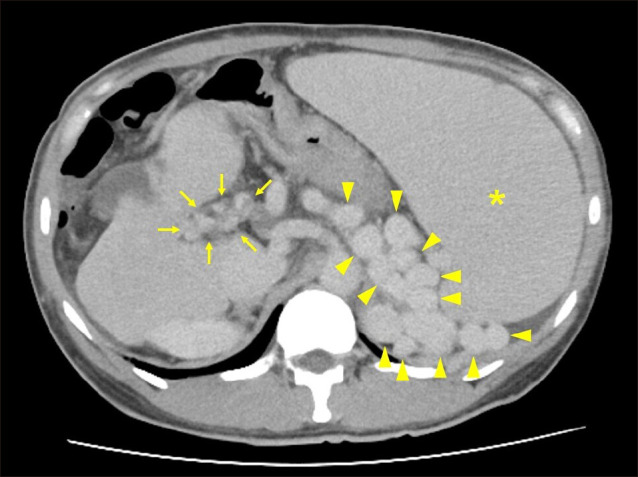
A previously healthy Japanese 40-year-old man presented to the gastroenterology department with a massive abdominal mass detected at a medical check-up. His vital signs were normal. He had no symptoms, including abdominal pain, constipation, loss of appetite, and body weight loss. Abdominal ultrasonography revealed severe splenomegaly (Fig. 1). Contrast-enhanced computed tomography showed splenomegaly, splenorenal shunt and cavernous transformation in the porta hepatis (Fig. 2). In addition, intra- and extrahepatic portal veins were unclear. A diagnosis of extrahepatic portal vein obstruction (EHPVO) was made.
FIG. 1. Abdominal ultrasonography revealing severe splenomegaly.
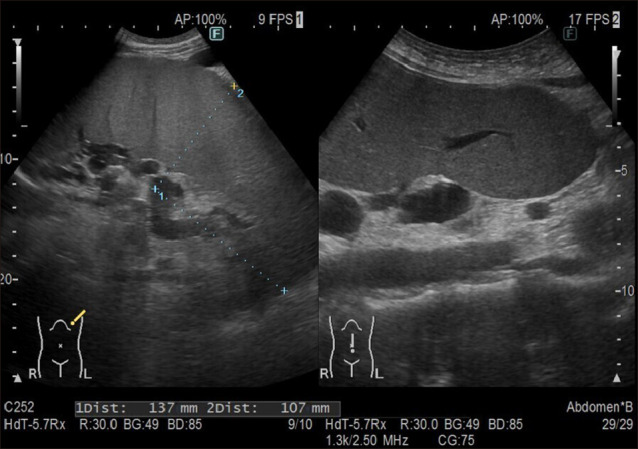
FIG. 2. Contrast-enhanced computed tomography showed splenomegaly (asterisk), splenorenal shunt (arrowheads) and cavernous transformation (arrows) in the porta hepatis.
EHPVO is a rare disease, particularly in the Europe or North America; thus, very few epidemiologic studies have been carried out.1 A Japanese nationwide survey reported that the male-to-female ratio was approximately 1:1, and the mean ages at symptom onset and diagnosis were approximately 30 and 33 years, respectively.1 Furthermore, the main symptoms were splenomegaly and esophageal varices, which appeared in over 60% of patients.1
Portal cavernoma is a network of porto-portal collaterals which develops as a consequence of prior portal vein obstruction.2 Obstruction leading to cavernoma is mostly related to thrombosis in adults.2 Risk factors for portal vein thrombosis include reduced portal flow velocity (e.g., cirrhosis), hypercoagulable state (e.g., myeloproliferative disorders, pregnancy, and oral contraceptives), vascular damage (e.g., abdominal trauma, intraabdominal surgical procedure, pancreatitis, cholecystitis, and cholangitis), and malignant vascular invasion.3
The key management issues in EHPVO are centered on portal hypertension and its complications: varices and splenomegaly.4 If the varices can be well controlled, the overall prognosis is considered relatively favorable.1 In the present case, the etiology was unknown. Routine evaluation showed severe esophageal varices. The patient underwent Hassab’s operation and splenectomy.
Footnotes
CONFLICT OF INTEREST STATEMENT: None declared.
References
- 1.Ohfuji S, Furuichi Y, Akahoshi T, Kage M, Obara K, Hashizume M, et al. Japanese periodical nationwide epidemiologic survey of aberrant portal hemodynamics. Hepatol Res. 2019;49:890–901. doi: 10.1111/hepr.13343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Franchis R, Bosch J, Garcia-Tsao G, Reiberger T, Ripoll C Baveno VII Faculty. Baveno VII - renewing consensus in portal hypertension. J Hepatol. 2022;76:959–974. doi: 10.1016/j.jhep.2021.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumar A, Sharma P, Arora A. Review article: portal vein obstruction--epidemiology, pathogenesis, natural history, prognosis and treatment. Aliment Pharmacol Ther. 2015;41:276–292. doi: 10.1111/apt.13019. [DOI] [PubMed] [Google Scholar]
- 4.Khanna R, Sarin SK. Noncirrhotic portal hypertension: current and emerging perspectives. Clin Liver Dis. 2019;23:781–807. doi: 10.1016/j.cld.2019.07.006. [DOI] [PubMed] [Google Scholar]


