Abstract
Objective:
Although small fish are an important source of micronutrients, the relationship between their intake and mortality remains unclear. This study aimed to clarify the association between intake of small fish and all-cause and cause-specific mortality.
Design:
We used the data from a cohort study in Japan. The frequency of the intake of small fish was assessed using a validated FFQ. The hazard ratio (HR) and 95 % confidence interval (CI) for all-cause and cause-specific mortality according to the frequency of the intake of small fish by sex were estimated using a Cox proportional hazard model with adjustments for covariates.
Setting:
The Japan Multi-Institutional Collaborative Cohort Study.
Participants:
A total of 80 802 participants (34 555 males and 46 247 females), aged 35–69 years.
Results:
During a mean follow-up of 9·0 years, we identified 2482 deaths including 1495 cancer-related deaths. The intake of small fish was statistically significantly and inversely associated with the risk of all-cause and cancer mortality in females. The multivariable-adjusted HR (95 % CI) in females for all-cause mortality according to the intake were 0·68 (0·55, 0·85) for intakes 1–3 times/month, 0·72 (0·57, 0·90) for 1–2 times/week and 0·69 (0·54, 0·88) for ≥ 3 times/week, compared with the rare intake. The corresponding HR (95 % CI) in females for cancer mortality were 0·72 (0·54, 0·96), 0·71 (0·53, 0·96) and 0·64 (0·46, 0·89), respectively. No statistically significant association was observed in males.
Conclusions:
Intake of small fish may reduce the risk of all-cause and cancer mortality in Japanese females.
Keywords: Small fish, All-cause mortality, Cancer, Cohort studies, Japanese
Introduction
Small fish are among the important sources of micronutrients such as Ca, Mg and vitamins A and D when consumed whole with bones and inner organs(1–6). These nutrients contribute to the prevention of non-communicable diseases, including cardiovascular disease (CVD) and cancer, through their antihypertensive, atherosclerosis-inhibiting and antitumour effects(7–12). Bone, eyes and inner organs of fish are reservoirs of most micronutrients, including Ca and vitamin A(1,2). Unlike large fish in which bones and organs are often discarded, small fish offer a unique advantage in that they can be consumed as a whole.
Japanese people habitually eat several types of small fish, including whitebait, Atlantic capelin (shishamo), Japanese smelt (Hypomesus nipponensis) (wakasagi), small horse mackerel, young sweetfish and small dried sardine, as a whole. These small fish are consumed in a variety of ways, such as raw or marinated in vinegar, simmered in soy sauce, salted semi-dried and deep-fried. Fish, such as capelin and smelt, are mostly 10–15 cm in length, whereas smaller ones, such as whitebait, are less than 3·5 cm in length(13). These small fish are retailed as frozen or refrigerated products throughout the year. The habit of eating small fish as a whole is also found in other Asian countries besides Japan and some African and European countries. In developing countries, the intake of affordable small fish as a whole is expected to improve severe micronutrient deficiency(1–3,14).
Fish intake has been suggested to be associated with a lower risk of all-cause, cancer and CVD mortality in several cohort studies and meta-analyses, with inconsistent findings for cancer mortality(15–20). Such association, however, has not been specifically assessed for the intake of small fish. Considering that intake of small fish as a whole including the bone and organs may be effective in reducing the mortality risk in a manner different from the ones for non-small fish, it is necessary to assess the association between mortality and the intake of small fish instead of fish consumption in general.
To address this issue, in the present study, we aimed at elucidating the association between the intake of small fish and the risk of all-cause, cancer and CVD mortality using data from a large-scale cohort study in Japan.
Methods
Participants
For the present analysis, participants, aged 35–69 years, in the Japan Multi-Institutional Collaborative Cohort (J-MICC) Study were included. The details of the J-MICC Study and the recruitment of participants were described previously(21). In brief, the J-MICC Study is a large cohort study in Japan, which was launched in 2005 and enrolled residents in the community, health check examinees and first-visit patients at a cancer hospital. Some participants were recruited in 2004. The baseline survey included 92 529 adults from 14 study areas (the dataset used in the present study was completed after cleaning the collected data on 1 June 2021). The sample size was determined considering the feasibility including budgets and statistical power for the incidence of major cancer types, which was the primary outcome of the J-MICC Study.
Figure 1 shows the flowchart for the selection of participants for the analysis. Participants without a follow-up, those with a self-reported medical history of any cancer, stroke, myocardial infarction and angina pectoris and those who died within a year from the baseline, were excluded. Furthermore, we excluded participants with missing data for the intake of small fish and those who deviated from the sex-specific mean ± 3 sd for total energy intake. Thus, 80 802 individuals (34 555 males and 46 247 females) were finally included in the present study.
Fig. 1.
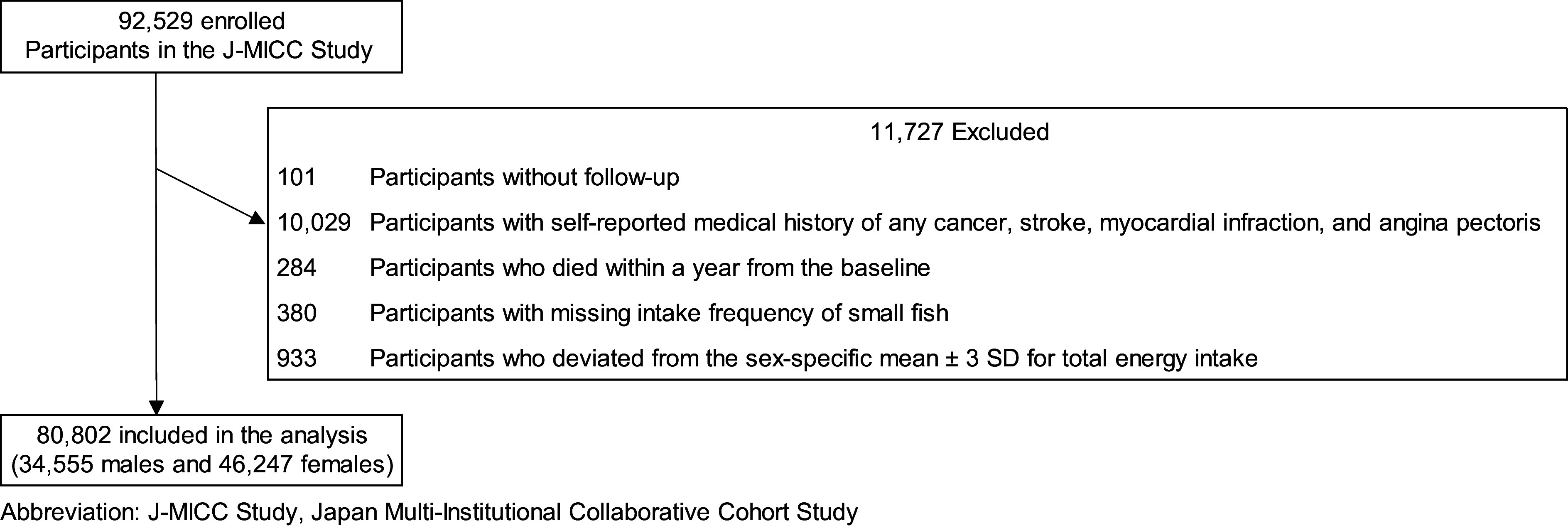
The flow chart for the selection of participants for the present study. (J-MICC Study, Japan Multi-Institutional Collaborative Cohort Study)
Assessment of lifestyle factors and dietary intake
The height and weight of participants were measured directly on the day of the survey in twelve areas and were self-reported by participants in two areas. BMI was calculated as weight in kilograms divided by the square of height in metres (kg/m2). Lifestyle factors, including smoking habit, alcohol consumption, education level, leisure-time physical activity, medical history, age at menarche, number of births and menopausal status were assessed using a self-administered questionnaire at baseline. For smoking habit, participants reported whether they were current smokers, had quit smoking or never smoked. Participants who reported smoking indicated the average number of cigarettes per d, and those who reported quitting indicated how many years (or months) ago they quit. Ethanol intake (g/d) was estimated for current drinkers (defined as those who consumed alcohol at least once a month during the last year) based on the reported consumption frequency and amount consumed each time for six alcoholic beverages (Japanese sake, shochu, shochu-based cocktails, beer, whisky and wine)(22). For education level, participants reported the last school level they graduated from (excluding dropout) from one of the following seven categories: elementary school or junior high school, high school, vocational school, junior college or technical school, college or university, graduate school and others. Participants from three study areas were not asked about their education level and were assigned to an additional category for missing data. Leisure-time physical activity was estimated based on the frequency and duration of leisure-time activities(23). Leisure-time physical activity was calculated as metabolic equivalent hours per d (MET·h/d) by multiplying the assigned daily mean frequency, mean duration (time in hours) and MET value together for each activity: low-intensity physical activity (e.g. walking and golf, assigned 3·4 MET), moderate-intensity physical activity (e.g. jogging and swimming, 7·0 MET) and high-intensity physical activity (e.g. marathon running and martial arts, 10 MET). The frequency (assigned as daily mean frequency) was reported in five categories as follows: none (0), 1–3 times/month (2/30), 1–2 times/week (1·5/7), 3–4 times/week (3·5/7) and ≥ 5 times/week (6/7). The mean duration (assigned as time in hours) was reported in six categories as follows: < 30 min (15/60), 30 min to < 1 h (45/60), 1 to < 2 h (1·5), 2 to < 3 h (2·5), 3 to < 4 h (3·5) and ≥ 4 h (4·0). The questionnaire was based on a similar validated survey used in the Japan Public Health Center-based Prospective Study(24). The patient’s medical history was self-reported, and the past and present history were considered a positive history. Age at menarche, number of births and menopausal status were also self-reported.
The average daily intake of energy, selected foods/food groups (green and yellow vegetables, light-coloured vegetables, fruit, meat and rice) and nutrients (Na, dietary fibre, n-3 HUFA (including EPA, DHA and docosapentaenoic acid), Ca, vitamin D, retinol and carotene) were estimated using a validated short FFQ, including forty-seven foods and beverages, based on the Standard Tables of Food Composition in Japan, the fifth revised edition at baseline(25–28). Retinol intake was estimated as retinol equivalents, and carotene intake was estimated as β-carotene equivalents(28). Only the baseline FFQ results were considered. Nutrient intakes from supplements were not included. The FFQ included seven questions that assessed the intake of fish (raw fish, grilled fish and boiled fish), small fish (Atlantic capelin and dried young sardines (whitebait)), canned tuna, crustacean and molluscs (shrimp, crab, octopus and squid), shellfish (clams and oysters), roe (salted cod roe and salmon roe) and fish-paste products (baked bar (chikuwa) and steamed cake (kamaboko)) with eight possible responses on intake frequency (rarely, 1–3 times/month, 1–2 times/week, 3–4 times/week, 5–6 times/week, 1 time/d, 2 times/d and ≥ 3 times/d). The items listed in parentheses in the FFQ are examples of questions preceding the parentheses. Atlantic capelin and dried young sardines (whitebait) were listed as examples of small fish in the parentheses. We evaluated the validity of the intake of small fish estimated using the FFQ by comparing the estimate with the intake based on 12-d dietary records. Both the intakes were loge-transformed. The Pearson’s correlation coefficients (de-attenuated for intra-individual variation) between the FFQ and dietary records were 0·48 for males and 0·51 for females(27). We adjusted for total energy from the intake of foods and nutrients using the density method(29). We then divided the subjects into sex-specific quartiles according to energy-adjusted intake of each food or nutrient. To validate the consumption of other foods as an adjusted covariate, the Spearman’s correlation coefficients (de-attenuated for intra-individual variation and energy-adjusted) between the FFQ and dietary records were calculated and determined to be 0·34 in males and 0·36 in females for green and yellow vegetables, 0·35 in males and 0·24 in females for light-coloured vegetables, 0·62 in males and 0·58 in females for fruit, 0·41 in males and 0·41 in females for meat and 0·67 in males and 0·61 in females for rice(27).
Regarding the total energy and nutrient intake adjusted as covariates, the Pearson’s correlation coefficients (de-attenuated for intra-individual variation, loge-transformed and energy-adjusted) between the FFQ and dietary records were determined as 0·49 in males and 0·44 in females for total energy, 0·24 in males and 0·35 in females for Na, 0·36 in males and 0·47 in females for dietary fibre, 0·36 in males and 0·35 in females for n-3 HUFA, 0·49 in males and 0·59 in females for Ca, 0·65 in males and 0·40 in females for vitamin D, 0·27 in males and 0·22 in females for retinol and 0·39 in males and 0·38 in females for carotene(26).
We calculated the Japanese diet index (JDI) to examine whether the intake of small fish is associated with mortality risk, independently of the degree of adherence to the Japanese diet. This is because the Japanese diet is reported to be associated with a lower risk of mortality(30,31). The original JDI consists of the following eight components: rice, miso soup, seaweeds, pickles, green and yellow vegetables, fish, green tea and beef and pork. We used only seven factors, excluding pickles, for the JDI because of no information on pickles. Pickles are important Na sources in the Japanese diet, so they are sometimes incorporated in an FFQ to estimate Na intake. In the development of the FFQ used in our study, however, pickles were not included because Na intake was not an original target nutrient. The method to estimate Na intake was devised after FFQ development. Since the FFQ is reasonably valid for small fish intake, it was appropriate for the present study hypothesis. The fish component of the JDI was calculated using the total consumption of fish and shellfish, including small fish. The beef and pork represent non-adherence to the Japanese diet, and participants received one point if their intake (g/d) was less than the sex-specific median for the entire population of this study. The remaining six components represent adherence to the Japanese diet; participants received one point if the intake (g/d) was more than or equal to the sex-specific median for the entire population of this study. The intakes of seven components for participants with missing data for the intake were considered zero. The JDI score ranged from 0 to 7, with higher scores indicating greater conformity to the Japanese diet.
Follow-up and endpoint
We followed eligible participants from the enrolment date (from 11 February 2004 to 31 March 2014) to 31 December 2017 in eleven study areas (Chiba, Aichi Cancer Center, Okazaki, Shizuoka, Takashima, Kyoto, Fukuoka, Saga, Kagoshima, Tokushima and Shizuoka-Sakuragaoka) or to 31 December 2018 in three ones (Kyushu and Okinawa Population Study (KOPS), Iga and Daiko). Information on residence and survival status was obtained from the resident registers annually or biennially. During the follow-up period, 4400 participants (5·4 %) were moved out of the study areas, and 165 participants (0·2 %) were unable to follow up because of other reasons. They were censored at the last date when they were known to reside in the study areas. The causes of death were identified based on the abstracts of death certificates provided by the Japanese Ministry of Health, Labour and Welfare and were coded according to the International Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10). The primary outcome of this study was death of all causes, and the secondary outcomes were death of cancer (ICD-10: C00–C97), CVD including heart disease and cerebrovascular disease (ICD-10: I00–I99) and other causes (non-cancer, non-CVD).
Statistical analysis
Participants were classified into four groups according to the frequency of the intake of small fish by sex, as follows: rarely, 1–3 times/month, 1–2 times/week and ≥ 3 times/week. Differences in the means of age and leisure-time physical activity between the frequency categories were tested using one-way ANOVA. Differences in the median of energy-adjusted intakes of small fish and non-small fish (raw fish, grilled fish and boiled fish; do not include other seafood items) between the frequency categories were analysed using the Kruskal-Wallis test. Differences in the proportions of categorical variables between the frequency groups were tested using the χ2 test. Because a considerable proportion of participants (40·8 %) filled out the FFQ and questionnaire for lifestyle factors only at baseline, only baseline responses to the FFQ and questionnaire were considered, as these were provided by all the participants.
The sex-specific hazard ratio (HR) and corresponding 95 % confidence interval (CI) for all-cause, cancer, CVD and other-cause mortality according to the frequency of the intake of small fish were estimated using the Cox proportional hazards model with adjustments for potential confounding factors. The end of follow-up was defined as the date of death, the date of moving out of the study area or the end of follow-up, whichever occurred first. The lowest category of the intake of small fish (rarely) was considered the reference group. The categories were determined so that each category has enough number of participants. The linear trends for the risk were evaluated using an ordinal number assigned to the frequency categories (rarely: 1; 1–3 times/month: 2; 1–2 times/week: 3; and ≥ 3 times/week: 4).
Four multivariable models were established as follows: Model 1: adjusted for age at baseline (as a continuous variable) and study areas (Chiba, Aichi Cancer Center, Okazaki, Shizuoka, Iga, Daiko, Takashima, Kyoto, Fukuoka, Saga, Kagoshima, Tokushima, Kyushu and Okinawa Population Study (KOPS), Shizuoka-Sakuragaoka). Model 2: adjusted for covariates in Model 1 plus BMI (< 18·5, 18·5 to < 25, ≥ 25 kg/m2), smoking habit (for males: never, former (quit smoking ≥ 10, 5 to < 10, < 5 years ago), current (< 20, 20–< 40, ≥ 40 cigarettes/d); for females: never, former (quit smoking ≥ 10, < 10 years ago), current (< 20, ≥ 20 cigarettes/d)), alcohol consumption (for males: never, former, current (< 23, 23 to < 46, ≥ 46 g/d ethanol); for females: never, former, current (< 23, ≥ 23 g/d ethanol); 23 g/d ethanol is equivalent to 180 mL of Japanese sake), education level (junior high school or under (≤ 9 years), high school (10–12 years), junior college or vocational school (13–15 years) and college, university or above (≥ 16 years)), leisure-time physical activity (MET·h/d; as a continuous variable) and self-reported medical history of hypertension, diabetes and dyslipidaemia (yes or no) for males; for females, the same covariates were used as in males, plus age at menarche (≤ 12, 13, 14, ≥ 15 years), number of births (none, 1, 2, 3, ≥ 4) and menopausal status (pre-menopausal, menopausal (age at menopause < 47, 47 to < 50, 50 to < 53, ≥ 53 years old)). Model 3: adjusted for covariates in Model 2 plus total energy intake (by quartile) and energy-adjusted intakes of green and yellow vegetables, light-coloured vegetables, fruit, meat, rice, Na and dietary fibre (by quartile) and JDI score (points of 0–1, 2, 3, 4, 5, 6–7). For Model 4, we additionally adjusted for intakes of nutrients abundant in small fish, including n-3 HUFA, Ca, vitamin D, retinol and carotene (by quartile) which might mediate the association between small fish and mortality. We did not conduct a formal mediation analysis. We consider Model 3 to represent the main result in the present study. We confirmed the proportional hazards assumption in Model 3 by including each frequency category for the intake of small fish (1–3 times/month, 1–2 times/week and ≥ 3 times/week) × time (continuous) interaction terms. The assumption was not violated (P > 0·05) except for the interaction term for the small fish ≥ 3 times/week group × time in the analysis of male cancer mortality (P = 0·04). We also assessed the interaction between sex and intake of small fish on the mortality risk with Model 3 including the cross-product term (i.e. sex (dichotomous) × category of small fish consumed (continuous)), representing the interaction. The adjustment variables in Model 3 were different between sexes. Thus, in this analysis, we excluded the female-specific variables (age at menarche, number of births and menopausal status) and adjusted for smoking habit and alcohol consumption to the same category used in females (smoking habit: never, former (quit smoking ≥ 10, < 10 years ago), current (< 20, ≥ 20 cigarettes/d)); alcohol consumption: never, former, current (< 23, ≥ 23 g/d ethanol)). The total energy intake and the intakes of food groups and nutrients were adjusted for sex-specific quartiles. The JDI was calculated with the sex-specific median for the entire population of this study.
We analysed 80 250 participants (34 169 males and 46 081 females), additionally excluding 552 participants who died 1–3 years after baseline measurements, using the same covariates as in Model 3. The participants who died within 1 year had been already excluded (Fig. 1). This analysis was added to consider the influence of diseases that might have existed at baseline over a longer period than that considered in Model 3 (3 years v. 1 year). We further analysed 75 121 participants (32 316 males and 42 805 females), excluding 5681 participants from the Aichi Cancer Center using the same covariates as in Model 3 because they might have included undiagnosed cancer patients at baseline. Additionally, we performed stratified analyses by age (≥ 60, < 60 years old), smoking status (never, (former or current)) and JDI score (≤ 3, ≥ 4 points), with adjustment for the same covariates as in Model 3. Effects of interactions between stratification variables and intake of small fish on the mortality risk were assessed with Model 3 including the cross-product term (i.e. stratification factors (dichotomous) × category of small fish consumed (continuous)), representing the interaction. Lastly, we considered the intake of non-small fish (raw fish, grilled fish and boiled fish; do not include other seafood items) for the association of the intake of small fish with all-cause, cancer, CVD and other-cause mortality using the same covariates as in Model 3 by further adjustment for the frequency of the intake of non-small fish (≤ 2 times/week, 3–4 times/week, 5–6 times/week and ≥ 1 time/d), excluding 115 participants (34 males and 81 females) with missing data for the intake of non-small fish.
Participants with missing data for covariates were included as additional categories in the analysis. A two-tailed P value < 0·05 was considered statistically significant. All statistical analyses were conducted using the SPSS software, version 28 (IBM) and Stata/SE17 (StataCorp).
Results
Characteristics of participants
Tables 1 and 2 present the baseline characteristics according to the frequency of the intake of small fish in males and females, respectively. The mean age (sd) of 80 802 eligible participants (34 555 males and 46 247 females) was 54·7 (9·4) years. Those with frequent intake of small fish were more likely to be aged, non-lean, non-smoker (never or former smoker), current drinker (in males), physically active and having hypertension and menopausal (in females). The distribution of education level and study area differed statistically significantly according to the frequency of the intake of small fish. The intake of small fish was positively correlated with the intake of all nutrients and foods (except for rice in males), total energy and the JDI score.
Table 1.
Baseline characteristics in males according to the frequency of the intake of small fish*
| Rarely | 1–3 times/month | 1–2 times/week | ≥ 3 times/week | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | P value | |
| Participants, n | 5046 | 14 579 | 9890 | 5040 | 34 555 | ||||||
| Age, years | |||||||||||
| Mean | 52·8 | 53·9 | 56·5 | 59·4 | 55·3 | < 0·001 | |||||
| sd | 9·6 | 9·4 | 8·9 | 8·2 | 9·4 | ||||||
| Study area | |||||||||||
| Kanto (Chiba) | 373 | 7·4 | 1227 | 8·4 | 683 | 6·9 | 292 | 5·8 | 2575 | 7·5 | < 0·001 |
| Chubu (Aichi Cancer Center, Okazaki, Shizuoka, Iga, Daiko, Shizuoka-Sakuragaoka) | 1573 | 31·2 | 5553 | 38·1 | 4050 | 41·0 | 1886 | 37·4 | 13 062 | 37·8 | |
| Kinki (Takashima, Kyoto) | 485 | 9·6 | 1389 | 9·5 | 973 | 9·8 | 540 | 10·7 | 3387 | 9·8 | |
| Shikoku (Tokushima) | 215 | 4·3 | 596 | 4·1 | 347 | 3·5 | 144 | 2·9 | 1302 | 3·8 | |
| Kyushu and Okinawa (Fukuoka, Saga, Kagoshima, KOPS) | 2400 | 47·6 | 5814 | 39·9 | 3837 | 38·8 | 2178 | 43·2 | 14 229 | 41·2 | |
| BMI, kg/m2 | |||||||||||
| 18·5–24·9 | 3238 | 64·2 | 9803 | 67·2 | 6730 | 68·0 | 3394 | 67·3 | 23 165 | 67·0 | < 0·001 |
| < 18·5 | 168 | 3·3 | 377 | 2·6 | 241 | 2·4 | 104 | 2·1 | 890 | 2·6 | |
| ≥ 25·0 | 1636 | 32·4 | 4390 | 30·1 | 2916 | 29·5 | 1538 | 30·5 | 10 480 | 30·3 | |
| Unknown | 4 | 0·1 | 9 | 0·1 | 3 | 0·0 | 4 | 0·1 | 20 | 0·1 | |
| Smoking habit | |||||||||||
| Never | 1522 | 30·2 | 4188 | 28·7 | 2883 | 29·2 | 1562 | 31·0 | 10 155 | 29·4 | < 0·001 |
| Former, quit ≥ 10·0 years before | 916 | 18·2 | 3126 | 21·4 | 2375 | 24·0 | 1302 | 25·8 | 7719 | 22·3 | |
| Former, quit 5·0–9·9 years before | 256 | 5·1 | 941 | 6·5 | 615 | 6·2 | 321 | 6·4 | 2133 | 6·2 | |
| Former, quit < 5·0 years before | 458 | 9·1 | 1373 | 9·4 | 884 | 8·9 | 434 | 8·6 | 3149 | 9·1 | |
| Current, < 20 cigarettes/d | 511 | 10·1 | 1420 | 9·7 | 933 | 9·4 | 421 | 8·4 | 3285 | 9·5 | |
| Current, 20–39 cigarettes/d | 1051 | 20·8 | 2751 | 18·9 | 1723 | 17·4 | 739 | 14·7 | 6264 | 18·1 | |
| Current, ≥ 40 cigarettes/d | 205 | 4·1 | 424 | 2·9 | 222 | 2·2 | 121 | 2·4 | 972 | 2·8 | |
| Unknown | 127 | 2·5 | 356 | 2·4 | 255 | 2·6 | 140 | 2·8 | 878 | 2·5 | |
| Alcohol consumption | |||||||||||
| Never | 1378 | 27·3 | 2948 | 20·2 | 1822 | 18·4 | 838 | 16·6 | 6986 | 20·2 | < 0·001 |
| Former | 209 | 4·1 | 397 | 2·7 | 256 | 2·6 | 183 | 3·6 | 1045 | 3·0 | |
| Current, < 23·0 g/d ethanol | 1678 | 33·3 | 5420 | 37·2 | 3560 | 36·0 | 1692 | 33·6 | 12 350 | 35·7 | |
| Current, 23·0–45·9 g/d ethanol | 865 | 17·1 | 2977 | 20·4 | 2122 | 21·5 | 1165 | 23·1 | 7129 | 20·6 | |
| Current, ≥ 46·0 g/d ethanol | 910 | 18·0 | 2821 | 19·3 | 2120 | 21·4 | 1157 | 23·0 | 7008 | 20·3 | |
| Unknown | 6 | 0·1 | 16 | 0·1 | 10 | 0·1 | 5 | 0·1 | 37 | 0·1 | |
| Education level | |||||||||||
| Junior high school (≤ 9 years) | 380 | 7·5 | 869 | 6·0 | 767 | 7·8 | 575 | 11·4 | 2591 | 7·5 | < 0·001 |
| High school (10–12 years) | 1550 | 30·7 | 4372 | 30·0 | 2932 | 29·6 | 1425 | 28·3 | 10 279 | 29·7 | |
| Junior college or vocational school (13–15 years) | 478 | 9·5 | 1338 | 9·2 | 813 | 8·2 | 390 | 7·7 | 3019 | 8·7 | |
| College, university or above (≥ 16 years) | 1447 | 28·7 | 5087 | 34·9 | 3213 | 32·5 | 1304 | 25·9 | 11 051 | 32·0 | |
| No question in the questionnaire | 1176 | 23·3 | 2848 | 19·5 | 2127 | 21·5 | 1319 | 26·2 | 7470 | 21·6 | |
| Others or unknown | 15 | 0·3 | 65 | 0·4 | 38 | 0·4 | 27 | 0·5 | 145 | 0·4 | |
| Leisure-time physical activity | |||||||||||
| MET·h/d | |||||||||||
| Mean | 1·6 | 2·0 | 2·4 | 2·7 | 2·1 | < 0·001 | |||||
| sd | 2·9 | 3·1 | 3·6 | 3·8 | 3·4 | ||||||
| Hypertension | |||||||||||
| No | 4034 | 79·9 | 11 522 | 79·0 | 7565 | 76·5 | 3698 | 73·4 | 26 819 | 77·6 | < 0·001 |
| Yes | 998 | 19·8 | 3024 | 20·7 | 2304 | 23·3 | 1334 | 26·5 | 7660 | 22·2 | |
| Unknown | 14 | 0·3 | 33 | 0·2 | 21 | 0·2 | 8 | 0·2 | 76 | 0·2 | |
| Diabetes | |||||||||||
| No | 4633 | 91·8 | 13 484 | 92·5 | 9000 | 91·0 | 4523 | 89·7 | 31 640 | 91·6 | < 0·001 |
| Yes | 401 | 7·9 | 1069 | 7·3 | 875 | 8·8 | 506 | 10·0 | 2851 | 8·3 | |
| Unknown | 12 | 0·2 | 26 | 0·2 | 15 | 0·2 | 11 | 0·2 | 64 | 0·2 | |
| Dyslipidaemia | |||||||||||
| No | 4278 | 84·8 | 12 371 | 84·9 | 8321 | 84·1 | 4309 | 85·5 | 29 279 | 84·7 | 0·452 |
| Yes | 752 | 14·9 | 2154 | 14·8 | 1535 | 15·5 | 713 | 14·1 | 5154 | 14·9 | |
| Unknown | 16 | 0·3 | 54 | 0·4 | 34 | 0·3 | 18 | 0·4 | 122 | 0·4 | |
| Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | ||
| Small fish intake†, g/1000 kcal/d | 0·0 | 0–0 | 1·1 | 1·0–1·2 | 2·1 | 1·9–2·3 | 5·7 | 4·9–8·4 | 1·3 | 1·0–2·2 | < 0·001 |
| Non-small fish intake†,‡, g/1000 kcal/d | 8·1 | 5·5–17·9 | 8·9 | 7·1–19·0 | 16·3 | 7·7–20·5 | 19·7 | 15·7–29·0 | 13·8 | 7·3–20·3 | < 0·001 |
| Energy intake, kcal/d | 1813·7 | 1613·7–2021·3 | 1849·8 | 1673·7–2050·4 | 1911·2 | 1741·7–2103·7 | 1961·6 | 1787·4–2164·8 | 1880·6 | 1697·4–2081·4 | < 0·001 |
| Rice intake†, g/1000 kcal/d | 229·6 | 180·1–278·5 | 228·3 | 182·7–274·4 | 234·2 | 188·3–278·3 | 238·3 | 191·5–278·7 | 231·3 | 185·3–276·9 | < 0·001 |
| Meat intake†, g/1000 kcal/d | 15·9 | 10·9–24·1 | 16·2 | 11·9–24·3 | 16·7 | 12·8–24·8 | 17·6 | 12·4–27·2 | 16·5 | 12·1–24·8 | < 0·001 |
| Fruits intake†, g/1000 kcal/d | 10·3 | 4·8–20·7 | 13·7 | 8·8–27·8 | 17·5 | 10·1–36·3 | 25·1 | 12·3–47·2 | 15·4 | 9·0–33·0 | < 0·001 |
| Green and yellow vegetables intake†, g/1000 kcal/d | 18·3 | 11·4–30·3 | 21·9 | 15·0–34·3 | 27·5 | 18·6–41·1 | 35·6 | 22·1–53·1 | 24·4 | 16·0–38·7 | < 0·001 |
| Light-coloured vegetables intake†, g/1000 kcal/d | 20·4 | 12·6–32·3 | 22·8 | 14·6–33·8 | 27·2 | 17·5–38·8 | 34·7 | 23·4–48·0 | 25·2 | 15·7–37·4 | < 0·001 |
| Na intake, mg/1000 kcal/d | 862·4 | 705·7–1060·3 | 893·6 | 749·3–1073·1 | 922·5 | 777·6–1109·3 | 1024·3 | 865·1–1235·8 | 916·4 | 765·3–1105·8 | < 0·001 |
| Dietary fibre intake, g/1000 kcal/d | 4·7 | 3·9–5·6 | 4·9 | 4·2–5·8 | 5·2 | 4·4–6·2 | 5·9 | 4·8–7·0 | 5·1 | 4·3–6·1 | < 0·001 |
| Ca intake, mg/1000 kcal/d | 226·3 | 185·7–276·6 | 236·6 | 197·9–287·3 | 249·1 | 208·0–302·6 | 284·2 | 235·2–344·1 | 245·2 | 202·8–299·7 | < 0·001 |
| Vitamin D intake, μg/1000 kcal/d | 2·6 | 2·0–3·7 | 3·0 | 2·5–4·2 | 3·9 | 2·9–4·8 | 5·6 | 4·6–7·0 | 3·6 | 2·6–4·8 | < 0·001 |
| n-3 HUFA intake, mg/1000 kcal/d | 269·7 | 216·3–400·0 | 309·6 | 250·2–438·2 | 394·4 | 283·9–486·9 | 516·2 | 421·7–655·8 | 361·8 | 262·4–484·6 | < 0·001 |
| Retinol intake, μg/1000 kcal/d | 343·8 | 276·2–489·0 | 428·4 | 308·4–585·9 | 491·1 | 342·3–638·9 | 537·2 | 380·4–703·3 | 447·0 | 315·6–608·5 | < 0·001 |
| Carotene intake, μg/1000 kcal/d | 1199·7 | 962·6–1574·6 | 1267·3 | 1036·9–1642·7 | 1406·8 | 1116·3–1825·9 | 1624·3 | 1218·8–2127·9 | 1336·3 | 1061·0–1764·9 | < 0·001 |
| JDI score, points | |||||||||||
| 0–1 | 1245 | 24·7 | 2222 | 15·2 | 603 | 6·1 | 68 | 1·3 | 4138 | 12·0 | < 0·001 |
| 2 | 1157 | 22·9 | 2787 | 19·1 | 1054 | 10·7 | 252 | 5·0 | 5250 | 15·2 | |
| 3 | 1054 | 20·9 | 3316 | 22·7 | 1853 | 18·7 | 586 | 11·6 | 6809 | 19·7 | |
| 4 | 872 | 17·3 | 3079 | 21·1 | 2448 | 24·8 | 1086 | 21·5 | 7485 | 21·7 | |
| 5 | 507 | 10·0 | 2141 | 14·7 | 2428 | 24·6 | 1542 | 30·6 | 6618 | 19·2 | |
| 6–7 | 211 | 4·2 | 1034 | 7·1 | 1504 | 15·2 | 1506 | 29·9 | 4255 | 12·3 | |
IQR, interquartile range; JDI, Japanese diet index; KOPS, Kyushu and Okinawa Population Study; MET, metabolic equivalent.
Values are numbers (percentages) unless indicated otherwise.
Food consumption of the total population including non-consumers was used.
Excluded thirty-four males with missing data for the intake of non-small fish.
Table 2.
Baseline characteristics in females according to the frequency of the intake of small fish*
| Rarely | 1–3 times/month | 1–2 times/week | ≥ 3 times/week | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | P value | |
| Participants, n | 5599 | 17 562 | 13 746 | 9340 | 46 247 | ||||||
| Age, years | |||||||||||
| Mean | 51·0 | 52·2 | 55·2 | 58·7 | 54·3 | < 0·001 | |||||
| sd | 9·6 | 9·2 | 9·1 | 8·2 | 9·4 | ||||||
| Study area | |||||||||||
| Kanto (Chiba) | 537 | 9·6 | 1962 | 11·2 | 1422 | 10·3 | 822 | 8·8 | 4743 | 10·3 | < 0·001 |
| Chubu (Aichi Cancer Center, Okazaki, Shizuoka, Iga, Daiko, Shizuoka-Sakuragaoka) | 1572 | 28·1 | 5563 | 31·7 | 4397 | 32·0 | 2516 | 26·9 | 14 048 | 30·4 | |
| Kinki (Takashima, Kyoto) | 520 | 9·3 | 1957 | 11·1 | 1707 | 12·4 | 1190 | 12·7 | 5374 | 11·6 | |
| Shikoku (Tokushima) | 174 | 3·1 | 362 | 2·1 | 260 | 1·9 | 134 | 1·4 | 930 | 2·0 | |
| Kyushu and Okinawa (Fukuoka, Saga, Kagoshima, KOPS) | 2796 | 49·9 | 7718 | 43·9 | 5960 | 43·4 | 4678 | 50·1 | 21 152 | 45·7 | |
| BMI, kg/m2 | |||||||||||
| 18·5–24·9 | 3930 | 70·2 | 12 810 | 72·9 | 10 089 | 73·4 | 6651 | 71·2 | 33 480 | 72·4 | < 0·001 |
| < 18·5 | 587 | 10·5 | 1649 | 9·4 | 1234 | 9·0 | 787 | 8·4 | 4257 | 9·2 | |
| ≥ 25·0 | 1070 | 19·1 | 3078 | 17·5 | 2400 | 17·5 | 1893 | 20·3 | 8441 | 18·3 | |
| Unknown | 12 | 0·2 | 25 | 0·1 | 23 | 0·2 | 9 | 0·1 | 69 | 0·1 | |
| Smoking habit | |||||||||||
| Never | 4397 | 78·5 | 14 577 | 83·0 | 11 978 | 87·1 | 8414 | 90·1 | 39 366 | 85·1 | < 0·001 |
| Former, quit ≥ 10·0 years before | 206 | 3·7 | 652 | 3·7 | 423 | 3·1 | 235 | 2·5 | 1516 | 3·3 | |
| Former, quit < 10·0 years before | 273 | 4·9 | 696 | 4·0 | 413 | 3·0 | 204 | 2·2 | 1586 | 3·4 | |
| Current, < 20 cigarettes/d | 395 | 7·1 | 976 | 5·6 | 523 | 3·8 | 258 | 2·8 | 2152 | 4·7 | |
| Current, ≥ 20 cigarettes/d | 253 | 4·5 | 468 | 2·7 | 265 | 1·9 | 144 | 1·5 | 1130 | 2·4 | |
| Unknown | 75 | 1·3 | 193 | 1·1 | 144 | 1·0 | 85 | 0·9 | 497 | 1·1 | |
| Alcohol consumption | |||||||||||
| Never | 3423 | 61·1 | 10 118 | 57·6 | 8359 | 60·8 | 6107 | 65·4 | 28 007 | 60·6 | < 0·001 |
| Former | 142 | 2·5 | 328 | 1·9 | 206 | 1·5 | 158 | 1·7 | 834 | 1·8 | |
| Current, < 23·0 g/d ethanol | 1666 | 29·8 | 6040 | 34·4 | 4488 | 32·6 | 2611 | 28·0 | 14 805 | 32·0 | |
| Current, ≥ 23·0 g/d ethanol | 356 | 6·4 | 1057 | 6·0 | 672 | 4·9 | 450 | 4·8 | 2535 | 5·5 | |
| Unknown | 12 | 0·2 | 19 | 0·1 | 21 | 0·2 | 14 | 0·1 | 66 | 0·1 | |
| Education level | |||||||||||
| Junior high school (≤ 9 years) | 331 | 5·9 | 911 | 5·2 | 878 | 6·4 | 888 | 9·5 | 3008 | 6·5 | < 0·001 |
| High school (10–12 years) | 1776 | 31·7 | 5809 | 33·1 | 4571 | 33·3 | 3002 | 32·1 | 15 158 | 32·8 | |
| Junior college or vocational school (13–15 years) | 1373 | 24·5 | 4999 | 28·5 | 3440 | 25·0 | 1978 | 21·2 | 11 790 | 25·5 | |
| College, university or above (≥ 16 years) | 535 | 9·6 | 1993 | 11·3 | 1461 | 10·6 | 738 | 7·9 | 4727 | 10·2 | |
| No question in the questionnaire | 1564 | 27·9 | 3792 | 21·6 | 3337 | 24·3 | 2687 | 28·8 | 11 380 | 24·6 | |
| Others or unknown | 20 | 0·4 | 58 | 0·3 | 59 | 0·4 | 47 | 0·5 | 184 | 0·4 | |
| Leisure-time physical activity | |||||||||||
| MET·h/d | |||||||||||
| Mean | 1·3 | 1·6 | 2·0 | 2·4 | 1·9 | < 0·001 | |||||
| sd | 2·5 | 2·7 | 3·0 | 3·4 | 2·9 | ||||||
| Hypertension | |||||||||||
| No | 4928 | 88·0 | 15 302 | 87·1 | 11 527 | 83·9 | 7604 | 81·4 | 39 361 | 85·1 | < 0·001 |
| Yes | 657 | 11·7 | 2219 | 12·6 | 2197 | 16·0 | 1711 | 18·3 | 6784 | 14·7 | |
| Unknown | 14 | 0·3 | 41 | 0·2 | 22 | 0·2 | 25 | 0·3 | 102 | 0·2 | |
| Diabetes | |||||||||||
| No | 5418 | 96·8 | 17 057 | 97·1 | 13 304 | 96·8 | 8952 | 95·8 | 44 731 | 96·7 | < 0·001 |
| Yes | 166 | 3·0 | 476 | 2·7 | 424 | 3·1 | 366 | 3·9 | 1432 | 3·1 | |
| Unknown | 15 | 0·3 | 29 | 0·2 | 18 | 0·1 | 22 | 0·2 | 84 | 0·2 | |
| Dyslipidaemia | |||||||||||
| No | 4881 | 87·2 | 15 178 | 86·4 | 11 590 | 84·3 | 7723 | 82·7 | 39 372 | 85·1 | < 0·001 |
| Yes | 698 | 12·5 | 2332 | 13·3 | 2107 | 15·3 | 1580 | 16·9 | 6717 | 14·5 | |
| Unknown | 20 | 0·4 | 52 | 0·3 | 49 | 0·4 | 37 | 0·4 | 158 | 0·3 | |
| Age at menarche, years | |||||||||||
| ≤ 12 | 1977 | 35·3 | 6432 | 36·6 | 4221 | 30·7 | 2345 | 25·1 | 14 975 | 32·4 | < 0·001 |
| 13 | 1368 | 24·4 | 4450 | 25·3 | 3478 | 25·3 | 2278 | 24·4 | 11 574 | 25·0 | |
| 14 | 1259 | 22·5 | 4015 | 22·9 | 3464 | 25·2 | 2467 | 26·4 | 11 205 | 24·2 | |
| ≥ 15 | 940 | 16·8 | 2579 | 14·7 | 2501 | 18·2 | 2202 | 23·6 | 8222 | 17·8 | |
| Unknown | 55 | 1·0 | 86 | 0·5 | 82 | 0·6 | 48 | 0·5 | 271 | 0·6 | |
| Number of births | |||||||||||
| None | 697 | 12·4 | 1528 | 8·7 | 864 | 6·3 | 594 | 6·4 | 3683 | 8·0 | < 0·001 |
| 1 | 653 | 11·7 | 2030 | 11·6 | 1423 | 10·4 | 879 | 9·4 | 4985 | 10·8 | |
| 2 | 2091 | 37·3 | 7669 | 43·7 | 6258 | 45·5 | 4200 | 45·0 | 20 218 | 43·7 | |
| 3 | 1193 | 21·3 | 4282 | 24·4 | 3677 | 26·7 | 2596 | 27·8 | 11 748 | 25·4 | |
| ≥ 4 | 473 | 8·4 | 1084 | 6·2 | 944 | 6·9 | 739 | 7·9 | 3240 | 7·0 | |
| Unknown | 492 | 8·8 | 969 | 5·5 | 580 | 4·2 | 332 | 3·6 | 2373 | 5·1 | |
| Menopausal status | |||||||||||
| Pre-menopausal | 2823 | 50·4 | 8104 | 46·1 | 4447 | 32·4 | 1740 | 18·6 | 17 114 | 37·0 | < 0·001 |
| Menopause at < 47 years old | 592 | 10·6 | 1689 | 9·6 | 1524 | 11·1 | 1203 | 12·9 | 5008 | 10·8 | |
| Menopause at 47–< 50 years old | 516 | 9·2 | 1639 | 9·3 | 1525 | 11·1 | 1204 | 12·9 | 4884 | 10·6 | |
| Menopause at 50–< 53 years old | 1012 | 18·1 | 3732 | 21·3 | 3753 | 27·3 | 3031 | 32·5 | 11 528 | 24·9 | |
| Menopause at ≥ 53 years old | 593 | 10·6 | 2242 | 12·8 | 2352 | 17·1 | 2045 | 21·9 | 7232 | 15·6 | |
| Unknown | 63 | 1·1 | 156 | 0·9 | 145 | 1·1 | 117 | 1·3 | 481 | 1·0 | |
| Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | ||
| Small fish intake†, g/1000 kcal/d | 0·0 | 0–0 | 1·0 | 0·9–1·1 | 1·9 | 1·8–2·1 | 5·6 | 4·7–8·4 | 1·5 | 0·9–2·2 | < 0·001 |
| Non-small fish intake†,‡, g/1000 kcal/d | 8·6 | 6·7–19·2 | 10·9 | 7·8–20·4 | 18·3 | 8·5–22·5 | 20·4 | 17·0–30·7 | 17·7 | 8·1–22·4 | < 0·001 |
| Energy intake, kcal/d | 1478·4 | 1322·2–1613·0 | 1512·3 | 1375·0–1636·4 | 1549·3 | 1416·8–1673·2 | 1591·1 | 1457·6–1718·7 | 1535·0 | 1394·7–1664·8 | < 0·001 |
| Rice intake†, g/1000 kcal/d | 176·1 | 128·5–217·8 | 177·1 | 134·8–218·3 | 182·1 | 141·3–224·9 | 192·1 | 150·1–235·1 | 181·6 | 138·8–224·1 | < 0·001 |
| Meat intake†, g/1000 kcal/d | 22·1 | 15·2–32·7 | 23·0 | 16·5–33·1 | 23·8 | 16·8–34·1 | 24·2 | 16·0–35·5 | 23·3 | 16·4–33·9 | < 0·001 |
| Fruits intake†, g/1000 kcal/d | 20·3 | 10·9–49·1 | 25·5 | 14·0–56·1 | 39·2 | 20·1–66·5 | 53·0 | 23·4–82·8 | 35·1 | 16·5–63·9 | < 0·001 |
| Green and yellow vegetables intake†, g/1000 kcal/d | 33·4 | 21·7–52·3 | 38·6 | 25·9–56·6 | 47·6 | 32·7–67·7 | 59·3 | 41·3–82·2 | 44·5 | 29·0–65·5 | < 0·001 |
| Light-coloured vegetables intake†, g/1000 kcal/d | 37·6 | 24·6–53·1 | 41·1 | 28·5–56·2 | 46·8 | 33·8–62·8 | 55·7 | 41·1–73·7 | 45·2 | 31·3–61·7 | < 0·001 |
| Na intake, mg/1000 kcal/d | 1029·2 | 866·8–1213·5 | 1068·5 | 919·2–1243·1 | 1105·5 | 961·6–1280·6 | 1205·6 | 1042·2–1408·8 | 1102·5 | 946·7–1287·0 | < 0·001 |
| Dietary fibre intake, g/1000 kcal/d | 6·5 | 5·6–7·7 | 6·8 | 5·9–8·0 | 7·4 | 6·4–8·7 | 8·3 | 7·0–9·7 | 7·2 | 6·1–8·5 | < 0·001 |
| Ca intake, mg/1000 kcal/d | 312·2 | 254·5–378·8 | 326·0 | 271·8–389·6 | 342·9 | 290·6–406·7 | 381·6 | 323·5–452·1 | 340·7 | 283·9–407·7 | < 0·001 |
| Vitamin D intake, μg/1000 kcal/d | 3·0 | 2·5–4·3 | 3·8 | 3·0–4·8 | 4·6 | 3·5–5·5 | 6·2 | 5·2–7·6 | 4·5 | 3·2–5·7 | < 0·001 |
| n-3 HUFA intake, mg/1000 kcal/d | 313·5 | 258·1–453·7 | 386·3 | 294·8–495·4 | 460·3 | 338·5–555·1 | 563·7 | 470·4–712·7 | 446·2 | 313·4–559·3 | < 0·001 |
| Retinol intake, μg/1000 kcal/d | 484·6 | 380·1–660·4 | 560·2 | 421·3–761·0 | 640·1 | 469·5–834·9 | 710·4 | 525·1–922·6 | 602·3 | 444·0–808·8 | < 0·001 |
| Carotene intake, μg/1000 kcal/d | 1829·0 | 1419·8–2421·8 | 1952·6 | 1531·6–2492·0 | 2180·5 | 1714·6–2766·8 | 2510·6 | 1965·1–3166·5 | 2114·9 | 1628·8–2720·8 | < 0·001 |
| JDI score, points | |||||||||||
| 0–1 | 1368 | 24·4 | 2431 | 13·8 | 669 | 4·9 | 116 | 1·2 | 4584 | 9·9 | < 0·001 |
| 2 | 1219 | 21·8 | 3264 | 18·6 | 1521 | 11·1 | 343 | 3·7 | 6347 | 13·7 | |
| 3 | 1233 | 22·0 | 4185 | 23·8 | 2655 | 19·3 | 963 | 10·3 | 9036 | 19·5 | |
| 4 | 958 | 17·1 | 3927 | 22·4 | 3624 | 26·4 | 2013 | 21·6 | 10 522 | 22·8 | |
| 5 | 576 | 10·3 | 2624 | 14·9 | 3323 | 24·2 | 3021 | 32·3 | 9544 | 20·6 | |
| 6–7 | 245 | 4·4 | 1131 | 6·4 | 1954 | 14·2 | 2884 | 30·9 | 6214 | 13·4 | |
IQR, interquartile range; JDI, Japanese diet index; KOPS, Kyushu and Okinawa Population Study; MET, metabolic equivalent.
Values are numbers (percentages) unless indicated otherwise.
Food consumption of the total population including non-consumers was used.
Excluded eighty-one females with missing data for the intake of non-small fish.
All-cause mortality
During the 724 115 person-year follow-up (mean, 9·0 years), we identified 2482 deaths (1618 in males and 864 in females), including 1495 cancer-related deaths (988 in males and 507 in females), 340 CVD deaths (204 in males and 136 in females) and 647 other-cause deaths (426 in males and 221 in females). In males, the top five sites for all cancer-related deaths were the lung (25·1 %), pancreas (12·2 %), stomach (10·9 %), esophagus (9·3 %) and colorectum (9·2 %). In females, the top five sites were the lung (16·6 %), pancreas (12·2 %), colorectum (11·8 %), breast (8·7 %) and stomach (7·1 %).
The association between the frequency of the intake of small fish and the risk of all-cause mortality by sex is shown in Table 3. In Models 1 and 2, with adjustment for multiple covariates, the intake of small fish was inversely associated with the risk of all-cause mortality in both sexes. In Model 3, with further adjustment for energy-adjusted intake of foods and nutrients and JDI score, the inverse association remained statistically significant in females, but not in males. The multivariable-adjusted HR (95 % CI) in females were 0·68 (0·55, 0·85) for intakes 1–3 times/month, 0·72 (0·57, 0·90) for 1–2 times/week and 0·69 (0·54, 0·88) for ≥ 3 times/week, compared with the rare intake (P for trend = 0·041). The corresponding HR (95 % CI) in males were 0·81 (0·69, 0·94), 0·84 (0·71, 0·99) and 0·87 (0·73, 1·05), respectively (P for trend = 0·391). In Model 4, with an additional adjustment for the energy-adjusted intake of nutrients abundant in small fish, the inverse association between the intake of small fish and all-cause mortality was observed in females although the HR for intake ≥ 3 times/week was higher than that in Model 3. No statistically significant association was observed in males in Model 4.
Table 3.
Multivariable-adjusted HR (95 % CI) for all-cause, cancer, CVD and other-cause mortality by sex according to the frequency of the intake of small fish
| Male | Female | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1–3 times/month | 1–2 times/week | ≥ 3 times/week | 1–3 times/month | 1–2 times /week | ≥ 3 times/week | P for interaction between sex and intake|| | |||||||||||
| Rarely | HR | 95 % CI | HR | 95 % CI | HR | 95 % CI | P for trend | Rarely | HR | 95 % CI | HR | 95 % CI | HR | 95 % CI | P for trend | ||
| Participants, n | 5046 | 14 579 | 9890 | 5040 | 5599 | 17 562 | 13 746 | 9340 | |||||||||
| Person-years | 43 476 | 127 245 | 87 526 | 45 597 | 50 112 | 157 300 | 125 102 | 87 757 | |||||||||
| All causes | |||||||||||||||||
| Deaths, n | 255 | 587 | 469 | 307 | 129 | 264 | 258 | 213 | |||||||||
| Model 1* | 1·00 | 0·76 | 0·65, 0·88 | 0·76 | 0·65, 0·89 | 0·78 | 0·66, 0·92 | 0·030 | 1·00 | 0·64 | 0·51, 0·79 | 0·64 | 0·52, 0·80 | 0·62 | 0·50, 0·78 | 0·003 | |
| Model 2† | 1·00 | 0·79 | 0·68, 0·91 | 0·80 | 0·68, 0·93 | 0·83 | 0·70, 0·98 | 0·128 | 1·00 | 0·69 | 0·55, 0·85 | 0·71 | 0·57, 0·89 | 0·69 | 0·55, 0·86 | 0·023 | 0·238 |
| Model 3‡ | 1·00 | 0·81 | 0·69, 0·94 | 0·84 | 0·71, 0·99 | 0·87 | 0·73, 1·05 | 0·391 | 1·00 | 0·68 | 0·55, 0·85 | 0·72 | 0·57, 0·90 | 0·69 | 0·54, 0·88 | 0·041 | |
| Model 4§ | 1·00 | 0·82 | 0·70, 0·95 | 0·87 | 0·73, 1·03 | 0·95 | 0·78, 1·17 | 0·968 | 1·00 | 0·68 | 0·54, 0·84 | 0·72 | 0·57, 0·91 | 0·76 | 0·58, 1·00 | 0·253 | |
| Cancer | |||||||||||||||||
| Deaths, n | 141 | 380 | 286 | 181 | 72 | 169 | 153 | 113 | |||||||||
| Model 1* | 1·00 | 0·84 | 0·69, 1·02 | 0·80 | 0·65, 0·98 | 0·80 | 0·64, 1·01 | 0·074 | 1·00 | 0·70 | 0·53, 0·92 | 0·66 | 0·50, 0·88 | 0·60 | 0·44, 0·81 | 0·004 | |
| Model 2† | 1·00 | 0·86 | 0·71, 1·05 | 0·82 | 0·67, 1·01 | 0·83 | 0·66, 1·04 | 0·130 | 1·00 | 0·73 | 0·55, 0·96 | 0·71 | 0·53, 0·94 | 0·63 | 0·46, 0·86 | 0·011 | 0·167 |
| Model 3‡ | 1·00 | 0·86 | 0·71, 1·05 | 0·83 | 0·67, 1·03 | 0·83 | 0·66, 1·06 | 0·161 | 1·00 | 0·72 | 0·54, 0·96 | 0·71 | 0·53, 0·96 | 0·64 | 0·46, 0·89 | 0·027 | |
| Model 4§ | 1·00 | 0·89 | 0·73, 1·09 | 0·88 | 0·70, 1·10 | 0·90 | 0·69, 1·18 | 0·493 | 1·00 | 0·70 | 0·53, 0·94 | 0·70 | 0·51, 0·95 | 0·69 | 0·48, 0·98 | 0·107 | |
| CVD | |||||||||||||||||
| Deaths, n | 38 | 67 | 59 | 40 | 20 | 41 | 39 | 36 | |||||||||
| Model 1* | 1·00 | 0·62 | 0·42, 0·93 | 0·68 | 0·45, 1·03 | 0·72 | 0·46, 1·14 | 0·374 | 1·00 | 0·74 | 0·43, 1·27 | 0·67 | 0·39, 1·17 | 0·68 | 0·39, 1·19 | 0·236 | |
| Model 2† | 1·00 | 0·67 | 0·45, 1·00 | 0·75 | 0·50, 1·14 | 0·82 | 0·52, 1·30 | 0·718 | 1·00 | 0·84 | 0·49, 1·44 | 0·80 | 0·46, 1·39 | 0·79 | 0·45, 1·39 | 0·463 | 0·867 |
| Model 3‡ | 1·00 | 0·71 | 0·47, 1·07 | 0·87 | 0·56, 1·34 | 0·97 | 0·59, 1·59 | 0·744 | 1·00 | 0·81 | 0·46, 1·40 | 0·78 | 0·44, 1·37 | 0·78 | 0·43, 1·42 | 0·486 | |
| Model 4§ | 1·00 | 0·71 | 0·47, 1·08 | 0·89 | 0·56, 1·40 | 1·11 | 0·63, 1·93 | 0·504 | 1·00 | 0·76 | 0·44, 1·33 | 0·75 | 0·42, 1·34 | 0·87 | 0·45, 1·68 | 0·785 | |
| Other causes | |||||||||||||||||
| Deaths, n | 76 | 140 | 124 | 86 | 37 | 54 | 66 | 64 | |||||||||
| Model 1* | 1·00 | 0·66 | 0·50, 0·88 | 0·74 | 0·55, 0·98 | 0·77 | 0·56, 1·06 | 0·387 | 1·00 | 0·47 | 0·31, 0·72 | 0·59 | 0·39, 0·88 | 0·64 | 0·42, 0·97 | 0·484 | |
| Model 2† | 1·00 | 0·71 | 0·54, 0·94 | 0·80 | 0·60, 1·07 | 0·85 | 0·62, 1·16 | 0·721 | 1·00 | 0·52 | 0·34, 0·80 | 0·69 | 0·46, 1·04 | 0·75 | 0·49, 1·14 | 0·950 | 0·905 |
| Model 3‡ | 1·00 | 0·74 | 0·56, 0·99 | 0·87 | 0·65, 1·18 | 0·95 | 0·67, 1·33 | 0·776 | 1·00 | 0·53 | 0·34, 0·81 | 0·70 | 0·46, 1·08 | 0·75 | 0·47, 1·19 | 0·925 | |
| Model 4§ | 1·00 | 0·73 | 0·55, 0·98 | 0·87 | 0·63, 1·19 | 1·03 | 0·70, 1·51 | 0·588 | 1·00 | 0·55 | 0·36, 0·85 | 0·76 | 0·48, 1·18 | 0·87 | 0·52, 1·44 | 0·759 | |
CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; JDI, Japanese diet index.
Adjusted for age and study area.
In males, values are adjusted for covariates in Model 1 plus BMI; smoking habit; alcohol consumption; education level; leisure-time physical activity; and self-reported medical history of hypertension, diabetes and dyslipidaemia.
In females, values are adjusted for covariates in Model 1 plus BMI; smoking habit; alcohol consumption; education level; leisure-time physical activity; self-reported medical history of hypertension, diabetes and dyslipidaemia; age at menarche; number of births; and menopausal status.
Adjusted for covariates in Model 2 plus total energy intake; energy-adjusted intakes of green and yellow vegetables, light-coloured vegetables, fruit, meat, rice, Na and dietary fibre; and JDI score.
Adjusted for covariates in Model 3 plus energy-adjusted intakes of n-3 HUFA, Ca, vitamin D, retinol and carotene.
Adjusted for sex; age; study area; BMI; smoking habit; alcohol consumption; education level; leisure-time physical activity; self-reported medical history of hypertension, diabetes and dyslipidaemia; total energy intake; energy-adjusted intakes of green and yellow vegetables, light-coloured vegetables, fruit, meat, rice, Na and dietary fibre; JDI score; and cross-product term (i.e. sex (dichotomous) × category of small fish consumed (continuous)), representing the interaction.
In the sensitivity analysis additionally excluding participants who died 1–3 years after the baseline survey and using the same covariates as in Model 3, the inverse association between the intake of small fish and all-cause mortality was almost unchanged in females. The HR (95 % CI) were 0·67 (0·53, 0·86) for intakes 1–3 times/month, 0·74 (0·57, 0·94) for 1–2 times/week and 0·67 (0·51, 0·88) for ≥ 3 times/week, compared with the rare intake (P for trend = 0·047). No statistically significant trend in the association was observed in males. The HR (95 % CI) were 0·82 (0·69, 0·98) for intakes 1–3 times/month, 0·83 (0·69, 0·99) for 1–2 times/week and 0·90 (0·73, 1·11) for ≥ 3 times/week, compared with the rare intake (P for trend = 0·560). In the analysis excluding participants from the Aichi Cancer Center and using the same covariates as in Model 3, the inverse association between the intake of small fish and all-cause mortality was also observed in females. The HR (95 % CI) were 0·71 (0·56, 0·90) for intakes 1–3 times/month, 0·76 (0·59, 0·98) for 1–2 times/week and 0·68 (0·51, 0·89) for ≥ 3 times/week, compared with the rare intake (P for trend = 0·041). No statistically significant association was observed in males. The HR (95 % CI) were 0·87 (0·73, 1·04) for intakes 1–3 times/month, 0·91 (0·75, 1·09) for 1–2 times/week and 0·99 (0·81, 1·22) for ≥ 3 times/week, compared with the rare intake (P for trend = 0·753). The P value for interaction between the intake of small fish and sex for all-cause mortality was not statistically significant (P for interaction = 0·238).
Cause-specific mortality
The associations between the frequency of the intake of small fish and the risk of cancer, CVD and other-cause mortality by sex are also shown in Table 3. In Model 3, the intake of small fish was associated with a statistically significant decrease in the risk of cancer mortality, and a linear trend was observed in females. The multivariable-adjusted HR (95 % CI) were 0·72 (0·54, 0·96) for intakes 1–3 times/month, 0·71 (0·53, 0·96) for 1–2 times/week and 0·64 (0·46, 0·89) for ≥ 3 times/week, compared with the rare intake (P for trend = 0·027). The association in males was not statistically significant, although its direction was the same as that in females. In Model 4, with an additional adjustment for the energy-adjusted intake of nutrients abundant in small fish, the inverse association between the intake of small fish and cancer mortality remained statistically significant in females. No statistically significant association was observed in males.
In the sensitivity analysis additionally excluding participants who died 1–3 years after the baseline survey and using the same covariates as in Model 3, the inverse association between the intake of small fish and cancer mortality was almost unchanged in females, whereas no association was detected in males. The HR (95 % CI) in females were 0·77 (0·55, 1·07) for intakes 1–3 times/month, 0·76 (0·54, 1·07) for 1–2 times/week and 0·63 (0·43, 0·93) for ≥ 3 times/week, compared with the rare intake (P for trend = 0·039). The corresponding HR (95 % CI) in males were 0·91 (0·72, 1·16), 0·84 (0·65, 1·09) and 0·91 (0·69, 1·22), respectively (P for trend = 0·460). In the analysis excluding participants from the Aichi Cancer Center and using the same covariates as in Model 3, the inverse association between the intake of small fish ≥ 3 times/week and cancer mortality was statistically significant in females, but not in males. The HR (95 % CI) in females were 0·79 (0·56, 1·12) for intakes 1–3 times/month, 0·83 (0·58, 1·18) for 1–2 times/week and 0·66 (0·45, 0·98) for ≥ 3 times/week, compared with the rare intake (P for trend = 0·081). The corresponding HR (95 % CI) in males were 0·98 (0·76, 1·26), 0·91 (0·70, 1·20) and 1·00 (0·74, 1·34), respectively (P for trend = 0·827). The intake of small fish was not clearly associated with the risk of CVD and other-cause mortality in both sexes. The P values for interaction between the intake of small fish and sex for the risk were 0·167 for cancer mortality, 0·867 for CVD mortality and 0·905 for other-cause mortality, none of which was statistically significant.
Stratified analysis
Tables 4 and 5 show the HR (95 % CI) for all-cause and cancer mortality according to the frequency of the intake of small fish in the analyses stratified by age, smoking status and JDI score. In the analysis stratified by age, no remarkable age-dependent differences were found in the directions of the associations between the intake of small fish and all-cause and cancer mortality in both sexes. The P values for interaction between the intake of small fish and age for the risk were 0·289 for all-cause mortality and 0·175 for cancer mortality in males. The corresponding P values in females were 0·827 for all-cause mortality and 0·909 for cancer mortality. As for the smoking status, the intake of small fish was inversely associated with the risk of all-cause and cancer mortality, especially in never-smoking females. The multivariable-adjusted HR (95 % CI) for all-cause mortality were 0·60 (0·47, 0·76) for intakes 1–3 times/month, 0·62 (0·48, 0·79) for 1–2 times/week and 0·61 (0·47, 0·79) for ≥ 3 times/week, compared with the rare intake (P for trend = 0·011). The corresponding HR (95 % CI) for cancer mortality were 0·62 (0·46, 0·85), 0·59 (0·43, 0·82) and 0·53 (0·37, 0·75), respectively (P for trend = 0·003). In males, no statistically significant association was observed in either smokers or never smokers. The P value for interaction between the intake of small fish and smoking status for the risk was 0·268 for all-cause mortality and 0·059 for cancer mortality in females. The corresponding P values in males were 0·892 for all-cause mortality and 0·400 for cancer mortality. Regarding the analysis stratified by the JDI score, the inverse associations between the intake of small fish and the risk of all-cause and cancer mortality were stronger in females with a high JDI score (≥ 4 points). The multivariable-adjusted HR (95 % CI) for all-cause mortality were 0·61 (0·45, 0·83) for intakes 1–3 times/month, 0·63 (0·46, 0·84) for 1–2 times/week and 0·56 (0·41, 0·77) for ≥ 3 times/week, compared with the rare intake (P for trend = 0·008). The corresponding HR (95 % CI) for cancer mortality were 0·61 (0·41, 0·93), 0·59 (0·40, 0·89) and 0·52 (0·34, 0·79), respectively (P for trend = 0·016). In males, the intake of small fish was inversely associated with the risk of all-cause and cancer mortality in the low JDI score (≤ 3 points) group. The multivariable-adjusted HR (95 % CI) for all-cause mortality were 0·73 (0·60, 0·88) for intakes 1–3 times/month, 0·68 (0·54, 0·86) for 1–2 times/week and 0·84 (0·61, 1·15) for ≥ 3 times/week, compared with the rare intake (P for trend = 0·038). The corresponding HR (95 % CI) for cancer mortality were 0·70 (0·55, 0·89), 0·57 (0·42, 0·77) and 0·60 (0·39, 0·91), respectively (P for trend < 0·001). Tests of interactions between the intake of small fish and JDI score for all-cause and cancer mortality were statistically significant in males, but not in females. The P values for the interaction of all-cause and cancer mortality were 0·045 and 0·002 in males and 0·525 and 0·621 in females, respectively.
Table 4.
Multivariable-adjusted HR (95 % CI) for all-cause mortality by sex according to the frequency of the intake of small fish in the analysis stratified by age, smoking status and JDI score*
| Male | Female | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rarely | 1–3 times/month | 1–2 times/week | ≥ 3 times/week | P for trend | P for interaction | Rarely | 1–3 times/month | 1–2 times/week | ≥ 3 times/week | P for trend | P for interaction | |
| ≥ 60 years old | 0·289 | 0·827 | ||||||||||
| Participants, n | 1468 | 4894 | 4346 | 3038 | 1282 | 4443 | 5274 | 5171 | ||||
| All-cause deaths, n | 159 | 369 | 332 | 247 | 71 | 130 | 168 | 164 | ||||
| HR | 1·00 | 0·78 | 0·82 | 0·85 | 0·467 | 1·00 | 0·62 | 0·71 | 0·69 | 0·264 | ||
| 95 % CI | 0·64, 0·94 | 0·67, 0·99 | 0·68, 1·05 | 0·46, 0·83 | 0·53, 0·96 | 0·51, 0·94 | ||||||
| < 60 years old | ||||||||||||
| Participants, n | 3578 | 9685 | 5544 | 2002 | 4317 | 13 119 | 8472 | 4169 | ||||
| All-cause deaths, n | 96 | 218 | 137 | 60 | 58 | 134 | 90 | 49 | ||||
| HR | 1·00 | 0·88 | 0·90 | 0·97 | 0·835 | 1·00 | 0·76 | 0·70 | 0·65 | 0·048 | ||
| 95 % CI | 0·69, 1·13 | 0·68, 1·20 | 0·68, 1·38 | 0·55, 1·05 | 0·49, 0·99 | 0·42, 0·99 | ||||||
| Smoker (former or current) | 0·892 | 0·268 | ||||||||||
| Participants, n | 3507 | 10 346 | 6981 | 3465 | 1177 | 2894 | 1691 | 874 | ||||
| All-cause deaths, n | 215 | 468 | 373 | 249 | 20 | 56 | 47 | 23 | ||||
| HR | 1·00 | 0·75 | 0·78 | 0·86 | 0·375 | 1·00 | 1·21 | 1·68 | 1·08 | 0·515 | ||
| 95 % CI | 0·63, 0·88 | 0·65, 0·93 | 0·70, 1·05 | 0·71, 2·06 | 0·94, 2·99 | 0·55, 2·12 | ||||||
| Never smoker | ||||||||||||
| Participants, n | 1522 | 4188 | 2883 | 1562 | 4397 | 14 577 | 11 978 | 8414 | ||||
| All-cause deaths, n | 40 | 118 | 96 | 58 | 106 | 207 | 211 | 187 | ||||
| HR | 1·00 | 1·10 | 1·14 | 0·91 | 0·657 | 1·00 | 0·60 | 0·62 | 0·61 | 0·011 | ||
| 95 % CI | 0·76, 1·58 | 0·78, 1·68 | 0·59, 1·41 | 0·47, 0·76 | 0·48, 0·79 | 0·47, 0·79 | ||||||
| JDI score ≤ 3 | 0·045 | 0·525 | ||||||||||
| Participants, n | 3456 | 8325 | 3510 | 906 | 3820 | 9880 | 4845 | 1422 | ||||
| All-cause deaths, n | 167 | 304 | 140 | 59 | 66 | 125 | 78 | 32 | ||||
| HR | 1·00 | 0·73 | 0·68 | 0·84 | 0·038 | 1·00 | 0·76 | 0·85 | 0·99 | 0·971 | ||
| 95 % CI | 0·60, 0·88 | 0·54, 0·86 | 0·61, 1·15 | 0·56, 1·04 | 0·60, 1·21 | 0·63, 1·56 | ||||||
| JDI score ≥ 4 | ||||||||||||
| Participants, n | 1590 | 6254 | 6380 | 4134 | 1779 | 7682 | 8901 | 7918 | ||||
| All-cause deaths, n | 88 | 283 | 329 | 248 | 63 | 139 | 180 | 181 | ||||
| HR | 1·00 | 0·96 | 1·03 | 0·98 | 0·868 | 1·00 | 0·61 | 0·63 | 0·56 | 0·008 | ||
| 95 % CI | 0·75, 1·22 | 0·81, 1·31 | 0·76, 1·26 | 0·45, 0·83 | 0·46, 0·84 | 0·41, 0·77 | ||||||
CI, confidence interval; HR, hazard ratio; JDI, Japanese diet index.
In males, HR were adjusted for age; study area; BMI; smoking habit; alcohol consumption; education level; leisure-time physical activity; self-reported medical history of hypertension, diabetes and dyslipidaemia; total energy intake; energy-adjusted intakes of green and yellow vegetables, light-coloured vegetables, fruit, meat, rice, Na and dietary fibre; and JDI score.
In females, HR were adjusted for the same covariates as in males plus age at menarche, number of births and menopausal status.
Table 5.
Multivariable-adjusted HR (95 % CI) for cancer mortality by sex according to the frequency of the intake of small fish in the analysis stratified by age, smoking status and JDI score*
| Male | Female | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rarely | 1–3 times/month | 1–2 times/week | ≥ 3 times/week | P for trend | P for interaction | Rarely | 1–3 times/month | 1–2 times/week | ≥ 3 times/week | P for trend | P for interaction | |
| ≥ 60 years old | 0·175 | 0·909 | ||||||||||
| Participants, n | 1468 | 4894 | 4346 | 3038 | 1282 | 4443 | 5274 | 5171 | ||||
| Cancer deaths, n | 85 | 249 | 198 | 144 | 34 | 77 | 95 | 81 | ||||
| HR | 1·00 | 0·92 | 0·86 | 0·89 | 0·376 | 1·00 | 0·65 | 0·71 | 0·61 | 0·134 | ||
| 95 % CI | 0·72, 1·19 | 0·66, 1·12 | 0·66, 1·19 | 0·43, 0·99 | 0·47, 1·08 | 0·40, 0·95 | ||||||
| < 60 years old | ||||||||||||
| Participants, n | 3578 | 9685 | 5544 | 2002 | 4317 | 13 119 | 8472 | 4169 | ||||
| Cancer deaths, n | 56 | 131 | 88 | 37 | 38 | 92 | 58 | 32 | ||||
| HR | 1·00 | 0·82 | 0·83 | 0·82 | 0·454 | 1·00 | 0·78 | 0·64 | 0·63 | 0·057 | ||
| 95 % CI | 0·59, 1·13 | 0·58, 1·20 | 0·52, 1·30 | 0·53, 1·15 | 0·41, 1·00 | 0·37, 1·08 | ||||||
| Smoker (former or current) | 0·400 | 0·059 | ||||||||||
| Participants, n | 3507 | 10 346 | 6981 | 3465 | 1177 | 2894 | 1691 | 874 | ||||
| Cancer deaths, n | 122 | 303 | 238 | 153 | 10 | 34 | 28 | 16 | ||||
| HR | 1·00 | 0·78 | 0·77 | 0·82 | 0·264 | 1·00 | 1·40 | 1·81 | 1·24 | 0·555 | ||
| 95 % CI | 0·63, 0·97 | 0·61, 0·98 | 0·63, 1·07 | 0·67, 2·91 | 0·82, 3·99 | 0·51, 3·04 | ||||||
| Never smoker | ||||||||||||
| Participants, n | 1522 | 4188 | 2883 | 1562 | 4397 | 14 577 | 11 978 | 8414 | ||||
| Cancer deaths, n | 19 | 76 | 48 | 28 | 61 | 135 | 125 | 95 | ||||
| HR | 1·00 | 1·37 | 1·10 | 0·81 | 0·179 | 1·00 | 0·62 | 0·59 | 0·53 | 0·003 | ||
| 95 % CI | 0·82, 2·29 | 0·63, 1·91 | 0·43, 1·52 | 0·46, 0·85 | 0·43, 0·82 | 0·37, 0·75 | ||||||
| JDI score ≤ 3 | 0·002 | 0·621 | ||||||||||
| Participants, n | 3456 | 8325 | 3510 | 906 | 3820 | 9880 | 4845 | 1422 | ||||
| Cancer deaths, n | 105 | 201 | 82 | 32 | 39 | 86 | 50 | 17 | ||||
| HR | 1·00 | 0·70 | 0·57 | 0·60 | < 0·001 | 1·00 | 0·84 | 0·83 | 0·84 | 0·511 | ||
| 95 % CI | 0·55, 0·89 | 0·42, 0·77 | 0·39, 0·91 | 0·57, 1·25 | 0·53, 1·30 | 0·46, 1·54 | ||||||
| JDI score ≥ 4 | ||||||||||||
| Participants, n | 1590 | 6254 | 6380 | 4134 | 1779 | 7682 | 8901 | 7918 | ||||
| Cancer deaths, n | 36 | 179 | 204 | 149 | 33 | 83 | 103 | 96 | ||||
| HR | 1·00 | 1·33 | 1·34 | 1·25 | 0·633 | 1·00 | 0·61 | 0·59 | 0·52 | 0·016 | ||
| 95 % CI | 0·92, 1·91 | 0·93, 1·92 | 0·86, 1·82 | 0·41, 0·93 | 0·40, 0·89 | 0·34, 0·79 | ||||||
CI, confidence interval; HR, hazard ratio; JDI, Japanese diet index.
In males, HR were adjusted for age; study area; BMI; smoking habit; alcohol consumption; education level; leisure-time physical activity; self-reported medical history of hypertension, diabetes and dyslipidaemia; total energy intake; energy-adjusted intakes of green and yellow vegetables, light-coloured vegetables, fruit, meat, rice, Na and dietary fibre; and JDI score.
In females, HR were adjusted for the same covariates as in males plus age at menarche, number of births and menopausal status.
Intake of small and non-small fish
Supplemental Table 1 summarises the associations between the frequency of the intake of small and non-small fish and the risk of all-cause, cancer, CVD and other-cause mortality by sex in the analysis, adjusting for the intake of small and non-small fish each other in addition to the covariates in Model 3. The intakes of both small and non-small fish were not statistically significantly associated with the risk of each mortality in males. In females, the intake of small fish was statistically significantly associated with a lower risk of all-cause and cancer mortality, but not with CVD and other-cause mortality, even after considering the intake of non-small fish. The multivariable-adjusted HR (95 % CI) for all-cause mortality according to the frequency of the intake of small fish were 0·68 (0·55, 0·85) for intakes 1–3 times/month, 0·72 (0·58, 0·91) for 1–2 times/week and 0·69 (0·54, 0·89) for ≥ 3 times/week, compared with the rare intake (P for trend = 0·050). The corresponding HR (95 % CI) for cancer mortality were 0·72 (0·54, 0·96), 0·72 (0·53, 0·97) and 0·65 (0·46, 0·90), respectively (P for trend = 0·034). Once a day or more frequent intake of non-small fish was associated with a lower all-cause mortality in females.
Discussion
In this large prospective study, the frequent intake of small fish was associated with a lower all-cause and cancer mortality in females. The association in males was not statistically significant, although its direction between the intake of small fish and cancer mortality was the same as in females. Regarding the association between the intake of small fish and all-cause mortality in males, the HR were lower for intakes 1–3 times/month or more, compared with the rare intake. The intake of small fish was not associated with CVD mortality in both sexes.
To our knowledge, this is the first study to demonstrate the association between intake of small fish and the risk of all-cause and cause-specific mortality. Small fish can be a component of a healthy diet. They are a good source of micronutrients such as Ca, vitamins and fatty acids when consumed with bones and organs(2,3,5,6). With regard to the relationship between nutrients in small fish and mortality risk, Ca intake is inversely associated with the risk of all-cause and CVD mortality, and some proportion of cancer mortality, such as mortality among patients with early-stage lung cancer(7,32,33); however, some reports suggest that high intake of Ca can increase the risk of cancer and CVD mortality(7,32,34). Thus, appropriate Ca intake, considering individual health status, such as pre-existing diseases (cancer, osteoporosis and heart disease), has been recommended(7). Because Ca from small fish with bones is highly bioavailable, small fish are a useful source of Ca(5,35). Another mechanism for the protective effect of small fish on mortality risk may involve the antitumour effects of vitamins A and D as well as n-3 PUFA. Focusing on the major sites associated with cancer death in Japan, recent meta-analyses have shown inverse associations between dietary vitamin A intake and the risk of lung, pancreatic, gastric and breast cancers(36–40). Vitamin D intake or serum 25-hydroxyvitamin D (25(OH)D) level has also been reported to be inversely associated with the risk of lung, breast and colorectal cancer morbidity and mortality(8,41–44). N-3 PUFA intake has been related to a reduced risk of breast cancer and is also inversely related to all-cause and CVD mortality in some reports; however, the association is still controversial(18,45–49).
In this study, an association between the intake of small fish and all-cause and cancer mortality was observed in females, and this association remained even after adjustment for female-specific factors, including age at menarche, number of births and menopausal status. One of the reasons underlying the difference in the effects of consumption of small fish on the risk of all-cause and cancer mortality between sexes in this study might be the difference in the cancer type causing cancer mortality among sexes; however, other reasons are unknown. The sex-based difference in the association between the intake of small fish and alcohol and/or other food consumption might provide another explanation although we did consider alcohol drinking and food consumption in the multivariable models. The P values for interaction between the intake of small fish and sex for the risk were not statistically significant. The sex difference, if any, could not be so large.
Vitamin A contributes to the prevention of cancer through antioxidant activity, induction of detoxifying enzymes and regulation of genes involved in cell morphogenesis, differentiation and proliferation(9,37). Vitamin D exerts antitumour effects by contact inhibition of proliferation, cell cycle stabilisation, promotion of apoptosis and anti-neoangiogenesis(8). N-3 HUFA suppress the progression of carcinogenesis and metastasis through the production of lipid peroxides and increased apoptosis of cancer cells(50). In Model 4 (Table 3), the adjustment for intakes of these nutrients based on the abovementioned findings weakened the inverse association between the intake of small fish and all-cause and cancer mortality. However, the association remained statistically significant in females. This suggests that the effects of these nutrients only partially explain the association of mortality risk, and other or unknown nutrients or physiologically active substances might exert protective effects. Some small fish are rich in Mg(4); however, this was not adjusted for in this study due to the limitation of FFQ. Mg intake reduces the risk of lung cancer(12). Serum Mg is also inversely correlated with all-cause and cancer mortality(51). The intake of small fish is expected to contribute to a well-balanced intake of micronutrients, such as Ca, vitamins A and D, n-3 PUFA and Mg.
Participants who consumed higher amounts of small fish could have had a healthier diet as shown in Tables 1 and 2 and demonstrated a lower mortality. To eliminate this confounding factor, we adjusted for the JDI score. The JDI score, which is a measure of the degree of adherence to the Japanese diet, is also an indicator of healthy dietary patterns as, in previous studies, higher JDI scores were reported to be associated with lower risk of all-cause and CVD mortality(30,31). Even after adjustment for the JDI score, the inverse association between the intake of small fish and all-cause and cancer mortality was scarcely altered in females, which suggests that the intake of small fish reduces the risk of all-cause and cancer mortality, independent of a healthy diet. Furthermore, in the analysis adjusting for the intake of non-small fish, the inverse association between the intake of small fish and the risk of all-cause and cancer mortality remained statistically significant in females. This suggests that the intake of small fish is associated with a reduced risk of all-cause and cancer mortality, independent of the intake of non-small fish.
The stratified analysis with respect to the smoking status revealed that the intake of small fish was inversely associated with the risk of all-cause and cancer mortality in female never smokers. We also adjusted for comprehensive smoking variables. These support that confounding by smoking is unlikely. The results of the analysis stratified by the JDI score showed that the inverse association between the intake of small fish and all-cause and cancer mortality was stronger in the high-JDI score group among females. In males, the inverse association was found in the low-JDI score group, but not found in all the males. Although the reason for this sex-based difference is unclear, for males with unhealthy dietary patterns, the intake of small fish may help compensate for the lack of nutrients in poor-quality diets.
The strengths of the present study are the large sample size, prospective design and the extensive adjustment for potentially important confounding factors. Nonetheless, this study has several limitations. First, changes in eating habits or lifestyle factors during the follow-up period could not be considered because the questionnaire was answered only once at the baseline survey by a considerable proportion of participants (40·8 %). Second, the use of an FFQ inevitably led to some misclassification of the intake of small fish, although the questionnaire was validated based on dietary records. The validity was not good for several food groups and nutrients included as covariates. Third, residual confounding, such as socio-economic status, cannot be completely ruled out, although we adjusted for many potential confounding factors. Fourth, the number of CVD death events might not be enough to conclude the association between the intake of small fish and the risk of CVD mortality. Finally, because the study area is limited to Japan, our findings are not generalisable to other countries.
In conclusion, we suggest that the intake of small fish reduces the risk of all-cause and cancer mortality in Japanese females.
Supporting information
Kasahara et al. supplementary material
Kasahara et al. supplementary material
Acknowledgements
We thank Dr Nobuyuki Hamajima of Nagoya University Graduate School of Medicine and Dr Hideo Tanaka of Kishiwada Public Health Center for supervising the entire study as previous principal investigators.
Financial support
This study was supported by Grants-in-Aid for Scientific Research on Priority Areas of Cancer (no. 17015018) and Innovative Areas (no. 221S0001) and by a JSPS KAKENHI Grant (no. 16H06277 and 22H04923, (CoBiA)) from the Japanese Ministry of Education, Culture, Sports, Science and Technology. The funders had no input into the study’s design; the collection, analysis and interpretation of data; the writing and revision of this article; or the decision to submit the article for publication.
Conflict of interest
All authors declare no conflicts of interest.
Authorship
The authors’ responsibilities were as follows – C.K. analysed data and wrote the paper; T.T. analysed data and extensively revised the paper; C.K. and K.W. designed research and had primary responsibility for final content; N.I. and C.G. provided essential materials; Y.T., Y. Kato, Y. Kubo, R.O., M.N., A.H., J.O., H.I., Y. Nishida, C.S., I.O., Y.N.K., Y. Nakamura, M.K., D.N., I.S., S.S., M.W., E.O., C.O., K.K., N.T., N.M., K.A., S.K.K., K.T. and K.M. conducted research. K.M. supervised the J-MICC Study. All authors read and approved the final manuscript.
Ethics of human subject participation
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving study participants were approved by the ethics committees of Nagoya University Graduate School of Medicine and other participating institutions in the J-MICC Study. Written informed consent was obtained from all the participants.
Based on the informed consent provided by the participants, some access restrictions apply, and the data cannot be made publicly available. Requests for data can be sent to Dr Kenji Wakai, Department of Preventive Medicine, Nagoya University Graduate School of Medicine, Japan (email: wakai@med.nagoya-u.ac.jp).
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the funding organisation.
Supplementary material
For supplementary material accompanying this paper, visit https://doi.org/10.1017/S1368980024000831.
References
- 1. Abbey L, Glover-Amengor M, Atikpo MO et al. (2017) Nutrient content of fish powder from low value fish and fish byproducts. Food Sci Nutr 5, 374–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Roos N, Leth T, Jakobsen J et al. (2002) High vitamin A content in some small indigenous fish species in Bangladesh: perspectives for food-based strategies to reduce vitamin A deficiency. Int J Food Sci Nutr 53, 425–437. [DOI] [PubMed] [Google Scholar]
- 3. Roos N, Wahab MA, Chamnan C et al. (2007) The role of fish in food-based strategies to combat vitamin A and mineral deficiencies in developing countries. J Nutr 137, 1106–1109. [DOI] [PubMed] [Google Scholar]
- 4. Ministry of Education Culture Sports Science and Technology-Japan Standard Tables of Food Composition in Japan – (2015) – (Seventh Revised Version). https://www.mext.go.jp/a_menu/syokuhinseibun/1365419.htm (accessed 25 April 2021).
- 5. Bourassa MW, Abrams SA, Belizan JM et al. (2022) Interventions to improve calcium intake through foods in populations with low intake. Ann N Y Acad Sci 1511, 40–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Beal T & Ortenzi F (2022) Priority micronutrient density in foods. Front Nutr 9, 806566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Li K, Wang XF, Li DY et al. (2018) The good, the bad, and the ugly of calcium supplementation: a review of calcium intake on human health. Clin Interv Aging 13, 2443–2452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Garland CF, Gorham ED, Mohr SB et al. (2009) Vitamin D for cancer prevention: global perspective. Ann Epidemiol 19, 468–483. [DOI] [PubMed] [Google Scholar]
- 9. Dawson MI (2000) The importance of vitamin A in nutrition. Curr Pharm 6, 311–325. [DOI] [PubMed] [Google Scholar]
- 10. Anderson JJ, Kruszka B, Delaney JA et al. (2016) Calcium intake from diet and supplements and the risk of coronary artery calcification and its progression among older adults: 10-year follow-up of the Multi-Ethnic Study of Atherosclerosis (MESA). J Am Heart Assoc 5, e003815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Han H, Fang X, Wei X et al. (2017) Dose-response relationship between dietary magnesium intake, serum magnesium concentration and risk of hypertension: a systematic review and meta-analysis of prospective cohort studies. Nutr J 16, 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dana N, Karimi R, Mansourian M et al. (2021) Magnesium intake and lung cancer risk: a systematic review and meta-analysis. Int J Vitam Nutr Res 91, 539–546. [DOI] [PubMed] [Google Scholar]
- 13. Ministry of Internal Affairs and Communications (2020) Statistics on Fishery and Aquaculture Production. https://www.e-stat.go.jp/stat-search/files?page=1&layout=datalist&toukei=00500216&tstat=000001015174&cycle=7&tclass1=000001015175&tclass2=000001162470&tclass3val=0 (accessed 17 October 2022).
- 14. Bogard JR, Hother AL, Saha M et al. (2015) Inclusion of small indigenous fish improves nutritional quality during the first 1000 days. Food Nutr Bull 36, 276–289. [DOI] [PubMed] [Google Scholar]
- 15. Hosomi R, Yoshida M & Fukunaga K (2012) Seafood consumption and components for health. Glob J Health Sci 4, 72–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mozaffarian D & Rimm EB (2006) Fish intake, contaminants, and human health: evaluating the risks and the benefits. JAMA 296, 1885–1899. [DOI] [PubMed] [Google Scholar]
- 17. Zhao LG, Sun JW, Yang Y et al. (2016) Fish consumption and all-cause mortality: a meta-analysis of cohort studies. Eur J Clin Nutr 70, 155–161. [DOI] [PubMed] [Google Scholar]
- 18. Zhang Y, Zhuang P, He W et al. (2018) Association of fish and long-chain n-3 fatty acids intakes with total and cause-specific mortality: prospective analysis of 421 309 individuals. J Intern Med 284, 399–417. [DOI] [PubMed] [Google Scholar]
- 19. Krieger JP, Cabaset S, Pestoni G et al. (2018) Dietary patterns are associated with cardiovascular and cancer mortality among Swiss adults in a census-linked cohort. Nutrients 10, 313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhang B, Xiong K, Cai J et al. (2020) Fish consumption and coronary heart disease: a meta-analysis. Nutrients 12, 2278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Takeuchi K, Naito M, Kawai S et al. (2021) Study profile of the Japan Multi-institutional Collaborative Cohort (J-MICC) study. J Epidemiol 31, 660–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sasakabe T, Wakai K, Kawai S et al. (2018) Modification of the associations of alcohol intake with serum low-density lipoprotein cholesterol and triglycerides by ALDH2 and ADH1B polymorphisms in Japanese men. J Epidemiol 28, 185–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Higashibata T, Hamajima N, Naito M et al. (2012) eNOS genotype modifies the effect of leisure-time physical activity on serum triglyceride levels in a Japanese population. Lipids Health Dis 11, 150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kikuchi H, Inoue S, Odagiri Y et al. (2020) Intensity-specific validity and reliability of the Japan Public Health Center-based prospective study-physical activity questionnaire. Prev Med Rep 20, 101169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tokudome S, Goto C, Imaeda N et al. (2004) Development of a data-based short food frequency questionnaire for assessing nutrient intake by middle-aged Japanese. Asian Pac J Cancer Prev 5, 40–43. [PubMed] [Google Scholar]
- 26. Tokudome Y, Goto C, Imaeda N et al. (2005) Relative validity of a short food frequency questionnaire for assessing nutrient intake v. three-day weighed diet records in middle-aged Japanese. J Epidemiol 15, 135–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Imaeda N, Goto C, Sasakabe T et al. (2021) Reproducibility and validity of food group intake in a short food frequency questionnaire for the middle-aged Japanese population. Environ Health Prev Med 26, 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ministry of Science and Technology (2000) Standard Tables of Food Composition in Japan, the Fifth Revised Edition. Tokyo: Printing Bureau, Ministry of Finance. [Google Scholar]
- 29. Brown CC, Kipnis V, Freedman LS et al. (1994) Energy adjustment methods for nutritional epidemiology: the effect of categorization. Am J Epidemiol 139, 323–338. [DOI] [PubMed] [Google Scholar]
- 30. Matsuyama S, Sawada N, Tomata Y et al. (2021) Association between adherence to the Japanese diet and all-cause and cause-specific mortality: the Japan Public Health Center-based Prospective Study. Eur J Nutr 60, 1327–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Abe S, Zhang S, Tomata Y et al. (2020) Japanese diet and survival time: the Ohsaki Cohort 1994 study. Clin Nutr 39, 298–303. [DOI] [PubMed] [Google Scholar]
- 32. Wang X, Chen H, Ouyang Y et al. (2014) Dietary calcium intake and mortality risk from cardiovascular disease and all causes: a meta-analysis of prospective cohort studies. BMC Med 12, 158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yu D, Takata Y, Smith-Warner SA et al. (2017) Prediagnostic calcium intake and lung cancer survival: a pooled analysis of 12 cohort studies. Cancer Epidemiol Biomarkers Prev 26, 1060–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chen F, Du M, Blumberg JB et al. (2019) Association among dietary supplement use, nutrient intake, and mortality among U.S. adults: a cohort study. Ann Intern Med 170, 604–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Larsen T, Thilsted SH, Kongsbak K et al. (2000) Whole small fish as a rich calcium source. Br J Nutr 83, 191–196. [PubMed] [Google Scholar]
- 36. Fulan H, Changxing J, Baina WY et al. (2011) Retinol, vitamins A, C, and E and breast cancer risk: a meta-analysis and meta-regression. Cancer Causes Control 22, 1383–1396. [DOI] [PubMed] [Google Scholar]
- 37. Yu N, Su X, Wang Z et al. (2015) Association of dietary vitamin A and beta-carotene intake with the risk of lung cancer: a meta-analysis of 19 publications. Nutrients 7, 9309–9324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Huang X, Gao Y, Zhi X et al. (2016) Association between vitamin A, retinol and carotenoid intake and pancreatic cancer risk: evidence from epidemiologic studies. Sci Rep 6, 38936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wu Y, Ye Y, Shi Y et al. (2015) Association between vitamin A, retinol intake and blood retinol level and gastric cancer risk: a meta-analysis. Clin Nutr 34, 620–626. [DOI] [PubMed] [Google Scholar]
- 40. He J, Gu Y & Zhang S (2018) Vitamin A and breast cancer survival: a systematic review and meta-analysis. Clin Breast Cancer 18, e1389–e1400. [DOI] [PubMed] [Google Scholar]
- 41. Liu J, Dong Y, Lu C et al. (2017) Meta-analysis of the correlation between vitamin D and lung cancer risk and outcomes. Oncotarget 8, 81040–81051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Qian M, Lin J, Fu R et al. (2021) The role of vitamin D intake on the prognosis and incidence of lung cancer: a systematic review and meta-analysis. J Nutr Sci Vitaminol (Tokyo) 67, 273–282. [DOI] [PubMed] [Google Scholar]
- 43. Voutsadakis IA (2021) Vitamin D baseline levels at diagnosis of breast cancer: a systematic review and meta-analysis. Hematol Oncol Stem Cell Ther 14, 16–26. [DOI] [PubMed] [Google Scholar]
- 44. Li C, Li H, Zhong H et al. (2021) Association of 25-hydroxyvitamin D level with survival outcomes in female breast cancer patients: a meta-analysis. J Steroid Biochem Mol Biol 212, 105947. [DOI] [PubMed] [Google Scholar]
- 45. Wang C, Harris WS, Chung M et al. (2006) n-3 Fatty acids from fish or fish-oil supplements, but not alpha-linolenic acid, benefit cardiovascular disease outcomes in primary- and secondary-prevention studies: a systematic review. Am J Clin Nutr 84, 5–17. [DOI] [PubMed] [Google Scholar]
- 46. Abdelhamid AS, Brown TJ, Brainard JS et al. (2018) n-3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev issue 7, CD003177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hu FB, Bronner L, Willett WC et al. (2002) Fish and n-3 fatty acid intake and risk of coronary heart disease in women. JAMA 287, 1815–1821. [DOI] [PubMed] [Google Scholar]
- 48. Innes JK & Calder PC (2020) Marine n-3 fatty acids for cardiovascular health: an update for 2020. Int J Mol Sci 21, 1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Zheng JS, Hu XJ, Zhao YM et al. (2013) Intake of fish and marine n-3 polyunsaturated fatty acids and risk of breast cancer: meta-analysis of data from 21 independent prospective cohort studies. BMJ 346, f3706. [DOI] [PubMed] [Google Scholar]
- 50. Moloudizargari M, Mortaz E, Asghari MH et al. (2018) Effects of the polyunsaturated fatty acids, EPA and DHA, on hematological malignancies: a systematic review. Oncotarget 9, 11858–11875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Leone N, Courbon D, Ducimetiere P et al. (2006) Zinc, copper, and magnesium and risks for all-cause, cancer, and cardiovascular mortality. Epidemiology 17, 308–314. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Kasahara et al. supplementary material
Kasahara et al. supplementary material


