Abstract
Penile tissue death caused by impaired blood flow and nerve damage is a severe but uncommon complication of diabetes mellitus known as diabetic penile necrosis. Diabetes related vascular and neurological issues result in reduced sensation and limited blood supply to the penis leading to this condition. The consequences on sexual function and quality of life are catastrophic though it's rare, hence early identification, treatment intervention cannot be over emphasized since they help prevent further deterioration including infections that arise from complications occasioned by delayed management.
Keywords: Penile gangrene, Diabetes mellitus, Dry gangrene
1. Introduction
Penile gangrene caused by insufficient blood supply, also known as ischemic penile gangrene, is a urologic condition that is infrequently studied and results in significant negative health outcomes. Diabetes mellitus, renal insufficiency, paraphimosis, prapism, Tourniquet syndrome,hindrance of venous outlet flow, and intravenous drug usage have all been linked to the development of this rare disease.1, 2, 3
Ischemic gangrene may also be caused by various factors, including penile prosthesis implantation, circumcision complications, acute arterial obstruction, Fournier gangrene syndrome, and incidents such as spider bites and bodily trauma. In addition to these causes, there are others that can result in ischemic gangrene.4
The etiology of penile necrosis holds no bearing on its severity, as it is a critical condition that could result in severe consequences like penis loss. It necessitates immediate and urgent treatment."
2. Case history
Upon arrival at the emergency department, a retired accountant aged 67 with uncontrolled diabetes requiring insulin was observed to have developed dark discoloration of his penile skin with loss of sensitivity; however, the glans remained unaffected. Additionally, he experienced difficulty with urination as well. These symptoms had been persistent for ten days leading up to his visit due to an inherent fear of hospitals or nosocomephobia that made it hard for him to initially reach out for medical assistance.
Despite struggling with poorly managed diabetes, he had no other medical conditions such as renal disease, atherosclerotic disease, or vasculopathy. Additionally, he denied any history of smoking and/or illicit drug abuse.
During the physical examination, a penis that was slightly black and unresponsive (Fig. 1) was observed. The blood count and chemistry tests did not reveal anything noteworthy. His hemoglobin A1C level was measured at 10. He displayed no indication of uncontrolled hypertension or smoking habits. He also tested negative for illicit drug use after undergoing a random urine screening test.
Fig. 1.
Isolated ischemia of the penile.
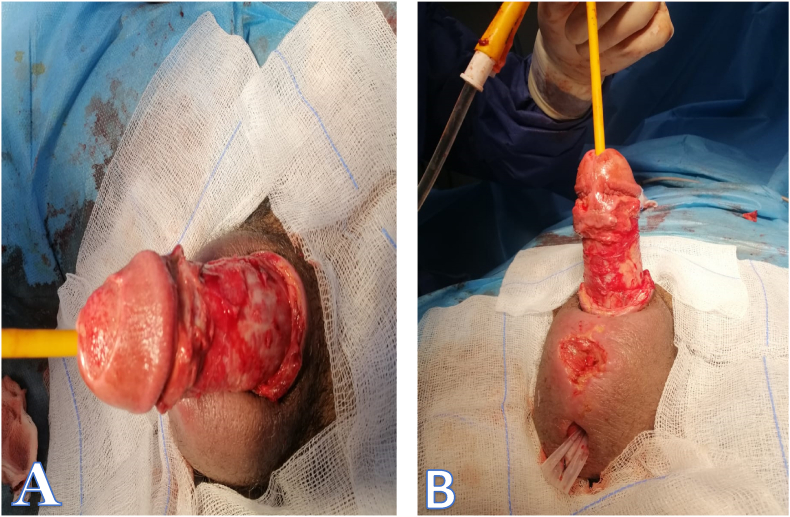
Surgical management of the patient included vesical catheter placement for urinary diversion and sequential debridement of the wound (Fig. 2). During surgery, it was observed that only penile skin had necrosis, while corpora cavernosa and glans were unaffected.
Fig. .2.
(A,B) Postoperative image showing sequential debridement of the wound, corpora cavernosa and glans were unaffected.
The cystoscopy revealed that both the anterior and posterior urethra were unaffected.
The examination of the removed tissue showed that there was dead and decaying tissue present.
The bladder catheter was removed 1 day after debridement as there was no urethral lesion.
The patient's condition remained stable, and they were allowed to leave.
After four weeks of debridement, we scheduled a reconstruction using a pedicled scrotal flap.
The patient received a 10-day course of prophylactic amoxicillin to prevent infection.
The patient was seen weekly for wound monitoring, which included regular observation to detect signs of infection or graft rejection and to assess the healing process. Additionally, dressing changes were performed to ensure proper wound care and promote healing.
3. Discussion
There are various kinds of gangrene, including dry gangrene, wet gangrene, and gas gangrene. The case in question showcases dry or ischemic gangrenes, which are commonly connected with uncontrolled diabetes. It has been proven that inadequately managed hypertension and diabetes often lead to instances of dry necrosis since end-stage renal disease causes calciphylaxis within the small arteries, resulting in tissue ischemia and ultimately causing its demise.3
Penile dry gangrene is a perilous condition resulting from inadequate blood supply to the penis, ultimately leading to tissue necrosis. This affliction typically arises as an offshoot of circulation-linked illnesses like diabetes mellitus that give rise to peripheral artery disease (PAD) and peripheral neuropathy—conditions characterized by impaired sensitivity and diminished flow in various body extremities, including the penis, among other areas.
Over time, diabetics with elevated blood sugar levels may experience nerve and blood vessel damage that constricts arteries and limits the flow of blood to the penis. This can cause penile tissue to become malnourished and oxygen-deprived, ultimately leading to its death through a condition referred to as gangrene. Dry gangrene brings about characteristic symptoms such as shriveling, darkening skin tone, and the overall desiccation of affected areas.
The diagnosis and treatment of penile dry gangrene rely mainly on anecdotal information. To evaluate penis vasculogenic necrosis, medical history and physical examination are the primary methods utilized. Penile angiography and ultrasound have been infrequently reported as being used in some cases.
Usually, dry penile necrosis is handled conservatively by either permitting autoamputation or undergoing surgery with serial wound debridements.4 As far as we know, there have been no instances of endovascular methods for penile revascularization specifically used to treat dry penile gangrene. Yet, angioplasty has proven to be a viable and secure option in certain cases.5 If performed earlier during the disease process, similar approaches using endovascular procedures may aid in safeguarding glans tissue and averting ischemia.
4. Conclusion
Although rare, dry gangrene of the penis can lead to severe consequences. It is crucial to distinguish between wet and dry types of gangrene and apply broad-spectrum antibiotics promptly. In situations where a patient has wet gangrene, removing the infected area via debridement may be necessary, or even amputation could be required for penile cases specifically. Conversely, if there are no signs indicating an infection, if it's found out that it’s a case of dry gangrene, conservative follow-up measures can suffice as treatment options.
5. Author agreements
All authors have read and approved the contents of this article for publication.
Ethics approval and consent to participate
The ethics committee of the Faculty of Medicine of Rabat has given us its agreement. Informed and verbal consent to participate in the study was provided by our patients. The reference number is not applicable.
Founding
Not applicable.
CRediT authorship contribution statement
Youssef Maachi: Writing – review & editing, Writing – original draft, Software, Resources, Data curation, Conceptualization. Jaafar Fouimtizi: Data curation. mouftah Babty: Formal analysis. amine slaoui: Resources. Tariq karmouni: Validation. Khalid El Khader: Validation. Abdellatif Koutani: Validation. Ahmed Iben Attya Andaloussi: Validation.
Declaration of Competing interest
There is no conflict of interest between the authors of this work.
Acknowledgements
Not applicable.
Contributor Information
Youssef Maachi, Email: ucef777@gmail.com.
mouftah Babty, Email: MouftahBabty@gmail.com.
References
- 1.Raman S.R., Kate V., Ananthakrishnan N. Coital paraphimosis causing penile necrosis. Emerg Med J. 2008;25(7):454. doi: 10.1136/emj.2007.054601. [DOI] [PubMed] [Google Scholar]
- 2.Kharbach Y., Tenkorang K., Bouchikhi A., et al. Elective gangrene of the corpus spongiosum of idiopathic origin: a case report. Can Urol Assoc J. 2014;8(11–12):E934–E937. doi: 10.5489/cuaj.2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haider I., Siddiqui M., Naji W., Sheikh M., Waqar A. Calciphylaxis leading to penile necrosis. J Pakistan Med Assoc. 2014;64(6):711–713. [PubMed] [Google Scholar]
- 4.Chiang I.N., Chang S.J., Kuo Y.C., Liu S.P., Yu H.J., Hsieh J.T. Management of ischemic penile gangrene: prompt partial penectomy and other treatment options. J Sex Med. 2008;5(11):2725–2733. doi: 10.1111/j.1743-6109.2008.00894.x. [DOI] [PubMed] [Google Scholar]
- 5.Wang T.D., Lee W.J., Yang S.C., et al. Clinical and imaging outcomes up to 1 year following balloon angioplasty for isolated penile artery stenoses in patients with erectile dysfunction: the PERFECT-2 study. J Endovasc Ther. 2016;23(6):867–877. doi: 10.1177/1526602816669337. [DOI] [PubMed] [Google Scholar]