Abstract
Study objective:
To characterize the demographic, clinical, and epidemiologic features of levamisole-associated neutropenia in cocaine or heroin users.
Methods:
State health departments were recruited for participation when the Centers for Disease Control and Prevention (CDC) was notified of potential cases by a clinician, a health department official, or a poison center between October 15, 2009, and May 31, 2010. A case was defined as a person with an absolute neutrophil count less than 1,000 cells/μL (or a WBC count <2,000 cells/μL) and a self-reported history or laboratory confirmation of cocaine or heroin use. Health department officials abstracted data from medical charts, attempted a patient interview, and submitted data to CDC for descriptive analysis.
Results:
Of the 46 potential cases reported from 6 states, half met eligibility criteria and had medical chart abstractions completed (n=23; 50%). Of these, close to half of the patients were interviewed (n=10; 43%). The average age was 44.4 years; just over half were men (n=12; 52%). The majority of patients presented to emergency departments (n=19; 83%). More than half presented with infectious illnesses (n=12; 52%), and nearly half reported active skin lesions (n=10; 44%). The majority of interview respondents used cocaine greater than 2 to 3 times a week (n=9; 90%), used cocaine more than 2 years (n=6; 60%), and preferred crack cocaine (n=6; 60%). All were unaware of exposure to levamisole through cocaine and of levamisole’s inherent toxicity (n=10; 100%).
Conclusion:
Physicians should suspect levamisole exposure in patients using illicit drugs, cocaine in particular, who present with unexplained neutropenia. Most patients reported chronic cocaine use and were unaware of levamisole exposure. Cocaine use is more prevalent among men; however, our results identified a higher-than-expected proportion of female users with neutropenia, suggesting women may be at higher risk. Emergency physicians and practitioners are uniquely positioned to recognize these patients early during their hospital course, elucidate a history of cocaine or other drug exposure, and optimize the likelihood of confirming exposure by arranging for appropriate drug testing.
INTRODUCTION
Background
As of July 2009, 69% or more of cocaine and 3% of heroin seized by the US Drug Enforcement Administration before arriving in the United States contained levamisole.1 Levamisole was historically used in humans as an immunomodulator for conditions such as rheumatoid arthritis, an adjunct chemotherapy agent, and an anthelmintic pharmaceutical. Human use was restricted in the United States in 2000 when an association between levamisole and agranulocytosis was discovered. Adverse health effects reported from oral levamisole include agranulocytosis, cutaneous vasculitis, and leukoencephalopathy.2,3 Today, the only Food and Drug Administration–approved use of levamisole is in livestock as an antiparasitic agent.2,4,5 However, levamisole is still used in humans outside the United States for various reasons.
Several case reports from the last few years describe patients who developed conditions such as neutropenia, agranulocytosis, and vasculitis after using cocaine that was either known or suspected to be contaminated with levamisole.6–9 Agranulocytosis and neutropenia are generally not caused by cocaine; however, these conditions have been associated with oral levamisole exposure.10 Why levamisole is added to cocaine is unknown. Proposed theories include to increase bulk, to enhance stimulatory effects; and to monitor supply, distribution, and sources of origin by the manufacturers of illicit drugs.5,11
The New Mexico Department of Health identified a cluster of unexplained agranulocytosis cases in cocaine users in early 2008. During the next year, additional cases of unexplained agranulocytosis in cocaine users were identified in other states.7 The US Substance Abuse and Mental Health Services Administration distributed a written alert to its stakeholders in September 2009, warning them of this public health issue. In October, after several state health departments reported cases of neutropenia or agranulocytosis in the setting of cocaine use,7 the National Center for Environmental Health of the Centers for Disease Control and Prevention (CDC) initiated multistate passive surveillance for these cases. Our objective was to characterize the epidemiologic and clinical features of patients presenting with neutropenia after exposure to cocaine or heroin potentially contaminated with levamisole.
MATERIALS AND METHODS
For the purpose of surveillance, a probable case was defined as any consenting patient older than 18 years and with (1) moderate to severe neutropenia defined as an absolute neutrophil count less than 1,000 cells/μL of blood without other obvious cause or WBC count less than 2,000 cells/μL of blood without other obvious cause; and (2) cocaine use in the past month according to self-report or detection of metabolites in blood or urine or heroin use in the past month according to self-report. A confirmed case met both of above criteria and also had laboratory confirmation of levamisole in urine according to gas chromatography mass spectroscopy (Figure).
Figure.
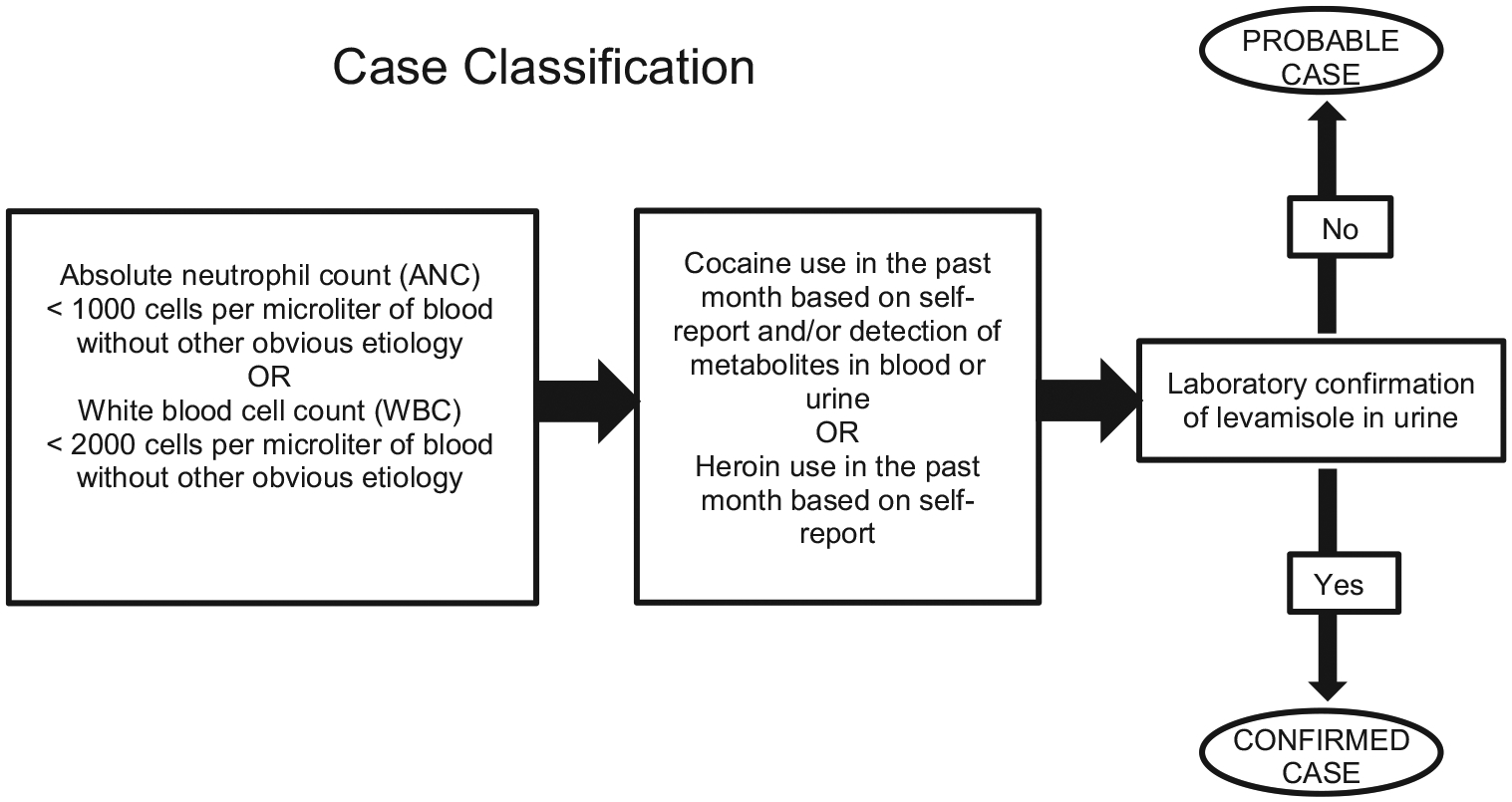
Flow chart describing probable and confirmed case classification.
In the aforementioned alert released by the Substance Abuse and Mental Health Services Administration and a Morbidity and Mortality Weekly Report article on the cluster of cases in New Mexico,7 clinicians and public health officials were asked to report potential cases to CDC.
Case identification was completed in one of 3 ways during the surveillance period (October 15, 2009—May 31, 2010). First, cases were identified by surveillance of the National Poison Data System, which is the national poison center reporting database for the 57 US poison centers and is managed by the American Association of Poison Centers.12 CDC collaborates with the American Association of Poison Centers to perform routine and event-specific surveillance for public health issues, using the National Poison Data System. During the study period, CDC monitored the National Poison Data System for reported cocaine exposures presenting with cytopenia. CDC and the American Association of Poison Centers then contacted the poison center where any such call originated during the study period and advised them to report the details of the call to their state health department for an eligibility determination. If the state was not already participating in surveillance, then CDC also contacted the state health department to inform them about this project and invite them to participate.
Second, a recent article on this topic7 encouraged clinicians to contact CDC with possible cases. Those clinicians were then referred to their state health department; CDC also contacted the health department to notify them of this issue and encourage participation in this study.
Third, participating states released their own health alert notice encouraging clinicians to report cases to their local or state health department. These alerts were distributed by state-specific press release and professional association e-mail lists.
A state or local health department representative contacted the reporting clinician after notification of a patient potentially fitting the case definition. After a possible case was reported by a clinician, a state health department representative confirmed eligibility, reviewed the medical record if available, and completed a data abstraction form to capture available demographic, exposure (within the last 30 days), health, sign and symptom, outcome, and laboratory testing result data. A patient interview was administered to available and willing participants by the state health department representative. This was used to collect additional information not captured by the data abstraction form about the patient’s demographics, medical history, history with drugs and alcohol, most recent experience with cocaine or heroin, and knowledge about levamisole. After receipt of medical record abstraction and interview forms, we reviewed available medication lists for all cases to ensure that there was no other obvious drug exposure that could have caused the neutropenia.13 Available medication lists were reviewed and patients were excluded if they were exposed to a drug that was associated with an increased risk of acute agranulocytosis in multiple observational studies.13
Primary Data Analysis
A descriptive analysis with SPSS (version 19.0; SPSS, Inc., Chicago, IL) was performed to provide basic information on case identification and how CDC, poison centers, and state health departments were notified for all possible cases. A detailed descriptive analysis (ie, counts and percentages) was then performed to characterize the epidemiologic, clinical, exposure, behavioral, and laboratory testing features of probable and confirmed cases.
RESULTS
A total of 46 possible cases were identified from the aforementioned processes and reported to CDC. Surveillance through the National Poison Data System identified 25 reported cocaine exposures with cytopenia from 12 states. CDC was directly contacted by 10 clinicians about 16 potential cases, and 5 other potential cases were reported directly to a state health department, which then notified CDC. Poison centers were typically notified by emergency physicians and other treating physicians and not by calls from the patients themselves. From this information, 15 state health departments were ultimately contacted to participate. Eight states agreed to participate, including California, Florida, Maine, Massachusetts, Michigan, Minnesota, New Mexico, and Vermont. Forty-one data abstraction forms were received by CDC; no information beyond the initial verbal report was received for 5 possible cases. Eighteen patients were excluded from the analysis because cocaine or heroin exposure was not documented (n=11), the patient’s absolute neutrophil count was greater than 1,000 cells/μL or WBC was greater than 2,000 cells/μL (n=5), or the patient had concurrent exposure to 1 or more drugs associated with neutropenia (n=2). One patient had a questionable recent exposure to prednisone, which was on the list used for exclusion13; however, we elected not to exclude this case primarily because the reference cited for this drug deemed the association unexplainable and likely “noncausal.”14 Of the remaining 23 cases, only 1 could be confirmed through urinalysis for levamisole, thereby leaving 22 classified as probable. Among the 23 probable and confirmed cases, 12 were from Michigan, 10 from New Mexico, and 1 from Minnesota. State health departments were largely notified of cases through their close working relationships with poison centers (n=16; 70% of potential or confirmed cases), directly by emergency physicians (n=2; 9%), a hospital infection control practitioner (n=2; 9%), and other hospital officials (n=3; 13%). Ten probable cases also completed interviews administered by local or state health department representatives.
The average age among the 23 probable and confirmed cases was 44.4 years (range 27 to 64 years), and slightly more than half were men (n=12; 52%). Of the 20 cases reporting race, 44% were black (n=10), followed by 30% white (n=7) and 13% American Indian or Alaskan Native (n=3). Five patients (22%) were Hispanic (Table).
Table.
Demographics, preferred form of cocaine and route of transmission, and concurrent conditions for confirmed and probable cases of neutropenia after cocaine use.
| Characteristic | Count | Percentage |
|---|---|---|
| Sex | ||
| Male | 12 | 52 |
| Female | 11 | 48 |
| Race | ||
| American Indian/Alaskan Native | 3 | 13 |
| Black | 10 | 44 |
| White | 7 | 30 |
| Unknown | 3 | 13 |
| Ethnicity | ||
| Hispanic/Latino | 5 | 22 |
| Not Hispanic/Latino | 15 | 65 |
| Unknown | 3 | 13 |
| Form of cocaine (recent use) | ||
| Crack | 12 | 52 |
| Powder | 1 | 4 |
| No cocaine* | 1 | 4 |
| Unknown | 9 | 39 |
| Mode of cocaine (recent use) | ||
| Smoke | 12 | 52 |
| Inject | 1 | 4 |
| Snort | 1 | 4 |
| No cocaine* | 1 | 4 |
| Unknown | 8 | 35 |
| Concurrent condition | ||
| Hepatitis C | 12 | 52 |
| HIV | 4 | 17 |
| High blood pressure | 4 | 17 |
| Diabetes | 4 | 17 |
| Asthma/chronic obstructive pulmonary disease | 2 | 9 |
| Cirrhosis | 2 | 9 |
| Vasculitis | 1 | 4 |
| Lupus | 1 | 4 |
| Cryoglobulinemia | 1 | 4 |
| Anemia | 1 | 4 |
| Esophageal varices | 1 | 4 |
| Pancreatitis | 1 | 4 |
One patient reported using only heroin.
Most cases presented to the ED (n=19, 83%), 1 presented to a primary care physician, and 1 presented to a cancer center; the remaining 2 presented to other hospital departments (not reported). The most commonly presenting chief complaint involved signs or symptoms indicating infectious disease (n=12; 52%) such as fever, sore throat, body aches, cellulitis or abscess, and neutropenia. Other complaints included chest pain (n=4; 17%), pain (n=2; 9%), altered mental status (n=2; 9%), generalized weakness (n=1; 4%), and alcohol intoxication (n=1; 4%). Frequency distributions for comorbidities among cases are listed in the Table. Half of the patients (n=12; 52%) had a history of hepatitis C. Other comorbidities included HIV (n=4; 17%) and diabetes (n=4; 16%).
Most cases reported exposure to only cocaine in the last 30 days (n=19; 83%). The others included cocaine and heroin exposure (n=2; 9%) and only heroin (n=1; 4%) exposure within the last 30 days. The majority of cases reported that their last cocaine exposure before hospital evaluation was through smoking (n=12; 52%), and crack was the most common form of cocaine reportedly used (n=12; 52%). Almost a third (n=7; 30%) of the 23 cases indicated at least 1 previous episode of neutropenia in the past 12 months. Of these 7, 3 reported 2 previous episodes (43%), 3 reported 1 previous episode (43%), and 1 reported 5 previous episodes (14%). One of these previous episodes was captured by this surveillance effort. Nearly half reported active skin lesions during the current episode of neutropenia (n=10; 44%), and several described the lesions as necrotic or ulcerative (n=5; 22%).
All cases had an absolute neutrophil count less than 1,000 cells/μL (n=22; 96%), except that 1 case was unknown or unrecorded, and most had a WBC count of less than 2,000 cells/μL (n=13; 57%). More than half had an absolute neutrophil count of less than 500 cells/μL (n=15; 65%), most were cocaine positive by urine testing (n=14; 61%), and almost a third were opiate positive (n=7; 30%). Of the 4 patients who submitted a urine sample for levamisole screening, only 1 tested positive for levamisole by gas chromatography mass spectroscopy.
Nearly half were admitted to the hospital (n=11; 48%), with 3 of those admitted to the ICU (n=3; 13%). A small number left the ED against medical advice (n=5; 22%), and a few were treated and discharged from the ED (n=3; 13%) or transferred to the psychiatric ward for attempted self-harm or schizophrenia (n=2; 8%). There was 1 death (4%). No cases were reportedly referred for substance abuse treatment.
Five cases (22%) received filgrastim to stimulate the production of neutrophils. Of these, 4 received more than 1 dose (n=4; 80%). Eight (35%) received hematologic consultation and 7 (30%) received a bone marrow aspiration to elucidate the origin of the neutropenia.
More than one third of all cases completed a standardized interview (n=10; 40%). The most commonly reported route of cocaine exposure was smoking (n=7; 70%), and the most common form was crack (n=6; 60%). The 1 confirmed case reported smoking of crack as his typical route of exposure and form of cocaine. Of cases interviewed, 2 (20%) reported using less than 1 g of cocaine daily and almost one third reported using greater than 1 g daily, with a range of 2 to 4 g (n=3; 33%). One patient reported using “5 dime-bags per day” and 4 (40%) reported no typical pattern or were not able to characterize their daily cocaine use. Half of the interviewed cases (n=5; 50%) reported using cocaine for greater than 10 years, 3 of them (30%) from 1 to 5 years. Most self-identified themselves as “sporadic” users, claiming that there was no regular pattern to their cocaine use (n=7; 70%). The majority (n=9; 90%) claimed to use cocaine greater than 2 to 3 times a week.
More than half of the interviewed cases (n=6; 60%) claimed that during the past 5 years, they usually bought their cocaine from the same supplier. None reported changing the type, brand, or street name of the cocaine they had been using. Half (n=5; 50%) reported that their latest batch of cocaine (before treatment for neutropenia) had a different taste from typical, describing it as a gasoline taste or other unappealing taste. Most interviewed cases (n=6; 60%) denied any change in the usual smell of the cocaine. More than half said the “high” from their latest batch was different than usual (n=6; 60%) and the remainder (n=4; 40%) claimed there was no difference. A fifth (n=2; 20%) claimed it was better or more intense than usual. Only 1 interviewed case (10%) claimed that the cocaine had any adverse effects, which, when described, were nonspecific. Most (n=6; 60%) reported sharing either the cocaine or drug paraphernalia with others, but only 1 reported that others developed any sort of similar illness (reported to be hives).
None of the interviewed cases reported knowing or being told their cocaine might contain levamisole. Only 1 had heard that levamisole was being used as a cocaine contaminant. Two (20%) reported that their cocaine dealer claimed there was “something special” about the last batch of cocaine purchased, but the claims were nonspecific. Only 1 patient (10%) reported that the cocaine had a special name. The majority reported that the cocaine was the usual price (n=8; 80%), whereas the rest said it was more expensive (n=2; 20%).
More than two thirds of interviewed cases claimed to have also smoked marijuana (n=7; 70%) recently and 2 had used alcohol lately (n=2; 20%). Half claimed to have used tobacco products daily (n=5; 50%). No other drugs were reportedly used within the last 30 days before treatment for neutropenia by any interviewed case.
LIMITATIONS
Passive surveillance cannot provide estimates of attack rate because cases were likely to be underreported during the surveillance period. The wide variety of case counts among states may reflect competing priorities among states and not necessarily true differences in case number, although cocaine use patterns vary throughout the Unites States.
Fourteen (61%) of the cases tested positive for hepatitis C, HIV, or both. Approximately 70% to 90% of habitual intravenous drug users have hepatitis C.15 Additionally, several studies have linked the use of drugs, particularly cocaine, and the risky behaviors associated with drug use (such as intravenous injection and unprotected sexual intercourse) with HIV infection.16,17 Both hepatitis C treatment and HIV have been associated with neutropenia. PEGylated interferon treatment used to suppress the hepatitis C virus can cause immunosuppression leading to neutropenia.18 We reviewed medication lists at presentation to the ED, and no patients reported currently receiving PEGylated interferon. HIV is a progressive disease affecting the body’s immune system. Therefore, neutropenia is a common occurrence in HIV-infected patients that can be caused by the HIV virus itself and/or from acquired related infections and malignancies.19 Cocaine further increases the risk for developing neutropenia because it has been shown to accelerate the replication of HIV.20,21 Thus, the neutropenia observed in the 4 HIV-infected cases may have had multiple contributing sources working independently or synergistically. Nine (39%) of the identified patients with neutropenia did not report having HIV or hepatitis C. The only commonality among them was the use of cocaine.
Our low yield for levamisole-positive urine samples (n=1) is a significant limitation. However, it can be explained by levamisole’s relatively short half-life and rapid clearance from the body.8 It is likely that at least some of the negative test results simply reflected that most levamisole had been eliminated from the body when sample collection occurred. Few laboratories have the capacity to screen urine for levamisole, and some samples had to be transported to other state laboratories, which might have contributed to negative results. During the surveillance period, some samples were used to develop a replicable urinary assay for levamisole for public health laboratories without a method, and this method is now published.22 Although most of our patients did not have confirmatory testing for levamisole, we believe that this is the most likely explanation for their neutropenia. Exposure to levamisole was suspected in all cases but could be confirmed in only 1.
DISCUSSION
Most of our cases entered the health care system through the ED, and most presented with infection-related health problems. These findings are not particularly surprising, given that chronic drug users use the ED significantly more than casual or nondrug users.23 Drug users may have few health care options available to them other than the ED, and in this study our patients all had moderate or severe neutropenia. Emergency physicians are likely to be the first health care practitioners to see these patients and are uniquely positioned to help elucidate exposure information (history of cocaine use or previous episodes of neutropenia) that may facilitate their subsequent evaluation and management while hospitalized. In addition, urine testing for cocaine metabolites or levamisole is more likely to be detected when the interval between last exposure and sample collection is short. Appropriate testing on urine collected on initial presentation is more likely to find detectable concentrations of levamisole. If a levamisole assay does not exist in the practitioner’s hospital or state health department laboratory, a published method is available for laboratories to follow.22 Any history of exposure to cocaine, especially in conjunction with detection of cocaine or levamisole in patient urine, may be helpful in the decision to forgo unnecessary, uncomfortable, and costly procedures such as bone marrow biopsies during the patient’s hospitalization.
A 2008 Canadian study found that the majority (64%) of their patients with neutropenia caused by levamisole-contaminated cocaine (n=42) were women.24 A more recent study found that among 203 cases of levamisole-associated complications, the majority of patients were women.25 Among the cases with neutropenia as a complication, most patients were also women (personal communication, Alexandre Larocque, MD, Université de Montréal, Montreal, Quebec, Canada, August 10, 2012). These findings are particularly interesting because most cocaine users in Canada, as well as the United States, are men.26,27 If all other variables were equal, one would expect more men to present with levamisole-associated complications such as neutropenia. Our study had an even distribution of neutropenia cases across sexes, which may still represent disproportionately high female representation according to sex patterns and cocaine use.27 When considered together, these findings suggest that women might be at higher risk of developing neutropenia after levamisole-contaminated cocaine use. Further study is needed to verify and explore reasons for this finding.
Our findings suggest that individuals with levamisole-contaminated cocaine-associated neutropenia are unaware of the addition of levamisole to their cocaine, which indicates that levamisole-contaminated cocaine is not being marketed as a unique or different product from other cocaine. In the beginning of this study, we had hoped to identify unique attributes of a levamisole-contaminated cocaine experience, thus suggesting that perhaps levamisole-contaminated cocaine was being marketed to users as a distinctly different cocaine experience. We were unable to identify any such unique attributes. However, such conclusions should be tempered by the fact that users have been exposed chronically to levamisole-contaminated cocaine since 2003, when levamisole was first detected in cocaine,10 and by our small study sample size. Furthermore, the variability in taste, odor, and experience reported by our interviewed patients might be limited by recall bias or an inconsistent drug supply rather than characteristics attributable to levamisole alone. Finally, patients were also generally unaware of the potential serious and life-threatening adverse health effects that can develop from levamisole-contaminated cocaine. Education about the dangerous health effects from exposure to levamisole-contaminated drugs should be incorporated in anti–drug abuse public health messaging. Such messages should include recommendations to seek medical treatment if users experience signs and symptoms of neutropenia such as frequent infections.
Some of our patients were treated with a granulocyte colony-stimulating factor for their neutropenia. Filgrastim is a granulocyte colony-stimulating factor therapy produced by recombinant DNA technology and is used to bolster the immune system in patients with immunosuppression from various conditions, such as postchemotherapy, myelodysplastic syndromes, and autoimmune disorders. Filgrastim selectively binds to hematopoietic stem cells, inducing proliferation and differentiation of the respective stem cells into granulocytes such as neutrophils and monocytes. Filgrastim and the costs of hospitalization can make treatment for levamisole-contaminated cocaine-induced neutropenia expensive. Therefore, not only can the levamisole-contaminated cocaine-induced health effects (ie, neutropenia, vasculitis) result in substantial morbidity and rarely mortality but also they can represent a significant cost for the patient and health care system. Although patients might recover from their neutropenia without granulocyte colony-stimulating factor therapy, practitioners who choose to use this therapy when faced with levamisole-associated neutropenia should be aware that evidence of clinical benefit is lacking.
Finally, the majority of our patients reported using only cocaine and not heroin, which supports current literature suggesting that cocaine is the predominant source for levamisole exposure in the United States compared with heroin. However, our findings, in conjunction with the detection of levamisole in heroin by the Drug Enforcement Administration,1 indicate that other illicit drug sources such as levamisole-contaminated heroin should be considered in the setting of unexplained neutropenia, agranulocytosis, and other known adverse health effects from levamisole.
Given the serious health effects associated with levamisole, the substantial associated health care costs, and the large number of people using cocaine in the United States (nearly 2 million people), levamisole-contaminated cocaine is an important emerging public health problem. Emergency physicians and practitioners are uniquely positioned to recognize these patients early during their hospital course, elucidate a history of cocaine (or other drug) exposure, and confirm exposure by collecting and sending urine specimens for cocaine and possibly levamisole testing. All of this information may subsequently facilitate decisionmaking with regard to optimization of patient management.
Editor’s Capsule Summary.
What is already known on this topic
Neutropenia and skin necrosis have emerged as a new complication of drug abuse presumably related to the cutting agent levamisole.
What question this study addressed
To characterize the demographic, clinical, and epidemiologic features of levamisole-associated neutropenia in a sample of illicit drug users.
What this study adds to our knowledge
Most patients in this 23-patient case series presented to an emergency department with infectious illnesses, and many reported active skin lesions. Most respondents used cocaine greater than 2 to 3 times a week for more than 2 years, preferred crack cocaine, and were unaware of levamisole’s toxicity.
How this is relevant to clinical practice
Emergency providers are uniquely positioned to recognize these patients early, elucidate a history of cocaine or heroin abuse, and potentially confirm exposure.
Funding and support:
By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
The authors acknowledge the contribution of the American Association of Poison Control Centers in case finding and data collection, as well as Kelly Gallagher, PhD, and Joan Baumbach, MD, of the New Mexico Department of Health in case finding and case review, and Amy Wolkin, MSPH, and Lauren Lewis, MD (National Center for Environmental Health, Centers for Disease Control and Prevention), for review of the protocol and article.
Footnotes
A podcast for this article is available at www.annemergmed.com.
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the Centers for Disease Control and Prevention or the institutions with which the authors are affiliated.
REFERENCES
- 1.Casale JF, Cobreil EM, Hays PA. Identification of levamisole impurities found in illicit cocaine exhibits. DEA Microgram. July-December 2008. Available at: http://www.usdoj.gov/dea/programs/forensicsci/microgram/journal_v6_num34/pg3.html. Accessed July 19, 2012. [Google Scholar]
- 2.Levamisole [package insert]. DRUGDEX. Greenwood Village, CO: Thomson Healthcare, 2012. [Google Scholar]
- 3.Waller JM, Feramisco JD, Alberta-Wszolek L, et al. Cocaine associated retiform purpura and neutropenia: is levamisole the culprit? J Am Acad Dermatol. 2010;63:530–535. [DOI] [PubMed] [Google Scholar]
- 4.Zhu NY, Legatt, DF, Turner AR. Agranulocytosis after consumption of cocaine adulterated with levamisole. Ann Intern Med. 2009; 150:287–289. [DOI] [PubMed] [Google Scholar]
- 5.Bradford M, Rosenberg B, Moreno J, et al. Bilateral necrosis of earlobes and cheeks: another complication of cocaine contaminated with levamisole. Ann Intern Med. 2010;152:758–759. [DOI] [PubMed] [Google Scholar]
- 6.Farhat EK, Muirhead TT, Chaffins ML, et al. Levamisole-induced cutaneous necrosis mimicking coagulopathy. Arch Dermatol. 2010;146:1320–1321. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC). Agranulocytosis associated with cocaine use—four States, March 2008–November 2009. MMWR Morb Mortal Wkly Rep. 2009;58: 1381–1385. [PubMed] [Google Scholar]
- 8.Kouassi E, Caille G, Lery L, et al. Novel assay and pharmacokinetics of levamisole and p-hydroxylevamisole in human plasma and urine. Biopharm Drug Dispos. 1986;7:71–89. [DOI] [PubMed] [Google Scholar]
- 9.Buchanan J Prevalence of levamisole in urine toxicology screens positive for cocaine in an inner-city hospital. JAMA. 2011;305: 1657–1658. [DOI] [PubMed] [Google Scholar]
- 10.Valentino AM, Fuentecilla K. Levamisole: an analytical profile. Microgram J. 2005;3:134–137. [Google Scholar]
- 11.Chang A, Osterloh J, Thomas J. Levamisole: a dangerous new cocaine adulterant. Clin Pharmacol Ther. 2010;88:408–411. [DOI] [PubMed] [Google Scholar]
- 12.Bronstein AC, Spyker DA, Cantilena JR, et al. 2010 Annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 28th annual report. Clin Toxicol. 2011;49:910–941. [DOI] [PubMed] [Google Scholar]
- 13.Andersohn F, Konzen C, Edeltraut G. Systematic review: agranulocytosis induced by nonchemotherapy drugs. Ann Intern Med. 2007;146:657–665. [DOI] [PubMed] [Google Scholar]
- 14.van der Klauw MM, Gousmit R, Halie MR, et al. A population-based case-cohort study of drug-associated agranulocytosis. Arch Intern Med. 1999;159:369–374. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Hepatitis C FAQs for health professionals. 2011. Available at: http://www.cdc.gov/hepatitis/HCV/HCVfaq.htm. Accessed July 19, 2012.
- 16.de Carvalho HB, Seibel SD. Crack cocaine use and its relationship with violence and HIV. Clinics (Sao Paulo). 2009;64: 857–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Larrat EP, Zierler S. Entangled epidemics: cocaine use and HIV disease. J Psychoactive Drugs. 1993;25:207–220. [DOI] [PubMed] [Google Scholar]
- 18.Tandon P, Doucette K, Fassbender K, et al. Granulocyte colony-stimulating factor for hepatitis C therapy-associated neutropenia: systematic review and economic evaluation. J Viral Hepat. 2011; 18:e381–393. [DOI] [PubMed] [Google Scholar]
- 19.Jaresko GS. Etiology of neutropenia in HIV-infected patients. Am J Health Syst Pharm. 1999;56(suppl 5):S5–S8. [DOI] [PubMed] [Google Scholar]
- 20.Roth MD, Tashkin DP, Choi R, et al. Cocaine enhances human immunodeficiency virus replication in a model of severe combined immunodeficient mice implanted with human peripheral blood leukocytes. J Infect Dis. 2002;185:701–705. [DOI] [PubMed] [Google Scholar]
- 21.Roth MD, Whittaker KM, Choi R, et al. Cocaine and σ−1 receptors modulate HIV infection, chemokine receptors, and the HPA axis in the huPBL-SCID model. J Leukoc Biol. 2005; 78:1198–1203. [DOI] [PubMed] [Google Scholar]
- 22.Trehy ML, Brown DJ, Woodruff JT, et al. Determination of levamisole in urine by gas chromatography–mass spectrometry. J Anal Toxicol. 2011;35:545–550. [DOI] [PubMed] [Google Scholar]
- 23.McGeary KA, French MT. Illicit drug use and emergency room utilization. Health Serv Res. 2000;35(1 pt 1):153–169. [PMC free article] [PubMed] [Google Scholar]
- 24.Knowles L, Buxton JA, Skuridina N, et al. Levamisole tainted cocaine causing severe neutropenia in Alberta and British Columbia. Harm Reduct J. 2009;6:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Larocque A, Hoffman RS. Levamisole in cocaine: unexpected news from an old acquaintance. Clin Toxicol. 2012;50:453. [DOI] [PubMed] [Google Scholar]
- 26.Focus on gender—a national survey of Canadians’ use of alcohol and other drugs–Canadian Addiction Survey (CAS). Health Canada; 2008. Available at: http://www.hc-sc.gc.ca/hc-ps/pubs/adp-apd/cas_gender-etc_sexe/index-eng.php. Accessed July 19, 2012. [Google Scholar]
- 27.Substance Abuse and Mental Health Services Administration. Results From the 2010 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse & Mental Health Services Administration; 2011. NSDUH Series H-41, HHS Publication No. (SMA) 11–4658. [Google Scholar]


