Abstract
Introduction
Mouthguards (MGs) have the potential to prevent contact sport‐related dental injuries. However, varying perceptions of their effectiveness persist, influencing recommendations by dental professionals.
Aim
To assess the attitudes, knowledge, and perceptions of orthodontists, other dental practitioners (general dentists and other dental specialists), and orthodontic patients involved in contact sports regarding the use of MGs.
Methodology
A cross‐sectional survey was designed to collect information from dental clinicians (orthodontists and other dental practitioners) and their orthodontic patients about using MGs during sports participation. A convenience sampling technique was used to recruit the participants for an online survey. A total of 107 (32 males/75 females) dental clinicians and 147 (75 males/72 females) orthodontic patients (mean age 17.5 ± 5.84 years) participated in the study. Pre‐validated questionnaires, specifically designed for dental clinicians and orthodontic patients, were used. Data were analyzed using SPSS software (version 28.0; SPSS).
Results
Nearly 50% of dental clinicians have recently recommended MGs to their patients in their clinical practice out of which 59% preferred the stock type; 33% of dental clinicians enquired their patients about involvement in contact sports during initial visits. The majority of orthodontic patients acquired knowledge about MGs through the Internet. More than half of orthodontic patients expressed unwillingness to pay for MGs, and 89% of orthodontic patients found using MGs during contact sports uncomfortable.
Conclusion
The findings provide valuable insights into the practices and attitudes of dental clinicians and orthodontic patients regarding MGs, their recommendations, and the comfort levels associated with using them during contact sports.
Keywords: contact sports, mouthguards, orthodontic treatment
1. INTRODUCTION
With an increase in the quantum of involvement in sports activities, especially among children and adolescents, there has been a proportional increase in the risk of trauma to the orofacial structures. The prevalence of orofacial and dental trauma has been reported to range between 20% and 60% and is attributed to the orientation of anatomic structures that makes them vulnerable to the impact/trauma during sports activities (Bruggesser et al., 2020; Petrović et al., 2016). Complimenting this fact, the combined prevalence of orofacial and dental sports‐related injuries was determined to be 40.6% (Tewari et al., 2023)
The majority of orthodontic treatment occurs either before or during adolescence, a period marked by an increase in the occurrence of dental injuries during participation in contact sports (Love et al., 1998). Orthodontic patients who participate in contact sports during their course of fixed appliance therapy may be more liable to orofacial injuries as a result of loosening or debonding of brackets, arch wire distortion, damage to the dento‐alveolar structures, and soft tissue laceration (Maeda et al., 2008). Furthermore, a recent study has emphasized the significance of the presence and type of orthodontic brackets in influencing the stress and strain experienced during traumatic impacts (Alves et al., 2020).
Nevertheless, it is believed that some of the contact sport‐related dental trauma can be prevented by wearing a mouthguard (MG) as it sustains the impact of trauma and dissipates that energy, which would otherwise be detrimental to the underlying dentition (Newsome et al., 2001; Owtad et al., 2015). There are three types of MGs, namely pre‐fabricated MGs (stock MGs, which are not customized for the patient), mouth‐formed or “boil‐and‐bite” MGs (crafted from a thermoplastic material that becomes pliable when heated and shaped by the wearer), and custom‐made MGs (fabricated using dental impressions).
The American Dental Association (ADA) has established guidelines specifying the particular sports that necessitate the use of MGs (Using, 2006). Moreover, a meta‐analysis suggests that the likelihood of experiencing an orofacial injury is approximately two times greater when not using an MG during sport (Knapik et al., 2007). Despite the protective nature of MGs, there is still a reluctance to wear them during sports activities, even among players who are aware of their benefits (Bergman et al., 2017; O'Malley et al., 2012; Tiryaki et al., 2017). This reluctance may be attributed to challenges associated with carrying out normal physiological functions, among other factors.
Notably, persistent divergence in the overall perception of the effectiveness and utility of MGs exists, which affects recommendations by dental professionals (Bastian et al., 2020; Bussell & Barreto, 2014). Various factors contribute to this divergence, including their beliefs, the type of sport, patients' requests, treatment acceptance, patient disclosure of participation in contact sports, the nature of malocclusion, the level and frequency of sports involvement, the influence of previous dentist, and their clinical exposure to patients presented with traumatic injuries (Bastian et al., 2020; Bussell & Barreto, 2014). While several studies have explored players' views, (Chapman, 1990; Galic et al., 2018; Hayashi et al., 2020; Lieger & von Arx, 2006; Meyfarth et al., 2023; O'Malley et al., 2012; Sarao et al., 2021) data are scarce regarding orthodontists' and other dental professionals' standpoint regarding the importance of MGs and their use by athlete patients undergoing orthodontic treatment.
Hence, the aim of this cross‐sectional study was:
-
–
To report on the attitude, knowledge, and perception of orthodontists and other dental practitioners (general dentists and other dental specialists) toward MGs.
-
–
To report on the attitude and perception of orthodontic patients involved in contact‐sport activities toward the use of MGs.
2. MATERIALS AND METHOD
2.1. Study design
This cross‐sectional survey was designed to determine the knowledge, perceptions, practice, and attitudes of dental clinicians (orthodontists and other dental practitioners) and their orthodontic patients toward the use of mouth guards during sports participation. The protocol was approved by the Deanship of Research/Jordan University of Science and Technology (Research ID20070048).
2.2. Eligibility criteria
The eligibility requirements encompassed the following conditions: dental clinicians providing orthodontic treatment to patients and patients undergoing orthodontic treatment, possessing the capability to access online content in English, and providing informed consent for the utilization of the recorded data.
2.3. Recruitment
A convenience sampling technique was used to recruit participants for the study. Self‐administered Google Forms questionnaires were circulated between January and March 2023. The surveys were circulated through emails and WhatsApp groups to maximize the response rate and to include a diverse population. The participants included were orthodontists, their orthodontic patients, and dental practitioners (DP) in Jordan. Out of 152 dental specialists who received the survey link, 124 responded and once the data had been cleaned 107 responses were considered for the final analysis (response rate 81.6%).
A total of 107 (32 males/75 females) dental clinicians with varying years of experience from various clinical settings (governmental and private practices) participated in an online survey.
The survey included orthodontic patients who had received treatment from the participating dental clinicians. Out of 174 patients who received the survey link, 157 responded, and once the data had been cleaned 147 responses were considered for the final analysis (response rate 90%).
One hundred forty‐seven orthodontic patients (75 Males/72 Females) within the age range of 14–20 (mean age 17.5 ± 5.84 years) who were undergoing active orthodontic treatment (either with removable or fixed orthodontic appliances) and involved in active sports participated in the study.
2.4. Instrumentation
A pre‐validated 13‐item and a 10‐item questionnaire, (Bastian et al., 2020; Bussell & Barreto, 2014) tailored specifically for dental clinicians and orthodontic patients respectively were circulated through e‐mails and WhatsApp messages. Some of the questions, which were extracted from the previously conducted qualitative study (Bussell & Barreto, 2014; Lieger & von Arx, 2006), underwent reformulation by the researchers and were included in the questionnaire. All participants provided informed consent as part of the questionnaire. The questionnaire included multiple‐choice questions (MCQs).
2.5. Data collection
Data was collected through an online questionnaire disseminated to participants. The purpose of the survey was explained to the participants; it was emphasized, to the patients, that survey participation was voluntary, their participation would not affect their treatment and at any time they could stop taking the survey. Participation in the survey was anonymous and responses were kept confidential.
2.6. Statistical analysis
Statistical analysis was performed using SPSS software (version 28.0; SPSS). Descriptive statistics were computed for demographic information as well as individual patient responses. Data were analyzed statistically using the Chi‐square test with a 95% confidence interval. p < 0.05 was considered statistically significant.
3. RESULTS
3.1. Dental clinicians
Out of the 107 dental professionals who completed the survey, 48.6% were orthodontists, 33.6% were general dental practitioners (who work in an orthodontic practice and provide orthodontic treatment with removable appliances), and 19% were dental specialists other than orthodontists (endodontists, prosthodontists, pediatric dentists). Of those, 38% had more than 10 years, 30% had more than 5 years, and 32% had less than 5 years of professional experience.
3.1.1. Current clinical practice and attitude
The responses from the participants are shown in Table 1.
Table 1.
Responses of dental practitioners and Orthodontists to each item based on current clinical practice, attitude, perception, and knowledge about mouthguards.
| Items | Responses | Frequency distribution counts (%) | P value | |
|---|---|---|---|---|
| DP | Orthodontists | |||
| CURRENT CLINICAL PRACTICE AND ATTITUDE | ||||
|
Yes | 20 (36.4) | 15 (28.8) | 0.407 |
| No | 35 (63.6) | 37 (71.2) | ||
|
Yes | 27 (49.1) | 22 (42.3) | 0.482 |
| No | 28 (50.9) | 30 (57.7) | ||
|
Stock type | 19 (70) | 10 (45) | 0.067 |
| Boil and bite type | 0 | 3 (14) | ||
| Custom made | 8 (30) | 9 (41) | ||
|
Yes | 20 (74) | 8 (36) | 0.007* |
| No | 7 (26) | 14 (64) | ||
|
Yes | 5 (19) | 2 (9) | 0.348 |
| No | 22 (81) | 20 (91) | ||
|
Yes | 14 (25) | 17 (33) | 0.409 |
| No | 41 (75) | 35 (67) | ||
|
Yes | 13 (93) | 13 (76) | 0.217 |
| No | 1 (7) | 4 (24) | ||
|
Yes | 47 (85) | 41 (79) | 0.371 |
| No | 8 (15) | 11 (21) | ||
|
Yes | 40 (73) | 29 (56) | 0.067 |
| No | 15 (27) | 23 (44) | ||
|
Orthodontist | 46 (83.6) | 38 (73.1) | 0.120 |
| General dentist | 5 (9.1) | 2 (3.8) | ||
| Coach | 4 (7.3) | 9 (17.3) | ||
| Parents | 0 (0) | 2 (3.8) | ||
| PERCEPTION AND KNOWLEDGE ABOUT MOUTHGUARDS DURING ORTHODONTIC TREATMENT | ||||
|
Remove the appliance and wear a mouthguard during sport | 50 (91) | 43 (83) | 0.125 |
| Refrain from the sport until treatment completion | 4 (7) | 3 (5) | ||
| Mouthguard is not necessary during active sporting | 1 (2) | 6 (12) | ||
|
Wear a mouthguard during sport | 48 (87) | 43 (83) | 0.092 |
| Refrain from the sport until treatment completion | 6 (11) | 3 (5) | ||
| Mouthguard is not necessary during active sporting | 1 (2) | 6 (12) | ||
|
Foot ball | 1 (1.8) | 1 (1.9) | 0.472 |
| Basket ball | 1 (1.8) | 1 (1.9) | ||
| Hockey | 2 (3.6) | 1 (1.9) | ||
| Volley ball | 2 (3.6) | 1 (1.9) | ||
| All contact sports | 48 (87.3) | 42 (90.4) | ||
| Not necessary at all | 1 (1.8) | 6 (1.9) | ||
Statistically significant
Out of 107 respondents, almost one‐half (46%) of dental clinicians (55% DP and 45% Orthodontists) recommended MGs to their patients in their practice recently; 38% of the clinicians had more than 10 years, 30% had more than 5 years, and 32% had less than 5 years of professional experience. Among all the respondents, 33% of dental clinicians (57% DP and 43% Orthodontists) reported that they routinely enquire about their patients' engagement in contact sports as part of history assessment during the initial consultation. When questioned whether they would recommend the use of MG if they were informed by their patients later during treatment about their involvement in contact sports, 82% of them (53% DP and 47% Ortho) expressed a positive response. Almost two‐thirds of the participants (64%) believed that obtaining patient consent is essential before making a recommendation for the use of MGs.
Of those who recently recommended MGs for their patients, 59% (66% DP and 34% Orthodontist) recommended the use of stock‐type MGs (Figure 1). Among all the respondents, only 29% (45% DP and 55% Orthodontists) indicated that they have in‐office MG fabrication facilities and of those, 84% mentioned that they would charge the patient for this service.
Figure 1.
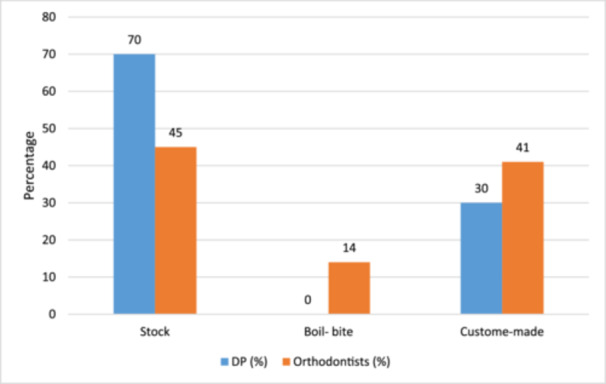
Type of mouthguards recommended by dental clinicians in their practice recently.
Of the dental clinicians who routinely recommended the use of MG during contact sports, 57% of them (71% DP and 29% Orthodontists) reported that their patients had complained of discomfort while wearing the MGs and the difference between DP and Orthodontists was statistically significant (p = 0.007). Additionally, 14% of them stated that their patients experienced trauma despite using the MG.
3.1.2. Dental clinicians' perception and knowledge about MG during orthodontic treatment
The majority of dental clinicians (84%) believed that the use of MGs is necessary and to be worn by orthodontic patients involved in all forms of contact sports. However, a few dental clinicians prioritize certain contact sports over others when it comes to mandating the use of MGs.
Of all the dental practitioners, 79% (55% DP and 45% Orthodontists) felt that the decision‐making with regard to the recommendation of MGs to orthodontic patients who actively play contact sports should primarily rest on orthodontists (Figure 2).
Figure 2.
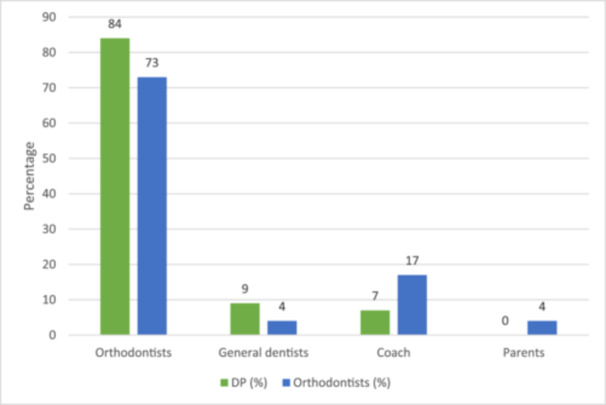
Perceptions of dental professionals concerning their role in decision‐making for recommending mouthguards to orthodontic patients.
Based on the orthodontic appliance type, the majority of dental practitioners claimed that they would advise their orthodontic patients with removable (87%) and fixed (85%) appliances to wear MGs during contact sports while the others recommended otherwise (Figures 3 and 4).
Figure 3.
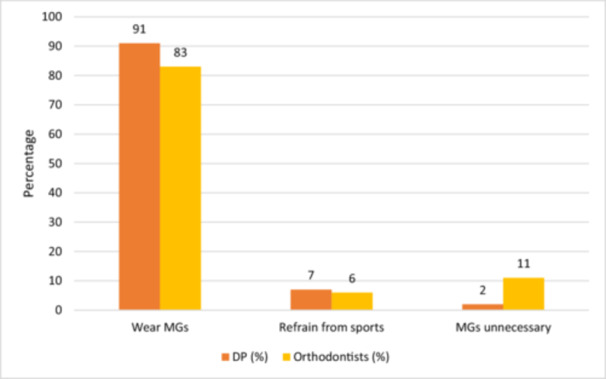
Dental Clinicians' perspectives on recommending mouthguards (MGs) for patients with removable appliances.
Figure 4.
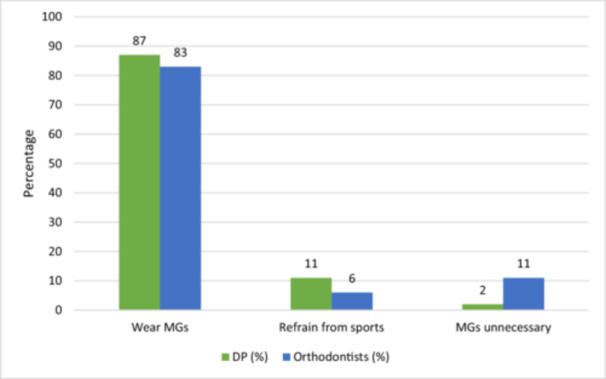
Dental clinicians' perspectives on recommending mouthguards (MGs) for patients with fixed appliance.
There were no statistically significant differences in most of the responses between the orthodontists and DP.
3.2. Patients
The descriptive data and the responses from the participants are shown in Tables 2 and 3 respectively. The distribution of subjects based on the type of sport is shown in Figure 5.
Table 2.
Demographic characteristics of the study population (orthodontic patients involved in contact sports).
| Age | 17.56 (5.84) years | |
| Gender | Females | 72 (49%) |
| Males | 75 (51%) | |
| Contact sports involved | Football | 60 (40.8%) |
| Martial arts | 35 (23.8%) | |
| Basketball | 28 (19%) | |
| Volley ball | 10 (6.8%) | |
| Hand ball | 7 (4.8%) | |
| Type of appliance | Fixed | 113 (76.9%) |
| Removable | 34 (23.1) | |
| Duration of appliance wear | Less than 6 months | 35 (23.8%) |
| 6months to year | 62 (42.2%) | |
| More than one year | 50 (34%) | |
Table 3.
Responses of orthodontic patients (involved in contact sports) to each item based on attitude and perception about mouthguards.
| Items | Response | Frequency distribution counts (%) | Total responses |
|---|---|---|---|
|
Yes | 65 (44.2%) | 127 |
| No | 62 (55.8%) | ||
|
Yes | 107 (72.8%) | 147 |
| No | 40 (27.2) | ||
|
Yes | 83 (56.5%) | 147 |
| No | 64 (43.5%) | ||
|
Orthodontist | 10 (6.8%) | 94 |
| Coach | 24 (16.3%) | ||
| General dentist | 9 (6.1%) | ||
| Friends | 21 (14.3%) | ||
| Internet and social media | 30 (20.4%) | ||
|
Yes | 57 (38.8%) | 147 |
| No | 90 (60.2%) | ||
|
Yes | 120 (81.6%) | 147 |
| No | 27 (18.4%) | ||
|
Yes | 71 (48.3%) | 147 |
| No | 76 (52.7%) | ||
|
Yes | 127 (86.4%) | 147 |
| No | 20 (13.6%) | ||
|
Yes | 112 (89.8%) | 120 |
| No | 15 (10.2%) | ||
|
It is Bulky | 35 (23.8%) | 105 |
| Difficulty in speech | 25 (17%) | ||
| Difficulty in breathing | 8 (5.4%) | ||
| Loose | 25 (17%) | ||
| Causes nausea | 12 (8.2%) |
Figure 5.
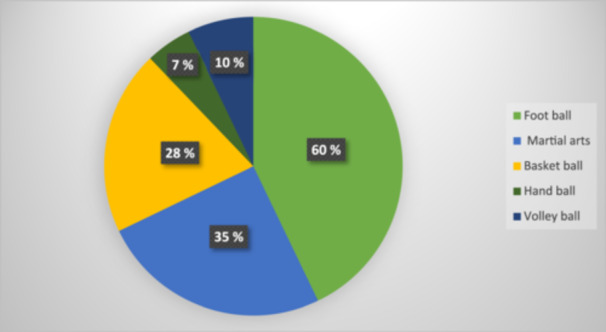
Distribution of orthodontic patients by the type of contact sports involved.
It is worth noting that some of the participants did not respond to some of the items in the questionnaire. Almost one‐half of the patients (44.2%) reported having experienced trauma to teeth/mouth while actively involved in contact sports.
The majority of them were under fixed orthodontic treatment (76.9%) and the rest (23.1%) were under treatment with removable appliances. Of those, 34% had been wearing the appliance for more than 1 year, 42.2% for a time period of about 6 months to 1 year, and 23% had less than 6 months of duration of wear.
3.2.1. Patients' perception and attitude toward MG during orthodontic treatment
More than two‐thirds of the included orthodontic patients (73%) reported that they had heard about MG before, primarily through internet sources as depicted in Figure 6.
Figure 6.
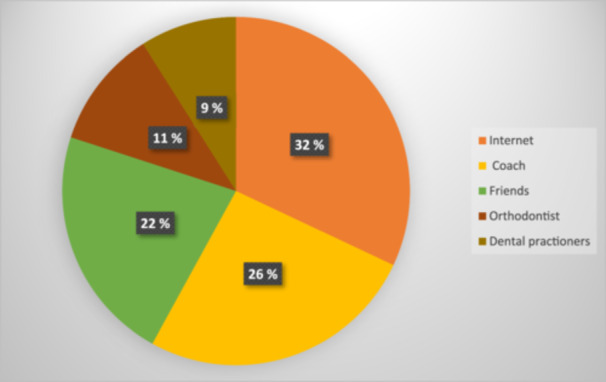
Sources through which orthodontic patients became acquainted with mouthguard.
The majority of orthodontic patients (82%) expressed their readiness to wear the MGs if recommended. However, more than one‐half (53%) showed reluctance to pay additional fees for the MGs.
More than one‐third of participating orthodontic patients (39%) claimed that they routinely use MG while playing contact sports, and the majority of those (86%) believed that MG would offer protection from trauma resulting from contact sports. However, 89% of orthodontic patients perceived wearing MGs while involved in contact sports to be an uncomfortable experience for multiple reasons (Figure 7).
Figure 7.
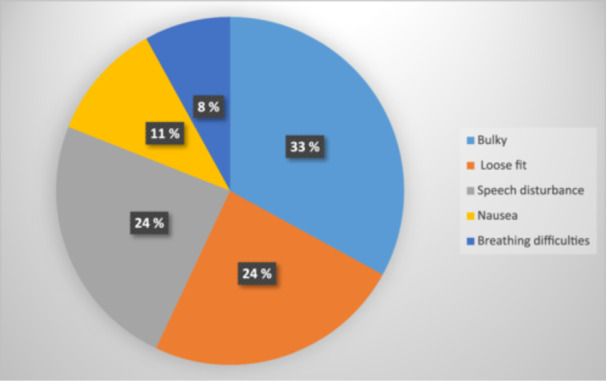
Factors contributing to discomfort due to mouthguard wear as perceived by orthodontic patients.
4. DISCUSSION
The risk of orofacial injuries in athletes involved in sports activities is inevitable. Undoubtedly, mouthguards offer protection to orofacial regions during sports activities. They provide a resilient and protective surface absorbing high‐impact energy from potentially traumatic blows, which otherwise would be transferred directly to the underlying dentition (Ferrari & De Medeiros, 2002). Evidence suggests poor acceptance of MGs among sports players with a lack of awareness regarding the risks of dental injury during sport (O'Malley et al., 2012; Tiryaki et al., 2017). Intriguingly, a recent survey conducted in the Middle East reported that 83% of the participants (parents of athletes) had no knowledge about the preventive aspect of MGs (Almalki et al., 2021).
The available evidence concerning the perception and acceptability of MGs among orthodontists and orthodontic patients is currently limited. Only a few studies have documented the perception of orthodontists in terms of the protective capabilities of MGs during contact sports (Bastian et al., 2020; Bussell & Barreto, 2014). To our knowledge, there is no quantitative study that explores and correlates both orthodontists and their own patients' standpoint on the use of MGs. Hence, this cross‐sectional study was conducted to report on the attitude, knowledge, and perception of orthodontists, dental practitioners, and orthodontic patients toward the use of MGs during contact sports activities.
In the present study, it was observed that around half of the orthodontic patients engaged in contact sports had experienced trauma. This appears to be higher than what has been reported for non‐orthodontic patients (less than 20%) (Meyfarth et al., 2023; Park et al., 2021). This discrepancy suggests that orthodontic patients may be more susceptible to traumatic injuries. The heightened risk of such injuries in orthodontic patients could be associated with pre‐existing malocclusions, particularly an increased overjet, or simply the presence of fixed orthodontic appliances, which increases the risk of oral soft‐tissue injuries when exposed to trauma due to sports due to the design of the appliance per se (Maeda et al., 2008).
In the current study, only 29% of dental clinicians enquired about their patients' involvement in contact sports as a part of history taking during their initial visit. This is in contrast to a recently conducted qualitative study, which reported that over half of the orthodontists or their staff intended to initiate discussion about contact sports involvement and mouthguards with patients, during the initial visits (Bastian et al., 2020; Bussell & Barreto, 2014).
In this investigation, it was noted that 46% of dental clinicians (45% orthodontists and 55% general dentists) recommended the use of MGs to their patients engaged in contact sports. Interestingly, fewer orthodontists recommended MGs to their patients compared to DP, which was in contrast with the findings of other surveys (Bastian et al., 2020; Bussell & Barreto, 2014) that reported more than 50% of orthodontists recommended MGs for their patients involved in contact sports. This difference in findings could potentially be explained by the relatively low number of dental clinicians who enquire about their patient's involvement in contact sports as part of their medical history during the initial visit. It is worth noting that patients are more likely to use MGs if their dental clinician educates them about the importance of mouthguard wear during contact sports activities (Bastian et al., 2020; Bussell & Barreto, 2014). Without asking about contact sports involvement, dental clinicians may overlook an important opportunity to educate patients on the importance of mouthguards.
The majority of dental clinicians displayed a positive attitude toward the use of MGs if their patients informed them about their involvement in contact sports during the course of treatment. However, it is worth noting that 64% of these clinicians would consider obtaining consent from patients or parents of the patients who are under‐aged before recommending MGs, primarily due to concerns about potential liabilities. This finding aligns with a previous study (Bastian et al., 2020) where some orthodontists believed it was necessary to inform their patients about the limitations of MGs in providing complete protection against traumatic injuries. According to dental clinicians, this approach is likely to ensure that patients have realistic expectations regarding the protective benefits of MGs and are well‐informed when making decisions about their use.
The majority of dental clinicians (79%) felt that the onus of recommending MGs to orthodontic patients is upon the orthodontists, among which less than half (45%) of orthodontists felt that it was their sole responsibility. This is consistent with a previous study, (Bastian et al., 2020) which found that most orthodontists believed that recommending MGs should be a shared responsibility of orthodontists, dentists, coaches, and parents rather than their sole responsibility. However, this standpoint among the participating dental clinicians did not align with that reported by the orthodontic patients. In the current investigation, patients reported that they were least likely to receive information about MGs from their dental clinicians. The fact that patients did not typically learn about MGs from their treating dental clinicians aligns with other studies (Bastian et al., 2020; Meyfarth et al., 2023), which found that coaches and clubs are the first to inform players under orthodontic treatment about MGs, rather than dental clinicians.
In contrast to other studies (Bastian et al., 2020; Bussell & Barreto, 2014), the current study found that stock MGs were the most preferred type of MG among dental clinicians. One plausible explanation for dental clinicians favoring stock‐type MGs could be their affordability, time factor, and widespread availability. However, it is important to note that stock‐type MGs lack retention features, relying on the athlete to maintain them in the mouth through biting, which does not guarantee an optimal fit, which in turn may explain the significant proportion of complaints about the utility of MGs reported by the patients. The majority of the orthodontic patients cited discomfort with the use of MGs owing primarily to its bulkiness followed by difficulty in articulation and fit.
Interestingly, few participating dental clinicians reported having an in‐office facility to fabricate custom‐made MGs. Their preference might be linked to the fact that custom‐made MGs offer better stability, retention, and user‐perceived comfort, which is a pivotal factor affecting compliance (Kalra et al., 2022). The potential financial advantages for clinicians could also play a role in their recommendation of custom‐made MGs. This is evident from a finding from the study, indicating that among the participating dental clinicians with an in‐house MG fabrication facility, the majority expressed an intention to charge their patients for custom‐made MGs. However, over half of the participating orthodontic patients were unwilling to bear additional expenses. This highlights that financial considerations may play a significant role in patients' preferences and adherence to using MGs. The potential cost associated with custom‐made MGs can be a barrier for some patients, which underscores the importance of considering affordability when discussing and recommending MGs to patients.
It is worth noting that a recent study involving orthodontic patients with fixed appliances participating in contact sports has found that custom‐made and mouth‐formed MGs offered a higher level of wearability in terms of patient preference compared to pre‐fabricated types (Kalra et al., 2022). Furthermore, custom‐made MGs have been proven better in absorbing impact and retaining their shape during laboratory impact testing when compared to pre‐fabricated or mouth‐formed types (Harrington et al., 2022). These findings suggest that there is a shifting paradigm concerning MG selection and that custom‐made MGs may offer superior performance and comfort.
The majority of the dental clinicians preferred their removable appliance patients to swap their appliances with MGs and fixed appliance patients to wear MGs while participating in contact sports during sports activities. This shows that dental clinicians believe in the protective ability of MGs regardless of the type of appliance, which was considered a barrier to recommendations by orthodontists in a previous study (Bussell & Barreto, 2014).
In the current study, some patients reported experiencing trauma even though they were wearing mouthguards. This could be attributed to several possible reasons such as inadequate fit and patient discomfort (as reported by some of the participating orthodontic patients), quality of MGs, improper use, impact severity, and wear and tear.
One strength of the current study is the inclusion of both clinicians (caregivers) and their patients (recipients of care) allowing the exploration of both clinicians' attitudes and patients' perceptions to provide a more holistic view of the situation. Furthermore, this study did not restrict patients' participation in a specific sport type.
Limitations of this study include utilizing a convenience sampling approach to select the participants, which may affect the generalizability of the study results. Also, the survey did not consider the potential impact of socioeconomic status on the affordability of MGs. Additionally, included patients were treated with different appliance types with variable severity of malocclusion, which may influence patients' experiences and outcomes.
5. CONCLUSION
Most of the dental clinicians expressed a positive attitude and belief toward the protective ability of MGs.
The majority of dental clinicians did not enquire but relied on patients to proactively disclose their sports activities before recommending mouthguards.
Patients primarily acquired knowledge about mouthguards from internet sources, rather than from their dental clinicians.
Patients expressed a willingness to wear mouthguards if they were recommended by dental clinicians, whom they regarded as trusted professionals.
Stock‐type MGs were the most preferred among the participating clinicians, reflected by the perceived discomfort of the orthodontic patients.
Patients expressed their reluctance to incur additional costs for MGs.
6. CLINICAL IMPLICATION
Given the increasing incidence of traumatic injuries, it has become imperative to implement regulations and strategies to make the use of MGs mandatory, especially in contact sports. Dental clinicians, particularly orthodontists, play a significant role in developing strategies to promote the adoption of MGs among athletes undergoing orthodontic treatment. Consideration of the financial status of the patients is essential to enhance adherence to MGs.
AUTHOR CONTRIBUTIONS
Shailaja Raghavan: Methodology; data analysis; writing—original draft. Elham S. Abu Alhaija: Conceptualization; methodology; data analysis; writing—original draft. Yousef Nasrawi: Methodology; data collection. Susan Al‐ Khateeb: Methodology; data collection. Samer Sunna: Methodology; data collection. All the authors contributed to revision and approval of the final manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The protocol was approved by the Deanship of research/Jordan University of Science and Technology (Research ID20070048).
ACKNOWLEDGMENTS
This project did not receive any support from funding organizations.
Raghavan, S. , Abu Alhaija, E. S. , Nasrawi, Y. , Al‐ Khateeb, S. , & Sunna, S. (2024). Un “boxing” the reality: Knowledge, attitude, and perception of orthodontists, dental practitioners, and orthodontic patients toward mouthguards' wear during contact sports—A cross‐sectional study. Clinical and Experimental Dental Research, 10, e904. 10.1002/cre2.904
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Almalki, S. A. , Almutairi, M. S. , Alotaibi, A. M. , Almutairi, A. S. , Albudayri, L. M. , & Almutairi, R. Z. (2021). Parental attitude and awareness toward preventive dentistry in Riyadh, Saudi Arabia: A cross‐sectional study. Journal of Pharmacy and Bioallied Sciences, 13(1), S257–S262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alves, J. C. C. , Borges, G. A. , Versluis, A. , Soares, C. J. , & Veríssimo, C. (2020). Effect of orthodontic bracket type and mouthguard presence on the stress and strain during a frontal impact. Brazilian Dental Journal, 31(5), 540–547. [DOI] [PubMed] [Google Scholar]
- Bastian, N. E. , Heaton, L. J. , Capote, R. T. , Wan, Q. , Riedy, C. A. , & Ramsay, D. S. (2020). Mouthguards during orthodontic treatment: Perspectives of orthodontists and a survey of orthodontic patients playing school‐sponsored basketball and football. American Journal of Orthodontics and Dentofacial Orthopedics, 157(4), 516–525.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman, L. , Milardović Ortolan, S. , Žarković, D. , Viskić, J. , Jokić, D. , & Mehulić, K. (2017). Prevalence of dental trauma and use of mouthguards in professional handball players. Dental Traumatology, 33(3), 199–204. [DOI] [PubMed] [Google Scholar]
- Bruggesser, S. , Kühl, S. , Solakoglu, Ö. , & Filippi, A. (2020). The prevalence of orofacial injuries in judo: A cross‐sectional study. Dental Traumatology, 36(4), 411–416. [DOI] [PubMed] [Google Scholar]
- Bussell, M. A. , & Barreto, L. S. (2014). The recommendation and provision of mouthguards: A survey of consultant orthodontists in the UK. Journal of Orthodontics, 41(2), 141–146. [DOI] [PubMed] [Google Scholar]
- Chapman, P. J. (1990). Orofacial injuries and international rugby players' attitudes to mouthguards. British Journal of Sports Medicine, 24(3), 156–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari, C. H. , & De Medeiros, J. M. F. (2002). Dental trauma and level of information: Mouthguard use in different contact sports. Dental Traumatology, 18(3), 144–147. [DOI] [PubMed] [Google Scholar]
- Filippi, A. , Petrovic, M. , Kühl, S. , Šlaj, M. , & Connert, T. (2016). Dental and general trauma in team handball. Swiss Dental Journal SSO—Science and Clinical Topics, 126(7–8), 682–686. [DOI] [PubMed] [Google Scholar]
- Galic, T. , Kuncic, D. , Poklepovic Pericic, T. , Galic, I. , Mihanovic, F. , Bozic, J. , & Herceg, M. (2018). Knowledge and attitudes about sports‐related dental injuries and mouthguard use in young athletes in four different contact sports‐water polo, karate, taekwondo and handball. Dental Traumatology, 34(3), 175–181. [DOI] [PubMed] [Google Scholar]
- Harrington, C. , Minhas, G. , Papageorgiou, S. N. , & Cobourne, M. T. (2022). What are the differences in protective characteristics of orthodontic mouthguards? An in vitro study. European Journal of Orthodontics, 44(1), 95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi, K. , Churei, H. , Tanabe, G. , Togawa, K. , Chowdhury, R. U. , & Ueno, T. (2020). Improving the wearing rate of mouthguards in the youth rugby category affects the total future mouthguard wearing rate. Dentistry Journal, 8(3), 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalra, A. , Harrington, C. , Minhas, G. , Papageorgiou, S. N. , & Cobourne, M. T. (2022). Wearability and preference of mouthguard during sport in patients undergoing orthodontic treatment with fixed appliances: A randomized clinical trial. European Journal of Orthodontics, 44(1), 101–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knapik, J. J. , Marshall, S. W. , Lee, R. B. , Darakjy, S. S. , Jones, S. B. , Mitchener, T. A. , delaCruz, G. G. , & Jones, B. H. (2007). Mouthguards in sport activities: History, physical properties and injury prevention effectiveness. Sports Medicine, 37(2), 117–144. [DOI] [PubMed] [Google Scholar]
- Lieger, O. , & von Arx, T. (2006). Orofacial/cerebral injuries and the use of mouthguards by professional athletes in Switzerland. Dental Traumatology, 22(1), 1–6. [DOI] [PubMed] [Google Scholar]
- Love, R. M. , Carman, N. , Carmichael, S. , & MacFadyen, E. (1998). Sport‐related dental injury claims to the New Zealand accident rehabilitation & compensation insurance corporation, 1993‐1996: analysis of the 10 most common sports, excluding rugby union. The New Zealand Dental Journal, 94(418), 146–149. [PubMed] [Google Scholar]
- Maeda, Y. , Matsuda, S. , Tsugawa, T. , & Maeda, S. (2008). A modified method of mouthguard fabrication for orthodontic patients. Dental Traumatology, 24(4), 475–478. [DOI] [PubMed] [Google Scholar]
- Meyfarth, S. R. S. , Rodrigues, K. A. B. , Von Held, R. , Sarkis, P. , Gouvea Junior, L. E. C. , Antunes, L. A. A. , & Antunes, L. S. (2023). An analysis of athletes' knowledge, acceptance and usability toward custom‐made mouthguards: Uncontrolled before–after study. Sport Sciences for Health, 19(1), 267–275. [Google Scholar]
- Newsome, P. R. H. , Tran, D. C. , & Cooke, M. S. (2001). The role of the mouthguard in the prevention of sports‐related dental injuries: A review. International Journal of Paediatric Dentistry, 11(6), 396–404. [DOI] [PubMed] [Google Scholar]
- O'Malley, M. , Evans, D. S. , Hewson, A. , & Owens, J. (2012). Mouthguard use and dental injury in sport: A questionnaire study of national school children in the west of Ireland. Journal of the Irish Dental Association, 58(4), 205–211. [PubMed] [Google Scholar]
- Owtad, P. , Shastry, S. , Papademetriou, M. , & Park, J. (2015). Management guidelines for traumatically injured teeth during orthodontic treatment. Journal of Clinical Pediatric Dentistry, 39(3), 292–296. [DOI] [PubMed] [Google Scholar]
- Park, H. K. , Park, J. Y. , Choi, N. R. , Kim, U. K. , & Hwang, D. S. (2021). Sports‐Related oral and maxillofacial injuries: A 5‐Year retrospective study, pusan national university dental hospital. Journal of Oral and Maxillofacial Surgery, 79(1), 203.e1–203.e8. [DOI] [PubMed] [Google Scholar]
- Sarao, S. K. , Rattai, J. , & Levin, L. (2021). Dental trauma among hockey players: preventive measures, compliance and injury types. Journal (Canadian Dental Association), 87, 8. [PubMed] [Google Scholar]
- Tewari, N. , Saji, S. , Goel, S. , Srivastav, S. , Alani, A. , Mathur, V. P. , Rahul, M. , & Bansal, K. (2023). Prevalence of sports‐related traumatic orofacial and dental injuries in Asian countries: A systematic review and meta‐analysis. The Journal of Sports Medicine and Physical Fitness, 63(9), 982–994. [DOI] [PubMed] [Google Scholar]
- Tiryaki, M. , Saygi, G. , Yildiz, S. O. , Yildirim, Z. , Erdemir, U. , & Yucel, T. (2017). Prevalence of dental injuries and awareness regarding mouthguards among basketball players and coaches. The Journal of Sports Medicine and Physical Fitness, 57(11), 1541–1547. [DOI] [PubMed] [Google Scholar]
- Using . (2006). Mouthguards to reduce the incidence and severity of sports‐related oral injuries. The Journal of the American Dental Association, 137(12), 1712–1720. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


