Abstract
Rhino-sinusal mucormycosis is an acute invasive fungal infection rarely encountered in the clinical setting, occurring in severe immunosuppressed patients. However, in patients suffering from COVID-19 disease a dramatic increase in the incidence of mucormycosis has been recorded. The aim of the study is to discuss the MRI findings of patients with COVID-19 associated mucormycosis. This is a retrospective review of 10 hospitalized and operated patients in three Otolaryngologic Departments between the 1st of February 2021 and the 30th of October 2021. All patients presented nasal mucormycosis, histologically verified along with documented SARS-CoV-2 positive RT-PCR test. The sinus involvement, extra sinus spread and peri-sinus invasion were documented in all patients. The correlation between MRI and intra-operative findings was also assessed. The black turbinate sign and peri-antral soft tissue infiltration are early MRI signs characteristic of mucormycosis. Moreoever, MRI has a significantly high positive predictive value for intra-operative findings in COVID-19 associated mucormycosis
Keywords: Mucormycosis , sinus , MRI , COVID-19
Introduction
Mucormycosis represents an acute invasive fungal sinusitis affecting severe immunosuppressed patients. In COVID-19 positive patients the number of rhino-sinusal mucormycosis cases has been increased dramatically [1, 2]. Risk factors associated with the development of invasive mucormycosis include the massive use of immunosuppressive drugs (high doses of corticosteroids), long broad-spectrum antibiotic therapy, oxygen therapy, prolonged hospitalisation, continuous ventilatory sustenance [3]. Since mucormycosis is ascribed with elevated mortality rates (40-80%), confirmatory early diagnosis is of paramount importance. Diagnosis is based on clinical signs, nasal endoscopy, imaging (Computed Tomography - CT and Magnetic Resonance Imaging-MRI) and biopsy [4]. Imaging is necessary for diagnostic approval, assessment of fungal infection extension and detection of complications. The aim of the present study is to analyse the MRI findings in mucormycosis patients recently infected with SARS-CoV-2.
Materials and Methods
Patients. The study was approved by the Ethic Committee of the “Iuliu Hațieganu” University of Medicine and Pharmacy Cluj-Napoca [No. 96/18.04.2022]. We performed a retrospective review of MRI data of mucormycosis biopsy confirmed cases. These patients were hospitalized between the 1st of February 2021 and the 30th of October 2021in three University Otolaryngologic Departments from Cluj-Napoca, Timisoara and Bucharest. Included were COVID-19 positive patients with preoperative MRI of the brain, orbit and paranasal sinuses. Positive COVID-19 infection was defined as a positive nasopharyngeal PCR reaction and/or classic chest imaging sign of COVID-19 infection.
Imaging Protocol. MRI of the paranasal sinuses, orbit and brain was performed on 3-T scanner (Siemens, Erlangen, Germany) using a 24-channel head-neck coil [5]. In addition to standard MRI scans, various sequences were acquired - short tau inversion recovery (STIR) for orbits and diffusion-weighted imaging (DWI) for optic nerves. T1 contrast enhanced sequences were acquired after intravenous injection of 0.1 mmol/kg body weight of Gadovist (Bayer Schering Pharma AG, Germany). All MRI images were analysed by three experienced radiologists. Signal intensity of the sinus content was recorded in each patient. Hyperintense signal in T2 fat suppression sequence was used to describe extra-sinus extension - in the retro-maxillary space, orbit, pterygopalatine and infratemporal fossa. Black turbinate sign on T1 post contrast sequence was defined as the absence of enhancement of the nasal mucosa of the turbinates [4, 6, 7].
Outcomes. Main outcomes assessed in this study were: involvement of the paranasal sinuses detected on MRI images, the proportion of patients presenting extra-sinus extension of the fungal disease, the correlation between MRI images and intraoperative findings. Thus, the positive predictive value (PPV) of MRI was determined.
Results
A total of 18 patients with post COVID-19 mucormycosis were initially enrolled in the study. However, out of 18 patients only 10 had an initial preoperative MRI scan and were included in the final analysis. The study comprised 6 male and 4 female patients, mean age was 53.5 years (range 35-72 years). A history of prior hospitalization was detected in 4 cases, steroid intake was present in 6 patients, oxygen therapy in 4 cases. Five patients were previously detected with type 2 diabetes, 3 cases were detected with diabetes at current presentation and 2 cases had normal glycaemic control.
Sinus hyperdensity was detected in 9 patients: the maxillary and ethmoid sinuses were the most frequently involved (Figure 1)-9 cases, sphenoid sinus affected in 7 cases (Figure 2) and frontal sinus involved in 6 patients. Black turbinate sign (Figure 3) was detected in 8 cases and peri-maxillary soft tissue infiltration (infratemporal and temporal fossa) in 6 cases (Figure 4). Palate extension of the fungal disease was detected in 3 cases. Orbital extension with proptosis was observed in 6 cases (Figure 5). Involvement of the extraocular muscles was detected in all these cases, most frequent involved was the inferior rectus (3 cases) and medial rectus in 2 cases. Orbital apex involvement was observed in 3 patients (Figure 6). Dural enhancement was noted in 4 cases and cerebritis was detected in 3 cases.
Figure 1.
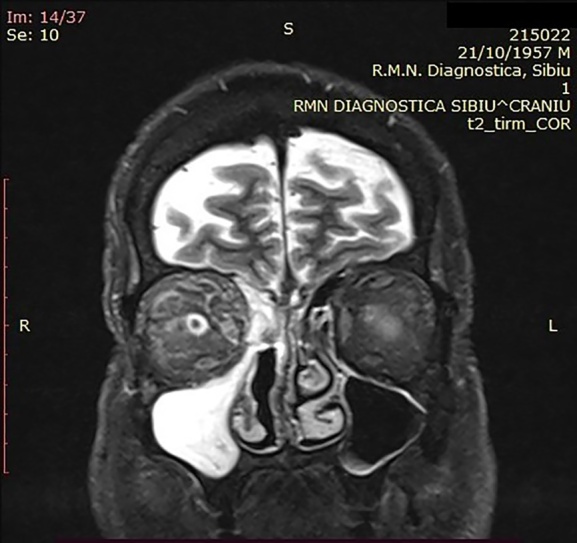
Mucormycosis-maxillary and ethmoid sinusitis with orbital invasion
Figure 2.

Involvement of the sphenoid bone-T2 fat suppression: extrasinus hyperintense signal indicates fungal involvement
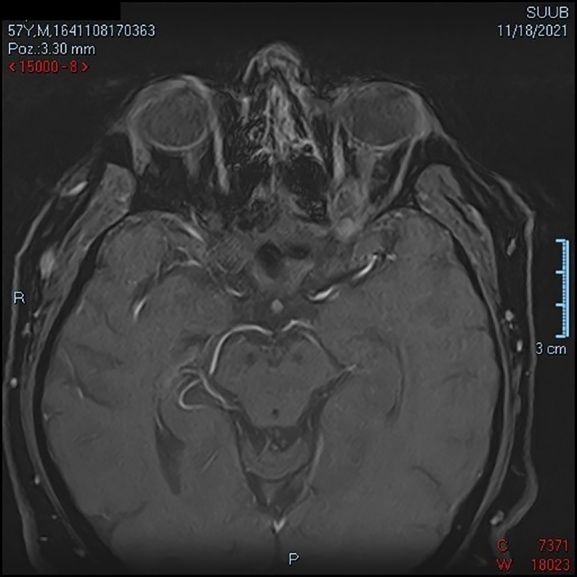
Figure 3.
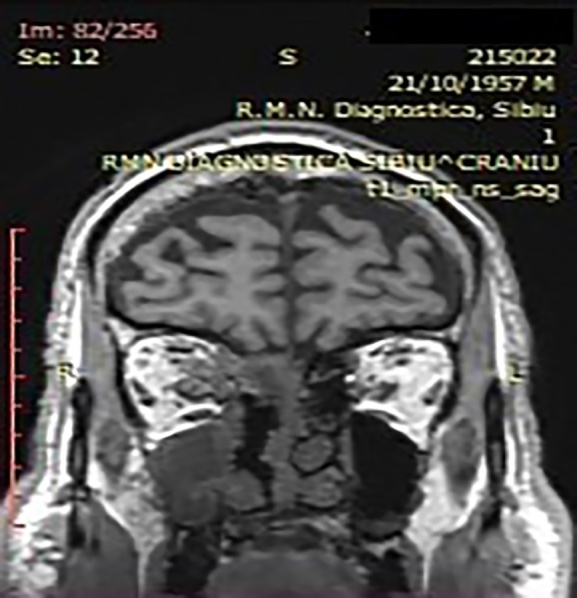
Black turbinate sign-absence of enhancement of nasal mucosa on T1 postcontrast. Invasion of the right orbit
Figure 4.
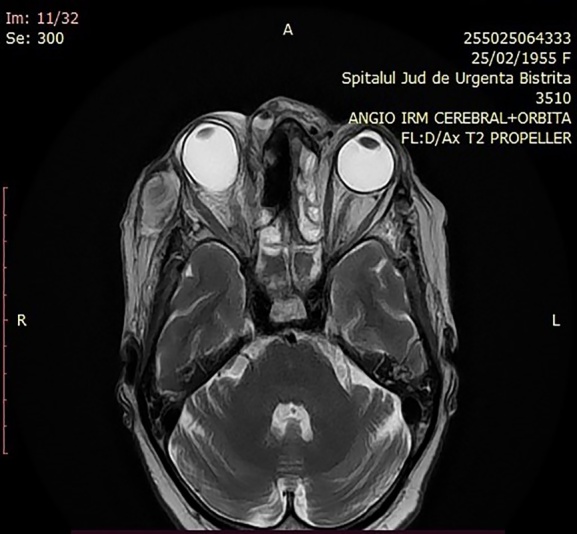
Invasion of the right orbit with proptosis. Abscess of the right temporal fossa
Figure 5.
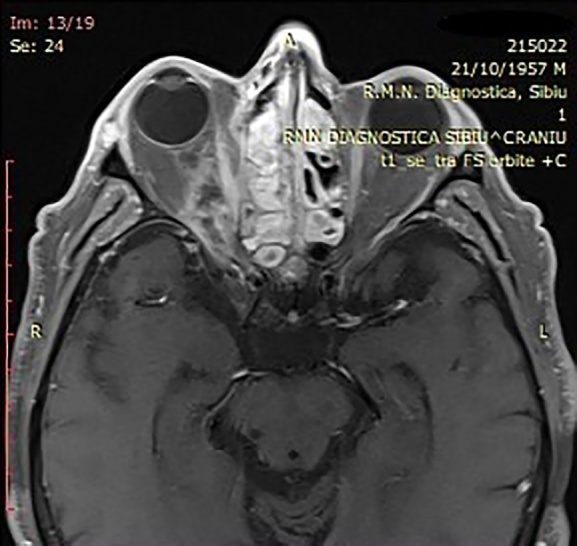
Abscess of the left orbit with enhancement of the medial rectus muscle
Figure 6.
Abscess of the left orbit
The correlation between MRI images and surgical findings is presented in Table 1 along with the calculation of PPV. The PPV value of the T2 fat suppression sequence in predicting ischemic tissues in various areas (infratemporal fossa, orbit, sphenoid bone, palate) was 80%, 80%, 70% and 80%, respectively.
Table 1.
Correlation between MRI and intra-operative findings with assessment of the positive predictive value (PPV).
|
Radiologic findings |
Operative findings Ischemia Healthy |
Statistics PPV |
|
Black turbinate* |
9 1 |
PPV=9/10=90% |
|
Infratemporal fossa involvement** |
8 2 |
PPV=8/10=80% |
|
Orbital involvement** |
8 2 |
PPV=8/10=80% |
|
Sphenoid bone involvement** |
7 3 |
PPV=7/10=70% |
|
Palate involvement** |
8 2 |
PPV=8/10=80% |
*Absence of enhancement of the turbinate mucosa on postcontrast MRI T1 sequence
**Bright signal on MRI T2 fat saturation sequence
Discussions
Mucormycosis represents an invasive fungal sinusitis having an acute or chronic course. COVID-19 associated mucormycosis usually demonstrates an acute fulminant invasive course during the active or recovering SARSC-CoV-2 disease. Immunosuppression represents the main risk factor associated with the development of sinusal mucormycosis, since only 9 to 19% of affected patients are immunocompetent. Other putative risk factors include diabetes, long term corticoid treatment, high ferritin levels associated with SARS-Cov-2, prolonged ventilatory support, high chest CT severity score [2, 3, 8].
Actually, Mucor is a widespread saprophytic fungus existing on dust and plants. Inoculation occurs through inhalation. The airstream lays down the fungus in the nasal cavity and subsequently Mucor colonizes the paranasal sinuses. Extra sinus spread ensues by direct soft tissue and bone invasion, by way of perivascular or perineural pathways toward the orbit and the brain [9]. Several routes of intracranial spread are described: erosion of the ethmoid roof, cribriform plate, along the cranial nerves, along the ethmoidal arteries, ophthalmic, internal carotid and basilar arteries [10].
In accordance with the literature, the maxillary and ethmoid sinuses are more frequently involved, followed by the sphenoid and frontal sinus. On imaging, mucosal thickening is detected while an air-fluid level is always absent [11]. On T2 sequences the maxillary content is constantly hypointense due to the existence of iron and manganese in the fungal content. The black turbinate sign defined as the as the absence of enhancement of the turbinates on T1 sequence is an early distinctive MRI sign of nasal mucormycosis. Nonenhancement of nasal mucosa represents ischemic and necrotic tissues secondary to vascular thrombosis. Periantral fat infiltration is another typical MRI sign suggestive of extension beyond the maxillary sinus either through bone erosion or perivascular invasion [12, 13]. The pre-antral and retro fat, the sphenopalatine foramen, nasopharynx, pterygopalatine and infratemporal fossa, buccal and masticator spaces are carefully examined.
The fungal disease extends into the pterygopalatine fossa either through bone erosion or spread via perivascular or perineural channels. Invasion of the pterygopalatine fossa is a prerequisite for extension in the middle fossa or cavernous sinus [13, 14].
Most of our patients presented with orbital invasion. Proptosis is a common feature in patients with mucormycosis suggestive of orbital extension of the disease and inflammation of the retro orbital fat. Enhancement and thickening of the inferior and medial rectus muscles are noted suggestive of disease extension from the maxillary and ethmoid sinus. Invasion of the ophthalmic artery results in diffusion restriction of the optic nerve and this is a strong prognostic sign of irreversible visual loss. In drastic raised intra-orbital pressure, another typic sign is described-the guitar-pick sign, a conical distortion of the posterior part of the ocular globe [15, 16].
The lack of enhancement on post contrast T1 sequence of the surrounding extra sinus spaces is suggestive of infarction and necrosis of the peri-sinus tissues due to direct fungus extension or perivascular or perineural invasion [17].
Orbital apex infiltration is credited a requirement for intracranial invasion in mucormycosis. Intracranial extension occurs either by direct bone erosion or through perineural spread along the maxillary and ophthalmic nerves. Dural invasion is suggested by thickening or enhancement on MRI. On MRI, early cerebritis looks as a T1 hypointense and T2 hyperintense area with patchy limited diffusion and absence of contrast enhancement. The temporal and frontal lobes are primarily involved in intracranial mucormycosis. Cerebritis is rapidly transformed into a brain abscess. The latter is described as an enhancing peripheric rim surrounding a non-enhancing central core. Cavernous sinus thrombosis is frequently encountered in mucormycosis. MRI signs include increase in the size of the sinus, abnormal signal intensity on T1 and T2 sequences, filling defect on post contrast [5, 18]. A histology study described in mucormycosis patients the spread of fungal hyphae within the elastic lamina of intermediate to large calibre arteries. This is why a scrupulous assessment of the intracranial and facial vessels is compulsory [19]. The branches of the internal and external carotid and cavernous sinus are carefully evaluated by means of angiographic sequences. MRI signs of vascular involvement include enhancement and thickening of the vascular wall, thrombosis which displays loss of normal flow void and absence of enhancement [20, 21].
In this study we assessed also the relationship between MRI images and intra-operative findings in these patients. We ascertained the good reliability of the bright sequence on T2 fat suppression sequence in ascertaining the extension of the fungal disease beyond the sinuses. High positive predictive values were determined for the involvement of the infratemporal fossa, orbit, sphenoid bone and palate.
However, there are certain limitation of our study. The reduced number of cases represent a major drawback, large cohorts similar to those published in the studies coming from India cannot be accomplished in our environment. The lack of follow-up is another limitation of our study.
Conclusions
In conclusion, all patients presented nasal mucormycosis along with SARS-CoV-2 positive test and the maxillary and ethmoid sinuses, were the most frequently involved in these patients.
Conflict of interests
None to declare.
References
- 1.Rawson TM, Moore LSP, Zhu N, Ranganathan N, Skolimowska K, Gilchrist M, Satta G, Cooke G, Holmes A. Bacterial and Fungal Coinfection in Individuals with Coronavirus: A Rapid Review To Support COVID-19 Antimicrobial Prescribing. Clin Infect Dis. 2020;71(9):2459–2468. doi: 10.1093/cid/ciaa530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharma S, Grover M, Bhargava S, Samdani S, Kataria T. Post coronavirus disease mucormycosis: a deadly addition to the pandemic spectrum. J Laryngol Otol. 2021;135(5):442–447. doi: 10.1017/S0022215121000992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Skiada A, Pavleas I, Drogari-Apiranthitou M. Epidemiology and Diagnosis of Mucormycosis: An Update. J Fungi (Basel) 2020;6(4):265–265. doi: 10.3390/jof6040265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Safder S, Carpenter JS, Roberts TD, Bailey N. The "Black Turbinate" sign: An early MR imaging finding of nasal mucormycosis. AJNR Am J Neuroradiol. 2010;31(4):771–774. doi: 10.3174/ajnr.A1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sehgal A, Kumar J, Garg A, Jain A, Meher R, Singh M, Goel R. MR imaging spectrum in COVID associated Rhino-Orbito-Cerebral mucormycosis with special emphasis on intracranial disease and impact on patient prognosis. Eur J Radiol. 2022;152:110341–110341. doi: 10.1016/j.ejrad.2022.110341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Silverman CS, Mancuso AA. Periantral soft-tissue infiltration and its relevance to the early detection of invasive fungal sinusitis: CT and MR findings. AJNR Am J Neuroradiol. 1998;19(2):321–325. [PMC free article] [PubMed] [Google Scholar]
- 7.Yadav T, Tiwari S, Gupta A, Garg PK, Khera PS, Rajagopal R, Goyal A, Soni K, Chugh A, Jain V, Sureka B, Elhence P, Misra S. Magnetic Resonance Imaging in Coronavirus Disease - 2019 Associated Rhino-Orbital-Cerebral Mucormycosis (CA-ROCM) - Imaging Analysis of 50 Consecutive Patients. Curr Probl Diagn Radiol. 2022;51(1):112–120. doi: 10.1067/j.cpradiol.2021.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seo J, Kim HJ, Chung SK, Kim E, Lee H, Choi JW, Cha JH, Kim HJ, Kim ST. Cervicofacial tissue infarction in patients with acute invasive fungal sinusitis: prevalence and characteristic MR imaging findings. Neuroradiology. 2013;55(4):467–473. doi: 10.1007/s00234-013-1147-8. [DOI] [PubMed] [Google Scholar]
- 9.Rupa V, Maheswaran S, Ebenezer J, Mathews SS. Current therapeutic protocols for chronic granulomatous fungal sinusitis. Rhinology. 2015;53(2):181–186. doi: 10.4193/Rhino14.183. [DOI] [PubMed] [Google Scholar]
- 10.Mazzai L, Anglani M, Giraudo C, Martucci M, Cester G, Causin F. Imaging features of rhinocerebral mucormycosis: from onset to vascular complications. Acta Radiol. 2022;63(2):232–244. doi: 10.1177/0284185120988828. [DOI] [PubMed] [Google Scholar]
- 11.Therakathu J, Prabhu S, Irodi A, Sudhakar SV, Yadav VK, Rupa V. Imaging features of rhinocerebral mucormycosis: A study of 43 patients. The Egyptian Journal of Radiology and Nuclear Medicine. 2018;1:447–452. [Google Scholar]
- 12.deShazo RD, O'Brien M, Chapin K, Soto-Aguilar M, Gardner L, Swain R. A new classification and diagnostic criteria for invasive fungal sinusitis. Arch Otolaryngol Head Neck Surg. 1997;123(11):1181–1188. doi: 10.1001/archotol.1997.01900110031005. [DOI] [PubMed] [Google Scholar]
- 13.John TM, Jacob CN, Kontoyiannis DP. When Uncontrolled Diabetes Mellitus and Severe COVID-19 Converge: The Perfect Storm for Mucormycosis. J Fungi (Basel) 2021;7(4):298–298. doi: 10.3390/jof7040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adulkar NG, Radhakrishnan S, Vidhya N, Kim U. Invasive sino-orbital fungal infections in immunocompetent patients: a clinico-pathological study. Eye (Lond) 2019;33(6):988–994. doi: 10.1038/s41433-019-0358-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Palacios E, Rojas R, Rodulfa J, González-Toledo E. Magnetic resonance imaging in fungal infections of the brain. Top Magn Reson Imaging. 2014;23(3):199–212. doi: 10.1097/RMR.0000000000000025. [DOI] [PubMed] [Google Scholar]
- 16.Chan LL, Singh S, Jones D, Diaz EM, Ginsberg LE. Imaging of mucormycosis skull base osteomyelitis. AJNR Am J Neuroradiol. 2000;21(5):828–831. [PMC free article] [PubMed] [Google Scholar]
- 17.Mossa-Basha M, Ilica AT, Maluf F, Karakoç Ö, Izbudak I, Aygün N. The many faces of fungal disease of the paranasal sinuses: CT and MRI findings. Diagn Interv Radiol. 2013;19(3):195–200. doi: 10.5152/dir.2012.003. [DOI] [PubMed] [Google Scholar]
- 18.Han Q, Escott EJ. The Black Turbinate Sign, A Potential Diagnostic Pitfall: Evaluation of the Normal Enhancement Patterns of the Nasal Turbinates. AJNR Am J Neuroradiol. 2019;40(5):855–861. doi: 10.3174/ajnr.A6037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mathur S, Karimi A, Mafee MF. Acute optic nerve infarction demonstrated by diffusion-weighted imaging in a case of rhinocerebral mucormycosis. AJNR Am J Neuroradiol. 2007;28(3):489–490. [PMC free article] [PubMed] [Google Scholar]
- 20.Theoret J, Sanz GE, Matero D, Guth T, Erickson C, Liao MM, Kendall JL. The "guitar pick" sign: a novel sign of retrobulbar hemorrhage. CJEM. 2011;13(3):162–164. doi: 10.2310/10.2310/8000.2011.110279. [DOI] [PubMed] [Google Scholar]
- 21.Turgut M , Challa S , Akhaddar A , et al., editors. Fungal Infections of the Central Nervous System: Pathogens, Diagnosis, and Management . 1st edition . Springer ; 2019 . [Google Scholar]


