Abstract
Introduction and importance:
Psoas abscess is a relatively uncommon condition that can present with vague clinical features. Patients with this condition often present in different ways to different specialties leading to delays in diagnosis and management.
Case presentation:
The authors present a 47-year-old woman with complaint of vague abdominal pain, fever, and raised inflammatory markers who underwent CT examination. On CT, a collection was noted in the right iliac fossa that extended along the right retroperitoneum through the retrocrural space in the right lung base communicating with a cavitary pulmonary lesion with air-fluid level. The psoas abscess was drained.
Clinical discussion:
Our case presents a number of rare and intriguing features. Notably, the patient, who was immunocompetent, experienced a primary Staphylococcus infection that swiftly progressed to a sizable pulmonary abscess, a phenomenon uncommon in such hosts. The rarity further extends to the source of infection, originating abdominally but culminating in thoracic complications through contiguous spread from a retroperitoneal site. Despite the potential severity, the patient’s outcome was remarkably positive
Conclusion:
This case underscores the potential rapidity of pulmonary involvement in psoas abscesses, emphasizing the need for heightened awareness and consideration of respiratory signs during preoperative assessments
Keywords: anesthesia, fistulization, hypoxemia, lung abscess, psoas abscess
Introduction
Highlights
The case describes a rare complication of a large lung abscess resulting from a psoas abscess.
The patient’s initial symptoms consisting of lower back pain, fever, and weight loss, followed by bronchitis and a right basal alveolar syndrome, are highlighted as key clinical features associated with this rare presentation.
The report underscores the challenges in diagnosing psoas abscesses due to their vague clinical features, and the crucial role of CT imaging.
The case details challenges faced during anesthesia, including desaturation and airway complications.
The postoperative follow-up and diagnostic imaging provided insights into the progression of the infection.
Despite the rare and serious nature of the case, the patient had an excellent outcome, contributing to the understanding of successful management strategies.
Lung abscess is most commonly caused by lung parenchymal disease. However, it can develop from hematogenous dissemination, direct spread from the mediastinum, and rarely from the abdominal cavity1. In the absence of an intrathoracic pathology, an intra-abdominal cause should be considered2.
Psoas abscess is a relatively uncommon condition that can present with vague clinical features. Psoas abscess is classified as primary or secondary, is thought to be involved in 5–10% of abdominal suppurations3.
The main objective of this study is to present an extremely rare case of large lung abscess that spread from a psoas abscess and to review the challenges concerned with diagnosis.
Patient and observation
Patient information
A 47-year-old female patient with no medical history was admitted to the operating room for the surgical drainage of an iliopsoas abscess.
Clinical findings
The patient’s history started 2 months before her admission when she complained of lower back pain, with localized inflammatory signs, fever, and a weight loss estimated at 8 kg. She seeked medical attention twice and received oral antibiotics and analgesia. As her clinical condition did not improve, she was admitted to the emergency department of the university hospital where an abdominal ultrasound showed a right iliopsoas abscess, confirmed by a thoraco-abdominopelvic CT scan (Fig. 1). The abscess was extending from 10th thoracic vertebra to the second lumbar vertebra and measuring 75 mm in its long axis, thoracic CT showed minimal condensation at the right lung basis. The patient was started on IV Ceftriaxone and Metronidazole, with surgical removal of the abscess programmed 2 days later.
Figure 1.
Preoperative CT scan imaging showing a psoas abscess measuring 75 mm in its long axis, with minial condensation at the right lung basis.
Anesthesia evaluation showed a conscious patient with a temperature 38.5°C, a blood pressure of 120/60 mmHg, heart rate of 90 bpm, respiratory rate of 14 cycles per minute and SpO2 at 96% on room air. Lung auscultation showed bilateral rhonchi and the airway examination showed no difficult intubation or ventilation criteria. Chest radiograph showed a basal right alveolar syndrome. Patient’s biology showed leukocytosis with Neutrophils at 23 000/mcl and CRP at 260 mg/l, Natremia at 140 mmol/l, and a normal renal function.
Therapeutic interventions
Patient was admitted to the operating room and it was decided the intervention would be conducted under general anesthesia because the patient was septic, and infection was contiguous to the lumber region. The patient was preoxygenated with a FiO2 at 1 for 3 min then induction of anesthesia was performed with fentanyl, propofol, and rocuronium. Patient was manually ventilated using an airway pressure of 20 cmH2O. Upon laryngoscopy the patient presented a desaturation at 80%, the laryngoscopic view showed a Cormack 1 grade with pus coming out of the vocal cords. The pus was aspirated, the patient was subsequently intubated with no difficulty and then received lung protective ventilation with a tidal volume of 8 ml/kg, PEEP at 10, and FiO2 at 0.5 titrated to a SpO2 of 90–92%. The patient had elevated peak airway pressures at 40 at Plateau pressure of 22, and required numerous tracheal aspirations as pus was abundantly coming out of the endotracheal tube. The arterial blood gaz showed a PaO2 to FiO2 ratio at 160. Surgery lasted 2 h and consisted of the abscess drainage with two Delbet blades, samples from the abscess and a distal protected sample from the trachea were sent for bacteriological analysis.
Follow-up and outcome of interventions
At the end of the surgery, the patient was kept intubated and sedated, then taken to the CT scan for etiologic diagnosis. The thoracic CT scan showed a right basal abscess, communicating with the iliopsoas abscess that extended to the vertebrae, and septic emboli on both lungs (Fig. 2). Patient was admitted to the ICU; the diagnostic work up was completed with blood cultures isolating a staphylococcus aureus. Tuberculosis GeneXpert testing, viral serologies and a heart ultrasound showing only minimal pericardial effusion. Bacteriological studies showed a methicillin resistant staphylococcus aureus, and the patient was started on vancomycin.
Figure 2.
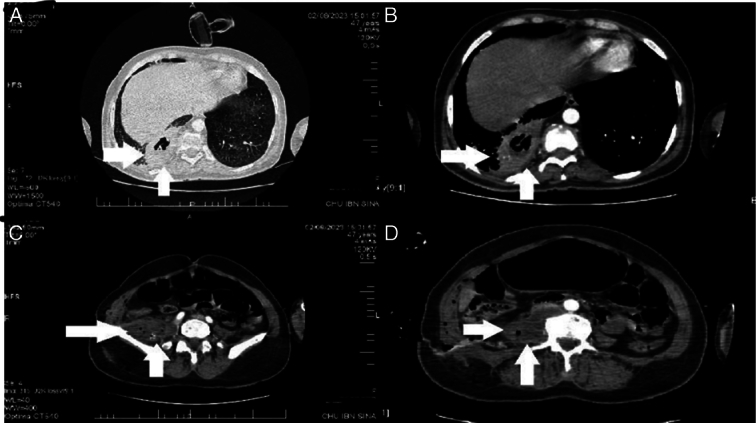
Postoperative CT scan imaging showing a psoas abscess, with right lung fistulization:. A. Parenchymal window of a cross-sectional image of thoracic CT illustrating fistulization of psoas abscess into pulmonary parenchyma. B. Mediastinal window of a cross-sectional image of thoracic CT illustrating fistulization of psoas abscess into pulmonary parenchyma. C. Pelvic CT scan revealing a right paravertebral hypodense collection measuring 75 mm in its long axis, accompanied by pubic osteitis. D. Abdominal CT scan demonstrating a right paravertebral hypodense collection containing air bubbles, with enhanced wall after contrast agent injection.
The patient received 3 days of pressure support ventilation, chest physiotherapy and tracheal aspirations, and progressively improved her oxygenation and respiratory mechanics. She was extubated on day 4 and stayed two additional days in the ICU before transfer to the pneumology department.
Discussion
This work has been reported in line with the Surgical CAse REport (SCARE) Criteria3.
Psoas abscesses, uncommon but not exceptional, are most often monomicrobial and are thought to be involved in 5–10% of abdominal suppurations4. Psoas abscess is classified as primary or secondary. A primary abscess occurs due to hematogenous or lymphatic spread of the causative organism from a distant site. Secondary abscesses occur as a result of direct expansion of a nearby infectious or inflammatory process into the psoas muscle5. Primary abscesses occur most often in patients with a history of diabetes, injection drug use, alcoholism, AIDS, renal failure, hematological malignancies, immunosuppression, or malnutrition6. Clinical signs of psoas abscess are not very specific. The diagnosis is determined by a prolonged infectious state associated with febrile back pain (pyogenic abscess) or not (cold abscess) and psoitis. In the majority of cases, a biological inflammatory syndrome (elevated CRP, VS, and leukocytes) is present, but is generally of little help in the diagnosis7. Positive diagnosis of abscesses is made radiologically. CT has a very high sensitivity (around 100%). It can be used to determine the extent of the abscess, to detect an underlying lesion, to guide puncture for microbiological analysis in order to realize the etiologic diagnosis, and to guide the placement of a drain for therapeutic purposes8.
Staphylococcus is the most common germ implicated in primary psoas abscesses (90% of cases), followed by streptococci (5%) and Escherichia coli (3%)5,6. Other germs rarely implicated in primary psoas abscesses include Brucella sp and Mycobacterium tuberculosis complex9.
Pulmonary abscess is a cavitary lesion containing necrotic lung tissue or an infected fluid component. It is most often caused by disease of the lung parenchyma. However, it can rarely develop from an intra-abdominal focus1. The retrocrural space connects the thoracic cavity to the retroperitoneum. This fact, combined with the different pressures between the thorax and abdomen and the direction of lymphatic flow, explains the development of pulmonary abscess following abdominal infection10.
Our case presents several rare and interesting features: the immunocompetent host, the primary type, the Staphylococcus infection, the rapid development to pulmonary abscess (involvement), the large size of the abscess, and the excellent outcome of the patient. A pulmonary empyema or abscess caused by an abdominal infection is a rare entity. However, when a retroperitoneal infection is established, it may eventually compromise the thoracic cavity by contiguous spread. After a review of the literature, we found few reports of rare cases complicated by pulmonary abscess/ empyema and iliopsoas abscess (Table 1).
Table 1.
Comparaison between cases with psoas abscess
| Reporter | Age (years) | Sex | Primary disease | Causative bacteria | Treatment | Outcome |
|---|---|---|---|---|---|---|
| Present case | 47 | Female | None | staphylococcus aureus | Operation Antibiotics Drainage | Transfer |
| Sakurai et al.11 | 80 | Male | None | Streptococcus intermedius | Antibiotics Drainage | Transfer |
| Liu et al.12 | 48 | Male | Diabetes | Streptococcus milleri | Operation Antibiotics Drainage | Discharge |
| Ito and Miura13 | 78 | Male | Diabetes | Negative | Antibiotics Drainage | Discharge |
Conclusion
Iliopsoas abscess is a rare entity, most often a monobacterial infection in the retroperitoneal space, that can rapidly involve the lungs by spreading through the retrocrural space. The presence of a pulmonary abscess must be considered during the preoperative evaluation of patients with a psoas access and respiratory signs, as thoracic involvement can be very quick and life-threatening respiratory complications can occur.
What is already known about it:
Psoas abscesses are most often a mono microbial infection developing primarily as hematogenous dissemination from a distant site or secondarily to a contiguous infection. The retroperitoneal infection may compromise the thoracic cavity and develop as a pulmonary abscess.
The anesthetic management of a psoas abcess drainage involves general anesthesia rather than spinal anesthesia because of the risk of infection dissemination to the intrathecal space.
What this study provides:
The pulmonary involvement in psoas abcesses can be very fast, and the presence of respiratory signs must prompt further investigation to anticipate respiratory complications.
The presence of a pulmonary abscess must be considered during the preoperative evaluation of a psoas abcess drainage in a patient with respiratory signs.
Limits of this study:
The rarity of our case limits the generalization of our findings.
While out comparison table is useful for highlighting the uniqueness of our case, the limited number of similar cases could be insufficient for drawing robust conclusions about the characteristics and outcomes of similar cases.
Lack of long-term follow-up.
Ethical approval
This is a case report talking about a rare situation but derived from ‘standard’ clinical practice so an ethics board approval was not required.
Consent
Written informed consent was obtained from the patient for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
Not applicable.
Author contribution
Z.S.: writing the paper (Original draft); H.Z.: writing the paper (Final version); I.E. and A.E.: data collection; S.C. and A.C.: proofreading; H.E. and A.C.: internal review; M.A. and A.B.: contributors; M.A. and A.A.: supervision.
Conflicts of interest disclosure
The authors declare no competing interest.
Research registration unique identifying number (UIN)
Not applicable.
Guarantor
Dr Ziani Hicham is the guarantor of this case report.
Data availability statement
Not applicable.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 19 April 2024
Contributor Information
Hicham Ziani, Email: drzianih@gmail.com.
Imane Elazzouzi, Email: drelazzouziimane@gmail.com.
Amine Chibani, Email: chibaniamine92@gmail.com.
Manal Arfaoui, Email: dr.arfaouimanal@gmail.com.
Abdelkader Benhlima, Email: abdel.benhlima@gmail.com.
Hamza Elhamzaoui, Email: elhamzaouihamza6@gmail.com.
Mustapha Alilou, Email: aliloumust@yahoo.fr.
Salim Chajai, Email: Salimchajai@gmail.com.
Amine Eddouali, Email: eddouali.amine@gmail.com.
Zakariae Slaihi, Email: z.slaihi@gmail.com.
Ahlam Chaieri, Email: ahlamc19@gmail.com.
Almahdi Awab, Email: mahdiawab@gmail.com.
References
- 1. Kuhajda I, Zarogoulidis K, Tsirgogianni K, et al. Abcès pulmonaire-étiologie, options de diagnostic et de traitement. Ann Transl Med 2015;3:183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dietrich A, Nicolas M, Iniesta J, et al. Empyema and lung abscess as complication of a perforated appendicitis in a pregnant woman. Int J Surg Case Rep 2012;3:622–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sohrabi C, Mathew G, Maria N, et al. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl 2023;109:1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Conde Redondo C, Estebanez Zarranz J, Rodrigues Toves A, et al. Traitement de l’abcès du psoas: drainage percutané ou chirurgie ouverte. Prog Urol 2000;10:418–423. [PubMed] [Google Scholar]
- 5. Shields D, Robinson P, Crowley TP. Abcès iliopsoas – revue et mise à jour de la littérature. Int J Surg 2012;10:466–469. [DOI] [PubMed] [Google Scholar]
- 6. Mallick IH, Thoufeeq MH, Rajendran TP. Abcès du psoas-iliaque. Postgrad Med J 2004;80:459–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Masso-Misse P, Yao GS, Essomba A, et al. Abcès primaires du psoas. Affection courante en milieu tropical. A propos de 87 cas. J Chir (Paris) 1994;131:201–204. [PubMed] [Google Scholar]
- 8. Malthora R, Singh KD, Bhan S, et al. Primary pyogenic abcess of the psoas muscle. J Bone Joint Surg Am 1992;74:278–284. [PubMed] [Google Scholar]
- 9. Cubukcu S, Gurbuz U, Çevilkol C, et al. Primary psoas abscess presented with only low back pain. Turk J Phys Med Rehab 2006;52:137–140. [Google Scholar]
- 10. Panicek DM, Benson CB, Gottlieb RH, et al. Le diaphragme : considérations anatomiques, pathologiques et radiologiques. RadioGraphiques 1988;8:28–29. [Google Scholar]
- 11. Sakurai M, Nagasawa H, Takeuchi I, et al. A case of an 80-year-old man with empyema and psoas abscess. Case Rep Emerg Med 2020;2020:8895785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Liu L, Goh ZW, Rhodes B. Empyema and psoas abscess in a previously undiagnosed diabetic patient. J N Zeal Med Assoc 2013;126:78–106. [PubMed] [Google Scholar]
- 13. Ito I, Miura A. A case of type 2 diabetes mellitus complicated with left iliopsoas abscess caused by a left femoral vein catheter during treatment for right pyothorax and right subphrenic abscess. Nihon. Ronen Igakkai zasshi Japanese J Geriatrics 2011;48:180–184. doi: 10.3143/geriatrics.48.180 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


