Abstract
Introduction
The present study is a mixed-methods exploratory study aiming to understand the lived experiences of females with phenylketonuria (PKU) in managing their health. The study aims to identify what individual, interpersonal, and environmental factors serve as facilitators and inhibitors, and how PKU intrudes on different realms of health.
Methods
Attendees of Emory's Metabolic Camp and female users of Medical Nutrition Therapy for Prevention (MNT4P) were recruited. Participants were administered the Illness Intrusiveness Ratings Scale (IIRS) survey and qualitatively interviewed. The IIRS survey was analyzed using descriptive statistics and the interviews were coded and assessed using inductive and deductive analysis.
Results
In total, 25 participants were included in analysis (adults, n = 20; adolescents, n = 5). In the IIRS survey, diet had the highest average impact score of 5.74 (SD = 2.05) and religious expression had the lowest average impact score of 1.74 (SD = 1.65). The most salient themes that arose from the qualitative interviews were related to concerns of pregnancy (n = 25), interactions with health care providers relative to PKU care (n = 23) and independent of PKU care (n = 21), social support (n = 21) and isolation (n = 12), financial issues (n = 22), and illness intrusiveness on general health management (n = 22).
Discussion
Adolescent and adult female participants with PKU identified significant concerns in individual, interpersonal, and environmental factors affecting the management of their health. Additionally, the illness intrusiveness of PKU impacted their physical, mental, and gynecological health. Future research should further assess the unique challenges faced by females with PKU and potential interventions to better address these barriers.
Keywords: Phenylketonuria, MPKU, Illness intrusiveness, Health management
1. Introduction
Phenylketonuria (PKU) is a rare metabolic disorder that arises from a mutation in the phenylalanine hydroxylase (PAH) gene, which encodes the PAH enzyme that converts the amino acid phenylalanine (Phe) into tyrosine (Tyr). Without PAH available to complete the conversion, individuals with PKU have an increased blood concentration of Phe. When untreated, this can lead to neurological and intellectual disabilities, as well as physical and psychological issues [1,2].
Optimal management of PKU is characterized by early detection through newborn screening and confirmatory testing, and with early initiation of stringent dietary therapy to prevent neurological sequelae [1]. Dietary intervention consists of a Phe-restricted diet, with supplementation of Phe-free protein formulas and low-protein modified foods, and, in some cases, pharmacological supplementation [[1], [2], [3]]. Currently, the two FDA-approved pharmaceutical treatments for PKU are sapropterin dichloride, an oral BH4 treatment, and pegvaliase, an injectable enzyme therapy [1,3]. To avoid negative neurocognitive and psychological outcomes later in life, individuals are counseled to maintain Phe blood concentration within the optimal range of 2–6 mg/dL, or 120–360 μmol/L throughout their lifetime [1,3].
Individuals with PKU face individual, interpersonal, and environmental barriers that impact their health management. Most studies have found a similar quality of life between individuals with PKU and the general population, yet there are significant exceptions in various realms of the lives of individuals with PKU [1]. Huijbregts et al. [4] found that adults with PKU had significantly worse multivariate effects in cognition, depression, anger, and pain than the general population. Adult women with PKU in the study scored significantly worse than adult men with PKU in fine motor functioning, sleep, pain, vitality, and depression.
Females of reproductive age with PKU face additional challenges, as they are at risk for having a child with maternal phenylketonuria (MPKU). MPKU can occur when a child is born to a woman with PKU who did not maintain metabolic control pre-conception and throughout pregnancy [[5], [6], [7]]. MPKU is associated with intellectual disability, microcephaly, congenital heart disease, and other birth defects of the fetus [[5], [6], [7]]. As the fetal blood Phe concentration can be up to twice as high as the mother, pregnant women are under a particular amount of pressure to maintain their Phe concentration between 2 and 6 mg/dL [6].
The unique stringent dietary management of individuals with PKU impacts how they can manage their health outside of PKU, yet there is a paucity of research addressing such. Further, there are few studies that attempt to differentiate between those health concerns caused by PKU and those caused by other unrelated factors. In terms of environmental and interpersonal factors impacting health management, some studies have described coordination challenges and health care provider ignorance regarding PKU-specific health care needs, yet there is little information about these same issues related to the general health of individuals with PKU, outside of their condition [[8], [9], [10]]. This study aims to qualitatively explore the experiences of females with PKU in managing their general health and how it is impacted by their PKU health management, and what personal, interpersonal, and environmental factors impede or facilitate their health management.
2. Materials and methods
2.1. Participants
Eligible participants were English-speaking biological females above the age of 13 years and diagnosed with PKU. The study was approved by the Emory University Institutional Review Board (IRB). Twenty-five participants were enrolled, including 15 participants interviewed and surveyed at Emory University's Metabolic Camp from June 19 to June 24, 2023, of which two were excluded as they did not meet the age requirement; 11 participants were interviewed and surveyed from Medical Nutrition Therapy for Prevention's (MNT4P) database and one participant was interviewed and surveyed from a list of past camp attendees. These interviews were conducted from November 2023 to February 2024.
2.2. Recruitment
The initial participants were recruited by convenience sampling at Emory University's Metabolic Camp, a week-long educational camp for adolescent and adult females with inherited metabolic disorders (IMD). Prior to enrollment, all participants provided written informed consent (and assent if under the age of 18 years) to participate in any research conducted at, or after the camp. Camp attendees were presented a summary of the research purpose and methods on June 19, 2023 and administered a physical sign-up sheet to participate in the study.
Subsequent participants were recruited by convenience sample from lists of females with PKU from the MNT4P database and past camp attendance records. MNT4P is a program based in Emory University's School of Medicine that provides medical foods and pay assistance to individuals with IMDs that reside in the state of Georgia. Individuals from the lists were sent an e-mail introducing the research and instructed to respond if they were interested in participating. MNT4P respondents were e-mailed a link to the consent form for the study via Emory RedCap, a secure web application used for survey management and data collection. Once consent was given, interview availability was obtained, and respondents were sent the Illness Intrusiveness Ratings Scale (IIRS) survey via Emory Redcap. Alternatively, past camp attendees were not administered a consent form, as their consent was obtained when they attended camp. They were sent the IIRS survey via Qualtrics. Interviews were scheduled based on respondent availability and conducted by Zoom and phone call. No compensation was offered to any participant involved in the study.
2.3. Data collection
2.3.1. Illness intrusiveness ratings scale survey
The IIRS survey is a validated 13-item self-report survey that assesses the impact of an illness's disruption on various aspects of one's life [11]. The survey asks respondents to rate how much their illness impacts an aspect of their life from “1” (Not Very Much) to “7” (Very Much). Survey items include Diet, Financial Situation, and Family Relations [11]. No survey items were adapted in the present study. Prior to each in-person interview at Emory's Metabolic Camp, a physical copy of the survey was administered to be completed in writing. Upon scheduling online interviews, an electronic survey was administered through Emory RedCap to participants in MNT4P, and through Qualtrics to past camp attendees.
2.3.2. Qualitative interviews
Qualitative interviews were semi-structured and lasted 30 to 60 min. Initial interviews at Emory University's Metabolic Camp were conducted in-person and subsequent interviews were conducted online and over the phone. The interview guides covered topics related to dietary management experiences, perceived illness intrusiveness of PKU, and individual, interpersonal, and environmental facilitators and barriers to health management. All interviews were audio recorded and transcribed by Abigail Aronoff, with assistance from the Rev. AI Transcription service.
2.4. Statistical analysis
Descriptive statistical analysis was conducted on IIRS survey responses using SAS 9.4 Analytics Software. Adolescent and adult ratings were stratified, and data were compared to assess differences in illness intrusiveness perception by age. All interviews were de-identified and uploaded to MaxQDA Plus 2022 (22.8.0) for qualitative thematic analysis. Codes and themes were construed inductively from recurring ideas across interviews, and deductively from the questions posed in the interview guide (Appendix). A codebook was created and revised throughout the coding process to guide thematic analysis.
3. Results
3.1. Demographic characteristics
Of the 27 participants surveyed, 25 were included in data analysis, as two participants did not meet the age requirement. Participants ranged in age from 15 to 58 years with a mean age of 24.8 (SD = 10.94), and a median age of 21 years. Of the participants, 20 were adults (at or above the age of 18 years), and five were minors (below the age of 18 years). Most of the participants identified as White (n = 23/25), one participant identified as mixed race, and one identified as Asian. Of the participants that knew an estimate of their household income level (n = 15/25), the mean income level was $87,967 (SD = $66,065) per year.
Most of the participants had completed a blood spot test for monitoring Phe and Tyr within the last year and knew an estimate of their most recent Phe blood concentrations (n = 19/25). Of these participants, 58% (n = 11/19), were within the target therapeutic range of a Phe concentration of 2–6 mg/dL, one participant was below the target range, and 28% (n = 7/19) were above the target range. Most (84%, n = 21/25) of participants reported being actively followed by a doctor or dietitian for PKU treatment at the time of the study and 80% (n = 20/25) reported being actively followed by a health care provider for non-PKU health care needs. (See Table 1.)
Table 1.
Demographic Characteristics.
| Participants (N = 25) | |
|---|---|
| Age, mean (SD) | 24.76 (10.94) |
| Adolescent (< 18 years) (n) | 20% (5) |
| Adult (≥ 18 years) (n) | 80% (20) |
| Race | |
| American Indian or Alaska Native (n) | 0% (0) |
| Asian (n) | 4% (1) |
| Black or African American (n) | 0% (0) |
| Native Hawaiian or Other Pacific Islander (n) | 0% (0) |
| White (n) | 92% (23) |
| Mixed (n) | 4% (1) |
| Phe Concentration | |
| <2 mg/dL (n) | 4% (1) |
| 2–6 mg/dL (n) | 44% (11) |
| >6 mg/dL (n) | 28% (7) |
| Missing (n) | 24% (6) |
| Household Income | |
| ≤$25,000 (n) | 4% (1) |
| >$25,000 ≤ $50,000 (n) | 24% (6) |
| >$50,000 ≤ $75,000 (n) | 0% (0) |
| >$75,000 ≤ $100,000 (n) | 8% (2) |
| >$100,000 (n) | 24% (6) |
| Missing (n) | 40% (10) |
| Ever Been Pregnant | |
| Yes (n) | 24% (6) |
| No (n) | 76% (19) |
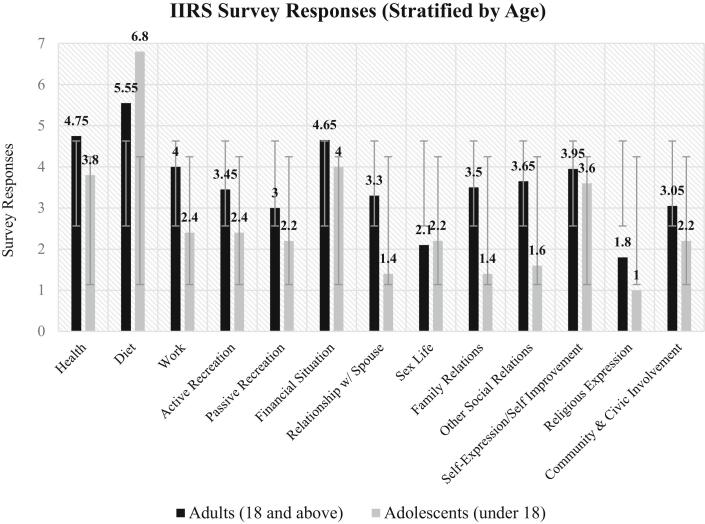
3.2. Illness intrusiveness
The mean IIRS score for all participants was 44.85 (SD = 18.42). Analysis revealed that PKU most impacted life domains related to dietary management, including diet (M = 5.74, SD = 2.05), financial situation (M = 4.70, SD = 2.41), and health (M = 4.67, SD = 2.08). PKU had the lowest impact on life domains related to religious expression (M = 1.74, SD = 1.65) and sex life (M = 2.07, SD = 2.22).
Adults (18 years and older) had a higher mean IIRS score (M = 46.75, SD = 20.31) than adolescents (below 18 years) (M = 35, SD = 9). The life domains that had the largest differences in impact from PKU among adults and adolescents related to interpersonal relationships, including family relations (Adult M = 3.50, Adolescent M = 1.40), other social relations, (Adult M = 3.65, Adolescent M = 1.60), and relationship with spouse (Adult M = 3.30, Adolescent M = 1.40). Both groups had the most similar average impact score for sex life (Adult M = 2.1, Adolescent M = 2.2). (See Fig. 1.)
Fig. 1.
IIRS Survey Responses Stratified By Age.
3.3. Qualitative interview key findings
Key themes that arose from the interviews fell into categories of individual factors, interpersonal factors, structural factors, illness intrusiveness, and dietary management.
3.3.1. Individual factors
3.3.1.1. Female identity and risks associated with pregnancy
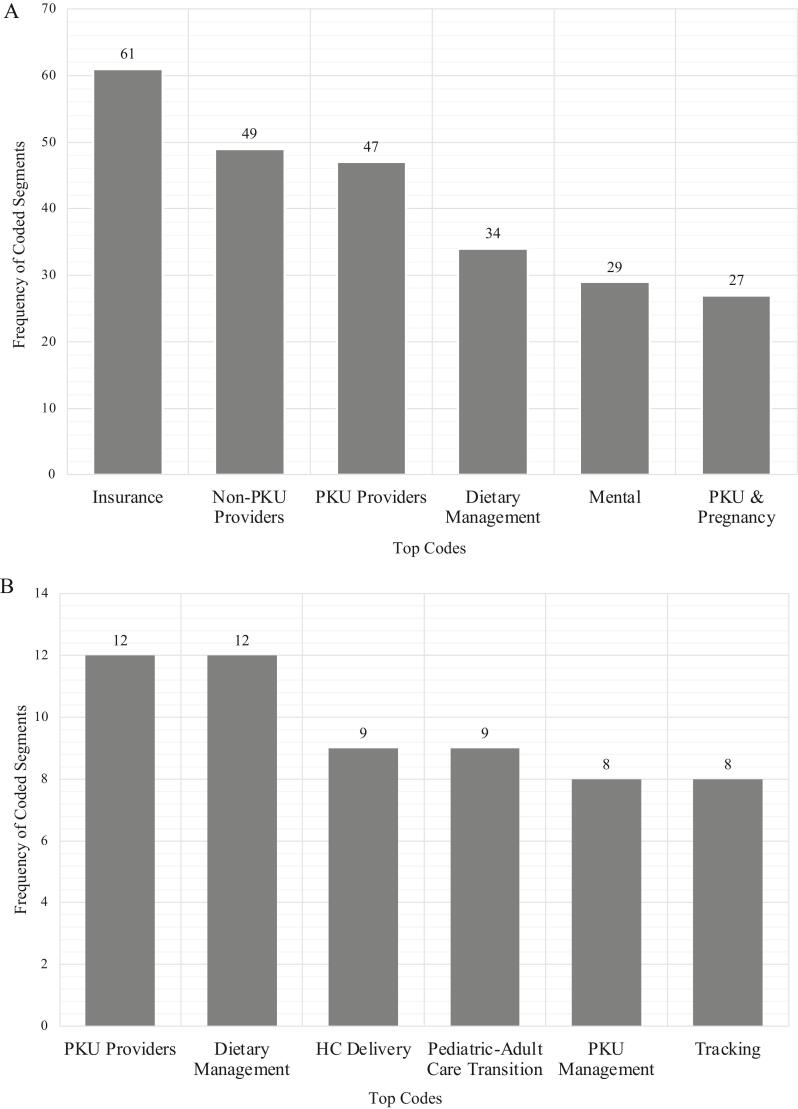
Of the demographic factors, female identity was the most prevalent in participants' lives, as females with PKU have the added burden of considering the risk of maternal PKU syndrome. Of the participants, six had previously been pregnant and two were pregnant at the time of the interview. Of the participants that had never been pregnant, all were deterred from having children, though adolescent participants discussed pregnancy notably less than adult participants (Fig. 2B). Of the concerns related to pregnancy, 58% (n = 11/19) of participants who had never been pregnant stated that they were worried about causing harm to their baby resulting in birth defects, 53% (n = 10/19) stated that they were deterred due to the stricter dietary management needed for pregnancy, 37% (n = 7/19) stated that their fear of pregnancy made them extra cautious with birth control use and sexual encounters, and two participants stated that they were deterred because they did not want to have a child with PKU.
Fig. 2.
A: Most Frequently Coded Segments Across Adult Interviews.
B: Most Frequently Coded Segments Across Adolescent Interviews.
All six participants that had biological children stated that their children were healthy. They talked about the extra monitoring and dietary management that accompanied their pregnancies, but none indicated that they were unable to comply. One participant, who was off diet at the time of her pregnancy, did not know she was pregnant until she was approximately 24 weeks along.
Participants discussed other ways in which their female identity impacted their health, such as others not taking their health concerns seriously. Three participants had brothers with PKU and recounted having had more difficulty in keeping their Phe concentrations within the target therapeutic range, grappling with pregnancy, and getting less medical attention than their siblings. Two participants discussed their struggle with the societal aspect of being a woman and having to maintain their PKU regimen.
3.3.1.2. Knowledge, attitudes, and self-efficacy with health management
Participants had differing attitudes and levels of knowledge related to their overall health management. Six participants expressly stated their extensive knowledge of how to manage PKU, including one adolescent participant. Conversely, one adult participant stated that they had a lack of knowledge about managing their PKU.
Most participants (78%, n = 18/23) had a positive attitude towards their health management. Additionally, 65% (n = 15/23) demonstrated self-efficacy in their ability to manage their diet and their health outside of PKU. Of these participants, 87% (n = 13/15) were adults.
Conversely, 26% (n = 6/23) of participants had a negative attitude towards their health management. Of these participants, 60% (n = 3/6) were adolescents. For most, their negative attitude was due to lack of confidence in their ability to manage their health. These participants indicated that their health was too difficult to manage based on the circumstances of their lives.
3.3.2. Interpersonal factors
3.3.2.1. Interactions with health care providers and their impacts on health management
Among all 25 participants, interactions with health care providers was the most salient interpersonal factor that impacted health management. Within this theme, 23 participants talked about their health care providers independent of their PKU care and 21 discussed their providers relative to their PKU care.
In terms of experiences with health care providers outside of PKU, 61% (n = 14/23) discussed having doctors that were unfamiliar with PKU. Partially due to this, nine of the participants stated that they try to avoid bringing up their diagnosis in appointments.
Six participants had experiences in which providers asked them to educate them on different aspects of PKU management, which caused feelings of unease for some. Further, three participants had a health care provider recommend a dietary change or medication that was not suitable to their dietary treatment.
Participants' accounts of their providers relative to PKU care differed from their accounts of other health care providers in that they had known their PKU provider much longer, most since birth. This theme was one of the most frequently coded segments for adolescents (Fig. 2B), and the third most coded segment across adult interviews (Fig. 2A). A third of participants (n = 7/21) discussed their close relationship with their PKU provider, including 40% of adolescent participants (n = 2/5). Two participants had PKU providers that had previously threatened to drop them from their care when they were noncompliant with their diets – both stated that this “tough love” pushed them to get on track again with their diet.
3.3.2.2. Social support with health management
Most participants (84%, n = 21/25) indicated that social support had an impact on their health management. Some participants discussed support from their friends and families, some from their clinics, and some from other individuals with PKU. The most common source of support mentioned was caregiver support; 67% (n = 14/21) of participants recounted the positive impacts on their health management as they aged, including 60% of adolescents (n = 3/5). Four adult participants also discussed positive social experiences from participating in camps aimed at individuals with rare genetic disorders.
About half (48%, n = 12/25) of participants indicated that they had experienced social issues related to their health management. Some participants indicated that they isolated themselves to avoid social conflict and bullying. Other participants felt isolated because they did not know anyone in their daily lives that also had PKU. Half (n = 6/12) stated that they had experienced bullying because of their diet in their childhood. For some, this had long-term effects into adulthood, such as hiding their diagnosis and avoiding drinking formula in public spaces.
3.3.3. Structural facilitators and inhibitors of health management
3.3.3.1. Insurance and health management costs
Of the structural factors, the most salient theme was insurance coverage, with 22 participants discussing its impact on health management. This was the top coded segment for adults (Fig. 2A), but not one of the notable themes for adolescent participants (Fig. 2B). Although a little more than half (n = 12/22) of participants had satisfactory insurance coverage at the time of the interview, 59% of participants (n = 13/22) had experienced obstacles with insurance coverage. Participants recounted hours of talking to insurance companies on the phone, delays in receiving their medical foods and formulas, and hindrances to their dietary management.
Of those who were dependents under their caregiver's insurance plan, eight participants expressed concern over transitioning to their own insurance plan in adulthood, as they had witnessed the struggles their caregiver had experienced in getting proper coverage, including one adolescent participant.
Most participants also discussed how high costs had served as a barrier for their health management. Of these participants, 80% (n = 12/15) had experienced high costs associated with medical foods, formulas, and pharmacological supplementation, whether or not it was partially covered under their insurance plan. Participants also had difficulties with covering copays for other medical visits and paying for low-protein groceries.
3.3.3.2. Geographical location and access to care
Most participants (64%, n = 16/25) indicated their geographical location as a major factor in their health management. Most participants experienced obstacles related to distance from their clinic. Most of these participants had to travel over an hour to go to their specialty clinic, with some participants having to travel over four hours to reach their clinic. One participant indicated that the rise of telehealth appointments in response to the pandemic made their appointments easier for them. Two participants also discussed how where they live impacts their access to resources: one participant used to live in a state with more coverage for medical foods than where they currently live, and that impacted their ability to pay for their dietary regimen. Another participant lived in a small town at the time of the interview and had experienced access barriers in finding low-protein groceries.
3.3.3.3. Pediatric-adult care transition
Twenty-one participants spoke of the transition from pediatric to adult care and of these participants, 52% (n = 11/21) had transitioned and 48% (n = 10/21) had not. Of those who had transitioned to adult care, 64% (n = 7/11) encountered insurance difficulties with the transition. Of those who had not transitioned to adult care, 60% (n = 6/10) were concerned about insurance difficulties with the transition. Additionally, 40% (n = 4/10) expressed concern over the increased responsibility they would undertake in their health management once transitioned to adult care.
When asked what could be done to improve the pediatric-adult care transition, four participants suggested more education for patients transitioning to adult care through informational classes and discussions with health care providers.
3.3.4. Dietary management of phenylketonuria
The majority of participants (74%, n = 17/23) discussed how their diet impacted the appeal of different foods and formulas. Of these participants, 41% (n = 7/17) expressed craving or having been curious about eating foods that were outside of their dietary regimen. For some, this led to feelings of distress and sadness when they could not eat the food. Conversely, 24% (n = 4/17) of participants found foods outside of their dietary regimen unappealing, as they were accustomed to their diet and did not have the taste for high protein foods.
Ten participants (40%) discussed experiences where there were no dietary options for them, including 60% (n = 3/5) of adolescents. In social settings, this led to feelings of isolation and sadness. Some participants talked about eating at restaurants with friends and family and not being able to eat with everyone else.
Nine participants discussed the extra planning that goes into the management of their diet. Some participants had created a dietary routine for themselves to help them manage their PKU.
Within the routine and planning of PKU management, the most discussed factor was the daily tracking of Phe intake. Of the nine participants who recounted their experience tracking daily Phe intake, 56% (n = 5/9) reported having trouble with consistency and accuracy. For some, this led to annoyance and fatigue.
3.3.5. Pharmacological supplementation
Most participants (72%, n = 18/25) reported having previously taken or currently using pharmacological supplementation for PKU treatment. Of these participants, 28% (n = 5/18) reported taking sapropterin dihydrochloride at the time of the interview, and 33% (n = 6/18) took it previously and stopped treatment. Of the current sapropterin dihydrochloride users, all were responders and developed a higher Phe intake than before the medication.
Of those who previously took sapropterin dihydrochloride and stopped treatment, their reasoning for stopping the medication included not responding to the medication, insurance not covering the pharmaceutical, and wanting a more reactive pharmacological supplement, such as pegvaliase.
At the time of the interview, 39% (n = 7/18) of those who reported using a pharmacological supplement were taking pegvaliase. Two participants reported previously taking pegvaliase and stopping treatment. At the time of the interview, two participants recently started pegvaliase, two had been taking it for over a year and had not experienced effects on their Phe intake, and three developed significant increases in their Phe intake. One participant experienced debilitating joint pain resulting from pegvaliase injections, which made her temporarily stop treatment, and another participant experienced scar tissue buildup at her injection site, which impacted her self-image. The two participants that previously took pegvaliase both stopped treatment after experiencing anaphylactic shock from the injection. One of these participant sustained a fear of trying new medications after this reaction.
3.3.6. Illness intrusiveness of phenylketonuria
The majority of participants (88%, n = 22/25) discussed their diagnosis impacting other realms of their lives. All of these participants reported PKU having some kind of impact on their mental wellbeing. Mental impacts from illness intrusiveness were one of the top coded segments for adult participants (Fig. 2A), but not among adolescents. Most participants experienced depression and anxiety and noticed higher rates when their Phe concentrations were not within their typical range or when they did not have access to their formula. Some had trouble differentiating whether the mental impacts they were experiencing were caused by PKU or something else. Eight participants also experienced neurological impacts because of their PKU management. Of the neurological impacts, forgetfulness and lack of focus were the most frequently mentioned.
In terms of physical health, 78% (n = 17/22) of participants reported an impact from their diagnosis. The most cited impacts were energy levels (n = 8), weight management (n = 5), and joint function (n = 5). Participants stated that when they did not drink enough formula or follow their diet, they had lower energy levels. One participant felt chronically tired and this impacted their social life, as they could not stay up late to socialize with their friends. Of the participants that had difficulty with weight management, most discussed how the dietary needs associated with PKU do not align with a typical weight loss diet; a few tried to find answers through their health care providers and research, but with no success. Other participants discussed how vitamin deficiencies in their diets resulted in joint issues and pains that impacted their ability to maintain physical health.
4. Discussion
This was an exploratory mixed-methods study to understand the health management experiences of adolescent and adult females with PKU. To the best of our knowledge, this is the first study centered on individuals with PKU to utilize the Illness Intrusiveness Ratings Scale (IIRS) survey to better understand how PKU impacts different life domains. Findings from interviews included perceived barriers and facilitators from individual, interpersonal, and environmental levels that impacted health management.
4.1. Maternal PKU
For females with PKU, the possibility of maternal PKU (MPKU) is cause for distress. Our study findings support existing literature in relation to participants expressing concern over maintaining targeted Phe concentrations prior to and during pregnancy, and the risk of causing harm to the baby [5,12]. This concern initiated anxiety for some around sexual encounters, even with the use of comprehensive contraceptive methods. The findings associated with previously pregnant participants supported prior literature, as most discussed the difficulty of maintaining the low Phe diet while pregnant [5]. Social support from the participant's partner and family seemed to have a protective effect on maintaining diet during pregnancy. Future research should further identify protective factors that can sustain dietary management for pregnant females with PKU.
4.2. Knowledge and self-efficacy
Most adolescent participants did not demonstrate self-efficacy and knowledge of their health management, partially because they still depended on their caregivers for their PKU management. This finding is consistent with data from Cazzorla et al. [13] that found most adolescent participants in the study did not know their daily Phe intake recommendations. For this reason, adolescent participants were concerned about the pediatric-adult care transition. Given that previous literature indicates dietary management success decreases with age [13,14], the lack of self-efficacy and knowledge among adolescent participants indicates the importance of increasing autonomy of adolescents in their health management to facilitate care transition. Other literature has proposed system-based interventions, such as transition preparation programs to increase knowledge and self-efficacy among patients amidst the care transition, yet these interventions are more feasible in countries with existing care transition plans, such as Canada and Ireland [15]. Future research should consider interventions that can be implemented in the United States in the absence of a national transition model for individuals with rare diseases.
4.3. Interactions with health care providers
Almost all participants expressed concern over their interactions with health care providers. Most participants felt their health care providers, other than those giving PKU care, were unfamiliar with PKU and this caused distress. Some participants reported being prescribed treatments or medications that were not compatible with their diagnosis. Previous research had similar findings, with patients expressing frustrations with having to educate their providers on their diagnosis [9,16]. When asked what advice they could give to health care providers, most participants expressed a need for their providers to educate themselves. There are a few resources available to medical professionals and students to increase education on rare diseases, notably from the National Organization of Rare Diseases (NORD). NORD offers Continuing Medical Education classes to providers, accredited rare disease education courses, and resources for patients [17]. These resources offer some supplementation to education, yet a restructuring of medical education could be addressed. For example, Jagiellonian University Medical College in Poland successfully instituted a rare disease training program to increase awareness and competency of medical students in treating rare diseases [18]. Future efforts could expand medical training in the United States to utilize these methods and address gaps in rare disease education early on.
4.4. Social issues and support
The social implications of PKU were prevalent among participants. Almost half of participants reported having experienced bullying and social isolation due to their diagnosis. This finding is consistent with previous literature that reported bullying due to dietary treatment among individuals with PKU [16]. The implications of this bullying led some participants to engage in disordered eating, hide formula consumption, and isolate themselves into adulthood. Previous literature has found that social isolation was a factor in adults with PKU being less likely than controls to form normal adult relationships [19]. Conversely, social support, especially caregiver support, was found to be a protective factor among participants in their dietary management. These data indicate the salience of social relationships as serving as a facilitator or inhibitor for health management. Most studies assessing the impact of social support focus on caregivers of children with PKU, so future research should address social support for adult individuals with PKU.
4.5. Insurance and out-of-pocket costs
Most participants had experienced difficulties with affordability of insurance coverage and formulas. Participants who stated they had satisfactory insurance coverage still had issues covering their medical foods and affording out-of-pocket costs associated with PKU. This lack of affordability is a common finding reported in the literature [[20], [21], [22], [23]]. To contextualize the cost, Rose et al. [22] found that, in the United States, the highest annual out-of-pocket costs for families with PKU were attributed to low-protein foods at $1615 for children, and $967 for adults. Further, each state has different coverage policies for dietary treatment through the state, Medicaid, WIC, and other programs [24]. Differential coverage among states was cause for frustration for participants when moving from state to state. Those with private health insurance also may experience difficulties in coverage of medical formula and low-protein foods as their third-party coverage does not have to comply with state mandates [23]. These findings point to an unmet need for financial assistance and coverage for individuals with PKU.
4.6. General health implications
Illness intrusiveness of PKU across various aspects of health was a significant issue for participants. Most participants indicated that their PKU diagnosis and treatment affected their physical, mental, and gynecological health. The most common physical issues caused by PKU were weight management, energy levels, and joint pains. Higher rates of difficulty with weight management and feelings of tiredness among adults with PKU have previously been reported in literature [16]. All participants reported mental implications of PKU, with depression and anxiety being the most common disorders. This finding aligns with literature that found higher rates of depression and anxiety of individuals with PKU compared to the general population [4,16,19,25]. Further, one study found that female subjects with PKU were at a higher risk for depression and anxiety than male subjects with PKU [19]. Future research should assess the causes of higher rates of depression and anxiety among females with PKU, and what can be done to mitigate these disparities.
4.7. Limitations
This study has some limitations in its design and analysis. Across interviews, some interview topics lacked depth, as this was an exploratory study covering a wide range of topics related to health management. Recruitment was done by convenience sampling from Emory University's Metabolic Camp and MNT4P's database, resulting in potential biases among participants regarding their health management, as these are both organizations that promote PKU dietary management. Further, there were differences in perceptions of location and its impact on health, as participants from Metabolic Camp lived across the United States, and enrollees of MNT4P all lived in Georgia. Additionally, there was a lack of racial diversity among participants, inhibiting a representative sample. Future research should qualitatively explore health management of a representative sample of individuals with PKU, at different levels of metabolic control.
5. Conclusion
The findings from this study indicate that females with PKU are significantly impacted by their diagnosis and treatment, and they experience unique challenges in their health management, including those related to mental health outcomes, social relationships, and affordability of health care treatments. Adolescent and adult females with PKU showed differences in perceptions of health management, including within areas related to social relationships, insurance access, and the pediatric-adult care transition. Future research should build on the findings of this study to create targeted interventions aimed at improving the health outcomes for females with PKU.
Funding
This publication was supported by the Southeast Regional Genetics Network (SERN), which is funded by the Health Resources and Services (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $600,000 with 0 % financed with non-governmental sources (5UH7MC30772–06-00). The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement by, HRSA, HHS, or the U.S. Government. For more information, please visit HRSA.gov.
CRediT authorship contribution statement
Abigail Aronoff: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Yue Guan: Writing – review & editing, Supervision. Saran Gurung: Writing – review & editing, Conceptualization. Dawn L. Comeau: Writing – review & editing, Supervision. Rani H. Singh: Supervision, Resources, Funding acquisition.
Declaration of competing interest
Abigail Aronoff, Yue Guan, Saran Gurung, Dawn Comeau, and Rani Singh have no conflicts of interest to report.
Acknowledgements
The authors would like to thank all participants from Emory University's Metabolic Camp and Medical Nutrition Therapy for Prevention who participated in this study, as well as Dr. Teresa Douglas for assisting with recruitment.
Appendix A.
| # | Theme | Quotes |
|---|---|---|
| 1 | Female Identity and Risks Associated with Pregnancy |
“I've always been super cautious about getting pregnant because I knew I wasn't in that range, so I've been religiously on birth control … I had a pregnancy scare when I think I was 19, and that kind of like shocked my, my life. And I'm like, okay, this is, this is a real thing. I gotta get something to protect my child because I know myself and I could not live with the idea of me being the reason that something happened to my child, whether they have to live with a mental disability or they have to live with a physical disability or something.” [Participant #11, 27 years old) “It was extremely difficult to be pregnant with PKU, at least in my experience because I had the taste for all the high protein stuff I wasn't supposed to have and I craved it my entire pregnancy so, so, so bad. But I had to be good.” [Participant #25, 21 years old] “I think also with the physicality of not being able to work out or be super skinny… being a woman is a lot and having PKU surely does not help that. Also, going places as a female on dates and having to explain like, ‘Oh, well, I can't eat that.’ Or being like, ‘Oh no, we can't go there for dinner or things.’ I mean, it impacts so much being a woman and having PKU, there's so much that people don't even think about.” [Participant #22, 30 years old] |
| 2 | Knowledge, Attitudes, and Self-Efficacy with Health Management |
“I feel like [PKU management] is going to get easier because I'll figure out more and more what to do with it, but as of now I'm kind of just figuring everything out.” [Participant #6, 23 years old] “I can assure you, I [was] the only 6-year-old thinking about, ‘Oh, these French fries probably have X amount of protein. That's my protein for the day.’ So, I think I've always been pretty good at like managing my own health. It's been so instilled in me growing up. It's been so important to manage.” [Participant #15, 19 years old] “Having to deal with PKU … you have to put in your a hundred percent, but I don't do that because that a hundred percent is too much for me.” [Participant #2, 15 years old] |
| 3 | Interactions with Health Care Providers and Their Impacts on Health Management |
“She knew what PKU was, like the name, but she did not know the specifics of like, what enzyme I'm missing, all that fun stuff. I usually explain it to them, but it is kind of nerve-wracking having to explain your own problems to the doctor.” [Participant #4, 19 years old] “There was this one time that I had a dietitian… and she suggested for me to start eating meat to get more protein and I was like, ‘No, that is a very bad idea.’” [Participant #1, 16 years old] “I love [my doctor]. If I had the choice of if I got [PKU] or not, I would get it just to meet [my doctor]. She is so freaking sweet. I love her. I, I don't want another doctor, like, hell no, I can't switch doctors. [My doctor] is my only one.” [Participant #11, 21 years old] |
| 4 | Social Support with Health Management |
“If you're able to find Facebook groups or this camp, for example, that's very helpful. Coming somewhere where it's so normal or being surrounded by people where it's normal, having that sense of normalcy and inclusion really helps.” [Participant #12, 24 years old] “I remember spilling my formula on the carpet one day in third grade, and people – because it doesn't smell pleasant – but people were like, ‘Ew, what is that?’ Stuff like that has kind of stuck with me my whole life, and I've had to work through some issues. So, I would say the hardest thing was incidents like that caused trauma that I struggle with.” [Participant #15, 19 years old] |
| 5 | Insurance and Health Management Costs |
“One insurance that I did get it covered, it was covering both my regular doctor and my [PKU] doctor, but then it wouldn't cover the medication, so that was a roadblock in itself, because I can survive without going to the doctor, but I can't survive without the [sapropterin dichloride], because I'm already eating this much protein. I'm used to it.” [Participant #14, 23 years old] “[Sapropterin dichloride was] about a thousand dollars a bottle. I think I was taking 14 pills a day and that really won't last you long.” [Participant #14, 23 years old] |
| 6 | Geographical Location and Access to Care | “I've got friends in Canada who have PKU and they're like, ‘We get a stipend every month for food and we get formula covered, you need to come here.’ And I have been so close so many times.” [Participant #22, 30 years old] |
| 7 | Pediatric-Adult Care Transition |
“I'm really scared of anything adult-related with healthcare, because I like to go to my appointments alone and I like to schedule them myself, but the whole idea of just dealing with it, but they expect me to be an adult about it is kind of something that I'm not used to.” (Participant #24, 18 years old] “You know how [genetic clinic] has the informational classes? Maybe something like this is what you need to do when you need to get insurance for your medicine, or your formula or food, or send out like brochures for the food because I don't know where to look.” [Participant #6, 23 years old] |
| 8 | Dietary Management of Phenylketonuria |
“The diet's easy enough because, at this point in my life, I don't want a lot of meat, seems a little gross, quite honestly. Makes it easy.” [Participant #16, 24 years old] “You have to wait to eat till you get home, so then you're sitting there not eating and it's like, well, this sucks.” [Participant #5, 18 years old] “I've even implemented some changes that have helped me. I put all of my PKU supplies in one drawer in my kitchen; I have my lancets, I have my filter papers, I have a pen, I have envelopes, I have all my Palynziq stuff. It's very accessible, very easy.” [Participant #12, 24 years old] “It's physically exhausting for me, like I don't want to do it. I get so annoyed that I have to weigh my food and do this and that, that I'm like, I'm just not going to eat right now.” [Participant #2, 15 years old] |
| 9 | Pharmacological Supplementation |
“And that's like – because on Kuvan I can have like triple what I normally have, like quadruple what I normally have almost.” “As soon as I injected myself, then since I was already panicking, my blood was already pumping, it moved quickly. So as soon as I felt my throat tighten up, then my whole body like went into a muscle spasm, like my whole, every muscle in my body tightened up, and I don't know if you ever had a Charley horse in your calf? Like that's what my entire body felt like.” |
| 10 | Illness Intrusiveness of Phenylketonuria |
“If I'm just having a really rough time with my mental health, I'm also having a really rough time with my PKU. They go hand-in-hand. It's a double-edged sword.” [Participant #12, 24 years old] “It's almost like having two different health systems in my body, like I have the PKU health that does its own thing and causes issues, but those issues can overlap into my normal body health. It's like having two bodies in one that have completely different systems. It's stressful because before I found [my doctor], a lot of times my health issues would overlap and so I couldn't decipher them and no one else could.” [Participant #10, 27 years old] |
Data availability
The data that has been used is confidential.
References
- 1.Van Spronsen F.J., Blau N., Harding C., Burlina A., Longo N., Bosch A.M. Phenylketonuria. Nat. Rev. Dis. Primers. 2021;7:36. doi: 10.1038/s41572-021-00267-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barta A.G., Sumánszki C., Turgonyi Z., Kiss E., Simon E., Serfőző C., et al. Health related quality of life assessment among early-treated Hungarian adult PKU patients using the PKU-QOL adult questionnaire. Mol. Genet. Metab. Rep. 2020;23 doi: 10.1016/j.ymgmr.2020.100589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vockley J., Andersson H.C., Antshel K.M., Braverman N.E., Burton B.K., Frazier D.M., et al. Phenylalanine hydroxylase deficiency: diagnosis and management guideline. Genet. Med. 2014;16:188–200. doi: 10.1038/gim.2013.157. [DOI] [PubMed] [Google Scholar]
- 4.Huijbregts S.C.J., Bosch A.M., Simons Q.A., Jahja R., Brouwers M.C.G.J., De Sonneville L.M.J., et al. The impact of metabolic control and tetrahydrobiopterin treatment on health related quality of life of patients with early-treated phenylketonuria: a PKU-COBESO study. Mol. Genet. Metab. 2018;125:96–103. doi: 10.1016/j.ymgme.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Ford S., O’Driscoll M., MacDonald A. Reproductive experience of women living with phenylketonuria. Mol. Genet. Metab. Rep. 2018;17:64–68. doi: 10.1016/j.ymgmr.2018.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rohde C., Thiele A.G., Baerwald C., Ascherl R.G., Lier D., Och U., et al. Preventing maternal phenylketonuria (PKU) syndrome: important factors to achieve good metabolic control throughout pregnancy. Orphanet J. Rare Dis. 2021;16:477. doi: 10.1186/s13023-021-02108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gama M.I., Pinto A., Daly A., Rocha J.C., MacDonald A. The impact of the quality of nutrition and lifestyle in the reproductive years of women with PKU on the long-term health of their children. Nutrients. 2022;14:1021. doi: 10.3390/nu14051021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Von Der Lippe C., Diesen P.S., Feragen K.B. Living with a rare disorder: a systematic review of the qualitative literature. Mol. Genet. Genomic Med. 2017;5:758–773. doi: 10.1002/mgg3.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ford S., O’Driscoll M., MacDonald A. Prescribing issues experienced by people living with phenylketonuria in the UK. Mol. Genet. Metab. Rep. 2019;21 doi: 10.1016/j.ymgmr.2019.100527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uhlenbusch N., Löwe B., Depping M.K. Perceived burden in dealing with different rare diseases: a qualitative focus group study. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2019-033353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devins G.M. Using the illness intrusiveness ratings scale to understand health-related quality of life in chronic disease. J. Psychosom. Res. 2010;68:591–602. doi: 10.1016/j.jpsychores.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 12.Roberts R.M., Muller T., Sweeney A., Bratkovic D., Gannoni A. Promoting psychological well-being in women with phenylketonuria: pregnancy-related stresses, coping strategies and supports. Mol. Genet. Metab. Rep. 2014;1:148–157. doi: 10.1016/j.ymgmr.2014.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cazzorla C., Bensi G., Biasucci G., Leuzzi V., Manti F., Musumeci A., et al. Living with phenylketonuria in adulthood: the PKU ATTITUDE study. Mol. Genet. Metab. Rep. 2018;16:39–45. doi: 10.1016/j.ymgmr.2018.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Medford E., Hare D.J., Wittkowski A. In: Demographic and Psychosocial Influences on Treatment Adherence for Children and Adolescents with PKU: A Systematic Review. Morava E., Baumgartner M., Patterson M., Rahman S., Zschocke J., Peters V., editors. vol. 39. Springer Berlin Heidelberg; Berlin, Heidelberg: 2017. pp. 107–116. JIMD Rep. Vol. 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sandquist M., Davenport T., Monaco J., Lyon M. The transition to adulthood for youth living with rare diseases. Children. 2022;9:710. doi: 10.3390/children9050710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ford S., O’Driscoll M., MacDonald A. Living with phenylketonuria: lessons from the PKU community. Mol. Genet. Metab. Rep. 2018;17:57–63. doi: 10.1016/j.ymgmr.2018.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Organization of Rare Diseases (NORD) Rare Disease Continuing Medical Education (CME) Video Library. Natl Organ Rare Dis NORD. https://rarediseases.org/cme-video-library/ n.d. (accessed February 26, 2024)
- 18.Kopeć G., Podolec P. Establishing a curriculum on rare diseases for medical students. J. Rare Cardiovasc. Dis. 2015:2. doi: 10.20418/jrcd.vol2no3.194. [DOI] [Google Scholar]
- 19.Gentile J.K., Ten Hoedt A.E., Bosch A.M. Psychosocial aspects of PKU: hidden disabilities – a review. Mol. Genet. Metab. 2010;99:S64–S67. doi: 10.1016/j.ymgme.2009.10.183. [DOI] [PubMed] [Google Scholar]
- 20.Therrell B.L., Lloyd-Puryear M.A., Camp K.M., Mann M.Y. Inborn errors of metabolism identified via newborn screening: ten-year incidence data and costs of nutritional interventions for research agenda planning. Mol. Genet. Metab. 2014;113:14–26. doi: 10.1016/j.ymgme.2014.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coakley K.E., Porter-Bolton S., Salvatore M.L., Blair R.B., Singh R.H. Food insecurity in females with phenylketonuria. JIMD Rep. 2020;53:103–110. doi: 10.1002/jmd2.12115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rose A.M., Grosse S.D., Garcia S.P., Bach J., Kleyn M., Simon N.-J.E., et al. The financial and time burden associated with phenylketonuria treatment in the United States. Mol. Genet. Metab. Rep. 2019;21 doi: 10.1016/j.ymgmr.2019.100523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berry S.A., Brown C., Grant M., Greene C.L., Jurecki E., Koch J., et al. Newborn screening 50 years later: access issues faced by adults with PKU. Genet. Med. 2013;15:591–599. doi: 10.1038/gim.2013.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilson K., Charmchi P., Dworetzky B. State statutes & regulations on dietary treatment of disorders identified through newborn screening. Catal. Center. 2016:1–80. [Google Scholar]
- 25.Jahja R., Huijbregts S.C.J., De Sonneville L.M.J., Van Der Meere J.J., Legemaat A.M., Bosch A.M., et al. Cognitive profile and mental health in adult phenylketonuria: a PKU-COBESO study. Neuropsychology. 2017;31:437–447. doi: 10.1037/neu0000358. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that has been used is confidential.