 36.Feng Q, Ai M, Huang L, Peng Q, Ai Y, Zhang L. Relationship between cerebral hemodynamics, tissue oxygen saturation, and delirium in patients with septic shock: a pilot observational cohort study. Front Med. (2021) 8:641104. doi: 10.3389/fmed.2021.641104, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nguyen DN, Huyghens L, Zhang H, Schiettecatte J, Smitz J, Vincent JL. Cortisol is an associated-risk factor of brain dysfunction in patients with severe sepsis and septic shock. Biomed Res Int. (2014) 2014:712742: 1–7. doi: 10.1155/2014/712742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Feng Q, Ai YH, Gong H, Wu L, Ai ML, Deng SY, et al. Characterization of sepsis and sepsis-associated encephalopathy. J Intensive Care Med. (2019) 34:938–45. doi: 10.1177/0885066617719750 [DOI] [PubMed] [Google Scholar]
- 39.Li XL, Xie JF, Ye XY, Li Y, Li YG, Feng K, et al. Value of cerebral hypoxic-ischemic injury markers in the early diagnosis of sepsis associated encephalopathy in burn patients with sepsis. Zhonghua Shao Shang Yu Chuang Mian Xiu Fu Za Zhi. (2022) 38:21–8. doi: 10.3760/cma.j.cn501120-20211006-00346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sprung CL, Peduzzi PN, Shatney CH, Schein RM, Wilson MF, Sheagren JN, et al. Impact of encephalopathy on mortality in the sepsis syndrome. The Veterans Administration Systemic Sepsis Cooperative Study Group. Crit Care Med. (1990) 18:801–6. doi: 10.1097/00003246-199008000-00001 [DOI] [PubMed] [Google Scholar]
- 41.Taylor SL, Morgan DL, Denson KD, Lane MM, Pennington LR. A comparison of the Ranson, Glasgow, and APACHE II scoring systems to a multiple organ system score in predicting patient outcome in pancreatitis. Am J Surg. (2005) 189:219–22. doi: 10.1016/j.amjsurg.2004.11.010, PMID: [DOI] [PubMed] [Google Scholar]
- 42.Hajjar I, Keown M, Frost B. Antihypertensive agents for aging patients who are at risk for cognitive dysfunction. Curr Hypertens Rep. (2005) 7:466–73. doi: 10.1007/s11906-005-0043-y [DOI] [PubMed] [Google Scholar]
- 43.Sonneville R, Vanhorebeek I, den Hertog HM, Chrétien F, Annane D, Sharshar T, et al. Critical illness-induced dysglycemia and the brain. Intensive Care Med. (2015) 41:192–202. doi: 10.1007/s00134-014-3577-0 [DOI] [PubMed] [Google Scholar]
- 44.Siew ED, Fissell WH, Tripp CM, Blume JD, Wilson MD, Clark AJ, et al. Acute kidney injury as a risk factor for delirium and coma during critical illness. Am J Respir Crit Care Med. (2017) 195:1597–607. doi: 10.1164/rccm.201603-0476OC, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. Long-term cognitive impairment after critical illness. N Engl J Med. (2013) 369:1306–16. doi: 10.1056/NEJMoa1301372, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brummel NE, Jackson JC, Pandharipande PP, Thompson JL, Shintani AK, Dittus RS, et al. Delirium in the ICU and subsequent long-term disability among survivors of mechanical ventilation. Crit Care Med. (2014) 42:369–77. doi: 10.1097/CCM.0b013e3182a645bd, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.