Abstract
Ayurveda is one of the oldest and most widely practiced traditional medical systems in the world. The ancient knowledge in this traditional medical system has yet to be fully explored. The interaction of rich knowledge from various traditional systems of medicine can open new pathways in the herbal drug discovery process. Apart from other hurdles in discovering plant-based medicines, the lack of knowledge of the differences and similarities between the theoretical doctrines of these systems is the greatest impediment to their convergence. Rasashastra is an Ayurvedic medicine section that deals with formulations that include minerals/metals, particularly Parad (mercury). According to the Ayurvedic Formulary of India, the most widely used heavy metals are mercury, arsenic, and lead. However, contemporary scientists are concerned about the use of heavy metals in Ayurvedic preparation. In this review article, we will discuss Ayurvedic medicine and the toxic effects of heavy metals.
Keywords: Ayurvedic Medicine, Heavy Metals, Herbal Medicine, Mercury
INTRODUCTION
Contemporary medications, also known as modern chemical medicines or pharmaceutical products, and traditional medicines, which are manufactured by conventional methods, are also widely used to effectively treat a variety of medical conditions.1 However, the risks associated with the use of contemporary medications have led millions of people throughout the world to turn to herbal and traditional medicines as alternative healing agents. Long-term use of modern medicine in chronic diseases has several negative consequences that most patients prefer to avoid, therefore they turn to traditional medicines.1 Many plants and their extracts found in traditional remedies have been demonstrated to exhibit a variety of biological functions.2 In the Indian system of medicine, there are over 300 formulations for treating jaundice and chronic liver diseases.3 Approximately 600 commercial traditional medicines with hepatoprotective properties are sold all over the world. Because of the enormous benefits, the majority of the world’s population relies on them in some form for various health benefits. According to World Health Organization research, traditional medicine is used as the major source of healthcare by 65% to 80% of the world’s population.4
Ayurveda is a traditional medical system with historical roots in the Indian subcontinent. Ayurveda is recognized as a medical system in India, Sri Lanka, Pakistan, Nepal, the UAE, Oman, Bangladesh, Saudi Arabia, Hungary, Bahrain, Malaysia, Serbia, Mauritius, Tanzania, Cuba, Switzerland, and Brazil, while only five countries of the European Union (EU) regulate its practices.5 Ayurveda focuses on disease prevention rather than disease therapy.6 Its origins can be traced back to the Indian subcontinent and has been practiced for more than 3,000 years. The phrase “Ayurveda” is a combination of two Sanskrit words: “Ayur,” which means “life,” and “Veda,” which means “knowledge or science.” As a result, Ayurveda is translated as the “science of life.” Ayurveda is based on the notion of keeping the interconnected relationships between the body and the mind in balance. It teaches the patients the value of knowing their body and mind and living in close interaction with nature.
Scientists have identified various bioactive substances in therapeutic plants used in Ayurveda. Rauwolfia alkaloids for hypertension, Guggulsterons as hypolipidemic agents, Mucuna pruriens for Parkinson’s disease, Picrosides for hepatic protection, Piperidines as bioavailability enhancers, Baccosides for mental retention, Psoralens for vitiligo, Phyllanthins as antivirals, Berberine, Curcumin for controlling infections, inflammation, and cancer, and Shatavarins and Withanolides as adjuvants and immunomodulators.5 Several Ayurvedic medications and formulations were also explored using a reverse pharmacology technique during the COVID-19 pandemic.5 Ayush-64, an Ayurvedic formulation used to treat malaria, has been repurposed as an adjuvant treatment for mild to moderate COVID-19.7 Anu Taila, a traditional Ayurvedic compound used for intranasal administration, demonstrated preventive potential with strong antiviral effectiveness, viral load decrease, and virus entry barrier.8 In a randomized controlled multicenter clinical trial, Withania somnifera (Ashwagandha) was found to be more effective and safer than hydroxychloroquine for COVID-19 prevention.9
Trace minerals such as zinc, gold, silver, iron, copper, magnesium, manganese, and chromium are required for particular biochemical reactions in the human body; yet they can be harmful at high levels of exposure.10 Heavy metals such as lead, arsenic, mercury, and cadmium are xenobiotics that can induce toxicity even at low doses.11,12,13,14 Metals (bhasmas) are highlighted as needed for appropriate biological functioning in Rasa Shastra Ayurveda, hence they are purposely implemented after “purification” (suddha) in the formulations. However, numerous recent research articles have shown that herbal medications are contaminated with lethal amounts of heavy metals. According to a study, 42 of 43 Ayurvedic remedies were randomly selected for analysis, and heavy metals such as mercury, lead, arsenic, and chromium were found in most of the formulations.10 Heavy metals are widely present in Ayurvedic remedies which affect negatively in the body.10
HISTORY
Ayurvedic literature has a comprehensive documentation of medicinal plants. The period of documentation can be categorized into four distinct phases. They are the Vedic period, The Classical period, the Medieval period, and the Modern period.15
1. Vedic period (circa 4000-1500 BCE)
The earliest references to Ayurveda can be found in the Vedas, the oldest sacred texts of India.16 The Rigveda, one of the oldest Vedas, mentions various medicinal plants and healing practices.
2. The classical period (circa 1500 BCE-700 CE)
The foundational text of Ayurveda, the “Charaka Samhita,” is attributed to the sage Charaka and is believed to have been written during this period.17 It covers a wide range of medical knowledge, including anatomy, diagnosis, and treatment. Another important text from this period is the “Sushruta Samhita,” attributed to the sage Sushruta. It focuses primarily on surgical techniques.
3. Medieval and post-Medieval periods (circa 700-1500 CE)
During this time, Ayurveda continued to develop and spread. The “Ashtanga Hridaya,” written by Vagbhata, is a significant text from this period, summarizing earlier Ayurvedic knowledge. Ayurveda received patronage from Indian rulers, including the Mughal emperors, which led to further advancements in the field.
4. Modern period (15th century-present)
The colonial period saw a decline in Ayurveda’s popularity as Western medicine gained prominence. In the 20th century, there was a resurgence of interest in Ayurveda, with efforts to promote indigenous medical systems in India. Modern research and integration of Ayurveda with conventional medicine have become more prevalent.
BASIC DOCTRINE PRINCIPLES
Ayurveda, the ancient system of medicine in India, is based on a set of fundamental principles and doctrines that guide its understanding of health, disease, and treatment. These principles form the core of Ayurvedic philosophy and practice. Here are the basic doctrine principles of Ayurveda:
1. Panchamahabhutas (five elements)
Ayurveda views the universe and all matter as composed of five fundamental elements: Earth (Prithvi), Water (Jala), Fire (Agni), Air (Vayu), and Ether (Akasha).18,19 These five elements (earth, water, fire, air, and ether) manifest themselves in the human body and influence health.
2. Tridosha (three doshas)
Ayurveda categorizes individuals into three primary constitutional types, or doshas (faults or defects): Vata, Pitta, and Kapha.18 These doshas are related to different combinations of the five elements (earth, water, fire, air, and ether) and influence an individual’s physical, mental, and emotional characteristics. Vata is associated with air and ether, Pitta with fire and water, and Kapha with earth and water.18 Health is believed to depend on the balance of these doshas, while imbalances can lead to disease.
3. Sapta dhatus (seven tissues)
Ayurveda recognizes seven essential tissues (Sapta Dhatus) in the human body, which are sequentially formed from the food we eat.18 These dhatus are:
I. Rakta Dhatu: blood
II. Mamsa Dhatu: muscles
III. Meda Dhatu: fat
IV. Asthi Dhatu: bone
V. Majja Dhatu: bone marrow
VI. Shukra Dhatu: reproductive fluid or semen
4. Agni (digestive fire)
Agni represents the digestive fire within the body responsible for breaking down and assimilating nutrients from food. Balanced Agni is essential for proper digestion, metabolism, and overall health. Ayurveda emphasizes maintaining Agni for optimal well-being.
5. Malas (waste products)
Malas describes the nature of waste products and their importance in maintaining health. Ayurveda recognizes three primary waste products: Malas (feces), Mutra (urine), and Sweda (sweat). Proper elimination of waste is crucial for maintaining health, as waste accumulation can lead to disease.
6. Prakriti (constitution)
Each individual has a unique constitution or Prakriti, which is determined by their dominant dosha or combination of doshas at birth. Understanding one’s Prakriti helps tailor lifestyle, diet, and treatment to maintain balance and prevent illness.
7. Vikriti (imbalance)
Vikriti refers to the current state of imbalance in an individual’s doshas, which may differ from their Prakriti. Identifying and addressing Vikriti is central to Ayurvedic diagnosis and treatment.
8. Dinacharya and ritucharya (daily and seasonal routines)
Ayurveda emphasizes the importance of daily and seasonal routines for maintaining balance and promoting health. These routines include practices related to diet, exercise, sleep, and self-care that are customized according to one’s constitution and the season.
9. Ahara (diet) and aushadha (herbs and medicines)
Ayurveda places great importance on diet as a means of maintaining health and treating imbalances. Herbal remedies and medicines are used to restore balance and promote healing, often tailored to an individual’s constitution.
10. Srotas (channels)
The body’s channels or pathways through which various substances flow are called Srotas which play an important role in the transportation of nutrients, energy, and waste in the body. There are both physical and subtle Srotas and keeping them clear and functional is essential for overall health. Srotas are the physiological channels through which substances flow in the body.
TOXICOLOGICAL ASPECTS
Ayurvedic medicine, like any other system of medicine, has its principles and practices related to toxicology. Ayurveda emphasizes the use of natural substances, including herbs, minerals, and animal products, in healing and wellness. However, it also acknowledges the potential for toxicity in certain substances and provides guidelines for their safe use. Here are some key aspects of toxicology in Ayurvedic medicine:
1. Herbal toxicology
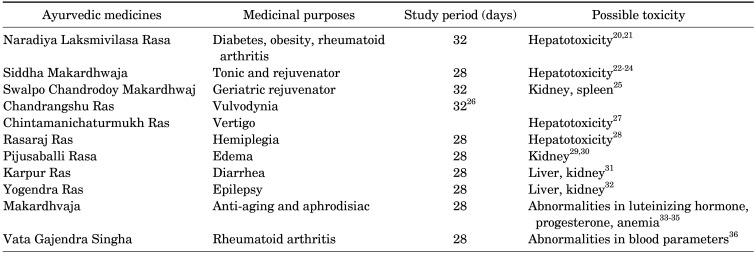
Ayurveda uses a wide range of herbs and plants for medicinal purposes. Some herbs, if not used appropriately, can show toxic effects (Table 1).20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36 Ayurvedic texts classify herbs according to their safety and potential toxicity. The “Bhavaprakasha Nighantu” and other Ayurvedic pharmacopeias provide information about the toxicity, dosage, and contraindications of various herbs.37
TABLE 1. Name of some Ayurvedic medicines that contain mercury and possible toxicity (study conducted in animals).
2. Individual tolerance and constitution
Ayurvedic practitioners consider the constitution of an individual (Prakriti) and current imbalance (Vikriti) when prescribing treatments. Some substances that may be well-tolerated by one person could be harmful to another. Ayurvedic practitioners must assess a patient’s constitution and susceptibility to potential toxicity.
3. Mineral and metal-based medicines
While Ayurveda often emphasizes the use of natural remedies and herbs, some Ayurvedic medicines may contain ingredients and heavy metals like mercury, lead, and arsenic that can be harmful to the liver, and kidney if not properly prepared, prescribed, or used.10
Rasa Shastra is an Ayurvedic branch that deals with formulations incorporating medications of metal/mineral origin. This branch covers their genesis, variations, physical and chemical characteristics, medicinal properties, and applications. As a result, this field is also known as ‘Ayurvedic Pharmaceutics’. Rasa Shastra is the study of metals such as gold, mercury, silver, copper, iron, tin, lead, and zinc, which are also traditionally known as Swarna, Parada or Rasa, Rajata, Tamra, Lauha, Vanga, Naga, and Yasada, respectively.38 These metals are necessary components of the human body and play an important role in human physiology. According to the Ayurvedic Formulary of India, mercury and lead are the most used heavy metals.38
Heavy metals can interfere with the normal physiological function of organs such as the brain, kidney, liver, and blood.39 Toxicity from heavy metals can have immediate or long-term repercussions. Long-term heavy metal exposure, among other things, can cause degenerative processes comparable to Parkinson’s disease, multiple sclerosis, muscular dystrophy, and Alzheimer’s disease. Ayurvedic herbal medicine products (HMPs) contain herbs, minerals, and metals.39 In the United States and overseas, at least 55 cases of heavy metal intoxication related to Ayurvedic HMPs in adults and children have been reported since 1978.40
1) Mercury (Parad)
There is a specialized branch of Ayurveda that is known as Rasa Shastra. Here, the term Rasa is a synonym of Mercury and Shastra means book or science; therefore, the word Rasa Shastra means the “Science of Mercury”.41 The evolution of Rasa Shastra as a specialized branch is traced to the great Buddhist Sage Naagaarjuna who is considered as ‘Father of Rasa Shastra’.41 It is believed to have begun to take on its full form with scientific documentation and classification during the eighth century. Additionally, Naagaarjuna is renowned for his great skill in handling mercury for alchemical and medicinal purposes.
The fact that this branch’s name comes from Parad (Rasa in Rasa-Shastra), suggests that medical professionals of that period placed an intense emphasis on using Parad or Rasa in medicinal uses. Rasa Shastra has existed since the Vedic period.42 It has also been reported that Buddhist sages were the first to use mercury and are believed to be one of the creators of treatment by using metals and minerals in their appropriate form.42 In addition to other metals, several medications used in Rasayana chikitsa (rejuvenation therapy) contain Parad. These are classified as Rasaousadhies.43 Since Rasaoushadies are effective in small doses and give quick relief as compared to pure herbal formulations, they have gained tremendous significance.43
The medication by Parad is quite effective. It is one of the crucial foundational components of Rasa-Ousadhies. When processed appropriately, it balances the three doshas (vata, pitta, and kapha) in the body. It has a soothing impact on our bodies, preventing illness consequently. Some of its effects include vrishya (an aphrodisiac), balya (a tonic), snigdha, rasayana (to revitalize), vrana shodhana and ropana (to treat wounds), krimighna (an antibiotic), and yogavahi.44 When used with Parad, several plants’ therapeutic effects are enhanced. It aids in mental stability and is regarded as the most effective disease-eradicator. Suitable carriers for preparations containing Parad include sugar, amla powder, ginger, and lemon juice.44 It is the metal in a liquid state which makes it unsuitable for use. To overcome this problem, scholars have mentioned certain procedures called Rasa-Bandha (mercurial bonds).
At the same time, Mercury (Parad) alone has been termed as a highly toxic and poisonous material and carries eight natural toxins within; those may cause certain negative effects; such as Naag dosha: wound, Bang dosha: eruption in skin, Agni dosha: burning in body, Mal dosha: stiffness all around, Chapalya dosha: loss of virility and sexual power, Vish dosha: death, Giri dosha: boils all over body and Asahyagni dosha: Maniac depression. There is always great emphasis that all such doshas of mercury should be eliminated first by performing various processing steps and then only processed mercury should be used for human consumption.
If mercury is not properly extracted and purified, it can be hazardous to the liver and other organs. Methylmercury (MeHg) at high concentrations can cause a range of diseases, including delayed growth and development, decreased reproductive success, liver dysfunction, and kidney damage.45 MeHg can also have negative impacts on prenatal growth, brain function, the cardiovascular system, and immunological function in adults and children.45
2) Arsenic
Arsenic is derived from the Greek word arsenikon meaning “potent”. It has been employed as a poison and a medicinal agent since ancient times. Susruta described arsenical compounds (Phenasma) as metallic poison before the year 2000 B.C. Charak Samhita (400 BC) describes the external usage of Orpiment and Realgar in skin ailments. However, the extensive usage of arsenic in Ayurveda was discovered around the eighth century, following the establishment of Rasa Sastra, as various arsenic compounds are found in treatments. Arsenicals are also used in the Siddha and Unani systems of medicine in India.
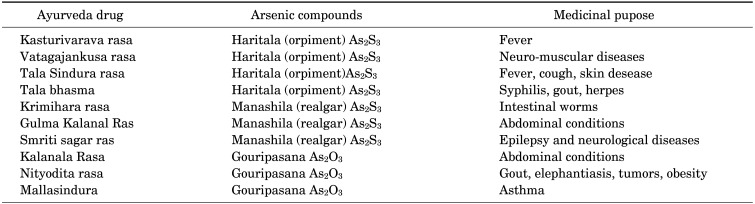
Haritala (Orpiment), Manashila (Realgar) and Gouripasana (White arsenic) are the three commonly used Arsenicals in Ayurveda for wide range of diseases (Table 2).46 Haritala (Orpiment) and Manashila (Realgar) come under Uparasa and Gouripasana (White arsenic) comes under Sadharana Rasa as per the Ayurveda Rasa sastra (Alchemy). Malla sindura and Rasa Manikya are two derivatives of White arsenic and Orpiment respectively used in certain cases of cancer by contemporary Ayurveda Practitioners.
TABLE 2. Some Ayurvedic medicines containing Arsenic compounds.
All arsenical compounds used in Ayurveda drugs are absorbed through the gastrointestinal system.47 Arsenical compounds have been used to regulate the blood counts of patients with hematological malignancies. There has been some observation of current Ayurvedic practitioners treating various solid tumors, such as nasal polyps, hemorrhoids, and elephantiasis.48 It may be due to the induction of apoptosis. The mechanism of arsenic–induced cell death is well understood in the application of As2O3, which is a potent cytotoxic and antitumor activity in vitro and vivo. Elevation of reactive oxygen species is a crucial early cellular event that happens after As2O3 therapy of target cells.49 Arsenic-containing chemicals are also effective modulators of the thioredoxin system, including thioredoxin, thioredoxin reductase, and NADPH. Some heavy metals, such as arsenic, are directly hepatotoxic, causing liver cell destruction and compromising overall liver function. Gauripasana (Arsenic trioxides) is a highly toxic compound than harital and manashila.50
3) Lead
Lead is a natural metal present in water and soil. Human exposure comes primarily through diet, air, drinking water, and ingestion of paint particles in the air, as well as occasionally through medicine. Even though lead has medicinal benefits, it is considered an unsafe metal in Ayurveda. Ayurvedic medications have been found to contain high levels of lead as well as other heavy metals, which constitute serious health risks.51 According to one investigation, lead was identified in 65% of 252 Ayurvedic medicines mixed with mercury.51
Lead accumulates in the brain, spleen, kidneys, liver, and lungs, as well as in blood, bone, and soft tissues.52 Lead in blood has a half-life of 30 days in people with normal renal function and a longer half-life in people with renal insufficiency.52 Excess lead, like other heavy metals, causes the creation of free radicals, which causes oxidative damage to biological components such as DNA and cell membranes.53 Lead inhibits DNA transcription, and vitamin D enzymatic production that maintains cell membrane integrity.
SAFETY CONCERN
The safety of medications and therapies has always been a top emphasis in the Ayurvedic system. Ayurveda takes pleasure in claiming to be the suddha (pure) approach to treatment that defines ailments without causing new ones. A medication or medicine that cures one sickness but causes another is deemed aśuddha or impure. The presence of bioactive plant components and other heavy metals such as mercury, lead, and arsenic are directly associated with the toxicity of medicinal plants and ayurvedic medicinal preparations. When it comes to heterogeneous, complex mixes of herbs and heavy metals, the situation becomes much more complicated. Several chronic studies in rats have found that only plant-based Ayurveda medicines have long-term negative effects on organs such as the liver, kidney, and spleen and glycemic index.54,55,56 Chronic studies have also found that Ayurvedic drugs elevated blood glucose levels in rats, which could lead to additional complications in diabetic patients.57 There are many examples of toxic endogenous compounds in the plant kingdom such as pyrrolizidine alkaloids (hepatotoxic, genotoxic, cytotoxic, phototoxic), furan derivatives (hepatotoxic, possible carcinogenic), epoxy-diterpenoids (hepatotoxic), anthraquinones (hepatotoxic), bis-benzylisoquinoline alkaloids (pulmonary toxicity), alkenylbenzenes (genotoxic, carcinogenic), ginkgolic acids (embryotoxic, cytotoxic, neurotoxic).58
Ayurvedic treatments are frequently made by various manufacturers without any regulations or safety concerns, and there may be a lack of uniformity in terms of the components utilized and their concentrations. This discrepancy can lead to variances in product potency and safety. Ayurvedic medications, unlike modern pharmaceuticals or contemporary medicines, frequently lack standardized manufacturing processes and quality control. As a result, the potency and safety of products from different manufacturers may differ. Various metals used in Ayurvedic medicine, including zinc, copper, and iron, have various therapeutic benefits in humans, but excessive doses of these metals can be fatal.59 Toxic concerns are increasingly serious due to insufficient Ayurvedic drug safety studies. Many Ayurvedic treatments have not been subjected to rigorous scientific testing to determine their safety and efficacy. It can be difficult to identify potential hazardous ingredients in these medicines without thorough scientific investigation and robust clinical trials.
Ayurvedic preparations or formulations should be strictly regulated by authorities.60 The government should introduce restrictions to prohibit direct access or over-the-counter purchases of Ayurvedic medicines. Clinicians or physicians should prescribe validated or authentic Ayurvedic remedies while also discussing drug dosage and toxicity with patients. Furthermore, heavy metal-containing ayurvedic medicine should be thoroughly evaluated to ensure the standard quality of the drug. Ayurvedic physiology, pathology, pharmacology (both basic and clinical), and medicines all require fundamental research. The government should devise a timetable for the gradual advance of Ayurvedic education and research. Science-based approaches to Ayurveda education, such as traditional Chinese medicine, can be encouraged, used, and instilled. It is commendable that China has almost 95% Department of Traditional Medicine in its government hospitals. That is why their ancient medicinal system has gained global renown and is widely accepted.61 Youyou Tu was awarded the Nobel Prize in Medicine for inventing Artemisinin, a medicine that has drastically reduced malaria fatality rates based on a traditional Chinese medicine cure.61 Similar strategies may be implemented in the healthcare system to promote the development of Ayurveda.
There are currently more than 600 different Ayurvedic preparations available for children and adults as herbal remedies to treat a variety of illnesses such as the common cold, diabetes, infertility, cardiovascular problems, psychiatric disorders, respiratory problems, rashes, and pain.62 A thorough examination of 193 Ayurvedic remedies indicated the presence of heavy metals in 20% of the products examined.62 Many of these drugs are produced in both India and the United States. Because they are promoted as supplements, they are not regulated by the United States Food and Drug Administration and are widely available in health food stores and on the internet. Over 20% of the Ayurvedic medicines manufactured and supplied by US and Indian corporations are thought to include harmful metals such as lead, mercury, and/or arsenic.51
QUALITY CONTROL
Quality control in Ayurvedic medicine requires understanding what is in the plant’s chemical components, what happens during manufacturing, and doing chemical and biological inspections before the finished product is sent to the client.63 The globe is raising serious concerns about the adulteration and contamination of traditional medicines. Furthermore, adulterants may be found in low-cost tree products with comparable biochemical or pharmacological component effects.64 All essential information about horticulture-related items should be carefully evaluated while developing medications to account for empirical and batch-to-batch variation. Based on the numerous standards outlined in the Ayurvedic Pharmacopoeia, it is critical to assess the description and analytical specifications of Ayurvedic formulations.65 Standardization methods should be used for all aspects of Ayurvedic medicine consistency, such as proper sample recognition, organoleptic analysis, volatile substance, pharmacognostic analysis, quantitative analysis, microbial load, xenobiotic, toxicity evaluation, phytochemical evaluation, and biochemical activity.65 Analytical parameters such as moisture content, ash values, extractive values, heavy metals, pesticide residues, and aflatoxins may help evaluate the quality of herbal raw materials. Various chromatographic techniques are frequently used to detect and maintain the quality of herbal medications or products. Though there are various chromatographic ways to segregation, the common thread is compound isolation through the use of mobile and stationary phase changes. Chromatographic techniques include GC, HPTLC, HPLC, HPLC-MS, GC-MS, NMR, and TLC, among others.66 All of these procedures may help to assess the phytoconstituents contained in complicated Ayurvedic medicines.
DISCUSSION
Ayurveda has a long history, however, there were several drawbacks in approaches to it that hampered its expansion, like the Western medical system. In most of the cases, the active components of the herbal medications provided were unknown, and many drugs still require further investigation for active constituent characterization and mechanism of action elucidation. Ayurveda medications continue to have downsides despite decades of using modern scientific techniques for drug analysis. Heavy metal adjuvants are routinely added to Ayurvedic medicines for their alleged therapeutic effects and to boost effectiveness. Lead, arsenic, and mercury are three heavy metals commonly found in Ayurvedic treatments. The current study indicated that users of Ayurvedic remedies may be at risk of heavy metal toxicity and urged for obligatory testing for hazardous heavy metals in Ayurvedic goods.
Footnotes
CONFLICT OF INTEREST STATEMENT: None declared.
References
- 1.Majeed A, Muhammad Z, Ahmad H, Rehmanullah, Hayat SS, Inayat N, et al. Nigella sativa L.: uses in traditional and contemporary medicines – an overview. Acta Ecol Sin. 2021;41:253–258. [Google Scholar]
- 2.Uddin MA, Akter F, Chowdhury IH, Asha UH, Tanny SZ, Sony TA, et al. Toxicological studies of leaf extract of Stevia rebaudiana Bertoni in Sprague-Dawley rats. Trop J Nat Prod Res. 2022;6:714–720. [Google Scholar]
- 3.Girish C, Pradhan SC. Indian herbal medicines in the treatment of liver diseases: problems and promises. Fundam Clin Pharmacol. 2012;26:180–189. doi: 10.1111/j.1472-8206.2011.01011.x. [DOI] [PubMed] [Google Scholar]
- 4.Chali BU, Hasho A, Koricha NB. Preference and practice of traditional medicine and associated factors in Jimma town, Southwest Ethiopia. Evid Based Complement Alternat Med. 2021;2021:9962892. doi: 10.1155/2021/9962892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chaudhary A. Gateway to global recognition of Ayurveda as the system of medicine - compulsory criteria of overseas regulators must be complied by India. J Ayurveda. 2023;17:75–78. [Google Scholar]
- 6.Thakur KS, Vahalia MK, Jonnalagadda VG, Rashmi K, Nadkarni SD, Gudi RV, et al. Evaluation of structural, chemical characterisation and safety studies of Samagandhak Kajjali, an Indian traditional Ayurvedic drug. J Pharmacogn Phytochem. 2014;2:57–67. [Google Scholar]
- 7.Chopra A, Tillu G, Chuadhary K, Reddy G, Srivastava A, Lakdawala M, et al. Co-administration of AYUSH 64 as an adjunct to standard of care in mild and moderate COVID-19: a randomized, controlled, multicentric clinical trial. PLoS One. 2023;18:e0282688. doi: 10.1371/journal.pone.0282688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rizvi ZA, Tripathy MR, Sharma N, Goswami S, Srikanth N, Sastry JLN, et al. Effect of prophylactic use of intranasal oil formulations in the hamster model of COVID-19. Front Pharmacol. 2021;12:746729. doi: 10.3389/fphar.2021.746729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chopra A, Srikanth N, Patwardhan B AYUSH CCRAS Research Group. Withania somnifera as a safer option to hydroxychloroquine in the chemoprophylaxis of COVID-19: results of interim analysis. Complement Ther Med. 2021;62:102768. doi: 10.1016/j.ctim.2021.102768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhalla A, Pannu AK. Are Ayurvedic medications store house of heavy metals? Toxicol Res (Camb) 2022;11:179–183. doi: 10.1093/toxres/tfab124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alissa EM, Ferns GA. Heavy metal poisoning and cardiovascular disease. J Toxicol. 2011;2011:870125. doi: 10.1155/2011/870125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mikulski MA, Wichman MD, Simmons DL, Pham AN, Clottey V, Fuortes LJ. Toxic metals in ayurvedic preparations from a public health lead poisoning cluster investigation. Int J Occup Environ Health. 2017;23:187–192. doi: 10.1080/10773525.2018.1447880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gitelman J, An H, Spilchuk V, Kim J. Lead toxicity from Ayurvedic medicines. CMAJ. 2023;195:E1010–E1012. doi: 10.1503/cmaj.230592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hardin J, Seltzer J, Suhandynata R, Spiegel B, Silver R, Thomas D, et al. Severe arsenic poisoning due to Ayurvedic supplements. Clin Case Rep. 2023;11:e7733. doi: 10.1002/ccr3.7733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomas V, Nair SNV, Ved DK, Shankar D. Controversial identities of medicinal plants in classical literature of Ayurveda. J Ayurveda Integr Med. 2020;11:565–572. doi: 10.1016/j.jaim.2019.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Narayanaswamy V. Origin and development of ayurveda: (a brief history) Anc Sci Life. 1981;1:1–7. [PMC free article] [PubMed] [Google Scholar]
- 17.Bhavana KR, Shreevathsa Medical geography in Charaka Samhita. Ayu. 2014;35:371–377. doi: 10.4103/0974-8520.158984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jaiswal YS, Williams LL. A glimpse of Ayurveda - the forgotten history and principles of Indian traditional medicine. J Tradit Complement Med. 2016;7:50–53. doi: 10.1016/j.jtcme.2016.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palsra P, Sharma S, Kumar R, Thamman R. Panchamahabhuta-five basic elements and their utility in Ayurveda: a review. Int Res J Ayurveda Yoga. 2022;5:166–174. [Google Scholar]
- 20.Hasan S, Sikder MM, Ali M, Hossain M, Zulfiquar TN, Akter F, et al. Toxicological studies of the Ayurvedic medicine “Naradiya Laksmivilasa Rasa” used in sinusitis. Biol Med (Aligarh) 2016;8:359 [Google Scholar]
- 21.Muneem SJS, Nasrin T, Hasan MR, Uddin MJ, Sikder MM, Bulbul L, et al. Preclinical lipid profile studies of an Ayurvedic preparation Naradiya Laksmivilasa Rasa after chronic administration to male Sprague-Dawley rats. Int J Pharm. 2017;7:210–216. [Google Scholar]
- 22.Sikder MM, Saha N, Asha UH, Neon MN, Akter K, Biswas MK, et al. Evaluation of pharmacological and toxicological studies of Ayurvedic medicine Siddha Makardhwaja on biological system of male Sprague-Dawley rats. Biol Med (Aligarh) 2018;10:434 [Google Scholar]
- 23.Sikder MM, Chakraborty P, Mahbub MR, Zulfiquar TN, Neon MN, Saha N, et al. Preclinical hematological profile studies of an ayurvedic medicine Siddha Makardhwaja after chronic administration to male Sprague-Dawley rats. Int J Basic Clin Pharmacol. 2018;7:93–97. [Google Scholar]
- 24.Sikder MM, Zulfiquar TN, Chowdhury IH, Akter K, Asha UH, Haque E, et al. Preclinical lipid profile studies of a classical Ayurvedic preparation, Siddha Makardhwaja (SMD), after chronic administration to male Sprague-Dawley rats. Biol Med (Aligarh) 2018;10:439 [Google Scholar]
- 25.Ali M, Sikder MM, Mondal UK, Leeza KA, Biswas MK, Hasan MR, et al. Toxicological studies of an Ayurvedic medicine “Swalpo Chandrodoy Makardhwaj” used as geriatric rejuvenator. Int J Pharm. 2017;7:84–89. [Google Scholar]
- 26.Leeza KA, Sikder MM, Sana T, Neon MN, Bulbul L, Fardous J, et al. Toxicological studies of an ayurvedic medicine Chandrangshu Ras. Int J Pharm. 2017;7:41–46. [Google Scholar]
- 27.Zulfiquar TN, Sikder MM, Sana T, Chowdhury IH, Saha N, Roy SC, et al. Organ body weight ratio toxicity studies of an Ayurvedic medicine Chintamanichaturmukh Ras used in vertigo. Int J Pharm. 2017;7:35–40. [Google Scholar]
- 28.Akter F, Sikder MM, Hasan S, Emu IJ, Ali M, Biswas MK, et al. Evaluation of pharmacological and toxicological studies of an ayurvedic medicine Rasaraj Ras on biological system of the male Sprague-Dawley rats. Int J Basic Clin Pharmacol. 2016;5:2371–2375. [Google Scholar]
- 29.Sony TA, Saha N, Chowdhury IH, Tripura S, Akter S, Mumu M, et al. Preclinical blood chemistry safety profile studies of “Pijusaballi Rasa” on the kidney function after chronic administration to male Sprague-Dawley rats. Biol Med (Aligarh) 2020;12:466 [Google Scholar]
- 30.Mahbub MR, Sikder MM, Sony TA, Jahan NN, Faruque MO, Zaman T, et al. Effect of Pijusaballi Rasa on thyroid hormones in Sprague-Dawley rats. Biol Med (Aligarh) 2020;12:467 [Google Scholar]
- 31.Sikder MM, Hasan MR, Lopa SS, Abedin N, Uddin MJ, Sarker MMR, et al. Toxicological studies of an Ayurvedic medicine “Karpur Ras” used in diarrhoea. Int J Pharm. 2015;5:472–477. [Google Scholar]
- 32.Hossain M, Hasan MR, Khalil M, Binoy MH, Sikder MM, Sony TA, et al. Toxicological studies of an ayurvedic medicine Yogendra Ras used in epilepsy. Int J Pharm. 2017;7:31–37. [Google Scholar]
- 33.Masud N, Sikder MM, Uddin MA, Roy SC, Biswas MK, Haque E, et al. Steroidal and gonadotropin hormone profile studies of a classical Ayurvedic preparation of “Makardhvaja” after chronic administration to male Sprague-Dawley rats. Biol Med (Aligarh) 2016;9:372 [Google Scholar]
- 34.Roy SC, Sikder MM, Sarker A, Uddin MA, Masud N, Hasan MR, et al. Preclinical anemia panel studies of “Makardhvaja” after chronic administration to male Sprague-Dawley rats. Biol Med (Aligarh) 2017;9:387 [Google Scholar]
- 35.Mondal UK, Uddin MA, Roy SC, Sana T, Sikder MM, Khalil M, et al. Preclinical lipid profile studies of a classical Ayurvedic preparation Makaradhwaj Ras after chronic administration to male Sprague-Dawley rats. Int J Pharm. 2017;7:65–70. [Google Scholar]
- 36.Saha N, Sikder MM, Uddin MA, Akter F, Asha UH, Sony TA, et al. Hematological studies of an Ayurvedic medicine “Vata Gajendra Singha” used in rheumatoid arthritis after chronic administration to male Sprague-Dawley rats. Trop J Nat Prod Res. 2023;7:2492–2497. [Google Scholar]
- 37.Kolhe R, Acharya R. Analyzing the drug safety issue in Bhavaprakasha Nighantu – a critical review. Ayurpharm Int J Ayurveda Allied Sci. 2015;4:183–196. [Google Scholar]
- 38.Reddy CS, Balekari U, Priyanka V, Sagar JV. Toxicokinetics and tissue distribution studies of mercury in Ayurvedic preparation- Shila sindur. Hygeia J Drugs Med. 2014;6:81–94. [Google Scholar]
- 39.Gogtay NJ, Bhatt HA, Dalvi SS, Kshirsagar NA. The use and safety of non-allopathic Indian medicines. Drug Saf. 2002;25:1005–1019. doi: 10.2165/00002018-200225140-00003. [DOI] [PubMed] [Google Scholar]
- 40.Saper RB, Kales SN, Paquin J, Burns MJ, Eisenberg DM, Davis RB, et al. Heavy metal content of Ayurvedic herbal medicine products. JAMA. 2004;292:2868–2873. doi: 10.1001/jama.292.23.2868. [DOI] [PubMed] [Google Scholar]
- 41.Savrikar SS, Ravishankar B. Introduction to 'Rasashaastra’ the iatrochemistry of Ayurveda. Afr J Tradit Complement Altern Med. 2011;8(5 Suppl):66–82. doi: 10.4314/ajtcam.v8i5S.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tripathi R, Kiran Concept of Rasayana in Rasa shastra. Int J Res Ayurveda Pharm. 2012;3:777–779. [Google Scholar]
- 43.Devanathan R. A review on Swarna Makshika. Int Res J Pharm. 2011;2:1–5. [Google Scholar]
- 44.Sarkar PK, Das S, Prajapati PK. Ancient concept of metal pharmacology based on Ayurvedic literature. Anc Sci Life. 2010;29:1–6. [PMC free article] [PubMed] [Google Scholar]
- 45.Yang L, Zhang Y, Wang F, Luo Z, Guo S, Strähle U. Toxicity of mercury: molecular evidence. Chemosphere. 2020;245:125586. doi: 10.1016/j.chemosphere.2019.125586. [DOI] [PubMed] [Google Scholar]
- 46.Panda AK, Hazra J. Arsenical compounds in Ayurveda medicine: a prospective analysis. Int J Res Ayurveda Pharm. 2012;3:772–776. [Google Scholar]
- 47.Chen Z, Chen GQ, Shen ZX, Sun GL, Tong JH, Wang ZY, et al. Expanding the use of arsenic trioxide: leukemias and beyond. Semin Hematol. 2002;39(2 Suppl 1):22–26. doi: 10.1053/shem.2002.33611. [DOI] [PubMed] [Google Scholar]
- 48.Treleaven J, Meller S, Farmer P, Birchall D, Goldman J, Piller G. Arsenic and Ayurveda. Leuk Lymphoma. 1993;10:343–345. doi: 10.3109/10428199309148558. [DOI] [PubMed] [Google Scholar]
- 49.Hu Y, Li J, Lou B, Wu R, Wang G, Lu C, et al. The role of reactive oxygen species in arsenic toxicity. Biomolecules. 2020;10:240. doi: 10.3390/biom10020240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Khandpur S, Malhotra AK, Bhatia V, Gupta S, Sharma VK, Mishra R, et al. Chronic arsenic toxicity from Ayurvedic medicines. Int J Dermatol. 2008;47:618–621. doi: 10.1111/j.1365-4632.2008.03475.x. [DOI] [PubMed] [Google Scholar]
- 51.Neon MN, Urmy SK, Barua A, Khan MAA, Biswas MK, Choudhuri MSK, et al. Preclinical Hba1c level studies of Makardhwaj Ras and Maha Sankha Bati after chronic administration to male Sprague-Dawley rats. Trop J Nat Prod Res. 2024;8:6234–6238. [Google Scholar]
- 52.Vaziri ND. Mechanisms of lead-induced hypertension and cardiovascular disease. Am J Physiol Heart Circ Physiol. 2008;295:H454–H465. doi: 10.1152/ajpheart.00158.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Flora SJ, Mittal M, Mehta A. Heavy metal induced oxidative stress & its possible reversal by chelation therapy. Indian J Med Res. 2008;128:501–523. [PubMed] [Google Scholar]
- 54.Sony TA, Hasan MR, Khatun MR, Sikder MM, Hossain M, Hasan S, et al. Toxicological studies of an Ayurvedic medicine (Brihot Chandrodoy Makardhwaj) used as rejuvenator. Int J Pharm. 2015;5:759–764. [Google Scholar]
- 55.Sana T, Sikder MM, Chakma P, Khalil M, Abedin N, Islam MA, et al. Toxicological studies of an Ayurvedic medicine Kankayana Gutika. Int J Pharm. 2017;7:44–50. [Google Scholar]
- 56.Sana T, Sikder MM, Abedin N, Islam MA, Barua A, Khan MA, et al. Toxicological evaluation of Guducyadi Louha, an ayurvedic formulation, on biochemical parameters of Sprague-Dawley rats. Int J Pharm. 2017;7:17–22. [Google Scholar]
- 57.Umma HA, Saha N, Sikder MM, Akter K, Sony TA, Sinha MH, et al. Preclinical HbA1c level studies of Brihat Khadir Batika and Chandraprabha Batika after chronic administration to male Sprague-Dawley rats. Int J Basic Clin Pharmacol. 2018;7:2151–2155. [Google Scholar]
- 58.Wang YK, Li WQ, Xia S, Guo L, Miao Y, Zhang BK. Metabolic activation of the toxic natural products from herbal and dietary supplements leading to toxicities. Front Pharmacol. 2021;12:758468. doi: 10.3389/fphar.2021.758468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sujatha Pushpakanthi Hewageegana HG, Hewageegana AU, Ashanthi Menuka Arawwawala LD. Purification, detoxification, and incineration methods of minerals and metals in traditional medicine formulations of Sri Lanka. Evid Based Complement Alternat Med. 2021;2021:6634553. doi: 10.1155/2021/6634553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Narayana DBA, Brindavanam NB, Shirsekar S. History of safe use of herbs - approaches for documenting evidence. J Ayurveda Integr Med. 2024;15:100849. doi: 10.1016/j.jaim.2023.100849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chauhan A, Semwal DK, Mishra SP, Semwal RB. Ayurvedic research and methodology: present status and future strategies. Ayu. 2015;36:364–369. doi: 10.4103/0974-8520.190699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Saper RB, Phillips RS, Sehgal A, Khouri N, Davis RB, Paquin J, et al. Lead, mercury, and arsenic in US- and Indian-manufactured Ayurvedic medicines sold via the Internet. JAMA. 2008;300:915–923. doi: 10.1001/jama.300.8.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cordell GA. Phytochemistry and traditional medicine – a revolution in process. Phytochem Lett. 2011;4:391–398. [Google Scholar]
- 64.Mukherjee PK, Bahadur S, Harwansh RK, Nema NK, Bhadra S. Development of traditional medicines: globalizing local knowledge or localizing global technologies. Pharma Times. 2013;45:39–42. [Google Scholar]
- 65.Pant J, Singh RM, Marwah H. Methods employed in quality control in Ayurveda. J Med Plants Stud. 2021;9:141–155. [Google Scholar]
- 66.Mukherjee PK, Kumar V, Kumar NS, Heinrich M. The Ayurvedic medicine Clitoria ternatea--from traditional use to scientific assessment. J Ethnopharmacol. 2008;120:291–301. doi: 10.1016/j.jep.2008.09.009. [DOI] [PubMed] [Google Scholar]