Abstract
Increasing participation in Medicaid among eligible individuals is critical for improving access to care among low-income populations. The administrative burdens of enrolling and renewing eligibility are a major barrier to participation. To reduce these burdens, the Affordable Care Act required states to adopt automated renewal processes that use available databases to verify ongoing eligibility. By 2019, nearly all states adopted automated renewals, but little is known about how this policy affected Medicaid participation rates. Using the 2015–2019 American Community Survey, we found that participation rates among nondisabled, nonelderly adults and children varied widely by state, with an average of 70.8% and 90.7%, respectively. Among Medicaid-eligible adults, participation was lower among younger adults, males, unmarried individuals, childless households, and those living in non-expansion states compared with their counterparts. State adoption of automated renewals varied over time, but participation rates were not associated with adoption. This finding could reflect limitations to current automated renewal processes or barriers to participation outside of the eligibility renewal process, which will be important to address as additional states expand Medicaid and pandemic-era protections on enrollment expire.
Keywords: Medicaid, administrative barriers, program participation
Introduction
Many more people are eligible for public programs than participate in them. This is a particular concern among programs that serve low-income Americans, including Medicaid.1 Prior evidence finds that participation in, or take-up of, Medicaid varies widely across states and eligibility categories, with eligible children being more likely to enroll than parents and childless adults, and higher participation rates in Medicaid expansion vs non-expansion states and in states with more generous Medicaid benefits.2-4
In Medicaid, many enrolled individuals lose coverage over time, with 14%–24% of adult enrollees facing a disruption in coverage each year.5-8 Coverage losses pose a risk that individuals may not re-enroll in Medicaid, even if they are eligible, given the administrative burdens that individuals face to both enrolling and maintaining enrollment in coverage.1 Discontinuity in Medicaid coverage has been associated with delayed and foregone preventive care, increased emergency department utilization, and worsened medication adherence.9,10 While coverage losses may occur because of fluctuations in an enrollee's eligibility, others are due to unsuccessful eligibility renewals. Under the Affordable Care Act (ACA), eligibility redeterminations for individuals qualifying solely on the basis of Modified Adjusted Gross Income (MAGI)—which include nondisabled, nonelderly adults, parents, and people who are pregnant—are conducted every 12 months and involve a verification of current income and residency. In an effort to streamline Medicaid eligibility renewals, the ACA required states to adopt a new process for these eligibility renewals—called automated or ex parte renewals.
In performing automated renewals, states attempt to verify that an enrollee's income remains within the state-specific threshold for their category of Medicaid eligibility using linkages with other databases containing income information, such as state tax and wage data, Social Security data, and information from other public programs.11 If this verification is successful, the enrollee receives notification of their ongoing enrollment. If verification is unsuccessful—for example, if income information is missing or if available information suggests an enrollee's income makes them ineligible—the state requests additional information from the enrollee in order to maintain coverage. While this process was required for most Medicaid enrollees starting in 2014 as part of the ACA,12 many states did not immediately adopt it, and those that have implemented it vary in the percentage of renewals that are successfully processed using the automated process.13-18
The effects of the automated renewal process on participation in the Medicaid program are unknown, although a cross-sectional evaluation of automated renewals suggested they may improve continuity of coverage.19 In addition, reducing administrative barriers in Medicaid—such as eliminating re-enrollment waiting periods, creating online enrollment and renewal interfaces, and reducing the frequency of renewals—has been shown to increase enrollment among low-income people.20 A fuller understanding of the effects of the automated renewal process is especially timely, as the Biden administration has signaled a priority to reduce administrative burdens in government programs21 and plans to expand the automated renewal process to all Medicaid beneficiaries.22 In addition, states have relied on the automated renewal process to redetermine eligibility for a sizable backlog of enrollees during the unwinding of the Public Health Emergency's (PHE’s) Medicaid continuous coverage provision.
We used nationally representative survey data prior to the COVID-19 pandemic to characterize Medicaid participation and evaluate the association between state implementation of automated renewals and Medicaid participation rates for adults and children living in expansion and non-expansion states. Using pre-pandemic data allows us to understand the association between automated renewals and participation during a period of relatively more stable Medicaid enrollment that is more reflective of the post-unwinding policy environment. We hypothesized that adopting automated renewals would increase Medicaid participation.
Data and methods
Data and study sample
We used publicly available, individual-level data from the American Community Survey (ACS) from 2015 to 2019 to capture annual health insurance enrollment status and other sociodemographic data, including household income and composition, state of residence, race/ethnicity, and education, which we used to estimate eligibility for Medicaid. We linked these individual-level data on participation with state-level information in each year on whether a state performed automated renewals and the percentage of all completed Medicaid eligibility renewals performed via the automated process. These data were taken from annual surveys conducted by the Kaiser Family Foundation (KFF) on Medicaid eligibility and enrollment policies and practices.13-18
The study population includes those likely eligible for Medicaid. We identified this group based on whether a respondent's household income in a given year was below their state's Medicaid/Children’s Health Insurance Program (/CHIP) income eligibility threshold for their household size and most likely category of eligibility (ie, child, parent, or childless adult). Tables S1–S3 show state income eligibility thresholds for each year in our study. Because the ACS does not include detailed immigration status, we limited our analysis to US citizens. The automated renewal policy was applied only to those whose Medicaid eligibility is determined using MAGI rules, which does not include disabled people and those 65 years and older; we excluded disabled individuals from our analysis based on self-report of receiving Supplemental Security Income.4
We used variables derived from IPUMS for defining the health insurance unit, which is designed to model the household for the purposes of eligibility for health insurance programs, including Medicaid.23 Health insurance status is collected by self-report at the time of the interview and applies to the entire survey year; respondents may report multiple sources of health insurance. Following the approach used in prior studies estimating participation using ACS data, we excluded individuals reporting other health insurance coverage and those reporting Medicaid without a known pathway to eligibility.4
Automated renewals
The KFF survey collects self-reported data from states annually on whether they performed automated renewals and, if so, what percentage of Medicaid eligibility renewals were successfully completed using the automated process (ie, <25%, 25%–50%, 50%–75%, >75%); Table S4 shows how states were classified in each study year. States performing automated renewals are intended to attempt renewal via the automated process for all MAGI-eligible enrollees. The primary analyses used a binary exposure definition of whether a state reported performing any vs no automated renewals in a given year. In sensitivity analyses, alternative specifications of the exposure were examined, including categories corresponding to the percentage of renewals successfully completed via automated renewals and a binary variable for whether states successfully completed less than or greater than or equal to 50% of renewals via the automated process.
Analysis
Our outcome of interest was Medicaid participation, defined as whether respondents we estimated to be Medicaid-eligible reported having Medicaid coverage in the ACS. We first examined unadjusted Medicaid participation rates across several individual sociodemographic and state characteristics and over time. Next, we examined the relationship between state adult and child Medicaid participation rates graphically and calculated a Pearson correlation coefficient. We also examined the percentage of states overall and by expansion status that adopted automated renewals and their reported success rates in each year, 2015–2019.
To assess the association between the implementation of automated renewals and Medicaid participation, we examined state participation rates by category of automated renewal success in 2015 and 2019, including the median and interquartile range of participation. We also examined the unadjusted participation rates by state for each state that newly adopted automated renewals during the study period compared with states that used or did not use automated renewals in all years of the study period.
Last, we conducted a repeat cross-sectional analysis to assess the association between the likelihood of Medicaid participation and the use of automated renewals at the state level using data from 2015–2019; our regression equation is available in the Supplementary material. The main analyses used linear probability models that included a binary, annually updated indicator for whether a state performed automated renewals in each year and state fixed effects to assess the within-state association between adoption of automated renewals and participation. Fourteen states newly adopted automated renewals during the study period, of which 9 adopted the policy in 2016.
The multivariable models were also adjusted for individual sociodemographic factors and state Medicaid program characteristics. Individual characteristics included age, gender, race/ethnicity, education, marital status, income, employment status, food stamp receipt, and rurality of residence. State characteristics included Medicaid expansion status and an index of Medicaid administrative burden; whether a state performed automated renewals was not included in the index.24 For children, parental education and employment status were used. We also included an interaction term between a state's automated renewal status and whether an individual reported receiving food stamp benefits, given that food stamp data may be used in verifying a Medicaid enrollee's income. Pregnancy status is not recorded in the ACS, so the models included an interaction between age group and gender. More detail on how the regression variables were defined is available in the Supplementary material. The models also adjusted for state fixed effects to assess within-state changes in participation with changes in automated renewal status over time, and calendar-year indicators to account for secular trends. Standard errors were clustered at the state level and all analyses were adjusted for person-level survey weights.
Because participation rates are generally higher for children relative to adults and because many states have continuous coverage provisions that apply to children and not adults, analyses were stratified for those 18 years and younger vs 19 years and above. We also stratified models between states that expanded and did not expand Medicaid to assess whether the association between automated renewal implementation and participation rates varied by expansion status. Expansion status was updated annually and was classified as of January 1 each year. In a sensitivity analysis, we also stratified our analysis by states whose Medicaid expansion status did not change during the study period. All analyses were performed using StataMP version 14 (StataCorp, College Station, TX).
Limitations
This study has several limitations. First, estimates of Medicaid eligibility and enrollment in the ACS could have errors, as states evaluate eligibility based on monthly income and the ACS collects annual household income measured at a single point in time. Insurance status, income, and household composition are all self-reported and could be subject to error. We were unable to directly evaluate some characteristics (eg, pregnancy, immigration status, etc) that affect Medicaid eligibility, and our estimates are limited to US citizens. In addition, 13 states have at least 1 year in which they were performing automated renewals, but the percentage of renewals successfully completed was not reported to KFF.
We were also unable to assess other potentially important outcomes related to automated renewals, like continuity or duration of coverage or the enrollee's experience with renewals, such as time spent on renewal paperwork or stress associated with renewal. Likewise, while we adjusted for a number of potential confounders at the individual and state levels, we did not use a quasi-experimental approach, such as a difference-in-differences design to assess the causal impact of automated renewals on participation due to limited pre-policy data for most states.
Results
Medicaid participation rates among nondisabled adults and children
Our study included an unweighted 1 039 717 person-years among Medicaid-eligible children and 675 546 person-years among Medicaid-eligible adults from 2015 to 2019, of which 937 649 children (90.2%; 90.8% after survey adjustment) and 478 374 adults (70.8%; 70.8% after survey adjustment) were enrolled in Medicaid (Table 1). National participation rates among adults and children were largely stable during the study period (Figure S1): in 2015, mean survey-adjusted participation was 90.8% among children and 68.9% among adults (Table S5) and, in 2019, participation was 89.6% and 70.0%, respectively (Table S6).
Table 1.
Percentage of Medicaid-eligible children and adults enrolled, by sociodemographic characteristics, 2015–2019.
| Medicaid enrolled, % | ||
|---|---|---|
| Children (n = 1 039 717) | Adults (n = 675 546) | |
| Age | ||
| 0–5 y | 92.8 | — |
| 6–12 y | 91.7 | — |
| 13–18 y | 86.6 | — |
| 19–34 y | — | 69.7 |
| 35–49 y | — | 71.6 |
| 50–64 y | — | 72.5 |
| Sex | ||
| Female | 90.8 | 77.4 |
| Male | 90.6 | 62.9 |
| Race/ethnicity | ||
| White | 89.3 | 70.6 |
| Black | 93.8 | 71.3 |
| AI/AN | 93.1 | 69.6 |
| AAPI | 90.0 | 75.9 |
| Hispanic | 90.2 | 69.7 |
| Socioeconomic characteristics | ||
| <100% FPL | 92.0 | 71.0 |
| ≥100% FPL | 88.2 | 69.8 |
| Food stamp recipient | 96.8 | 85.1 |
| Any parent with Medicaid | 99.8 | — |
| No parent with Medicaid | 84.9 | — |
| Married | — | 75.6 |
| Not married | — | 69.8 |
| Any child in household | — | 79.4 |
| No child in household | — | 66.5 |
| At least 1 parent employed | 90.2 | — |
| No parent employed | 92.1 | — |
| Employed | — | 71.1 |
| Unemployed | — | 70.6 |
| Not in labor force | — | 70.6 |
| Parental education/education | ||
| Less than high school | 87.5 | 69.8 |
| High school graduate | 91.9 | 70.1 |
| Some college or more | 91.4 | 72.3 |
| State features | ||
| Expansion state | 92.8 | 71.6 |
| Non-expansion state | 87.9 | 61.8 |
| Automated renewal success rate | ||
| No automated renewals | 91.6 | 69.4 |
| <25% | 88.4 | 67.5 |
| 25%–50% | 91.7 | 75.3 |
| 50%–75% | 92.3 | 70.9 |
| >75% | 92.7 | 69.9 |
| State Medicaid administrative burden | ||
| Low | 93.0 | 72.4 |
| Medium | 91.3 | 70.7 |
| High | 87.4 | 66.0 |
Abbreviations: AAPI, Asian American/Pacific Islander; AI/AN, American Indian/Alaska Native; CHIP, Children’s Health Insurance Program; FPL, Federal Poverty Level.
Source: Authors’ analysis of data from the American Community Survey, 2015–2019. Numbers (n) presented are unweighted person-years. Values represent proportions of the age 19–64 population enrolled who are estimated to be eligible for Medicaid/CHIP given their household size, income, and state-year of residence. Excludes those with private or other public health insurance. Estimates are adjusted for survey weighting.
Across the study period, Medicaid-eligible adults who were female, married, and had a child residing in the household were more likely to enroll in Medicaid compared with male, unmarried, and childless adults (77.4% vs 62.9%, 75.6% vs 69.8%, and 79.4% vs 66.5%, respectively; Table 1). Participation was higher among older-aged adults (19–34 years: 69.7%; 35–49 years: 71.6%; 50–64 years: 72.5%). There were no large racial differences in participation rates among adults, although adults identifying as Asian American/Pacific Islander (75.9%) had the highest Medicaid participation rates. Children with a parent in Medicaid were more likely to enroll compared with those without a parent in Medicaid (99.8% vs 84.9%; Table 1). For children, participation was higher among younger-age children (0–5 years: 92.8%; 6–12 years: 91.7%; 13–18 years: 86.6%).
Mean participation rates were higher in Medicaid expansion states for adults (71.6%) and children (92.8%) compared with non-expansion states (adult mean: 61.8%; child mean: 87.9%). States with low administrative burden had higher participation than those with high administrative burden, both for adults (72.4% vs 66.0%) and children (93.0% vs 87.4%).
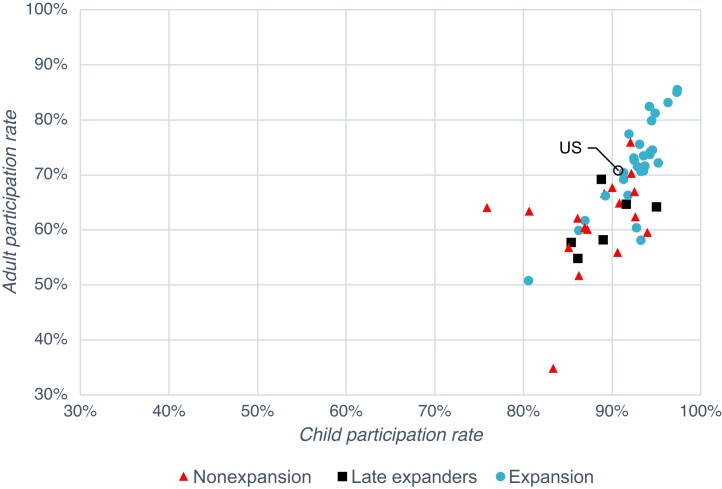
Across the study period, state-level adult and child Medicaid participation rates were correlated (r = 0.69; see Figure 1), although there was wider variation in adult compared with child participation rates. The state with the highest participation among adults, Massachusetts, had an average participation rate of 85.5% compared to 34.8% in the state with the lowest adult participation, Texas. Child participation ranged from 97.4% (Massachusetts) to 75.9% (Utah).
Figure 1.
Adult and child Medicaid participation rates, by state, 2015–2019. Source: Authors’ analysis of data from the American Community Survey, 2015–2019. Participation rates calculated from the proportion reporting Medicaid insurance of those estimated to be for Medicaid/CHIP given their household size, income, and state-year of residence. Excludes those with private or other public health insurance. Abbreviation: CHIP, Children’s Health Insurance Program.
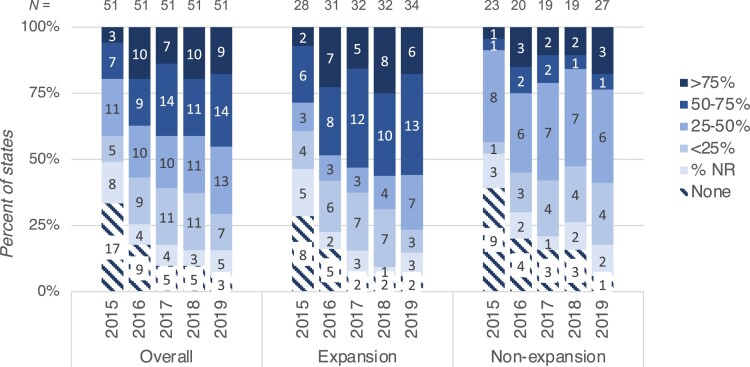
Automated renewals
Over time, more states began processing Medicaid eligibility renewals via an automated mechanism, and states reported performing a greater share of renewals successfully in 2019 compared with 2015 (Figure 2). In 2015, 33.3% (n = 17) of states did not perform automated renewals, compared to 5.9% in 2019 (n = 3). The share of states successfully completing 50%–75% or more than 75% of renewals via an automated mechanism increased from 19.6% in 2015 to 45.1% in 2019. Among expansion states, 28.6% (n = 8) in 2015 and 5.9% (n = 2) in 2019 did not perform automated renewals compared to 39.1% (n = 9) in 2015 and 3.7% (n = 1) in 2019 among non-expansion states. Of expansion states, 28.6% and 55.9% had automated renewal success rates of 50%–75% or more than 75% in 2015 and 2019, respectively, compared with 8.7% and 23.5% of non-expansion states in 2015 and 2019.
Figure 2.
Reported automated renewal success rates for 50 states and Washington, DC, by expansion status, 2015–2019. Source: Kaiser Family Foundation (KFF) annual surveys of state Medicaid eligibility and enrollment practices.13-18 “% NR” states do not report the automated renewal success rates, but did perform automated renewals.
Association between participation and automated renewal implementation
The unadjusted relationship between category of automated renewal success rate and Medicaid participation in 2015 and in 2019 for both children and adults is shown in Figure S2. Figure S3 shows the unadjusted participation rate over time for states always performing automated renewals, never performing automated renewals, and each state that implemented automated renewals during the study period.
In adjusted analyses, the implementation of automated renewals and Medicaid participation were not significantly associated among children (−0.12 percentage points [95% CI: −2.43, 2.19]) and adults (0.66 percentage points [95% CI: −3.30, 4.62]) (Table 2). The lack of association was consistent across expansion (children: 0.51 percentage points [95% CI: −3.26, 4.27]; adults: 0.42 percentage points [95% CI: −4.03, 4.88]) and non-expansion states (children: −0.91 percentage points [95% CI: −3.17, 1.35]; adults: 1.15 percentage points [95% CI: −3.10, 5.40]).
Table 2.
Association between state adoption of automated renewals and Medicaid participation, 2015–2019.
| Coefficient (95% CI), percentage points | P | |
|---|---|---|
| Adults | ||
| Overall | 0.66 (−3.30, 4.62) | .74 |
| Expansion states | 0.42 (−4.03, 4.88) | .85 |
| Non-expansion states | 1.15 (−3.10, 5.40) | .58 |
| Children | ||
| Overall | −0.12 (−2.43, 2.19) | .92 |
| Expansion states | 0.51 (−3.26, 4.27) | .79 |
| Non-expansion states | −0.91 (−3.17, 1.35) | .41 |
Abbreviations: CHIP, Children’s Health Insurance Program; KFF, Kaiser Family Foundation.
Source: Authors’ analysis of data from the American Community Survey and KFF annual surveys of state Medicaid eligibility and enrollment practices, 2015–2019. Participation rates calculated from proportion of those estimated to be eligible for Medicaid/CHIP that report having Medicaid insurance. Excludes those with private or other public health insurance. Adjusted for age, gender, an age group by gender interaction, race/ethnicity, education, marital status, income, employment status, food stamp receipt, a food stamp by automated renewal interaction, rurality of residence, state Medicaid expansion status, state Medicaid administrative burden, and state and year fixed effects; for children, parental education and employment status were used.
In sensitivity analyses, these results were also consistent in analyses that used alternative specifications of the automated renewal variable (ie, categories of automated renewal success rate, <50 vs ≥50% automated renewal success rate) and in analyses that limited analysis to states that did not change Medicaid expansion status over the study period (Tables S7 and S8).
Discussion
Using nationally representative survey data, we found that, in 2019, approximately 7 in 10 Medicaid-eligible adults enrolled in Medicaid and 9 in 10 eligible children enrolled. While participation did not change substantially between 2015 and 2019, participation was lower among older children; younger, male, and unmarried adults; childless households; and those living in non-expansion states compared with their counterparts. A growing number of states implemented automated renewals over time, with expansion states more likely to report processing a greater proportion of applications successfully. We did not, however, find an association between the adoption of automated Medicaid eligibility renewals and participation rates in Medicaid among eligible children and adults.
Our findings contrast with prior work, which has found a lower risk of churning—or temporary losses of coverage—with the successful performance of automated renewals. One study using a single year of Medicaid enrollment data found that enrollees in both Medicaid expansion and non-expansion states that performed automated renewals had a lower risk of experiencing a churning event,19 and a descriptive analysis found that states with greater success at performing automated renewals had lower rates of churning.25 Our study leveraged multiple years of data and adjusted for relevant sociodemographic determinants of participation, but examined annual Medicaid participation rates and was unable to assess churning or changes in Medicaid coverage during the year.
Importantly, we did not evaluate other potential outcomes that could be associated with automated renewals, such as improved coverage continuity, reduced burdens on enrollees, increased trust in government efficacy, or greater administrative efficiency for Medicaid programs. In addition, we were unable to fully account for other potential barriers to Medicaid participation, such as limited awareness of the program or eligibility requirements, challenging application systems, difficulty obtaining enrollment assistance, inability to prove income or residency status, or fluctuations in income leading to temporary gaps in eligibility. Other work suggests that a suite of policies aimed at reducing administrative burdens—eliminating re-enrollment waiting periods, creating online enrollment and renewal interfaces, reducing the frequency of renewals, among others—may be necessary to improve Medicaid participation.20
In addition, significant variability in the implementation of automated renewals exists and could influence the policy's impact on participation. We observed that many states grew more successful at completing automated renewals over time, which may reflect improvements in process design. States have discretion over several aspects of the process, including the degree to which automated renewals require manual processing, the number and type of databases queried for income information, and whether and to what degree discrepancies in enrollee-reported and database-verified income are tolerated.26 It is also possible that the automated renewal process could be used in a way that dampens participation and enrollment. States may periodically check available data on enrollees; if a change in income is identified, the enrollee must go through another eligibility redetermination, regardless of how recently it was performed.27 In this way, building stronger ties to income databases—as the automated renewal process requires—could lead to increased disenrollment of Medicaid beneficiaries if a state chooses to perform and act on periodic data checks.
Other state actions in the renewal process could also have affected our findings. States may have compensatory mechanisms in place to protect participation if they do not perform automated renewals or if an attempted automated renewal is unsuccessful. Medicaid agencies have long processed eligibility renewals without the assistance of third-party data and may therefore be able to do so as efficiently as if they were automated. If a renewal cannot be processed automatically, states also dictate the subsequent attempt at manual renewal, including how enrollee outreach is performed, the methods by which an enrollee can return a request for information (eg, by phone, in-person, by mail, online), and whether a renewal form pre-populated with enrollee information is sent.
We also found that Medicaid participation varied widely across states and individual characteristics. Medicaid expansion states had higher participation rates than non-expansion states, consistent with prior work.3 Adults had lower and more variable participation rates across states than for children and those with less formal education and lower income had lower participation rates. Similar to our findings, work performed both before and after the ACA found that female respondents, parents, and those with other eligible family members had higher Medicaid participation.2-4 This understanding can help outreach efforts better target eligible individuals with a lower propensity to enroll or remain enrolled.
State processes for improving the success rate of automated renewals for eligible beneficiaries are especially relevant with the recent unwinding of the PHE and its restriction on disenrolling Medicaid beneficiaries. In processing the large backlog of renewals, states used the automated renewal mechanism to reduce the number of “procedural denials”—disenrollments that occur not because someone has been deemed to be ineligible but because the state is unable to confirm ongoing eligibility. This may happen if the state has incorrect address information, an enrollee is unable to return a request for information, or if manual processing errors occur. However, the rate of pre-pandemic procedural denials has been found to be higher in states that report greater automated renewal success rates.28 Indeed, since unwinding began in April 2023, over 10 million people have been disenrolled for Medicaid as of November 2023, with an estimated 71% of those being terminated for procedural reasons.29 In some states, automated renewals were initially processed at the household level, which led to inappropriate disenrollment of children whose Medicaid eligibility thresholds were higher than adults in the same household.30 Our findings using pre-pandemic data are consistent with these reports, which suggest that nuanced attention to the details of the automated renewal process is necessary to achieve the policy's intended goal.31
Conclusion
Medicaid participation varies widely across eligibility groups, states, and individual sociodemographic characteristics, including gender and parental status. This variation may reflect, in part, differences in administrative barriers to getting and maintaining coverage. Implementation of an automated Medicaid eligibility renewal process designed to improve coverage continuity was not associated with increased program participation among Medicaid-eligible children and adults during the pre-pandemic era. As the PHE unwinding concludes, states may need to invest in multifaceted efforts—including and going beyond the automated renewal process—to ensure that the Medicaid-eligible individuals enroll and remain enrolled.
Supplementary Material
Acknowledgments
The authors thank KFF for their tireless work in documenting Medicaid policy practices and the millions of participants in the American Community Survey, without which this work would not be possible.
Contributor Information
Daniel B Nelson, Department of Population Medicine, Harvard Medical School, Boston, MA 02215, United States.
Phillip M Singer, Department of Political Science, University of Utah, Salt Lake City, UT 84112, United States.
Vicki Fung, Department of Medicine, Mongan Institute, Massachusetts General Hospital, Boston, MA 02114, United States.
Supplementary material
Supplementary material is available at Health Affairs Scholar online.
Funding
D.B.N. received support from a National Research Service Award T32 grant and V.F. received support from grants from the Agency for Healthcare Research and Quality (AHRQ) and the National Institutes of Health (NIH) during completion of this work.
Notes
- 1. Herd P, Moynihan DP. Administrative Burden: Policymaking by Other Means. Russell Sage Foundation; 2019. [Google Scholar]
- 2. Sommers BD, Tomasi MR, Swartz K, Epstein AM. Reasons for the wide variation in Medicaid participation rates among states hold lessons for coverage expansion in 2014. Health Aff (Millwood). 2012;31(5):909–919. 10.1377/hlthaff.2011.0977 [DOI] [PubMed] [Google Scholar]
- 3. Decker SL, Abdus S, Lipton BJ. Eligibility for and enrollment in Medicaid among nonelderly adults after implementation of the Affordable Care Act. Med Care Res Rev. 2022;79(1):125–132. 10.1177/1077558721996851 [DOI] [PubMed] [Google Scholar]
- 4. Haley JM, Kenney GM, Wang R, Lynch V, Buettgens M. Medicaid/CHIP participation reached 93.7 percent among eligible children in 2016. Health Aff (Millwood). 2018;37(8):1194–1199. 10.1377/hlthaff.2018.0417 [DOI] [PubMed] [Google Scholar]
- 5. Goldman AL, Sommers BD. Among low-income adults enrolled in Medicaid, churning decreased after the Affordable Care Act. Health Aff (Millwood). 2020;39(1):85–93. 10.1377/hlthaff.2019.00378 [DOI] [PubMed] [Google Scholar]
- 6. Simon AE, Schoendorf KC. Medicaid enrollment gap length and number of Medicaid enrollment periods among US children. Am J Public Health. 2014;104(9):e55–e61. 10.2105/AJPH.2014.301976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cholera R, Anderson D, Raman SR, et al. Medicaid coverage disruptions among children enrolled in North Carolina Medicaid from 2016 to 2018. JAMA Health Forum. 2021;2(12):e214283. 10.1001/jamahealthforum.2021.4283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brantley E, Ku L. Continuous eligibility for Medicaid associated with improved child health outcomes. Med Care Res Rev. 2022;79(3):404–413. 10.1177/10775587211021172 [DOI] [PubMed] [Google Scholar]
- 9. Sommers BD, Gourevitch R, Maylone B, Blendon RJ, Epstein AM. Insurance churning rates for low-income adults under health reform: lower than expected but still harmful for many. Health Aff (Millwood). 2016;35(10):1816–1824. 10.1377/hlthaff.2016.0455 [DOI] [PubMed] [Google Scholar]
- 10. Roberts ET, Pollack CE. Does churning in Medicaid affect health care use? Med Care. 2016;54(5):483–489. 10.1097/MLR.0000000000000509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Centers for Medicare & Medicaid Services . Ex parte renewal: strategies to maximize automation, increase renewal rates, and support unwinding efforts. Web presentation. Accessed October 20, 2022. https://www.medicaid.gov/sites/default/files/2022-10/ex-parte-renewal-102022.pdf
- 12. Heberlein M, Brooks T, Alker J, Artiga S, Stephens J. Getting into Gear for 2014: Findings from a 50-State Survey of Eligibility, Enrollment, Renewal, and Cost-Sharing Policies in Medicaid and CHIP, 2012–2013. Kaiser Commission on Medicaid and the Uninsured; 2013. [Google Scholar]
- 13. Brooks T, Touschner J, Artiga S, Stephens J, Gates A. Modern Era Medicaid: January 2015 Findings from a 50-State Survey of Eligibility, Enrollment, Renewal, and Cost-Sharing Policies in Medicaid and CHIP as of January 2015. The Henry J. Kaiser Family Foundation; 2015. [Google Scholar]
- 14. Brooks T, Miskell S, Artiga S, Cornachione E, Gates A. Medicaid and CHIP eligibility, enrollment, renewal, and cost sharing policies as of January 2016: findings from a 50-state survey. Kaiser Family Foundation Report; 2016.
- 15. Brooks T, Wagnerman K, Artiga S, Cornachione E, Ubri P. Medicaid and CHIP eligibility, enrollment, renewal, and cost sharing policies as of January 2017: findings from a 50-state survey. Kaiser Family Foundation Report; 2017.
- 16. Brooks T, Wagnerman K, Artiga S, Cornachione E. Medicaid and CHIP eligibility, enrollment, renewal, and cost sharing policies as of January 2018: findings from a 50-state survey. Kaiser Family Foundation Report; 2018.
- 17. Brooks T, Roygardner L, Artiga S, Pham O, Dolan R. Medicaid and CHIP Eligibility, Enrollment, and Cost Sharing Policies as of January 2019: Findings from a 50-State Survey. Kaiser Family Foundation; 2019. [Google Scholar]
- 18. Brooks T, Roygardner L, Artiga S, Pham O, Dolan R. Medicaid and CHIP Eligibility, Enrollment, and Cost Sharing Policies as of January 2020: Findings from a 50-State Survey. Kaiser Family Foundation; 2020. [Google Scholar]
- 19. Ku L, Platt I. Duration and continuity of Medicaid enrollment before the COVID-19 pandemic. JAMA Health Forum. 2022;3(12):e224732. 10.1001/jamahealthforum.2022.4732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fox AM, Stazyk EC, Feng W. Administrative easing: rule reduction and Medicaid enrollment. Public Adm Rev. 2020;80(1):104–117. 10.1111/puar.13131 [DOI] [Google Scholar]
- 21. Office of Information and Regulatory Affairs; Office of Management and Budget; Executive Office of the President of the United States . Tackling the time tax: how the federal government is reducing burdens to accessing critical benefits and services. 2023. Accessed August 21, 2023. https://www.whitehouse.gov/wp-content/uploads/2023/07/OIRA-2023-Burden-Reduction-Report.pdf.
- 22. Centers for Medicare & Medicaid Services, US Department of Health and Human Services . Streamlining the Medicaid, Children's Health Insurance Program, and Basic Health Program Application, Eligibility Determination, Enrollment, and Renewal Processes. Federal Register, 42 CFR Parts 431, 435, 457, and 600. 2022 87(172):54760-54855.
- 23. Lukanen E, Hest R, Turner K. Defining family for studies of health insurance coverage. State Health Access Data Assistance Center Issue Brief. 2023.
- 24. Fox AM, Feng W, Zeitlin J, Howell EA. Trends in state Medicaid eligibility, enrollment rules, and benefits. Health Aff (Millwood). 2020;39(11):1909–1916. 10.1377/hlthaff.2019.01350 [DOI] [PubMed] [Google Scholar]
- 25. Medicaid and CHIP Payment and Access Commission . An updated look at rates of churn and continuous coverage in Medicaid and CHIP. October 2021. Accessed January 14, 2022. https://www.macpac.gov/publication/an-updated-look-at-rates-of-churn-and-continuous-coverage-in-medicaid-and-chip-abstract/.
- 26. Brooks T, Gardner A, Yee P, et al. Medicaid and CHIP Eligibility, Enrollment, and Renewal Policies as States Prepare for the Unwinding of the Pandemic-Era Continuous Enrollment Provision. Georgetown Center for Children and Families and Kaiser Family Foundation; 2023. [Google Scholar]
- 27. Medicaid and CHIP Learning Collaborative . Coverage learning collaborative: Medicaid and CHIP renewals and redeterminations. Accessed January 13, 2021. https://www.medicaid.gov/sites/default/files/2021-01/renewals-redeterminations.pdf
- 28. Schpero WL, Brahmbhatt D, Liu MX, Ndumele CD, Chatterjee P. Variation in procedural denials of Medicaid eligibility across states before the COVID-19 pandemic. JAMA Health Forum. 2023;4(11):e233892. 10.1001/jamahealthforum.2023.3892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kaiser Family Foundation (KFF) . Medicaid enrollment and unwinding tracker; 2023. Accessed 2 November 2023. https://www.kff.org/report-section/medicaid-enrollment-and-unwinding-tracker-overview/.
- 30. Tsai D. Letter to state Medicaid directors from the Centers for Medicare and Medicaid Services. August 30, 2023. Accessed January 4, 2024. https://www.medicaid.gov/sites/default/files/2023-08/state-ltr-ensuring-renewal-compliance.pdf
- 31. Medicaid and CHIP Payment and Access Commission . Increasing the rate of ex parte renewals. September 2023. Accessed October 1, 2023. https://www.macpac.gov/wp-content/uploads/2023/09/Increasing-the-Rate-of-Ex-Parte-Renewals-Brief.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.