Abstract
Background:
C5 palsy (C5P) is a recognized potential postoperative complication of cervical spine surgery but has rarely been reported following an open esophageal diverticulectomy.
Methods:
A 61-year-old underwent an open esophageal diverticulectomy for symptomatic Zencker’s diverticulum.
Results:
Postoperatively, she presented with right upper extremity weakness and sensory deficits consistent with a C5P that was later confirmed by electromyography.
Conclusion:
The potential for C5P after esophageal diverticulectomy for symptomatic Zencker’s diverticulum is rare. Postoperative recognition and appropriate management are critical to recovery.
Keywords: C5 palsy, Cervical spine, Cervical spondylosis, Esophageal diverticulum

INTRODUCTION
C5 palsy (C5P) is a well-documented potential complication following cervical spine surgery, occurring in 0–30% of patients.[4,8,10] While cases of C5P following anterior and posterior cervical spine surgery have been widely described,[2,3,6,7,9] cases following open esophageal diverticulectomy are rare.
CASE PRESENTATION
A 61-year-old female with a history of Crohn’s disease presented initially with 1 year of dysphagia and a 40 lb weight loss. A barium esophagram revealed a Zencker’s diverticulum just above the thoracic inlet. The patient agreed to proceed with a transoral stapling with possible open diverticulectomy. Under general endotracheal anesthesia (i.e., Macintosh blade under direct laryngoscopy), she underwent flexible upper gastrointestinal endoscopy. A 2.5 cm Zencker’s diverticulum was identified above the cricopharyngeus muscle. A resolution clip was placed in the diverticulum apex. Stapling attempts using a rigid endoscope to place the bivalved diverticula blade into both the diverticula and esophagus were unsuccessful. The procedure was aborted and converted to an open repair utilizing a left anterior sternocleidomastoid approach; the diverticula was removed, and the esophagostomy was oversewn in a two-layer fashion. The final endoscopy confirmed the diverticulum was excluded, the esophagus patent and the leak test was negative.
Postoperative course
Immediately postoperatively, the patient awoke with significant proximal right upper extremity weakness (manual muscle testing grade ⅕ in deltoid and biceps) and near-complete sensory loss from the right shoulder to the elbow. She was diagnosed clinically with a right C5P. The brachial plexus magnetic resonance was normal [Figure 1]. The magnetic resonance imaging of the cervical spine, however, documented multilevel cervical spondylosis with moderate C4–5 right and severe left C4–5 foraminal stenosis, with foraminal spondylotic encroachment at the C5–6 and C7–T1 levels [Figure 2]. Her symptoms gradually improved within 4 postoperative months, with sensory deficits resolved and right deltoid and biceps strength recovered to the 4/5 level. In addition, the electromyography confirmed normal motor unit recruitment.
Figure 1:
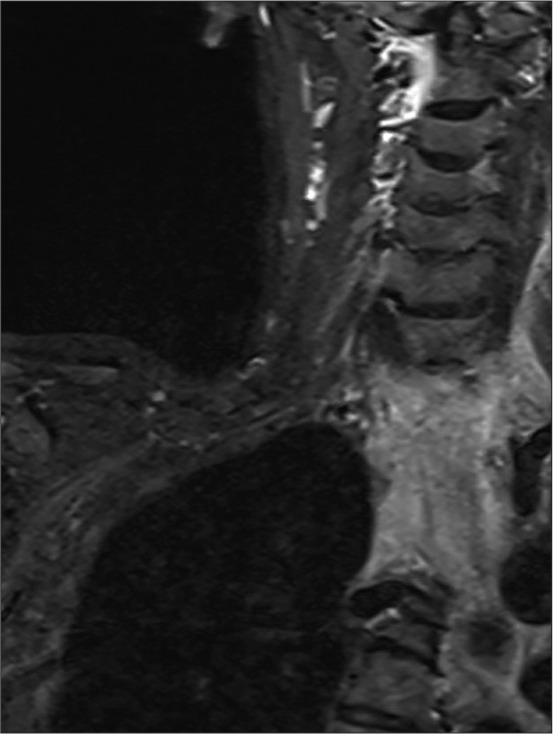
Coronal brachial plexus magnetic resonance imaging short-tau inversion recovery sequence showing grossly normal appearance without associated signal change throughout the brachial plexus.
Figure 2:
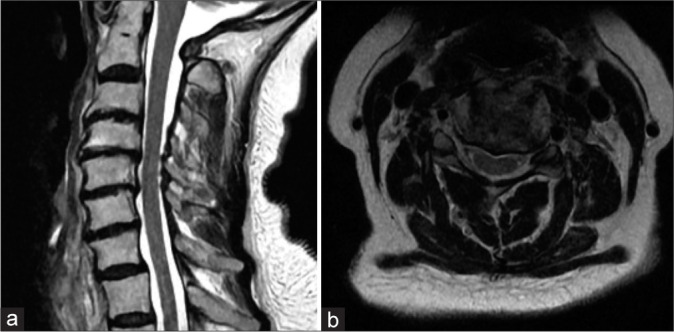
(a) Sagittal T2-weighted magnetic resonance imaging (MRI) of the cervical spine showing multilevel spondylotic changes. (b) Axial T2-weighted MRI of the cervical spine at the C4–5 level showing severe left and moderate right foraminal stenosis.
DISCUSSION
Laryngoscopy and basic airway maneuvers may result in sufficient extension of the cervical spine to result in neurological damage.[1,5] A summary table of pertinent references describing C5 palsy incidence, diagnosis, and injury mechanisms is provided in Table 1. Notably, identifying signs and symptoms of cervical spondylosis preoperatively and avoiding perioperative cervical hyperextension maneuvers should help avoid the new onset of C5 root and/or cord compromise postoperatively.
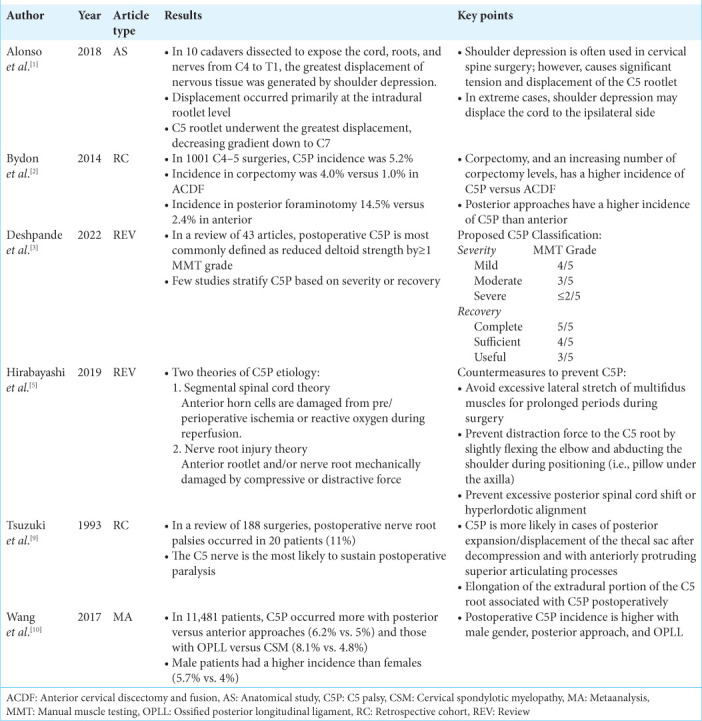
Table 1:
Reference summary table.
CONCLUSION
In patients with severe pre-existing cervical spondylosis, care should be taken to avoid excess shoulder retraction and stretch injuries during intubation, laryngoscopy/endoscopy, and, in this case, open esophageal diverticulectomy for symptomatic Zencker’s diverticulum.
Footnotes
How to cite this article: Wilkinson BM, Polavarapu H, Maloney BB, Draytsel D, Hazama A. C5 palsy following esophageal diverticulum resection. Surg Neurol Int. 2024;15:157. doi: 10.25259/SNI_264_2024
Contributor Information
Brandon Michael Wilkinson, Email: wilkinsb@upstate.edu.
Hanish Polavarapu, Email: polavarh@upstate.edu.
Brendan Bernard Maloney, Email: malonebr@upstate.edu.
Dan Draytsel, Email: draytsed@upstate.edu.
Ali Hazama, Email: hazamaa@upstate.edu.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Alonso F, Voin V, Iwanaga J, Hanscom D, Chapman JR, Oskouian RJ, et al. Potential mechanism for some postoperative C5 palsies: An anatomical study. Spine (Phila Pa 1976) 2018;43:161–6. doi: 10.1097/BRS.0000000000002281. [DOI] [PubMed] [Google Scholar]
- 2.Bydon M, Macki M, Kaloostian P, Sciubba DM, Wolinsky JP, Gokaslan ZL, et al. Incidence and prognostic factors of C5 palsy: A clinical study of 1001 cases and review of the literature. Neurosurgery. 2014;74:595–605. doi: 10.1227/NEU.0000000000000322. [DOI] [PubMed] [Google Scholar]
- 3.Deshpande N, Stino AM, Smith BW, Little AA, Yang LJ, Park P, et al. Defining postoperative C5 palsy and recovery: A systematic review. J Neurosurg Spine. 2022;38:457–64. doi: 10.3171/2022.11.SPINE221067. [DOI] [PubMed] [Google Scholar]
- 4.Gu Y, Cao P, Gao R, Tian Y, Liang L, Wang C, et al. Incidence and risk factors of C5 palsy following posterior cervical decompression: A systematic review. PLoS One. 2014;9:e101933. doi: 10.1371/journal.pone.0101933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirabayashi S, Kitagawa T, Yamamoto I, Yamada K, Kawano H. Postoperative C5 palsy: Conjectured causes and effective countermeasures. Spine Surg Relat Res. 2018;3:12–6. doi: 10.22603/ssrr.2018-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nassr A, Eck JC, Ponnappan RK, Zanoun RR, Donaldson WF, 3rd, Kang JD. The incidence of C5 palsy after multilevel cervical decompression procedures: A review of 750 consecutive cases. Spine (Phila Pa 1976) 2012;37:174–8. doi: 10.1097/BRS.0b013e318219cfe9. [DOI] [PubMed] [Google Scholar]
- 7.Sakaura H, Hosono N, Mukai Y, Ishii T, Yoshikawa H. C5 palsy after decompression surgery for cervical myelopathy: Review of the literature. Spine (Phila Pa 1976) 2003;28:2447–51. doi: 10.1097/01.BRS.0000090833.96168.3F. [DOI] [PubMed] [Google Scholar]
- 8.Shou F, Li Z, Wang H, Yan C, Liu Q, Xiao C. Prevalence of C5 nerve root palsy after cervical decompressive surgery: A meta-analysis. Eur Spine J. 2015;24:2724–34. doi: 10.1007/s00586-015-4186-5. [DOI] [PubMed] [Google Scholar]
- 9.Tsuzuki N, Abe R, Saiki K, Okai K. Paralysis of the arm after posterior decompression of the cervical spinal cord. II. Analyses of clinical findings. Eur Spine J. 1993;2:197–202. doi: 10.1007/BF00299446. [DOI] [PubMed] [Google Scholar]
- 10.Wang T, Wang H, Liu S, Ding WY. Incidence of C5 nerve root palsy after cervical surgery: A meta-analysis for last decade. Medicine (Baltimore) 2017;96:e8560. doi: 10.1097/MD.0000000000008560. [DOI] [PMC free article] [PubMed] [Google Scholar]


