Abstract
Overview:
The availability of blood components has increased the number of indications for transfusing cats, and fresh whole blood is readily accessible to clinicians because it can be taken from in-house donor cats or ‘volunteer’ feline blood donors. A certain amount of risk remains to the recipient cat, as immediate or delayed adverse reactions can occur during or after transfusion, related to immunemediated mechanisms. This article, however, focuses on adverse events caused by infectious agents, which may originate either from contamination of blood following incorrect collection, storage or transfusion, or from transfusion of contaminated blood obtained from an infected donor.
Prevention of blood contamination:
In cats, blood cannot be collected through a closed system and, therefore, collection of donor blood requires a multi-step manipulation of syringes and other devices. It is crucial that each step of the procedure is performed under the strictest aseptic conditions and that bacterial contamination of blood bags is prevented, as bacterial endotoxins can cause an immediate febrile reaction or even fatal shock in the recipient cat.
Prevention of disease transmission:
With a view to preventing transmission of blood-borne infectious diseases, the American College of Veterinary Internal Medicine has adopted basic criteria for selecting pathogens to be tested for in donor pets. The worldwide core screening panel for donor cats includes feline leukaemia virus, feline immunodeficiency virus, Bartonella species and feline haemoplasma. The list should be adapted to the local epidemiological situation concerning other vector-borne feline infections. The most practical, rapid and inexpensive measure to reduce transfusion risk is to check the risk profile of donor cats on the basis of a written questionnaire. Blood transfusion can never, however, be considered entirely safe.
Introduction
Over recent decades, small animal transfusion medicine has made significant progress, contributing to the development of emergency medicine and critical care. The availability of blood components has increased the number of indications for transfusing cats and dogs, even if the evidence-based benefit is still lacking in certain cases. 1
Fresh whole blood is readily available to clinicians because it can be taken from in-house donor cats or ‘volunteer’ feline blood donors. Thanks to the commercial availability of in-house typing kits and gel cross-match systems for cats, blood transfusion in veterinary practice has become safer and more accessible. 2 However, blood transfusion implies a certain amount of risk to the recipient cat and, to some extent, the donor cat as well, which is subjected to an invasive procedure requiring sedation. 3 These risks always need to be carefully weighed against the achievable benefits. In terminal patients, blood transfusion should be avoided and other treatment options considered. 4 Surprisingly, blood transfusion did not reduce the risk of 30-day mortality in humans in a critical care setting in one multi-centre, randomised controlled study. 5
Immediate or delayed adverse reactions can occur during or after transfusion, related to immune-mediated mechanisms. The severity of these reactions varies from a mild febrile reaction to a severe, life-threatening circulatory overload or haemolytic crisis. The prevention of this risk is not the objective of these guidelines, and guidance is provided elsewhere.1,2,4,6 –10
This guideline article focuses on the prevention of transmission of infectious disease related to blood transfusion in cats. Adverse events caused by infectious agents may originate from: contamination of blood following incorrect collection, storage or transfusion; or transfusion of contaminated blood obtained from an infected donor.
Prevention of contamination of donor blood
The blood collection procedure in cats is associated with a greater risk of contamination than in dogs or humans. In cats, blood cannot be collected through a closed system, and therefore a multi-step manipulation of syringes and other devices is required, with the help of several assistants. This increases the risk of contamination. In general, 50 ml of blood is collected from donor cats using three (20 ml) or five (10 ml) different syringes, each containing the appropriate quantity of anticoagulant obtained from a human blood collection bag. 4 Usually, a T-connector and a three-way tap connect the intravenous (IV) needle to the syringes, which are filled with blood and then gently rotated by an assistant. The blood collected into the syringes is then immediately transferred into a single, plain blood collection bag through the injection port (Figure 1). Finally, blood is transfused through a giving set which is inserted into another port of the bag at the time of the transfusion procedure.
Figure 1.
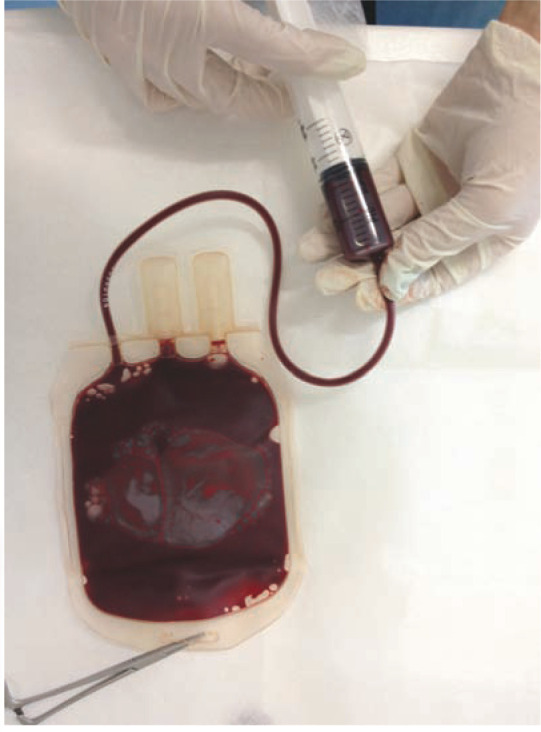
Transfer of blood collected with syringes into a single, plain blood collection bag through the injection port. Courtesy of Eva Spada, University of Milan, Milan, Italy
It is crucial that each step of the process is performed under the strictest aseptic conditions, even in an emergency. 11 The disposable equipment should be placed on sterile surfaces, and staff should wear sterile gloves and masks. Each syringe should be immediately sealed with its capped needle, both after adding the anticoagulant and after collecting the blood until it is transferred into the bag. Surgical preparation of the ventral neck of the donor is necessary. The longer the delay between blood collection and transfusion, the higher the risk of contamination of the collected blood. Collected blood should be stored at 4°C. However, the blood bag should not be stored once the giving set has been inserted.
Similar principles apply in the case of autologous transfusion, a procedure reported in dogs in emergency situations such as for treatment of haemothorax or haemoperitoneum. Here, blood is collected from the body cavity using cell salvage devices and transfused after appropriate washing.10,12
Bacterial contamination of blood bags can cause an immediate febrile reaction in the recipient if bacterial endotoxins are produced by cold-growing gram-negative bacteria, such as Pseudomonas species, or coliforms, such as Serratia marcescens. The latter microorganism has been isolated from contaminated feline blood bags and from transfused cats that presented with fever, vomiting, diarrhoea, jaundice and even death. 13 Fatal endotoxin-related shock is the most dangerous consequence in such cases.
Blood bags should be visually inspected before use and discarded if there is any suspected change in colour or other visible abnormality. 14
Prevention of transmission of blood-borne infectious diseases
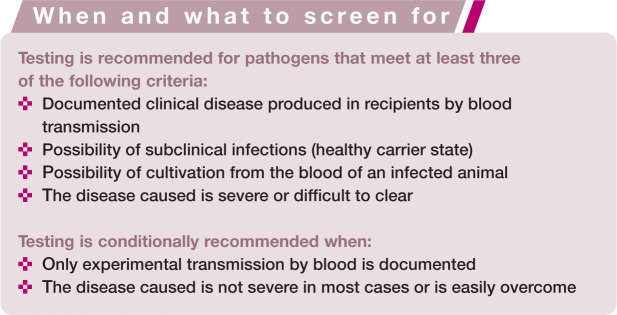
Information on feline blood-borne infectious agents is becoming increasingly available, in particular in relation to vector-borne pathogens.15,16 In 2005, in a consensus statement on canine and feline blood donor screening for infectious diseases, the American College of Veterinary Internal Medicine (ACVIM) adopted basic criteria for selecting pathogens to be tested for in donor pets. 14 Testing is recommended for pathogens in certain circumstances, as highlighted in the box below.
In line with these criteria, the worldwide core screening panel for donor cats (Table 1) includes: feline leukaemia virus (FeLV), feline immunodeficiency virus (FIV), Bartonella species and feline haemoplasma.14,21,22 However, the list of pathogens to be tested in donor cats should be adapted to the local epidemiological situation. 23 Other infectious agents that may be investigated in endemic areas are listed in Table 2.
Table 1.
Core pathogens for worldwide screening of candidate blood donors
| Pathogen | Diagnostic tests |
|---|---|
| Feline leukaemia virus (FeLV) | FeLV provirus PCR*† |
| Feline immunodeficiency virus (FIV) | Rapid anti-FIV antibody test on blood serum/plasma* |
| Mycoplasma haemofelis | Blood PCR |
| Candidatus Mycoplasma haemominutum | |
| Candidatus Mycoplasma turicensis | |
| Bartonella species | Anti-Bartonella antibodies (IFAT) and/or blood PCR |
For more information on these pathogens, see Hosie et al, 17 Lutz et al, 18 Pennisi et al 19 and Willi et al. 20 PCR = polymerase chain reaction; IFAT = immunofluorescence antibody test
Tests for anti-FIV antibodies and FeLV DNA should be confirmed negative at least 3 months after the last exposure
In life-threatening emergency situations, donors can be screened using rapid FeLV antigen tests, but owners should be informed about the higher risk
Table 2.
Pathogens to be considered for screening of candidate blood donors based on local epidemiological information
| Pathogen | Diagnostic tests |
|---|---|
| Cytauxzoon felis | Blood PCR in endemic areas |
| Babesia species | Blood PCR in endemic areas* |
| Leishmania infantum | Blood PCR in endemic areas |
| Ehrlichia species | Blood PCR in endemic areas* |
| Anaplasma phagocytophilum | Anti-A phagocytophilum antibodies (IFAT) and blood PCR in endemic areas |
Two common feline infectious agents – Toxoplasma gondii and feline coronavirus (FCoV) – do not meet the ACVIM criteria and are not included in donor screening panels. 14 The presence of antibodies against FCoV in blood products may passively immunise transfused cats. In the case of contact with the virus in the weeks following transfusion, these cats could be exposed to the risk of antibody-dependent enhancement of macrophage infection.27,28 Although there have been no reports of feline infectious peritonitis (FIP) following blood transfusion in cats, FCoV-antibody negative blood bank donors are preferred.
Although Rickettsia felis and Rickettsia of the other spotted fever group can infect cats, the organisms have never been detected by molecular methods in cat blood. At present, there is no indication for testing cats for these pathogens. 29
The risk of transmission of pathogens associated with xenotransfusion (transfusion of blood obtained from a different animal species, usually dogs) is theoretically zero for FIV, FeLV and feline haemoplasmas but may be relevant for vector-borne infections, some of which are more common in dogs than in cats. 30 Xenotransfusion should be restricted to exceptional circumstances (eg, emergencies in the event of lack of compatible feline blood or oxygen carrier solution), as it is associated with delayed immune-mediated haemolysis and a very short life span of the transfused erythrocytes. 31
Molecular techniques have significantly increased the sensitivity and specificity of diagnostic testing for the detection of feline blood-borne agents, and their use has increased the safety of blood products. Healthy cats that test negative for FeLV p27 antigenaemia can still harbour provirus integrated in their DNA, which means their blood can transmit FeLV infection to transfused cats. 18 Blood bank donors should, therefore, be tested for FeLV provirus using PCR. In life-threatening emergency situations, transfusions from donors can be screened using rapid FeLV antigen tests, but owners should be informed about the risk.
The screening of blood donors is also influenced by costs. In human medicine, individual blood units are usually tested for several pathogens of major concern (eg, HIV, hepatitis B, hepatitis C, Treponema pallidum); while, for cost reasons, no testing is done for other transmissible blood-borne agents from healthy carriers (Cytomegalovirus, West Nile virus, prions, Leishmania, etc). The preliminary selection of potential human donors is based on history and a risk assessment related to history of travel, sexual behaviour and certain medical procedures.
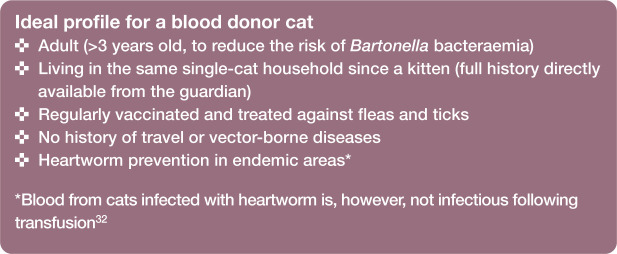
This is also true in the veterinary field; the most useful, practical, rapid and inexpensive measure to reduce transfusion risk is to check the risk profile of donor cats prior to transfusion, on the basis of a written questionnaire completed by the guardian of the donor cat (see box on page 591). This questionnaire can be presented at the time of obtaining informed consent for blood donation. The ideal low-risk profile of a donor cat is described below.
Risk should be reassessed prior to each transfusion. Risk assessment may eliminate the need to repeat expensive and time-consuming screening for blood-borne pathogens in cats with low-risk profiles. The required frequency of testing varies according to the pathogen (seasonal exposure or not) and the individual recipient’s risk of acquiring the infection. The ABCD does not recommend the use of closed colony donors, which are cats specifically bred for blood banks, as it is preferable from a welfare perspective for cats to live in a more natural environment.
If no feline blood is available from a blood bank, veterinary practitioners should be able to rely on an adequate number of pre-selected potential donors evaluated as being low-risk cats and negative for blood-borne pathogens of interest. Free-roaming cats should never be considered as potential donors. Shelter cats can potentially be considered, dependent on their history and the quality of management of the shelter. Physical examination performed after history taking should include an accurate observation and combing of the coat to exclude the presence of fleas and ticks. Cats with fleas or ticks should not be considered as donors. 14
Occasional donors recruited in emergency settings always reduce the level of safety of blood transfusion. The need to find a compatible blood donor rapidly may lead to the neglect of important requirements in terms of donor health. Moreover, only in-house tests can be used for assessing donors in emergency cases, which implies they will be screened only for retroviral infections following a physical examination, complete blood count (CBC), biochemical profile and urinalysis. Where this approach is used, records of the donor and recipient cats should be taken; additionally an EDTA blood sample from the donor should be kept (can be the same tube and sample as taken for CBC), stored frozen at −20°C, for possible further investigations.
Other uses of blood products in practice
Topical application of blood serum is used empirically as anticollagenolytic treatment in the medical management of deep corneal ulcers (Figure 2).33,34 The autologous preparation is cheap to prepare and easy to administer in practice but strict aseptic conditions are required, as described above for the collection of blood. Sterile disposables (tube, pipette, eye dropper bottle) should be used to prevent bacterial contamination. The preparation should be stored at 4°C and used as soon as possible (preferably within 48 h) because the high administration frequency (up to once an hour) increases the risk of contamination of the contents of the eye drop bottle. In the case of very young kittens, or when it is impractical to bleed the patient, homologous (feline) or even canine serum may be used. The administration of canine serum reduces the risk of feline pathogen transmission to the ocular mucosa and damaged corneal tissue. 34 In the case of homologous serum, the donor should be carefully selected, respecting the same criteria as apply for blood transfusion. However, as there have been no controlled studies of the efficacy and safety of this therapy in cats, it should not be encouraged.
Figure 2.
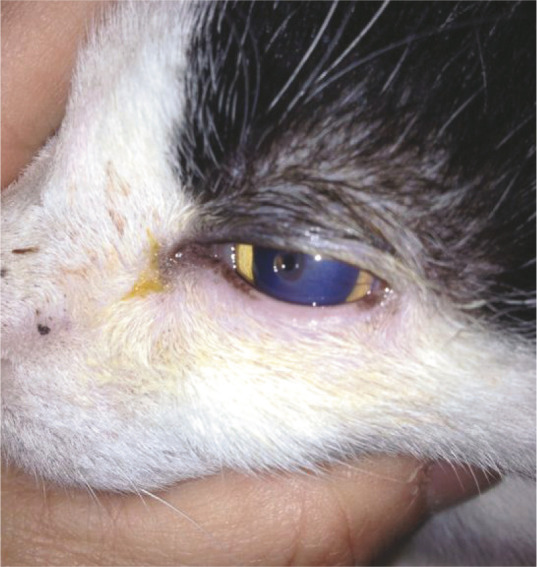
Topical application of autologous blood serum is used empirically as anticollagenolytic treatment in the medical management of corneal lesions, but the procedure requires strict asepsis. Courtesy of Maria Grazia Pennisi, University of Messina, Messina, Italy
Autologous platelet-rich plasma is increasingly used for treating orthopaedic conditions in veterinary practice, including feline practice. The risk of bacterial contamination during preparation of the concentrate must be minimised by strict hygiene. 35
Conclusion
Blood transfusion can be a life-saving treatment with a crucial impact on anaesthetic and surgical possibilities or intensive care, but it can never be considered totally safe. The development of infectious diseases in recipient cats is an iatrogenic risk that must be minimised by the highest standards of clinical veterinary practice. Despite increasing data on blood-borne infections and the availability of more sensitive diagnostic techniques, the risk of transmitting pathogens using the blood of healthy infected carriers cannot be eliminated entirely. The most cost-effective action is to reduce this risk by the pre-selection of low-risk donors.
Key Points
Each step of the blood transfusion procedure should be performed under strict aseptic conditions, even in emergencies.
The longer the delay between blood collection and transfusion, the higher the risk of contamination of the collected blood.
Blood bags should be visually inspected before use and should be discarded if there is any suspicion of change in colour or other visible abnormality.
The core screening panel for donor cats worldwide includes FeLV, FIV, Bartonella species and feline haemoplasma.
Although the onset of FIP following blood transfusion in cats has not been reported, FCoV antibody negative donors are preferred.
The most practical, rapid and inexpensive preventive measure is to assess the risk profile of donor cats.
Risk assessment may eliminate the need for repeating expensive and time-consuming screening for blood-borne pathogens in cats with a low-risk profile.
Free-roaming cats should never be considered as potential donors.
Blood transfusion should be avoided in terminal patients.
Footnotes
Funding: The authors received no specific grant from any funding agency in the public, commercial or not-for-profit sectors for the preparation of this article. The ABCD is supported by Merial, but is a scientifically independent body and its members receive no stipends from Merial.
The authors do not have any potential conflicts of interest to declare.
References
- 1. Davidow B. Transfusion medicine in small animals. Vet Clin Small Anim 2013; 43: 735–756. [DOI] [PubMed] [Google Scholar]
- 2. Rudd S. Feline blood types and blood typing methods. In: Harvey A, Tasker S. (eds). BSAVA manual of feline practice. Quedgeley: BSAVA, 2013, pp 454–456. [Google Scholar]
- 3. Spada E, Proverbio D, Bagnagatti De Giorgi G, et al. Clinical and haematological responses of feline blood donors anaesthetized with a tiletamine and zolazepam combination. J Feline Med Surg 2015; 17: 338–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rudd S. Blood transfusion. In: Harvey A, Tasker S. (eds). BSAVA manual of feline practice. Quedgeley: BSAVA, 2013, pp 456–460. [Google Scholar]
- 5. Hérbert PC, Wells G, Blajchman A, et al. A multicentre, randomized, controlled clinical trial of transfusion requirements in critical care. New Engl J Med 1999; 340: 409–417. [DOI] [PubMed] [Google Scholar]
- 6. Barfield D, Adamantos S. Feline blood transfusions. A pinker shade of pale. J Feline Med Surg 2011; 13: 11–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. BSAVA Scientific Committee. Scientific information document. Blood transfusions. J Small Anim Pract 2000; 41: 431–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Helm J, Knottenbelt C. Blood transfusion in dogs and cats. 1. Indications. In Practice 2010; 32: 184–189. [Google Scholar]
- 9. Helm J, Knottenbelt C. Blood transfusion in dogs and cats. 2. Practicalities of blood collection and administration. In Practice 2010; 32: 231–237. [Google Scholar]
- 10. Kisielewicz C, Self IA. Canine and feline blood transfusions: controversies and recent advances in administration practices. Vet Anaesth Analg 2014; 41: 233–242. [DOI] [PubMed] [Google Scholar]
- 11. FECAVA. FECAVA key recommendations for hygiene and infection control in veterinary practice. http://www.fecava.org/sites/default/files/files/Hygiene%20poster.pdf. 2013.
- 12. Tasker S. Management of haematological disorders. In: Harvey A, Tasker S. (eds). BSAVA manual of feline practice. Quedgeley: BSAVA, 2013, pp 452–454. [Google Scholar]
- 13. Hohenhaus AE, Drusin LM, Garvey MS. Serratia marcescens contamination of feline whole blood in a hospital blood bank. J Am Vet Med Assoc 1997; 210: 794–798. [PubMed] [Google Scholar]
- 14. Wardrop KJ, Reine N, Birkenheuer A, et al. Canine and feline blood donor screening for infectious diseases. J Vet Intern Med 2005; 19: 135–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Beugnet F, Marié J-L. Emerging arthropod-borne diseases of companion animals in Europe. Vet Parasitol 2009; 163: 298–305. [DOI] [PubMed] [Google Scholar]
- 16. Vilhena H, Martinez-Diaz VL, Cardoso L, et al. Feline vector-borne pathogens in the north and centre of Portugal. Parasit Vectors 2013; 6: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hosie MJ, Addie D, Belák S, et al. Feline immunodeficiency. ABCD guidelines on prevention and management. J Feline Med Surg 2009; 11: 575–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lutz H, Addie D, Belák S, et al. Feline leukemia. ABCD guidelines on prevention and treatment. J Feline Med Surg 2009; 11: 565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pennisi MG, Addie D, Belák S, et al. Bartonella species infection in cats: ABCD guidelines on prevention and management. J Feline Med Surg 2013; 15: 563–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Willi B, Boretti FS, Baumgartner C, et al. Prevalence, risk factor analysis, and follow up of infections caused by three feline hemoplasma species in cats in Switzerland. J Clin Microbiol 2006; 44: 961–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Reine NJ. Infection and blood transfusion: a guide to donor screening. Clin Tech Small Anim Pract 2004; 19: 68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gary AT, Richmond HL, Tasker S, et al. Survival of Mycoplasma haemofelis and “Candidatus Mycoplasma haemominutum” in blood of cats used for transfusion. J Feline Med Surg 2006; 8: 321–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hackett TB, Jensen WA, Lehman TL, et al. Prevalence of DNA of Mycoplasma haemofelis, “Candidatus Mycoplasma haemominutum”, Anaplasma phagocytophilum and species of Bartonella, Neorickettsia, and Ehrlichia in cats used as blood donors in the United States. J Am Vet Med Assoc 2006; 229: 700–705. [DOI] [PubMed] [Google Scholar]
- 24. Carli E, Trotta M, Chinelli R, et al. Cytauxzoon sp. infection in the first endemic focus described in domestic cats in Europe. Vet Parasitol 2012; 183: 343–352. [DOI] [PubMed] [Google Scholar]
- 25. Hartmann K, Addie D, Belák S, et al. Babesiosis in cats. ABCD guidelines on prevention and management. J Feline Med Surg 2013; 15: 643–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pennisi MG, Addie D, Belák S, et al. Leishmaniosis in cats. ABCD guidelines on prevention and management. J Feline Med Surg 2013; 15: 638–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Takano T, Kawakami C, Yamada S, et al. Antibody-dependent enhancement occurs upon re-infection with the identical serotype virus in feline infectious peritonitis virus infection. J Vet Med Sci 2008; 70: 1315–1321. [DOI] [PubMed] [Google Scholar]
- 28. Bàlint Á, Farsang A, Szeredi L, et al. Recombinant feline coronaviruses as vaccine candidates confer protection in SPF but not in conventional cats. Vet Microbiol 2014; 169: 154–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lappin MR, Hawley J. Presence of Bartonella species and Rickettsia species DNA in the blood, oral cavity, skin and claw beds of cats in the United States. Vet Dermatol 2009; 20: 509–514. [DOI] [PubMed] [Google Scholar]
- 30. Otranto D, Dantas-Torres F. Canine and feline vector-borne diseases in Italy: current situations and perspectives. Parasit Vectors 2010; 3: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bovens C, Gruffydd-Jones T. Xenotransfusion with canine blood in the feline species: review of the literature. J Feline Med Surg 2013; 15: 62–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lee AC, Atkins CE. Understanding feline heartworm infection: disease, diagnosis and treatment. Top Companion Anim Med 2010; 25: 224–230. [DOI] [PubMed] [Google Scholar]
- 33. Hartley C. Treatment of corneal ulcers. What are the medical options? J Feline Med Surg 2010; 12: 384–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mitchell N. Management of eye disease. In: Harvey A, Tasker S. (eds). BSAVA manual of feline practice. Quedgeley: BSAVA, 2013, pp 335–341. [Google Scholar]
- 35. Hoareau GL, Jandrey KE, Burges J, et al. Comparison of the platelet-rich plasma and buffy coat protocols for preparation of canine platelet concentrates. Vet Clin Pathol 2014; 43: 513–518. [DOI] [PubMed] [Google Scholar]