Abstract
Objective:
To determine if nutritional risk in early childhood is associated with parent-reported school concerns.
Design:
A prospective cohort study conducted through the TARGet Kids! primary care research network (2011–2018). Nutritional risk was measured between 18 months and 5 years of age using validated parent-completed NutriSTEP® questionnaires with eating behaviour and dietary intake subscores (0 = lowest and 68 = highest total nutritional risk score). Parent-reported school concerns were measured at school age (4–10 years of age) and included: speech and language; learning; attention; behaviour; social relationships; physical coordination; fine motor coordination and self-help skills and independence. The primary outcome was any parent-reported school concerns, and individual school concerns were used as secondary outcomes. Multiple logistic regression models were conducted adjusting for clinically relevant confounders to assess the relationship between nutritional risk and school concerns.
Setting:
Toronto, Canada.
Participants:
Children aged 18 months to 10 years.
Results:
The study included 3655 children, 52 % were male, mean NutriSTEP® score was 14·4 (sd 6·4). Each 1 sd increase in NutriSTEP® total score was associated with a 1·18 times increased odds of school concerns (adj OR: 1·18, 95 % CI 1·07, 1·28, P = 0·0004), and high nutritional risk was associated with a 1·42 times increased odds of school concerns (adj OR: 1·42, 95 % CI 1·13, 1·78, P = 0·002).
Conclusions:
Nutritional risk in early childhood was associated with school concerns. Nutritional interventions in early childhood may reveal opportunities to enhance school outcomes.
Keywords: Nutritional risk, Eating behaviours, Dietary intake, School concerns, Cognitive development, Brain development, Children
Healthy nutrition in early childhood is crucial for optimal growth and development(1). The first few years of life are important for developing healthy eating behaviours as a child learns what, when and how to eat, both through direct experience and by observing others, which may have lasting effects on their health and development(2). Nutrition in early childhood, including the absence of malnutrition, as well as adequate intake of vital macronutrients and micronutrients, is essential for normal brain development(3,4). Early life nutrition is an essential component of primary care well-child visits conducted across the US and Canada(1,5).
The relationship between nutrition and cognitive development in young children has largely focused on chronic under nutrition in low- and middle-income countries(6), breast-feeding(7,8), short-term fasting (including skipping breakfast)(9) and specific nutrient deficiencies including protein(3), Fe(10), iodine(11) and long-chain PUFA(12), all of which affect key cognitive processes. Optimising cognitive development in early childhood has long-term consequences for an individual’s behaviour in school and academic achievement(1). However, few studies have examined how overall dietary quality and eating behaviours of children under 5 years of age affect cognitive development and related functional outcomes(13–15). A systematic review by Tandon et al. in 2016 did look at this relationship and found that healthy diets in early childhood (under 5 years of age) were associated with better cognitive outcomes in young children(13). However, all of the reviewed studies focused on complex measures of dietary recall that are time-consuming and impractical in the primary care setting, and all have focused on academic outcomes or tasks for specific executive functions(13).
The parent-completed Nutrition Screening for Toddlers and Preschoolers (NutriSTEP®) are validated questionnaires for assessing nutritional risk in children aged 18 months to 5 years and only take 5 min to complete(16,17). NutriSTEP® questionnaires may be a useful tool for paediatricians and/or other child health care providers as they can be easily administered for screening of nutritional risk. Paediatricians and other health care providers have the capacity to improve early childhood nutrition, and this may be an intervention target with a goal of optimising cognitive development. In 2018, the American Academy of Pediatrics Committee on Nutrition published a policy statement titled Advocacy for Improving Nutrition in the First 1000 Days to Support Childhood Development and Adult Health(1), which emphasised a paediatrician’s role in identifying early nutritional risk. It is important to better understand the relationship between a simple easy-to-complete measure of nutritional risk and cognitive development among typically developing children.
The primary objective of this study was to determine whether nutritional risk in early childhood (defined using the NutriSTEP® total score) was associated with school concerns. Secondary objectives were to: (1) determine whether the eating behaviour and dietary intake subscores of NutriSTEP® were associated with school concerns and (2) determine whether NutriSTEP® total score was associated with each individual school concern (speech and language; learning; attention; behaviour; social relationships with other children; physical coordination; fine motor coordination; self-help skill and independence). We hypothesised higher nutritional risk would be associated with increased odds of school concerns.
Methods
Study design
A prospective cohort study was conducted through The Applied Research Group for Kids (TARGet Kids!) (www.targetkids.ca) primary care research network in Toronto, Canada.
Participants
Healthy children were recruited from primary care paediatrician or family physician offices and followed prospectively at each well-child visit between 2011 and 2018. The TARGet Kids! cohort data collection methodology has been previously described(18). This study included healthy children enrolled between birth and 5 years, as per the TARGet Kids protocol. Children were excluded if they had health conditions affecting growth (e.g. failure to thrive, cystic fibrosis), chronic condition(s) except for asthma, if they were born premature (<32 weeks gestation) or if they were diagnosed with autism, developmental delays or learning problems prior to 18 months of age.
Measurements
Participants’ parents or guardians completed detailed questionnaires at the time of enrolment and at each subsequent TARGet Kids! visit. Parent-reported measures were adapted from the Canadian Community Health Survey, which included information on child characteristics, demographics as well as age-specific health and behavioural information. NutriSTEP® questionnaires were collected annually starting at 18 months, and the school concerns question was collected at age 4 years and then annually at subsequent TARGet Kids! visits.
Exposures
The primary exposure was nutritional risk, which was measured using two validated seventeen-item parent-completed NutriSTEP® questionnaires: one for ages 18–35 months (Toddler NutriSTEP®)(17) and one for ages 36–60 months (Preschooler NutriSTEP®)(16). NutriSTEP® was designed to identify children at nutritional risk, which is defined as ‘the presence of characteristics or risk factors that can lead to impaired nutritional status’(19). The questionnaires only take 5 min for parents to complete and have been validated against a registered dietitian’s clinical assessment (criterion standard), which included parent-reported 3-d food records and growth measurements among a multicultural group of Canadian children(16,17).
The Toddler and Preschooler NutriSTEP® questionnaires are both reliable and valid for screening for nutritional risk. According to data from the validation studies, the total NutriSTEP® scores and dietitian nutrition risk ratings were correlated with Spearman rho scores of 0·67 (P-value < 0·000) and 0·48 (P-value = 0·01) for the Toddler and Preschooler NutriSTEP® questionnaires, respectively(16,17). The area under the ROC curve for moderate and high dietitian risk ratings (rating was on a ten-point scale: 1–4 low risk, 5–7 moderate risk, 8–10 high risk(16)) was 84·6 % and 82·7 % and 81·5 % and 73·8 % for the Toddler and Preschooler NutriSTEP® questionnaires, respectively(16,17). The NutriSTEP® total score was reliable between parental responses (2–4 weeks later) with intra-class correlations of 0·92 and 0·89 for the Toddler and Preschooler NutriSTEP®, respectively(16,17).
The seventeen questions are equally weighted in both questionnaires with total scores ranging from 0 (lowest nutritional risk) to 68 (highest nutritional risk)(16,17). Questions were divided a priori into the following five subscales: dietary intake, eating behaviours, parental concerns about food and activity, screen time duration and the use of vitamin/mineral supplements(20,21).
The primary exposures were: NutriSTEP® total score (continuous variable from 0 to 68) and high nutritional risk (dichotomised as low or high using a NutriSTEP® cut-off score of ≥21)(16,17). For NutriSTEP® scores above 21, it is recommended that ‘the child’s eating and activity habits can be improved by making some changes (e.g. talking to a health professional)’(16,17). The NutriSTEP® total score closest to the time of measurement of the outcome for each child was used in the analysis. The secondary exposure measures include the NutriSTEP® eating behaviours subscore and the NutriSTEP® dietary intake subscore(8,20,21). See supplementary material for details on specific questions included in these subscores.
Outcomes
The primary outcome was the presence of school concerns at ages 4–10 years. In Ontario, Canada, most children complete 2 years of kindergarten before entering grade 1 at the age of 6 years. We measured school concerns using the parent-completed question ‘has the school expressed any concern about your child’s (please select one or more of the following): speech and language; learning; attention; behaviour; social relationships with other children; physical coordination; fine motor coordination; self-help skill and independence; and no concern’. This outcome was dichotomised into yes concern (a yes response to one or more school concerns ever in the past) or no concern (always a no response to school concerns). Secondary outcomes were individual school concerns separately (dichotomised as either yes or no concern).
Covariates
We identified potential confounders of the relationship between nutritional risk and school concerns a priori through a literature review. All variables known or suspected to influence the relationship between exposure and outcome were included as covariates in the final analysis. All covariates were measured at the same time as the outcome. Covariates included child sex(22), child age(23), child ethnicity(23), maternal education(22), family income(22), breast-feeding duration(8,24–26), family living arrangements(22), the WHO age- and sex-standardised zBMI(22,27), birth weight(28) and a diagnosis of developmental delay(29,30). Child ethnicity was collapsed into either European, non-European or mixed-ethnicity categories. Maternal education was dichotomised into either college/university or primary/high school education. Total family income prior to tax was categorised into four groups: (1) <$60 000, (2) $60 000–$99 000, (3) $100 000–$150 000 and (4) above $150 000. Breast-feeding duration was defined as the duration of breast-feeding of any kind (i.e. including both exclusive and nonexclusive breast-feeding), determined using the question ‘For how long has your child been breastfed?’(31). Family living arrangements were dichotomised into two categories: (1) lives with two parents in the same household and (2) lives with two parents alternating households or lives with one parent only. We assessed if the relationship between NutriSTEP® and school concerns was different in: (1) children with a physician diagnosis of developmental delay; and (2) younger v. older children using interaction terms in the model (younger v. older children was added in a post hoc analysis). Trained research staff embedded within each practice site collected physical measurements, using standardised anthropometric protocols(32), including weight (using a precision digital scale) and height/length (using a stadiometer for children >2 years and length board for children <2 years)(33). BMI was calculated as weight in kg divided by height in metres squared, and age- and sex-standardised z scores were calculated using the WHO growth standards(33).
Medidata RAVE was used as the secure electronic data repository, and all data were stored at the Applied Health Research Centre at St. Michael’s Hospital, Toronto.
Statistical analysis
Descriptive statistics were calculated for the exposures, outcome and covariates for all children and those classified as low and high nutritional risk.
A multiple logistic regression model was used to examine the relationship between NutriSTEP® total score and school concerns, adjusting for all covariates. A 1 sd change was calculated by taking: child’s NutriSTEP® total score – NutriSTEP® sample mean (14·4)/NutriSTEP® sample standard deviation (sd 6·4). We used a generalised variance inflation factor test to test for multicollinearity in order to ensure the models produced stable effects(34). All covariates were included in the final models regardless of statistical significance to avoid bias that can arise from variable selection techniques. We tested for a physician-diagnosed developmental delay and age as interaction terms in the model. Further, we used multiple imputation (n 20) to avoid bias that can result from missing data (all covariates had <15 % missing data). We repeated this approach using the high nutritional risk cut-off score, and eating behaviour and dietary intake subscores and the individual school concerns separately. We applied the Šidák correction technique when investigating the individual school concerns, which lowers the α value to account for the effect of multiple testing.
Statistical analyses were conducted using SAS statistical software version 9.4 (SAS Institute Inc.)(35). P-values and 95 % CI are both included for individual interpretation of clinical significance.
Ethics approval
Parents of TARGet Kids! participants provided informed consent for primary data collection, and ethics approval was obtained from the Research Ethics Boards at the Hospital for Sick Children and Unity Health Toronto. The study is registered at www.clinicaltrials.gov (NCT01869530).
Results
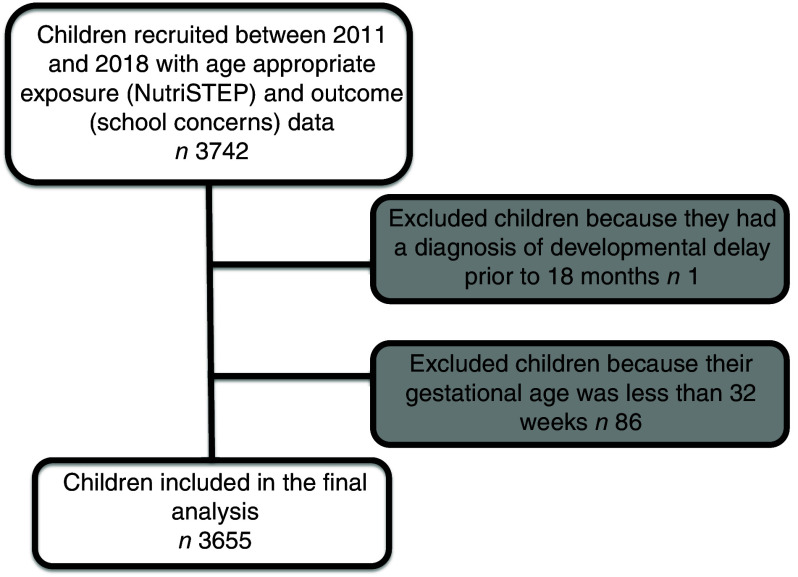
The study included 3655 children (Fig. 1). Fifty-two percentage were male, and mean age at outcome was 67 months (sd 19; range 48–130 months). The mean NutriSTEP® score was 14·4 (sd 6·4; range 0–45), and the number of children classified as high nutritional risk (i.e. NutriSTEP® score ≥ 21) was 591 (16 %) (Table 1). Twenty-seven percentage of parents reported school concerns. The most commonly reported school concerns were: attention (11 %), speech and language (10 %), behaviour problem (9 %) and learning problem (8 %). Children above 6 years of age (≥72 months) had a higher frequency of parent-reported school concerns with 42 % reporting any concern compared with 19 % of children <72 months). This difference was most apparent for the learning, attention and behaviour concerns. Two thousand two hundred and fifty-nine children (62 %) had exposure and outcome measured at the same visit. The mean number of days between the exposure and outcome measurement was 379 (sd 560; range 0–2539 d). The majority of data came from the preschooler NutriSTEP® (n 3635 or 99·5 %) v. the toddler NutriSTEP® (n 18 or 0·5 %).
Fig. 1.
Participant flow diagram
Table 1.
Baseline characteristics
| All (n 3655) | High nutritional risk ≥ 21 * (n 591) | Low nutritional risk < 21 (n 3064) | |||||
|---|---|---|---|---|---|---|---|
| Variable | n | n | % | n | % | n | % |
| Male | 3654 | 1910 | 52 | 345 | 58 | 1565 | 51 |
| Age at outcome (months) | 3655 | 67 | 19 | 67 | 18 | 67 | 19 |
| Child ethnicity | 3447 | ||||||
| European | 2065 | 60 | 202 | 36 | 1863 | 64 | |
| Non-European | 568 | 16 | 208 | 37 | 360 | 12 | |
| Mixed ethnicity | 814 | 24 | 146 | 26 | 668 | 23 | |
| Maternal education | 3634 | ||||||
| College/university | 3365 | 93 | 482 | 82 | 2883 | 95 | |
| High school or public school | 269 | 7 | 103 | 18 | 166 | 5 | |
| Family income | 3579 | ||||||
| <$60 000 | 483 | 13 | 198 | 35 | 285 | 9 | |
| $60 000–$99 000 | 595 | 17 | 131 | 23 | 464 | 15 | |
| $100 000–$150 000 | 692 | 19 | 102 | 18 | 590 | 20 | |
| Above $150 000 | 1809 | 51 | 141 | 25 | 1668 | 55 | |
| Breast-feeding duration (months) | 3580 | 10·7 | 7·4 | 9·5 | 8·1 | 10·9 | 7·2 |
| Family marital status | 3649 | ||||||
| Lives with 2 parents same household | 335 | 92 | 501 | 85 | 2844 | 93 | |
| Lives with 1 parent or alternates between 2 households | 304 | 8 | 88 | 15 | 216 | 7 | |
| Birth weight (g) | 3126 | 3·3 | 0·6 | 3·1 | 10·6 | 3·3 | 0·6 |
| BMI z-score† | 3650 | 0·1 | 1·0 | 0·02 | 1·2 | 0·2 | 0·9 |
| Any diagnosis of developmental delay‡ | 3548 | 156 | 4 | 45 | 8 | 111 | 4 |
| NutriSTEP®total score, mean (sd) | 3655 | 14·4 | 6·4 | 25·1 | 4·3 | 12·3 | 4·3 |
NutriSTEP®, Nutrition Screening for Toddlers and Preschoolers.
Data presented as mean (sd) or frequency (%).
A NutriSTEP® score ≥ 21 is categorised as high nutritional risk and low nutritional risk is categorised as scores <21.
BMI z-score = age- and sex-standardised BMI.
Either autism, developmental delay and/or a learning problem.
It was estimated that each 1 sd increase in NutriSTEP® total score was associated with an 18 % increased odds of school concerns (adj OR: 1·18, P-value 0·0004 and 95 % CI 1·07, 1·28). High nutritional risk (i.e. NutriSTEP® score ≥ 21) was associated with a 42 % increased odds of school concerns compared with low nutritional risk (adj OR: 1·42, P-value 0·002 and 95 % CI 1·13, 1·78). The adjusted OR for the eating behaviours and dietary intake subscores were adj OR: 1·03 (P-value 0·53 and 95 % CI 0·94, 1·12) and adj OR: 1·08 (P-value 0·07 and 95 % CI 0·99, 1·18), respectively. (Table 2). It was also estimated that increases in NutriSTEP® total score were associated with increased odds of many individual school concerns including learning, attention, social relationship with other children, physical coordination, fine motor coordination and self-help skills and independence (Table 3 and see online supplementary material, Supplemental Table 1). The OR for speech and language as well as behaviour were directionally similar to the other school concerns but did not reach statistical significance (P-values > 0·05). An interaction between NutriSTEP® and physician-diagnosed developmental delay revealed a P-value of 0·6, making this interaction unlikely, and it was not included in the final model. In a post hoc analysis, we included an interaction between NutriSTEP® and age in months at outcome. This revealed a P-value of 0·09, making this interaction probable, and thus we stratified the analysis based on age (<72 and ≥72 months). The relationship between nutritional risk and school concerns was evident among children <72 months but not among children ≥72 months; NutriSTEP® total score was associated with a 33 % increased odds of school concerns among children <72 months (adj OR: 1·33, P-value < 0·0001 and 95 % CI 1·18, 1·49) but not among children ≥72 months (adj OR: 1·01, P-value = 0·89 and 95 % CI 0·88, 1·16) (Table 4 post hoc analysis).
Table 2.
Logistic regression analysis between nutritional risk (Nutrition Screening for Toddlers and Preschoolers (NutriSTEP®) total score, high nutrition risk, eating behaviour subscore, and dietary intake subscore) and school concerns, n 3653
| Unadjusted | Adjusted* | |||
|---|---|---|---|---|
| Exposure variable | OR | P-value; 95 % CI | adj OR | P-value; 95 % CI |
| NutriSTEP® total score | 1·20 | < 0·0001; 1·12, 1·29 | 1·18 | 0·0004; 1·07, 1·28 |
| High nutritional risk† | 1·50 | < 0·0001; 1·24, 1·81 | 1·42 | 0·002; 1·13, 1·78 |
| NutriSTEP® eating behaviour subscore | 1·11 | 0·004; 1·04, 1·20 | 1·03 | 0·53; 0·94, 1·12 |
| NutriSTEP® dietary intake subscore | 1·1 | 0·007; 1·03, 1·19 | 1·08 | 0·07; 0·99, 1·18 |
Model adjusted for child sex, child age, child ethnicity, maternal education, family income, breast-feeding duration, family living arrangements, zBMI, birth weight and a diagnosis of developmental delay.
A NutriSTEP® score ≥ 21 is categorised as high nutritional risk.
Table 3.
Logistic regression analysis between nutritional risk (Nutrition Screening for Toddlers and Preschoolers (NutriSTEP®) total score) and individual school concerns
| Adjusted* | ||
|---|---|---|
| Outcome variable (n)‡ | adj OR | P-value; 95 % CI† |
| Speech and language (n 377) | 1·13 | 0·07; 0·94, 1·34 |
| Learning (n 297) | 1·34 | < 0·0001; 1·09, 1·65 |
| Attention (n 399) | 1·16 | 0·02; 0·97, 1·38 |
| Behaviour (n 318) | 1·11 | 0·15; 0·91, 1·34 |
| Social relationships with other children (n 232) | 1·19 | 0·03; 0·95, 1·48 |
| Physical coordination (n 71) | 1·57 | 0·005; 1·01, 2·45 |
| Fine motor coordination (n 234) | 1·28 | 0·0025; 1·02, 1·59 |
| Self-help skills and independence (n 118) | 1·41 | 0·0023; 1·04, 1·92 |
Model adjusted for child sex, child age, child ethnicity, maternal education, family income, breast-feeding duration, family living arrangements, zBMI, birth weight and a diagnosis of developmental delay.
The Šidák corrected alpha is 0·0064.
The number of children with a yes response to the individual school concern.
Table 4.
Stratified logistic regression analysis (children <72 months and ≥72 months) between nutritional risk (Nutrition Screening for Toddlers and Preschoolers (NutriSTEP®) total score, high nutrition risk, eating behaviour subscore and dietary intake subscore) and school concerns (post hoc analysis)
| Age at outcome | ||||
|---|---|---|---|---|
| Exposure variable | <72 months, n 2358, adj OR* | P-value; 95 % CI | ≥72 months, n 1297, adj OR* | P-value; 95 % CI |
| NutriSTEP® total score | 1·33 | < 0·0001; 1·18, 1·49 | 1·01 | 0·89; 0·88, 1·16 |
| High nutritional risk† | 2·01 | < 0·0001; 1·49, 2·71 | 0·92 | 0·63; 0·65, 1·30 |
| NutriSTEP® eating behaviour subscore | 1·14 | 0·02; 1·02, 1·29 | 0·91 | 0·17; 0·80, 1·04 |
| NutriSTEP® dietary intake subscore | 1·13 | 0·04; 1·01, 1·27 | 1·00 | 0·97; 0·88, 1·14 |
Model adjusted for child sex, child age, child ethnicity, maternal education, family income, breast-feeding duration, family living arrangements, zBMI, birth weight and a diagnosis of developmental delay.
A NutriSTEP® score ≥ 21 is categorised as high nutritional risk.
Discussion
In this prospective cohort study, we found that higher nutritional risk among a group of young healthy urban children (18 months to 5 years) was associated with increased odds of school concerns. Nutrients play a critical role in cell proliferation, DNA synthesis, neurotransmitter and hormone metabolism, as well as enzyme systems all of which can impact the developing brain(36). Furthermore, beyond the nutrients themselves, the eating experience provides an opportunity for children to learn which can affect their psychosocial and emotional development(37). A child learns self-regulation through determining the timing, amount and pace of a meal(37). Also, early feeding experiences and encouragement of developmentally appropriate eating behaviours may impact feeding behaviours later in life(37). Both the nutritional value of food and eating behaviours are important in young children and may impact a child’s later cognitive development(36). Optimising cognitive development in early childhood has long-term consequences for an individual’s behaviour in school, academic achievement, job potential and lifetime success(1).
Previous research has suggested that dietary patterns established prior to school age may influence food choices later in life(38,39). However, many of the studies which examined the relationship between a child’s diet in early life and cognitive development have largely focused on breast-feeding(24–26) and specific nutrient deficiencies (e.g. protein(3), Fe(10), iodine(11) and long-chain PUFA(12)), with only a few studies looking at the relationship between dietary patterns in early life and cognitive outcomes(13–15). It is important to investigate the diet more broadly as individuals consume combinations of foods. Overall diet, including dietary intake and eating behaviours, may serve as an early target for dietary interventions aimed at improving cognitive development and related functional outcomes in children.
A systematic review conducted in 2016 by Tandon et al. found eight studies (all longitudinal cohorts in England, Scotland and Australia) that examined the relationship between dietary patterns among children <5 years and later cognitive development(13). They found that healthy diets in early childhood were associated with better cognitive outcomes. The outcomes in these studies focused on academic outcomes or tasks for specific executive functions, and there was a large degree of variability across the measures used(13). Further, all of the studies focused on dietary patterns including complex, often burdensome, quantitative measures of assessing total diet (e.g. 24-h diet recalls, FFQ or food diaries), dietary patterns, meal composition and other measures of overall diet(13). Use of such quantitative methods for assessing diet quality is time-consuming and impractical in primary care and public health settings. In contrast to measures used in the Tandon et al. review, NutriSTEP® is an easy and feasible questionnaire to administer in the primary care or public health settings. Further, many of the studies in the Tandon et al. review were not able to control for important confounders, including ethnicity, measured BMI, breast-feeding or socio-economic disparities, which are important when trying to understand the independent impact of nutrition on cognitive development(13).
This study is the first to assess the relationship between nutritional risk using validated questionnaires that include composite measures of both dietary intake and eating behaviour in early childhood and parent-reported school concerns. We found that higher nutritional risk was associated with increased odds of school concerns and this relationship persisted even after adjusting for a number of potential confounders including child sex, age, ethnicity, zBMI, maternal education, family income, breast-feeding duration, family living arrangements, birth weight and a diagnosis of developmental delay. We did not find evidence to support a different effect of nutritional risk in children with and without physician-diagnosed developmental delay on school concerns. Potentially due to the young ages of children in this cohort, few were diagnosed with developmental delay, which may have limited our ability to detect a modifying effect. There was some evidence that higher nutritional risk was associated with increased odds of some of the individual school concerns and all estimated OR were in the expected direction (all OR > 1). NutriSTEP® was designed as a screening tool for nutritional risk, but this study also suggests that it may have predictive validity for school concerns. In a post hoc analysis, we did find evidence that the relationship between nutritional risk and school concerns may be different depending on the age at outcome of the child; thus, we stratified our analysis based on age (<72 and ≥72 months). We choose 72 months (or 6 years) as this is the year children usually enter grade 1 in Canada. After stratifying the analysis it appears, the relationship between nutritional risk and school concerns is evident among younger children (<72 months) but not older children (≥72 months). This could be due to the shorter time window between exposure and outcome for the younger age group (although 62 % of children had their exposures and outcome measured at the same time); parents had a longer time to observe older children and thus had more chance to potentially notice a concern, which is a challenge of using ‘ever yes to school concern’; and the nutritional risk may itself change over time for children, which was not measured in this study.
The speed of brain growth in early life may be particularly sensitive to dietary factors(40). Given that early childhood is an important stage for the development of good eating habits, and at the same time, a critical stage in cognitive development, understanding the relationship between nutrition and cognitive development in early childhood is important for developing prevention interventions aimed to improve children’s school success. Interventions that target eating behaviours and dietary intake, with a goal to reduce nutritional risk in early childhood, may have a beneficial impact on a child’s development. Screening children in primary care for nutritional risk and applying appropriate dietary interventions may reduce children’s risk of poor cognitive development and school concerns. Future research could assess the relationship between nutritional risk and child development in early life using teachers as an alternative respondent (e.g. Early Development Instrument(41)). Future research could also investigate the role of NutriSTEP® as a screening tool for other developmental outcomes and to better investigate some of the individual school concerns.
There were several strengths of this study. It was a large prospective cohort of young children and included a validated questionnaire for assessing nutritional risk. Detailed parent-reported questionnaire data were available for multiple potential confounders, and thus we were able to adjust the models for many established risk factors of child development. This study also had a number of limitations. Causality cannot be inferred due to the observational study design. Both the exposure and outcome were from parent-reported questionnaires and therefore may have been subject to response bias including social desirability and/or recall bias. There are slight differences between the two NutriSTEP® questionnaires (particularly around age-specific eating behaviours; see supplementary material for details on the questions included in these subscores); however, over 99 % of the data came from the preschooler NutriSTEP®, and thus these differences likely did not impact the results. The question about the presence of school concerns is not a validated measure for assessing a child’s development with a wide range of individual concerns. The conclusions related to the individual school concerns data are limited, and lack of significant findings for speech and language as well as behaviour should be interpreted with caution; future research should focus on each concern separately (e.g. association between nutritional risk and school concern for speech/language). Future work is needed to better understand this relationship with a non-parent-reported outcome, such as a teacher-reported measure. We included age at outcome as a confounder in the analysis and stratified the analysis based on age; however, future research exploring the association between nutritional risk and smaller age ranges may help identify critical time periods. A parent report of a physician diagnosis of developmental delay is an important potential effect modifier that we included in our study; however, some children in this young cohort may have a developmental concern but have not yet received a formal diagnosis. Finally, participation in TARGet Kids! is voluntary, which puts the sample at risk of selection bias; however, the sociodemographic characteristics of the TARGet Kids! cohort have been compared with Canadian census data, which found the participants had higher household income and higher maternal education levels but were otherwise comparable to the Canadian population(42).
Conclusion
Nutritional risk in early childhood was associated with school concerns, after controlling for potential confounding variables. NutriSTEP® is an easy and feasible questionnaire to administer and may be useful in the primary care or public health settings. Nutrition interventions in early childhood targeting both diet and eating behaviours may have an impact on improving developmental outcomes among school-age children.
Acknowledgements
Acknowledgements: We thank all of the participating families for their time and involvement in TARGet Kids! and are grateful to all practitioners who are currently involved in the TARGet Kids! practice-based research network. Financial support: Funding to support TARGet Kids! was provided by multiple sources including the Canadian Institutes for Health Research (CIHR), namely the Institute of Human Development, Child and Youth Health and the Institute of Nutrition, Metabolism and Diabetes (CIHR; FRN-115059), as well as the St. Michael’s Hospital Foundation (2012-0051-GF). Funding to support the first author, Dr. Jessica Omand, was provided by the Canadian Child Health Clinician Scientist Program, Restracomp through the Clinician Scientist Training Program (CSTP) at the Hospital for Sick Children and Thor E. and Nicole Eaton Family Charitable Foundation Fellowship at the Hospital for Sick Children’s Centre for Brain & Mental Health. Funding agencies had no role in the design, collection, analyses or interpretation of the results of this study or in the preparation, review or approval of the manuscript. Conflict of interest: J.A.O. none. M.J. none. J.L.M. received an unrestricted research grant for a completed investigator-initiated study from the Dairy Farmers of Canada (2011–2012) and Ddrops provided non-financial support (vitamin D supplements) for an investigator-initiated study on vitamin D and respiratory tract infections (2011–2015). P.C.P. received unrestricted research grants for completed investigator-initiated studies from Danone Institute of Canada (2002–2004 and 2006–2009), Dairy Farmers of Ontario (2008–2010). Mead Johnson Nutrition provided non-financial support (Fer-In-Sol® liquid iron supplement) (2011–2017) for an ongoing investigator-initiated trial of iron deficiency in young children that was funded by Canadian Institutes of Health Research (FRN no. 115059). J.R.S. none. C.D.G.K.S. none. M.A. none. C.S.B. received a research grant from the Centre for Addiction and Mental Health Foundation (CAMH 2017–2020). Authorship: Dr J.A.O. conceptualised and designed the study, carried out the initial analyses, drafted the initial manuscript and revised the manuscript. Dr C.S.B. conceptualised and designed the study as well as critically reviewed/revised the manuscript for important intellectual content. Drs M.J., J.L.M., P.C.P., J.R.S and M.A. helped refine the study design and reviewed/revised the manuscript. Dr C.D.G.K.S. helped refine the study design, contributed to the interpretation of the results and reviewed/revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research participants were approved by the Research Ethics Boards at the Hospital for Sick Children and Unity Health Toronto. Written informed consent was obtained from all subjects/patients.
Collaborators: * TARGet Kids! Collaborators – Co-Leads: Catherine S. Birken, Jonathon L. Maguire; Advisory Committee: Ronald Cohn, Eddy Lau, Andreas Laupacis, Patricia C. Parkin, Michael Salter, Peter Szatmari, Shannon-Weir; Science Review and Management Committees: Laura N. Anderson, Cornelia M. Borkhoff, Charles Keown-Stoneman, Christine Kowal, Dalah Mason; Site Investigators: Murtala Abdurrahman, Kelly Anderson, Gordon Arbess, Jillian Baker, Tony Barozzino, Sylvie Bergeron, Dimple Bhagat, Gary Bloch, Joey Bonifacio, Ashna Bowry, Caroline Calpin, Douglas Campbell, Sohail Cheema, Elaine Cheng, Brian Chisamore, Evelyn Constantin, Karoon Danayan, Paul Das, Mary Beth Derocher, Anh Do, Kathleen Doukas, Anne Egger, Allison Farber, Amy Freedman, Sloane Freeman, Sharon Gazeley, Charlie Guiang, Dan Ha, Curtis Handford, Laura Hanson, Leah Harrington, Sheila Jacobson, Lukasz Jagiello, Gwen Jansz, Paul Kadar, Florence Kim, Tara Kiran, Holly Knowles, Bruce Kwok, Sheila Lakhoo, Margarita Lam-Antoniades, Eddy Lau, Denis Leduc, Fok-Han Leung, Alan Li, Patricia Li, Jessica Malach, Roy Male, Vashti Mascoll, Aleks Meret, Elise Mok, Rosemary Moodie, Maya Nader, Katherine Nash, Sharon Naymark, James Owen, Michael Peer, Kifi Pena, Marty Perlmutar, Navindra Persaud, Andrew Pinto, Michelle Porepa, Vikky Qi, Nasreen Ramji, Noor Ramji, Danyaal Raza, Alana Rosenthal, Katherine Rouleau, Caroline Ruderman, Janet Saunderson, Vanna Schiralli, Michael Sgro, Hafiz Shuja, Susan Shepherd, Barbara Smiltnieks, Cinntha Srikanthan, Carolyn Taylor, Stephen Treherne, Suzanne Turner, Fatima Uddin, Meta van den Heuvel, Joanne Vaughan, Thea Weisdorf, Sheila Wijayasinghe, Peter Wong, John Yaremko, Ethel Ying, Elizabeth Young, Michael Zajdman; Research Team: Farnaz Bazeghi, Vincent Bouchard, Marivic Bustos, Charmaine Camacho, Dharma Dalwadi, Christine Koroshegyi, Tarandeep Malhi, Sharon Thadani, Julia Thompson, Laurie Thompson; Project Team: Mary Aglipay, Imaan Bayoumi, Sarah Carsley, Katherine Cost, Karen Eny, Theresa Kim, Laura Kinlin, Jessica Omand, Shelley Vanderhout, Leigh Vanderloo; Applied Health Research Centre: Christopher Allen, Bryan Boodhoo, Olivia Chan, David W.H. Dai, Judith Hall, Peter Juni, Gerald Lebovic, Karen Pope, Kevin Thorpe; Mount Sinai Services Laboratory: Rita Kandel, Michelle Rodrigues, Hilde Vandenberghe.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980021001725.
click here to view supplementary material
References
- 1. Schwarzenberg SJ & Georgieff MK (2018) Committee on Nutrition. Advocacy for improving nutrition in the first 1000 days to support childhood development and adult health: American Academy of Pediatrics Policy Statement. Pediatrics 141, e20173716. [DOI] [PubMed] [Google Scholar]
- 2. Birch L, Savage JS & Ventura A (2007) Influences on the development of children’s eating behaviours: from infancy to adolescence. Can J Diet Pract Res 68, s1–s56. [PMC free article] [PubMed] [Google Scholar]
- 3. Grantham-McGregor S (1995) A review of studies of the effect of severe malnutrition on mental development. J Nutr 125, 2233S–2238S. [DOI] [PubMed] [Google Scholar]
- 4. Pollitt E, Gorman KS, Engle PL et al. (1995) Nutrition in early life, the fulfillment of intellectual potential. J Nutr 125, 1111S–1118S. [DOI] [PubMed] [Google Scholar]
- 5. Caring for Kids (2016) Canadian Paediatric Society Schedule of Well-child Visits. https://www.caringforkids.cps.ca/handouts/pregnancy-and-babies/schedule_of_well_child_visits (accessed January 2021).
- 6. Vaivada T, Gaffey MF & Bhutta ZA (2017) Promoting early child development with interventions in health and nutrition: a systematic review. Pediatrics 140, e20164308. [DOI] [PubMed] [Google Scholar]
- 7. Lee H, Park H, Ha E et al. (2016) Effect of breastfeeding duration on cognitive development in infants: 3-year follow-up study. J Korean Med Sci 31, 579–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Borkhoff CM, Dai DWH, Jairam JA et al. (2018) Breastfeeding to 12 month and beyond: nutrition outcomes at 3 to 5 years of age. Am J Clin Nutr 108, 354–362. [DOI] [PubMed] [Google Scholar]
- 9. Rampersaud GC, Pereira MA, Girard BL et al. (2005) Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Dietetic Assoc 105, 743–760. [DOI] [PubMed] [Google Scholar]
- 10. Georgieff MK (2011) Long-term brain and behavioral consequences of early iron deficiency. Nutr Rev 69, S43–S48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Prado EL & Dewey KG (2014) Nutrition and brain development in early life. Nutr Rev 72, 267–284. [DOI] [PubMed] [Google Scholar]
- 12. Colombo J, Carlson SE, Cheatham CL et al. (2013) Long-term effects of LCPUFA supplementation on childhood cognitive outcomes. Am J Clin Nutr 98, 403–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tandon PS, Tovar A, Jayasuriya AT et al. (2016) The relationship between physical activity and diet and young children’s cognitive development: a systematic review. Prev Med Rep 3, 379–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Theodore RF, Thompson J, Waldie KE et al. (2009) Dietary patterns and intelligence in early and middle childhood. Intelligence 37, 506–513. [Google Scholar]
- 15. Smithers LG, Golley RK, Mittinty MN et al. (2012) Dietary patterns at 6, 15 and 24 months of age are associated with IQ at 8 years of age. Dev Epidemiol 27, 525–535. [DOI] [PubMed] [Google Scholar]
- 16. Randall Simpson JA, Keller HH, Rysdale LA et al. (2008) Nutrition Screening Tool for Every Preschooler (NutriSTEP): validation and test-retest reliability of a parent-administered questionnaire assessing nutrition risk of preschoolers. Eur J Clin Nutr 62, 770–780. [DOI] [PubMed] [Google Scholar]
- 17. Randall Simpson J, Gumbley J, Whyte K et al. (2015) Development, reliability, and validity testing of Toddler NutriSTEP: a nutrition risk screening questionnaire for children 18–35 months of age. Appl Physiol Nutr Metab 40, 877–886. [DOI] [PubMed] [Google Scholar]
- 18. Carsley S, Borkhoff CM, Maguire JL et al. (2015) Cohort Profile: The Applied Research Group for Kids (TARGet Kids!). Int J Epidemiol 44, 776–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. American Dietetic Association (1994) ADA’s definitions for nutrition screening and nutrition assessment. J Am Diet Assoc 94, 838–839. [DOI] [PubMed] [Google Scholar]
- 20. Persaud N, Ziai H, Lebovic G et al. (2017) Parent reported nutritional risk, laboratory indices of cardiometabolic risk, in preschool-aged children. J Pediatr Endocrinol Metab 30, 839–846. [DOI] [PubMed] [Google Scholar]
- 21. Persaud N, Maguire JL, Lebovic G et al. (2013) Association between serum cholesterol and eating behaviours during early childhood: a cross-sectional study. CMAJ 185, E531–E536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Florence MD, Asbridge M & Veugelers PJ (2008) Diet quality and academic performance. J Sch Health 78, 209–215. [DOI] [PubMed] [Google Scholar]
- 23. Janus M & Duku E (2007) The school entry gap: socioeconomic, family, and health factors associated with children’s school readiness to learn. Early Educ Dev 18, 375–403. [Google Scholar]
- 24. Bar S, Milanaik R & Adesman A (2016) Long-term neurodevelopmental benefits of breastfeeding. Curr Opin Pediatr 28, 559–566. [DOI] [PubMed] [Google Scholar]
- 25. Belfort MB, Anderson PJ, Nowak VA et al. (2016) Breast milk feeding, brain development, and neurocognitive outcomes: a 7-year longitudinal study in infants born at less than 30 weeks’ gestation. J Pediatr 177, 133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kramer MS, Aboud F, Mironova E et al. (2009) Breastfeeding and child cognitive development. Arch Gen Psychiatr 65, 578–584. [DOI] [PubMed] [Google Scholar]
- 27. He J, Chen X, Fan X et al. (2019) Is there a relationship between body mass index and academic achievement? A meta-analysis. Public Health 167, 111–124. [DOI] [PubMed] [Google Scholar]
- 28. Feinstein L, Sabates R, Sorhaindo A et al. (2008) Dietary patterns related to attainment in school: the importance of early eating patterns. J Epidemiol Community Health 62, 734–739. [DOI] [PubMed] [Google Scholar]
- 29. Lichtenwalter L, Freeman R, Lee M et al. (1993) Providing nutrition services to children with special needs in a community setting. Top Clin Nutr 8, 75–78. [Google Scholar]
- 30. The American Dietetic Association (1995) Position of the American Dietetic Association: nutrition services for children with special health needs. J Am Dietetic Assoc 95, 809–812. [PubMed] [Google Scholar]
- 31. Li R, Scanlon KS & Serdula MK (2005) The validity and reliability of maternal recall of breastfeeding practice. Nutr Rev 63, 103–110. [DOI] [PubMed] [Google Scholar]
- 32. NHANES III (1988–1994) (2019) Anthropometric Procedure Videos. https://wwwn.cdc.gov/nchs/nhanes/nhanes3/AnthropometricVideos.aspx (accessed August 2019).
- 33. World Health Organization (2006) WHO child growth standards. Methods and development: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age. https://www.who.int/childgrowth/publications/technical_report_pub/en/ (accessed August 2019).
- 34. Hair JF, Anderson RE, Tatham RL et al. (1995) Multivariate Data Analysis, 3rd ed. Englewood Cliffs, NJ: Prentice-Hall. [Google Scholar]
- 35. SAS (2019) Institute Inc SAS. https://www.sas.com/en_us/software/sas9.html (accessed August 2019).
- 36. Nyaradi A, Li J, Hickling S et al. (2013) The role of nutrition in children’s neurocognitive development, from pregnancy through childhood. Front Hum Neurosci 7, 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Satter E (1990) The feeding relationship: problems and interventions. J Pediatr 117, S181–S189. [DOI] [PubMed] [Google Scholar]
- 38. Northstone K & Emmett P (2008) Are dietary patterns stable throughout early and mid-childhood? A birth cohort study. Br J Nutr 100, 1069–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mikkila V, Rasanen L, Raitakari OT et al. (2005) Consistent dietary patterns identified from childhood to adulthood: the Cardiovascular Risk in Young Finns study. Br J Nutr 93, 923–931. [DOI] [PubMed] [Google Scholar]
- 40. Isaacs EB, Gadian DG, Sabatini S et al. (2008) The effect of early human diet on caudate volumes and IQ. Pediatr Res 63, 308–314. [DOI] [PubMed] [Google Scholar]
- 41. Janus M & Offord DR (2007) Development and psychometric properties of the Early Development Instrument (EDI): a measure of children’s school readiness. Can J Behav Sci/Revue canadienne sciences du comportement 39, 1–22. [Google Scholar]
- 42. Shah N, Parkin PC, Anderson L et al. (2018) Assessing the generalizability of the target kids! cohort. American public health association annual meeting, Expo. https://apha.confex.com/apha/2018/meetingapp.cgi/Paper/416993 (accessed August 2019).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980021001725.
click here to view supplementary material