Dear Editor,
Herpes simplex virus (HSV) and varicella zoster virus are ubiquitous members of the Herpesviridae family. Their cutaneous manifestation is typically characterized by painful grouped vesicles over an erythematous base, often with a prodrome of burning, itching, or pain. Herpetic syringitis is an infrequently described histological pattern reported almost exclusively in HIV-infected patients. We present this rare manifestation of HSV in an immunocompetent host.
A 32-year-old man presented with multiple raised lesions over the penis of three days duration. A few pinhead-sized raised lesions appeared initially, associated with a mild burning sensation. The lesions then progressed over the next 24 to 48 h, to become three times their original size. There was one episode of fever, two days before the lesions appeared which lasted for 24 h.
He gave a history of his last sexual contact with an acquaintance 7–10 days back. There was no history of burning micturition, swelling in the inguinal region, per urethral discharge, or similar complaints in the past.
Venereological examination revealed five papules with raised margins and an indurated base that did not bleed on touch [Figure 1]. The lymph nodes were not palpable, and the rest of the venereological examination was unremarkable. Tzanck smear did not yield any positive findings.
Figure 1.

Raised skin-colored papules present over glans penis
A skin biopsy was performed from one of the papular lesions keeping differentials of genital warts, papular lesions of syphilis, and atypical presentation of genital herpes. The histopathological examination revealed spongiotic mucosa with occasional neutrophilic exocytosis, and the ulcerated area showed crusting in the form of lymphocytes, neutrophils, and cell debris enmeshed in fibrin. The subepithelial tissue delineated eccrine coils, lined by cells showing nucleomegaly, nuclear chromatin margination, and nuclear molding suggestive of Herpes viral inclusions [Figure 2]. The surrounding tissue showed a dense mixed inflammatory infiltrate along with plump, endothelial cell-lined, proliferating capillaries. It did not reveal any evidence of HPV-like inclusions, intracellular organisms, or dominant plasma cell infiltrates. Immunohistochemistry (IHC) revealed endothelial cells, which were highlighted by CD34 (membranous), and eccrine glands, highlighted by CK7 [Figure 3].
Figure 2.
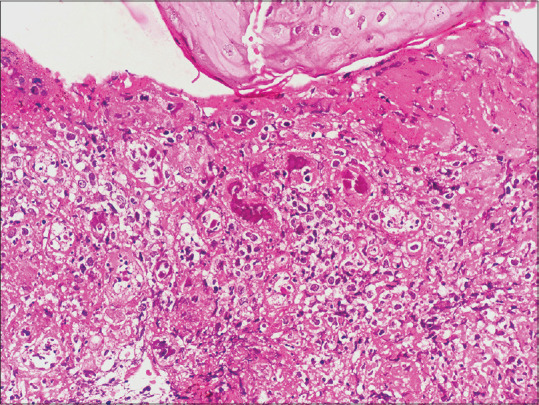
Subepithelial tissue delineated eccrine coils lined by cells showing nucleomegaly, nuclear chromatin margination, and nuclear molding suggestive of herpes viral inclusions (H and E, 200x)
Figure 3.
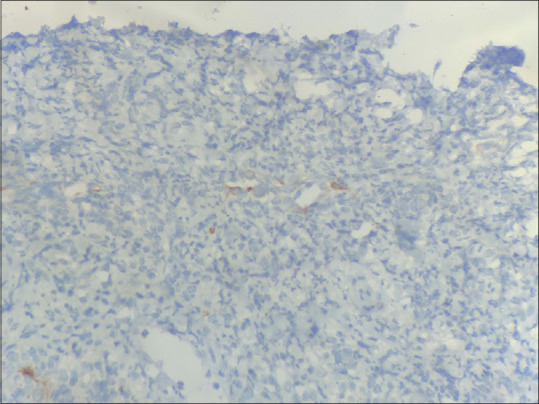
Immunohistochemistry (100x) showed Cytokeratin 7 highlighting the eccrine coils
Serological examination revealed seropositivity for both IgM and IgG antibodies against HSV-2. Other viral markers to rule out human immunodeficiency virus (HIV) infection, hepatitis B, and hepatitis C were negative. The gram stain and culture did not reveal any microbial evidence. Based on the serology, histopathological, and IHC findings, a diagnosis of herpetic syringitis was made. He was managed with tablet acyclovir 400 mg thrice daily for seven days with complete resolution of the lesions.
HSV is a highly contagious virus and a member of the Herpesviridae family, which also includes varicella zoster virus (VZV) and others.[1] The HSV-1 and HSV-2 viruses, as well as varicella zoster viruses, comprise the α sub-group and are distinguished by their short replicative cycle, induction of cytopathology in monolayer cell cultures, and broad host range.[2]
The cutaneous lesions of Herpes simplex virus type 1 (HSV-1) and Herpes simplex virus type 2 (HSV-2) are traditionally described as painful, grouped vesicles on an erythematous base, often with a prodrome of burning, itching, or pain, involving the mucocutaneous tissue, that is, the mouth, lips, or genitals.[3]
Histopathological examination under low-power illumination often reveals shallow vesicles or ulcers with ballooning keratinocytes, acantholysis, and necrosis. Cytopathic changes include enlarged and pale keratinocytes with steel-gray nuclei, marginated chromatin, multinucleated cells, nuclear molding, and eosinophilic intranuclear (Cowdry Type A) inclusions.[1,2,3]
Herpetic changes are most commonly noted in the epidermis; however, dermal including adnexal structures are also frequently involved. Commonly involved structures include the epidermis, hair follicles, sebaceous glands, nerves, blood vessels (lymphocytic, leukocytoclastic vasculitis), and eccrine glands and ducts, out of which the hair follicles and sebaceous glands are most frequently affected.[4,5]
Herpetic syringitis is a rare manifestation characterized by the involvement of the eccrine gland epithelium by the Herpes simplex virus, and few such reports are available in the literature.[6] Among the cases reported, three patients were immunodeficient. One patient had Hodgkin’s disease, and two patients were suffering from acquired immunodeficiency syndrome (AIDS). Syringitis has also been mentioned in cases with varicella zoster virus in reports by Alonso-Pérez et al. and Horie et al.[7,8]
The increased incidence of herpetic syringitis in AIDS patients has been postulated by Muñoz et al., according to whom the immunodeficiency state might induce an alteration of eccrine secretion and allow the viral infection to progress from the epidermis into the ducts of the eccrine sweat gland.[4] Involvement limited to adnexa, may be a clue to herpes infection in patients who are immunocompromised.[6] We report this unique case of herpetic syringitis in an immunocompetent patient who presented with genital papular lesions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hoyt B, Bhawan J. Histological spectrum of cutaneous herpes infections. Am J Dermatopathol. 2014;36:609–19. doi: 10.1097/DAD.0000000000000148. [DOI] [PubMed] [Google Scholar]
- 2.Chisholm C, Lopez L. Cutaneous infections caused by Herpesviridae: A review. Arch Pathol Lab Med. 2011;135:1357–62. doi: 10.5858/arpa.2010-0156-RS. [DOI] [PubMed] [Google Scholar]
- 3.Leinweber B, Kerl H, Cerroni L. Histopathologic features of cutaneous herpes virus infections (herpes simplex, herpes varicella/zoster): A broad spectrum of presentations with common pseudolymphomatous aspects. Am J Surg Pathol. 2006;30:50–8. doi: 10.1097/01.pas.0000176427.99004.d7. [DOI] [PubMed] [Google Scholar]
- 4.Muñoz E, Valks R, Fernández-Herrera J, Fraga J. Herpetic syringitis associated with eccrine squamous syringometaplasia in HIV-positive patients. J Cutan Pathol. 1997;24:425–8. doi: 10.1111/j.1600-0560.1997.tb00817.x. [DOI] [PubMed] [Google Scholar]
- 5.Rinder HM, Murphy GF. Eccrine duct involvement by herpes zoster. Arch Dermatol. 1984;120:261–2. [PubMed] [Google Scholar]
- 6.Sedrak MP, Marek M, Matherene R, Kelly B. Syringitis: A clue to herpes infection. Dermatol Online J. 2012;18:6. [PubMed] [Google Scholar]
- 7.Alonso-Pérez A, Fraga J, Delgado Y, Aragüés M, Nam-Cha S, García-Díez A. Nodular herpes zoster with herpetic syringitis and no epidermal involvement in a patient with Burkitt lymphoma. Am J Dermatopathol. 2006;28:194–6. doi: 10.1097/00000372-200606000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Horie C, Mizukawa Y, Yamazaki Y, Shiohara T. Varicella-zoster virus antigen expression of eccrine gland and duct epithelium in herpes zoster lesions. Br J Dermatol. 2011;165:802–7. doi: 10.1111/j.1365-2133.2011.10462.x. [DOI] [PubMed] [Google Scholar]


