Abstract
Patient group The majority of cats will develop radiographic evidence of degenerative joint disease by the time they are 12 years of age, and many will suffer from a decline in quality of life associated with undiagnosed and untreated orthopedic disease.
Practical relevance A focused, efficient orthopedic examination, including gait observation and palpation (awake and under sedation), supplemented with appropriate history, is key in ruling in, or out, clinically important musculoskeletal disease. Identifying problems assists in both developing a diagnostic plan and monitoring response to treatment.
Clinical challenges Many clinicians feel uncomfortable in their ability to reliably perform an orthopedic examination in the cat, and diagnosis and evaluation of response to treatment in cats with orthopedic disease can be challenging. Hands-on training in feline orthopedic examination is limited in many veterinary curricula. Additional constraints may include failure to obtain important information in the history that indicates feline orthopedic disease, lack of appropriate facilities in which to conduct a complete orthopedic examination, and inability to obtain the most important information during the time available to conduct the examination. These problems can create gaps in the practitioner’s ability to provide excellent care for a large proportion of the feline population.
Goals The above challenges can mostly be overcome with advanced planning and with consideration of the unique behavioral aspects related to feline handling. As discussed in this review, the aim of the initial orthopedic examination is to localize the problem to a specific limb, ideally to a region or joint of the limb, which can further direct diagnostics such as radiography or arthrocentesis. This should provide a basis for follow-up and assessment of whether treatment strategies are effective.
Orthopedic disease, particularly osteoarthritis (OA), is emerging as one of the most important disease conditions in cats, with some studies indicating a prevalence of up to 90% in cats.1,2 Still much remains unknown about the etiology, prevention and treatment of feline orthopedic disease, and its recognition is often a challenge in the clinical setting.
Relevant patient history
Studies of feline OA were originally performed retrospectively and focused on radiographic signs, with the owner’s complaint being evaluated as a secondary goal. Godfrey reported clinical signs in only 21 of 63 cats with retrospectively evaluated appendicular OA: 11 had recorded lameness, five a stiff gait, two difficulty jumping, and one each showed weakness, inactivity and a shuffling thoracic limb gait. 3 Additional retrospective radiographic reports of OA in cats have also found a very low (4–16%) rate of owner-reported lameness.1,4
Cats with orthopedic disease are unlikely to come into the clinic for a classic lameness, as seen in dogs; however, when a lame cat is observed by an owner, clinically important disease is almost always present.
Clarke and Bennett asked the question: does this low rate of clinical signs represent a poor correlation of clinical signs, or is clinical OA in cats associated with other signs than lameness? 5 In their prospective study of 28 cats with OA, designed to identify clinical signs, they found that ability to jump, height of jump, lameness, stiff gait and activity level of cats were signs that clients could recognize that might improve with treatment. 5 Others have reported that cats may present with other signs, such as decreased appetite and grooming, and behavioral change. In general, many cats with orthopedic disease are unlikely to come into the clinic for a classic lameness, as seen in dogs; however, when a lame cat is observed by an owner, clinically important disease is almost always present.
It is appropriate to ask owners about a decrease in activities: walking, running, ability to jump up/down, grooming, playing with other pets, chasing objects and playing with toys.
Client questionnaires have begun to be utilized in veterinary medicine based on work undertaken in human medicine, with the premise that a validated, short, simple questionnaire would be able to help the clinician identify problems that might not be obvious on routine history, and would provide a tool to monitor results of treatment. Although several of these questionnaires have been developed for use in dogs with orthopedic disease,6–8 a validated questionnaire for the cat has yet to be published. However, a client-specific outcome measure questionnaire used to evaluate cats with OA has been published, 9 and the same research group has also developed a questionnaire designed for validation in cats with OA. 10
Based on this preliminary work, it is appropriate to ask owners about a decrease in activities (walking, running, ability to jump up and down, grooming, playing with other pets, chasing objects and playing with toys), which may indicate a need to look further for possible musculoskeletal disease.
Examination facilities
It is axiomatic in veterinary medicine that for ‘every diagnosis missed by not knowing, ten are missed for not looking’. Just as in other species, orthopedic examination in the cat, when performed in a consistent, structured manner, can yield valuable information regarding the type and extent of disease, and help direct further diagnostics. However, most veterinarians find that orthopedic examination of the dog is much easier: dogs will walk on a leash, are more easily restrained and many dogs will tolerate a longer examination period than will a cat. Additionally, there are logistical concerns. Many veterinarians can relay stories of cats, turned loose for gait analysis, that have found their way into the ceiling, under built-in cabinets, or behind a large mass of computer cables with little enthusiasm for being safely extricated (Figure 1).
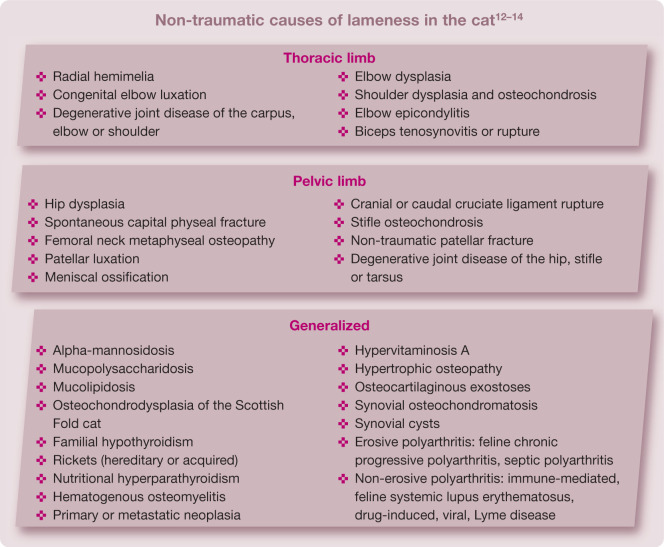
Figure 1.

Cats will naturally seek out the least accessible place to hide – in this case, under a bank of rolling cages. It is well worth testing an examination room on some well-behaved staff cats first, to identify any potential problem areas
The practice should identify an area that is free of such hazards and will allow a cat to roam, off leash, away from other animals and behind closed doors that can stay closed until the examination is complete. When testing an appropriate room in the practice, bring in several well-behaved staff cats first so you can identify any potential problem areas and get an idea of how a cat might explore the room.
Gait analysis
The first portion of the orthopedic examination is devoted to watching the cat walk and, if possible, chase an object or jump.
What is needed
Having an experienced, cat-savvy veterinary technician or nurse assisting with the examination is important for obtaining good results, and blocking out enough time to allow an unhurried examination is essential. In addition to the examination table/counter top and any chairs in the room, it may be helpful to have a small ‘obstacle course’ to encourage jumping, comprising a few lower objects (ie, no more than about 12 inches/30 cm high), such as a closed box or footstool. Requesting that the owner bring along a few cat toys, particularly objects the cat likes to chase, can help to distract or motivate an anxious cat.
What to do
Many cats will venture out of an open carrier placed on the floor if given a few minutes to acclimate. Failing this, the cat may be gently removed after detaching the top from the carrier and placed in the middle of the floor. The reassembled carrier should be placed as far away as possible, door open but with the assistant at the ready to prevent re-entry, as the cat may well decide that the carrier is the best place to hide.
The first few steps of the examination may be revealing, and for cats with profound musculoskeletal disease that are unwilling to take more than a few steps, will demonstrate at the very least whether they have a thoracic limb or pelvic limb lameness (see video 1, DOI: 10.1177/1098612X11432822), or possibly signs of neurologic disease such as ataxia or weakness.
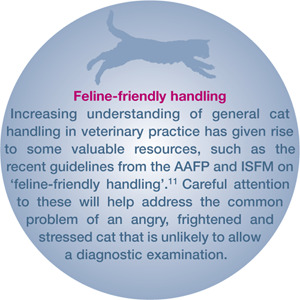
For a cat that is reluctant but able to move about the room, enticement with a toy or laser pointer can be surprisingly effective, even in a hospital setting (Figure 2). Although the personality and disposition of the cat may dictate to some degree whether or not it attempts to jump on and off objects in the examination room, the ability to easily navigate such obstacles may help rule out important musculoskeletal and neurologic (spinal or vestibular) disease.
Figure 2.
One-year-old domestic shorthair cat chasing a laser pointer during the gait analysis portion of the orthopedic examination
It may be possible to evaluate stride length and compare joint flexion and extension angles while the cat is walking or navigating obstacles (eg, cavaletti poles – see video 2, DOI: 10.1177/1098612X11432822), and detect a difference between right and left limbs. Videotaping the examination and playback in loop or slow motion will assist in this process.
What to look for
Cats may unload or favor a painful limb, even at rest (Figure 3), and in some cases observation of the cat sitting or lying in a ‘sphinx’ position may demonstrate asymmetry or an inability to completely flex the hock, stifle, hip or elbow.
A cat with unilateral thoracic limb lameness may have a noticeable ‘head bob’, as seen in the dog, with the head going ‘down on the sound’ limb and up (thereby decreasing the load) on the affected limb.
Cats with bilateral thoracic limb or pelvic limb lameness may take short, choppy steps with the affected limbs, and shift weight forward onto the thoracic limbs for pelvic limb lameness and back towards the pelvic limbs in the case of thoracic limb lameness.
Cats with unilateral pelvic limb lameness may have a hip hike (the hip will be elevated when the painful leg strikes the ground) or the tail may be used asymmetrically to shift weight towards the more normal side when the cat is in motion.
A unilateral pelvic limb plantigrade stance may be consistent with an Achilles tendon rupture in the cat; 15 a bilateral pelvic limb plantigrade stance may indicate neuromuscular weakness. Further examination will be able to differentiate the two. 16
Figure 3.

Four-year-old domestic shorthair cat with a painful right thoracic limb. The cat is sitting with the weight shifted towards the pelvic limbs, and the right carpus and elbow are slightly flexed as more weight is shifted towards the left thoracic limb
Objective evaluation of lameness in the cat.
One of the difficulties in assessing treatment of feline orthopedic disease is a lack of standardization of gait analysis, and lack of an objective ‘gold standard’ tool, such as the force plate used in many canine studies. Standing pressure mat analysis has been useful for identifying unilateral limb lameness in the cat, but has limited clinical application.17,18 Collar-mounted, accelerometer-based activity monitors are used to objectively monitor activity in cats as a surrogate for mobility and have been successfully used in two studies evaluating response to treatment.9,19 Pressure-sensitive walkway evaluation has been used in clinical evaluation after onychectomy, but to date has not been reported for evaluation of other types of musculoskeletal disorders in client-owned cats.20–22
Although direct observation and palpation is inherently subjective, it is appropriate and worthwhile to record the findings using some type of scoring system.
Although direct observation and palpation is inherently subjective, it is still appropriate and worthwhile to record the findings using some type of scoring system. Morton et al reported a four-point scoring system used for evaluating the cat standing, in motion and on palpation; with a score of 1 reflecting a sound or pain-free cat, and a score of 4 reflecting non-weightbearing on the affected limb or marked pain on gentle manipulation of the limb. 23 Visual analog scores for pain have also been reported in cats with orthopedic disease as part of a study evaluating response to non-steroidal anti-inflammatory drugs. 24
Standing palpation
What is needed
Standing palpation may be undertaken on the floor if the cat is more comfortable, or on an examination table. Generally this is a one-person job, with the technician standing just out of the view of the cat but ready to assist if necessary.
What to do and what to look for
Limb symmetry and spinal palpation
With the cat facing in the same direction as the examiner, the spine and limbs should be palpated for symmetry. The major muscle masses of the thoracic limbs to be compared include the supra- and infraspinatus, the triceps, and the flexors and extensors of the antebrachium. For the pelvic limbs, the hamstrings, quadriceps, cranial tibial muscles and gastrocnemius/soleus group should be compared, and the Achilles tendon palpated with the cat in a weightbearing position. At the same time, the elbows, carpi, stifles and hocks should be compared with regards to diameter and presence or absence of detectable joint effusion.
Spinal conditions often present with gait abnormality or pain that can seem to be musculoskeletal in origin, hence the importance of spinal column palpation. The normal cat should be able to have the neck fully extended with the chin pointing to the ceiling, flexed ventrally until the chin contacts the sternum, and also flexed fully laterally until the nose contacts the side of the thorax bilaterally. The spinal column should be palpated, from ventral for the cranial cervical vertebrae, and dorsally, with firm finger pressure on either side of the dorsal spinous processes, for the thoracic and lumbar spine. A normal cat will tolerate full extension of the tail and lateral motion. It should be kept in mind that lumbosacral disc disease has been reported in the cat and can present with a history of difficulty jumping. 15
Limb joints and segments
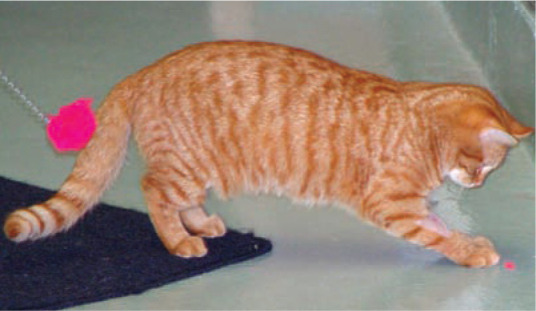
The clinician should next carefully palpate and manipulate each portion of each limb. Attention should be paid to flexion and extension of each joint, palpation of each large muscle mass, and deep palpation of the long bones. Some cats will better tolerate this process if the limbs are slightly suspended above the table by supporting the cat under the thorax with the hand placed around each thoracic limb (Figure 4). Each digit should be flexed and extended, and special attention paid to the pads and digits if the cat has been declawed. Although goniometry is generally not performed at this point (except perhaps in a well-behaved cat, with the help of an assistant to position the goniometer), normal flexion and extension angles for the carpus, elbow, shoulder, tarsus, stifle and hip have been published, along with varus and valgus measurements for the carpi and tarsi, in the sedated and non-sedated cat. 25
Figure 4.

Assessment of elbow extension. Note that the front half of the cat is supported
When performing standing palpation, leave until last the obvious painful area, as determined either from the history or from observations made during gait analysis.
When palpating the pelvic limbs, many normal cats will mildly resent manipulation of the patella as the examiner checks for luxation, and will kick away. Pelvic limb contact with the table may make it difficult to assess the limb. To prevent traction, the examiner may lift the cat up (to palpate the right patella) using the right arm and hand under the thorax of the cat, and rest the abdomen over the examiner’s hip, allowing the outer pelvic limb to fully extend, relaxing the quadriceps mechanism (Figure 5a). The examiner can then attempt medial and lateral luxation of the patella using the left hand. The cat can be switched to the examiner’s other side to palpate the left patella (Figure 5b). As for the dog, a grade I (grade A) 26 luxation is defined as luxation that occurs when manual pressure is applied to the patella with the limb in extension, with spontaneous reduction when the patella is released. Contrary to the dog, grade I (grade A) patellar luxation may be normal in the cat. 27 (For further discussion, see the accompanying article in this special issue by Grierson.) 26
Figure 5.
(a) Cat supported with the right limb suspended to allow palpation of the right patella. (b) Cat switched to examiner’s opposite hip to allow manipulation of the left patella
Hips
When examining the hip, the examiner should remember to perform abduction in addition to flexion, extension and rotation. Although normal abduction angles in the cat have not been reported, in the author’s experience most cats can easily obtain 90° of pain-free abduction, similar to dogs. Furthermore, cats with OA of the hip resent hip abduction, sometimes more so than flexion and extension.
Postural reactions and hopping
It may also be appropriate at this time to attempt postural reaction testing if there is any possibility of neurologic involvement. While testing of knuckling can be valuable to assess proprioception in cats, the author has found that it can be falsely normal even in cats with fairly profound neurologic disease, so normal knuckling responses should not be assumed to rule out neurologic disease. Hopping should always be included in the examination if there is any suspicion of neurologic disease based on the history or gait analysis. It should be kept in mind that cats with painful limbs may be reluctant to fully bear weight, and so orthopedic disease can also affect their ability to hop.
Palpation in lateral recumbency
At this stage of the assessment, the veterinary technician should step in and gently assist with restraint, as many cats resent being held in lateral recumbency. The examiner will now have the opportunity to visually examine the claws and digits from a better perspective and with a little more control than during the standing examination. Essentially, the examination that was undertaken with the cat standing should be repeated, with emphasis placed on performing some of the maneuvers that cannot be done during the standing examination; in particular, assessment of the cranial drawer test (Figure 6), the Ortolani sign and, if possible, measurement of joint angles as referred to above.
Figure 6.
Assessment of stifle instability (cranial drawer test) in the unsedated cat. Note the location of the examiner and the hand placement
Sedated examination.
In the author’s practice, sedated examination is considered very valuable in the cat, and tends to be performed as a standard part of the examination unless the cat is either very well behaved and patient, or other medical conditions preclude it. The goal is not to achieve a surgical plane of sedation, but merely to facilitate restraint. This is particularly useful in a fractious cat that is difficult to examine while awake, but can still give a pain response (pulls the limb away, turns or vocalizes) when a diseased area is encountered (Figure 7), but does not respond to palpation of non-painful areas.
Figure 7.

Abnormal appearance of the nail bed in an adult domestic shorthair cat presenting with a forelimb lameness of several months duration. Digit amputation and biopsy revealed squamous cell carcinoma
Specific sedation protocols are beyond the scope of this article, but there are many good options dependent on the signalment and general health of the cat. 2 For healthy, young to middle-aged cats, the author would commonly use a combination of glycopyrrolate (0.011 mg/kg) combined with butorphanol (0.4 mg/kg) given intramuscularly, followed about 10 minutes later with intramuscular dexmedetomidine (5–20 µg/kg) and reversed with atipamezole as needed or on completion of the examination.
The clinician should carefully screen for heart murmurs prior to sedation – they have been found to be present in up to 10% of cats presenting for orthopedic examination at the author’s institution. Ideally, sedation should allow for more thorough examination, and be followed immediately by imaging diagnostics and, if indicated, arthrocentesis.
Cranial drawer test
Cranial drawer motion is assessed in the same way as in the dog. The examiner generally stands behind the cat, and places the right hand with the forefinger on the cranial surface of the patella, and the thumb gently parallel to the plane of the fabellae on the caudal aspect of the joint. The left hand is placed with the forefinger on the cranial surface of the tibial tuberosity, and the thumb just caudal to the fibular head (Figure 6). The femur is stabilized with the stifle joint in a standing angle, and the examiner attempts to move the tibia cranially (or caudally, an isolated caudal cruciate tear can occur in the cat although a cranial cruciate tear is more common). Although a very slight amount of ‘drawer’ motion may be present, the stifle should be stable during this maneuver. The test should be repeated with the stifle in mid-flexion and mid-extension as well.
Common mistakes in attempting to perform this test include incorrect hand placement, failure to test with the stifle in the proper angle, and failure to repeat after sedation if initial results are inconclusive or cannot be obtained. In animals with a history of trauma, varus and valgus evaluation is very important as stifle luxation, involving rupture of one or both collateral ligaments in addition to one or both cruciate ligaments, seems to be more common in the cat than in the dog.
Ortolani sign
The Ortolani sign is an indicator of excessive hip joint laxity, which may be seen in young cats (definitive ages not reported but likely less than 2 years old) with hip dysplasia. To perform the test, the cat may be examined either on its side or back. With the examiner standing behind the cat, one hand is placed over the spine (away from the hip), while the stifle and hip are each aligned at about 90° of flexion. While gently lifting up the femur at the level of the stifle with the left hand, pressure is applied up the shaft of the femur in an attempt to subluxate the hip. At the same time, the limb is abducted away from the midline of the body, and the examiner looks for evidence of relocation of the femoral head in its normal position (ie, a palpable, visual or audible click or pop as the hip reduces into its normal position). As in the dog, cats with hip pain will resent this test and may be able to overcome it using muscular forces, so repeating the maneuver after sedation may be indicated.
Thoracic limb assessment
No special maneuvers are required for the thoracic limb; however, the examiner should take advantage of lateral recumbency to check varus/valgus as well as to repeat flexion and extension of the carpus, elbow and shoulder. OA commonly affects the elbow joint, so recording of any thickening, crepitus, loss of range of motion and possible pain on internal or external rotation is an important part of the examination. Although classic brachial plexus tumors are very rarely reported in the cat, the examiner should still take the time to palpate the axillary region for masses, as well as looking for muscle atrophy, decreased/absent cutaneous sensation, ipsilateral Horner’s syndrome, lack of ipsilateral cutaneous trunci reflex, pain or enlarged lymph nodes that may require further diagnostic investigation.
Key points
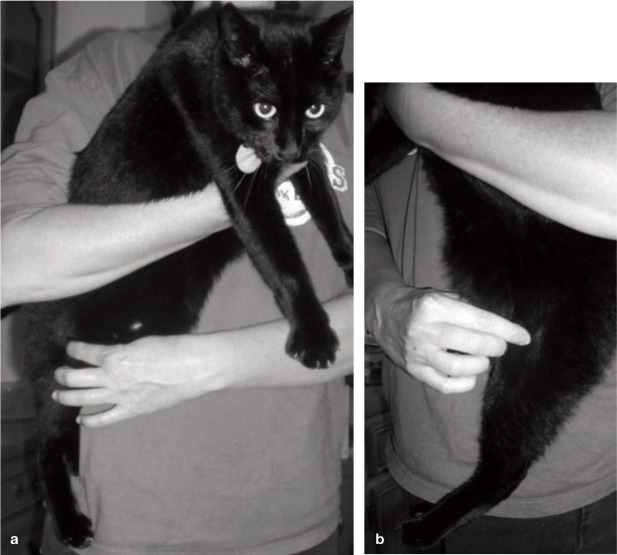
Utilize the recently published AAFP/ISFM guidelines on feline-friendly handling to facilitate a positive environment.
Identify a ‘cat safe’ room in the practice where the examination can be conducted.
Do most of the examination with minimal to no restraint, with the cat standing.
Don’t forget to assess the spine and look for neurologic disease.
Utilize appropriate sedation as a regular part of the examination.
Don’t rush the examination.
Funding
The author received no specific grant from any funding agency in the public, commercial or not-for-profit sectors for the preparation of this review article.
Conflict of interest
The author declares that there is no conflict of interest.
References
- 1. Hardie E, Roe S, Martin F. Radiographic evidence of degenerative joint disease in geriatric cats: 100 cases (1994–1997). J Am Vet Med Assoc 2002; 220: 628–32. [DOI] [PubMed] [Google Scholar]
- 2. Lascelles B. Cross-sectional study evaluating the prevalence of radiographic degenerative joint disease in domesticated cats. Vet Surg 2010; 39: 535–44. [DOI] [PubMed] [Google Scholar]
- 3. Godfrey D. Osteoarthritis in cats: a retrospective radiological study. J Small Anim Pract 2005; 46: 425–29. [DOI] [PubMed] [Google Scholar]
- 4. Clarke S, Mellor D, Clements D, et al. Prevalence of radiographic signs of degenerative joint disease in a hospital population of cats. Vet Rec 2005; 157: 793–99. [DOI] [PubMed] [Google Scholar]
- 5. Clarke S, Bennett D. Feline osteoarthritis: a prospective study of 28 cases. J Small Anim Pract 2006; 47: 439–45. [DOI] [PubMed] [Google Scholar]
- 6. Hudson JT, Slater MR, Taylor L, Scott MS, Kerwin S. Assessing repeatability and validity of a visual analogue scale questionnaire for use in assessing pain and lameness in dogs. Am J Vet Res 2004; 65: 1634–43. [DOI] [PubMed] [Google Scholar]
- 7. Wiseman-Orr ML, Scott M, Reid J, Nolan AM. Validation of a structured questionnaire as an instrument to measure chronic pain in dogs on the basis of effects on health-related quality of life. Am J Vet Res 2006; 67: 1826–36. [DOI] [PubMed] [Google Scholar]
- 8. Hielm-Bjorkman AK, Rita H, Tulamo R. Pyschometric testing of the Helsinki chronic pain index by completion of a questionnaire in Finnish by owners of dogs with chronic signs of pain caused by osteoarthritis. Am J Vet Res 2009; 70: 727–34. [DOI] [PubMed] [Google Scholar]
- 9. Lascelles B, Hansen B, Roe S, et al. Evaluation of client-specific outcome measures and activity monitoring to measure pain relief in cats with osteoarthritis. J Vet Intern Med 2007; 21: 410–16. [DOI] [PubMed] [Google Scholar]
- 10. Zamprogno H, Hansen BD, Bondell HD, et al. Item generation and design testing of a questionnaire to assess degenerative joint disease-associated pain in cats. Am J Vet Res 2010; 71: 1417–24. [DOI] [PubMed] [Google Scholar]
- 11. Rodan I, Sundahl E, Carney H, et al. AAFP and ISFM feline-friendly handling guidelines. J Feline Med Surg 2011; 13: 364–75. (Also available at www.catvets.com and www.isfm.net ) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hubler M, Arnold S, Langley-Hobbs SJ. Hereditary and congenital musculoskeletal diseases. In: Montavon PM, Voss K, Langley-Hobbs SJ, eds. Feline orthopedic surgery and musculoskeletal disease. Edinburgh: Saunders Elsevier; 2009: 41–54. [Google Scholar]
- 13. Voss K. Diseases of bone. In: Montavon PM, Voss K, Langley-Hobbs SJ, eds. Feline orthopedic surgery and musculoskeletal disease. Edinburgh: Saunders Elsevier; 2009: 55–62. [Google Scholar]
- 14. Voss K, Langley-Hobbs S. Diseases of joints. In: Montavon PM, Voss K, Langley-Hobbs SJ, eds. Feline orthopedic surgery and musculoskeletal disease. Edinburgh: Saunders Elsevier; 2009: 63–74. [Google Scholar]
- 15. Harris JE, Dhupa S. Lumbosacral intervertebral disk disease in six cats. J Am Anim Hosp Assoc 2008; 44: 109–15. [DOI] [PubMed] [Google Scholar]
- 16. Mizisin AP, Shelton GD, Burgers ML, Powell HC, Cuddon PA. Neurological complications associated with spontaneously occurring feline diabetes mellitus. J Neuropathol Exp Neurol 2002; 61: 872–84. [DOI] [PubMed] [Google Scholar]
- 17. Carroll G, Howe L, Peterson K. Analgesic efficacy of preoperative adminstration of meloxicam or butorphanol in onychectomized cats. J Am Vet Med Assoc 2005; 226: 913–19. [DOI] [PubMed] [Google Scholar]
- 18. Carroll G, Narbe R, Peterson K, Kerwin S, Taylor L, DeBoer M. A pilot study: sodium urate synovitis as an acute model of inflammatory response using objective and subjective criteria to evaluate arthritic pain. J Vet Pharmacol Ther 2008; 31: 456–65. [DOI] [PubMed] [Google Scholar]
- 19. Lascelles B, DePuy V, Thomson A, et al. Evaluation of a therapeutic diet for feline degenerative joint disease. J Vet Intern Med 2010; 24: 487–95. [DOI] [PubMed] [Google Scholar]
- 20. Lascelles B, Findley K, Correa M, Marcellin-Little D, Roe S. Kinetic evaluation of normal walking and jumping in cats, using a pressure-sensitive walkway. Vet Rec 2007; 160: 512–16. [DOI] [PubMed] [Google Scholar]
- 21. Romans C, Conzemius M, Horstman C, Gordon W, Evans R. Use of pressure platform gait analysis in cats with and without bilateral onychectomy. Am J Vet Res 2004; 65: 1276–78. [DOI] [PubMed] [Google Scholar]
- 22. Robinson DA, Romans C, Gordon-Evans WJ, Evans RB, Conzemius M. Evaluation of short-term limb function following unilateral carbon dioxide laser or scalpel onychectomy in cats. J Am Vet Med Assoc 2007; 230: 353–58. [DOI] [PubMed] [Google Scholar]
- 23. Morton CM, Grant D, Johnston L, Letellier IM, Narbe R. Clinical evaluation of meloxicam versus ketoprofen in cats suffering from painful acute locomotor disorders. J Feline Med Surg 2011; 13: 237–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Murison PJ, Tacke S, Wondratschek C, et al. Postoperative analgesic efficacy of meloxicam compared to tolfenamic acid in cats undergoing orthopaedic surgery. J Small Anim Pract 2010; 51: 526–32. [DOI] [PubMed] [Google Scholar]
- 25. Jaeger G, Marcellin-Little D, DePuy V, Lascelles B. Validity of goniometric joint measurements in cats. Am J Vet Res 2007; 68: 822–26. [DOI] [PubMed] [Google Scholar]
- 26. Grierson J. Hips, elbows and stifles. Common joint diseases in the cat. J Feline Med Surg 2012; 14: 23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Loughin C, Kerwin S, Hosgood G, et al. Clinical signs and results of treatment in cats with patellar luxation: 42 cases (1992–2002). J Am Vet Med Assoc 2006; 228: 1370–75. [DOI] [PubMed] [Google Scholar]