Abstract
Background/Objective: No-shows have a negative effect on healthcare outcomes. It is unclear, however, whether patients’ distance from the clinic is associated with higher no-show rates. To fill this knowledge gap, we examined the relationship between patients’ distance from the clinic and no-shows in a rural provider network.
Methods: Data from Marshfield Clinic Health System’s scheduling system, including 263,464 recent patient appointments in 2021 were analyzed. The outcome was no-shows, defined as when patients missed an appointment (categorized as yes/no). The exposure was the distance to the clinic, measured in miles as a straight-line distance from the clinic in the patient’s zip code to the facility where the appointment was held (classified as <5 miles, 5-10, 10-20; >20, and used as continuous). Covariates were patient demographics, appointments, providers, and insurance status. Chi-square and logistic regression were used with p-values ≤.05 considered statistically significant.
Results: The no-show rate was 8.0%. Patients who lived <5 miles (8.3%) and >20 miles (8.2%) from the clinic had higher no-show rates than those who lived between 10-20 miles (8.0%) and 5-10 miles (7.6%), at P=0.001. In the adjusted model, the odds of no-show were similar between patients who did not show and those who did (OR:1.00,95%CI:1.00-1.00). No-shows were more likely among male patients compared to females (OR:1.14,95%CI:1.11-1.18), Spanish compared to English speakers (OR:1.34,95%CI:1.20-1.50), prior no-show compared to no prior no-show (OR:4.42,95%CI:4.27-4.48), >4 weeks lead time compared to <1 day (OR:5.45,95%CI:4.98-5.97), and Medicaid compared to non-Medicaid patients (OR:1.56,95%CI:1.49-1.63).
Conclusion: Our analysis showed patients who lived <5 miles and >20 miles from the clinic had higher no-show rates. The odds of a no-show were comparable between patients who showed up and those who did not. Male patients, Spanish-speaking patients, patients with a history of no-shows, and Medicaid beneficiaries were more likely to miss their appointments. Understanding the impact of these variables on no-show rates can assist healthcare providers in developing strategies to improve patient access and reduce no-show rates. These findings imply that rural patients may face a variety of barriers when seeking healthcare, necessitating a comprehensive approach to addressing this issue.
Keywords: Distance from the Clinic, No-Show Appointments, Rural Provider Network
No-show patients are those who fail to show up for booked appointments or cancel at the last minute, leaving the health facility unable to fill the appointment time.1,2 No-show appointments cause health centers to lose time and money while also disrupting the continuity of care for the patients.3 No-shows by patients result in inefficient clinic operations, high clinic expenses, and low patient satisfaction.3 While the rate of no-shows varies by health center, an average of 42% of appointments are missed.4 According to one study, a hospital reported 62 no-show appointments per day, costing an estimated $3 million.5 According to another source, missed appointments cost the United States $150 billion per year.6 Patients who do not attend clinic appointments have a significant impact on delivery, cost of care, and resource planning; hence, there is a need to address the factors that contribute to patient no-shows. While the tolerable level of no-shows can vary depending on the specific operational and environmental contexts of different clinics, our research aims to shed light on the prevalence and impacts of such occurrences.1,2 In many settings, a certain degree of no-shows is anticipated and deemed acceptable, although healthcare providers endeavor to minimize this to ensure optimal operational efficiency and patient care.3,5 Our research not only explores the existing norms, but also attempts to identify the distinctive challenges posed by the geographical and demographic context of our study area.
While developed countries like the U.S. benefit from established infrastructure and advanced transportation systems, accessing healthcare services in rural areas presents unique challenges. Contrary to the popular belief that well-built roads and available transportation systems are synonymous with easy access, rural regions in the U.S. still face nuanced barriers to healthcare. For instance, while transportation might be available, the long distances involved could discourage patients from attending their appointments due to the time and cost implications of the journey, or due to unpredictable factors like weather conditions in certain areas. Moreover, even in developed settings, certain socio-economic groups may still lack consistent access to personal transportation, relying instead on public or shared modes that might not always align conveniently with their appointment schedules.7–10 Additionally, perceptions about the distance might psychologically deter patients, regardless of the objective transportation availability. As such, understanding the dynamics of “access” in rural areas within a developed nation’s context is pivotal.
Several factors are associated with no-shows. In an analysis of 1,243 low-income patients’ electronic health record data, younger patients and Black or African American patients had a higher no-show rate, but there was no difference in gender or location.11 Individual and social barriers were cited as reasons for missed visits by low-income people with a no-show rate of 50% or higher. Women, geriatric patients, mental health patients, and those seeking sub-specialty health care services are more likely to no-show, and the day of the week and month of the appointment also have an impact on patient no-shows.5 As a result, lowering patient no-show rates is critical for improving clinic efficiency, as well as addressing the factors associated with no-shows to improve access.
Previous research has found a link between a higher no-show rate and younger patients; however, there were no differences in no-show rates between males and females, and no differences in no-show rates based on patient location.11 Males (rather than females) and younger patients, on the other hand, were found to be more likely to miss appointments in studies conducted outside the U. S. (United Kingdom), and according to research conducted at a large tertiary hospital in South Korea, insurance type impact high rates of no-shows.12–14 Some researchers focused on the negative impact of increased appointment lead time on high clinic no-show rates among ophthalmology appointments, as well as historical attendance behavior as a significant predictor of missing an appointment.15,16 Others have looked at how transportation issues, such as vehicle access, affect no-shows among people with lower incomes, the under/uninsured, and children.7–10 While previous studies contributed to our understanding of which factors are associated with no-shows, their findings were mixed, and it is unclear whether patients’ distance from the clinic is related to higher no-show rates. Studies did not investigate how the patient’s distance from the clinic in a rural setting, as well as other demographics (Spanish patients) and provider characteristics (specialty and type of provider) influence no-shows. As a result, in a rural provider network, we investigated the relationship between patients’ distance from the clinic and no-shows. Our findings fill an important gap in the literature on rural healthcare service delivery by informing contextual interventions to reduce patient no-show rates. Addressing the factors associated with no-shows is critical for improving clinic performance and promoting efficiency measures, as well as improving access and reducing health inequalities in rural patient populations.
Methods
Our study adopted a retrospective cohort design, leveraging extensive datasets from Marshfield Clinic Health System’s (MCHS) scheduling system to investigate the association between patients’ distance from the clinic and appointment no-shows. A cohort of 263,464 patient appointments from the year 2021 was meticulously analyzed to discern patterns and correlations, with the intention of extracting meaningful insights to enhance healthcare accessibility and efficiency in rural settings. By employing a comprehensive analytical approach, this study aimed to elucidate the multifaceted relationship between geographical accessibility and appointment adherence, contributing valuable knowledge to the discourse on healthcare delivery and resource optimization in rural healthcare networks.1,2,17
Clinic Setting and Data Sources
We analyzed data (N=263,464) containing the most recent patient appointments if they had more than one within a 12-month period in 2021 from the MCHS scheduling system. MCHS is an integrated rural health system that covers Wisconsin and Michigan’s Upper Peninsula, representing 170 specialties, a health plan, research, and education initiatives, and aims to improve people’s lives by providing accessible, cost-effective, and compassionate healthcare. Our Clinic was founded in 1916 in compliance with Wisconsin law and is one of only a few significant autonomous nonprofit medical clinics in the United States. A patient can make an appointment with one of our MCHS providers by calling one of the care teams or scheduling an appointment online through the patient portal. If the patient is unsure whom to contact, they can also contact the resource information coordinator.
Ethics Approval
All the procedures and protocols of our study strictly adhered to the ethical guidelines to ensure the utmost integrity, respect, and protection of participants’ rights and data. This study involved the analysis of de-identified data, and thus, participants’ confidentiality and anonymity were rigorously maintained. Our research received formal approval from the MCHS Institutional Review Board (IRB#: IRB00000673) and was granted exemption status, mitigating the necessity for further IRB reviews. The requirement to acquire authorization for the usage of specific Protected Health Information was also duly waived, pursuant to the stipulations of our IRB exemption.
Study Measures
The dependent variable was a no-show, characterized as when a patient missed an appointment without informing the healthcare provider ahead of time,1,2,17 for the most recent patient appointments if they had more than one in a 12-month period (January-December) in 2021. No-show was used as a binary outcome (yes/no).
The independent variable was the patient’s distance to the center/clinic, measured in miles as a straight-line distance from the clinic in the patient’s zip code to the facility where the appointment was held. The patient’s distance to the clinic was classified into four categories: < 5 miles, 5–10 miles, 10–20 miles, and > 20 miles, and was used as a continuous variable.
Covariates included patient demographics, appointment characteristics and appointment history, provider characteristics, and insurance information. Patient demographics were gender, measured as the sex of the patient (categorized as female and male), age, measured as the year between the patient’s date of birth and the current date (American Medical Association) designations as infants (1 year), children (1-12 years), adolescents (13-17 years), adults (18-64 years), and older adults (65 and older), and oral language of the patient (English, Spanish, and other: Hmong, Sign, etc.).
Appointment Characteristics/History
Items included were the number of scheduled appointments (categorized as one to ten and more than ten), appointment month (January to December), appointment day of the week (Monday to Friday), appointment duration in minutes (< 30 minutes, 30 to 60 minutes, and > 60 minutes), and appointment lead time/scheduled ahead days (< a day, within 2 weeks, > 2 weeks). Appointment history was prior no-show, one year retrospectively measured as the number of appointment no-shows for the patient for a year prior to the appointment date categorized as binary (no/yes).
Provider and Insurance Characteristics
Items included were provider specialty (categorized as not attributed, primary care, and specialty care) and provider type (categorized as Medical Doctor (MD)/physician and Non-physician/Allied Health). Insurance variables included Medicare, Medicaid, commercial, and other government insurance, with each insurance variable classified as binary (yes/no).
Statistical Analysis
We used Stata SE/17.0 to perform all analyses,18 and P≤0.05 was used to define statistical significance. First, patient demographics, appointment characteristics, provider characteristics, and insurance information were summarized and compared between groups using Chi-square tests to investigate univariate differences by study outcome (no-show). Second, an adjusted logistic regression was used to determine the independent relationship between patient distance to the clinic and no-show while controlling for covariates such as patient demographics, appointment characteristics, and provider and insurance information. The independent association between patient distance to the clinic and no-show, as well as other variables that were significant in the adjusted model, was presented using odds ratios (OR) and respective 95% confidence intervals (CI). Following our statistical analysis and summary of key findings, we used the Chat Generative Pre-Trained Transformer (Chat GPT) from OpenAI (2022) to propose supplementary insights that can enhance our discussion of the results. All methods and tools, including large language artificial intelligence (AI) models, have advantages and disadvantages that should be carefully considered.19
Results
A bivariate analysis of factors associated with no-show appointments in a rural healthcare system (MCHS) in 2021 is shown in Table 1. There were 21,077 (8.0%) no-shows out of 263,464 most recent patient appointments in 2021. More patients (36.1%) lived < 5 miles and > 20 miles (33.0%) from the clinic, followed by those who lived between 10–20 miles (17.6%) and 5–10 miles (13.3%). Patients who lived < 5 miles (8.3%) and > 20 miles (8.2%) from the clinic had a higher no-show rate than those who lived between 10–20 miles (8.0%) and 5–10 miles (7.6%), at P=0.001.
Table 1.
Characteristics and factors associated with no-shows in a rural healthcare system, 2021
| Study variables | Is no-show appointment | |||
|---|---|---|---|---|
| No: 242,387 (92.0%) |
Yes: 21,077 (8.0%) |
Total: 263,464 (N) |
P value | |
| Patient gender | ||||
| Female | 131543 | 11058 | 142601 | <0.001 |
| 92.3 | 7.8 | 100.0 | ||
| 54.3 | 52.5 | 54.1 | ||
| Male | 110844 | 10019 | 120863 | |
| 91.7 | 8.3 | 100.0 | ||
| 45.7 | 47.5 | 45.9 | ||
| Age (American Medical Association’s designations) | ||||
| Infants (1 year) | 1761 | 132 | 1893 | <0.001 |
| 93.03 | 7.0 | 100 | ||
| 0.7 | 0.6 | 0.7 | ||
| Children (1-12 years) | 27333 | 2709 | 30042 | |
| 91.0 | 9.0 | 100.0 | ||
| 11.3 | 12.9 | 11.4 | ||
| Adolescents (13-17 years) | 14641 | 1491 | 16132 | |
| 90.8 | 9.2 | 100.0 | ||
| 6.0 | 7.1 | 6.1 | ||
| Adults (18-64 years) | 114852 | 13860 | 128712 | |
| 89.2 | 10.8 | 100.0 | ||
| 47.4 | 65.8 | 48.9 | ||
| Older adults (65 and older) | 83800 | 2885 | 86685 | |
| 96.7 | 3.3 | 100.0 | ||
| 34.6 | 13.7 | 32.9 | ||
| Patient language | ||||
| English | 238327 | 20265 | 258592 | <0.001 |
| 92.2 | 7.8 | 100.0 | ||
| 98.3 | 96.2 | 98.2 | ||
| Spanish | 2607 | 433 | 3040 | |
| 85.8 | 14.2 | 100.0 | ||
| 1.1 | 2.1 | 1.2 | ||
| Other (Hmong, Sign, etc.) | 1453 | 379 | 1832 | |
| 79.3 | 20.7 | 100.0 | ||
| 0.6 | 1.8 | 0.7 | ||
| Number of appointments scheduled | ||||
| One to two | 116980 | 10193 | 127173 | <0.001 |
| 92.0 | 8.0 | 100.0 | ||
| 48.3 | 48.4 | 48.3 | ||
| Three to four | 47607 | 4327 | 51934 | |
| 91.7 | 8.3 | 100.0 | ||
| 19.6 | 20.5 | 19.7 | ||
| Five to six | 25441 | 2265 | 27706 | |
| 91.8 | 8.2 | 100.0 | ||
| 10.5 | 10.8 | 10.5 | ||
| Seven to eight | 15359 | 1330 | 16689 | |
| 92.0 | 8.0 | 100.0 | ||
| 6.3 | 6.3 | 6.3 | ||
| Nine to ten | 9779 | 844 | 10623 | |
| 92.1 | 8.0 | 100.0 | ||
| 4.0 | 4.0 | 4.0 | ||
| More than ten | 27221 | 2118 | 29339 | |
| 92.8 | 7.2 | 100.0 | ||
| 11.2 | 10.1 | 11.1 | ||
| Patient distance to the clinic | ||||
| < 5 miles | 83032 | 7464 | 90496 | 0.001 |
| 91.7 | 8.3 | 100.0 | ||
| 36.0 | 36.8 | 36.1 | ||
| 5 - 10 miles | 30810 | 2524 | 33334 | |
| 92.4 | 7.6 | 100.0 | ||
| 13.4 | 12.4 | 13.3 | ||
| 10 - 20 miles | 40472 | 3509 | 43981 | |
| 92.0 | 8.0 | 100.0 | ||
| 17.6 | 17.3 | 17.6 | ||
| > 20 miles | 75837 | 6759 | 82596 | |
| 91.8 | 8.2 | 100.0 | ||
| 33.0 | 33.4 | 33.0 | ||
| Appointment month | ||||
| January | 7206 | 819 | 8025 | <0.001 |
| 89.8 | 10.2 | 100.0 | ||
| 3.0 | 3.9 | 3.1 | ||
| February | 7421 | 779 | 8200 | |
| 90.5 | 9.5 | 100.0 | ||
| 3.1 | 3.7 | 3.1 | ||
| March | 9161 | 881 | 10042 | |
| 91.2 | 8.8 | 100.0 | ||
| 3.8 | 4.2 | 3.8 | ||
| April | 9213 | 948 | 10161 | |
| 90.7 | 9.3 | 100.0 | ||
| 3.8 | 4.5 | 3.9 | ||
| May | 9122 | 910 | 10032 | |
| 90.9 | 9.1 | 100.0 | ||
| 3.8 | 4.3 | 3.8 | ||
| June | 13030 | 1421 | 14451 | |
| 90.2 | 9.8 | 100.0 | ||
| 5.4 | 6.7 | 5.5 | ||
| July | 15664 | 1451 | 17115 | |
| 91.5 | 8.5 | 100.0 | ||
| 6.5 | 6.9 | 6.5 | ||
| August | 19929 | 1801 | 21730 | |
| 91.7 | 8.3 | 100.0 | ||
| 8.2 | 8.5 | 8.3 | ||
| September | 22121 | 2059 | 24180 | |
| 91.5 | 8.5 | 100.0 | ||
| 9.1 | 9.8 | 9.2 | ||
| October | 29308 | 2408 | 31716 | |
| 92.4 | 7.6 | 100.0 | ||
| 12.1 | 11.4 | 12.0 | ||
| November | 38785 | 3093 | 41878 | |
| 92.6 | 7.4 | 100.0 | ||
| 16.0 | 14.7 | 15.9 | ||
| December | 61427 | 4507 | 65934 | |
| 93.2 | 6.8 | 100.0 | ||
| 25.3 | 21.4 | 25.0 | ||
| Appointment day of the week | ||||
| Monday | 48647 | 4842 | 53489 | <0.001 |
| 91.0 | 9.1 | 100.0 | ||
| 20.1 | 23.0 | 20.3 | ||
| Tuesday | 54067 | 4858 | 58925 | |
| 91.8 | 8.2 | 100.0 | ||
| 22.3 | 23.1 | 22.4 | ||
| Wednesday | 52372 | 4222 | 56594 | |
| 92.5 | 7.5 | 100.0 | ||
| 21.6 | 20.0 | 21.5 | ||
| Thursday | 49155 | 3981 | 53136 | |
| 92.5 | 7.5 | 100.0 | ||
| 20.3 | 18.9 | 20.2 | ||
| Friday | 38146 | 3174 | 41320 | |
| 92.3 | 7.7 | 100.0 | ||
| 15.7 | 15.1 | 15.7 | ||
| Duration of the appointment in minutes | ||||
| < 30 minutes | 71104 | 5573 | 76677 | <0.001 |
| 92.7 | 7.3 | 100.0 | ||
| 29.3 | 26.4 | 29.1 | ||
| 30 to 60 minutes | 168762 | 15209 | 183971 | |
| 91.7 | 8.3 | 100.0 | ||
| 69.6 | 72.2 | 69.8 | ||
| > 60 minutes | 2521 | 295 | 2816 | |
| 89.5 | 10.5 | 100.0 | ||
| 1.0 | 1.4 | 1.1 | ||
| Appointment lead time/scheduled ahead days | ||||
| Less than a day | 23294 | 545 | 23839 | <0.001 |
| 97.7 | 2.3 | 100.0 | ||
| 9.6 | 2.6 | 9.1 | ||
| Within 2 weeks | 62352 | 4422 | 66774 | |
| 93.4 | 6.6 | 100.0 | ||
| 25.7 | 21.0 | 25.3 | ||
| More than 2 weeks | 156741 | 16110 | 172851 | |
| 90.7 | 9.3 | 100.0 | ||
| 64.7 | 76.4 | 65.6 | ||
| Provider specialty | ||||
| Not attributed | 13871 | 1495 | 15366 | <0.001 |
| 90.3 | 9.7 | 100.0 | ||
| 5.7 | 7.1 | 5.8 | ||
| Primary care | 116808 | 9395 | 126203 | |
| 92.6 | 7.4 | 100.0 | ||
| 48.2 | 44.6 | 47.9 | ||
| Specialty care | 111708 | 10187 | 121895 | |
| 91.6 | 8.4 | 100.0 | ||
| 46.1 | 48.3 | 46.3 | ||
| Provider type | ||||
| Medical Doctor (MD)/physician | 139853 | 11340 | 151193 | <0.001 |
| 92.5 | 7.5 | 100.0 | ||
| 57.7 | 53.8 | 57.4 | ||
| Non-physician/Allied Health | 102534 | 9737 | 112271 | |
| 91.3 | 8.7 | 100.0 | ||
| 42.3 | 46.2 | 42.6 | ||
| Medicare | ||||
| No | 206690 | 19175 | 225865 | <0.001 |
| 91.5 | 8.5 | 100.0 | ||
| 85.3 | 91.0 | 85.7 | ||
| Yes | 35697 | 1902 | 37599 | |
| 94.9 | 5.1 | 100.0 | ||
| 14.7 | 9.0 | 14.3 | ||
| Medicaid | ||||
| No | 218772 | 17376 | 236148 | <0.001 |
| 92.6 | 7.4 | 100.0 | ||
| 90.3 | 82.4 | 89.6 | ||
| Yes | 23615 | 3701 | 27316 | |
| 86.5 | 13.6 | 100.0 | ||
| 9.7 | 17.6 | 10.4 | ||
| Commercial | ||||
| No | 234819 | 20007 | 254826 | <0.001 |
| 92.2 | 7.9 | 100.0 | ||
| 96.9 | 94.9 | 96.7 | ||
| Yes | 7568 | 1070 | 8638 | |
| 87.6 | 12.4 | 100.0 | ||
| 3.1 | 5.1 | 3.3 | ||
| Other government insurance | ||||
| No | 235492 | 20630 | 256122 | <0.001 |
| 92.0 | 8.1 | 100.0 | ||
| 97.2 | 97.9 | 97.2 | ||
| Yes | 6895 | 447 | 7342 | |
| 93.9 | 6.1 | 100.0 | ||
| 2.8 | 2.1 | 2.8 | ||
| Prior no-show, one year retrospectively | ||||
| No | 209448 | 12798 | 222246 | <0.001 |
| 94.2 | 5.8 | 100.0 | ||
| 86.4 | 60.7 | 84.4 | ||
| Yes | 32939 | 8279 | 41218 | |
| 79.9 | 20.1 | 100.0 | ||
| 13.6 | 39.3 | 15.6 | ||
First row has frequencies; second row has row percentages, and third row has column percentages
The percentages have been rounded to a decimal, so they might not add up to 100%.
Male patients had a higher no-show rate (8.3%) than female patients (7.8%), despite there being more female appointments (54.1%) than male appointments (45.9%), at P<0.001. Adults (48.9%) and older adults (32.9%) had more appointments than children (11.4%), adolescents (6.1%), and infants (0.7%). However, adults (10.8%), adolescents (9.2%), and children (9.0%) had a higher no-show rate than infants (7.0%) and older adults (3.3%), at P<0.001. Although English-speaking patients (98.2%) had more appointments than Spanish-speaking patients (1.2%) and others such as Hmong and Sign languages (0.7%), Spanish speakers had a higher no-show rate (14.2%) than English-speaking patients (7.8%) and others (1.8%), at P<0.001. More patients (69.8%) had appointments lasting 30-60 minutes, followed by those lasting < 30 minutes (25.3%) and > 60 minutes (1.1%). However, the no-show rate was higher among patients who had appointments lasting > 60 minutes (10.5%), followed by appointments lasting 30-60 minutes (8.3%), and < 30 minutes (7.3%). More patients (65.5%) had more than 4 weeks of appointment lead time, followed by those with less than 2 weeks (25.3%) and less than a day (9.1%). Patients with more than 4 weeks of appointment lead time (9.3%) had a higher no-show rate than those with less than 2 weeks (6.6%) and less than a day (2.3%), at P<0.001. Patients who had no prior no-shows (84.4%) had more appointments than those who had prior no-shows (15.6%). Patients with prior no-shows, on the other hand, had a higher no-show rate (20.1%) than patients without prior no-shows (5.8%), at P<0.001. Patients with primary care appointments (47.9%) had more appointments than those with specialty care (46.3%) and those without a provider specialty (5.8%). However, the no-show rate was higher among patients’ appointments not attributed to a provider specialty (9.7%), compared to specialty care (8.4%) and primary care appointments (7.4%), at P<0.001. Patients had more appointments with physicians (57.4%) than with non-physician/allied health professionals (42.6%), and no-show rates were higher with allied health professionals (8.7%) than with physicians (7.4%), at P<0.001. Medicare patients had fewer appointments (14.3%) than those without Medicare insurance (85.7%), and the no-show rate was higher for those without Medicare insurance (8.5%) than for Medicare patients (5.1%), at P<0.001. Medicaid patients had fewer appointments (10.4%) than those without Medicaid insurance (89.6%), but their no-show rate was higher (13.6%) than that of patients without Medicaid (7.5%), at P<0.001. Patients with commercial insurance had fewer appointments (3.3%) than those without commercial insurance (96.7%), but their no-show rate was higher (7.9%) than that of patients without commercial insurance (5.1%), at P<0.001.
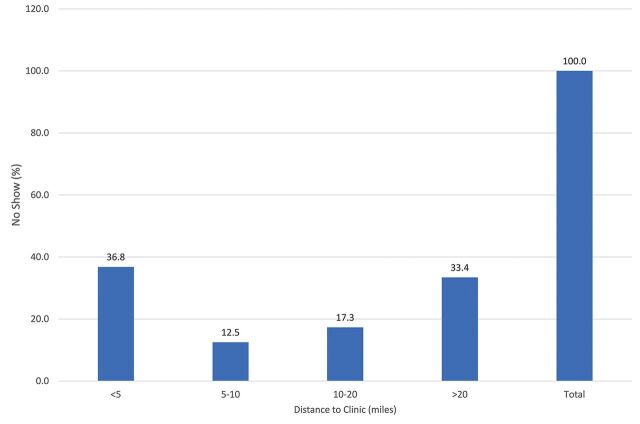
The impact of patient distance to the clinic on no-shows is shown in Figure 1. Of the 21,077 no-shows in 2021, patients who lived < 5 miles from the clinic (36.8%) and > 20 miles (33.4%) had a higher no-show than those who lived between 10–20 miles (17.3%) and 5–10 miles (12.5%), at P=0.001.
Figure 1.
Impact of patient distance to the clinic on no-show, 2021 (n=21,077), P=0.001
The adjusted analysis of factors associated with no-show appointments in a rural healthcare system in 2021 is presented in Table 2. Adjusted analysis indicates that for every unit increase in patient distance to the clinic, the odds of no-show were similar to patients who showed up for their appointment (OR:1.00, 95% CI: 1.00-1.00). In addition, other factors were statistically significantly associated with no-shows in the adjusted model. Male patients were more likely to miss appointments than female patients (OR:1.14, 95% CI: 1.11-1.18). Older adults were less likely to miss appointments than infants (OR:0.35, 95% CI: 0.28-0.43). Patients who spoke other languages, such as Hmong and sign (OR:2.85, 95% CI: 2.52-3.22) and Spanish (OR:1.34, 95% CI: 1.20-1.50), were more likely to miss appointments than English speakers. Patients with appointments lasting 30 to 60 minutes were more likely to miss them than patients with appointments lasting < 30 minutes (OR:1.05, 95% CI: 1.01-1.09). Patients with more than 4 weeks of appointment lead time (OR:5.45, 95% CI: 4.98-5.97), and those with less than 2 weeks (OR:3.05, 95% CI: 2.78-3.36) were more likely to miss appointments than patients with less than a day of lead time. Patients with specialty care appointments (OR:0.83, 95% CI: 0.77-0.88), and those with primary care appointments (OR:0.73, 95% CI: 0.68-0.78) were less likely to miss appointments than patients who were not attributed to a provider specialty. Patients who had appointments with allied health professionals were more likely to miss them than patients who had appointments with physicians (OR:1.18, 95% CI: 1.15-1.22). Medicare patients were less likely to miss appointments than non-Medicare patients (OR:0.90, 95% CI: 0.85-0.96). Medicaid patients were more likely to miss appointments than non-Medicaid patients (OR:1.56, 95% CI: 1.49-1.63). Patients with commercial insurance were more likely to miss appointments than patients with no commercial insurance (OR:1.32, 95% CI: 1.23-1.42). Patients with prior no-show history were more likely to miss appointments than patients with no prior no-show history (OR:4.42, 95% CI: 4.27-4.48).
Table 2.
Factors associated with no-show (Adjusted analysis)
| Study variables | OR | Lower 95% CI | Upper 95% CI | Sig |
|---|---|---|---|---|
| Patient distance to the clinic | 1.00 | 1.00 | 1.00 | *** |
| Patient gender: Female | Ref. | |||
| Male | 1.14 | 1.11 | 1.18 | *** |
| Age: Infants (1 year) | Ref. | |||
| Children (1-12 years) | 0.87 | 0.71 | 1.08 | |
| Adolescents (13-17 years) | 0.89 | 0.72 | 1.10 | |
| Adults (18-64 years) | 1.02 | 0.83 | 1.25 | |
| Older adults (65 and older) | 0.35 | 0.28 | 0.43 | *** |
| Patient language: English | Ref. | |||
| Spanish | 1.34 | 1.20 | 1.50 | *** |
| Other (Hmong, Sign, etc.) | 2.85 | 2.52 | 3.22 | *** |
| Number of appointments scheduled: One to two | Ref. | |||
| Three to four | 0.87 | 0.83 | 0.91 | *** |
| Five to six | 0.77 | 0.73 | 0.82 | *** |
| Seven to eight | 0.71 | 0.67 | 0.77 | *** |
| Nine to ten | 0.66 | 0.61 | 0.72 | *** |
| More than ten | 0.51 | 0.47 | 0.54 | *** |
| Appointment month: January | Ref. | |||
| February | 0.96 | 0.86 | 1.07 | |
| March | 0.88 | 0.79 | 0.97 | ** |
| April | 0.94 | 0.85 | 1.04 | |
| May | 0.93 | 0.84 | 1.03 | |
| June | 1.06 | 0.96 | 1.17 | |
| July | 0.91 | 0.82 | 1.00 | ** |
| August | 0.86 | 0.78 | 0.94 | *** |
| September | 0.92 | 0.84 | 1.01 | * |
| October | 0.82 | 0.75 | 0.89 | *** |
| November | 0.79 | 0.72 | 0.86 | *** |
| December | 0.75 | 0.69 | 0.82 | *** |
| Appointment day of the week | Ref. | |||
| Tuesday | 0.92 | 0.88 | 0.96 | *** |
| Wednesday | 0.83 | 0.79 | 0.87 | *** |
| Thursday | 0.83 | 0.79 | 0.87 | *** |
| Friday | 0.82 | 0.78 | 0.86 | *** |
| Duration of the appointment in minutes | Ref. | |||
| 30 to 60 minutes | 1.05 | 1.01 | 1.09 | *** |
| > 60 minutes | 0.99 | 0.86 | 1.13 | |
| Appointment lead time/: Less than a day | Ref. | |||
| Within 2 weeks | 3.05 | 2.78 | 3.36 | *** |
| More than 4 weeks | 5.45 | 4.98 | 5.97 | *** |
| Provider specialty: Not attributed | Ref. | |||
| Primary care | 0.73 | 0.68 | 0.78 | *** |
| Specialty care | 0.83 | 0.77 | 0.88 | *** |
| Provider type: Medical Doctor (MD)/physician | Ref. | |||
| Non-physician/Allied health | 1.18 | 1.15 | 1.22 | *** |
| Medicare: No | Ref. | |||
| Yes | 0.90 | 0.85 | 0.96 | *** |
| Medicaid: No | Ref. | |||
| Yes | 1.56 | 1.49 | 1.63 | *** |
| Commercial: No | Ref. | |||
| Yes | 1.32 | 1.23 | 1.42 | *** |
| Other government insurance: No | Ref. | |||
| Yes | 1.00 | 0.90 | 1.11 | |
| Prior no-show, one year retrospectively: No | Ref. | |||
| Yes | 4.42 | 4.27 | 4.58 | *** |
* P<0.05;
** P<0.01,
***; P<0.001
Discussion
No-shows have a negative impact on healthcare outcomes, and prior research found no differences in no-show rates based on patient location.11 However, it was unclear whether patients’ distance from the clinic is related to higher no-show rates in a rural setting or in a rural provider network. Our study looked at the relationship between patient distance from the clinic and their likelihood of missing appointments (no-shows). The bivariate analysis revealed that patients who lived < 5 miles from the clinic and those who lived > 20 miles away had higher no-show rates than those who lived between 5 and 20 miles away. This finding is significant, because it suggests that patient distance to the clinic is a substantial factor that can influence appointment attendance. Patients who live close to the clinic may believe it is simple to reschedule or make up a missed appointment, whereas patients who live far away may face more logistical challenges in attending appointments, such as transportation issues. Understanding what causes no-shows can help clinics and healthcare providers develop targeted interventions to improve attendance rates. Clinics in areas where many patients live more than 20 miles away, for example, may want to consider providing transportation assistance to help these patients get to their appointments. Clinics in areas where many patients live within 5 miles of the clinic may want to implement reminder systems or other interventions to help these patients keep their appointments. Overall, the findings of this study emphasize the importance of taking patient distance to the clinic into account when analyzing and addressing factors that contribute to no-show rates.
Transportation issues are frequently cited as a major barrier to healthcare access, which could explain why patients who lived further away from the clinic had a higher no-show rate, particularly in rural areas, for those with lower incomes, and for those who are under/uninsured.9,10 Increased travel times and distances may necessitate rescheduling or delaying appointments.10 In a study of 200 children who had a history of missing clinical appointments, 51% of parents cited transportation issues as the primary reason for not attending appointments.7 A second study of 183 caregivers of urban children discovered that transportation barriers accounted for 50% of no-shows.8 Vehicle access was a primary predictor of whether patients in rural Appalachian mountains (60-90 miles from central healthcare facilities) could receive routine health care.9 While transportation is a significant barrier, it does not account for the entire problem and may not explain why patients who lived closer to the clinic (within 5 miles) had a higher no-show rate. Forgetfulness, personal health issues, family and employer obligations, and other issues such as long clinic wait times, bad weather, and financial problems are all major reasons.20
We also discovered that certain patient demographics (gender, age, and language) influence no-shows. Male patients were found to be 1.1 times more likely than female patients to miss appointments, according to the study. This finding is significant, because it suggests that when developing interventions to reduce no-show rates, clinics and healthcare providers should consider gender-based factors. To improve attendance rates, they may need to conduct targeted outreach efforts or provide appointment reminder systems tailored specifically to male patients. Furthermore, the study discovered that older adults were 0.4 times less likely to miss appointments than infants. This finding emphasizes the importance of taking age-related factors into account when analyzing patient no-show rates. To improve infant and young child attendance rates, healthcare providers may want to implement age-specific interventions, such as sending appointment reminders to parents or guardians. Finally, the study discovered that patients who spoke other languages (Hmong and Sign) and Spanish were 2.9 and 1.3 times more likely to miss appointments than English speakers, respectively. This finding emphasizes the significance of overcoming language barriers in healthcare settings. Language assistance services or translated materials may be offered by providers to improve communication and reduce the likelihood of missed appointments among patients with Limited-English-proficient (LEP). Overall, these findings emphasize the importance of considering a variety of factors that may influence patient attendance rates, such as gender, age, and language barriers. Healthcare providers can improve attendance rates and ensure patients receive the care they require by developing targeted interventions that address these factors.
Previous research has found a link between a higher no-show rate and younger patients; however, there were no differences in the no-show rate between male and female participants.11 Our findings have similarities and differences with a previous retrospective cohort analysis in the UK, which discovered that males (compared to females) were 1.1 times more likely to miss appointments, older patients aged more than 90 years were 2.2 times more likely to miss appointments, but younger patients aged 16-30 years were 1.2 times more likely to miss appointments.13 Previous research21 indicates that communication barriers frequently impede LEP patient no-shows, and the number of LEP patients in the U.S. is growing. Patients who do not understand the scheduling procedure or why attending a future appointment is critical may miss it, and when language is a barrier, both patients and providers risk missing out on critical information. Patients also missed appointments due to cultural insensitivity and felt disrespected by their healthcare providers or medical staff.4,21 Other issues associated with missing appointments without notifying clinic staff include emotions, perceived disrespect, and a lack of understanding of the scheduling system.4 Additionally, many patients experienced anticipatory fear and anxiety about both procedures and bad news about their diagnosis or health status.4
Moreover, we discovered that specific patient appointment characteristics (lead time and prior no-show history) influence no-shows. We discovered that patients with more than 4 weeks of appointment lead time were 5.5 times more likely to miss appointments than patients with less than a day of lead time. This finding is significant, because it suggests that when scheduling appointments, clinics and healthcare providers should consider the length of appointment lead times. Offering more flexible scheduling options, such as same-day appointments or shorter lead times, may help reduce missed appointments. Furthermore, patients with a prior no-show history were found to be 4.4 times more likely to miss appointments than patients with no prior no-show history. This finding emphasizes the importance of keeping track of and dealing with patient no-shows. To improve attendance rates, healthcare providers may want to implement targeted interventions, such as appointment reminders or follow-up phone calls, for patients who have a history of missed appointments. In general, these findings emphasize the importance of taking into account a variety of factors that can influence patient attendance rates, such as appointment lead time and prior no-show history. Healthcare providers can improve attendance rates and ensure patients receive the care they require by developing targeted interventions that address these factors.
Appointment lead times influence clinic no-show rates. A 12-month cross-sectional study15 of 51,529 ophthalmology appointments discovered that clinic no-show rates increased as appointment lead time increased. With a 2-week lead time for appointments, the average no-show rate was 9.1% for the resident and 2.4% for the faculty clinics, respectively. Another study that examined administrative data from the Veterans Administration Corporate Data Warehouse, including 1,206,271 unique appointment records at 13 Veterans Administration Medical Centers, discovered that a person’s historical attendance behavior in the 2 years preceding the current appointment is the best predictor of whether they will miss an appointment.16
Furthermore, we found that no-shows are impacted by specific provider characteristics (provider type and specialty). Patients who had appointments with allied health professionals were found to be 1.2 times more likely to miss them than patients who had appointments with physicians. This finding is significant, because it suggests that clinics and healthcare providers should consider the type of provider when scheduling appointments. Offering more flexible scheduling options, such as scheduling appointments with physicians rather than allied health professionals, could help reduce the likelihood of missed appointments. Moreover, patients with specialty care appointments and those with primary care appointments were 0.8 and 0.7 times less likely to miss appointments, respectively, than patients who were not assigned to a provider specialty, according to our study. This discovery emphasizes the significance of provider continuity in patient care. When patients have a designated provider who is familiar with their medical history and needs, they are more likely to attend appointments. Ultimately, these findings indicate that provider specialty should be considered when analyzing and addressing patient no-show rates. Understanding how different types of providers influence appointment attendance allows healthcare providers to develop targeted interventions to improve attendance rates and ensure patients receive the care they require. Provider features can impact no-show rates. While limited studies were found to help explain this section of our finding, a study of 1,252,127 appointments at a large tertiary hospital in Seoul, Korea, discovered that online/telephone appointments for treatment and surgery had much higher no-show odds ratios.12
Finally, we discovered that no-shows are affected by insurance status. Our research reveals that Medicare patients were 0.9 times less likely to miss appointments than non-Medicare patients. This finding is significant, because it suggests that having insurance coverage, such as Medicare, may increase the likelihood that patients will attend appointments. This finding also emphasizes the importance of expanding insurance coverage to ensure that all patients have access to healthcare. Furthermore, we discovered that Medicaid patients were 1.6 times more likely to miss appointments than non-Medicaid patients, and commercial insurance patients were 1.3 times more likely to miss appointments than non-commercial insurance patients. These findings imply that the type of insurance coverage may have an effect on appointment attendance. To improve attendance rates among patients with Medicaid or commercial insurance, healthcare providers may need to consider implementing targeted interventions such as appointment reminders or outreach efforts. Overall, these findings emphasize the importance of taking insurance status into account when analyzing and addressing patient no-show rates.
Previous research conducted outside of the United States discovered that the type of insurance is a significant factor in no-shows.12 Our findings are similar but also differ with a recent study14 that identified factors associated with no-show rates in an academic otolaryngology practice that discovered increased clinic no-show rates are associated with insurance type. Patients with Medicaid (28%), Medicare (15.3%), and commercial insurance (12.9%) had significantly different overall no-show rates.14 While this study focused on a medical specialty involving the ears, nose, and throat, and our findings were similar, our study focused on all specialty care and primary care.
Study Strengths and Limitations
First, the study used a large sample of patient appointments (N=263,464) from an integrated rural health scheduling system (MCHS). Our findings, however, are unweighted and may not be applicable to predominantly urban health system settings, nor do they apply nationally. Second, while removing duplicate appointment data from the same patient assisted us in determining the correct study sample, our sample does not capture the total number of scheduled appointments for the patient over time, because we only included the most recent patient appointments if they had more than one within a 12-month period in 2021, despite patients having multiple appointments over time. This implies that our findings do not apply to the patient’s total number of scheduled appointments or to patients who had multiple appointments over time. Third, while we included language (English, Spanish, and others) to identify differences, the sample profile did not allow for comparison of race and ethnic groups, because rural Wisconsin is predominantly White, English speakers. Finally, we were unable to account for the patients’ socioeconomic status, level of education, and medical conditions, all of which can play a significant role in no-shows.22 These strengths and limitations can be used to interpret our findings and inform future research.
Study Implications
Despite these limitations, our findings could have far-reaching implications for policy and clinical practice. To reduce no-show rates, the first step is perhaps to identify a large at-risk population for no-shows and address the issue using a multi-method approach based on our findings. This approach has been shown to reduce no-shows and could be used in rural clinic settings. For example, after an intervention that identified a large at-risk population for no-shows focused on a cohort of 141 patients’ study from the overall clinic, primarily African American women on Medicaid, the rate of no-show appointments in the cohort fell from 33.3% to 17.7%, and the overall clinic rate fell from 10% to 7%; this decrease persisted for the 33-month observation period following the intervention.23 The greatest improvement in appointment keeping occurred after a modified advanced access schedule was implemented clinic-wide.
Secondly, we recommend more personalized reminder interventions to reduce no-shows by reducing the lag time between setting the appointment and the actual date of the appointment to improve access to care. This is because a recent retrospective study24 using electronic medical record data from 11 facilities affiliated with a New York City-based network of Federally Qualified Health Centers, including 53,149 visits for 41,495 unique patients, discovered that reminders had little effect on no-show rates overall (no show rate before: 41.6%, after: 42.1%). There was a 2% decrease in no-shows for individuals who had appointments before and after the reminder. Another study included 534 new and 1,920 follow-up patients from a children’s hospital’s pulmonology and gastroenterology clinics, and the overall rate of no-shows was significantly lower for visits scheduled within 0 to 30 days compared to 30 days or more (23% vs. 47%).25 This suggests that the time to appointment is a risk factor for no-shows, and that more personalized reminder interventions may reduce no-shows to improve access to care, particularly among medically underserved populations.
Finally, because no-shows have a negative impact on healthcare access, several healthcare systems have developed evidence-based predictive models to predict appointment no-shows and develop strategies to mitigate their consequences.2,17,33,22,26–32 These models included those that predicted no-shows in specific diseases or conditions (HIV-infected patients),29 no-show probabilities incorporated into a scheduling system that achieved a $100 projected benefit per patient,31 planning systems that reduced patients’ waiting time for medical services by 6% to 8%,26 and scheduling systems that increased center utilization from 46% to 72.9%.33 Some other evidence-based predictive model used electronic health records from a single general pediatrics clinic,26 created a large data framework for identifying no-shows through feature engineering and machine learning,2 and proposed a model to predict ambulatory patients’ no-shows to exam appointments at a radiology department of a major Brazilian public hospital.27 While models for predicting no-shows and devising countermeasures have been developed, the majority of research has recommended situation-specific solutions, and the current literature has failed to provide generally applicable principles for designing appointment systems, particularly for rural communities. Our study shed light on rural patients to reduce patient no-shows, improve clinic performance and efficiency, and develop contextual measures aimed at identifying and addressing factors and reasons for no-show rates in underserved rural patient populations.
Understanding the generally accepted levels of no-shows is crucial for interpreting the implications of our findings. Existing literature suggests varying thresholds of acceptable no-show rates across different healthcare settings and specialties, but any level of no-shows can have significant repercussions on clinic operations and patient outcomes.3,5 The 8% no-show rate identified in our study indicates a substantial burden on the healthcare system, emphasizing the urgency of addressing this issue. Our findings contribute to the ongoing dialogue about acceptable levels of no-shows and offer insights for establishing more context-specific standards, particularly for rural healthcare providers.6,7 It is essential for future studies to continue exploring this aspect, focusing on establishing benchmarks that are realistic, sustainable, and in the best interest of both healthcare providers and patients.
Conclusion
Our results demonstrate that patients’ distance from the clinic, male patients, Spanish speakers, younger patients, longer lead time, prior no-show histories, appointments not assigned to a specialty, and Medicaid patients all increased the likelihood of no-shows in a rural health system. Examining the long-term health outcomes of patients who have no-shows is one of the research recommendations. Changes in practice or procedures to address this issue include offering transportation, increasing awareness and access to personalized reminders and social services, ensuring that social care workers are contacting clients with higher no-show rates, and counseling patients on the value of preventative care.
Acknowledgments
The authors extend their sincere appreciation to David S Puthoff, PhD, from the Office of Research and Sponsored Programs at Marshfield Clinic Research Institute for his valuable intellectual contributions and editorial assistance. The Analytics and Data Science Team and the Marshfield Clinic Research Institute - Office of Research Computing and Analytics at the Marshfield Clinic Health System are also acknowledged for their indispensable contribution to this study. Their expertise and commitment have played a pivotal role in the success of this research project.
References
- 1.Marbouh D, Khaleel I, Al Shanqiti K, et al. . Evaluating the impact of patient no-shows on service quality. Risk Manag Healthc Policy. 2020;13:509-517. doi: 10.2147/RMHP.S232114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daghistani T, AlGhamdi H, Alshammari R, AlHazme RH.. Predictors of outpatients’ no-show: big data analytics using apache spark. Journal of Big Data. 2020;7(1):108. doi: 10.1186/s40537-020-00384-9. [DOI] [Google Scholar]
- 3.Li Y, Tang SY, Johnson J, Lubarsky DA.. Individualized No-Show Predictions: Effect on Clinic Overbooking and Appointment Reminders. Production and Operations Management. 2019;28(8):2068-2086. doi: 10.1111/poms.13033. [DOI] [Google Scholar]
- 4.Lacy NL, Paulman A, Reuter MD, Lovejoy B.. Why we don’t come: patient perceptions on no-shows. Ann Fam Med. 2004;2(6):541-545. doi: 10.1370/afm.123.Medline [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lacy NL, Paulman A, Reuter MD, Lovejoy B.. Why we don’t come: patient perceptions on no-shows. Ann Fam Med. 2004;2(6):541-545. doi: 10.1370/afm.123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amberger C, Schreyer D.. What do we know about no-show behavior? A systematic, interdisciplinary literature review. Journal of Economic Surveys. 2022;1-40. doi: 10.1111/joes.12534. Available at: https://onlinelibrary.wiley.com/doi/epdf/10.1111/joes.12534 [DOI] [Google Scholar]
- 7.Silver D, Blustein J, Weitzman BC.. Transportation to clinic: findings from a pilot clinic-based survey of low-income suburbanites. J Immigr Minor Health. 2012;14(2):350-355. doi: 10.1007/s10903-010-9410-0 [DOI] [PubMed] [Google Scholar]
- 8.Yang S, Zarr RL, Kass-Hout TA, Kourosh A, Kelly NR.. Transportation barriers to accessing health care for urban children. J Health Care Poor Underserved. 2006;17(4):928-943. doi: 10.1353/hpu.2006.0137 [DOI] [PubMed] [Google Scholar]
- 9.Arcury TA, Preisser JS, Gesler WM, Powers JM.. Access to transportation and health care utilization in a rural region. J Rural Health. 2005;21(1):31-38. doi: 10.1111/j.1748-0361.2005.tb00059.x. [DOI] [PubMed] [Google Scholar]
- 10.Syed ST, Gerber BS, Sharp LK.. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38(5):976-993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boshers EB, Cooley ME, Stahnke B.. Examining no-show rates in a community health centre in the United States. Health Soc Care Community. 2022;30(5):e2041-e2049. doi: 10.1111/hsc.13638. [DOI] [PubMed] [Google Scholar]
- 12.Suk MY, Kim B, Lee SG, You CH, Hyun Kim T.. Evaluation of patient no-shows in a tertiary hospital: Focusing on modes of appointment-making and type of appointment. Int J Environ Res Public Health. 2021;18(6):3288. doi: 10.3390/ijerph18063288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ellis DA, McQueenie R, McConnachie A, Wilson P, Williamson AE.. Demographic and practice factors predicting repeated non-attendance in primary care: a national retrospective cohort analysis. Lancet Public Health. 2017;2(12):e551-e559. doi: 10.1016/S2468-2667(17)30217-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fiorillo CE, Hughes AL, I-Chen C, et al. . Factors associated with patient no-show rates in an academic otolaryngology practice. Laryngoscope. 2018;128(3):626-631. doi: 10.1002/lary.26816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McMullen MJ, Netland PA.. Lead time for appointment and the no-show rate in an ophthalmology clinic. Clin Ophthalmol. 2015;9:513-516. doi: 10.2147/OPTH.S82151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Milicevic AS, Mitsantisuk K, Tjader A, Vargas DL, Hubert TL, Scott B.. Modeling patient no-show history and predicting future appointment behavior at the veterans administration’s outpatient mental health clinics: NIRMO-2. Mil Med. 2020;185(7-8):e988-e994. doi: 10.1093/milmed/usaa095. [DOI] [PubMed] [Google Scholar]
- 17.Lin Q, Betancourt B, Goldstein BA, Steorts RC.. Prediction of appointment no-shows using electronic health records. J Appl Stat. 2020;47(7):1220-1234. doi: 10.1080/02664763.2019.1672631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.StataCorp. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC. [Google Scholar]
- 19.Korngiebel DM, Mooney SD.. Considering the possibilities and pitfalls of Generative Pre-trained Transformer 3 (GPT-3) in healthcare delivery. NPJ Digit Med. 2021;4(1):93. doi: 10.1038/s41746-021-00464-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ofei-Dodoo S, Kellerman R, Hartpence C, Mills K, Manlove E.. Why Patients Miss Scheduled Outpatient Appointments at Urban Academic Residency Clinics: A Qualitative Evaluation. Kans J Med. 2019;12(3):57-61. [PMC free article] [PubMed] [Google Scholar]
- 21.McNeilly MD, Anderson NB, Armstead CA, et al. . The perceived racism scale: a multidimensional assessment of the experience of white racism among African Americans. Ethn Dis. 1996;6(1-2):154-166. [PubMed] [Google Scholar]
- 22.Carreras-García D, Delgado-Gómez D, Llorente-Fernández F, Arribas-Gil A.. Patient No-Show Prediction: A Systematic Literature Review. Entropy (Basel). 2020;22(6):675. Published 2020 Jun 17. doi: 10.3390/e22060675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DuMontier C, Rindfleisch K, Pruszynski J, Frey JJ 3rd.. A multi-method intervention to reduce no-shows in an urban residency clinic. Fam Med. 2013;45(9):634-641. [PubMed] [Google Scholar]
- 24.Ruggeri K, Folke T, Benzerga A, et al. . Nudging New York: adaptive models and the limits of behavioral interventions to reduce no-shows and health inequalities. BMC Health Serv Res. 2020;20(1):363. Published 2020 Apr 26. doi: 10.1186/s12913-020-05097-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Drewek R, Mirea L, Adelson PD.. Lead Time to Appointment and No-Show Rates for New and Follow-up Patients in an Ambulatory Clinic. Health Care Manag (Frederick). 2017;36(1):4-9. doi: 10.1097/HCM.0000000000000148 [DOI] [PubMed] [Google Scholar]
- 26.Huang Y, Hanauer DA.. Patient no-show predictive model development using multiple data sources for an effective overbooking approach. Appl Clin Inform. 2014;5(3):836-860. Published 2014 Sep 24. doi: 10.4338/ACI-2014-04-RA-0026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Benedito Zattar da Silva R, Fogliatto FS, Garcia TS, Faccin CS, Zavala AAZ.. Modelling the no-show of patients to exam appointments of computed tomography. Int J Health Plann Manage. 2022;37(5):2889-2904. doi: 10.1002/hpm.3527 [DOI] [PubMed] [Google Scholar]
- 28.Cayirli T, Veral E.. Outpatient scheduling in health care: A review of literature. Production and Operations Management. 2009;12(4):519-549. doi: 10.1111/j.1937-5956.2003.tb00218.x. [DOI] [Google Scholar]
- 29.Woodward B, Person A, Rebeiro P, Kheshti A, Raffanti S, Pettit A.. Risk Prediction Tool for Medical Appointment Attendance Among HIV-Infected Persons with Unsuppressed Viremia. AIDS Patient Care STDS. 2015;29(5):240-247. doi: 10.1089/apc.2014.0334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Torres O, Rothberg MB, Garb J, Ogunneye O, Onyema J, Higgins T.. Risk factor model to predict a missed clinic appointment in an urban, academic, and underserved setting. Popul Health Manag. 2015;18(2):131-136. doi: 10.1089/pop.2014.0047 [DOI] [PubMed] [Google Scholar]
- 31.Daggy J, Lawley M, Willis D, et al. . Using no-show modeling to improve clinic performance. Health Informatics J. 2010;16(4):246-259. doi: 10.1177/1460458210380521 [DOI] [PubMed] [Google Scholar]
- 32.Norris JB, Kumar C, Chand S, Moskowitz H, Shade SA, Willis DR.. An empirical investigation into factors affecting patient cancellations and no-shows at outpatient clinics. Decision Support Systems. 2014;57(1):428-443. doi: 10.1016/j.dss.2012.10.048. [DOI] [Google Scholar]
- 33.Glowacka KJ, Henry RM, May JH.. A hybrid data mining/simulation approach for modelling outpatient no-shows in clinic scheduling. Journal of the Operational Research Society. 2009;60(8):1056-1068. doi: 10.1057/jors.2008.177. [DOI] [Google Scholar]