Introduction
When pondering recent advances in any clinical discipline there is a tendency to focus on new techniques, drugs, surgical instruments, and at the most fundamental level, on molecular biology. This article is no exception, as progress in all these spheres is essential if headway is to be made. But we are all also aware that new surgical tools quite soon become tarnished, replaced, and even forgotten. We have therefore included topics where the “advance” has served to highlight how little we know rather than how much progress has been made. We hope these finding will soon affect clinical practice.
Summary points
Several new topical drugs have been developed for open angle glaucoma which can be used alone or in combination
Outcome of glaucoma surgery can be improved in high risk patients by topically applied antimetabolites
Endoscopic devices permit direct visualisation for many intraocular and extraocular surgical procedures
Early exposure to light is not a factor in the development of retinopathy of prematurity
Effectiveness of the standard treatment of amblyopia has been called into question
Many visually impaired elderly people in the community are unidentified and do not get treatment or support
Guidelines are available on breaking the news of a child’s visual impairment to parents
Methods
This review is not systematic but a pot pourri of topics identified with the rationale stated in the introduction in mind. Although we did not do a detailed critical appraisal of all cited publications, most of the reported findings remain uncontroversial. Where this is not so, we refer to any ongoing debate.
Primary open angle glaucoma
Primary open angle glaucoma is one of the biggest causes of vision impairment worldwide and affects over five million people. Although its genetic basis is slowly unfurling,1 these findings have yet to affect management. Glaucoma has traditionally been perceived as having a “correct order of treatment,” with medical management followed by microsurgical filtration surgery, sometimes with laser surgery in between.
Topical β blockers form the mainstay of medical management but their side effects restrict their usefulness in chronic obstructive pulmonary disease, particularly asthma and heart conduction defects. Three new drugs have arrived which are useful when β blockers are contraindicated or fail to control intraocular pressure. The topical carbonic anhydrase inhibitor dorzolamide reduces intraocular pressure by reducing production of aqueous humour. It is as effective as β blockers at reducing intraocular pressure and avoids the systemic side effects of existing oral carbonic anhydrase inhibitors—electrolyte imbalance, paraesthesiae of extremities, fatigue, and indigestion.2 The second new drug is brimonidine tartrate, which is used as a 0.2% solution. It is a highly selective α2 agonist and lowers intraocular pressure mainly by reducing production of aqueous humour.3 Care is needed, as with other α agonists, in patients with cardiovascular disease. The most common side effects are a burning and stinging sensation of the eyes, conjunctival hyperaemia, blurred vision, dry mouth, drowsiness, fatigue, and headache. The third drug, latanoprost, is a selective prostaglandin F2α agonist.4 It increases the outflow of aqueous humour through the uveal and scleral tissues. The flow rate is high and it bypasses the obstructed site of normal drainage—the trabecular meshwork. Complications include pigmentation of the iris, conjunctival hyperaemia, and corneal deposits. Treatment for glaucoma has four main drug classes all acting by different mechanisms: β adrenergic antagonists (timolol), cholinergic agonists (pilocarpine), carbonic anhydrase inhibitors (acetazolamide), and adrenergic agonists (brimonidine). Latanoprost is useful because it produces additional reduction of intraocular pressure in combination with any of the above drugs.4
In the past, maximum medical treatment for glaucoma included a combination of up to four drugs. Nowadays, filtration surgery (trabeculectomy) is usually considered when a combination of two preparations fails to control the glaucomatous process. The healing response after trabeculectomy is probably the most important determinant of success—that is, reduced intraocular pressure. The intraocular pressure of certain glaucomatous eyes is notoriously difficult to control especially in Afro-Caribbeans, young patients, and those who have had previous conjunctival surgery or prolonged topical treatment. Recently, antimetabolites have been used to improve postoperative wound healing. Two drugs predominate, 5-fluorouracil and mitomycin C,5 and their effectiveness may be augmented by intensive use of topical steroids and wound suture lysis.5,6
Endolaser surgery
Ophthalmologists have long championed minimally invasive surgery, and advances in laser and endoscopic techniques have facilitated several important innovations in oculoplastic, glaucoma, and vitreoretinal surgery.
Carbon dioxide lasers are effective at sealing small blood and lymphatic vessels, but in the past they generated unacceptable surrounding heat damage. This has now been minimised with short energy delivery time in the new lasers which are used for cosmetic surgery.7
Modern endoscopes greatly improve intranasal visibility and have enabled surgeons to use lasers to create a passage between the lacrimal sac and nasal cavity during endonasal dacryocystorhinostomy.8 Endonasal laser dacryocystorhinostomy, which can be performed as outpatient surgery, has several advantages including eliminating a cutaneous scar, good haemostasis, better visualisation, and preservation of lacrimal anatomy. Success rates of endonasal laser dacryocystorhinostomy at 66% to 82% are lower than the 90% reported for traditional transcutaneous methods,8,9 so it remains to be seen if it represents a lasting advance in lacrimal drainage surgery.
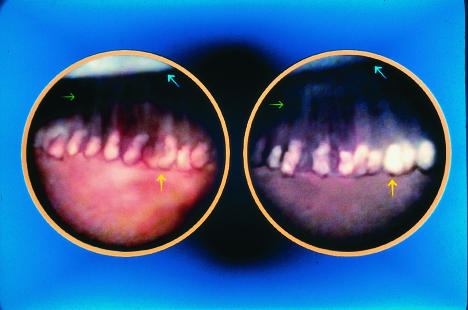
Endoscopes are also currently being evaluated to deliver laser energy under direct observation within the eye for treating glaucoma and vitreoretinal disorders. In glaucoma, ablation of the ciliary processes is used to control the intraocular pressure with minimal inflammation of the surrounding tissues (fig 1).10
Figure 1.
Internal view of ciliary processes before (left) and after (right) diode laser endoscopic cyclophotocoagulation. Ciliary process (yellow arrow) whitens after treatment. Green arrow indicates zonular fibres. Blue arrow indicates lens
Paediatric ophthalmology
Preterm birth
The increased survival of preterm babies carries several short and long term implications for the visual system. Retinopathy of prematurity was initially thought to be due solely to high levels of oxygen administration. However, its persistence despite meticulous oxygen control led to a feeling of resignation that severe retinopathy is an almost unavoidable and unpredictable consequence of extreme prematurity. Intriguingly, this unpredictability may, in some instances, have a molecular basis, as advanced retinopathy of prematurity has been reported in association with missense mutation of the Norrie gene.11 This aside, extreme prematurity remains the greatest risk factor for sight threatening disease together with high levels of oxygen and fluctuations in oxygen during the first few weeks after birth.12
Standard of care remains a critical issue in avoiding retinopathy of prematurity. Middle income countries where neonatal care is less than ideal, such as those in Latin America13 and eastern Europe,14 have a higher incidence of severe disease and blindness than Britain or the United States. Furthermore, the condition affects larger babies in middle income countries than it does in Britain and the United States, where severe disease is virtually confined to babies under 1500 g birth weight and gestational age less than 32 weeks. These two factors are the inclusion criteria for screening in Britain,15 illustrating how guidelines developed in one country may not be universally applicable.
Early exposure to light was thought to be a possible factor in retinopathy of prematurity. Premature babies are reared in a bright and generally continuously lit environment16 whereas the fetal period is spent in almost complete darkness in a term pregnancy. A recent randomised controlled trial showed no difference in retinopathy of prematurity between babies who had goggles applied within 24 hours of birth to reduce light exposure and those exposed to routine ambient nursery light (fig 2).17
Figure 2.
Preterm infant with eyes shielded by light reducing goggles
Amblyopia
Most British children are screened at around 3-4 years of age for amblyopia and strabismus. The value of this has been questioned by a recent systematic review,18 which concluded that there is insufficient evidence to screen for amblyopia, cosmetically non-obvious squint, and refractive error as there is little evidence that these conditions are disabling and the interventions to correct them do more good than harm. The conclusions were controversial,19 but the case against screening arises partly from the lack of evidence that occlusion therapy is effective—the main treatment for the past 250 years. This is mainly because of the difficulties of measuring vision in early childhood and monitoring compliance with treatment. A solution may be at hand as objective monitoring of treatment is now available.20 Drug treatments of amblyopia have not entered routine clinical practice, though improvements in visual acuity have been reported with neurotransmitter precursors (levodopa) and neuromodulators (citicoline).21
Vision related quality of life
Although visual acuity remains the measure of vision that ophthalmologists consider most important, it does not correlate with patients’ perception of their visual handicap22 and is non-informative about many of life’s activities, such as education and independent living. To determine patients’ perceptions of the outcome of an intervention a range of quality of life questionnaires have been developed. Some evaluate general health (for example, SF-36, EuroQol, sickness impact profile), while others are vision focused (VF-14 (14 item measure of visual function in cataract), visual quality of life, activities of daily vision scale).23 The relation between vision and general health is complex, and the tools need to contain both general and specific questions so that the effect of visual deficits on general health can be sensitively evaluated. “Trouble with seeing” has been reported to have greater impact on general functional status and wellbeing than other health problems, including hypertension, history of myocardial infarction, type II diabetes, and headache.24 Worryingly, reduced visual acuity is associated with a greater risk of subsequent physical disability among older able bodied people, including hip fractures in women, and a reduced likelihood of improvement for those already disabled.25
Many patients with bilateral cataracts have no measurable vision related health dysfunction, but for those that do surgery improves scores on measures of visual functional quality of life.26 There are also additional gains from removal of the cataract from the second eye.27 This finding is important as about a third of all cataract operations are on second eyes.26 Patients prefer multifocal rather than monofocal intraocular lens implants after cataract removal because they impose fewer restrictions on visual tasks.28 However, vision related quality of life instruments found no significant difference between good and poor outcome after cataract surgery.26 No association has been found between preoperative and postoperative visual acuities and patients’ assessment of visual function.26,29
The sensitivity of vision related quality of life tools needs to be improved to take account of the fact that treatment is now usually undertaken at an early stage when functional limitations are few. This is an exciting field, not least because it shifts attention to patient centred issues. Perhaps in future, quality of life questions might be incorporated into routine preoperative assessment and help reduce the wide variation in thresholds for ophthalmic surgery.30
Visual impairment
Recent research emphasises the inadequacies of current management. Losing sight over a short period generates several reactive phases including shock, pining, depression, and resolution.31 But this is only a small part of the story. Most elderly people lose their sight slowly through uncorrected refractive error, cataract, age related macular degeneration, glaucoma, etc. There is a massive non-recognition of these visual problems in the community.32,33 The adult visually impaired population has a high prevalence of additional disability (35%), particularly of hearing, and women over 60 years are more likely to be widowed than their sighted counterparts (55% v 30%). Visually impaired people are also more likely to be closer to the poverty line and to live on their own and are less likely to own their home.32 Those of working age are less likely to find employment, and retaining jobs is particularly difficult.
Although most visually impaired people have useful sight, there is underprovision of visual aids, inadequate training in their use (only 13% use their aids), and poor understanding of simple methods of improving visual function for daily living (for example, by lighting).34 Registration as being partially sighted or blind should be a trigger for support, but this is not always so. In a recent survey of 500 blind or partially sighted elderly people (93% of whom were registered), 21% had never received a visit from a social worker, and for most (72%) support and information came from friends and relatives.35 Those surveyed also reported loneliness as a special problem, and most had difficulties with daily tasks such as shopping, cooking, and reading their post.
A recent systematic review concluded that screening asymptomatic older people in the community for vision impairment is not justified as no trials have reported improvement of vision.35 We question the review’s premise that vision impairment in this age group can usually be reduced by treatment. Non-recognition of vision impairment is associated with lack of treatment and support. Furthermore, medical care should not be confined to treatable conditions. Recognition is the conduit to specialist medical, social, and other services, all of which can help minimise the handicapping effect of the impairment. Every person with vision impairment needs an eye examination. Registration as blind or partially sighted, for all its defects does trigger some support. Local and national organisations for visually impaired people have an important role and have initiated the development of multiprofessional integrated services.36 These organisation often provide low vision aids to help with many daily tasks, including reading. Finally, clinicians should be sensitive to the medical needs of the blind. For example, many blind people are afraid that they may develop a serious or life threatening medical condition for which the earliest sign is visual (for example, a rash or melaena) and that these signs will be unnoticed.
A particular challenge, especially for childhood vision impairment, is breaking the news to the family. According to a recent study, it is not a task that clinicians do well.37 As most childhood vision impairment has its origins at birth or before, this issue usually arises early in infancy. For many parents the way the news is broken is unsatisfactory—they report delays, insensitive handling, seeming lack of interest, lack of privacy, insufficient information, infrequent review, etc.
The way parents learn that their child has a disability can have lasting effects on the child and family. In addition, even if medical treatment is not possible clinicians and others can offer considerable support and information. Taking the Time makes several important and positive recommendations to help clinicians.36 Speedy referral to specialist services is required when a severe vision deficit is suspected. The diagnosis should be given in private, and a review appointment should be offered within a couple of weeks to give the parents a chance to discuss their child’s condition. Try to give parents written information which can be updated according to subsequent progress; this can be in the form of a personal letter. The care of visually disabled children requires multiprofessional input, and links with the community support services, such as the peripatetic teaching service, should be established as soon as possible. Do not forget the value of parents’ support organisations. Finally, the person who is bearer of bad news also has the first opportunity to take positive supportive steps for the family. If doctors are open with the family and other professionals the parents will come to regard them as an advocate and ally to work with.
Conclusion
We have touched on selected important ophthalmic advances in the treatment of glaucoma, endoscopic surgery, retinopathy of prematurity, and other paediatric disorders. However, recent surveys and research have shown how little we know about vision as it relates to life and how limited is our care of visually impaired children and adults. These results are critical evidence which we hope will act as the springboard for improving clinical care; indeed the development of patient centred quality of life tools is confirmation that real progress is already being made.
References
- 1.Booth A, Churchill A, Anwar R, Menage M, Markham A. The genetics of primary open angle glaucoma. Br J Ophthalmol. 1997;81:409–414. doi: 10.1136/bjo.81.5.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strahlman E, Tipping R, Vogel R International Dorzolamide Study Group. A double masked, randomised 1 year study comparing dorzolamide (Trusopt), timolol, and betaxolol. Arch Ophthalmol. 1995;113:985–986. doi: 10.1001/archopht.1995.01100080061030. [DOI] [PubMed] [Google Scholar]
- 3.Walters TR. Development and use of brimonidine in treating acute and chronic: a review of safety, efficacy, dose response, and dosing studies. Surv Ophthalmol. 1996;41(suppl 1):S19–S26. doi: 10.1016/s0039-6257(96)82028-5. [DOI] [PubMed] [Google Scholar]
- 4.Hoyng PFJ, Rulo A, Greve E, Watson P, Alm A. The additive intraocular pressure lowering effect of latanoprost in combined therapy with other ocular hypotensive agents. Surv Ophthalmol. 1997;41 (suppl 2):S93–S98. doi: 10.1016/s0039-6257(97)80014-8. [DOI] [PubMed] [Google Scholar]
- 5.Katz GJ, Higgingbotham EJ, Lichter PR, Skuta GL, Musch DC, Bergstrom TJ, et al. Mitomycin C versus 5-fluorouracil in high risk glaucoma filtering surgery. Ophthalmology. 1995;102:1263–1269. doi: 10.1016/s0161-6420(95)30875-5. [DOI] [PubMed] [Google Scholar]
- 6.Khaw PT, Occleston NL, Schultz G, Grierson I, Sherwood MB, Larkin G. Activation and suppression of fibroblast function. Eye. 1994;8:188–195. doi: 10.1038/eye.1994.44. [DOI] [PubMed] [Google Scholar]
- 7.Fitzpatrick RE, Goldman MP. Advances in carbon dioxide laser surgery. Clin Dermatol. 1995;13:35–47. doi: 10.1016/0738-081x(94)00025-w. [DOI] [PubMed] [Google Scholar]
- 8.Shun-Shin GA, Thurairajan G. External dacryocystorhinostomy—an end of an era? Eye. 1997;81:716–717. doi: 10.1136/bjo.81.9.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lim JI, Lynn M, Capone A, Jr, Aaberg TM, Sr, Martin DF, Drews-Botsch C. Ciliary body endophotocoagulation during pars plana vitrectomy in eyes with vitreoretinal disorders and concomitant uncontrolled glaucoma. Ophthalmology. 1996;103:1041–1046. doi: 10.1016/s0161-6420(96)30569-1. [DOI] [PubMed] [Google Scholar]
- 10.Tarbet KJ, Custer PL. External dacryocystorhinostomy. Surgical success, patient satisfaction, and economic cost. Ophthalmology. 1995;102:1065–1070. doi: 10.1016/s0161-6420(95)30910-4. [DOI] [PubMed] [Google Scholar]
- 11.Shastry BS, Pendergrast SD, Hatzer MK, Liu X, Trese MT. Identification of missense mutations in the Norrie disease gene associated with advanced retinopathy of prematurity. Arch Ophthalmol. 1997;115:651–655. doi: 10.1001/archopht.1997.01100150653015. [DOI] [PubMed] [Google Scholar]
- 12.Cunningham S, Fleck BW, Elton RA, McIntosh N. Transcutaneous oxygen levels in retinopathy of prematurity. Lancet. 1995;346:1464–1465. doi: 10.1016/s0140-6736(95)92475-2. [DOI] [PubMed] [Google Scholar]
- 13.Gilbert C, Rahi J, Eckstein M, O’Sullivan J, Foster A. Retinopathy of prematurity in middle-income countries. Lancet. 1997;350:12–14. doi: 10.1016/S0140-6736(97)01107-0. [DOI] [PubMed] [Google Scholar]
- 14.Bagdoniené R, Sirtautiené . Threshold retinopathy of prematurity in Lithuania: tendencies during three years. In: Reibaldi A, Di Pietro M, Scuderi A, Malerbi E, editors. Progress in retinopathy of prematurity. Amsterdam: Kluger; 1997. pp. 31–36. [Google Scholar]
- 15.Report of a Joint Working Party of the Royal College of Ophthalmologists and the British Association of Perinatal Medicine. Retinopathy of prematurity: guidelines for screening and treatment. Early Hum Dev. 1996;46:239–258. [PubMed] [Google Scholar]
- 16.Bullough J, Rea MS. Lighting for neonatal intensive care units: some critical information for design. Light Res Technol. 1996;28:189–198. [Google Scholar]
- 17.Reynolds JD, Hardy RJ, Kennedy KA, Spencer R, van Heuven WAJ, Fielder AR.for the Light Reduction in Retinopathy of Prematurity (LIGHT-ROP) Cooperative Group. Lack of efficacy of light reduction in preventing retinopathy of prematurity N Engl J Med 19983381572–1576. [DOI] [PubMed] [Google Scholar]
- 18.Snowdon SK, Stewart-Brown SL. Preschool vision screening: results of a systematic review. York: NHS Centre for Reviews and Dissemination; 1997. (Report 9.) [Google Scholar]
- 19.Moseley MJ. Preschool vision screening: a recent report calls for a halt. Br J Ophthalmol. 1998;82:722–723. doi: 10.1136/bjo.82.7.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fielder AR, Irwin M, Auld R, Cocker KD, Jones HS. Compliance in amblyopia therapy: objective monitoring of occlusion. Br J Ophthalmol. 1995;79:585–589. doi: 10.1136/bjo.79.6.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Campos E. Amblyopia. Surv Ophthalmol. 1995;40:23–39. doi: 10.1016/s0039-6257(95)80044-1. [DOI] [PubMed] [Google Scholar]
- 22.Hart PM, Chakravarthy U, Stevenson MR. Questionnaire-based survey on the importance of quality of life measures in ophthalmic practice. Eye. 1998;12:124–126. doi: 10.1038/eye.1998.20. [DOI] [PubMed] [Google Scholar]
- 23.Frost NA, Sparrow JM, Durant JS, Donovan JL, Peters TJ, Brookes ST. Development of a questionnaire for measurement of vision-related quality of life. Ophthalmic Epidemiol (in press). [DOI] [PubMed]
- 24.Lee PP, Spritzer K, Hays RD. The impact of blurred vision on functioning and well-being. Ophthalmology. 1997;104:390–396. doi: 10.1016/s0161-6420(97)30303-0. [DOI] [PubMed] [Google Scholar]
- 25.Salive ME, Guralnik J, Glynn RJ, Christen W, Wallace RB, Ostfeld AM. Association of visual impairment with mobility and physical function. J Am Geriatr Soc. 1994;42:287–292. doi: 10.1111/j.1532-5415.1994.tb01753.x. [DOI] [PubMed] [Google Scholar]
- 26.Desai P, Reidy A, Minassian DC, Vafidis G, Bolger J. Gains from cataract surgery: visual function and quality of life. Br J Ophthalmol. 1996;80:868–871. doi: 10.1136/bjo.80.10.868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laidlaw DA, Harrad RA, Hopper DC, Whitaker A, Donovan JL, Brookes ST, et al. Randomised trial of effectiveness of second eye cataract surgery. Lancet. 1998;352:925–929. doi: 10.1016/s0140-6736(97)12536-3. [DOI] [PubMed] [Google Scholar]
- 28.Javitt JC, Wang F, Trentacost DJ, Rowe M, Tarantino N. Outcomes of cataract extraction with multifocal intraocular lens implantation. Ophthalmology. 1997;104:589–599. doi: 10.1016/s0161-6420(97)30265-6. [DOI] [PubMed] [Google Scholar]
- 29.Mangione CM, Phillips RS, Lawrence MG, Seddon JM, Orav EJ, Goldman L. Improved visual function and attenuation of declines in health-related quality of life after cataract extraction. Arch Ophthalmol. 1994;112:1419–1425. doi: 10.1001/archopht.1994.01090230033017. [DOI] [PubMed] [Google Scholar]
- 30.Jones HS, Yates JM, Spurgeon P, Fielder AR. Geographical variations in rates of ophthalmic surgery. Br J Ophthalmol. 1996;80:784–788. doi: 10.1136/bjo.80.9.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fitzgerald RG, Parkes CM. Blindness and loss of other sensory and cognitive functions. BMJ. 1998;316:1160–1163. doi: 10.1136/bmj.316.7138.1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bruce IW, McKennell AC, Walker EC. Blind and partially sighted adults in Britain: the RNIB survey. Vol. 1. London: HMSO; 1991. [Google Scholar]
- 33.Reidy A, Minassian DC, Vafidis G, Joseph J, Farrow S, Wu J, et al. Prevalence of serious eye disease and visual impairment in a north London population: population based cross sectional study. BMJ. 1998;316:1643–1646. doi: 10.1136/bmj.316.7145.1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baker M, Winyard S. Lost vision: older visually impaired people in the UK. London: Royal National Institute for the Blind; 1998. [Google Scholar]
- 35.Smeeth L, Iliffe S. Effectiveness of screening older people for impaired vision in community setting: systematic review of evidence from randomised controlled trials. BMJ. 1998;316:660–663. doi: 10.1136/bmj.316.7132.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shuttleworth GN, Dunlop A, Collins JK, James CRH. How effective is an integrated approach to low vision rehabilitation? Two year follow up results from South Devon. Eye. 1995;79:719–723. doi: 10.1136/bjo.79.8.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Taking the time. Telling parents their child is blind or partially sighted. London: Royal National Institute for the Blind; 1996. [Google Scholar]