Abstract
Background
It is well known that adequate water intake and moisturizer application improves skin barrier function.
Objective
This study was conducted to analyze the effects of daily water intake and moisturizer application on skin barrier function and the degree of response to barrier recovery.
Methods
Participants with daily water intake more than 1 L were classified as high daily water intake group (H) and those with less than 1 L as low daily water intake group (L). Each group was subcategorized into four groups according to intervention method: additional water intake (H1, L1), moisturizer (H2, L2), both (H3, L3), and control (H4, L4). Transepidermal water loss (TEWL) and stratum corneum hydration (SCH) were measured at baseline during the 2nd and 4th week.
Results
A total of 43 participants completed the study (H: 22, L: 21). At baseline, there was no significant difference in SCH and TEWL in any on the anatomical sites between the high daily water intake and low daily water intake groups. However, SCHs of left forearm (group H2, p=0.004; group H3, p=0.004), left hand dorsum (group H2, p=0.010; group H3, p=0.026), and left shin (group H2, p=0.016; group H3, p=0.001) in group H2 and H3 were significantly increased in the 4th week as compared to the baseline values.
Conclusion
The results suggest that the degree of water intake may be related to improved skin barrier function. However, application of additional moisturizers had more favorable impact on skin hydration as compared to additional water intake.
Keywords: Emollients, Public health, Water intake
INTRODUCTION
Water comprises 45%–70% of the total body weight, making water intake essential for maintaining human physiology1,2,3. Even 4%–6% of body fluid loss is considered dehydration, affecting physical activity and mental function4,5. Likewise, in the skin physiology, cutaneous water content is known to play an important role in various functions, and its deficiency is related to dermatological dysfunctions6. According to Dietary Reference Intakes for Koreans (Ministry of Health & Welfare and The Korean Nutrition Society, 2015), the mean daily water intake of Korean adults aged 19–49 years was 884.25 ml, which is insufficient compared to the recommended water intake of 2 L by World Health Organization (WHO). Two studies by Palma et al.7 demonstrated that additional daily intake of 2 L of water improved the skin hydration in those who did not usually drink enough water6.
In general, dermatologists recommend moisturizers. Moisturizers provide moisture to the skin and prevent loss of moisture, and are commonly used in skin care products and cosmetics8,9. However, as there is no study from Korea regarding the effect of oral water intake on skin moisturization, we studied how water intake would affect the improvement of skin barrier function in Koreans, and also compared it with the effect of moisturizer application.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board (IRB) of the Inje University Busan Paik Hospital (IRB No. 16-0022). This study was performed in one center (Department of Dermatology, Busan Paik Hospital, Inje University, Busan, Korea) from April to June in 2017.
Participants
Healthy female volunteers in their 20s to 40s were allowed to participate in this study. Those who had any dermatologic disorders were excluded from the study. The participants were classified into higher water intake (H) and lower water intake (L) groups according to their daily water intake. As the average water intake of Koreans is 884.25 ml and a bottle of drink used on a daily basis is generally provided in 250-ml or 500-ml bottles, H and L groups were separated on the basis of 1 L of water intake, for the ease of measurement. Each group was randomly subcategorized according to four different interventions: group 1 with additional water intake of 2 L (H1, L1) a day, group 2 with additional moisturizer application three times a day (H2, L2), group 3 with both additional 2 L water intake plus moisturizer application three times a day (H3, L3), and group 4 with no intervention as control groups (H4, L4). The participants were asked to maintain their usual water intake and topical applications on their face and body during the study and instructed to follow the additional designated interventions according to the groups.
Criteria of compliance
For the additional water intake groups, 112 bottles of natural mineral water, 500 ml each (masinda®; Donga-otsuka Co., Seoul, Korea), were provided. Two bottles were to be taken in the morning and two bottles in the afternoon. For the additional moisturizer application groups, two bottles of moisturizing cream (atobarrier® cream; Aestura Co., Seoul, Korea), 100 ml each, were provided and daily application thrice—in the morning, at noon, and in the evening was instructed.
The criteria of compliance were as follows: 1. More than 80% of additional water intake (should not miss drinking more than 22 bottles of 500 ml for 28 days). 2. More than 80% of moisturizer application (should not miss moisturizer application more than 16 times for 28 days). All participants were asked to record additional daily water intake or moisturizer application on provided self-evaluation sheet, and those who did not accomplish each allotment were excluded.
Environment control and measurements
During each visit, the participants were seated in a 10-m2, rectangular, double door room with a thermos hygrostat facility installed (PVR30M4P, specification: 76.03 m2; Bumyang Air Conditioning Company Ltd., Seoul, Korea), in Inje University Busan Paik Hospital clinical trial center, where the temperature and the relative humidity of the room were recorded for 24 hours. The participants were at rest for 20 minutes for acclimatization. All measurements were performed at 20.0°C–22.0°C and relative humidity of 50.0%–52.0%. Measurements were taken at five different sites of the face or body: forehead, left cheek, left forearm, left hand dorsum, and left shin. The skin surface hydration was assessed with a Corneometer® (CM 825; Courage & Khazaka Electronic GmbH, Cologne, Germany) represented as stratum corneum hydration (SCH). The probe was applied perpendicular to the skin surface with a constant pressure. For each participant, three consecutive measurements were taken, and the mean value was recorded. Transepidermal water loss (TEWL) was measured with a Tewameter® (TM300; Courage & Khazaka Electronic GmbH). The probe was held in place, perpendicular and touching the skin surface with the lowest pressure, until a stable TEWL value was established (for approximately 90 seconds). TEWL was measured thrice, with a 10-seconds interval between each measurement.
On day 1, the baseline of the measurements was measured and those of the 2nd and the 4th week were evaluated. One dermatologist took the measurements to eliminate inter-rater errors.
Safety evaluation
For safety of the participants, signs of nausea, vomiting, or dizziness were noted during each visit, and body mass index and blood pressure were checked. Body mass index was measured after an 8-hours fast, and blood pressure was measured using an automatic blood pressure meter after 20 minutes of rest.
Statistical analysis
All data were expressed as mean ± standard deviations. The statistical analysis was performed using SPSS (ver. 23.0 for Windows; IBM Corp., Armonk, NY, USA). Baseline SCH and TEWL were compared between group H and group L by independent t-test. Repeated measure analysis of variance test was used to analyze serial change among the subgroups, followed by post hoc multiple comparisons using the Bonferroni’s method. Independent t-test was used to compare the difference of SCH and TEWL between each corresponding intervention groups (i.e., H1 vs. L1, H2 vs. L2, H3 vs. L3, and H4 vs. L4 groups) at each visit. Statistical significance was set as p-values<0.05.
RESULTS
Demographic information and group
A total of 50 healthy Korean females in their 20s to 40s, who voluntarily participated in this study and provided written informed consent were enrolled (group H of 24, group L of 26). Their mean age was 28.7 years (range, 21–39 years). Among them, seven participants dropped out during the study and all the 43 participants (group H of 22, group L of 21) (Table 1) who completed the study met the criteria of compliance with the recommendations of additional water intake or moisturizer application.
Table 1. Numbers of the enrolled participants.
| Groups | No. of initial participants | No. of dropouts | No. of final participants |
|---|---|---|---|
| H1 | 6 | 1 | 5 |
| H2 | 6 | 1 | 5 |
| H3 | 8 | 0 | 8 |
| H4 | 4 | 0 | 4 |
| L1 | 7 | 0 | 7 |
| L2 | 7 | 0 | 7 |
| L3 | 6 | 3 | 3 |
| L4 | 6 | 2 | 4 |
| Total | 50 | 7 | 43 |
H: high daily water intake group, L: low daily water intake group.
Serial changes in mean values of SCH and TEWL in each subgroup
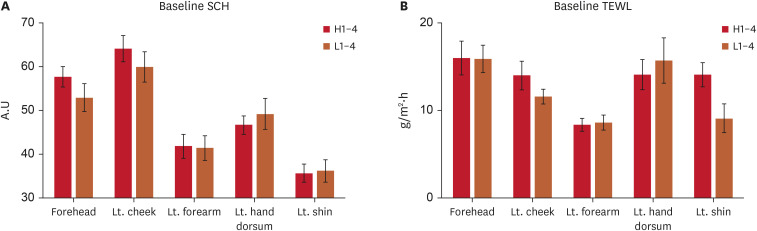
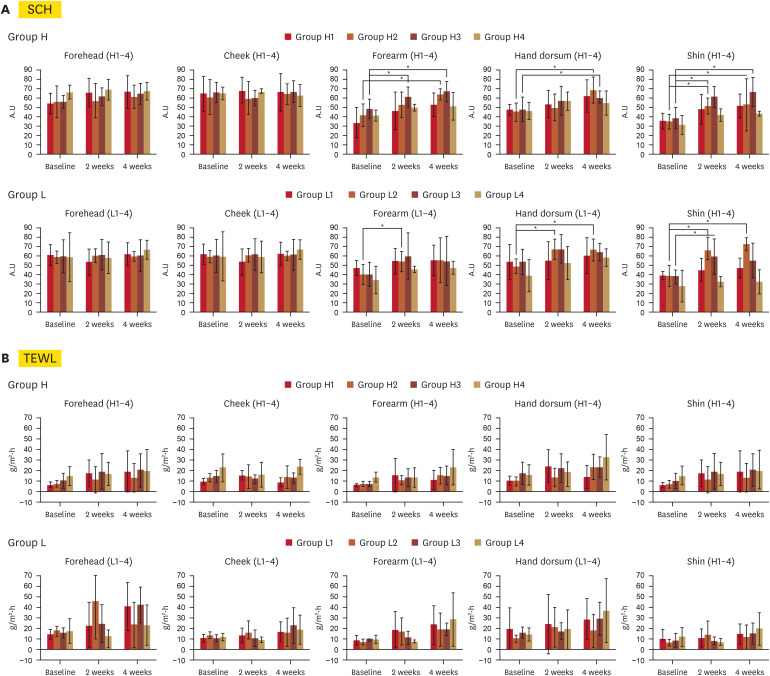
Results from SCH and TEWL are summarized in Supplementary Tables 1 and 2. There were no significant differences in the initial SCH and TEWL at any anatomical site between the high daily water intake and low daily water intake groups (Fig. 1). Regarding SCH (Supplementary Table 1), in group H1 and L1, with additional water intake, no significant changes were observed, except for left shin in the 4th week in group H1 (Table 2). However, in group H2 and H3, with additional moisturizer application, the SCH of left shin significantly increased within 2 weeks (group H2, p=0.006; group H3, p=0.001). Moreover, SCHs of both groups further increased in the 4th week (group H2, p=0.016; group H3, p=0.001). Furthermore, SCHs of left forearm (group H2, p=0.004; group H3, p=0.004) and left hand dorsum (group H2, p=0.010; group H3, p=0.026) were significantly increased in the 4th week as compared to the baseline values. However, when comparing group H2 with H3, there were no significant differences between the two groups. Also, among group L, group L2 showed significant change of SCH in left forearm (2nd week, p=0.043), left hand dorsum (2nd week, p=0.004; 4th week, p=0.005) and left shin (2nd week, p=0.001; 4th week, p<0.001), and group L3 showed significant change in left shin (2nd week, p=0.029) (Fig. 2A). Regarding TEWL, however, there was no significant change in any of the groups over the whole period (Supplementary Table 2, Fig. 2B).
Fig. 1. Baseline SCH and TEWL. There was no significant difference in (A) baseline SCH and (B) baseline TEWL in any on the anatomical sites between H1–4 and L1–4 groups.
SCH: stratum corneum hydration, TEWL: transepidermal water loss, Lt.: left, H: high daily water intake group, L: low daily water intake group.
Table 2. The p-values for stratum corneum hydration changes in groups with additional water intake (group H1 and L1).
| Groups | p-value | |||
|---|---|---|---|---|
| D0 vs. D14 | D14 vs. D28 | D0 vs. D28 | ||
| Group H1 | ||||
| Forehead | 0.181 | 0.920 | 0.175 | |
| Lt. cheek | 0.765 | 0.885 | 0.901 | |
| Lt. forearm | 0.240 | 0.590 | 0.052 | |
| Lt. hand dorsum | 0.433 | 0.419 | 0.129 | |
| Lt. shin | 0.128 | 0.720 | 0.034* | |
| Group L1 | ||||
| Forehead | 0.823 | 0.050 | 0.025 | |
| Lt. cheek | 0.248 | 0.242 | 0.929 | |
| Lt. forearm | 0.263 | 0.923 | 0.284 | |
| Lt. hand dorsum | 0.914 | 0.651 | 0.559 | |
| Lt. shin | 0.255 | 0.740 | 0.093 | |
Lt.: left, H: high daily water intake group, L: low daily water intake group.
*Statistically significant (p<0.05).
Fig. 2. SCH and TEWL changes in different anatomical areas of the participants who were divided into group H and group L. Changes of (A) SCH and (B) TEWL in different anatomical areas of the participants who were divided into group H and group L.
SCH: stratum corneum hydration, TEWL: transepidermal water loss, H: high daily water intake group, L: low daily water intake group.
*p<0.05.
The difference between each comparative subgroup at each visit (group H vs. group L)
Group L1 showed higher SCH than group H1 at baseline in left forearm (p=0.049). Group L2 showed higher SCH than group H2 in left hand dorsum (p=0.027) and left shin (p=0.019), in 2nd week. There was no other significantly different SCH at 4th week or TEWL, over the whole period (Supplementary Table 3).
DISCUSSION
One of the important functions of the skin is to protect the human body by forming a barrier between the external environment and the body. In particular, stratum corneum of the epidermis mainly constitutes the physical barrier10. The water content of the stratum corneum is normally approximately 30% of its weight, and the stratum corneum acts as a water-retaining barrier. The amount of skin hydration is determined by supply of water from the dermis and transcutaneous water loss to the external environment11,12.
The application of moisturizer on the skin is thought to form a membrane on the skin, preventing the evaporation of moisture and directly supplying moisture to the epidermis and dermis. Many studies emphasize the positive effects of applying moisturizer for patients with abnormal barrier function, such as atopic dermatitis or xerotic eczema13,14. Additionally, some literature has found that applying moisturizer is beneficial even for people with normal barrier function15,16. Oral water intake is also assumed to be beneficial for skin hydration and its function, as adequate water intake has been shown to be beneficial for various aspects of general health conditions3,8. However, little is known about the in vivo effect of various factors on skin physiology17, and a few recent studies demonstrate favorable effects of skin hydration through oral water intake7,8,18.
With the favorable effects observed in previous studies, our study aimed to identify changes in SCH and TEWL with additional water intake or the application of moisturizer. According to the results, there was no significant serial change of SCH in the control group and in the group H1 and L1, where participants were instructed to consume additional 2 L of water. However, after an additional 4 weeks of moisturizer application, group H2 showed significant increase of SCH in left shin, left forearm, and left hand dorsum, and group L2 showed significant increase of SCH in left shin and left hand dorsum. In other words, in a short period of time, the application of additional moisturizers had a more positive impact on the increase in skin hydration compared to additional water intake. Additionally, SCH in the group H3 and L3 showed a tendency to increase, but no significant changes occurred when both additional water intake and moisturizer application were executed. Moreover, when comparing group H2 with H3, there was no significant differences in SCH. This result underscores the significance of moisturizer use. As for TEWL, our study didn’t find any meaningful differences. This result suggests that measuring the difference of TEWL in the normal skin of healthy people is challenging.
We also compared the degree of skin hydration between those who usually drink more than 1 L of water and those who do not. We expected a decrease in the degree of skin hydration in those who drink less than 1 L of water as compared to those who drink more than 1 L. However, there was no statistically significant difference of SCH and TEWL between the two groups. Meanwhile, what is notable is that SCH showed a tendency to be higher on the forehead, left cheek, and left forearm of the group H, which is thought to be contributed by 1 L of daily water intake to a certain extent. Additionally, the hands and shins, which are frequently in contact or exposed to external surroundings, and areas where women wear skirts or shorts, are thought to have shown different tendency compared to other anatomical areas such as forehead, cheek, and forearm. However, dividing into two groups based on 1 L of water intake was less than the WHO’s 2 L water intake suggestion. Because of this, there may not have been any significant differences between the two groups.
It was difficult to present statistical significance because each subgroup was allocated a relatively small numbers of participants. Further, short duration of the study i.e., 1 month, was insufficient to judge the effect of water intake. However, this study is useful as it provides the direction for further research by measuring and comparing the changes in the serial SCH and TEWL, following additional water intake and application of moisturizers. Similar to previous studies, this study also showed a tendency to increase skin moisture content with increased water intake7,8,18.
In the short duration of time, the application of additional moisturizers had more favorable impact on skin hydration as compared to additional water intake. This result suggests that for patients who need immediate improvement in skin moisture content, applying a moisturizer rather than increasing water intake will be helpful. Also, this effect is remarkable on arms or legs exposed to the external environment. However, further studies are needed to understand the effects of long-term water intake on skin barrier function and skin moisture content.
Footnotes
FUNDING SOURCE: None.
CONFLICTS OF INTEREST: The authors have nothing to disclose.
DATA SHARING STATEMENT: Data used to support the findings of this study are available from the corresponding author upon request.
SUPPLEMENTARY MATERIALS
Stratum corneum hydration changes in different anatomical areas of the participants who were divided into group H and group L
Transepidermal water loss changes in different anatomical areas of the participants who were divided into group H and group L
The p-values of each comparative subgroup (group H vs. group L)
References
- 1.Chumlea WC, Guo SS, Zeller CM, Reo NV, Siervogel RM. Total body water data for white adults 18 to 64 years of age: the Fels Longitudinal Study. Kidney Int. 1999;56:244–252. doi: 10.1046/j.1523-1755.1999.00532.x. [DOI] [PubMed] [Google Scholar]
- 2.Jéquier E, Constant F. Water as an essential nutrient: the physiological basis of hydration. Eur J Clin Nutr. 2010;64:115–123. doi: 10.1038/ejcn.2009.111. [DOI] [PubMed] [Google Scholar]
- 3.Popkin BM, D’Anci KE, Rosenberg IH. Water, hydration, and health. Nutr Rev. 2010;68:439–458. doi: 10.1111/j.1753-4887.2010.00304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riebl SK, Davy BM. The hydration equation: update on water balance and cognitive performance. ACSM’s Health Fit J. 2013;17:21–28. doi: 10.1249/FIT.0b013e3182a9570f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pross N, Demazières A, Girard N, Barnouin R, Santoro F, Chevillotte E, et al. Influence of progressive fluid restriction on mood and physiological markers of dehydration in women. Br J Nutr. 2013;109:313–321. doi: 10.1017/S0007114512001080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosado C, Rodrigues LM. In vivo study of the physiological impact of stratum corneum sampling methods. Int J Cosmet Sci. 2003;25:37–44. doi: 10.1046/j.1467-2494.2003.00171.x. [DOI] [PubMed] [Google Scholar]
- 7.Palma L, Marques LT, Bujan J, Rodrigues LM. Dietary water affects human skin hydration and biomechanics. Clin Cosmet Investig Dermatol. 2015;8:413–421. doi: 10.2147/CCID.S86822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Palma ML, Tavares L, Fluhr JW, Bujan MJ, Rodrigues LM. Positive impact of dietary water on in vivo epidermal water physiology. Skin Res Technol. 2015;21:413–418. doi: 10.1111/srt.12208. [DOI] [PubMed] [Google Scholar]
- 9.Lodén M. The clinical benefit of moisturizers. J Eur Acad Dermatol Venereol. 2005;19:672–688. doi: 10.1111/j.1468-3083.2005.01326.x. [DOI] [PubMed] [Google Scholar]
- 10.Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, McMichael AJ, et al. Fitzpatrick's dermatology. 9th ed. New York: McGraw-Hill Education; 2019. pp. 207–213. [Google Scholar]
- 11.Bouwstra JA, Groenink HWW, Kempenaar JA, Romeijn SG, Ponec M. Water distribution and natural moisturizer factor content in human skin equivalents are regulated by environmental relative humidity. J Invest Dermatol. 2008;128:378–388. doi: 10.1038/sj.jid.5700994. [DOI] [PubMed] [Google Scholar]
- 12.Richter T, Peuckert C, Sattler M, Koenig K, Riemann I, Hintze U, et al. Dead but highly dynamic--the stratum corneum is divided into three hydration zones. Skin Pharmacol Physiol. 2004;17:246–257. doi: 10.1159/000080218. [DOI] [PubMed] [Google Scholar]
- 13.Shim JH, Park JH, Lee JH, Lee DY, Lee JH, Yang JM. Moisturizers are effective in the treatment of xerosis irrespectively from their particular formulation: results from a prospective, randomized, double-blind controlled trial. J Eur Acad Dermatol Venereol. 2016;30:276–281. doi: 10.1111/jdv.13472. [DOI] [PubMed] [Google Scholar]
- 14.Hon KL, Ching GK, Leung TF, Choi CY, Lee KK, Ng PC. Estimating emollient usage in patients with eczema. Clin Exp Dermatol. 2010;35:22–26. doi: 10.1111/j.1365-2230.2009.03341.x. [DOI] [PubMed] [Google Scholar]
- 15.Crowther JM, Sieg A, Blenkiron P, Marcott C, Matts PJ, Kaczvinsky JR, et al. Measuring the effects of topical moisturizers on changes in stratum corneum thickness, water gradients and hydration in vivo. Br J Dermatol. 2008;159:567–577. doi: 10.1111/j.1365-2133.2008.08703.x. [DOI] [PubMed] [Google Scholar]
- 16.Lee SS, Kim SY, Im M, Lee Y, Lee JB, Seo YJ. The influence of physiologic lipid containing moisturizer on the normal skin barrier. Korean J Dermatol. 2011;49:339–344. [Google Scholar]
- 17.Williams S, Krueger N, Davids M, Kraus D, Kerscher M. Effect of fluid intake on skin physiology: distinct differences between drinking mineral water and tap water. Int J Cosmet Sci. 2007;29:131–138. doi: 10.1111/j.1467-2494.2007.00366.x. [DOI] [PubMed] [Google Scholar]
- 18.Mac-Mary S, Creidi P, Marsaut D, Courderot-Masuyer C, Cochet V, Gharbi T, et al. Assessment of effects of an additional dietary natural mineral water uptake on skin hydration in healthy subjects by dynamic barrier function measurements and clinic scoring. Skin Res Technol. 2006;12:199–205. doi: 10.1111/j.0909-752X.2006.00160.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Stratum corneum hydration changes in different anatomical areas of the participants who were divided into group H and group L
Transepidermal water loss changes in different anatomical areas of the participants who were divided into group H and group L
The p-values of each comparative subgroup (group H vs. group L)