Abstract
Introduction
Balance and postural control are related to hearing and hearing loss, but whether they can be improved with hearing aid use in older adults is not clear. We systematically reviewed controlled studies in which balance and hearing were tested in experienced older hearing aid users to determine the potential effects of hearing aid use on balance.
Methods
The review was pre-registered in PROSPERO and performed in accordance with PRISMA. The question, inclusion, and exclusion criteria were defined using the Population, Intervention, Control, Outcomes and Study design (PICOS) framework. Older adults with hearing loss and no experience with hearing aids, or balance tests conducted without hearing aids in hearing aid users served as controls.
Results
A total of 803 studies were screened, eight of which met the inclusion and exclusion criteria and were included in the final review. Five of the eight studies found a significant correlation between the use of hearing aids and the outcomes of the balance tests. The quality of the studies was limited or moderate.
Key Discussion
The role of hearing aids in balance and postural control is unclear because of the quality of the papers and the sparse reporting of hearing status and hearing aids quality of fitting and use.
Keywords: Hearing, Hearing Aids, Older adults, Balance, Postural control
Introduction
Untreated hearing loss in older adults is correlated with negative consequences in many aspects of life – cognitive status [1, 2], loneliness [3, 4], depression, and reduced quality of life [5, 6]. In recent years, evidence is accumulating for the contribution of hearing impairment to reduced postural stability [7–10] and increased risk of falls [11, 12].
Falls are a major concern in older adults, affecting health and quality of life. The World Health Organization (WHO) reports a yearly occurrence of more than 37 million falls which are severe enough to require medical attention, and about 684,000 fatal falls. As reported by WHO, older people have the highest risk of death and injury caused by falls, and the risk increases with age [13]. The strongest predictors of falls are previous falls and balance/walking problems [14].
The Role of Hearing and Hearing Loss in Balance Control
There are several reasons to think that balance and postural control (defined as the ability to control the body in space for balance and orientation) issues could be related to hearing and hearing loss, and therefore that using hearing aids could have a positive direct or indirect effect on these functions. These are described briefly in the following paragraphs as motivation for the current review.
First, the proximity of the end organs of the auditory system and the vestibular system often results in common pathologies caused by one etiology. These include, for example, Meniere disease [15], and pathologies due to acoustic trauma [16, 17], viral infections [18], and age-related changes in the cochlea and peripheral vestibular organs [19, 20]. It was shown that in cases of vestibular loss, the role of auditory cues increases [21] and introducing auditory input in challenging conditions (standing on foam) can substantially reduce sway [22].
Second, auditory input is one of the factors involved in maintaining postural control. Studies have shown that introducing auditory information (e.g., white noise [23]) may improve stability and reduce sway in both young and older adults [24, 25] regardless of the presence of visual distraction [23]. Hearing loss can result in uncertainty in orientation [26–29] and increased self-limitations on mobility and physical activities [24]. Improving audibility can thus improve access to auditory information, making it available for balance control.
Third, in older adults with hearing impairment, larger attentional resources are allocated to listening, such that fewer resources are available when divided attention is needed [30, 31]. Since walking and mobility depend on both automatic and executive control [32], reduced available resources can affect executive control while trying to maintain control during walking and mobility [16, 26, 29]. While there is evidence for longitudinal, plasticity-driven, improved speech perception (for review see: Lavie et al. [33]), and improved cognition when using hearing aids (see review in Kalluri et al. [34] and Sanders et al. [35]), the evidence for improved attention is mixed [35, 36].
Hearing Aid Use and Falls
Hearing aids are the most common rehabilitation devices for older adults with hearing loss. When used, properly fitted hearing aids improve audibility and can facilitate speech recognition [33]. In addition, a growing body of research asked whether hearing aids can be used to mitigate the harmful side-effects of age-related hearing loss in other areas, such as falls. In a large-scale study, Riska et al. [37] inspected this association by reviewing self-reported history of falls and self-reported hearing loss in 17,923 individuals, 549 of them were hearing aid users. While they found that the odds of falling increased with increasing self-reported hearing difficulty, hearing aid use had no effect on the odds for falls or fall-related injuries. However, hearing acuity was not tested in this study and self-reports of hearing loss can underestimate hearing status [38]. Moreover, balance was not objectively tested as well in this study.
The Current Review
In the current review, we ask whether the use of hearing aids can improve balance and thus reduce risk of falls in older adults with hearing impairment. We targeted studies in which both balance and hearing were objectively tested in older adults. As explained above, long-term use of hearing aids can result not only in improved audibility but also in plastic changes in speech perception [33], improved cognitive status [39, 40], and alternations of the nervous system [41, 42]. Therefore, we targeted studies that included experienced hearing aid users. Inclusion criteria were as follows: adults age ≥55 years; participants who had no neurological or cognitive problems; hearing status was evaluated through behavioral hearing test; balance and postural controls were objectively evaluated and were not determined merely with participants’ self-reports; participants who had at least mild hearing loss; participants who use hearing aids were included in the study; peer reviewed papers that were published in English. Inclusion and exclusion criteria were defined according to PICOS (Population, Intervention, Control, Outcomes and Study design) framework (see Table 1).
Table 1.
PICOS inclusion and exclusion criteria
| Key concepts, synonyms | Inclusion and exclusion criteria |
|---|---|
| Participants | Older adults with presbyacusis/presbycusis/age-related hearing loss, no neurological or cognitive problems. |
| Intervention | Use of hearing aids. |
| Control | Older adults with hearing loss who are not using hearing aids, or balance tests without hearing aids in hearing aid users. |
| Outcome | Aided or unaided measures of balance and postural control. |
| Study design | Peer-reviewed experimental and quasi-experimental studies. Reported direct assessments of hearing and balance/postural control. |
Methods
The study protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) (Registration number: CRD42022337283). The review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.
Three of the authors (N.T., N.S-Z., and S.C.) systematically searched five databases: CINAHL, SCOPUS, COCHRANE, PubMed, and AgeLine with the following search terms: For age: “older adult*” OR aging* OR old* OR senior* OR elder* OR aged* OR geriatric*. For hearing loss and hearing aid use: “hearing aid*” OR “aural rehabilitation” OR “hearing device*” OR “hearing rehabilitation” OR “hearing loss” OR presbycusis OR presbyacusis OR “hearing amplification” OR “hearing impair” OR “impaired hearing”. For balance/postural control: “postural control” OR gait* OR “postural balance” OR fall* OR walking OR presbyvestibulopathy OR mobility OR imbalance OR balance OR Stability OR “time up and go” OR posture OR “postural sway” OR “one legged standing” OR “one legged stance” OR “fall injury*”. The last search was conducted in April 2022.
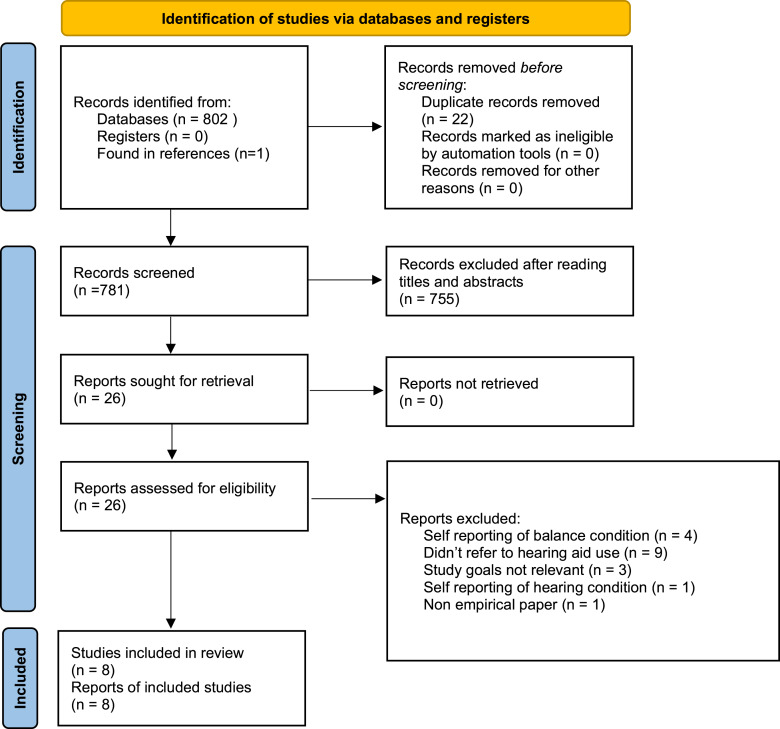
Three authors screened the papers independently by title and abstract (N.T., N.S-Z., and S.C.). Out of the 802 papers that were screened, 26 articles (see Prisma) were independently assessed by three of the authors (N.T., N.S-Z., and S.C.). When needed, the authors discussed whether certain papers should or should not be included in the review, and an agreement was reached. The papers included in the final review were read by all five authors (L.L., K.B., N.T., S.C., and N.S-Z.). From each paper, the results of all relevant outcome measures were extracted (see Table 2).
Table 2.
Summary of studies included in the current systematic review
| Study | No. of groups | inclusion criteria | Groups and numbers | Age range, years, mean, standard deviation | Hearing | Hearing aid use | |
|---|---|---|---|---|---|---|---|
| 1 | Kowalewski et al. [43], 2018 | 3 | Recruited: 47. Participated: young adults normal hearing (20); older adults normal hearing (20); older adults with hearing loss [probably hearing aid users] (19), young adults | Young: 27.2±3/0; older adults normal hearing: 68.7±4.3; older adults hearing impaired: 73.2±9.1 | NS | Not specifically detailed. It seems that the old hearing-impaired adults used hearing aids, but details on time of use or type of hearing aids are not provided. | |
| 2 | Ibrahim et al. [44], 2019 | 2 | Normal hearing and hearing aid users, age +18 years. Hearing loss group: unilateral or bilateral moderate to severe hearing loss, with at least 6 months of hearing aid use. | Normal hearing (21, of whom 4 with high frequency loss), hearing aid users (9) | Normal: 37.09±15.9 years; hearing loss: 58.5±21.2 years | Normal hearing group: valid audiogram (13 participants) or online screening test (8 participants), of whom 4 normal hearing (<20 dB in all frequencies) and 4 with loss higher than 30 dB in 4,000 and 8,000 Hz. Hearing loss group: hearing not described. | |
| 3 | McDaniel et al. [45], 2018 | 1 | Adult hearing aid users (22) | 58–81 (mean 68.5) | Mild to moderately severe. Average audiogram available. Average audibility index 41 right ear, 33 left ear | Bilateral hearing aids with frequency transposition, 3 months to 10 years’ experience, average 3.5 years | |
| 4 | Ninomiya et al. [46], 2021 | 2 | Adults with hearing loss, who use bilateral hearing aids for more than 1 year (HA) (10); normal hearing adults (N) (10) | HA group: 62–79, average 63.4; N group: 62–75, average 71.2 years | HA group: average 53.8–70 dB | HA group: 1–8 years, average 3.7 years | |
| 5 | Rumalla et al. [47], 2015 | 1 | Adults, age › 65 years, use hearing aids 3 months or more, aided thresholds of 25 dB or worse in each ear, could understand English-spoken directions, and could ambulate without assistive devices. | Older adults with hearing loss (14) | 65–91, average: 77 | NS. Mean audiometric gain: 12.75 dB SPL | NS |
| 6 | Negahban et al. [48], 2017 | 2 | Age >60 years, could ambulate without assistive device, bilateral hearing loss 40–70 dB; aided group: bilateral hearing aid use ≥3 months | Aided group (use hearing aids) (22) and unaided group (25) | 67±3.5 years, 67.1±5.5 years. Group names NS | PTA 4 frequencies: 40–70 dB; aided PTA in aided group20-35 dB | Aided group: bilateral hearing aid use 33.5±16.68 months |
| 7 | Criter and Gustavson [49], 2020 | 3 | Community-dwelling adults, age >60 years. Criteria to ensure safe participation in the study detailed in previous studies | Recruited: 86. Final participants: nonaudiology patients (28), audiology patients with hearing aids (18), audiology patients without hearing aids (28) | Nonaudiology patients: 60–81 (70.6±5.5); audiology patients with hearing aids: 69–81 (72.9±3.2); audiology patients without hearing aids 61–84 (71.5±6.6). | NS | NS |
| 8 | Vitkovic et al. [50], 2016 | 3 | Normal hearing: no hearing loss (>20 dB HL in both ears across the frequency range); hearing impaired: 4 frequencies PTA >20 dB HL; vestibular-impaired: documented vestibular dysfunction of any degree or configuration; all subjects: free from any orthopedic or neurological conditions that may affect balance and did not require any balance or walking aids to maintain a quiet stance | Normal hearing (50), hearing loss (28, 17 of them hearing aid users), vestibular-impaired (19). | Normal hearing 28.84 (21–56); hearing loss 65.3 (26–80) of which - unaided 66.7 (45–80), aided 64.7 (26–79); vestibular loss 63.6 (34–83) | Mean 4 freq. PTA, Rt, Lt: normal hearing: 3.8 (3.5) 3.3 (3.5); hearing loss unaided 29.9 (6.3) 34.2 (13.2); hearing loss aided 49.0 (16.7) 47.8 (13.4); Vestibular loss: 27.9 (13.4) 28.0 (21.7). Type of audiograms described | 17 subjects were fitted with hearing aids bilaterally (4 BTE, 6 RITE, 1 ITE, 2 ITC, 3 CIC) and 2 with 1 BTE |
| Study | Balance and falls | Exclusion criteria | Relevant measures | Other measures (questionnaires, other tests) | Relevant results | Comments/conclusions | |
|---|---|---|---|---|---|---|---|
| 1 | Kowalewski et al. [43], 2018 | No history of vestibular, somatosensory or balance impairments. | Motion sickness/dizziness. Medications that affect balance. Undiagnosed cognitive or sensory impairment | Dual task (auditory and balance). Balance: maintain balance with 3 balance conditions of unexpected (backwards) surface translations. Auditory: repeat sentence in noise. 3 conditions: 1. Single task balance. 2. Dual task, hearing impaired adults used their hearing aids. 3. Hearing loss: hearing impaired adults tested unaided; adults with normal hearing – audio files manipulated to simulate hearing loss. Outcome measures: number of compensatory steps to correct imbalance and sentence in noise scores. | Older adults with hearing loss have poorer reactive balance (take greater number of steps required to regain balance) compared to young adults and older adults with normal hearing. Wearing hearing aids did not reduce the number of steps required to regain balance. | Very poor description of participants and results | |
| 2 | Ibrahim et al. [44], 2019 | Balance disorders that increase risk of falls during Romberg and Tandem tests; use of medications that can cause hearing loss or affect balance; use of walking aid; history of stroke. | Auditory: 48 trials of sound localization, particularly front-back with high-pass and low-pass narrow band, with or without hearing aids or earplugs. Postural stability: Romberg on foam (goal: maintain balance for 30 s); Tandem test (goal: maintain posture for 30 s). Both tests performed in two conditions: with/without hearing aids (hearing loss group) and with/without earplugs (normal hearing group). Each test performed 3 times for each condition | DHI (Dizziness Handicap Inventory) | Normal participants balance performance was not affected by absence of auditory input (using earplugs). Hearing aid users: balance was better in aided versus unaided conditions: Tandem: 18±8.8 s unaided, 21.5±8.2 aided (mean improvement: 3.36 s). Romberg on foam: 13.3±9.2 s unaided, 17.9±8.4 s aided (mean improvement 4.4 s). Localization improved when using hearing aids (hearing loss group, 5 participants tested): score unaided: average correct score 50.1% for low-pass filtered sound and 64.5% for high pass; aided results: 71.6% for low-pass (+29), 76.8% for high pass (+26) or when tested without earplugs (normal group) | Hearing had significant effect on postural stability. Note: some statistical analyses were not performed on the full study cohort. Only 5 participants performed the localization test. | |
| 3 | McDaniel et al. [45], 2018 | No vestibular disfunction. 7 participants (32%) had fallen at least once in 3 years prior the study, 5 participants (23%) had concerns regarding their balance. | Degenerative neurological disease, history of stroke, spinal and/or hip replacement, medications with potential balance-altering effects. Excluded due to undiagnosed cognitive or sensory impairment or withdrew from study: 5 young adults, 13 older adults with normal hearing, 3 older adults with hearing loss. | Sensory Organization Tests (SOT) – 6 conditions – data collected regarding efficacy of proprioceptive, visual and vestibular senses, and the ability to use these senses to regulate balance. Multitalker babble at 65 dB SPL was presented during tests from front stereo loudspeakers at ear level, 1 m from participants’ head, to provide additional sensory stimulation. Each of the 6 conditions was tested twice: with and without the hearing aids | No significant differences in the SOT composite score between aided and unaided conditions. No differences between and among each of the test conditions in aided versus unaided tests. | The results suggest that in experienced hearing aid users, using their hearing aids during SOT does not change balance. However, ceiling effect might have obscure differences between aided and unaided conditions | |
| 4 | Ninomiya et al. [46], 2021 | HA: no abnormalities in vestibular test including vestibulo-ocular reflex test and head impulse test (exclusion criteria) | No history of neurological or muscular disease | Posturography in an unechoing room. Measures: displacement of center of foot pressure (COP). 4 test conditions, each tested twice: with and without hearing aids (HA group); with and without sound (normal hearing group) | HA group: hearing aid use decreased the total path area. Maximum COP displacement in ML (mediolateral) axis was not affected by hearing aid use (5.86 cm and 5.73 cm, eyes open; 2.77 and 2.66 cm, eyes open). In AP (anteroposterior) axis hearing aids significantly decreased the maximum COP displacement (4.53 and 4.26 cm). Hearing aids reduced average sway velocity (3.39 cm/s and 3.18 cm/s). In ML axis hearing aids decreased the average sway velocity (1.8 cm/s and 1.67 cm/s). Similar results in and AP axis (1.80 cm/s and 1.70 cm/s). | Auditory cues improved the total path area in challenging conditions in HA users and in normal-hearing participants | |
| 5 | Rumalla et al. [47], 2015 | Prior to testing, none of the participants reported a perceived difference in balance or performance due to wearing hearing aids. For the Activities-specific Balance Confidence (ABC) Scale test, 13 of the 14 participants scored as having a high level of physical functioning, and one participant scored at a moderate level of physical functioning | History of degenerative neurologic disease, stroke, spinal stenosis, joint replacement, or balance-altering medication or surgery | Auditory: average gain at 0.5, 1.0, 2.0, and 4.0 kHz defined as dB SPL of amplification required for sound to be perceived as a comfortable conversational sound. Postural stability: 1. the Romberg on foam test 2. the tandem stance test. Both tests probably with eyes closed. Tests administered twice, with hearing aids on and off. Broad band noise 0–4 kHz, 65 dB presented during tests. In both tests, the results were measured in seconds (max 30 s). A trial was terminated if participants moved arms or feet, opened eyes, stepped, or required spotter to maintain balance. | Questionnaire: ABC Scale Question prior to testing: participants were asked: “Do you feel that your hearing aids make your balance better, worse, or is there no difference?” Questions after testing: 1. “Do you feel that the sound made your balance better, worse, or no difference?” 2. “Do you feel that you performed better with your hearing aids on, hearing aids off, or no difference?” | Romberg on foam: 10/14 participants better in aided than in the unaided condition; other four achieved maximum of 30 s in both conditions. Significant difference in balance between unaided (mean score 17.0±10.2 s, median 14.3 s), and aided (25.6±7.8 s, median 30.0 s). Tandem: significant improvement in aided compared to unaided condition. Unaided mean 4.5±3.3 s, median 3.2 s; aided mean 9.8±7.4 s, median 5 9.6 s. The four participants who had reached the ceiling of 30 s in both the unaided and aided conditions on the foam test showed improvement with amplification in the more difficult tandem test. Mean improvement on foam test for the 14 participants: 8.5 s; improvement for the 10 participants who did not have a ceiling effect: 11.6 s (mean audiometric gain: 13.9 dB SPL). Mean improvement on tandem test for all 14 participants: 5.3 s. For the four participants who reached a ceiling effect on the foam, mean improvement on tandem test: 8.7 s (mean audiometric gain 5 9.8 dB SPL). | Wearing hearing aids provide a significant improvement in balance and a decreased risk of falling in older adults with hearing loss. (The ABC test results did not show any correlation to the participants’ overall performance on both tests). |
| 6 | Negahban et al. [48], 2017 | Hearing loss due to otosclerosis or middle ear infections, a history of neurological diseases, surgical operation on lower limbs or spine within 6 months prior to study, pain in lower limb during standing (e.g., knee or low back pain) | Static balance: stand with eyes open and eyes closed on rigid surface and on a foam pad (4 conditions). Indicators for postural stability were COP parameters including mean velocity, standard deviation (SD) velocity (in anteroposterior (AP) and mediolateral (ML) directions), and sway area. Aided group assessed twice (hearing aids on and hearing aids off), unaided group assessed once. The experiment was performed in a regular room with ambient sound. Hearing: hearing thresholds with hearing aids on and off | height, BMI | Interaction of group by postural conditions significant for SD velocity in AP and ML directions. Multiple comparisons: open eyes-foam surface: greater SD velocity in the off-aided than the on-aided, and the unaided than the on-aided. No significant differences between off-aided and unaided group for SD velocity in AP and ML. Pearson correlation coefficient between time of acquisition hearing aids and benefit of hearing aids (i.e., difference between off-aided and on-aided conditions) on postural control for the SD velocity in both AP and ML directions: significant positive correlation for SD velocity in AP (r = 0.50, p = 0.017), but not in ML (r = 0.31, p = 0.15) direction. | Using hearing aids provided a significant improvement in postural stability (as indicated by decreased SD velocity) among older adults with hearing loss. On-aided was always recorded first followed by off-aided. Therefore, the observed changes could be in part due to fatigue or other factors not related to hearing aids. | |
| 7 | Criter and Gustavson [49], 2020 | NS | No hearing aids (use of cochlear implant or assistive listening device ALD). Excluded after recruitment: use of cochlear implant (2), use of ALD (1), oldest audiology patients with hearing aids (8) and oldest audiology patients without hearing aids (1) | Time Up and Go (TUG) | Questionnaires: HHIE (only unaided scores used), DHI (Dizziness Handicap Inventory), ABC Scale. Questions regarding health, hearing, balance and fall history (no. of fall within 12 months prior to study) | Significant correlation between HHIE score and no. of falls in audiology patients. More falls in audiology patients without hearing aids. Trend towards increase fall risk. HHIE also in positive correlation with DHI in audiology patients without hearing aids. Small nonsignificant differences in TUG among the groups. | participants excluded for not having hearing aids and to equalize average age of the groups |
| 8 | Vitkovic et al. [50], 2016 | Vestibular impaired group: documented vestibular dysfunction of any degree or configuration | Hearing loss group: any vertiginous episodes or imbalance problems | Static postural sway measured via a Nintendo Wii Balance Board (WBB), 16 trials in 4 standing conditions (firm and foam surface, eyes open and close) and 4 acoustic environments (ambient room, sound-treated room with the subject wearing E-A-R earplugs, sound-treated room with a continuous white noise presented from a front speaker 106 cm away and a sound-treated room with a moving noise). Outcome measures: total center of pressure (CoP) path length, which quantifies the total amount of sway during a trial. participants with hearing loss were tested with and without their hearing aids | Height, years with hearing loss | Sway in normal hearing subjects was increased when there were fewer sound cues available. In participants with hearing loss sound slightly increased sway, but when tested in aided conditions, participants had less sway in the presence of sound. There was no significant effect of sound environment or aided condition (p > 0.05), but there was a significant interaction (p = 0.048). | A spatial hearing map contributes to balance control. The amplification provided by the hearing aids increase access to spatial cues utilized for balance control. |
HA, hearing aids; NS, not specified; PTA, pure tone average; BTE, behind the ear; RITE, receiver in the ear; ITE, in the ear; ITC, in the ear; CIC, completely in the canal; SOT, sensory organization test; COP, center of pressure; HHIE-S, hearing handicap inventory for the elderly (screening).
Quality of Evidence
LL and KB separately evaluated each study’s quality according to the Downs and Black [51] checklist, which consists of 27 questions relating to reporting, external and internal validity, and statistical power. Final ratings were discussed and agreed upon.
Results
Out of 802 studies, seven studies were included in the final review, as shown in the PRISMA flow diagram (see Fig. 1). One additional paper [50] was detected through a reference list of another paper. This paper’s title does not refer to hearing aids or hearing rehabilitation, and thus could not have been detected through the systematic search. Outcome measures were considered relevant when balance was measured with and without hearing aids.
Fig. 1.
The PRISMA literature search.
Data Extraction
Hearing and Hearing Aids
In all eight studies (see Table 2), older participants who use hearing aids were included. In the majority of the studies, other populations were also included: older hearing-impaired participants who do not use hearing aids (three studies), participants with vestibular disorders (one study), and young adults (two studies). Hearing status was poorly described in the majority of the studies. Average audiogram was presented in only one paper [45], and one paper described average 4 frequencies PTA in each ear for each group [50]. Two papers described either average range of hearing levels across groups [46] or average 4 frequencies PTA across groups + aided PTA in the aided group [48]. The remaining four papers did not give any description of hearing status or specified just mean audiometric gain with hearing aids without details regarding participants hearing [47]. Length of hearing aid use was 3 months–17 years, but only three studies documented this information [45, 46, 48]. McDaniel et al. [45] additionally reported that hearing aids had frequency transposition, and Vitcovitch et al. [50] also documented the types of hearing aids. No further data were available (e.g., average daily use, technology of hearing aids, fitting strategy, etc.).
Balance and Falls
Information regarding balance and falls as well as factors that might have an effect on posture control was available in the majority of the papers as a part of the description of participants’ characteristics or of the exclusion criteria. In seven of the eight studies, participants with documented vestibular deficits were not included. One study included a vestibular-impaired group.
Relevant Measures
In the majority of studies, the role of auditory input in balance and postural control was investigated with balance tests that were conducted in various background noises. Various balance tests were used: Romberg and tandem tests (two studies), static balance on rigid and foam surfaces (two studies, one of them with Wii Balance Board), Sensory Organization Tests (one study), osturography (one study), Timed Up and Go (one study), and dual task (balance task: maintain balance on a changing surface, one study).
Use of Hearing Aids and Balance/Postural Control
To test the role of hearing aids, tests were conducted with and without hearing aids in six of the studies and with hearing aids on and off in one study. In one study [49], hearing aid status during test was not described.
The studies included in the current review had mixed findings. Overall, the majority of the studies found a significant correlation between the use of hearing aids and the outcomes of the balance tests. Of the eight studies, five studies found evidence for better balance in aided conditions than in unaided conditions [44, 46–48, 50]. In one of these studies [46], three out of the four outcome measures indicated positive effects of hearing aid use, and one measure (COP displacement in the mediolateral axis) was not affected by the use of hearing aids. Three studies showed no effect of hearing aid use [43, 45, 49].
Using hearing aids improved balance (e.g., in the Romberg and tandem tests and in posturography), reduced sway during balance control, and improved postural control. Balance tests indicated longer times until fail (in the Romberg and tandem tests) and decreased maximum center of pressure displacement.
Quality of Individual Studies and Overall Evidence Base
The results of the quality assessment are presented in Table 3. The total quality grades of the individual studies ranged from 12 to 16 points (43–57% of the maximum possible score). The quality of five of the eight papers included in the current review was 12–13 points. This translates to limited quality (based on Rechberger et al. [52]). The quality of the remaining three papers was 15–16 points (moderate quality). These grades stem mainly from low external and internal validity, general lack of power analysis, and low-to-moderate reporting.
Table 3.
Methodological quality of individual studies assessed according to the checklist of Downs and Black [51]
| Studies | Quality of reporting (Q1–10) max score = 11 | External validity (Q11–13) max score = 3 | Internal validity – bias (Q14–10) max score = 7 | Internal validity – confounding selection bias) (Q21–26) max score = 6 | Power (Q27) max score = 1 | Total | |
|---|---|---|---|---|---|---|---|
| 1 | Kowalewski et al. [43], 2018 | 7 | 1 | 2 | 2 | 0 | 12 |
| 2 | Ibrahim et al. [44], 2019 | 7 | 1 | 3 | 1 | 1 | 13 |
| 3 | McDaniel et al. [45], 2018 | 8 | 1 | 4 | 3 | 0 | 16 |
| 4 | Ninomiya et al. [46], 2021 | 9 | 1 | 4 | 1 | 0 | 15 |
| 5 | Rumalla et al. [47], 2015 | 8 | 1 | 4 | 3 | 0 | 16 |
| 6 | Negahban et al., 2017 [48] | 7 | 1 | 4 | 1 | 0 | 13 |
| 7 | Criter and Gustavson [49], 2020 | 8 | 1 | 2 | 2 | 0 | 13 |
| 8 | Vitkovic et al. [50], 2016 | 5 | 1 | 4 | 2 | 0 | 12 |
Consistent with Kalluri et al. [34], we scored question 27 as 1 if a power analysis was conducted and 0 if not. The maximum possible score was thus 28.
Discussion
Overall, the majority of the studies screened in the current review found a significant correlation between the use of hearing aids and improved balance. These findings were apparent in a variety of tests and outcome measures, most of them testing static balance (e.g., Romberg, Tandem, static postural sway measured via a Nintendo Wii Balance Board, maintain balance with three balance conditions of unexpected (backwards) surface translations). Participants with documented balance disorders or vertigo were excluded from the majority of the studies. Therefore, even when improved balance with hearing aids was documented in the studies, it is not clear whether these findings are reflected in everyday behavior.
But while the majority of the studies found various indications for the beneficial effects of using hearing aids on balance control, these results should be interpreted with caution. First, the overall quality of the studies was limited to moderate. Three of the five studies that found significant improvement in balance tests when tested in aided conditions (with hearing aids) had limited scores (12–13 points, 44–48% of the maximum possible score). Indeed, some of the limitations of studies concerning the use of hearing aids are inevitable (e.g., lack of randomization in intervention with hearing aids or lack of blindness which is impossible to achieve when both participants and experimenters are aware of the use of hearing aids). But the low scores in the majority of the studies stemmed also from low to moderate reporting and methodological issues like lack of power analysis and, in some cases, improper use of the statistical tests. Furthermore, the poor level of reporting on hearing status and the use of hearing aids makes it impossible to infer what the actual role of hearing aids in balance and postural controls is, since crucial information such as length of hearing aid use, average daily use or quality of fitting were generally not reported. Moreover, data on hearing status were not always available and usually poorly described. Future studies should take these into consideration so that outcomes can be summarized across studies (e.g., with meta-analysis).
In the current review, we were looking for studies that included experienced users of hearing aids. If hearing aid use has the potential to induce long-term changes in various auditory and nonauditory variables, studies that inspect the effects of prolonged use of hearing aids should not refrain from a thorough inspection of the quality of hearing aid fitting nor from the inspection of the actual use of hearing aids by the study participants.
A major objective in testing the connection between hearing rehabilitation and balance is the endeavor to reduce fall risk in older individuals. Whether the use of hearing aids can prevent or reduce falls may affect counseling for older hearing-impaired adults. Unfortunately, the low quality of the studies included in the current review and lack of adequate data concerning hearing and hearing aid use do not allow any clinically relevant conclusion. Therefore, we conclude that the current body of literature is not sufficient to infer that using hearing aids can improve balance and postural control, and counseling regarding this connection should be cautious.
Acknowledgments
We thank the staff of the University of Haifa Library for their guidance and support throughout the review process.
Statement of Ethics
An ethics statement is not applicable because this study is based exclusively on published literature.
Conflict of Interest Statement
The authors declare no conflict of interests.
Funding Sources
The Israeli Science Foundations (Grant No. 206/18) supports the empirical work of Karen Banai and Limor Lavie.
Author Contributions
Limor Lavie and Karen Banai designed the study. Limor Lavie, Nawras Tobia, Neta Slav-Zarfati, Shefi Castel, and Karen Banai defined the search terms and participated in various stages of the systematic literature review. Karen Banai and Limor Lavie evaluated the quality of the studies. Limor Lavie wrote the first draft of the manuscript. Limor Lavie and Karen Banai edited and revised the manuscript. Limor Lavie, Nawras Tobia, Neta Slav-Zarfati, Shefi Castel, and Karen Banai approved the final version.
Funding Statement
The Israeli Science Foundations (Grant No. 206/18) supports the empirical work of Karen Banai and Limor Lavie.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article. Further inquiries can be directed to the corresponding author.
References
- 1. Lin FR. Hearing loss and cognition among older adults in the United States. J Gerontol A Biol Sci Med Sci. 2011;66(10):1131–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lin FR, Yaffe K, Xia J, Xue QL, Harris TB, Purchase-Helzner E, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173(4):293–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Weinstein BE, Ventry IM. Hearing impairment and social isolation in the elderly. J Speech Hear Res. 1982;25(4):593–9. [DOI] [PubMed] [Google Scholar]
- 4. Mick P, Kawachi I, Lin FR. The association between hearing loss and social isolation in older adults. Otolaryngol Head Neck Surg. 2014;150(3):378–84. [DOI] [PubMed] [Google Scholar]
- 5. Davis JC, Robertson MC, Ashe MC, Liu-Ambrose T, Khan KM, Marra CA. International comparison of cost of falls in older adults living in the community: a systematic review. Osteoporos Int. 2010;21(8):1295–306. [DOI] [PubMed] [Google Scholar]
- 6. Mulrow CD, Aguilar C, Endicott JE, Velez R, Tuley MR, Charlip WS, et al. Association between hearing impairment and the quality of life of elderly individuals. J Am Geriatr Soc. 1990;38(1):45–50. [DOI] [PubMed] [Google Scholar]
- 7. Agmon M, Lavie L, Doumas M. The association between hearing loss, postural control, and mobility in older adults: a systematic review. J Am Acad Audiol. 2017;28(6):575–88. [DOI] [PubMed] [Google Scholar]
- 8. Foster JI, Williams KL, Timmer BH, Brauer SG. The association between hearing impairment and postural stability in older adults: a systematic review and meta-analysis. Trends Hear. 2022;26:23312165221144155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Morris B, Cosetti M, Kelly J, Yang J, Harel D, Medlin A, et al. Differing postural control patterns in individuals with bilateral and unilateral hearing loss. Am J Otolaryngol. 2023;44(4):103866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zarei H, Norasteh AA, King L. The effect of auditory cues on static postural control: a systematic review and meta-analysis. Audiol Neurootol. 2022;27(6):427–36. [DOI] [PubMed] [Google Scholar]
- 11. Jiam NT-L, Li C, Agrawal Y. Hearing loss and falls: a systematic review and meta-analysis. Laryngoscope. 2016;126(11):2587–96. [DOI] [PubMed] [Google Scholar]
- 12. Lin FR, Ferrucci L. Hearing loss and falls among older adults in the United States. Arch Intern Med. 2012;172(4):369–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO (26.4.2021). Falls. https://www.who.int/news-room/fact-sheets/detail/falls. [Accessed 20 Oct 2022].
- 14. Jia H, Lubetkin EI, DeMichele K, Stark DS, Zack MM, Thompson WW. Prevalence, risk factors, and burden of disease for falls and balance or walking problems among older adults in the U.S. Prev Med. 2019;126:105737. [DOI] [PubMed] [Google Scholar]
- 15. Proctor LR. Results of serial vestibular testing in unilateral Ménière’s disease. Am J Otol. 2000;21(4):552–8. [PubMed] [Google Scholar]
- 16. Chen YJ, Young YH. Secondary endolymphatic hydrops after acoustic trauma. Otol Neurotol. 2016;37(5):428–33. [DOI] [PubMed] [Google Scholar]
- 17. Wang YP, Hsu WC, Young YH. Vestibular evoked myogenic potentials in acute acoustic trauma. Otol Neurotol. 2006;27(7):956–61. [DOI] [PubMed] [Google Scholar]
- 18. Cohen BE, Durstenfeld A, Roehm PC. Viral causes of hearing loss: a review for hearing health professionals. Trends Hear. 2014;18:2331216514541361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gluth MB, Nelson EG. Age-related change in vestibular ganglion cell populations in individuals with presbycusis and normal hearing. Otol Neurotol. 2017;38(4):540–6. [DOI] [PubMed] [Google Scholar]
- 20. Say MA, Sevik Elicora S, Erdem D, Bilgin E, Baklaci D. Evaluation of the vestibular system in individuals with presbycusis using video head impulse test and videonystagmography. Acta Otolaryngol. 2021;141(6):545–50. [DOI] [PubMed] [Google Scholar]
- 21. Lubetzky AV, Gospodarek M, Arie L, Kelly J, Roginska A, Cosetti M. Auditory input and postural control in adults: a narrative review. JAMA Otolaryngol Head Neck Surg. 2020;146(5):480–7. [DOI] [PubMed] [Google Scholar]
- 22. Maheu M, Sharp A, Pagé S, Champoux F. Congenital deafness alters sensory weighting for postural control. Ear Hear. 2017;38(6):767–70. [DOI] [PubMed] [Google Scholar]
- 23. Ross JM, Balasubramaniam R. Auditory white noise reduces postural fluctuations even in the absence of vision. Exp Brain Res. 2015;233(8):2357–63. [DOI] [PubMed] [Google Scholar]
- 24. Zhong X, Yost WA. Relationship between postural stability and spatial hearing. J Am Acad Audiol. 2013;24(9):782–8. [DOI] [PubMed] [Google Scholar]
- 25. Tanaka T, Kojima S, Takeda H, Ino S, Ifukube T. The influence of moving auditory stimuli on standing balance in healthy young adults and the elderly. Ergonomics. 2001;44(15):1403–12. [DOI] [PubMed] [Google Scholar]
- 26. Viljanen A, Kaprio J, Pyykkö I, Sorri M, Koskenvuo M, Rantanen T. Hearing acuity as a predictor of walking difficulties in older women. J Am Geriatr Soc. 2009;57(12):2282–6. [DOI] [PubMed] [Google Scholar]
- 27. Viljanen A, Kaprio J, Pyykkö I, Sorri M, Pajala S, Kauppinen M, et al. Hearing as a predictor of falls and postural balance in older female twins. J Gerontol A Biol Sci Med Sci. 2009;64(2):312–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gispen FE, Chen DS, Genther DJ, Lin FR. Association between hearing impairment and lower levels of physical activity in older adults. J Am Geriatr Soc. 2014;62(8):1427–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mikkola TM, Polku H, Portegijs E, Rantakokko M, Rantanen T, Viljanen A. Self-reported hearing status is associated with lower limb physical performance, perceived mobility, and activities of daily living in older community-dwelling men and women. J Am Geriatr Soc. 2015;63(6):1164–9. [DOI] [PubMed] [Google Scholar]
- 30. Wingfield A, Tun PA. Spoken Language comprehension in older adults: interactions between sensory and cognitive change in normal aging. Semin Hear. 2001;22(03):287–302. [Google Scholar]
- 31. Wingfield A, Tun PA, McCoy SL. Hearing loss in older adulthood: what it is and how it interacts with cognitive performance. Curr Dir Psychol Sci. 2005;14(3):144–8. [Google Scholar]
- 32. Clark DJ. Automaticity of walking: functional significance, mechanisms, measurement and rehabilitation strategies. Front Hum Neurosci. 2015;9:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lavie L, Shechter L, Banai K. Plastic changes in speech perception in older adults with hearing impairment following hearing aid use: a systematic review. Int J Audiol. 2021;20:1–9. [DOI] [PubMed] [Google Scholar]
- 34. Kalluri S, Ahmann B, Munro KJ. A systematic narrative synthesis of acute amplification-induced improvements in cognitive ability in hearing-impaired adults. Int J Audiol. 2019;58(8):455–63. [DOI] [PubMed] [Google Scholar]
- 35. Sanders ME, Kant E, Smit AL, Stegeman I. The effect of hearing aids on cognitive function: a systematic review. PLoS One. 2021;16(12):e0261207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shinn-Cunningham BG, Best V. Selective attention in normal and impaired hearing. Trends Amplif. 2008;12(4):283–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Riska KM, Peskoe SB, Kuchibhatla M, Gordee A, Pavon JM, Kim SE, et al. Impact of hearing aid use on falls and falls-related injury: results from the health and retirement study. Ear Hear. 2022;43(2):487–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Tsimpida D, Kontopantelis E, Ashcroft D, Panagioti M. Comparison of self-reported measures of hearing with an objective audiometric measure in adults in the English longitudinal study of ageing. JAMA Netw Open. 2020;3(8):e2015009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dawes P, Emsley R, Cruickshanks KJ, Moore DR, Fortnum H, Edmondson-Jones M, et al. Hearing loss and cognition: the role of hearing AIDS, social isolation and depression. PLoS One. 2015;10(3):e0119616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mahmoudi E, Basu T, Langa K, McKee MM, Zazove P, Alexander N, et al. Can hearing aids delay time to diagnosis of dementia, depression, or falls in older adults? J Am Geriatr Soc. 2019;67(11):2362–9. [DOI] [PubMed] [Google Scholar]
- 41. Glick HA, Sharma A. Cortical neuroplasticity and cognitive function in early-stage, mild-moderate hearing loss: evidence of neurocognitive benefit from hearing aid use. Front Neurosci. 2020;14:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Karawani H, Jenkins KA, Anderson S. Neural and behavioral changes after the use of hearing aids. Clin Neurophysiol. 2018;129(6):1254–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kowalewski V, Patterson R, Hartos J, Bugnariu N. Hearing loss contributes to balance difficulties in both younger and older adults. J Prev Med. 2018;3(2):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ibrahim I, da Silva SD, Segal B, Zeitouni A. Postural stability: assessment of auditory input in normal hearing individuals and hearing aid users. Hear Bal Commun. 2019;17(4):280–7. [Google Scholar]
- 45. McDaniel DM, Motts SD, Neeley RA. Effects of bilateral hearing aid use on balance in experienced adult hearing aid users. Am J Audiol. 2018;27(1):121–5. [DOI] [PubMed] [Google Scholar]
- 46. Ninomiya C, Hiraumi H, Yonemoto K, Sato H. Effect of hearing aids on body balance function in non-reverberant condition: a posturographic study. PLoS One. 2021;16(10):e0258590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Rumalla K, Karim AM, Hullar TE. The effect of hearing aids on postural stability. Laryngoscope. 2015;125(3):720–3. [DOI] [PubMed] [Google Scholar]
- 48. Negahban H, Bavarsad Cheshmeh Ali M, Nassadj G. Effect of hearing aids on static balance function in elderly with hearing loss. Gait Posture. 2017;58:126–9. [DOI] [PubMed] [Google Scholar]
- 49. Criter RE, Gustavson M. Subjective hearing difficulty and fall risk. Am J Audiol. 2020;29(3):384–90. [DOI] [PubMed] [Google Scholar]
- 50. Vitkovic J, Le C, Lee SL, Clark RA. The contribution of hearing and hearing loss to balance control. Audiol Neurootol. 2016;21(4):195–202. [DOI] [PubMed] [Google Scholar]
- 51. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Rechberger V, Biberschick M, Porthun J. Effectiveness of an osteopathic treatment on the autonomic nervous system: a systematic review of the literature. Eur J Med Res. 2019;24(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article. Further inquiries can be directed to the corresponding author.