Abstract
Overview:
Cryptococcosis is worldwide the most common systemic fungal disease in cats; it is caused by the Cryptococcus neoformans– Cryptococcus gattii species complex, which includes eight genotypes and some subtypes (strains) with varying geographical distribution, pathogenicity and antimicrobial susceptibility. Cats acquire the infection from a contaminated environment. The prognosis is favourable in most cases, provided a diagnosis is obtained sufficiently early and prolonged treatment is maintained.
Infection:
Basidiospores are the infectious propagules of Cryptococcus species as they penetrate the respiratory system and induce primary infection. Asymptomatic colonisation of the respiratory tract is more common than clinical disease. Avian guanos, particularly pigeon droppings, offer favourable conditions for the reproduction of C neoformans. Both Cryptococcus species are associated with decaying vegetation.
Disease signs:
Cryptococcosis caused by C neoformans or C gattii is indistinguishable clinically. The disease can present in nasal, central nervous system (which can derive from the nasal form or occur independently), cutaneous and systemic forms.
Diagnosis:
An easy and reliable test for cryptococcosis diagnosis is antigen detection in body fluids. Only isolation and polymerase chain reaction allow identification of the species genotype.
Disease management:
Amphotericin B, ketoconazole, fluconazole and itraconazole have all been used to treat cats. Surgical excision of any nodules in the skin, nasal or oral mucosa assists recovery. Continued treatment is recommended until the antigen test is negative.
Prevention:
Efficient preventive measures have not been demonstrated. Vaccines are not available.
Agent properties
Feline cryptococcosis, discovered over a century ago, is a non-contagious systemic fungal disease acquired from a contaminated environment. For this reason it is not considered a zoonotic disease; animals may serve as sentinel hosts.
Feline cryptococcosis is caused by basidiomycetous yeasts of the genus Cryptococcus belonging to the C neoformans–C gattii complex. A previous classification distinguished five serotypes (A, B, C, D, AD) according to antigenic characteristics of the capsular polysaccharide. 1 The updated nomenclature based also on genotyping differentiates two main species affecting cats: C neoformans – including the varieties C n var grubii (former serotype A) and C n var neoformans (former serotype D) – and C gattii (former serotypes B and C). According to molecular characterisation, isolates from the C neoformans–C gattii complex include eight genotypes and some subtypes (strains) with varying geographical distribution, pathogenicity and antimicrobial susceptibility. 2
Small-size infectious propagules such as basidiospores (<2 µm) and desiccated yeast cells (<3 µm) are easily dispersed by air flow and can penetrate the respiratory system where the primary infection takes place. The fungus can differentiate into several morphological forms including yeast, chlamydospores, pseudohyphae and hyphae under certain conditions, but it is typically present in the yeast form in mammalian hosts, reproducing by mitosis in animal tissues.3,4
Other species that have been rarely reported are C albidus, which may affect immunocompromised cats, and C magnus isolated in cats affected by otitis.5,6
Epidemiology
Cryptococcosis affects humans, cats, dogs, ferrets, horses, goats, sheep, cattle, dolphins, birds, koalas and other marsupials. 1 It has a worldwide distribution and is observed more commonly in cats than in dogs. 7
Unfortunately, Cryptococcus is not usually identified to the species and molecular level with routine diagnostic sampling, and data regarding the feline disease in Europe are from single case reports or small case series, since the disease usually occurs sporadically. 8 Larger retrospective studies are available from Canada, Australia and California.7,9–13
The disease is usually rare or sporadic. However, in 1999, a large-scale outbreak of cryptococcosis caused by C gattii for the first time involved humans, terrestrial (dogs, cats, ferrets, llamas, horses, birds) and marine (porpoises Phocoenoides dalli) animals; it occurred on southern Vancouver Island, British Columbia, Canada in a region characterised by wet, mild winters and dry, warm summers. It is now well known that C gattii has a worldwide distribution with a high prevalence along the Pacific coast of North America. In Europe, it has been reported from Austria, Denmark, France, Germany, Greece, Italy, the Netherlands, Portugal, Spain, Sweden and the United Kingdom. 2 C n var grubii also has a worldwide distribution and is commonly isolated from affected individuals in various animal species. C neoformans is considered a cosmopolitan opportunistic pathogen in human urban populations, whereas C gattii is a true pathogen, more prevalent in rural areas. 1
Environmental exposure and asymptomatic colonisation of the respiratory tract are more common than the clinical disease.14,15 Asymptomatic carriage of C gattii has been recognised in 4.3% of cats, 1.1% of dogs and in 2% of wild animals (squirrels) trapped in British Columbia.10,16
C neoformans ecology is usually related to the presence of avian guanos, particularly pigeon droppings, which offer favourable conditions for the mitotic amplification and reproduction of the fungus, but both Cryptococcus species have been associated with decaying vegetation such as eucalyptus leaves. 17 Pigeons serve as C neoformans carriers, which likely contributes to the worldwide distribution, as they carry Cryptococcus species on their beaks, feathers and legs. 18 Animals, plants, soil and waterways are the sources from where the potential pathogen may be contracted.
Cats are five to six times more likely to be affected by the disease than dogs, and three times more than horses. 7 Retrospective studies of feline cases tended to show a preponderance in males, although this finding was not confirmed in other studies.7,13,19–23 Pedigree breeds such as Ragdoll, Birman, Siamese and Himalayan were considered more often affected than non-pedigree domestic cats but, again, this finding has not been confirmed in more recent studies.7,12,13,20,24 In contrast with other animal species, where usually young adults contract the infection, cats of all ages may be affected.7,20 No seasonal trend in the diagnosis of infection has been observed. 7 Also lifestyle does not seem to be a risk factor – the disease has been reported in indoor cats, too.
Pathogenesis
Cryptococcus is primarily an airborne pathogen, and the nasal cavity is usually the primary site of infection in cats and dogs. In most cases there is only a subclinical colonisation without the invasion of the epithelium. 10 When invasion of mucosal tissues occurs, disease develops locally and/or systemically. In both people and cats, the infection may follow ingestion of desiccated yeast cells or, more rarely, cutaneous inoculation of fungal forms. The incubation period varies from months to years, and the source of infection often remains unknown. The virulence (genotype) and burden of the inhaled organisms influence the outcome of infection. From the upper respiratory tract the infection may spread locally to the central nervous system (CNS) through the ethmoid bone, and rarely also to the lower respiratory tract or systemically. 25
There are temperature-sensitive strains which are unable to grow at temperatures >37.0°C and may cause infections only at body sites where the temperature is lower (skin, nose, scrotum).26,27
Immunity
Antibodies produced against capsular antigens are not protective. Persistent infections can occur because the capsule of cryptococcal yeast forms inhibits phagocytosis, and other virulence factors such as melanin production protect the yeast cells from oxidative damage. The organism is, therefore, able to survive inside phagocytic cells such as macrophages and neutrophils and can be disseminated with these cells.2,24,28
Some studies have suggested that cryptococcosis has a higher prevalence or a less favourable outcome in feline leukaemia virus- or feline immunodeficiency virus-infected cats,19,21 but this conclusion has not been shared by others.12,13,20,29,30 The disease has been reported in cats undergoing chemotherapy or with a concurrent opportunistic infection; hence, a role for immunocompetence cannot be excluded in the pathogenesis of feline cryptococcosis.24,31
Clinical signs
Cryptococcosis caused by C neoformans or C gattii is clinically indistinguishable.
This disease can present in several different clinical forms, including the nasal form, CNS form (which can derive from the nasal form or occur independently), the cutaneous form and the systemic form. Geographical differences in the prevalence of some clinical presentations are postulated as being a consequence of the distribution of genotypes with different virulence. Abnormalities in blood tests are non-specific, if present, showing an inflammatory process.
Nasal form
The nasal form is the most common in cats, presenting as a chronic sinonasal disease, either alone or together with local spread to the skin, subcutis, bones and regional (submandibular) lymph nodes.7,12,20 It induces naso-facial swelling followed by deep non-healing ulceration draining gelatinous exudate, chronic nasal discharge (monolateral or bilateral) with serous, mucopurulent or bloody aspect, stertor and inspiratory dyspnoea, sneezing and snuffling and submandibular lymphadenopathy (Figures 1–3). Anorexia and subsequent weight loss may also be a result of anosmia affecting cats with chronic nasal disease. Cryptococcus is an important differential in cats with chronic nasal discharge, regardless of whether or not facial swelling and/or skin ulceration is present.
Figure 1.
Nasal cryptococcosis: chronic monolateral nasal discharge and mild nasal deformity. Courtesy of Maria Grazia Pennisi
Figure 2.

Cryptococcal disease: severe nasofacial swelling and deformity. Courtesy of Maria Grazia Pennisi
Figure 3.

Cryptococcal disease: ulcerated skin nodules on the face. Courtesy of Maria Grazia Pennisi
In some cases, a fleshy mass may protrude from one or both nostrils. Nasopharyngeal granulomas (resembling polyps or cancer) presenting with stertor, inspiratory dyspnoea and open-mouth breathing have also been described. 32 Proliferative or ulcerated lesions in the oral cavity or pharynx may additionally develop. Otitis media/interna with vestibular signs may occur.33,34 Lower respiratory tract disease may follow and may manifest radiologically as only pulmonary or mediastinal nodules.
CNS form
CNS involvement most likely arises following local dissemination through the cribriform plate; in such cases, sudden blindness due to optical neuritis appears, together with seizure or behavioural changes. In other cases dissemination probably occurs haematogenously and induces granulomatous encephalomyelitis with solitary or multiple lesions.13,35 Many cats show head or spinal pain; other signs of meningeal involvement (hyperaesthesia, nuchal rigidity) are not common. 13
Cutaneous form
Cutaneous forms are characterised by solitary or multiple dermal to subcutaneous nodules in the skin: the former are suggestive of direct inoculation, the latter of haematogenous spread from the primary site of infection. 1 The nodules are usually non-pruritic and not painful, and commonly accompanied by regional lymphadenopathy.
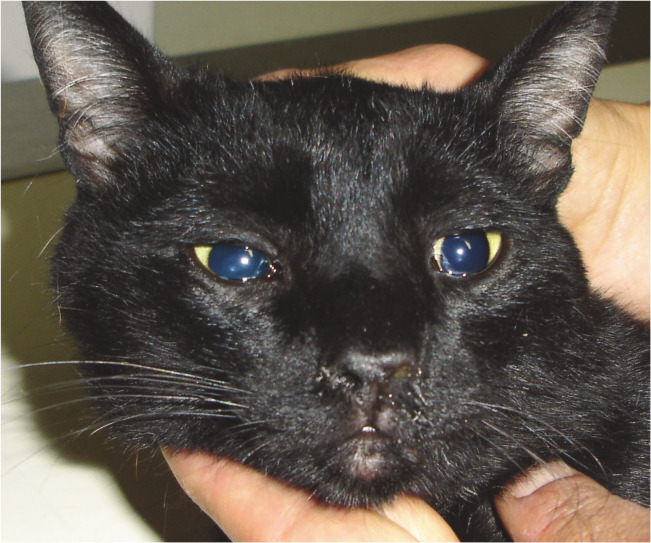
Systemic form
Systemic forms may occur through haematogenous dissemination and manifest with signs of meningoencephalomyelitis (see CNS form), uveitis, chorioretinitis, osteomyelitis and polyarthritis, systemic lymphadenitis or multi-organ involvement, including the kidneys (Figures 4 and 5). Apathy and cachexia appear in cats with severe dissemination during the prolonged chronic course of the disease. The systemic form arising from dissemination may or may not follow classical nasal disease.25,36
Figure 4.

Cryptococcal disease: keratouveitis and cryptococcoma in the anterior chamber. Courtesy of Maria Grazia Pennisi
Figure 5.

Thoracic radiography, ventrodorsal view: diffuse, multiple, poorly defined nodules with blurred margins in the lungs of a cat with systemic cryptococcosis. Courtesy of Maria Grazia Pennisi
Diagnosis
An easy and reliable test for cryptococcosis diagnosis is antigen detection in body fluids. Alternatively, samples can be collected from lesions and submitted for cytology, culture, histopathology and polymerase chain reaction (PCR). These include: pleural or peritoneal effusions; cerebrospinal fluid (CSF); specimens collected from bronchoalveolar lavage; fine needle aspirates from nodules or enlarged lymph nodes; or biopsies taken from any affected tissues.
An increased risk of cerebellar herniation after CSF collection is suspected and this invasive procedure should be considered only when a CNS disease compatible with feline cryptococcosis is not confirmed using other suitable biological samples [EBM grade III]. 13
Isolation and PCR give the opportunity to identify the species and the genotype (PCR only) involved.
Antigen detection
Antigen detection in blood is the test of choice, if available, because it is fast, reliable and minimally invasive. Cryptococcal capsular antigen may be detected by latex cryptococcal antigen agglutination test (LCAT) on serum, CSF or urine. The sensitivity and specificity of the test is improved by pre-treating samples with heat and a proteinase (pronase, often included in commercial diagnostic kits) and is considered good in cats [EBM grade III]. 1 In some cases, false-negative results may occur [EBM grade IV]. 35 If the antigen test is negative, and cryptococcosis is still a possibility, tissue samples should be submitted for cytology, histology and culture. In case of titres <200 a confirmatory cytology, culture or PCR is suggested.
LCAT titre is also an efficient way of monitoring the efficacy of therapy. Treatment is usually continued until a negative LCAT is obtained, but it has been reported that the titre continues to decrease after stopping therapy in cats with clinical resolution but still remains positive [EBM grade III]. 29
Cytology
Cytology can be an easy tool to diagnose cryptococcosis because the appearance of the organisms is characteristic and the number of yeasts in the lesions is usually high; however, a negative result does not exclude the diagnosis. Appropriate cytological samples can be obtained using impression smears from ulcerated skin lesions, fine needle aspirates of nodules, impression smears of biopsy samples or bronchoalveolar lavage fluid or CSF taps. In the case of renal involvement yeast may be seen in the urinary sediment. 37
Smears stained with Romanowsky-type stain (Wright, Diff Quick, Giemsa) may show pink to violet, round or budding extracellular yeasts that vary in size (4–15 µm) and shape and are typically surrounded by a more or less clear, thick halo corresponding to the unstained capsule (Figures 6 and 7). If Gram stain is used, the organism appears Gram- positive with a Gram-negative (pink) capsule. A pyogranulomatous inflammatory pattern is usually seen. Although filamentous forms are not commonly observed in tissues, these atypical morphological forms of C neoformans may be present in cats.26,27
Figure 6.

Diff Quick stained smear of nasal exudate from a cat with C neoformans infection. Note the prominent capsule (clear halo) and narrow-necked budding (arrow). Courtesy of Richard Malik, University of Sydney Veterinary School, Australia
Figure 7.

Diff Quick stained smear of fine needle aspirate of a cryptococcal lesion. Note the enormous capsule surrounding the yeast cells. Courtesy of Mark Krockenberger
Histology
Biopsy samples of nasal mucosa, lymph nodes or skin nodules may be obtained for histology, but they may also provide impression smears for cytology and material for culture and PCR. Haematoxylin-eosin stained sections show eosinophilic bodies surrounded by a clear halo and a pyogranulomatous reaction (Figure 8). Mayer’s mucicarmine method specifically stains the capsule of Cryptococcus. Immunohistochemistry on tissue sections is used for species differentiation, using monoclonal antibodies (Figure 9). 38
Figure 8.
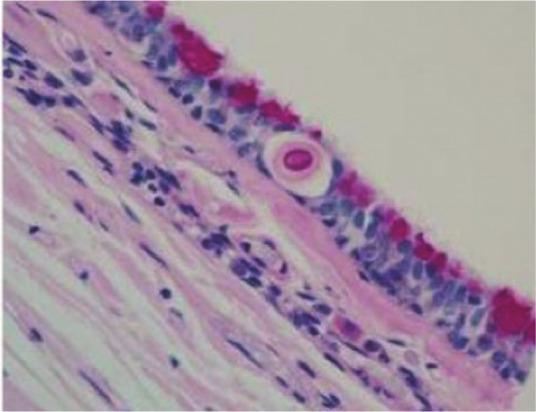
Early invasion of C gattii into the respiratory epithelium of a koala. Note the eosinophilic body surrounded by a clear halo. Courtesy of Mark Krockenberger
Figure 9.
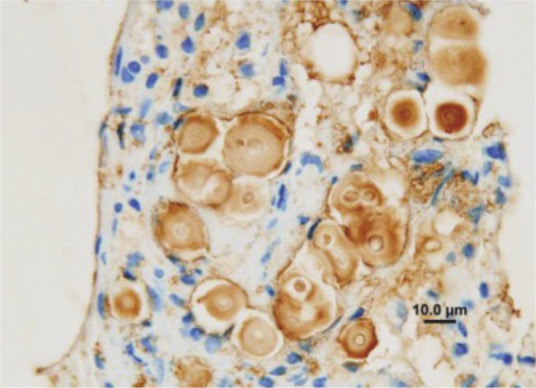
Use of immunohistology to demonstrate C gattii in histological sections. It is possible to conclusively identify Cryptococcus species in paraffin-embedded formalin-fixed tissue sections using monoclonal antibodies directed against different capsular epitopes. These show up as brown precipitates, highlighting both the yeast cell body and its capsule. Note also the narrow neck budding. Courtesy of Mark Krockenberger
Culture
Culture should be performed if the antigen test is negative, when titres are low or absent. Only samples from nasal biopsies should be submitted for culture, because the presence of Cryptococcus in nasal discharge cultures is not considered evidence of disease. Positive culture of biopsy samples and histological changes consistent with infection are considered diagnostic and may be used to test the sensitivity towards antifungal drugs.
Culture of biopsy samples is more sensitive than cytology in confirming infection [EBM grade III]. Cryptococcus is easily isolated in Sabouraud dextrose agar after incubation at 25°C and 37°C for 10 days but also on bacterial standard media. It is now possible to differentiate C neoformans from C gattii by a specific agar test. 2
When samples are contaminated by bacteria, as occurs in nasal secretions, media containing antibiotics are useful. 1
PCR
PCR has been developed for genetic identification in CSF, urine, serum and biopsy samples, but is not used routinely in practice.39–41
Antibody detection
Antibody detection is not a diagnostic tool because it cannot distinguish subclinical infection from disease.
Diagnostic imaging
Advanced diagnostic imaging techniques (CT and MRI) are frequently used in the evaluation of chronic nasal and CNS signs. Abnormal findings in feline cryptococcosis are the presence of chronic rhinitis, frontal sinusitis and/or intranasal or intracranial focal solitary or multifocal masses or fluid-filled lesions [EBM grade III]. 13 Confirmation of diagnosis is not possible by imaging alone, but resolution of a mass lesion can be followed up by MRI in cats under medical therapy.42,43 MRI findings may also include meningeal enhancement, and optic nerve and cribriform plate involvement. 13
Prognosis
The prognosis is favourable in most cases, provided the diagnosis is obtained sufficiently early (before dissemination or before the development of irreversible lesions) and patients and owners comply with a long course of treatment (months) and follow-up (years).
Although information on outcomes is quite limited, it seems that cats have a more favourable prognosis than dogs or horses, which more frequently develop lower respiratory, disseminated and neurological disease with associated higher mortality [EBM grade III].7,11,13,29
In one retrospective study, disease severity did not influence outcome, although the presence of CNS involvement had a significantly adverse impact on the outcome of therapy [EBM grade III]. 29 By contrast, alteration of the mental status was the only negative prognostic factor in a retrospective study on cats with the CNS form of cryptococcosis, and complete recovery was also documented in cats with a CNS form [EBM grade III].13,43
Treatment
No prospective controlled studies exist on the treatment of feline cryptococcosis and all data are based on retrospective studies and case reports. Treatment guidelines have not been established and the choice of appropriate antifungal drug depends on many factors. Owner compliance is crucial, because of the high costs in terms of both money and time commitment required for treatment.
Some retrospective studies on treatment outcomes in feline cryptococcosis have been reported, using a variety of criteria for evaluating the success of therapy.21,44,45 In the largest retrospective study performed on 59 cats, 68% had a successful outcome [EBM grade III]. 29 Most of them needed one single course of therapy of several months (1–24) duration and few cats received a second course of therapy because of clinical recurrence or raised LCAT titre. According to a more recent retrospective study, the clinical outcome may be favourable in approximately two-thirds of treated cats [EBM grade III]. 7 Most recovered cats were presented with sinonasal or single skin, subcutis or intestinal lesions, and the ones that did not recover had CNS or disseminated disease.
Amphotericin B, ketoconazole, fluconazole and itraconazole have all been used to treat cats. With regard to the effect of different therapeutic protocols, there was no significant difference in outcome between cats treated with amphotericin B-containing protocols and those treated with azole monotherapy using fluconazole or itraconazole [EBM grade III]. 29
The median cumulative dose of amphotericin B for cats cured at the first attempt was 16 mg/kg (range 7–23 mg/kg). This was higher than the previously recommended cumulative dose of 4–8 mg/kg. The median duration of treatment for fluconazole-treated cats was significantly shorter (4 months; range 1–8 months) than the median for the itraconazole group (9 months; range 3–24 months). Liposomal formulations of amphotericin B may be better tolerated but are very expensive and not easily available. Recommendations for treatment based on case studies are that fluconazole or itraconazole are good choices. In CNS or systemic cases, amphotericin B alone or in combination with flucytosine may be the first choice, followed by prolonged treatment with fluconazole or itraconazole. 29 Cats with pre-existing renal disease should be treated with itraconazole or fluconazole only. Fluconazole seems to be more effective than itraconazole for infections involving the CNS, eye and urinary tract, and is also better tolerated [EBM grade III].1,24,43 Resistance to fluconazole was reported with some isolates that nevertheless were susceptible to other azoles. 2
The clinical condition of cats with cerebral cryptococcosis may worsen soon after starting amphotericin B therapy, presumably due to an inflammatory response and increased intracranial pressure. Short-acting corticosteroid (dexamethasone or prednisolone sodium succinate) therapy is reported to be of immediate benefit in such cases and associated with improved chance of survival in the short term.13,29
Surgical excision of any nodules located in the skin, nasal or oral mucosa must be considered as a valuable aid in cats under medical therapy [EBM grade III]. 46
In general, treatment is recommended until the antigen test is negative. If the antigen test is negative at the time of diagnosis and the disease was confirmed by other methods, or if the antigen test is not available, treatment should be continued until at least 2–4 months after resolution of clinical signs. See Table 1 for treatment options.
Table 1.
Treatment of cryptococcosis
| Drug/therapy | Dose and duration | Comments |
|---|---|---|
| Itraconazole | 50–100 mg/cat q24h | Good absorption without food. Oral solution better than capsules. Hepatotoxicity possible; monitor liver enzymes periodically/monthly |
| Amphotericin B | 0.25 mg/kg q48h IV to a total dose of 4–16 mg/kg | Treatment of choice for CNS infection and/or systemic disease. Significant nephrotoxicity; monitor renal function frequently/weekly |
| Flucytosine | 25–50 mg/kg PO q6h | Synergistic with amphotericin B; do not use as single treatment |
| Fluconazole | 50 mg/cat q12h | Suggested treatment of choice, especially for CNS infection. Good absorption without food. Monitor liver enzymes |
| Terbinafine | 10 mg/kg q24h | Use if resistance to azoles |
| Surgical excision | Skin, oropharyngeal and nostril granulomas |
iv = intravenous, PO = oral, CNS = central nervous system
Prevention
Free-roaming cats in rural areas are potentially more exposed to Cryptococcus, even though urban cats can be contaminated through pigeon guano. The presence of avian guanos, particularly pigeon droppings, and some decaying vegetation substrates such as eucalyptus leaves, may be considered a risk factor. 17 A knowledge of local fungal habitats that carry the largest risks of exposure and about seasonal variations in the production of infectious propagules would be useful to develop preventive measures for both human and animal infection.
Footnotes
Funding: The authors received no specific grant from any funding agency in the public, commercial or not-for-profit sectors for the preparation of this article. The ABCD is supported by Merial, but is a scientifically independent body.
The authors do not have any potential conflicts of interest to declare.
Key Points
Cryptococcosis is worldwide the most common systemic fungal disease in cats caused by the C neoformans–C gattii species complex.
Cryptococcosis is a non-contagious rare or sporadic disease acquired by cats, usually by inhalation of organisms from a contaminated environment.
Cryptococcosis is not considered a zoonosis; animals may serve as sentinels for exposure of human beings.
The disease can present in several clinical forms, including the nasal form, CNS form (which can either derive from the nasal form or occur independently), cutaneous form and systemic form.
Diagnosis can be confirmed using a rapid agglutination antigen test on serum or body fluids.
The prognosis is favourable, if the diagnosis is obtained early and owners cooperate with a long course of treatment (months) and follow-up (years).
Surgical excision of nodules located in the skin, nasal or oral mucosa is valuable adjunctive treatment for cats undergoing antibiotic therapy.
Antifungal treatment choices include amphotericin B, ketoconazole, fluconazole or itraconazole, based on individual assessment.
Avian guano, particularly pigeon droppings, and decaying vegetation substrates such as eucalyptus leaves are risk factors.
References
- 1. Sykes JE, Malik R. Cryptococcosis. In: Greene CE. (ed). Infectious diseases of the dog and cat. 4th ed. St Louis: Saunders, Elsevier, 2012, pp 621–634. [Google Scholar]
- 2. Lester SJ, Malik R, Bartlett KH, Duncan CG. Cryptococcosis: update and emergence of Cryptococcus gattii. Vet Clin Pathol 2011; 40: 4–17. [DOI] [PubMed] [Google Scholar]
- 3. Alspaugh JA, Davidson RC, Heitman J. Morphogenesis of Cryptococcus neoformans. Contrib Microbiol 2000; 5: 217–238. [DOI] [PubMed] [Google Scholar]
- 4. Lin X, Heitman J. The biology of the Cryptococcus neoformans species complex. Annu Rev Microbiol 2006; 60: 69–105. [DOI] [PubMed] [Google Scholar]
- 5. Kano R, Kitagawat M, Oota S, Oosumit T, Murakami Y, Tokuriki M, et al. First case of feline systemic Cryptococcus albidus infection. Med Mycol 2008; 46: 75–77. [DOI] [PubMed] [Google Scholar]
- 6. Kano R, Hosaka S, Hasegawa A. First isolation of Cryptococcus magnus from a cat. Mycopathologia 2004; 157: 263–264. [DOI] [PubMed] [Google Scholar]
- 7. McGill S, Malik R, Saul N, Beetson S, Secombe C, Robertson I, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995–2006. Med Mycol 2009; 47: 625–639. [DOI] [PubMed] [Google Scholar]
- 8. Castella G, Abarca L, Cabanes FJ. Criptococosis y animales de Compañía. Rev Iberoam Micol 2008; 25: S19–S24. [DOI] [PubMed] [Google Scholar]
- 9. Craig S, Lester S, Black W, Fyfe M, Raverty S. Multispecies outbreak of cryptococcosis on southern Vancouver Island, British Columbia. Can Vet J 2002; 43: 792–794. [PMC free article] [PubMed] [Google Scholar]
- 10. Duncan C, Stephen C, Lester S, Bartlett KH. Follow-up study of dogs and cats with asymptomatic Cryptococcus gattii infection or nasal colonization. Med Mycol 2005; 43: 663–666. [DOI] [PubMed] [Google Scholar]
- 11. Duncan C, Stephen C, Campbell J. Clinical characteristics and predictors of mortality for Cryptococcus gattii infection in dogs and cats of southwestern British Columbia. Can Vet J 2006; 47: 993–998. [PMC free article] [PubMed] [Google Scholar]
- 12. O’Brien CR, Krockenberger MB, Wigney DI, Martin P, Malik R. Retrospective study of feline and canine cryptococcosis in Australia from 1981 to 2001: 195 cases. Med Mycol 2004; 42: 449–460. [DOI] [PubMed] [Google Scholar]
- 13. Sykes JE, Sturges BK, Cannon MS, Gericota B, Higgins RJ, Trivedi SR, et al. Clinical signs, imaging features, neuropathology, and outcome in cats and dogs with central nervous system cryptococcosis from California. J Vet Intern Med 2010; 24: 1427–1438. [DOI] [PubMed] [Google Scholar]
- 14. Malik R, Wigney DI, Muir DB, Love DN. Asymptomatic carriage of Cryptococcus neoformans in the nasal cavity of dogs and cats. J Med Vet Mycol 1997; 35: 27–31. [PubMed] [Google Scholar]
- 15. Connolly JH, Krockenberger MB, Malik R, Canfield PJ, Wigney DI, Muir DB. Asymptomatic carriage of Cryptococcus neoformans in the nasal cavity of the koala (Phascolarctos cinereus). Med Mycol 1999; 37: 331–338. [DOI] [PubMed] [Google Scholar]
- 16. Bartlett KH, Fyfe MW, MacDougall LA. Environmental Cryptococcus neoformans var gattii in British Columbia, Canada. Am J Respir Crit Care Med 2003; 167: A499. [Google Scholar]
- 17. Fortes ST, Lazéra MS, Nishikawa MM, Macedo RC, Wanke B. First isolation of Cryptococcus neoformans var gattii from a native jungle tree in the Brazilian Amazon rainforest. Mycoses 2001; 44: 137–140. [DOI] [PubMed] [Google Scholar]
- 18. Pal M. Cryptococcus neoformans var neoformans and munia birds. Mycoses 1989; 32: 250–252. [DOI] [PubMed] [Google Scholar]
- 19. Gerds-Grogan S, Dayrell-Hart B. Feline cryptococcosis: a retrospective study. J Am Anim Hosp Assoc 1997; 33: 118–122. [DOI] [PubMed] [Google Scholar]
- 20. Malik R, Wigney DI, Muir DB, Gregory DJ, Love DN. Cryptococcosis in cats: clinical and mycological assessment of 29 cases and evaluation of treatment using orally administered fluconazole. J Med Vet Mycol 1992; 30: 133–144. [DOI] [PubMed] [Google Scholar]
- 21. Jacobs GJ, Medleau L, Calvert C, Brown J. Cryptococcal infection in cats: factors influencing treatment outcome, and results of sequential serum antigen titers in 35 cats. J Vet Intern Med 1997; 11: 1–4. [DOI] [PubMed] [Google Scholar]
- 22. Flatland B, Greene RT, Lappin MR. Clinical and serologic evaluation of cats with cryptococcosis. J Am Vet Med Assoc 1996; 209: 1110–1113. [PubMed] [Google Scholar]
- 23. Lester SJ, Kowalewich NJ, Bartlett KH, Krockenberger MB, Fairfax TM, Malik R. Clinicopathologic features of an unusual outbreak of cryptococcosis in dogs, cats, ferrets, and a bird: 38 cases (January to July 2003). J Am Vet Med Assoc 2004; 225: 1716–1722. [DOI] [PubMed] [Google Scholar]
- 24. Trivedi SR, Sykes JE, Cannon MS, Wisner ER, Meyer W, Sturgess BK, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988–2010). J Am Vet Med Assoc 2011; 239: 357–369. [DOI] [PubMed] [Google Scholar]
- 25. Martins DB, Zanette RA, França RT, Howes F, Azevedo MI, Botton SA, et al. Massive cryptococcal disseminated infection in a immunocompetent cat. Vet Dermatol 2011; 22: 232–234. [DOI] [PubMed] [Google Scholar]
- 26. Bemis DA, Krahwinkel DJ, Bowman LA, Mondon P, Kwon-Chung KJ. Temperature-sensitive strain of Cryptococcus neoformans producing hyphal elements in a feline nasal granuloma. J Clin Microbiol 2000; 38: 926–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lin X. Cryptococcus neoformans: morphogenesis, infection, and evolution. Infect Genet Evol 2009; 9: 401–416. [DOI] [PubMed] [Google Scholar]
- 28. Urban CF, Lourido S, Zychlinsky A. How do microbes evade neutrophil killing? Cell Microbiol 2006; 8: 1687–1696. [DOI] [PubMed] [Google Scholar]
- 29. O’Brien CR, Krockenberger MB, Martin P, Wigney DI, Malik R. Long-term outcome of therapy for 59 cats and 11 dogs with cryptococcosis. Aust Vet J 2006; 84: 384–392. [DOI] [PubMed] [Google Scholar]
- 30. Norris JM, Bell ET, Hales L, Toribio JA, White JD, Wigney DI, et al. Prevalence of feline immunodeficiency virus infection in domesticated and feral cats in eastern Australia. J Feline Med Surg 2007; 9: 300–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Graham KJ, Brain PH, Spielman D, Martin PA, Allan GS, Malik R. Concurrent infection with Cryptococcus neoformans/ gattii species complex and Mycobactcerium avium affecting the subcutis and bone of a pelvic limb in a cat. J Feline Med Surg 2011; 13: 776–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Malik R, Martin P, Wigney DI, Church DB, Bradley W, Bellenger CR, et al. Nasopharyngeal cryptococcosis. Aust Vet J 1997; 75: 483–488. [DOI] [PubMed] [Google Scholar]
- 33. Beatty JA, Barrs VR, Swinney GR, Martin PA, Malik R. Peripheral vestibular disease associated with cryptococcosis in three cats. J Feline Med Surg 2000; 2: 29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Paulin J, Morshed M, Armién AG. Otitis interna induced by Cryptococcus neoformans var grubii in a cat. Vet Pathol 2013; 50: 260–263. [DOI] [PubMed] [Google Scholar]
- 35. Belluco S, Thibaud JL, Guillot J, Krockenberger MB, Wyers M, Blot S, Colle MA. Spinal cryptococcoma in an immunocompetent cat. J Comp Pathol 2008; 139: 246–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tisdall PL, Martin P, Malik R. Cryptic disease in a cat with painful and swollen hocks: an exercise in diagnostic reasoning and clinical decision-making. J Feline Med Surg 2007; 9: 418–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Brandt LE, Blauvelt MM. What is your diagnosis? Urine sediment from a southern California cat with weight loss. Vet Clin Pathol 2010; 39: 517–518. [DOI] [PubMed] [Google Scholar]
- 38. Krockenberger MB, Canfield PJ, Kozel TR, Shinoda T, Ikeda R, Wigney DI, et al. An immunohistochemical method that differentiates Cryptococcus neoformans varieties and serotypes in formalin-fixed paraffin-embedded tissues. Med Mycol 2001; 39: 523–533. [DOI] [PubMed] [Google Scholar]
- 39. Kano R, Fujino Y, Takamoto N, Tsujimoto H, Hasegawa A. PCR detection of the Cryptococcus neoformans CAP59 gene from a biopsy specimen from a case of feline cryptococcosis. J Vet Diagn Invest 2001; 13: 439–442. [DOI] [PubMed] [Google Scholar]
- 40. Okabayashi K, Kano R, Watanabe T, Hasegawa A. Serotypes and mating types of clinical isolates from feline cryptococcosis in Japan. J Vet Med Sci 2006; 68: 91–94. [DOI] [PubMed] [Google Scholar]
- 41. Meyer W, Castañeda A, Jackson S, Huynh M, Castañeda E. Molecular typing of IberoAmerican Cryptococcus neoformans isolates. Emerg Infect Dis 2003; 9: 189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Karnik K, Reichle JK, Fischetti AJ, Goggin JM. Computed tomographic findings of fungal rhinitis and sinusitis in cats. Vet Radiol Ultrasound 2009; 50: 65–68. [DOI] [PubMed] [Google Scholar]
- 43. Hammond JJ, Glass EN, Bishop TM, Kent M, De Lahunta A. Imaging diagnosis – intracranial cryptococcal mass in a cat. Vet Radiol Ultrasound 2011; 52: 306–308. [DOI] [PubMed] [Google Scholar]
- 44. Medleau L, Jacobs GJ, Marks MA. Itraconazole for the treatment of cryptococcosis in cats. J Vet Intern Med 1995; 9: 39–42. [DOI] [PubMed] [Google Scholar]
- 45. Davies C, Troy GC. Deep mycotic infections in cats. J Am Anim Hosp Assoc 1996; 32: 380–391. [DOI] [PubMed] [Google Scholar]
- 46. Hunt GB, Perkins M, Foster SF, Barrs VR, Swinney GR, Malik R. Nasopharyngeal disorders of dogs and cats: a review and retrospective study. Compend Contin Educ Pract Vet 2002; 24: 184–199. [Google Scholar]


