ABSTRACT
CONTEXT AND OBJECTIVE:
Serological testing for CA125 has been widely used to detect endometriosis and to monitor its progression. However, controversy still exists regarding the usefulness of the plasma CA125 assay for diagnosing endometriosis. Furthermore, some authors have described superficial endometriosis as a cyclical and normal phenomenon in women’s lives, and have indicated that development and progression of this disease would only occur in some women as a result of immunological changes. This study aimed to determine the frequency of endometriosis and the correlation between serum CA125 levels and the presence of endometriotic lesions in the peritoneum of asymptomatic fertile patients.
DESIGN AND SETTING:
Cross-sectional study at the Family Planning outpatient clinic of Faculdade de Medicina do ABC.
METHODS:
Eighty asymptomatic fertile patients who underwent tubal sterilization surgery were studied. Blood and peritoneum samples were collected. CA125 levels were measured from blood samples, and peritoneum biopsies were studied using histopathological tests.
RESULTS:
Histopathological evaluation of the peritoneum revealed that 16.25% of the patients had minimal or mild endometriosis. There was no statistically significant difference in CA125 levels between patients with and without endometriosis.
CONCLUSION:
The presence of endometriotic lesions in the peritoneum of fertile patients supports the hypothesis that incidental findings of minimal or mild endometriosis may not be of clinical significance, and that the progression of the disease probably occurs as a result of immunological and genetic abnormalities. Serum CA125 levels did not show any diagnostic significance with regard to detecting the disease.
KEY WORDS: Endometriosis, Pelvic pain, Infertility, Dysmenorrhea, CA-125 antigen
RESUMO
CONTEXTO E OBJETIVO:
O teste sorológico para CA125 tem sido largamente usado para detectar e monitorar a progressão da endometriose, entretanto, a utilidade do ensaio do CA125 plasmático para o diagnóstico da endometriose ainda é controversa. Além disso, alguns autores descreveram a endometriose superficial como sendo um fenômeno cíclico e normal na vida de uma mulher, e que o desenvolvimento e progressão desta doença ocorreriam apenas em algumas mulheres como resultado de alterações imunológicas. Este estudo teve como objetivo determinar a freqüência de endometriose e a correlação entre os níveis séricos de CA125 e a presença de lesões endometrióticas em peritônio de pacientes férteis assintomáticas.
TIPO DE ESTUDO E LOCAL:
Estudo transversal realizado no Ambulatório de Planejamento Familiar da Faculdade de Medicina do ABC.
MÉTODOS:
Foram estudadas 80 pacientes férteis assintomáticas submetidas à cirurgia de esterilização tubária. Amostras de sangue e peritônio foram coletadas. Os níveis de CA125 foram medidos a partir das amostras de sangue e as biópsias de peritônio foram estudadas por ensaio histopatológico.
RESULTADOS:
O estudo histopatológico do peritônio revelou que 16,25% das pacientes apresentavam endometriose mínima e leve. Os níveis de CA125 não demonstraram diferença estatística significante entre pacientes com e sem endometriose.
CONCLUSÃO:
A presença de lesões endometrióticas em peritônio de pacientes férteis reforça a hipótese de que achados acidentais de endometriose mínima e leve podem não ter significância clínica, e que é provável que a progressão da doença ocorra como resultado de alterações genéticas e imunológicas. Os níveis séricos de CA125 não demonstraram significância diagnóstica para a detecção da doença.
PALAVRAS-CHAVE: Endometriose, Dor pélvica, Infertilidade, Dismenorréia, Antígeno Ca-125
INTRODUCTION
An endometriotic lesion is defined as the presence of endometrial tissue outside the uterus, thus causing infertility, pelvic pain and dysmenorrhea.1 Estimates of the frequency of endometriosis range from 10-15% in women of reproductive age2 up to 50% in women with fertility problems1 and around 60%-70% in women with chronic pelvic pain.3 However, up to 20% of women may have endometriosis without presenting any symptoms.1
In clinical practice, severe endometriosis can be diagnosed with high accuracy by means of pelvic examination and through using imaging tools such as transvaginal ultrasonography4 and magnetic resonance.5 However, these methods are not sensitive enough to detect mild endometriosis,6 and laparoscopy or laparotomy is necessary in order to confirm the diagnosis and classify the stage of endometriosis according to the criteria of the American Fertility Society.7
Some authors have described superficial endometriosis as a cyclical and normal phenomenon in women’s lives, and have indicated that development and progression of this disease would only occur in some women as a result of immunological changes.8,9 Thus, the low specificity of the diagnostic methods available, along with the severity of the disease, has motivated new studies to search for noninvasive diagnostic methods to detection endometriosis.6
Serological testing for CA125 has been widely used to detect endometriosis and to monitor its progression.10 However, controversy still exists regarding the usefulness of the plasma CA125 assay for diagnosing endometriosis.11,12 Moreover, only a small and limited number of studies in the literature have combined peritoneal and serum samples,3 especially among asymptomatic fertile women.
OBJECTIVE
This study aimed to determine the frequency of endometriosis and the correlation between serum CA125 levels and the presence of endometriotic lesions in the peritoneum of asymptomatic fertile patients.
MATERIAL AND METHODS
Patients
Eighty fertile women with no symptoms of endometriosis such as infertility, pelvic pain and/or dysmenorrhea (aged 21-44 years, mean: 33.68 ± 4.63) were studied. All of the subjects were attending the Family Planning outpatient clinic of Faculdade de Medicina do ABC (FMABC), Santo André, Brazil, and underwent surgery for tubal sterilization as a familiar planning measure.
The study protocol was approved by the local research ethics committee. All patients gave their informed consent for inclusion in the study.
METHODS
Histopathological evaluation
The patients underwent laparoscopic surgery for tubal sterilization and, during the procedure, small pieces of peritoneum were excised from four different sites: left and right ovarian fossae, and left and right sacrouterine ligaments.
The biopsy specimens were fixed in a 10% formalin solution and embedded in paraffin. Histological sections (3-5 mm thick) were cut and stained with hematoxylin-eosin. A total of 320 microscope slides stained with hematoxylin-eosin were studied (Figure 1).
Figure 1. Photomicrographs at 100 X (A) and 400 X (B and C) of histological findings from peritoneum of asymptomatic fertile patients showing endometriosis (A and B), compared with normal tissue (C) (hematoxylin-eosin staining).
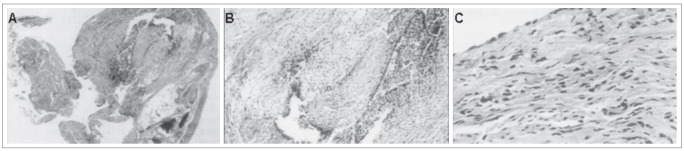
The criterion for histological classification of endometriosis was identification of stromal endometrioid or epithelial elements of Müllerian type, with or without stroma, associated with signs of hemorrhage and fibrosis.
After histological confirmation of the diagnosis of endometriosis, the lesions were classified morphologically, based on the variations in appearance of the ectopic endometrial structures.13 The morphological criteria for the analysis were: stromal disease, when only endometrial stroma was found; well-differentiated disease, when glands similar to topical endometrium were found; undifferentiated disease, when the appearance of the glands was different from topical endometrium; and mixed disease, when the appearance of the glands was atypical or undifferentiated.14 Endometriosis was staged according to the revised American Fertility Society (r-AFS) classification.15
Serum CA125 level
Blood samples were collected on the first three days of the cycle prior to surgery. After collection, the blood samples were immediately centrifuged; the serum was removed, placed in a cryotube and frozen at -80 °C. Serum CA125 levels were measured in accordance with the manufacturer’s instructions (BYK-Sangtec Diagnostica GmbH, Germany). When the CA125 values were higher than 35 U/ml, a second measurement was performed to confirm the result.
Statistical analysis
The Mann-Whitney test was performed to compare the serum CA125 levels among the patients. The significance level was set at 5% (a £ 0.05).
RESULTS
The histopathological evaluation revealed that 13 (16.25%) out of these 80 patients (without any symptoms of endometriosis like infertility, dysmenorrhea and/or pelvic pain) showed level I or II endometriotic lesions. Of these patients, six (7.5%) had typical and four (5.0%) had atypical lesions. In three patients (3.8%), lesions were found only in the histopathological evaluation study (unapparent endometriosis). In six of these cases, the endometriosis was located in sacrouterine ligaments, and in five in ovarian fossae. In two cases, we found lesions at more than one site. No ovarian endometriosis was observed.
No statistical difference in serum CA125 levels was observed between patients with and without endometriosis: means of 26.9 and 28.3 U/ml, respectively (P = 0.6389 and sample power of 67%).
DISCUSSION
Endometriosis, a chronic painful inflammatory disease that is one of the most common gynecological disorders,7 is defined as the presence of a steroid hormone-dependent endometrium-like tissue consisting of glands and stroma that grows outside the uterine cavity. The target tissues and organs include the fallopian tubes, ovaries, peritoneum, colon, rectovaginal region and bladder.16 Endometriosis causes infertility, pelvic pain and dysmenorrhea.1,17 However, up to 20% of women may have endometriosis without presenting any symptoms.7 It is a polygenic/multifactorial disease that includes not only hormonal and immunological factors, but also genetic factors.17
Considerable efforts have been made towards searching for noninvasive diagnostic methods to detect endometriosis. Moreover, the use of biomarkers has been widely discussed. Abrão et al.8 evaluated serum CA125, C-reactive protein, amyloid A protein and anticardiolipin antibodies during the menstrual phase and the middle follicular phase. They found that CA125 was the marker presenting the highest levels during the menstrual phase, between the first and third days of the cycle.
The high levels of CA125 in the bloodstream observed in the presence of an endometriotic ovarian cyst and/or endometriosis with deep infiltration suggest that this antigen may pass into the circulation from endometrial cells in patients with endometriosis.18,19 The CA125 released by the endometrium may reach the blood stream and lymphatic circulation via the peritoneal route, starting from retrograde menstruation, thereby allowing contact with local inflammatory reactions and thus releasing coelomic CA125.20 Another explanation for the increased levels of CA125 in the bloodstream could be its access into the abdominal cavity through tubal reflux, thus resulting in absorption by peritoneal lymphatic vessels. Despite the mechanisms proposed, doubts still persist about the real mechanism of CA125 release into the circulation, considering that retrograde menstruation is still controversial and that the levels of this marker change during the postmenopausal period.20 Koninckx and Martin21 evaluated CA125 and concluded that superficial endometriosis causes elevation of CA125 levels in peritoneal fluid, whereas the deep disease causes their elevation in blood.
Several hypotheses have been raised to explain the cause of elevated serum CA125 at the time of menstruation in patients with endometriosis. They include higher membrane CA125 concentration in ectopic cells than in eutopic endometrial cells;22 bleeding relating to eutopic endometrium;23 increased transition of CA125 from endometrial tissue to peritoneum, relating to retrograde menses and eutopic endometrium;22,23 an enlarged surface area of endometrial tissue;24 inflammatory reaction due to the presence of endometriotic foci; and blood and endometrial shedding into the peritoneal cavity.23,24
Many studies have reported that serum CA125 levels were higher in patients with endometriosis, especially in those at an advanced level, suggesting that monitoring of CA125 in peripheral blood might reflect its behavior in the abdominal environment.3,25
On the other hand, some authors consider superficial endometriosis to be a physiological and intermittent condition in women during their reproductive years, whereas its progression, characterized as deep infiltrative endometriosis and/or endometrial ovarian cysts, is considered to be the true disease.9,13,19,26 Divergences persist regarding the natural history of endometriosis, its symptoms, extent, location and staging. The presence of pelvic pain, especially dysmenorrhea, plus infertility and dyspareunia, are the trio that characterizes the disease.9
In the present study, 16.25% of the patients had mild endometriosis, and the serum CA125 levels showed no difference between fertile asymptomatic women with and without endometriosis, although the number of cases investigated was small. Moreover, endometriosis was observed in healthy peritoneum of fertile women,27 in the same way as reported by Nezhat et al.,28 Nisolle et al.29 and Balasch et al.30 among women with infertility and pelvic pain.
CONCLUSION
In conclusion, the data suggest that incidental findings of minimal/mild endometriosis may not be of clinical significance, and progression of the disease probably occurs as a result of immunological and genetic abnormalities.The serum CA125 levels in our study did not show any diagnostic significance for detecting the disease.
Faculdade de Medicina do ABC, Santo André, São Paulo, Brazil
Sources of funding: Not declared
REFERENCES
- 1.Missmer SA, Cramer DW. The epidemiology of endometriosis. Obstet Gynecol Clin North Am. 2003;30(1):1–19. doi: 10.1016/s0889-8545(02)00050-5. vii. [DOI] [PubMed] [Google Scholar]
- 2.Mahmood TA, Templeton A. Prevalence and genesis of endometriosis. Hum Reprod. 1991;6(4):544–549. doi: 10.1093/oxfordjournals.humrep.a137377. [DOI] [PubMed] [Google Scholar]
- 3.Amaral VF, Ferriani RA, Sá MF, et al. Positive correlation between serum and peritoneal fluid CA-125 levels in women with pelvic endometriosis. Sao Paulo Med J. 2006;124(4):223–227. doi: 10.1590/S1516-31802006000400010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dessole S, Farina M, Rubattu G, Cosmi E, Ambrosini G, Nardelli GB. Sonovaginography is a new technique for assessing rectovaginal endometriosis. Fertil Steril. 2003;79(4):1023–1027. doi: 10.1016/s0015-0282(02)04952-x. [DOI] [PubMed] [Google Scholar]
- 5.Stratton P, Winkel C, Premkumar A, et al. Diagnostic accuracy of laparoscopy, magnetic resonance imaging, and histopathologic examination for the detection of endometriosis. Fertil Steril. 2003;79(5):1078–1085. doi: 10.1016/s0015-0282(03)00155-9. [DOI] [PubMed] [Google Scholar]
- 6.Kitawaki J, Ishihara H, Koshiba H, et al. Usefulness and limits of CA-125 in diagnosis of endometriosis without associated ovarian endometriomas. Hum Reprod. 2005;20(7):1999–2003. doi: 10.1093/humrep/deh890. [DOI] [PubMed] [Google Scholar]
- 7.Renner SP, Strick R, Oppelt P, et al. Evaluation of clinical parameters and estrogen receptor alpha gene polymorphisms for patients with endometriosis. Reproduction. 2006;131(1):153–161. doi: 10.1530/rep.1.00787. [DOI] [PubMed] [Google Scholar]
- 8.Abrão MS, Podgaec S, Filho BM, Ramos LO, Pinotti JA, de Oliveira RM. The use of biochemical markers in the diagnosis of pelvic endometriosis. Hum Reprod. 1997;12(11):2523–2527. doi: 10.1093/humrep/12.11.2523. [DOI] [PubMed] [Google Scholar]
- 9.Vercellini P, Trespidi L, Panazza S, Bramante T, Mauro F, Crosignani PG. Laparoscopic uterine biopsy for diagnosing diffuse adenomyosis. J Reprod Med. 1996;41(4):220–224. [PubMed] [Google Scholar]
- 10.Cheng YM, Wang ST, Chou CY. Serum CA-125 in preoperative patients at high risk for endometriosis. Obstet Gynecol. 2002;99(3):375–380. doi: 10.1016/s0029-7844(01)01731-8. [DOI] [PubMed] [Google Scholar]
- 11.Harada T, Kubota T, Aso T. Usefulness of CA19-9 versus CA125 for the diagnosis of endometriosis. Fertil Steril. 2002;78(4):733–739. doi: 10.1016/s0015-0282(02)03328-9. [DOI] [PubMed] [Google Scholar]
- 12.Somigliana E, Viganò P, Tirelli AS, et al. Use of the concomitant serum dosage of CA 125, CA 19-9 and interleukin-6 to detect the presence of endometriosis. Results from a series of reproductive age women undergoing laparoscopic surgery for benign gynaecological conditions. Hum Reprod. 2004;19(8):1871–1876. doi: 10.1093/humrep/deh312. [DOI] [PubMed] [Google Scholar]
- 13.Hoeger KM, Guzick DS. An update on the classification of endometriosis. Clin Obstet Gynecol. 1999;42(3):611–619. doi: 10.1097/00003081-199909000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Abrao MS, Neme RM, Carvalho FM, Aldrighi JM, Pinotti JA. Histological classification of endometriosis as a predictor of response to treatment. Int J Gynaecol Obstet. 2003;82(1):31–40. doi: 10.1016/s0020-7292(03)00079-1. [DOI] [PubMed] [Google Scholar]
- 15.Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil Steril. 1997;67(5):817–821. doi: 10.1016/s0015-0282(97)81391-x. [DOI] [PubMed] [Google Scholar]
- 16.Giudice LC, Kao LC. Endometriosis. Lancet. 2004;364(9447):1789–1799. doi: 10.1016/S0140-6736(04)17403-5. [DOI] [PubMed] [Google Scholar]
- 17.Bulun SE, Zeitoun KM, Takayama K, Sasano H. Estrogen biosynthesis in endometriosis: molecular basis and clinical relevance. J Mol Endocrinol. 2000;25(1):35–42. doi: 10.1677/jme.0.0250035. [DOI] [PubMed] [Google Scholar]
- 18.Pittaway DE, Rondinone D, Miller KA, Barnes K. Clinical evaluation of CA-125 concentrations as a prognostic factor for pregnancy in infertile women with surgically treated endometriosis. Fertil Steril. 1995;64(2):321–324. [PubMed] [Google Scholar]
- 19.Koninckx PR. Is mild endometriosis a condition occurring intermittently in all women? Hum Reprod. 1994;9(12):2202–2205. doi: 10.1093/oxfordjournals.humrep.a138419. [DOI] [PubMed] [Google Scholar]
- 20.Bon GG, Kenemans P, Dekker JJ, et al. Fluctuations in CA 125 and CA 15-3 serum concentrations during spontaneous ovulatory cycles. Hum Reprod. 1999;14(2):566–570. doi: 10.1093/humrep/14.2.566. [DOI] [PubMed] [Google Scholar]
- 21.Koninckx PR, Martin DC. Deep endometriosis: a consequence of infiltration or retraction or possibly adenomyosis externa? Fertil Steril. 1992;58(5):924–928. doi: 10.1016/s0015-0282(16)55436-3. [DOI] [PubMed] [Google Scholar]
- 22.Niloff JM, Knapp RC, Jones G, Schaetzl EM, Bast RC., Jr Recombinant leukocyte alpha interferon in advanced ovarian carcinoma. Cancer Treat Rep. 1985;69(7-8):895–896. [PubMed] [Google Scholar]
- 23.Falconer H, Bambra CS, Chai D, Cornillie FJ, Hill JA, D’Hooghe TM. The effect of endometriosis, cycle stage, lymphocyte suppression and pregnancy on CA-125 levels in peritoneal fluid and serum in baboons. Hum Reprod. 2005;20(11):3033–3038. doi: 10.1093/humrep/dei181. [DOI] [PubMed] [Google Scholar]
- 24.Johansson J, Santala M, Kauppila A. Explosive rise of serum CA 125 following the rupture of ovarian endometrioma. Hum Reprod. 1998;13(12):3503–3504. doi: 10.1093/humrep/13.12.3503. [DOI] [PubMed] [Google Scholar]
- 25.Koninckx PR, Meuleman C, Oosterlynck D, Cornillie FJ. Diagnosis of deep endometriosis by clinical examination during menstruation and plasma CA-125 concentration. Fertil Steril. 1996;65(2):280–287. [PubMed] [Google Scholar]
- 26.Nisolle M, Nervo P. J Gynecol Obstet Biol Reprod. 8 Pt 2. Vol. 32. Paris: 2003. Endométriose stade I et II: implications physiopathologiques, cliniques et thérapeutiques [Physiopathology and therapeutic management of stage I and II endometriosis] pp. S11–S14. [PubMed] [Google Scholar]
- 27.Barbosa CP, de Souza AM, Bianco B, Christofolini DM, Mafra FA, de Lima GR. OC-125 immunostaining in endometriotic lesion samples. Arch Gynecol Obstet. 2009 doi: 10.1007/s00404-009-1055-7. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 28.Nezhat F, Allan CJ, Nezhat C, Martin DC. Nonvisualized endometriosis at laparoscopy. Int J Fertil. 1991;36(6):340–343. [PubMed] [Google Scholar]
- 29.Nisolle M, Casanas-Roux F, Anaf V, Mine JM, Donnez J. Morphometric study of the stromal vascularization in peritoneal endometriosis. Fertil Steril. 1993;59(3):681–684. [PubMed] [Google Scholar]
- 30.Balasch J, Creus M, Fábregues F, et al. Visible and non-visible endometriosis at laparoscopy in fertile and infertile women and in patients with chronic pelvic pain: a prospective study. Hum Reprod. 1996;11(2):387–391. doi: 10.1093/humrep/11.2.387. [DOI] [PubMed] [Google Scholar]


